Abstract
Introduction:
Hypertension is an overwhelming global challenge. Appropriate lifestyle modifications are the cornerstone for the prevention and control of hypertension. In this regard, lack of knowledge and poor attitude toward lifestyle modification have been a major setback.
Objective:
To assess knowledge, attitude and practice of lifestyle modification recommended for hypertension management and the associated factors among adult hypertensive patients in Harar, Eastern Ethiopia.
Methods:
Hospital-based cross-sectional study was conducted among 274 hypertensive patients in Hiwot Fana Specialized University Hospital, from 1 March to 30 May 2019. The pre-tested structured questionnaire was used, and the data were collected through an interview. The data were analyzed using SPSS version 20. A multivariate logistic regression model was fitted to determine independent predictors of knowledge and practice of lifestyle modifications among hypertensive patients. Adjusted odds ratio (AOR) at 95% confidence interval (CI) was used for predicting the independent effect of each variable on the outcome variables.
Results:
From the total participants, 200 (73.0%) of participants had good knowledge, 182 (66.4%) had favorable attitude and 136 (49.6%) had good practice on lifestyle modification recommended for hypertension management. Regarding factors associated with lifestyle modification, being in age range of 46–64 years (AOR: 4.08, 95% CI: 1.14–14.56); having formal education (AOR: 3.93, 95% CI: 1.27–12.23); being government employee (AOR: 8.06, 95% CI: 1.40–46.32) and being housewives (AOR: 5.10, 95% CI: 1.26–20.79) were factors significantly associated with good knowledge of lifestyle modification, However, favorable attitude was found to be the only factor associated with good practice of lifestyle modification (AOR: 9.20, 95% CI: 2.60–32.24).
Conclusion:
In the current study, knowledge and attitude toward lifestyle modification recommended for hypertension management was fairly good but practice level was poor. Concerted strategies are required to increase the knowledge, attitude and practice of the lifestyle modification measures in this population group.
Keywords: Lifestyle modification, hypertension, knowledge, attitude, practice
Introduction
Arterial hypertension, also known as high or raised blood pressure (BP), is a global public health issue. It contributes to the burden of heart disease, stroke and kidney failure, hence to premature mortality and disability.1 According to World Health Organization (WHO) 2013 report, globally cardiovascular disease accounts for approximately 17 million deaths a year, nearly one-third of the total. Of these, hypertension-related complications account for 9.4 million deaths worldwide every year.1 Developing countries share significant burden as they are experiencing epidemiological transition from communicable to non-communicable chronic diseases.2 For example, in Africa, Ethiopia included, 15% of the population is thought to have hypertension.3,4 The prevalence of hypertension was found to be high among adults aged ⩾50 years, ranging from 22.3% to 90.0%.5
The factors contributing to the hypertension are mainly environmental, genetic and behavioral factors such as smoking, high alcohol intake and high fat intake. These risk factors can be counteracted through lifestyle modification (LSM).6–9 According to WHO, increment in prevalence of hypertension and other cardiovascular disease in developing countries has been associated with aging of the populations, urbanization and socioeconomic changes favoring sedentary habits.1
Hypertension can be adequately managed through drug treatment as well as lifestyle changes. LSM, in addition to lowering BP, can also reduce other cardiovascular risk factors.10 Furthermore, the involved cost is minimal and there are hardly any risks. Hypertensive patients irrespective of their disease stage are encouraged to adopt these measures.11,12 Unawareness of LSM and failure to apply it was one of the identified patient-related barriers to BP control.13
In hypertensive individuals, LSM can be recommended as an initial treatment before starting drug therapy or as an adjuvant. LSM has proven role in hypertension management. For example, according to Whelton et al.,14 LSM can decrease systolic blood pressure (SBP) approximately by 11 mmHg. Moreover, LSM may enable drug step-down and drug withdrawal ultimately when the control is deemed adequate, particularly in patients who are highly committed to maintain lifestyle changes.
Different types of LSMs are indicated for hypertension management, including weight loss for obese patients, sodium reduction not exceeding 1.5 g daily, alcohol intake reduction, smoking cessation, avoidance of excessive caffeine, diet modification such as low intake of saturated and total fat and increase in fruits and vegetables intake.15,16 Despite its proven effect, the implementation of LSM is often the overlooked part of hypertension management. One problem for lack of LSM among hypertensive patient is lack of awareness and poor practice. For example, a study conducted in Ghana showed mean knowledge score on LSM of 2.5 (standard deviation (SD): 1.25) out of 517 whereas in Nigeria only 33 out of 104 (31.7%) had good knowledge.18 Similarly, the study participant displayed poor attitude and adherence toward LSM in both study.
Various both modifiable and non-modifiable factors have been associated with poor implementation of LSM. Age, educational status, monthly income, years since diagnosis and co-morbidity were among factors significantly associated with LSM practice.19 Gender and educational background were associated with knowledge of LSM.17 It is important to identify modifiable factors and work toward improving it in order to adequately control hypertension and prevent its sequel. The few existing studies conducted in Ethiopia indicated inconsistent data.19–21 For instance, the level of good practice to LSM was found to be 23% in Addis Ababa21 whereas it was found to be 61.39% in Bishoftu.20 As our knowledge goes, there is no published study conducted in the study setting. In this study, we examined KAP toward LSM recommended for hypertension management and factors associated with knowledge and practice of LSM among adult hypertensive patients on chronic care unit Hiwot Fana Specialized University Hospital (HFSUH).
Methods and materials
Study area and period
The study was conducted in HFSUH from 1 March to 30 May 2019. HFSUH is located in Harar City which is found about 525 km from Addis Ababa in eastern part of Ethiopia. HFSUH was established in 1941. It is a referral hospital for population in Harar city and its surrounding. The hospital has different inpatient and outpatient departments. This study was conducted in outpatient chronic care unit of HFSUH.
Study design
Hospital-based cross-sectional study was conducted to assess the level of knowledge, attitude and practice (KAP) toward LSM recommended for hypertension management among adult hypertensive patients in chronic care unit of HFSUH.
Population
All adult hypertensive patients who were on follow-up visit in chronic care unit of HFSUH were source population, whereas all adult hypertensive patients visiting the chronic care unit during the study period were study population. All adult hypertensive patients who had follow-up visit in chronic care unit of HFSUH in the study period were included, and those adult hypertensive patients who were newly diagnosed (less than a year) were excluded from the study.
Sample size and sampling techniques
Sample size was determined using single proportion formula with 95% confidence level, 5% degree of precision and taking the proportion of hypertensive patients who had sufficient knowledge (72.3%), positive attitude (68.32%) and good practice (61.39%) of LSM obtained from a previous study conducted in Bishoftu General Hospital.20 We considered the largest sample size, which was 364. Since our source population was less than 10,000, finite population correction was used. Then, adding 5% non-responses on the largest sample size, the final sample size was 292. All consecutive adult hypertensive patients visiting chronic care unit of HFSUH during the study period and who fulfill the inclusion criteria were included for the purpose of the study.
Data collection tools and data collection procedure
Data were collected through face-to-face interview using a pre-tested structured questionnaire. The questionnaire was adapted from similar studies and other related documents investigating KAP of LSM recommended for hypertension management.14,17,19,20,22,23 It contains all necessary variables regarding socio-demographics characteristics, KAP of LSM of the respondents. Data were collected by two BSc nurses who have had training on the subject matter and experience in data collection.
Data quality control
The quality of data was assured by pre-testing the questionnaire, training of the data collectors and supervising the data collection process. Well-designed questionnaire of English version was prepared by the investigators and translated in to local languages (Afaan Oromoo and Amharic). The instrument was pre-tested before the study period on 5% of the sample patients in Jugel Hospital which is located in Harar City, and amendments were made accordingly. The data collectors were given 1 day training concerning interviewing technique and appropriate data recording. Close supervision was made by investigators during the data collection through observation and review of the questionnaires filled and giving feedback to the data collectors.
Statistical analyses
Data were entered, cleaned and analyzed using SPSS Version 20 for windows. Appropriate descriptive statistics such as mean (with SD), median (with interquartile range (IQR)) and frequencies (with percentages) were used to describe the study population in relation to relevant variables. Bivariate and multivariate analysis with 95% confidence interval (CI) was employed to infer associations between the independent and dependent variables. Binary logistic regression was used to calculate the crude odds ratio (COR) with 95% CI. Each variable was entered into a logistic regression model so as to determine the presence of statistical significant association with the outcome variable. Multicollinearity among selected independent variables was checked through variance inflation factor (VIF), and none was found. All the explanatory variables with a P-value ⩽0.05 in the bivariate analyses were included in the final multivariable logistic model in order to identify the independent predictors of knowledge and practice of LSM. P-value <0.05 was considered statistically significant. Assumption on fitness of goodness of the final model was checked by Hosmer and Lemeshow test and was found fit.
Ethical consideration
Ethical approval was obtained from School of Pharmacy, College of Health and Medical Sciences, Haramaya University. A legal authorization letter was written from College of Health and Medical Sciences to study setting to get permission before data collection. The data collectors conducted interview after explaining the purpose of the study. Participation was on voluntary basis, and confidentiality was maintained to encourage accurate and honest self-disclosure. The information obtained was made anonymous and de-identified prior to analysis to ensure confidentiality.
Operational definition
Knowledge
In order to measure the level of knowledge toward LSM recommended for hypertension management among hypertensive patient, we used 10 multiple-choice questions. If respondents get the right answer, it was coded as Yes “1” if not it was coded as No “0.” The respondent’s knowledge scores were aggregated and ranged 0–10. Based on the cumulated score, respondents, who scored mean and above, were considered to have “Good knowledge”; while those who score below mean were considered as having “Poor knowledge” toward LSM to manage hypertension.
Attitude
To determine the level of attitude, a set of nine statements pertaining to LSM recommended for hypertension management among hypertensive patients were included in the questionnaire, and respondents were asked to record whether they agreed strongly, agreed slightly, had no opinion about the statement under consideration, disagree slightly, disagree strongly (a five-point Likert-type scale). Based on the cumulated score, respondents, who scored median value and above, were considered to have “favorable attitude”; while those who score below median were considered as having “unfavorable attitude” toward LSM.
Practice
In order to determine the extent of practice of LSM recommended for hypertension management among hypertensive patient, we used a set of nine multiple-choice questions. If respondents practiced correctly each question, it was coded as Yes “1” if not it was coded as No “0.” The respondent’s practice scores were aggregated and ranged 0–9. Based on the cumulated score, respondents, who scored mean and above, were considered to have “Good practice”; while those who score below mean were considered as having “Poor practice” toward LSM to manage hypertension.
Results
Socio-demographic characteristics
A total of 274 hypertensive patients participated in the study with a response rate of 94%. Half of the total respondents were females (138, 50.4%); 158 (57.7%) of the respondents were between ages 46 and 64 years. The mean age of the study participants was 56.36 years (±11.79, SD). Majority (250, 91.2%) of them were currently married; 204 (74.5%) were urban dwellers, 164 (59.9%) had formal education and 104 (38.0%) were government employee. Nearly two-third (63.5%) of the respondents had an average monthly income below 1000.00 Ethiopian Birr (ETB). Almost two-third (63.7%) of the respondents had normal (18.5–24.9) body mass index (BMI). The mean (±SD) BMI of the participants was 24.07 (±3.21) kg/m2. All the study participants were on antihypertensive medication (Table 1).
Table 1.
Socio-demographic characteristics of hypertensive patients at chronic care unit of HFSUH, Harar, Eastern Ethiopia, 2019 (N = 274).
| Variable | Category | Frequency | % |
|---|---|---|---|
| Sex | Male | 136 | 49.6 |
| Female | 138 | 50.4 | |
| Age (year) | ⩽45 | 48 | 17.5 |
| 46–64 | 158 | 57.7 | |
| ⩾65 | 68 | 24.8 | |
| Ethnicity | Oromo | 114 | 41.6 |
| Amhara | 124 | 45.3 | |
| Harari | 22 | 8.0 | |
| Others | 14 | 5.1 | |
| Religion | Christian | 182 | 66.4 |
| Muslim | 92 | 33.6 | |
| Marital status | Currently married | 250 | 91.2 |
| Not married | 24 | 8.8 | |
| Area of residence | Urban | 204 | 74.5 |
| Rural | 70 | 25.5 | |
| Educational status | No formal education | 110 | 40.1 |
| Formal education | 164 | 59.9 | |
| Occupation | Farmer | 34 | 12.4 |
| Government employee | 104 | 38.0 | |
| Merchant | 34 | 12.4 | |
| Housewife | 102 | 37.2 | |
| Body mass index (kg/m2) | <18.5 | 10 | 3.7 |
| 18.5–24.9 | 172 | 63.7 | |
| ⩾25 | 88 | 32.6 | |
| Average monthly income (ETB) | ⩽1000 | 174 | 63.5 |
| 1001–2500 | 46 | 16.8 | |
| ⩾2500 | 54 | 19.7 | |
| Duration on follow-up (year) | ⩽5 | 182 | 66.4 |
| >5 | 92 | 33.6 | |
| Duration on antihypertensive medication (year) | ⩽5 | 184 | 67.2 |
| >5 | 90 | 32.8 |
HFSUH: Hiwot Fana Specialized University Hospital; ETB: Ethiopian Birr.
Knowledge of hypertensive patients on LSM
A total of 10 knowledge questions were forwarded to assess the respondents’ level of knowledge toward LSM recommended for hypertension management. All 274 (100%) of the respondents were able to recall their recent BP measurement which was further confirmed by cross-checking their follow-up records. Of the respondents, 254 (92.7%) were able to mention at least one LSM recommended for hypertension management. Over two-third (71.5%) of them understood the importance of maintaining normal body weight to controlling their BP. Over three-fourth 78.8%, 77.4% and 78.8% knew the effect of drinking alcohol, smoking cigarette and chewing Khat on controlling BP, respectively (Table 2). Regarding the overall knowledge level of the respondents, 200 (73.0%) participants had good knowledge about LSM recommended for hypertension management (Figure 1).
Table 2.
Respondents level of knowledge toward LSM recommended for hypertension management among hypertensive patients at chronic care unit of HFSUH, Harar, Eastern Ethiopia, 2019 (N = 274).
| Knowledge questions | Yes (%) | No (%) |
|---|---|---|
| Knows recent BP measurement | 274 (100) | 0 (0) |
| Aware of LSM to manage hypertension | 252 (92.0) | 22 (8.0) |
| Can mention at least one LSM to manage hypertension | 254 (92.7) | 20 (7.3) |
| Knows the importance of maintaining normal body weight to controlling BP | 196 (71.5) | 78 (28.5) |
| Knows the importance of diet in controlling BP | 230 (83.9) | 44 (16.1) |
| Know the importance of reducing salt intake in controlling BP | 244 (89.1) | 30 (10.9) |
| Know the importance of regular physical activity in controlling BP | 244 (89.1) | 30 (10.9) |
| Know the effect of drinking alcohol on controlling BP | 216 (78.8) | 58 (21.2) |
| Know the effect of cigarette smoking on controlling BP | 212 (77.4) | 62 (22.6) |
| Know the effect of chewing Khat on controlling BP | 216 (78.8) | 58 (21.2) |
LSM: lifestyle modification; HFSUH: Hiwot Fana Specialized University Hospital; BP: blood pressure.
Figure 1.
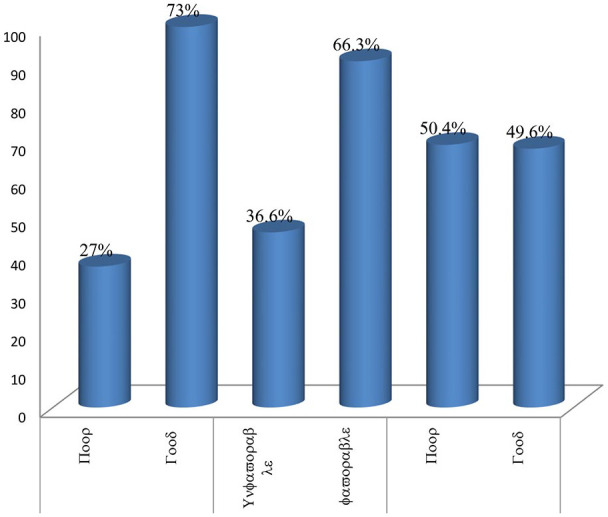
Overall respondents level of knowledge, attitude and practice status of LSM recommended for hypertension management among adult hypertensive patients at chronic care unit of HFSUH, Harar, Eastern Ethiopia, 2019 (N = 274).
Attitude of hypertensive patients on LSM
A total of nine attitude assessment questions were forwarded to respondents to assess their level of attitude toward LSM recommended for hypertension management. Majority (89.8%) of the respondents either strongly or slightly agreed on importance of education during their follow-up about LSM recommended for hypertension management. Three-fourth (76.6%) of the respondents either strongly or slightly agreed in importance of maintaining normal body weight to control their BP. Majority (79.6%) of the respondents either strongly or slightly disagree for the question stated as excessive alcohol intake has no effect on BP (Table 3). Regarding the overall attitude score of the respondents, 182 (66.4%) of the participants had favorable attitude toward LSM recommended for hypertension management (Figure 1).
Table 3.
Respondents level of attitude toward LSM recommended for hypertension management among hypertensive patients at chronic care unit of HFSUH, Harar, Eastern Ethiopia, 2019 (N = 274).
| Attitude question | Strongly agree (%) | Agree slightly (%) | Neutral (%) | Disagree slightly (%) | Strongly disagree (%) |
|---|---|---|---|---|---|
| Education during follow-up on LSM about hypertension is essential component of HTN management | 234 (85.4) | 12 (4.4) | 28 (10.2) | 0 (0) | 0 (0) |
| Regular checking of BP is important part of BP management | 256 (93.4) | 6 (2.2) | 12 (4.4) | 0 (0) | 0 (0) |
| Maintaining normal body weight is important for controlling BP | 202 (73.7) | 8 (2.9) | 64 (27.0) | 0 (0) | 0 (0) |
| Controlling diet is important for controlling BP | 230 (83.9) | 6 (2.2) | 36 (13.1) | 2 (0.73) | 0 (0) |
| Controlling salt intake is important for controlling BP | 244 (89.1) | 2 (0.73) | 28 (10.2) | 0 (0) | 0 (0) |
| Regular physical activity is important part of controlling BP | 244 (89.1) | 4 (1.5) | 24 (8.8) | 0 | 1 (0.73) |
| Excessive alcohol intake has no effect on BP | 16 (5.8) | 0 | 40 (14.6) | 2 (1.5) | 214 (78.1) |
| Khat chewing has no effect on BP | 18 (6.6) | 0 | 52 (19.0) | 4 (1.5) | 200 (73.0) |
| Smoking cigarette has no effect on BP | 16 (5.8) | 0 | 40 (14.6) | 2 (0.73) | 216 (78.8) |
LSM: lifestyle modification; HFSUH: Hiwot Fana Specialized University Hospital; BP: blood pressure; HTN: hypertension.
Practice level of hypertensive patients on LSM
A total of nine practice assessment questions were forwarded to respondents to assess their extent of practice toward LSM recommended for hypertension management. Regarding regular checking of BP and weight, almost all (96.4%) of the respondents regularly check their BP and below half (42.3%) check their body weight regularly. Majority (83.2%) of the respondents regularly conduct physical activity for about 30 min/day for most days of the week. Nearly half (42%) of the participants did not plan regularly to include diets rich in fruits, vegetables and low-fat dairy products in meal program. Significant proportion (19%) of hypertensive patients chews Khat (Table 4). Regarding the overall practice level of the respondents, 136 (49.6%) of the participants had good practice of LSM recommended for hypertension management (Figure 1).
Table 4.
Respondents level of practice toward LSM recommended for hypertension management among hypertensive patients at chronic care unit of HFSUH, Harar, Eastern Ethiopia, 2019 (N = 274).
| Practice question | Yes (%) | No (%) |
|---|---|---|
| Check BP regularly | 264 (96.4) | 10 (3.6) |
| Check weight regularly | 116 (42.3) | 158 (57.7) |
| Regularly plan to include diet rich in fruits, vegetables and low-fat dairy products in meal program | 158 (57.7) | 116 (42.3) |
| Regularly eat diet rich with high cholesterola | 42 (15.3) | 232 (84.7) |
| Regularly consume salt free or low salt diet | 222 (81.0) | 52 (19.0) |
| Regularly drink alcohola | 22 (8.0) | 252 (92.0) |
| Conduct physical activity regularly (at least 30 min/day, most days of the week) | 228 (83.2) | 46 (16.8) |
| Chew Khata | 52 (19.0) | 222 (81.0) |
| Smoke cigarettea | 12 (4.4) | 262 (95.6) |
LSM: lifestyle modification; HFSUH: Hiwot Fana Specialized University Hospital; BP: blood pressure.
For these practice questions, those who responded “Yes” were given “0” and responded “No” were given “1” for the purpose of analysis.
Factors associated with knowledge and practice of LSM
In multivariate logistic regression analysis, age, educational status and occupation of the respondents showed a significant association with knowledge of LSM. Those respondents in age range of 46–64 years were 4.08 times (adjusted odds ratio (AOR): 4.08, 95% CI: 1.14–14.56) more likely to have good knowledge of LSM than their younger (⩽45 years) counterparts. Respondents who attended formal education were almost four times (AOR: 3.93, 95% CI: 1.27–12.23) more likely to have good knowledge of LSM compared to those who did not attend formal education. The study also demonstrated that respondents who were government employee and housewives were eight times (AOR: 8.06, 95% CI: 1.40–46.32) and five times (AOR: 5.10, 95% CI: 1.26–20.79) more likely to have good knowledge of LSM compared to farmers (Table 5).
Table 5.
Bivariate and multivariate logistic regression analysis of factors associated with knowledge of LSM recommended for hypertension management among hypertensive patients at chronic care unit of HFSUH, Harar, Eastern Ethiopia, 2019 (N = 274).
| Variables | Category | Knowledge |
COR (95% CI) | P-value | AOR (95% CI) | P-value | |
|---|---|---|---|---|---|---|---|
| Poor (N = 37) | Good (N = 100) | ||||||
| Age group | ⩽45 | 22 (45.8%) | 26 (54.2%) | 1.00 | 1.00 | ||
| 46–64 | 40 (25.3%) | 118 (74.7%) | 2.50 (0.97–6.45) | 0.059 | 4.08 (1.14–14.56) | 0.03 | |
| ⩾65 | 12 (17.6%) | 56 (82.4%) | 3.95 (1.20–13.01) | 0.024 | 4.90 (0.87–27.71) | 0.07 | |
| Educational status | Non-educated | 54 (49.0%) | 56 (51.0%) | 1.00 | 1.00 | ||
| Educated | 20 (23.8%) | 144 (76.2%) | 6.94 (2.98–16.19) | <0.001 | 3.93 (1.27–12.23) | 0.02 | |
| Residence | Urban | 92 (70.8%) | 38 (29.2%) | 3.25 (1.43–7.38) | 0.005 | 1.967 (0.53–7.27) | 0.31 |
| Rural | 46 (63.9%) | 26 (36.1%) | 1.00 | 1.00 | |||
| Occupation | Farmer | 24 (70.6%) | 10 (29.4%) | 1.00 | <0.001 | ||
| Government employee | 10 (9.6%) | 94 (90.4%) | 22.56 (5.61–90.78) | 8.06 (1.40–46.32) | 0.02 | ||
| Merchant | 8 (23.5%) | 26 (76.5%) | 7.80 (1.69–36.06) | 0.009 | 3.49 (0.38–31.77) | 0.27 | |
| Housewife | 32 (31.4%) | 70 (68.6%) | 5.25 (1.58–17.42) | 0.007 | 5.10 (1.26–20.79) | 0.02 | |
| Average monthly income (ETB) | ⩽1000 | 60 (34.5%) | 114 (65.5%) | 1.00 | 1.00 | ||
| 1001–2500 | 8 (17.4%) | 38 (82.6%) | 2.50 (0.78–8.02) | 0.123 | 2.311 (0.37–14.49) | 0.37 | |
| ⩾2500 | 6 (11.1%) | 48 (88.8%) | 4.21 (1.17–15.13) | 0.028 | 2.528 (0.40–15.94) | 0.32 | |
| Duration on follow-up (year) | ⩽5 | 64 (35.9%) | 118 (64.8%) | 1.00 | 1.00 | ||
| >5 | 10 (10.9%) | 82 (89.1%) | 4.45 (1.60–12.37) | 0.004 | 3.007 (0.88–10.25) | 0.079 | |
LSM: lifestyle modification; HFSUH: Hiwot Fana Specialized University Hospital; ETB: Ethiopian Birr; COR: crude odds ratio; AOR: adjusted odds ratio; CI: confidence interval.
00: reference group.
In multivariate logistic regression analysis, only attitude had statistically significant association with respondents level of practice of LSM. Accordingly, respondents who had favorable attitude toward LSM recommended for hypertension management were over nine times (AOR: 9.20, 95% CI: 2.60–32.24) more likely to have good practice of LSM than those who had unfavorable attitude (Table 6).
Table 6.
Bivariate and multivariate logistic regression analysis of factors associated with practice of LSM recommended for hypertension management among hypertensive patients at chronic care unit of HFSUH, Harar, Eastern Ethiopia, 2019 (N = 274).
| Variables | Category | Practice |
COR (95% CI) | P-value | AOR (95% CI) | P-value | |
|---|---|---|---|---|---|---|---|
| Poor (N = 69) | Good (N = 68) | ||||||
| Educational status | Non-educated | 70 (63.6%) | 40 (36.4%) | 1.00 | 1.00 | ||
| Educated | 68 (41.5%) | 96 (58.5%) | 2.47 (1.22–4.99) | 0.012 | 1.149 (0.44–3.03) | 0.779 | |
| Occupation | Farmer | 24 (70.6%) | 10 (29.4%) | 1.00 | 1.00 | ||
| Government employee | 38 (36.5%) | 66 (63.5%) | 4.17 (1.27–13.65) | 0.018 | 1.64 (0.39–6.86) | 0.882 | |
| Merchant | 16 (47.1%) | 18 (52.9%) | 2.70 (0.66–11.09) | 0.168 | 1.31 (0.27–6.42) | 0.753 | |
| House wife | 70 (50.8%) | 42 (41.2%) | 1.68 (0.52–5.48) | 0.390 | 0.92 (0.25–3.42) | 0.364 | |
| Knowledge | Poor | 58 (78.4%) | 16 (21.0%) | 1.00 | 1.00 | ||
| Good | 80 (40%) | 120 (60.0%) | 5.437 (2.26–13.10) | <0.001 | 1.32 (0.38–4.60) | 0.661 | |
| Attitude | Unfavorable | 76 (82.6%) | 16 (17.4%) | ||||
| Favorable | 62 (34.1%) | 120 (65.9%) | 5.09 (2.33–11.13) | <0.001 | 9.20 (2.60–32.24) | 0.001 | |
LSM: lifestyle modification; HFSUH: Hiwot Fana Specialized University Hospital; COR: crude odds ratio; AOR: adjusted odds ratio; CI: confidence interval.
00: reference group.
Discussion
Hypertension remains as one of the most important public health challenges worldwide because of the associated morbidity, mortality and cost to the society. Despite the availability of safe and effective antihypertensive medications and the existence of clear treatment guidelines, hypertension is still inadequately controlled in a large proportion of patients worldwide. Unawareness and negative attitude toward LSM, which is important part of hypertension management, remain a major challenge.24 This study assessed the level of KAP of LSM and associated factors among hypertensive patients.
In the present study, 73.0% of the participants had good knowledge about LSM recommended for hypertension management. This is consistent with study conducted in Bishoftu, Ethiopia20 where 72.3% of the participants had good knowledge toward LSM recommended for hypertension management. However, our study finding is higher than studies conducted in Ghana,17 North-Western Nigeria,18 South-Western Nigeria,22 South-East Nigeria25 and Imo Nigeria23 where only 30%, 31%, 33%, 42.6% and 26.7% patients had good knowledge toward LSM recommended for hypertension management, respectively. The difference in the study finding could be due to difference in study setting, residence and educational status. Unlike our study, some studies were community based,23,25 some conducted on rural dwellers23 and the other was conducted on patients which in majority had no formal education (68.3%).18
Two-third (66.4%) of our study participants had favorable attitude toward LSM recommended for hypertension management. This is consistent with findings from other hospital-based study in Bishoftu, Ethiopia,20 Enugu, Nigeria22 and Turkey26 where more than 50% of the participants had positive attitude toward LSM. However, it is lower than finding of study in North-Western Nigeria where almost all (99%) of the study participants had positive attitude. The discrepancy might be due to the difference in attitude measurement. In our study, we used median to classify level of attitude toward LSM whereas in Nigerian study they categorized attitude as positive if respondents score between 23 and 44 and as negative if respondents score between 0 and 22 out of 44.
Regarding the overall practice level of the respondents, nearly half (49.6%) had good practice of LSM recommended for hypertension management. This finding is comparable with studies reported from South-East (42.5%) and North-West (56.7%) Nigeria.18,25 However, the finding is higher than study conducted in southern Ethiopia19 where only 27.3% of the participants had practiced recommended LSMs. The difference could be due to difference in study setting. Unlike the southern Ethiopia study which was conducted in General hospitals, the present study is conducted in specialized university hospital where health service is provided through collaborative effort of health professionals from different specialized fields. The other reason may be due to difference in level of awareness about LSM. In present study, 92.0% were aware of LSM recommended for hypertension management whereas in study conducted in south Ethiopia significant proportions (42.4%) not hear information about LSM.
In this study age, educational status and occupation of the respondents showed a significant association with knowledge of LSM in multivariate logistic regression analysis. Those respondents who were in age range of 46–64 years were 4.08 times more likely to have good knowledge of LSM than their younger (⩽45 years) counterparts (AOR: 4.08, 95% CI: 1.14–14.56, P = 0.03). This association is possibly explained as with increasing age one can learn more from experience. The other possible justification is that out of 164 (59.8%) respondents from the category of formal education, majority (58.5%) were in the age range of 46–64 years. In our study, there was no association between age ⩾65 years and knowledge of LSM. This could be due to older persons have less education, decreased cognitive function and more co-morbidities which may decrease their level of understanding.
Respondents who attended formal education were almost four times more likely to have good knowledge of LSM compared to those who did not attend formal education (AOR: 3.93, 95% CI: 1.27–12.23, P = 0.02). The association between effect of educational background and knowledge of LSM was further supported by study from Ghana.17 Having formal education plays a positive role in increasing the knowledge of respondents about LSM recommended for hypertension management. Educated clients would have better access to health-related information than non-educated clients and would have greater autonomy to make decision and have greater ability to use quality health care services. In other way, illiteracy may reduce the ability of clients to understand issues during counseling.
The study also demonstrated that respondents who were government employee were eight times more likely to have good knowledge of LSM compared to farmers (AOR: 8.06, 95% CI: 1.40–46.32, P = 0.02). Similarly, respondents whose occupation was housewives were five times more likely to have good knowledge of LSM compared to farmers (AOR: 5.10, 95% CI: 1.26–20.79, P = 0.02).
In the present study, only attitude had statistically significant association with level of practice of LSM in multivariate analysis. Accordingly, respondents who had favorable attitude toward LSM recommended for hypertension management were over nine times more likely to have good practice of LSM than those who had unfavorable attitude (AOR: 9.20, 95% CI: 2.60–32.24, P = 0.001). This means the better the patients had positive attitude toward LSM, the better they practiced healthy LSM. This was further supported by study conducted to assess KAP toward LSM among type 2 diabetic mellitus patients.27
In current study, age, educational status and monthly income did not show significant association with practice of LSM. This is in contrast to previous study conducted in southern Ethiopia where these variables showed significant association with practice of LSM.19 A possible explanation could be due to difference in study setting. In our study, there was no significant association between knowledge and practice of LSM. This means that being knowledgeable did not necessarily willingness to observe healthy lifestyle habits. This was also supported by another study.27
Although the study has many strengths, yet the study does have some limitations. First, the study is a single-center study. In addition, the data were self-report from the participants; hence, poor attitudes and practices might be denied, which affect the result of the study.
Conclusion
The study found that levels of knowledge and attitude toward LSM recommended for hypertension management were fairly good but practice level was poor. Age range of 46–64 years, having formal education, being government employee and being housewives were factors significantly associated with good knowledge of LSM, whereas favorable attitude was the only factor significantly associated with good LSM practice. Therefore, an integrated effort from different health discipline is needed to improve patient’s KAP toward LSM for hypertension management.
Acknowledgments
The authors would like to thank the hospital officials, data collectors and study participants for their contribution.
Footnotes
Author contributions: S.B., K.M.M, A.T., A.N.M. and Y.A. conceived the study, participated in the design, data analysis and interpretation of the result. S.B., K.M.M., A.T., A.N.M. and Y.A. were involved in data acquisition and writing the draft manuscript. K.M.M., S.B., A.T., A.N.M. and Y.A. critically reviewed the manuscript. All authors read and approved the manuscript.
Availability of data and materials: Please contact the author for data requests.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from Research Ethics Review Committee, School of Pharmacy, College of Health and Medical Sciences, Haramaya University (ethics approval number: SOP/2399/03/2019).
Informed consent: Written informed consent was obtained from all subjects before the study.
ORCID iDs: Kirubel Minsamo Mishore  https://orcid.org/0000-0001-9931-1068
https://orcid.org/0000-0001-9931-1068
Assefa Tola  https://orcid.org/0000-0002-2155-6097
https://orcid.org/0000-0002-2155-6097
Yohanes Ayele  https://orcid.org/0000-0002-6473-7752
https://orcid.org/0000-0002-6473-7752
References
- 1. World Health Organization. A global brief on hypertension: World Health Day, 2013, https://www.who.int/cardiovascular_diseases/publications/global_brief_hypertension/en/#:~:text=The%20Global%20brief%20on%20hypertension%2C%20published%20on%20the%20occasion%20of,and%20premature%20death%20and%20disability.
- 2. Local Experts focus on problems of detecting treating hypertension in Africa First Pan-African meeting on hypertension which took place December 2–5, 2005 in Yaoundé, Cameroon. Medscape Cardiol 2006; 10(1). [Google Scholar]
- 3. Khan MU, Shah S, Hameed T. Barriers to and determinants of medication adherence among hypertensive patients attended National Health Service Hospital, Sunderland. J Pharm Bioallied Sci 2014; 6(2): 104–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Vrijens B, Vincze G, Kristanto P, et al. Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ 2008; 336: 1114–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bosu WK, Reilly ST, Aheto JMK, et al. Hypertension in older adults in Africa: a systematic review and meta-analysis. PLoS ONE 2019; 14(4): e0214934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ibekwe R. Modifiable risk factors of hypertension and socio-demographic profile in Oghara, Delta state; prevalence and correlates. Ann Med Health Sci Res 2015; 5(1): 71–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pilakkadavath Z, Shaffi M. Modifiable risk factors of hypertension: a hospital-based case-control study from Kerala, India. J Family Med Prim Care 2016; 5(1): 114–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Unnissa G, Swamy KK. Diet and heart disease. 3rd ed. Secunderabad: National Institute of Nutrition, 1998, pp. 65–70. [Google Scholar]
- 9. Yang MH, Kang SY, Lee JA, et al. The effect of lifestyle changes on blood pressure control among hypertensive patients. Korean J Fam Med 2017; 38(4): 173–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. van de Vijver S, Akinyi H, Oti S, et al. Status report on hypertension in Africa—consultative review for the 6th session of the African union conference of ministers of health on NCD’s. Pan Afr Med J 2013; 16: 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wods LS. Cardiac nursing. 5th ed. Philadelphia, PA: Lippincott Williams, 2005, p. 85. [Google Scholar]
- 12. Al-Gelban KS, Khan MY, Al-Khaldi YM, et al. Adherence of primary health care physicians to hypertension management guidelines in the Aseer region of Saudi Arabia. Saudi J Kidney Dis Transpl 2011; 22(5): 941–948. [PubMed] [Google Scholar]
- 13. Anthony H, Valinsky L, Inbar ZGC, et al. Perceptions of hypertension treatment among patients with and without diabetes. BMC Family Practice 2012; 13: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American heart association task force on clinical practice guidelines. J Am Coll Cardiol 2018; 71: 127–248. [DOI] [PubMed] [Google Scholar]
- 15. Aronow WS. Lifestyle measures for treating hypertension. Arch Med Sci 2017; 13(5): 1241–1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Nicoll R, Henein MY. Hypertension and lifestyle modification: how useful are the guidelines. Br J Gen Pract 2010; 60(581): 879–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Marfo AF, Owusu-Daaku F, Addo MO, et al. Ghanaian hypertensive patients understanding of their medicines and lifestyle modification for managing hypertension. Int J Pharm Pharmaceut Sci 2014; 6(4): 165–170. [Google Scholar]
- 18. Hadiza S, Yakasai AM, Yau JA, et al. Factor analysis of knowledge, attitude and practice of life style modification measures among hypertensive patients in North-Western Nigeria. J Med Res 2017; 3(2): 74–78. [Google Scholar]
- 19. Buda ES, Hanfore LK, Fite RO, et al. Lifestyle modification practice and associated factors among diagnosed hypertensive patients in selected hospitals, South Ethiopia. Clin Hypertens 2017; 23: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Daniel DSRK. Assessment of knowledge, attitude and practice of hypertensive patients towards the non-medical management of hypertension in Bishoftu General Hospital, 2016. Pharmaceut Chem J 2017; 4(1): 48–59. [Google Scholar]
- 21. Tibebu A, Mengistu D, Negesa L. Adherence to recommended lifestyle modifications and factors associated for hypertensive patients attending chronic follow-up units of selected public hospitals in Addis Ababa, Ethiopia. Patient Prefer Adherence 2017; 11: 323–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ike SO, Aniebue PN, Aniebue UU. Knowledge, perceptions and practices of lifestyle-modification measures among adult hypertensives in Nigeria. T R Soc Trop Med Hyg 2010; 104(1): 55–60. [DOI] [PubMed] [Google Scholar]
- 23. Osuala EO, Abimbola OO, Kadiri S. Knowledge, attitude to hypertension and lifestyle habits of rural Dwellers in Owerri–Nkwoji, Imo State, Nigeria. J Public Health Epidiol 2014; 6: 48–51. [Google Scholar]
- 24. Begum ML, Dhar SP, Mahmud A, et al. Knowledge, attitude and practice of life style modification in the management of hypertension. Med Clin Res 2017; 2(3): 1–4. [Google Scholar]
- 25. Okwuonu CG, Emmanuel CI, Ojimadu NE. Perception and practice of lifestyle modification in the management of hypertension among hypertensives in South east Nigeria. Int J Biomed Res 2014; 3: 121–131. [Google Scholar]
- 26. Heymann AD, Gross R, Tabenkin H, et al. Factors associated with hypertensive patients’ compliance with recommended lifestyle behaviors. Isr Med Assoc J 2011; 13(9): 553–557. [PubMed] [Google Scholar]
- 27. Adem AM, Gebremariam ET, Gelaw BK, et al. Assessment of knowledge, attitude, and practices regarding lifestyle modification among type 2 diabetic mellitus patients attending Adama Hospital Medical College, Oromia region, Ethiopia. Global J Med Res 2014; 14(7): 37–48. [Google Scholar]


