Abstract
Background: Disparities in obesity-promoting feeding patterns begin in pregnancy and infancy, underscoring the need for early primary prevention in high-risk groups. We sought to determine the impact of a primary care-based child obesity prevention intervention beginning during pregnancy on maternal infant feeding practices, knowledge, and styles at 10 months in low-income Hispanic families.
Methods: The Starting Early Program (StEP) randomized controlled trial enrolled pregnant women at a third trimester visit. Women (n = 533) were randomized to standard care or an intervention with prenatal/postpartum individual nutrition counseling and nutrition and parenting support groups coordinated with pediatric visits. Feeding practices (breastfeeding, family meals, juice, and cereal in the bottle) were assessed using questions from the Infant Feeding Practices Study II. Feeding styles were assessed using the Infant Feeding Style Questionnaire. We analyzed impacts on feeding practices, knowledge, and styles using regression analyses adjusting for covariates.
Results: Four hundred twelve mothers completed 10-month assessments. Intervention mothers were more likely to give breast milk as the only milk source [adjusted odds ratio (AOR) 1.65, 95% confidence interval (CI) 1.06–2.58] and have daily family meals (AOR 1.91, 95% CI 1.19–3.05), and less likely to give juice (AOR 0.60, 95% CI 0.39–0.92) or cereal in the bottle (AOR 0.54, 95% CI 0.30–0.97) compared to controls. Intervention mothers were more likely to exhibit lower pressuring, indulgent and laissez-faire feeding styles, and to have higher knowledge. Attending a greater number of group sessions increased intervention impacts.
Conclusions: StEP led to reduced obesity-promoting feeding practices and styles, and increased knowledge and provides great potential for population-scalability.
Keywords: feeding style, Hispanic/Latino, infant feeding, obesity prevention, primary care
Introduction
Early child obesity has significant adverse effects on health across the life course.1 Many feeding patterns that promote child obesity begin during pregnancy and infancy, and these are difficult to change once established.2 Economic and ethnic differences exist, with low-income and Hispanic children less likely to be exclusively breastfed, and more likely to have cereal in the bottle, higher juice intake, and caregivers with less responsive feeding styles.3 They are more likely to exhibit rapid infant weight gain and have a higher prevalence of overweight in the first 2 years of life than non-Hispanic white infants.3 These differences underscore the need for early primary prevention targeting high-risk families to prevent obesity-promoting feeding patterns and to decrease disparities in obesity prevalence.
Several trials of child obesity preventive interventions beginning in pregnancy or infancy have shown positive impacts on feeding and weight using community or nurse home visiting models. These programs were conducted either outside of the United States,4–6 or in primarily middle-income US communities,7,8 limiting their generalizability to low-income US communities. While home visiting programs for high-risk children have resulted in improved outcomes in development9 and obesity,10,11 their overall reach is limited, and alternative methods are needed to obtain population level outcomes in low-income communities.9
Many preventive interventions are based in primary health care settings. Prenatal primary care-based interventions focusing on maternal health and breastfeeding have reduced excess pregnancy weight gain and increased breastfeeding initiation.12,13 Programs providing continuous support across pre and postpartum settings have shown greatest impacts.14 In pediatrics, many successful primary care-based programs have promoted child development and school readiness.15,16 Pediatric primary care-based obesity prevention programs have shown some improvements in child feeding and weight, but have begun too late to impact obesity-related feeding patterns such as cereal in the bottle and exclusive breastfeeding.17,18 Currently, there are no comprehensive pediatric obesity prevention interventions based in prenatal and pediatric primary care that target obesity-promoting infant feeding patterns.
Therefore, we designed the Starting Early Program (StEP), a primary care-based child obesity prevention program for low-income, Hispanic families beginning in pregnancy and continuing through child age 3 years. The main intervention components, based on social learning theory19 included (1) prenatal and postpartum individual nutrition counseling; and (2) nutrition and parenting support groups (NPSG) coordinated with primary care pediatric visits. Evaluation at infant age 3 months found significant intervention impacts on feeding and activity.20,21
We assessed intervention efficacy in improving maternal feeding practices, knowledge, and styles at infant age 10 months, a developmental period with increased self-feeding and solid food consumption. We hypothesized that the intervention group would have (1) increased healthy infant feeding practices, such as more breastfeeding and less juice; (2) higher maternal infant feeding knowledge; and (3) more responsive feeding styles, than the standard care control group. Additionally, we hypothesized that attending more intervention sessions would result in greater impact.
Methods
Study Design
We conducted a randomized controlled trial to test the efficacy of the StEP compared to a standard care control group. This study was conducted in the prenatal and pediatric clinics of a large urban public hospital and an affiliated health center. This study was approved by the Institutional Review Board of NYU School of Medicine, and by NYC Health + Hospitals/Bellevue, and was registered on clinicaltrials.gov (NCT01541761).
Subjects
We included pregnant women who were at least 18 years old, Hispanic, English/Spanish speaking, with a singleton uncomplicated pregnancy, and who intended to receive pediatric care at the study sites. We excluded women with severe medical or psychiatric illness (e.g., sickle cell disease, psychosis) or fetal anomalies (e.g., chromosomal disorders). Women with diabetes, depression, or intrauterine growth restriction were not excluded. Our three-step eligibility screening process was previously described.20,21 Interested eligible women signed informed written consent, and completed baseline assessments. Enrollment took place between August 2012 and December 2014. Women were randomized at a prenatal visit after 32 weeks gestational age to intervention or control groups using a random number generator, stratified by site.
Starting Early Program
StEP was delivered by bilingual English/Spanish registered dietitians (RD), who were certified lactation counselors. The main intervention components were (1) individual nutrition counseling in the prenatal and postpartum periods; and (2) NPSG coordinated with well-child visits.
The NPSG addressed feeding (e.g., responsive feeding, age appropriate healthy foods, portion sizes, breastfeeding, healthy formula feeding), activity (e.g., promoting active play, reducing media exposure), and general parenting (e.g., family meals, soothing without feeding). Consistent groups of four to eight families were seen together from the 1-month visit until children reached 3 years to encourage peer interaction and social support. NPSG included a family meal to encourage healthy modeling, responsive feeding and self-feeding. Picture-based plain language handouts and two nutrition education DVDs were provided.
Seven intervention sessions occurred before the 10-month assessment, including 2 individual nutrition counseling sessions in the third trimester and the peri-partum period, and 5 NPSG at the 1, 2, 4, 6, and 9-month well-child visits (Table 1). We assessed intervention fidelity during 57% of the NPSG sessions. Of the sessions assessed, we found that 94% provided all curriculum components.
Table 1.
Summary of Starting Early Program Content Before the 10-Month-Old Assessment
| StEP sessions | Time | Content | |
|---|---|---|---|
| 1 | Individual | Third trimester prenatal visit | Discussed: |
| Introduction to Starting Early Program and RD/certified lactation counselor who will work with intervention subjects for next 3 years | |||
| Healthy infant feeding and benefits of breastfeeding | |||
| Assessment of feeding intentions and perceived barriers | |||
| Problem solving for perceived barriers | |||
| 2 | Individual | Postpartum hospital stay | Discussed: |
| Healthy infant feeding and benefits of breastfeeding | |||
| Assessment of feeding intentions and perceived barriers | |||
| Demonstrated and practiced: | |||
| Lactation support (skin-to-skin, latch assistance) | |||
| Healthy bottle feeding (infant led feeding) | |||
| Offered on-going support for lactation and other infant feeding issues | |||
| Scheduled pediatric visits and NPSG | |||
| 3 | NPSG-1 | Infant 1 month pediatric visit | Discussed: |
| Breastfeeding and healthy bottle feeding | |||
| Recognizing infant feeding cues | |||
| Nonfeeding related infant soothing techniques | |||
| Demonstrated and practiced: | |||
| Sharing positive and negative feeding experiences | |||
| Strategizing solutions to common feeding concerns | |||
| Recognizing cues with baby face photos | |||
| Pointing out cues in nutrition DVD (distributing DVD to take home) | |||
| Identifying their infant's hunger/fullness cues during observed feeding | |||
| Soothing without feeding (e.g., swaddling, swinging) | |||
| 4 | NPSG-2 | Infant 2-month pediatric visit | Discussed: |
| How much to feed | |||
| Recognizing infant feeding cues | |||
| Meaning of infant crying | |||
| Avoiding early introduction of complementary food or liquids | |||
| Importance of movement, activity and tummy time for infants | |||
| Demonstrated and practiced: | |||
| Identifying feeding cues (BINGO game) | |||
| Soothing without feeding (e.g., swaddling, swinging) | |||
| Tummy time together on blankets and floor mats | |||
| 5 | NPSG-3 | Infant 4-month pediatric visit | Discussed: |
| Breastfeeding and healthy bottle feeding | |||
| Signs of infant readiness to eat solids | |||
| Reasons to wait until age 6 months to introduce solids | |||
| Healthy first foods | |||
| Healthy sleep routines | |||
| Demonstration and practice: | |||
| Identifying developmental signs that indicate delaying introduction of solids until 6 months | |||
| Preparing commercial and homemade infant cereal | |||
| 6 | NPSG-4 | Infant 6-month pediatric visit | Discussed: |
| Introduction of complementary foods | |||
| Age-appropriate portion sizes | |||
| Examples of healthy meal and snack routines | |||
| Responsive feeding | |||
| Interacting and talking during meals | |||
| Avoiding media exposure during meals | |||
| Demonstrations and practice: | |||
| Preparing homemade baby food purees (banana and sweet potatoes) | |||
| Comparing taste of commercial and homemade baby foods | |||
| Eating family meal together in the group | |||
| Identifying active ways to play together | |||
| 7 | NPSG-5 | Infant 9-month pediatric visit | Discussed: |
| Feeding the older infant: self-feeding, healthy portion sizes, meal and snack patterns, family meals, water and human milk or formula as primary drink, and cup introduction | |||
| Parent's role in feeding: offering infants healthy foods and allowing the infant to decide how much to eat | |||
| Demonstrations and practice: | |||
| Eating family meal together in the group | |||
| Measuring out appropriate infant portion sizes | |||
| Identifying their infant's hunger and fullness cues during group meal | |||
| Practicing self-feeding in high chairs | |||
| Demonstration of sugar quantity in juice and fruit punch | |||
Both the intervention and control groups received routine prenatal, postpartum, and pediatric primary care. This included one individual prenatal nutrition consultation and the availability of prenatal group childbirth and breastfeeding classes. Additional prenatal nutritionist visits were offered as standard care for poor weight gain, obesity, and diabetes. Pediatric visits were scheduled according to American Academy of Pediatrics Bright Futures guidelines. Additional medical or nutrition visits were based on the provider's discretion.
Assessments
Assessments at infant age 10 months included telephone-administered surveys and medical record review conducted by research assistants who were not informed of subject group assignment. Intervention RDs did not perform outcome assessments.
Maternal infant feeding practices
Feeding practices were assessed using questions adapted from the Infant Feeding Practices Study II, a national longitudinal study of infant feeding.22 Breastfeeding was assessed by asking: “What kind of milk is your baby drinking now?” Breast milk as the only milk source was defined as breast milk only versus any other milk or combination of milk. Introduction of cereal, water, and juice in the bottle and juice intake were assessed. Self-feeding was evaluated by asking: “Does your baby use his/her fingers to feed him/herself?” The number of times the infant ate fruit and vegetables and a family meal together in the last 7 days was assessed. These practices were dichotomized as 7 or more versus less than 7 to estimate daily behaviors.
Maternal infant feeding knowledge
Feeding knowledge was assessed using eight questions generated from the StEP curriculum. A total knowledge score was created from the sum of the correct responses, with higher scores representing greater knowledge.
Maternal infant feeding styles
Feeding styles were assessed using the Infant Feeding Style Questionnaire,23 which was validated in low-income Hispanic mothers.24 Five feeding style domains, comprised of 13 subscales, were assessed: (1) responsive included two subscales: attention (e.g., talking to infant during feeding; α = 0.84) and satiety (e.g., recognizing when infant is hungry and full; α = 0.92); (2) pressuring/controlling included three subscales: pressuring to finish (e.g., encourage finishing food even if full; α = 0.79), pressuring with cereal (e.g., adding cereal to the bottle to increase fullness; α = 0.78), and pressuring to soothe (e.g., feeding immediately to stop crying; α = 0.84); (3) restrictive/controlling included two subscales: amount consumed (e.g., careful not to feed too much even if hungry; α = 0.75) and diet quality (e.g., not letting child eat junk foods; α = 0.85); (4) indulgent included four subscales: permissive (e.g., allow fast food if child wants it; α = 0.82), coaxing (e.g., allow fast food to make sure child gets enough; α = 0.89), soothing (e.g., allow fast food to keep child from crying; α = 0.87) and pampering (e.g., allow fast food to keep child happy; α = 0.94); and (5) laissez-faire included two subscales: attention (e.g., watches TV while feeding; α = 0.80) and diet quality (e.g., does not limit sugary foods; α = 0.91). Mean subscale scores range from 1 to 5, with higher scores indicating higher levels of the construct.
Family characteristics
Baseline demographic information included maternal age, parity, education, employment, marital status, and country of origin. Prenatal depressive symptoms were defined as a score of 5 or greater on the Patient Health Questionnaire-9.25 Prenatal food insecurity was assessed using the Core Food Security Module.26 “Food secure” was defined as no more than two food insecure conditions and “food insecure” as three or more. Participation in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) and the Supplemental Nutrition Assistance Program (SNAP) was assessed. Prepregnancy weight status, infant sex, delivery type, gestational age, and birth weight were obtained from the medical record.
Statistical Analyses
Sample size estimates were based on capacity to detect impacts on obesity reduction. To achieve 80% power to detect 15% reduction in obesity with 30% loss to follow-up and alpha of 0.05, we needed to enroll 500 pregnant women. The data were analyzed by using SPSS version 18.0 (SPSS, Inc., Chicago, IL). We performed intent-to-treat analyses, with participants allocated to their given group and assessed based on this assignment. We performed univariate analyses to examine baseline characteristics by group. We examined bivariate relationships between group and feeding practices, knowledge, and styles using independent samples t-tests and chi-square analyses for continuous and categorical variables respectively. We used logistic and linear regression analyses to determine relationships between intervention group status and feeding outcomes adjusting for covariates. All models adjusted for maternal education, marital status, first child, prepregnancy obesity status, and child sex. The distribution of five feeding style subscales were skewed: laissez-faire attention (skewness [standard error] = 1.37 [0.12]); indulgent permissive (1.54 [0.12]); indulgent coaxing (3.67 [0.12]); indulgent soothing (3.38 [0.12]) and indulgent pampering (3.15 [0.12]). Multiple linear regression analyses for these five subscales were performed using log-transformation to account for skewing. Using within intervention group analyses, we explored relationships between dose as an ordinal variable (number of visits attended ranging from 0 to 5) and feeding practices, styles, and knowledge, using correlations and chi-square analyses.
Results
Study Sample
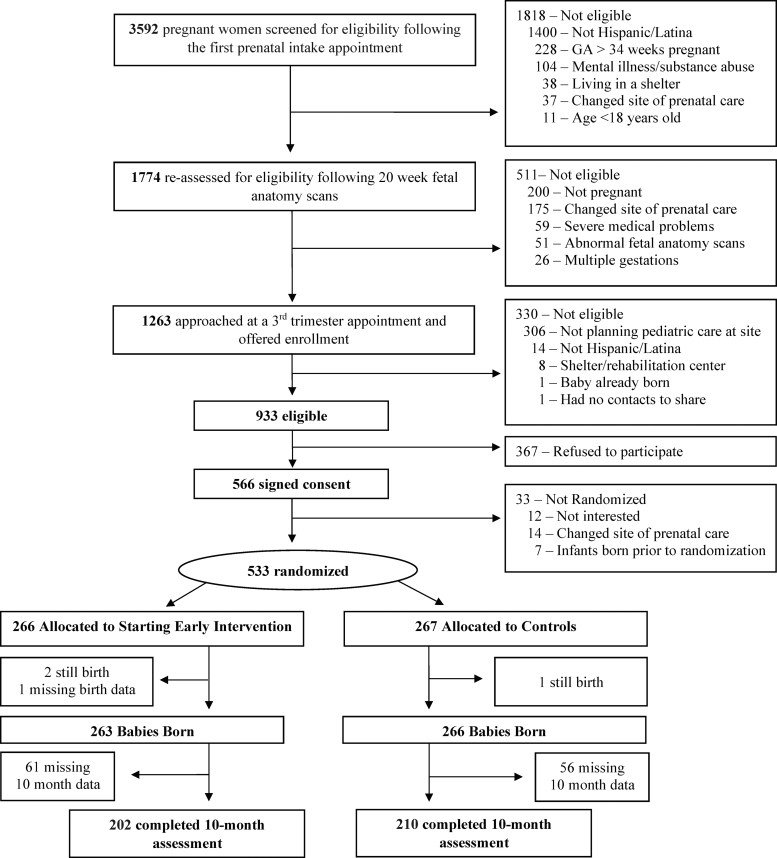
All pregnant women presenting for their first prenatal visit between August 2012 and December 2014 were identified by their primary care providers and screened for potential eligibility (Fig. 1). Four hundred twelve mother–infant pairs (202 intervention, 210 control) completed the 10-month assessment (78% of infants born) and were included in these analyses, mean (standard deviation) child age 10.6 (0.7) months. Groups did not differ in baseline characteristics (Table 2). Mothers who did not complete the 10-month assessment were similar to those who did, except they were younger (26.3 years vs. 28.1 years, p < 0.003) and more likely first-time mothers (51.2% vs. 33.3%, p < 0.001).
Figure 1.
Participant enrollment and assessment through infant age 10 months.
Table 2.
Baseline Characteristics for the 10-Month-Old Analytic Sample
| Family characteristics |
n = 412 |
|
|---|---|---|
| |
Control (n = 210) |
Intervention (n = 202) |
| Mother (prenatal) | Mean (SD) | Mean (SD) |
| Age (years) | 28.8 (8.5) | 28.9 (5.9) |
| n (%) | n (%) | |
| Primiparous | 75 (35.7) | 62 (30.7) |
| Education (less than high school) | 64 (30.5) | 76 (37.6) |
| Working | 63 (30.1) | 49 (24.4) |
| Married or living as married | 152 (72.4) | 149 (73.8) |
| US born | 38 (18.1) | 40 (19.8) |
| Depressive symptoms | 65 (31.0) | 68 (33.8) |
| Household food insecurity | 70 (34.5) | 60 (30.2) |
| WIC participant | 180 (85.7) | 180 (89.1) |
| SNAP participant | 77 (36.7) | 76 (37.6) |
| Prepregnancy obese status | 61 (29.0) | 55 (27.4) |
| |
n = 412 |
|
|---|---|---|
| |
Control (n = 210) |
Intervention (n = 202) |
| Child (birth) | Mean (SD) | Mean (SD) |
| Birth weight (kg)a |
3.40 (0.49) |
3.37(0.45) |
| |
n (%) |
n (%) |
| Large for gestational agea |
27 (12.9) |
17 (8.5) |
| C-sectiona |
50 (23.9) |
46 (22.5) |
| Premature <37 weeks gestational agea |
4 (2.0) |
6 (3.2) |
| Male sex | 104 (49.5) | 98 (48.5) |
Control, n = 209; Intervention, n = 200.
WIC, Special Supplemental Nutrition Program for Women, Infants, and Children; SNAP, Supplemental Nutrition Assistance Program, commonly known as food stamps; SD, standard deviation.
Intervention Dose
All intervention participants attended the prenatal session; 96.4% received postpartum counseling. Intervention participants could have attended five NPSG sessions before this assessment (13.4% attended none; 9.9% attended 1; 9.9% attended 2; 18.8% attended 3; 21.8% attended 4; 26.2% attended 5). Median number of group visits was 3. No adverse events, such as discomfort discussing curriculum, were reported.
Intervention Effects on Feeding Practices and Knowledge
At infant age 10 months, more intervention mothers reported breast milk as the only milk source than controls [adjusted odds ratio (AOR) 1.65, 95% CI 1.06–2.58] (Table 3). The intervention mothers were less likely to have introduced juice (AOR 0.60, 95% CI 0.39–0.92), given juice in a bottle (AOR 0.51, 95% CI 0.33–0.79) or cereal in a bottle (AOR 0.54, 95% CI 0.30–0.97). Intervention pairs were more likely to have daily family meals (AOR 1.91, 95% CI 1.19–3.05). The intervention group was significantly more likely to answer two questions correctly: breast milk or formula should be a baby's main drink at 9 months, and babies do not need juice. They displayed higher knowledge scores than controls (AOR 1.63, 95% CI 1.08–2.46).
Table 3.
Starting Early Program Impacts on Maternal Infant Feeding Practices and Knowledge at 10 Months
| Maternal infant feeding practices (n = 412) | Group, n (%) |
p | AORa | 95% CI | |
|---|---|---|---|---|---|
| Control (n = 210) | Intervention (n = 202) | ||||
| Breastfeeding at 10 months | |||||
| Any breast milk at 10 months | 114 (54.3) | 122 (60.4) | 0.23 | 1.20 | 0.81–1.80 |
| Breast milk as the only milk source at 10 months | 48 (22.9) | 67 (33.2) | 0.02* | 1.65 | 1.06–2.58 |
| Other feeding at 10 months | |||||
| Introduced juice (ever) | 155 (73.8) | 126 (62.4) | 0.02* | 0.60 | 0.39–0.92 |
| Ever given juice in the bottle | 77 (36.7) | 46 (22.8) | 0.003* | 0.51 | 0.33–0.79 |
| Ever given water in the bottle | 140 (66.7) | 114 (56.4) | 0.03* | 0.65 | 0.43–0.97 |
| Ever given cereal in the bottle | 38 (18.1) | 20 (10.0) | 0.02* | 0.54 | 0.30–0.97 |
| Self-feeding | 194 (92.4) | 179 (88.6) | 0.24 | 0.61 | 0.31–1.21 |
| Family meals daily | 147 (70.0) | 165 (81.7) | 0.006* | 1.91 | 1.19–3.05 |
| Fruit consumption daily | 173 (82.4) | 164 (81.2) | 0.80 | 0.94 | 0.57–1.56 |
| Vegetable consumption daily | 141 (67.1) | 134 (66.3) | 0.92 | 0.99 | 0.66–1.50 |
| Individual knowledge questions (n = 410) | Correct answer, n (%) |
p | AORa | 95% CI | |
|---|---|---|---|---|---|
| Control (n = 209) | Intervention (n = 201) | ||||
| Baby food from a jar is better than homemade baby foodb |
200 (95.7) |
193 (96.0) |
1.00 |
1.13 |
0.42–3.06 |
| Fruits and vegetables should be given to babies at almost every meal or snack |
193 (92.8) |
185 (92.0) |
0.85 |
0.88 |
0.42–1.84 |
| Breast milk or formula is still a baby's main drink at 9 months |
174 (83.3) |
184 (91.5) |
0.01* |
2.10 |
1.13–3.91 |
| Babies should not eat meals with the rest of the familyb |
200 (95.7) |
189 (94.0) |
0.51 |
0.76 |
0.31–1.89 |
| Babies need juiceb |
134 (64.1) |
154 (76.6) |
0.007* |
1.93 |
1.23–3.03 |
| 10-month-old babies can drink from a cup |
174 (83.3) |
176 (87.6) |
0.26 |
1.37 |
0.78–2.40 |
| You should talk to your baby during mealtime |
192 (91.9) |
179 (89.1) |
0.40 |
0.72 |
0.37–1.41 |
| Babies can begin to feed themselves around 9 months |
164 (78.5) |
160 (79.6) |
0.81 |
1.06 |
0.65–1.71 |
| High knowledge score | 65 (31.3) | 85 (42.3) | 0.02* | 1.63 | 1.08–2.46 |
| Mean (SD) | p | B (SE)a | 95% CI | ||
|---|---|---|---|---|---|
| Total knowledge score | 6.86 (1.0) | 7.06 (1.1) | 0.046* | 0.20 (0.10) | 0.001–0.40 |
Models adjusted for maternal education, obesity, marital status, first child, child sex.
Statements in which the correct response was “false.”
Significant with p < 0.05.
AOR, adjusted odds ratio; CI, confidence interval.
Intervention Effects on Feeding Styles
The intervention group exhibited lower subscale scores in pressuring/controlling, indulgent and laissez-faire domains compared to controls. Intervention subjects had lower pressuring to finish (2.52 vs. 2.79, p = 0.002) and pressuring with cereal mean scores (1.98 vs. 2.27, p = 0.002) (Table 4). In the indulgent domain, intervention subjects had lower permissive mean scores (1.33 vs. 1.43, p = 0.03) and in the laissez-faire domain, intervention mothers had lower mean low-attention scores (1.47 vs. 1.65, p = 0.003). Intervention impacts on responsive or restrictive domains were not found.
Table 4.
Starting Early Program Impacts on Maternal Infant Feeding Styles at 10 Months
| Maternal infant feeding stylesa | Group (n = 408)b |
p | B | 95% CI | ||
|---|---|---|---|---|---|---|
| Control (n = 209) | Intervention (n = 199) | |||||
| Responsive | Attention | 4.00 (0.87) | 3.92 (0.85) | 0.37 | −0.04 | −0.14 to 0.05 |
| Satiety | 4.45 (0.47) | 4.48 (0.51) | 0.55 | 0.04 | −0.06 to 0.14 | |
| Pressuring | Finishing | 2.79 (0.88) | 2.52 (0.82) | 0.002* | −0.15 | −0.25 to −0.06* |
| Cereal | 2.27 (1.03) | 1.98 (0.86) | 0.002* | −0.16 | −0.25 to −0.06* | |
| Soothing | 2.53 (1.19) | 2.63 (1.18) | 0.41 | 0.02 | −0.07 to 0.12 | |
| Restrictive | Amount consumed | 3.96 (1.06) | 3.82 (1.04) | 0.19 | −0.07 | −0.16 to 0.03 |
| Diet quality | 4.19 (0.66) | 4.17 (0.65) | 0.71 | −0.01 | −0.11 to 0.09 | |
| Indulgent | Permissive | 1.43 (0.49) | 1.33 (0.45) | 0.03* | −0.11 | −0.20 to −0.01* |
| Coaxing | 1.15 (0.28) | 1.15 (0.35) | 0.76 | 0.002 | −0.10 to 0.10 | |
| Soothing | 1.16 (0.30) | 1.14 (0.34) | 0.44 | −0.06 | −0.15 to 0.04 | |
| Pampering | 1.17 (0.31) | 1.15 (0.34) | 0.53 | −0.04 | −0.14 to 0.05 | |
| Laissez-faire | Attention | 1.65 (0.67) | 1.47 (0.58) | 0.003* | −0.16 | −0.26 to −0.06* |
| Diet quality | 1.71 (0.60) | 1.75 (0.65) | 0.52 | 0.02 | −0.08 to 0.12 | |
Scores ranged from 1 to 5, with higher scores indicating higher levels of the given construct.
Four hundred eight mothers had complete data for the feeding style questionnaire.
Significant with p < 0.05.
Dose Effect
Within the intervention group, we found that the increasing number of NPSG sessions attended was correlated with giving breast milk as the only milk source (spearman correlation r = 0.19; p = 0.006), giving less cereal in the bottle (r = −0.25; p < 0.001); higher knowledge scores (r = 0.25; p < 0.001); and lower pressuring with cereal (r = −0.21; p = 0.003). Attending ≥4 sessions was associated with giving only breast milk (22.9% vs. 44.3%, p = 0.002). Attending 2–3 sessions and 4–5 sessions decreased adding cereal in the bottle in a dose-dependent manner compared to 0–1 sessions respectively (21.7% vs. 10.3% vs. 4.2%, p = 0.005).
Discussion
StEP, a comprehensive child obesity prevention intervention integrated into prenatal and pediatric primary care, improved maternal infant feeding knowledge, styles, and practices at infant age 10 months. The intervention group showed greater breastfeeding, reduced juice and cereal in the bottle, and increased family meals than controls. Intervention participants had higher knowledge and lower nonresponsive feeding styles. Dose-dependent effects were found.
The benefits of utilizing primary care include the following: (1) the high frequency of and adherence to prenatal and pediatric primary care visits, which provide access to high-risk families on a population scale; (2) building on pre-existing provider relationships; (3) using existing infrastructure to lower cost; and (4) decreased need for additional transportation. Primary care-based programs, including Video Interaction Project27,28 and Healthy Steps,29 have successfully improved developmental outcomes by utilizing health care to reach low-income families. To our knowledge, only one other primary care-based early obesity prevention study has reported impacts on child obesity in the United States.18 This small yet promising pilot of a group pediatric primary care visit model with added emphasis on obesity prevention showed reduced obesity at age 2 years among the intervention group compared to children receiving standard care. Although the intervention began when the infants were 1 month old, 70% of intervention mothers, versus 17% of controls, had received group prenatal care, which may have contributed to program impact. Although StEP uses a group approach, it does not require group primary care visits, facilitating its scalability and allowing for a seamless supportive intervention from pregnancy through infancy.
StEP shared key similarities to other successful early obesity prevention programs and included several innovations to enhance its effects in low-income families. Similar to interventions conducted outside the United States,4–6,10 StEP targeted feeding, activity, and general parenting skills comprehensively, rather than focusing on only one domain. Those with greatest impacts also began prenatally.5 Similar to the INSIGHT trial in the United States,7,8,30 StEP focused on promoting responsive parenting and developing routines. StEP innovations developed specifically for low-income populations included program delivery by culturally competent bilingual RDs, who provided support during pregnancy, after delivery and throughout infancy. All program materials were sensitive to poverty-related challenges, such as food insecurity, which have been associated with obesity-promoting maternal attitudes and styles.31 StEP content was developed for mothers with low health literacy, using plain language and picture-based messaging. The NPSG content was novel in that it incorporated social learning theory important for adult behavior change and focused on interactive demonstrations and active practicing of skills.19
StEP impacted obesity-promoting feeding practices more prevalent in low-income Hispanic families than other economic and ethnic groups.3 Numerous breastfeeding promotion interventions have shown that support that occurs in both pre- and postpartum settings are most effective.12–14 Our program adds to this by showing that a comprehensive child obesity prevention program occurring in the pre- and postpartum primary care settings can increase breastfeeding even later in infancy. StEP intervention mothers had higher rates of exclusive breastfeeding at 10 months (33.2%) than those at 6 months (21.2%) for women in New York State generally.32 Intervention subjects showed increased family meals and lower juice intake and cereal in the bottle. While intervention infants were more than 50% likely to have breast milk as their only milk source, and not to have juice, the clinical impact of these improvements is difficult to estimate. A recent meta-analysis found that while juice is associated with only small BMI increases in older children, children less than 2 years may be more susceptible to weight gain from drinking juice.33 Longitudinal follow-up is needed to determine long-term impacts of these feeding practices on growth. In addition to changing practices, StEP increased knowledge, in particular with respect to knowledge about milk and juice consumption, two of the main practices impacted.
Intervention mothers exhibited lower nonresponsive feeding styles subscales compared to controls. Nonresponsive feeding styles have a longitudinal relationship with infant weight trajectories34 and are known to be more prevalent in low-income ethnic minority mothers beginning in early infancy.35 Decreasing nonresponsive feeding styles may prevent the disruption of infant self-regulation, leading to eating in the absence of hunger and increased caloric intake.35 Despite lowering pressuring, indulgent and laissez-faire subscales, we did not impact responsive or restrictive feeding styles. This may be due to overall high scores across these domains, demonstrating similarities with prior studies of Hispanic mothers.24
This study has several limitations. Infant feeding practices were based on maternal report, which can reflect social desirability biases. However, survey questions were adapted from nationally utilized questions. Participants were low-income Hispanic mothers, limiting generalizability to other populations. The follow-up period was infant age 10 months. It is unknown whether these changes in feeding practices, knowledge, and styles will be sustained, although the magnitude and type of changes found are similar to those at infant age 3 months. A strength is our high retention rate; with nearly 80% follow-up 1 year into the randomized controlled trial. This high retention rate may be due to prenatal enrollment and the strong social support provided by program staff.
In conclusion, our findings demonstrate that StEP improved infant feeding practices, knowledge, and styles at infant age 10 months. Integration into the framework of frequent primary health care visits in pregnancy and infancy provides the ability to reach high-risk families, with potential for population-wide application. Longitudinal follow-up will determine the long-term impacts of StEP on dietary and lifestyle habits, and ultimately child obesity.
Acknowledgments
We would like to thank the Starting Early Program staff who contributed to this project.
Funding Information
This work is supported by the National Institute of Food and Agriculture, U.S. Department of Agriculture, under award number 2011-68001-30207 and by the National Institute of Health/National Institute of Child Health and Human Development (NIH/NICHD) through a K23 Mentored Patient-Oriented Research Career Development Award (K23HD081077; PI Gross).
Author Disclosure Statement
No competing financial interests exist.
References
- 1. Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: Systematic review. Int J Obes 2011;35:891–898 [DOI] [PubMed] [Google Scholar]
- 2. Cameron AJ, Spence AC, Laws R, et al. A review of the relationship between socioeconomic position and the early-life predictors of obesity. Curr Obes Rep 2015;4:350–362 [DOI] [PubMed] [Google Scholar]
- 3. Taveras EM, Gillman MW, Kleinman KP, et al. Reducing racial/ethnic disparities in childhood obesity: The role of early life risk factors. JAMA Pediatr 2013;167:731–738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Daniels LA, Mallan KM, Nicholson JM, et al. Outcomes of an early feeding practices intervention to prevent childhood obesity. Pediatrics 2013;132:e109–e118 [DOI] [PubMed] [Google Scholar]
- 5. Wen LM, Baur LA, Simpson JM, et al. Effectiveness of home based early intervention on children's BMI at age 2: Randomized controlled trial. BMJ 2012;344:e3732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Campbell KJ, Lioret S, McNaughton SA, et al. A parent-focused intervention to reduce infant obesity risk behaviors: A randomized trial. Pediatrics 2013;131:652–660 [DOI] [PubMed] [Google Scholar]
- 7. Savage J, Birch L, Marini M, et al. Effect of the INSIGHT responsive parenting intervention on rapid infant weight gain and overweight status at age 1 year: A randomized clinical trial. JAMA Pediatr 2016;170:742–749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Paul IM, Savage JS, Anzman-Frasca S, et al. Effect of a responsive parenting educational intervention on childhood weight outcomes at 3 years of age. JAMA 2018;320:461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Avellar S, Paulsell D, Sama-Miller E, et al. Home visiting evidence of effectiveness review: Executive summary. Office of Planning, Research and Evaluation, Administration for Children and Families, U.S. Department of Health and Human Services. Washington, DC, 2016
- 10. Taylor B, Gray A, Galland B, et al. Targeting sleep, food, and activity in infants for obesity prevention: An RCT. Pediatrics 2017;139:e20162037. [DOI] [PubMed] [Google Scholar]
- 11. Ordway MR, Sadler LS, Holland ML, et al. A home visiting parenting program and child obesity: A randomized trial. Pediatrics 2018;141:e20171076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bonuck K, Stuebe A, Barnett J, et al. Effect of primary care intervention on breastfeeding duration and intensity. Am J Public Health 2014;104(Suppl 1):S119–S127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Vesco KK, Karanja N, King JC, et al. Efficacy of a group-based dietary intervention for limiting gestational weight gain among obese women: A randomized trial. Obesity (Silver Spring) 2014;22:1989–1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Patnode C, Henninger M, Senger C, et al. Primary care interventions to support breastfeeding: Updated systematic review for the U.S. preventive services task force. Evidence Synthesis No. 143. AHRQ Publication No. 15-05218-EF-1, 2016 [PubMed]
- 15. Cates CB, Weisleder A, Berkule Johnson S, et al. Enhancing parent talk, reading, and play in primary care: Sustained impacts of the Video Interaction Project. J Pediatr 2018;199:49–56.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cates CB, Weisleder A, Mendelsohn AL. Mitigating the effects of family poverty on early child development through parenting interventions in primary care. Acad Pediatr 2016;16(3 Suppl):S112–S120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. French GM, Nicholson L, Skybo T, et al. An evaluation of mother-centered anticipatory guidance to reduce obesogenic infant feeding behaviors. Pediatrics 2012;130:e507–e517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Machuca M, Arevalo S, Hackley B, et al. Well baby group care: Evaluation of a promising intervention for primary obesity prevention in toddlers. Child Obes 2016;12:171–178 [DOI] [PubMed] [Google Scholar]
- 19. Bandura A. Social Learning Theory. Prentice Hall: Englewood Cliffs, NJ, 1977
- 20. Gross R, Mendelsohn A, Gross M, et al. Randomized controlled trial of a primary care-based child obesity prevention intervention on infant feeding practices. J Pediatr 2016;174:171–177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gross R, Mendelsohn A, Yin H, et al. Randomized controlled trial of an early child obesity prevention intervention: Impacts on infant tummy time. Obesity (Silver Spring) 2017;25:920–927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Fein SB, Labiner-Wolfe J, Shealy KR, et al. Infant feeding practices study II: Study methods. Pediatrics 2008;122(Suppl 2):S28–S35 [DOI] [PubMed] [Google Scholar]
- 23. Thompson AL, Mendez MA, Borja JB, et al. Development and validation of the infant feeding style questionnaire. Appetite 2009;53:210–221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wood CT, Perreira KM, Perrin EM, et al. Confirmatory factor analysis of the infant feeding styles questionnaire in Latino families. Appetite 2016;100:118–125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med 2001;16:606–613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bickel G, Nord M, Price C, et al. Guide to Measuring Household Food Security, Revised 2000. US Department of Agriculture, Food and Nutrition Service: Alexandria, VA, 2000
- 27. Mendelsohn AL, Huberman HS, Berkule SB, et al. Primary care strategies for promoting parent-child interactions and school readiness in at-risk families: The Bellevue project for early language, literacy, and education success. Arch Pediatr Adolesc Med 2011;165:33–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Weisleder A, Cates C, Dreyer B, et al. A promotion of positive parenting and prevention of socioemotional disparities. Pediatrics 2016;137:e20153239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Minkovitz C, Strobino D, Hughart N, et al. Early effects of the Healthy Steps for young children program. Arch Pediatr Adolesc Med 2001;155:470–479 [DOI] [PubMed] [Google Scholar]
- 30. Hohman E, Paul I, Birch L, Savage J. INSIGHT responsive parenting intervention is associated with healthier patterns of dietary exposures in infants. Obesity (Silver Spring) 2017;25:185–191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gross RS, Mendelsohn AL, Fierman AH, et al. Food insecurity and obesogenic maternal infant feeding styles and practices in low-income families. Pediatrics 2012;130:254–261 [DOI] [PubMed] [Google Scholar]
- 32. CDC National Center for Chronic Disease Prevention and Health Promotion: Breastfeeding Report Card United States, 2018 Division of Nutrition, Physical Activity, and Obesity. Available at www.cdc.gov/breastfeeding (last accessed December9, 2019)
- 33. Auerbach BJ, Wolf FM, Hikida A, et al. Fruit juice and change in BMI: A meta-analysis. Pediatrics 2017;139:e20162454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hughes S, Power T, O'Connor T, et al. Maternal feeding styles and food parenting practices as predictors of longitudinal changes in weight status in Hispanic preschoolers from low-income families. J Obes 2016;2016:7201082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. DiSantis KI, Hodges EA, Johnson SL, Fisher JO. The role of responsive feeding in overweight during infancy and toddlerhood: A systematic review. Int J Obes 2011;35:480–492 [DOI] [PMC free article] [PubMed] [Google Scholar]