Objectives
The aims of the study were to perform the first systematic review of pediatric syncope etiologies and to determine the most common diagnoses with credible intervals (CredIs).
Methods
Review was performed within Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines and used Embase, Scopus, PubMed, and the Cochrane Controlled Trial databases. The following inclusion criteria for the articles were used: minimum of 10 patients, standard definition of syncope used, subjects who were 21 years or younger, and subjects who were either a consecutive retrospective group or a prospective group. No restrictions were made regarding language of the studies, but an English abstract was required. The following information was collected: purpose of the study, definition of syncope, number of patients, patient age range, inclusion/exclusion criteria, and etiologies of syncope.
Results
Of the 500 articles initially identified, 11 studies met the inclusion criteria and were the basis for this review. Three thousand seven hundred patients were included, ranging in age from 3 months to 21 years. The most common etiologies identified were vasovagal (52.2%; 95% CredI, 50.6–53.9), postural orthostatic tachycardia syndrome (13.1%; 95% CredI, 12.1–14.2), and cardiac causes (4.0%; 95% CredI, 3.39–4.65). A total of 18.3% (95% CredI, 17.0–19.5) of patients were found to have syncope of unknown cause.
Conclusions
Syncope is a common pediatric complaint. Most cases seen are a result of benign causes, with only a small percentage because of serious medical conditions. In addition, most syncopal episodes in the pediatric population are diagnosed clinically or with minimally invasive testing, emphasizing the importance of a detailed history and physical examination.
Key Words: pediatric syncope, vasovagal syncope, postural orthostatic tachycardia syndrome, cardiac syncope
Syncope, defined as the transient loss of consciousness and postural tone with a spontaneous recovery, is a common pediatric complaint. One or more syncopal episodes affects approximately 15% of children younger than 18 years.1 Variability in clinical presentation of childhood syncope along with the uncertainty in etiology often results in a costly and unnecessarily detailed inpatient or outpatient evaluation; the uncertainty also generates significant anxiety for parent and patient alike. The etiologies associated with syncope in the pediatric population range from vasovagal dysfunction to hypertrophic cardiomyopathy to seizure disorders.2 Although many etiologies of syncope and the incidence of each have been identified in previous studies, there has not been a systematic review that combines the data from the various institutions in an organized manner that can be of use to clinicians.
The goal of this study was to develop a comprehensive differential diagnosis of childhood syncope including the relative probabilities and 95% credible intervals (CredIs) for each clinical entity using a systematic review of the world's literature and Bayesian meta-analysis. Such a compendium would serve as a guide for the evaluation of the pediatric patient with syncope.
METHODS
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines.
Inclusion Criteria
Eligible studies met the following criteria: (1) a minimum of 10 patients per report with a clinical diagnosis of syncope, using a definition of syncope chosen by each study's authors; (2) subjects who were 21 years or younger; and (3) subjects who were part of a consecutive retrospective or a prospective group. Language of the study was not restricted, but an abstract in English was required.
Search
The key words used to search for articles were “pediatric syncope.” Embase, Scopus, PubMed, and the Cochrane Controlled Trial databases were searched first to determine whether or not a previous systematic review was available. Determining that none existed, two of the authors independently searched for references that fulfilled inclusion criteria. The results of these searches were combined.
Screening
Articles were first selected by one researcher and then reviewed by the second researcher to determine relevance and eligibility. In the absence of a consensus, a third author broke the tie. For each article, the following information was recorded: the purpose of the study, the definition of syncope used, the number of patients, the age range of the patients included, the inclusion and exclusion criteria used, and the etiologies of syncope determined by each study. For the purpose of this review, the major etiological categories of syncope were as follows: vasovagal (neurocardiogenic), idiopathic, cardiac, neurologic, psychiatric, orthostatic hypotension, postural orthostatic tachycardia syndrome (POTS), benign paroxysmal positional vertigo, tilt induced, intoxication, hypoglycemia, diabetes, anemia, subarachnoid hemorrhage, hyperventilation, breath holding spells, trauma, migraine headache, DeMorier syndrome, and muscular dystrophy. In areas with detailed information, subcategory analyses were performed. Initial data collection was reviewed by a second author for accuracy.
Statistical Analysis
A Bayesian methodology for point estimation and CredI calculation was used.3 The studies were ordered chronologically, and the rate from the first study was expressed as a β probability mass and used as the conjugate prior for the next study, expressed as a Bernoulli function. The resulting posterior β probability mass was used as the conjugate prior for the next study, and the process was repeated until all of the studies had been included. From the last posterior distribution, the overall estimate of the proportion was determined along with symmetrical 95% CredIs. All calculations were performed with the base package in R.
RESULTS
Study Selection
The results of the literature search are shown in Figure 1. The search of the PubMed, EMBASE, and SCOPUS databases produced 500 citations. Initial screening based on article title excluded 458 studies. Of the 42 that remained, 17 were excluded after review of the abstract. The full text of 25 remaining articles was reviewed. Fourteen articles were excluded: 8 were review articles or chapters from books, 5 did not adequately discuss etiologies, and 1 included subjects older than 21 years.
FIGURE 1.
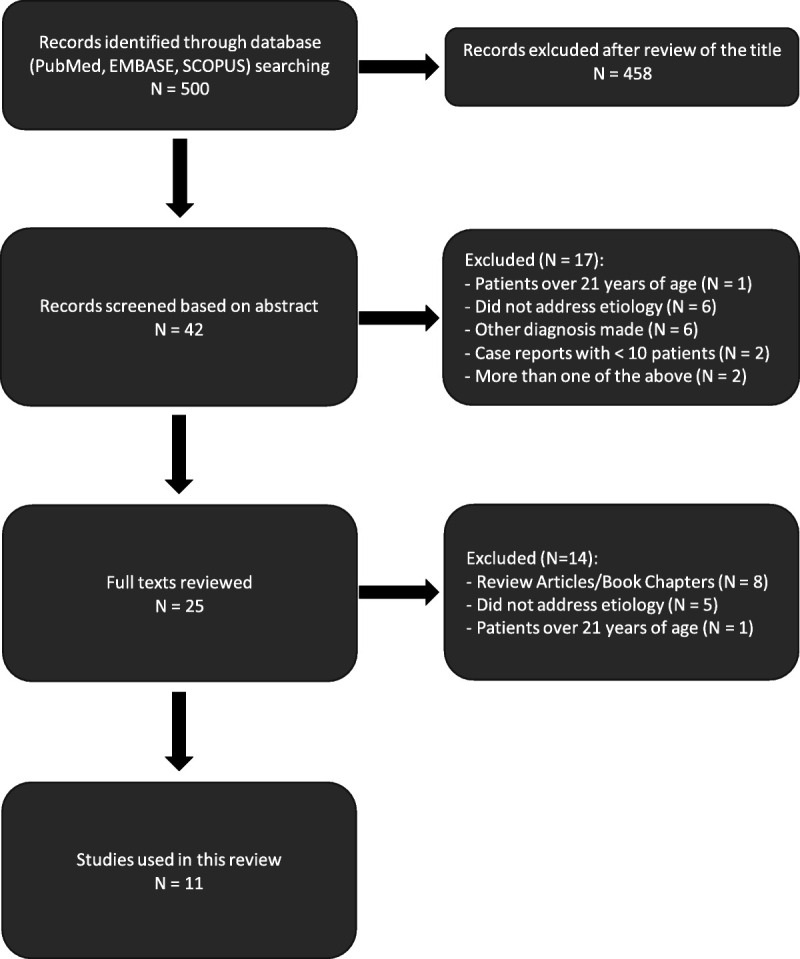
Results of the literature search and selection of articles.
Eleven studies met the inclusion criteria for this review and are summarized in Table 1. Overall, 3700 patients form the basis of this study. Subjects ranged in age from 3 months to 21 years. The summary of etiology by category is shown in Table 2. Vasovagal syncope accounted for 52.2% (95% CredI, 50.6–53.9) of cases, whereas 18.3% (95% CredI, 17.0–19.5) of cases had no identifiable etiology. Postural orthostatic tachycardia syndrome accounted for 13.1% (95% CredI, 12.1–14.2) of cases. Cardiac, neurological, and psychiatric disorders accounted for less than 10% of cases in aggregate.
TABLE 1.
Summary of Research Articles
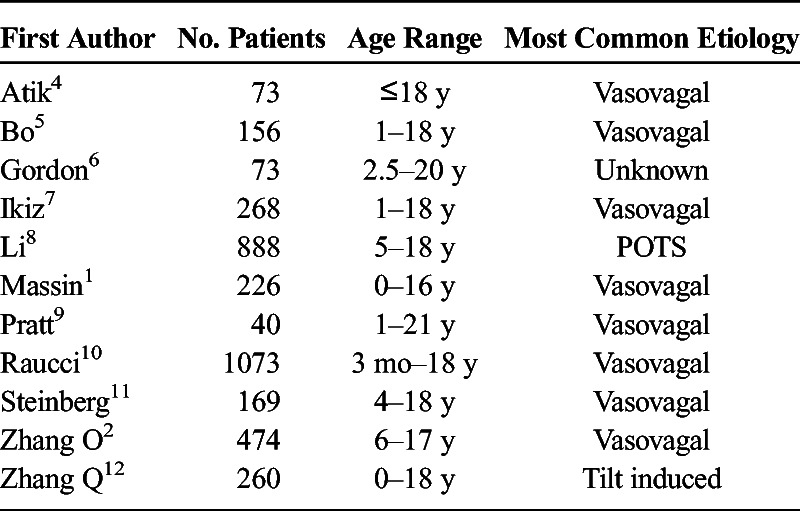
TABLE 2.
Summary Table by Syncopal Etiologies
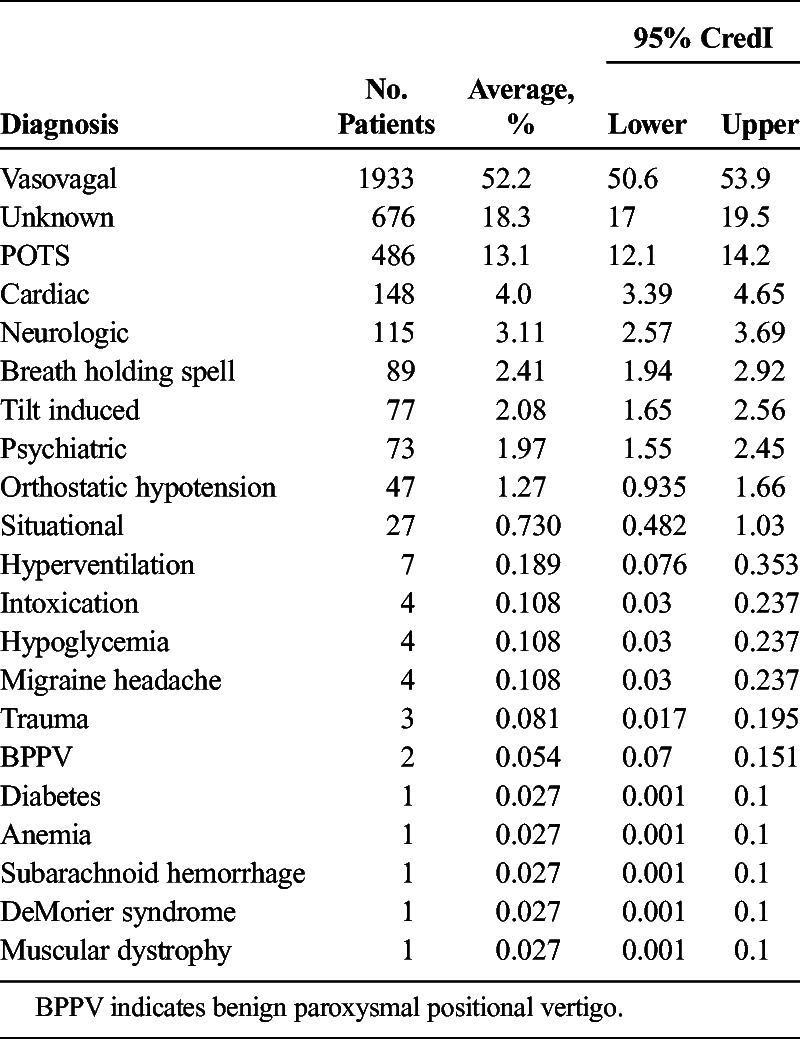
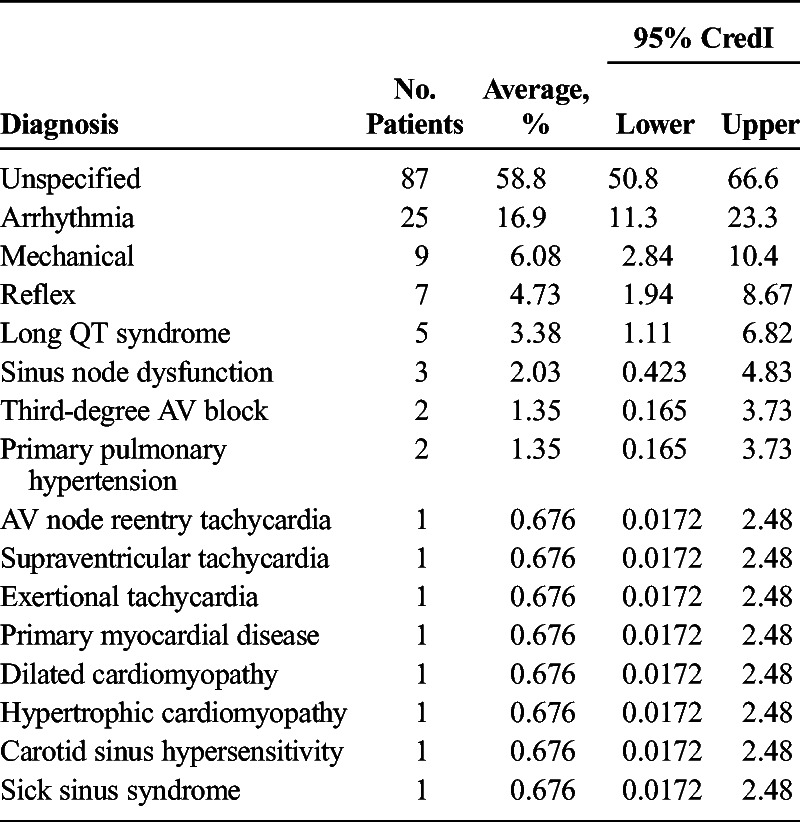
Table 3 shows a detailed breakdown of the cardiac etiologies, which accounted for 4.0% (95% CredI, 3.39–4.65) of cases overall. Of those subjects with cardiac etiologies, 58.8% (95% CredI, 50.8–66.6) were of an unspecified origin. Arrhythmias were identified in 16.9% (95% CredI, 11.3–23.3) of cardiac subjects. Long QT interval accounted for 3.38% (95% CredI, 1.11–6.82), whereas dilated cardiomyopathy and hypertrophic cardiomyopathy accounted for less than 2% of cardiac cases in aggregate.
TABLE 3.
Cardiac Etiologies of Syncope
Neurological disorders (Table 4) accounted for 3.11% (95% CredI, 2.57–3.69) of syncopal cases overall. Afebrile seizures accounted for 18.3% (95% CredI, 11.8–25.8) of neurological etiologies; 74.8% (95% CredI, 66.5–82.3) of neurological disorders were not specified.
TABLE 4.
Neurological Etiologies of Syncope
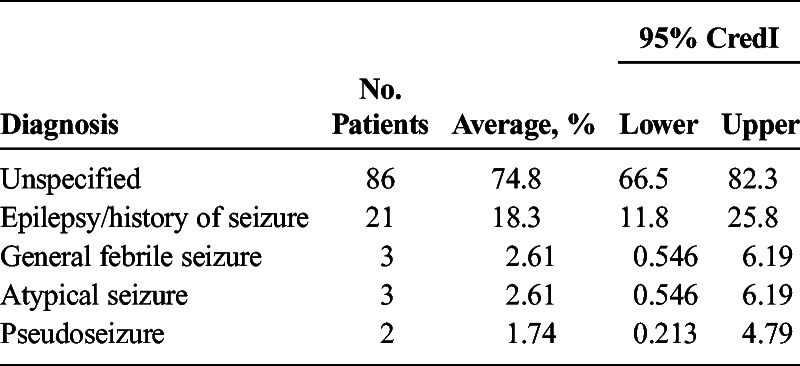
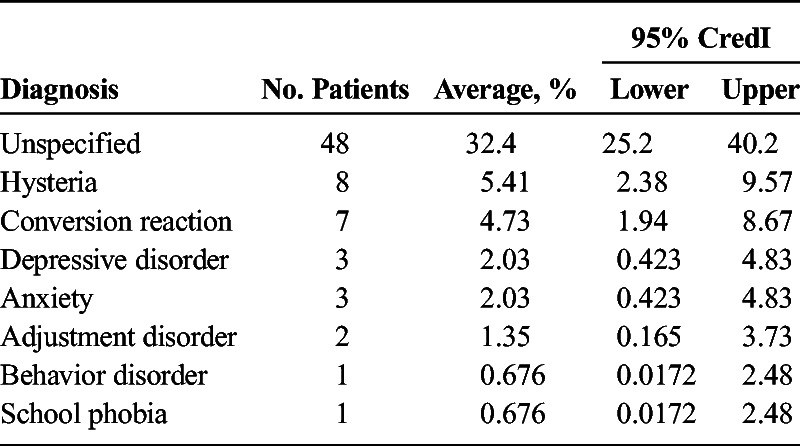
Table 5 provides a detailed view of psychiatric etiologies, which accounted for 1.97% (95% CredI, 1.55–2.45) of syncopal cases. Most psychiatric etiologies were unspecified. Breath holding spells accounted for 2.39% (95% CredI, 1.92–2.9) of total cases. Uncommon causes of childhood syncope (<1% of total case per category) included the 12 other diagnoses shown in Table 2.
TABLE 5.
Psychiatric Etiologies of Syncope
DISCUSSION
Syncope is a common pediatric complaint. Eleven studies, consisting of a total of 3700 patients, met the inclusion criteria and were the basis for this analysis. More than 80% of these patients were found to have a diagnosable cause of syncope.
Vasovagal syncope was found to be the most common cause of syncope in this study. Patients with vasovagal syncope tend to present after their first episode of syncope, which is often preceded by a stressor, such as prolonged standing or emotional distress. The diagnostic criteria for vasovagal syncope include the absence of another cause or etiology, a positive response to a head-up tilt test with a vasovagal reaction (hypotension and/or bradycardia), and no underlying chronic or acute illness.13 Patients diagnosed with vasovagal syncope typically have a good prognosis. Most do not require any medications and do well with lifestyle modifications, such as increased salt-water intake. However, in patients whose symptoms do not improve, β blockers, hydrocortisone, fludrocortisone, midodrine, or serotonin reuptake inhibitors can be used.4
Postural orthostatic tachycardia syndrome was found to be the second most commonly diagnosed cause of syncope in this study. Patients typically present after their first episode of syncope, which is often accompanied by dizziness, palpitations, pallor, headache, etc.8 The diagnostic criteria are a greater than 30-bpm increase in heart rate during a tilt-table test or heart rate exceeding 120 bpm within 10 minutes after rotating the table from horizontal to vertical position.4 Patients diagnosed with POTS generally do well. Most do not require medications. However, in patients who have persistent symptoms, midodrine, β blockers, or serotonin reuptake inhibitors can be used.4
In many of the cases where a definite etiology was discovered, the diagnoses were made on the basis of a detailed history and physical examination and, in few cases, minimally invasive testing.
Limitations
As with any systematic review, there are limitations to this study. For example, many of the studies chosen did not provide information regarding patient follow-up. This could have not only been helpful but could have also potentially led to a difference in the number of cases attributed to unknown origin. In addition, this review chose studies that defined syncope as a “transient loss of consciousness (and postural tone)” or whose definitions were very similar to that. However, it is difficult to get a sense of what each study would have considered “transient,” as many of the studies did not give an exact time constraint. Therefore, future studies should aim to provide a more robust follow-up of patients who have experienced syncope, especially when the cause is unknown, to determine whether the patient has repeat episodes, which could help clinicians determine the etiology. In addition, a more precise definition of syncope, giving an expected range of time, would be helpful in ensuring uniformity of future studies.
CONCLUSIONS
In summary, syncope is a common complaint seen in the pediatric population. The present study, the first systematic review of syncope in children, confirms that most cases seen are a result of benign causes, with only a small percentage because of serious medical conditions. In addition, these data indicate that most syncopal episodes in the pediatric population can be diagnosed with only minimally invasive testing, such as the tilt-table test, emphasizing the importance of a detailed history and physical examination during management and discouraging the use of invasive procedures unless indicated by the history and physical. Despite the limitations of this study, it provides useful information to clinicians about the most common causes of syncope in the pediatric population, and it provides clinicians with a starting point as they discuss possible etiologies and diagnostic testing with their patients and patients' family members.
Footnotes
Disclosure: The authors declare no conflict of interest.
REFERENCES
- 1.Massin MM Bourguignont A Coremans C, et al. Syncope in pediatric patients presenting to an emergency department. J Pediatr. 2004;145:223–228. [DOI] [PubMed] [Google Scholar]
- 2.Zhang O Du J Wang C, et al. The diagnostic protocol in children and adolescents with Syncope: a multi-centre prospective study. Acta Paediatr. 2009;98:879–884. [DOI] [PubMed] [Google Scholar]
- 3.Kruschke JK. Chapter 5. Inferring a binomial proportion via exact mathematical analysis. In: Doing Bayesian Analysis. Burlington, MA: Academic Press; 2011. [Google Scholar]
- 4.Atik SU Dedeoglu R Koka A, et al. Our experience in the diagnosis and treatment of postural orthostatic tachycardia syndrome, vasovagal syncope and inappropriate sinus tachycardia in children. Turk Kardiyol Dern Ars. 2017;45:227–234. [DOI] [PubMed] [Google Scholar]
- 5.Bo I Carano N Agnetti A, et al. Syncope in children and adolescents: a two-year experience at the department of paediatrics in Parma. Acta bio-medica: Atenei Parmensis. 2009;80:36–41. [PubMed] [Google Scholar]
- 6.Gordon T Moodie D Passalacqua M, et al. A retrospective analysis of the cost-effective workup of syncope in children. Cleve Clin J Med. 1987;54:391–394. [DOI] [PubMed] [Google Scholar]
- 7.Ikiz MA Cetin II Ekici F, et al. Pediatric syncope: is detailed medical history the key point for differential diagnosis? Pediatr Emerg Care. 2014;30:331–334. [DOI] [PubMed] [Google Scholar]
- 8.Li C Cheng W Hongwei W, et al. Underlying diseases in syncope of children in China. Med Sci Monit. 2011;17:PH49–PH53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pratt JL, Fleisher GR. Syncope in children and adolescents. Pediatr Emerg Care. 1989;5:80–82. [DOI] [PubMed] [Google Scholar]
- 10.Raucci U Scateni S Tozzi AE, et al. The availability and the adherence to pediatric guidelines for the management of syncope in the emergency department. J Pediatr. 2014;165:967–972. [DOI] [PubMed] [Google Scholar]
- 11.Steinberg LA, Knilans TK. Syncope in children: diagnostic tests have a high cost and low yield. J Pediatr. 2005;146:355–358. [DOI] [PubMed] [Google Scholar]
- 12.Zhang Q Zhu L Wang C, et al. Value of history taking in children and adolescents with cardiac syncope. Cardiol Young. 2013;23:54–60. [DOI] [PubMed] [Google Scholar]
- 13.Tao C Tang C Chen S, et al. Autonomic Nervous Function in Vasovagal Syncope of Children and Adolescents. Neuroscience Bulletin. 2019;35:937–940. [DOI] [PMC free article] [PubMed] [Google Scholar]


