Abstract
A new viral disease named COVID-19 spread rapidly into a pandemic in early 2020. Most countries have active community transmission and imposed measures such as social distancing and travel restrictions to mitigate its effect. Many sporting events all over the globe were canceled or postponed. In this article, we briefly discuss some important topics regarding the COVID-19 pandemic and propose a strategy to manage return to play in professional athletes. We searched the PubMed and Google Scholar databases to identify articles published through May 12, 2020, using the following keywords: “coronavirus,” “COVID-19,” “SARS-CoV-2,” “athlete,” and “return to play.” Although athletes have a lower risk of severe disease, preventive measures are still very important for minimizing time away from training, avoiding potential complications, slowing the pandemic spread, and ultimately protecting the health of those with a higher risk of complications and death. Athletes may present with mild disease, but complications such as pulmonary fibrosis and myocardial injuries have to be considered. Although still controversial, athletes should be evaluated before return to play and monitored accordingly afterward via proper clinical assessments and testing.
Keywords: athlete, COVID-19, return to play, preparticipation
In December 2019, a new coronavirus (SARS-CoV-2) was found to be causing an outbreak of severe acute respiratory syndrome in Wuhan, China.21 The virus spread rapidly over several provinces and then globally. The disease caused by this new virus was named COVID-19 (coronavirus disease 2019). On March 11, 2020, the World Health Organization declared COVID-19 to be a pandemic because of the large number of people affected worldwide. Currently, the situation is in the pandemic phase (phase 6), with increased and sustained transmission in the general population. Most countries now have active community transmission and are trying to mitigate the effect of the disease using measures such as social distancing and travel restrictions.
In the sports industry, preventive measures among athletes and staff were initially enforced, followed quickly by events held without spectators and eventually the cancellation or postponement of these events (eg, Summer Olympic Games and Union of European Football Associations European Football Championship).
Historically, pandemics usually last for 12 to 36 months. To decrease the duration of this period, a highly effective treatment protocol, yet to be discovered, and/or achieving group immunity would be necessary. Vaccine development usually takes several years, and it is estimated that, according to the transmissibility of the virus, more than 60% of the population needs to be infected and gain long-term protection to achieve group immunity.
The clinical manifestations of COVID-19 are mainly respiratory, and the clinical course is usually mild. However, a small percentage of patients, especially the elderly and those with comorbidities, can develop a severe condition, with several complications and poor outcomes, including death. Although the most frequent severe complications associated with SARS-CoV-2 involve the airways, other systems, namely the cardiovascular, can be affected.
The effect of this new disease on athletes’ health and performance remains unknown, and physicians will face several challenges before return to play (RTP) is permitted. In this article, we present a brief discussion of crucial topics and possible solutions for the management of athletes in the context of the COVID-19 pandemic.
For this review, we searched the PubMed and Google Scholar databases to identify English-written articles published up to May 12, 2020, using the following keywords: “coronavirus,” “COVID-19,” “SARS-CoV-2,” “athlete,” and “return to play.” In addition, we manually searched the reference lists of most primary articles.
COVID-19 Is Clinically Relevant
The clinical presentation of COVID-19 ranges from asymptomatic or mild symptoms to severe illness and death. The most common symptoms are fever and coughing, with severe illness occurring in 16% of the patients after hospital admission.6 In a study of 72,314 cases reported in China, 81% of cases were mild (absent or mild pneumonia); 14%, severe (hypoxia, dyspnea, >50% lung involvement within 24-48 hours); and 5%, critical (shock, respiratory failure, multiorgan dysfunction). Of all confirmed cases in this series, 2.3% resulted in death.20
Pneumonia and acute respiratory distress syndrome are the main respiratory complications of COVID-19. A meta-analysis reported respiratory failure or acute respiratory distress syndrome, a life-threatening lung injury, in 20% of the patients.22 The long-term effects of these complications remain to be clarified, but some patients could develop pulmonary fibrosis. In these cases, reduced lung function may persist, with a pattern of restrictive lung disease, leading to decreased exercise capacity.5 Some reports of patients who recovered from COVID-19 have shown a 20% to 30% drop in lung function.
Although most complications involve the airways, cardiac, liver, and kidney dysfunction have also been reported. In fact, cardiac involvement is somewhat frequent, mainly in critically ill patients admitted to intensive care units, and has been implicated in those with the worst outcomes. Among cardiac complications, myocarditis (including fulminant cases), malignant arrhythmia, acute heart failure, and acute coronary syndromes have been reported.8 In some cohorts, up to 20% of patients have shown elevated troponin levels, including asymptomatic patients without known cardiovascular risk factors or previous cardiac disease. This increased level of troponin corresponds to acute myocardial injuries and myocarditis, documented in 8.0% of 1527 patients included in a meta-analysis.15 The mechanisms responsible for acute myocardial injuries in patients with COVID-19 are poorly understood, but an inflammatory reaction with a cytokine storm is the most likely hypothesis.8
The clinical course of acute disease may be important in evaluations before athletes resume sports because the persistence of some structural or functional changes, especially cardiac and respiratory, could influence physical performance and constitute a trigger for exercise-related clinical complications, including sudden death.
Not only must clinicians be aware of the potential chronic complications of COVID-19, but they should also anticipate the potential long-term adverse effects of some therapeutic modalities being implemented (eg, anti-inflammatory drugs, antimalarial drugs, antiviral drugs, steroids, or immunosuppressants).4
Immune System Response in Athletes
Susceptibility to a viral infection depends largely on the viral load and virulence, the host’s general health status, and innate and adaptive immune system responses.16 SARS-CoV-2 is a highly infectious coronavirus that can be transmitted by asymptomatic carriers over a relatively long period. While engaging in regular moderate exercise is beneficial in improving the immune system and preventing viral infections, an asymptomatic athlete can potentially infect others in close proximity if preventive measures are not taken.16
The immune system can become temporarily suppressed when performing acute bouts of prolonged endurance exercise. Competitive athletes must train at increased intensive workloads to improve their physical condition, potentially placing them at a higher risk of upper respiratory tract infections.7,11,16 Athletes should be closely monitored with respect to training loads, nutritional aspects, and sleeping and mood patterns to recognize the early signs of overtraining.
How to Prevent an Infection
Athletes have a higher risk of transmission when they do not adhere to social distancing or personal hygiene measures. Athletes frequently train in groups, engage in contact and team sports, share training equipment and practice surfaces, or travel in aircrafts and other closed-environment collective vehicles.7,16 SARS-CoV-2 remains viable in aerosols for up to 3 hours and is detectable on steel and plastic for up to 3 days.19 Respiratory droplets can float for a longer time in steam and vapor-rich environments, such as a changing room, which also enhances the risk of transmission.16 Some proposed preventive measures are summarized in Table 1.
Table 1.
Measures to Prevent SARS-CoV-2 Infections in Athletes
| Avoid unnecessary contact with infected people or surfaces |
| Wear a mask whenever outside or in contact with an infected person |
| Monitor temperature daily before practice |
| Frequently wash hands |
| Cover the mouth and nose when coughing or sneezing |
| Safely discard used tissue paper |
| Properly cover foods before serving |
| Use individual cutlery, cups, and dishes |
| Avoid steam and vapor-rich environments, such as changing rooms |
| Avoid traveling in closed-environment collective vehicles |
| Shower before (in contact sports) and after training or competitions |
| Change and launder clothing used in daily training |
| Disinfect equipment and training surfaces with diluted bleach before and after each utilization |
| Clean any minor abrasions with water and soap before applying antiseptic solution and bandages |
Training Outside…With a Mask?
Training outside has been permitted in most countries. If running or cycling outdoors is not feasible, athletes must comply with social distancing guidelines and other preventive measures. Distancing between individual persons has been recommended at 1.5 to 2.0 m, which is based on the dispersal of influenza virus–infected respiratory droplets (up to 1.829 m or 6 ft)2 and assumes that the majority of respiratory droplets either fall to the ground or evaporate before reaching said distance. However, unpublished data by B. Blocken et al (2020, unpublished) have suggested that, while this distance may be appropriate for people standing still, it does not consider the airflow patterns generated by the person’s movement. This group performed an aerodynamics study that simulated microdroplet dispersion of up to 5 m when slipstream walking at 4 km/h and up to 10 m when slipstream running at 14.4 km/h, thus alerting athletes who are training outdoors of the need to further increase interpersonal distances to be protected.
Wearing a mask is one preventive measure and is recommended when circulating outside of the house, but it can be burdensome while exercising. It must be kept in mind that the higher the respiratory flow rate through a surgical mask, the higher the penetration rate of aerosols; at rest, the penetration rate is 25%, and it is much higher while exercising.16 At near maximal ventilation flow rates, a surgical mask provides little protection and may also contribute to re-aerosolization of the trapped virus. Moreover, above the second ventilatory threshold and close to maximal loading, masks can hamper exercise performance, an effect attributed to an increase in inspiratory resistance and inspiratory time, with decreased tidal volume and increased peak inspiratory pressure and CO2 retention.16 Therefore, for the professional athlete performing at the highest intensity, using a mask may not be recommended.
How to Manage an Athlete With COVID-19
It is controversial as to whether an athlete can train with symptoms of an acute infectious illness. Despite not being evidence-based, the “neck check” rule is often applied in sports medicine to clear (or not) an athlete to train. If the symptoms are only “above the neck” (eg, rhinorrhea, nasal congestion, sore throat, or sneezing), the athlete is allowed to train at a lower intensity level than usual; if any “below the neck” symptoms are present (eg, fever, malaise, severe coughing, gastrointestinal symptoms, or myalgia), the athlete should not train.9
While COVID-19 is associated with high morbidity and mortality for people older than 60 years or those with chronic clinical conditions, it is important to remain vigilant with younger, healthier, and physically fit people.7 Athletes may experience only mild symptoms such as headaches, sore throat, rhinorrhea, fatigue, and muscle aches, and, similar to other young people, might recover over 5 to 7 days.7 There is, however, evidence that a second phase of possible clinical deterioration can occur 7 to 9 days after onset.7
As with other illnesses, athletes with COVID-19 who develop a fever must not be allowed to train and must seek immediate medical advice, ideally staying at home until told otherwise.16 Until more is known about this pandemic, COVID-19 must always be included in the differential diagnosis, especially in the presence of unusual symptoms such as anosmia and ageusia. For that reason, any symptomatic athlete should abstain from training, and return to training after COVID-19 should be more conservative than with other simpler upper respiratory tract infections, consisting of a more prolonged rest period (at least 7 days from symptom resolution).7,16 It is recommended that swabs for reverse transcription polymerase chain reaction testing be collected from both the oropharynx and nasopharynx and that the patient be quarantined at home for another 2 weeks after hospital discharge. It is reasonable that this 2-week period is also followed when clearing the athlete to use any club facilities.3
Toresdahl and Asif18 suggested that, for athletes with COVID-19, low-intensity training may be attempted during the period after the complete resolution of symptoms, provided that the athlete remains isolating at home and that progression to regular training may occur afterward.15 Although no case reports have been published for athletes with COVID-19 to date, after the symptomatic period, any signs or symptoms consistent with postviral fatigue syndrome should be identified and managed accordingly.
When and How to Return to Play
Before clearing an athlete to RTP, one must ensure individual and collective safety conditions. All athletes who have recovered from COVID-19 should undergo a precompetitive evaluation. Even those who are asymptomatic or have a mild disease evolution can present with subclinical lesions associated with exercise-induced complications.3 Among these lesions, cardiac fibrosis and pulmonary fibrosis are the most relevant, constituting a potential trigger for clinical complications such as cardiac dysfunction, malignant arrhythmia, and a reduction of lung capacity. It should be highlighted that myocarditis is an underdiagnosed cause of sudden death in athletes that must also be excluded in this setting.
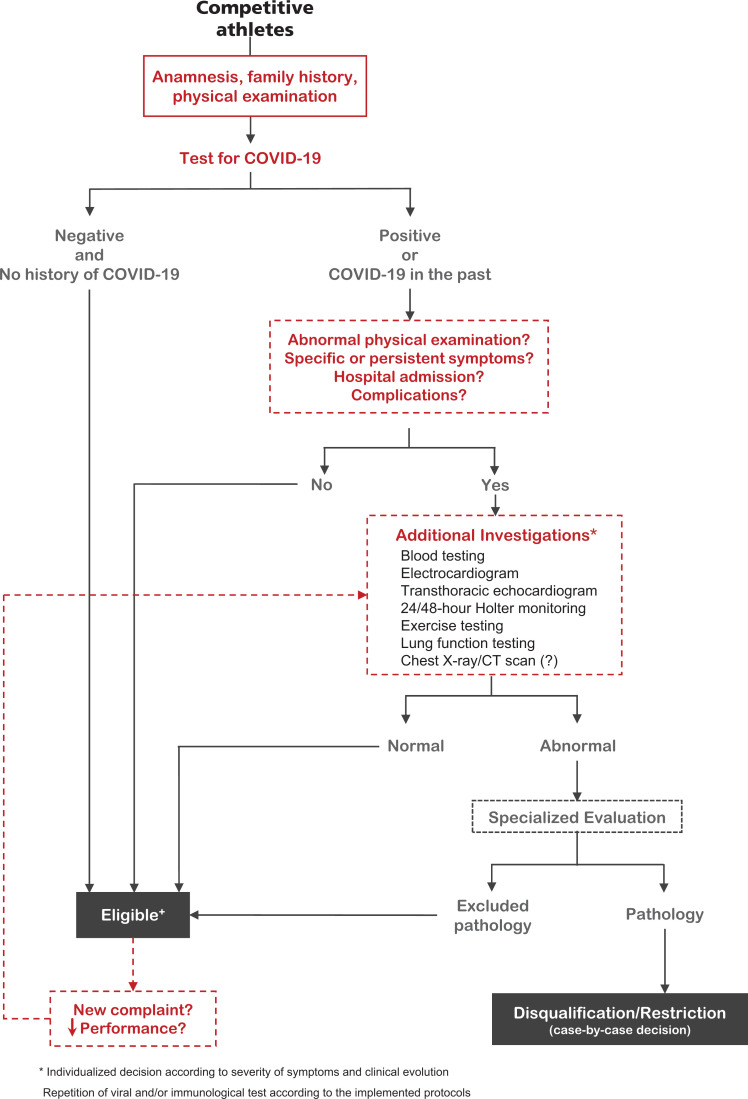
All athletes (whether asymptomatic, mildly sick, or untested) must be thoroughly evaluated before resuming exercise training. This evaluation may be complemented with additional examinations, including blood tests, electrocardiograms, transthoracic echocardiograms, maximal exercise testing, 24-hour Holter monitoring, or lung function tests.4 The examinations to include in preparticipation screening should be selected according to the presentation and severity of the disease (eg, asymptomatic, mild symptoms, hospital admission, or intensive care unit admission). Particularly in exercise testing and lung function assessments, it is important to ensure safety and minimize the risk of transmission, following all recommended protective measures. In the current phase of the pandemic, it may be difficult to find available facilities to perform exercise testing, and thus, other assessments should be considered for low-risk patients according to clinical manifestations.4 The infection status must be verified by viral reverse transcription polymerase chain reaction and serology-based testing, which is repeated when indicated. In addition, cardiac signs/symptoms suggestive of myocarditis, ongoing myocardial injuries (troponin measurements), and arrhythmia (24- to 48-hour Holter monitoring) must be excluded. Athletes with abnormal findings or those with a more serious clinical evolution of the disease (eg, need for hospital admission) should undergo more specific examinations, such as cardiac magnetic resonance imaging for the suspicion of myocarditis. Athletes with a definite diagnosis of myocarditis must undergo a period of detraining of 3 to 6 months and should be re-evaluated before resuming training to confirm the normalization of left ventricular systolic function, serum biomarkers of a myocardial injury, and absence of clinically significant arrhythmia at rest and during exercise.4,18 In Figure 1, we propose a workflow for evaluating professional athletes before clearing them to RTP.
Figure 1.
Clinical evaluation of professional athletes before return to play. All competitive athletes should undergo a clinical evaluation and be tested for an active SARS-CoV-2 infection. Athletes who have had suspected or confirmed COVID-19 in the past, or who are now positive, and present with suggestive symptoms or abnormal physical examination findings, or have a history of recent hospital admission or complications due to COVID-19, should undergo additional assessments according to the presentation and severity of the disease. Throughout this process, physicians should remain attentive to any athletes developing new symptoms or those with decreased performance, even if they tested negative previously. CT, computed tomography.
A simple mnemonic to reinforce the main steps before RTP is “TEAM”: Test (virus/immunity status), Evaluate (clinical signs and symptoms), Assess (blood, heart, and lungs), and Mask (prevention and protection) (Figure 2).
Figure 2.

Proposed approach to return to play (RTP): “TEAM.” The main steps before RTP are the following: Test (virus/immunity status), Evaluate (clinical signs and symptoms), Assess (blood, heart, and lungs), and Mask (prevention and protection).
Mental Health
Exercise has a beneficial effect on mental health by reducing the risk of anxiety and depression. The COVID-19 pandemic has caused a paradigm shift in the normal routines of almost every citizen in the world. Confinement and social distancing can be detrimental to an athlete’s mental health. Athletes may currently be facing questions such as uncertainty of if/when competitions will resume and loss of income. Other factors, such as excessive unoccupied time, worse training routines, isolation away from their home (eg, if under mandatory isolation at a training location in a different country), fear of becoming ill or infecting others, and lack of a healthy sleeping or nutritional routine, can also be present.7 It is important for support teams to monitor any athlete under these conditions or with previous mental health issues to respond more rapidly to any imbalances.13
Injury Prevention
Despite the fact that most professional athletes continue training in isolation during the confinement period, it is important that sufficient time be provided to achieve the same fitness level as before the lockdown. Under these conditions, training should ideally be monitored remotely by a strength and conditioning coach or exercise physiologist for the correct technical execution of exercises, physiological parameter monitoring, and injury prevention.12
If sports governing bodies decide to resume and finish competitions before the beginning of the new season, it will result in a very congested calendar. A football study showed that, during a congested period, there is a higher risk of muscle injuries, specifically the hamstring and quadriceps.1 In addition, ≤4 days of recovery between matches has been associated with a higher risk of injuries in comparison with that with ≥6 days of rest.18 According to the International Olympic Committee consensus statement on loading in sports, if there are fewer than 4 days of rest between matches, squad rotation should be considered.17
Team physicians must acknowledge that, upon returning to normal training and competitions this season, overscheduling competitive moments may play an important role in not only acute and overuse musculoskeletal injuries but also acute illnesses.14,17 More than ever, load management and injury prevention strategies must be implemented.10,14,17
“Stay at Home” (Take-Home) Message
COVID-19 is a new disease with an enormous socioeconomic effect. The possibility of a second peak could threaten the sustainability of national health systems, and political decisions must take into account the medical and scientific community. Until there is an effective treatment or cure, one must be cautious about the reliability of viral and serological tests.
Sports medicine is facing many challenges during this new pandemic. While no effective treatment or cure is available, one must proceed with extreme caution when resuming sporting activities for both professional and recreational athletes. The mediagenic exposure of elite athletes and the social responsibility of sports will likely pave the way for the management of return to sports for the general population, balancing the risks with the multiple benefits of physical exercise for health.
There is still much to be learned, and only by playing as a “TEAM” can we defeat COVID-19 so that athletes can return to the playing field as quickly and safely as possible.
Footnotes
Final revision submitted July 9, 2020; accepted July 28, 2020.
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Bengtsson H, Ekstrand J, Hägglund M. Muscle injury rates in professional football increase with match congestion: an 11-year follow up of the UEFA Champions League injury study. Br J Sports Med. 2013;47(12):743–747. [DOI] [PubMed] [Google Scholar]
- 2. Bischoff WE, Swett K, Leng I, Peters TR. Exposure to influenza virus aerosols during routine patient care. J Infect Dis. 2013;207:1037–1046. [DOI] [PubMed] [Google Scholar]
- 3. Chen D, Xu W, Lei Z, et al. Recurrence of positive SARS-CoV-2 RNA in COVID-19: a case report. Int J Infect Dis. 2020;93:297–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dores H, Cardim N. Return to play after COVID-19: a sport cardiologist’s view. Published online May 7, 2020 Br J Sports Med. doi:10.1136/bjsports-2020-102482 [DOI] [PubMed] [Google Scholar]
- 5. George PM, Wells AU, Jenkins RG. Pulmonary fibrosis and COVID-19: the potential role for antifibrotic therapy. Lancet Respir Med. 2020;8(8):807–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Guan W, Ni Z, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hull JH, Loosemore M, Schwellnus M. Respiratory health in athletes: facing the COVID-19 challenge. Lancet Respir Med. 2020;8(6):557–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol. 2020;5(7):831–840. doi:10.1001/jamacardio.2020.1286 [DOI] [PubMed] [Google Scholar]
- 9. Metz JP. Upper respiratory tract infections: who plays, who sits? Curr Sports Med Rep. 2003;2(2):84–90. [DOI] [PubMed] [Google Scholar]
- 10. Mugele H, Plummer A, Steffen K, Stoll J, Mayer F, Müller J. General versus sports-specific injury prevention programs in athletes: a systematic review on the effect on injury rates. PLoS One. 2018;13(10):e02056 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Nieman DC. Upper respiratory tract infections and exercise. Thorax. 1995;50(12):1229–1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pelliccia A, Solberg EE, Papadakis M, et al. Recommendations for participation in competitive and leisure time sport in athletes with cardiomyopathies, myocarditis, and pericarditis: position statement of the Sport Cardiology Section of the European Association of Preventive Cardiology (EAPC). Eur Heart J. 2019;40(1):19–33. [DOI] [PubMed] [Google Scholar]
- 13. Reardon CL, Hainline B, Aron CM, et al. Mental health in elite athletes: International Olympic Committee consensus statement (2019). Br J Sports Med. 2019;53(11):667–699. [DOI] [PubMed] [Google Scholar]
- 14. Schwellnus M, Soligard T, Alonso JM, et al. How much is too much? (Part 2) International Olympic Committee consensus statement on load in sport and risk of illness. Br J Sports Med. 2016;50(17):1043–1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Shi S, Qin M, Shen B, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5(7):802–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. So RC, Ko J, Yuan YW, Lam JJ, Louie L. Severe acute respiratory syndrome and sport: facts and fallacies. Sports Med. 2004;34(15):1023–1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Soligard T, Schwellnus M, Alonso JM, et al. How much is too much? (Part 1) International Olympic Committee consensus statement on load in sport and risk of injury. Br J Sports Med. 2016;50(17):1030–1041. [DOI] [PubMed] [Google Scholar]
- 18. Toresdahl BG, Asif IM. Coronavirus disease 2019 (COVID-19): considerations for the competitive athlete. Sports Health. 2020;12(3):221–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382(16):1564–1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. Published online February 24, 2020 JAMA. doi:10.1001/jama.2020.2648 [DOI] [PubMed] [Google Scholar]
- 21. Zhou M, Zhang X, Qu J. Coronavirus disease 2019 (COVID-19): a clinical update. Front Med. 2020;14(2):126–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Zhu J, Ji P, Pang J, et al. Clinical characteristics of 3,062 COVID-19 patients: a meta-analysis. Published online April 15, 2020 J Med Virol. doi:10.1002/jmv.25884 [DOI] [PMC free article] [PubMed] [Google Scholar]