Abstract
The Intervention for those Recently Informed of their Seropositive Status (IRISS) and other positive psychological interventions (PPIs) have demonstrated psychological and physical health benefits. However, meta-analyses suggest that PPIs may have differential effects depending on participants’ sociodemographic and psychological characteristics. We therefore examined potential moderators of effects of IRISS for adults newly diagnosed with HIV (N=159). While IRISS had similar effects on positive emotion across most subgroups (age, race, education, stress), depression was a significant moderator for positive emotion. When examining effects of IRISS on antidepressant use, age, race, education, depression, and perceived stress emerged as significant moderators. Neither optimism nor life events significantly moderated effects of IRISS on any outcome. Results have clinical implications that practitioners can use to inform which patients are most likely to benefit from PPI.
Keywords: positive psychology, HIV, emotion, stress, coping, depression, moderator, age, race, socioeconomic status
Introduction
Distress is common in people living with HIV (PLWH) and contributes to poorer medical outcomes (Bengtson et al., 2016; Bhatia et al., 2011; Gaynes et al., 2015). Conversely, positive emotion in PLWH is associated with benefits including better healthcare engagement and reduced mortality risk (Carrico & Moskowitz, 2014; Moskowitz, 2003). Based on this evidence, we developed an Intervention for those Recently Informed of their Seropositive Status (IRISS), a multicomponent program designed to increase positive emotions in people newly diagnosed with HIV (Moskowitz et al., 2014). In a randomized controlled trial (RCT), participants receiving IRISS demonstrated higher levels of past-day positive emotion than controls at post-intervention and follow-up through 15-months post-diagnosis (Moskowitz et al., 2017). Moreover, IRISS demonstrated a large, statistically significant effect on antidepressant use, which increased over time only in controls (Moskowitz et al., 2017).
While IRISS and other positive psychological interventions (PPI) have demonstrated efficacy for improving psychosocial and physical health among varying samples (e.g., Addington et al., 2018; Bolier et al., 2013; Massey et al., 2018; Moskowitz et al., 2019), meta-analyses have uncovered heterogenous effect sizes, indicating that PPI efficacy may differ by participant characteristics or study methodology (Sin & Lyubomirsky, 2009). Effectiveness of various emotion regulation strategies is increasingly recognized as context-dependent (Aldao, 2013). Identifying moderators of PPI efficacy is therefore a critical direction for well-being research (NIH, 2018).
Earlier moderator analyses suggest that PPIs may particularly benefit older adults (Sin & Lyubomirsky, 2009) and participants experiencing depression (Sin & Lyubomirsky, 2009), distress (Folkman, 1997; Zautra et al., 2005), or stressful events (Charlson et al., 2014). Individuals with lower (vs. higher) income and education levels may respond more favorably to PPI components such as positive reappraisal (Hittner et al., 2018; Troy et al., 2017). Additionally, optimism is associated with better psychological and physical health and may moderate effects of stress management interventions in healthcare (Antoni et al., 2001; Carver & Scheier, 2014). Race/ethnicity also may influence emotion regulation (Aldao, 2013) and is important to consider given racial/ethnic disparities in psychological well-being and treatment in PLWH (Bengtson et al., 2016). However, prior research has not examined race/ethnicity as a moderator of PPI effects in PLWH or other populations. The present analyses therefore test sociodemographic factors (age, race, income, education), optimism, depression, and stress as potential moderators of the effects of IRISS on positive emotion and antidepressant use, as these outcomes were significantly influenced by the intervention (Moskowitz et al., 2017).i
Materials and Methods
IRISS methods and primary results were previously reported (Moskowitz et al., 2014, 2017), approved by Institutional Review Boards, and registered with ClinicalTrials.gov (#NCT00720733). Eligibility criteria included: (1) HIV diagnosed within past 12 weeks; (2) English- or Spanish-speaking; and (3) age ≥18. Consenting participants were randomized to IRISS (eight skills with evidence for increasing positive emotions: noticing positive events, capitalizing/savoring, gratitude, mindfulness, positive reappraisal, personal strengths, attainable goals, and acts of kindness; n=80) or control (interviews with a sympathetic facilitator about topics such as life history, health, and social network; n=79). Both conditions included six sessions (five in-person, one phone).
Participants completed assessments at baseline, post-intervention/control, and two follow-ups (3-, 5-, 10- and 15-months post-diagnosis, respectively). Analyses herein test potential moderators: age; race/ethnicity (1=minority, 0=White); education (1=college degree or higher, 0=no college degree); income (1: ≥$30,000, 0: <$30,000)ii; trait optimism (Scheier et al., 1994); stress [perceived stress (Cohen, 1988); number of positive, negative and total life events since last assessment (Sarason et al., 1978)]; and baseline depressive symptoms (Radloff, 1977). Outcome measures include antidepressant use since last assessment (0=none, 1=any) and past-day positive and negative emotion [modified Differential Emotions Scale (Fredrickson, 2013) administered using the Day Reconstruction Method (Kahneman et al., 2004); aggregated mean positive and negative emotion ratings (0 not at all, to 4 very much so) across all episodes reported for the past day resulted in composite measures of past-day positive and negative emotion at each assessment].
Analyses included longitudinal mixed effects models (Singer & Willett, 2003) for positive and negative emotion (continuous outcomes) and longitudinal generalized estimating equations (Zeger et al., 1988) for antidepressant use (categorical outcome). Continuous predictors were grand-mean centered. For each outcome, we tested linear and quadratic (time2) change over time (months since baseline); we present only linear results for positive and negativei emotion because the quadratic patterns were non-significant. For all models, we examined main effects of time, condition (IRISS=1, control=0), the moderator of interest, and all higher-order interactions among these predictors. Significant interactions among continuous moderators were probed comparing high (+1SD above mean) vs. low (−1SD below mean) levels of the moderator.
Results
In the final sample (Table 1, N=159), most identified as male (91.7%) and gay or bisexual (84.1%). Just over half had not completed college (56.6%), reported annual income <$30,000 (51.6%), and were racial/ethnic minorities (55.4%). Retention was equivalent across conditions; approximately 70% (n=56 IRISS; n=58 control) completed the 15-month assessment (Moskowitz et al., 2017).
Table 1.
Sample characteristics by randomization arm (N=159)
| Randomization Arm | |||
|---|---|---|---|
| Characteristic | IRISS (n=80) | Control (n=79) | Total Sample (N=159) |
| Age | 35.6 (10.2) | 36.5 (9.7) | 36.0 (9.9) |
| Gender | |||
| Male | 71 (88.8%) | 73 (94.8%) | 144 (91.7%) |
| Female | 7 (8.8%) | 4 (5.2%) | 11 (7.0%) |
| MTF Transgender | 2 (2.5%) | 0 (0%) | 2 (1.3%) |
| Education | |||
| Less than college degree | 51 (63.7%) | 39 (49.4%) | 90 (56.6%) |
| College degree or higher | 29 (36.6%) | 38 (48.1%) | 67 (42.1%) |
| Yearly Household Income | |||
| ≤ $29,999 | 47 (58.8%) | 35 (44.3%) | 82 (51.6%) |
| ≥ $30,000 | 28 (35.0%) | 39 (49.4%) | 67 (42.1%) |
| Race/Ethnicity | |||
| American Indian | 1 (1.4%) | 1 (1.4%) | 2 (1.4%) |
| Asian/Pacific Islander | 9 (12.2%) | 3 (4.2%) | 12 (8.2%) |
| Black | 16 (21.6%) | 15 (20.8%) | 31 (21.2%) |
| Latino | 16 (21.6%) | 15 (20.8%) | 31 (21.2%) |
| Latino/Black | 2 (2.7%) | 3 (4.2%) | 5 (3.4%) |
| White | 30 (40.5%) | 35 (48.6%) | 65 (44.5%) |
| Baseline Optimism | 15.2 (4.9) | 15.6 (4.9) | 15.4 (4.9) |
| Baseline Depressive Symptoms | 22.1 (12.9) | 20.6 (14.4) | 21.4 (13.7) |
| Life Events (Total) | |||
| Baseline | 6.3 (3.6) | 5.7 (3.6) | 6.0 (3.6) |
| 5 Months | 5.4 (3.0) | 4.0 (2.7) | 4.7 (2.9) |
| 10 Months | 5.2 (2.8) | 4.0 (2.4) | 4.6 (2.7) |
| 15 Months | 5.4 (3.3) | 4.6 (3.0) | 5.0 (3.1) |
| Life Events (Positive) | |||
| Baseline | 3.4 (2.4) | 3.0 (2.6) | 3.2 (2.5) |
| 5 Months | 3.7 (2.5) | 2.5 (1.9) | 3.1 (2.3) |
| 10 Months | 3.5 (2.6) | 2.3 (1.8) | 2.9 (2.3) |
| 15 Months | 3.5 (2.7) | 3.0 (2.4) | 3.3 (2.5) |
| Life Events (Negative) | |||
| Baseline | 2.5 (2.5) | 2.4 (2.5) | 2.4 (2.5) |
| 5 Months | 1.4 (1.5) | 1.2 (1.3) | 1.3 (1.4) |
| 10 Months | 1.2 (1.4) | 1.3 (1.3) | 1.2 (1.3) |
| 15 Months | 1.3 (1.4) | 1.2 (1.5) | 1.3 (1.5) |
| Perceived Stress | |||
| Baseline | 8.3 (1.5) | 8.2 (1.6) | 8.3 (1.6) |
| 5 Months | 8.4 (1.7) | 8.4 (1.7) | 8.4 (1.7) |
| 10 Months | 8.3 (1.5) | 8.2 (1.6) | 8.2 (1.5) |
| 15 Months | 8.0 (1.7) | 8.4 (1.3) | 8.2 (1.5) |
Note. Values represent mean (SD) for continuous variables and n (%) for categorical variables.
Moderation Effects on Positive Emotion
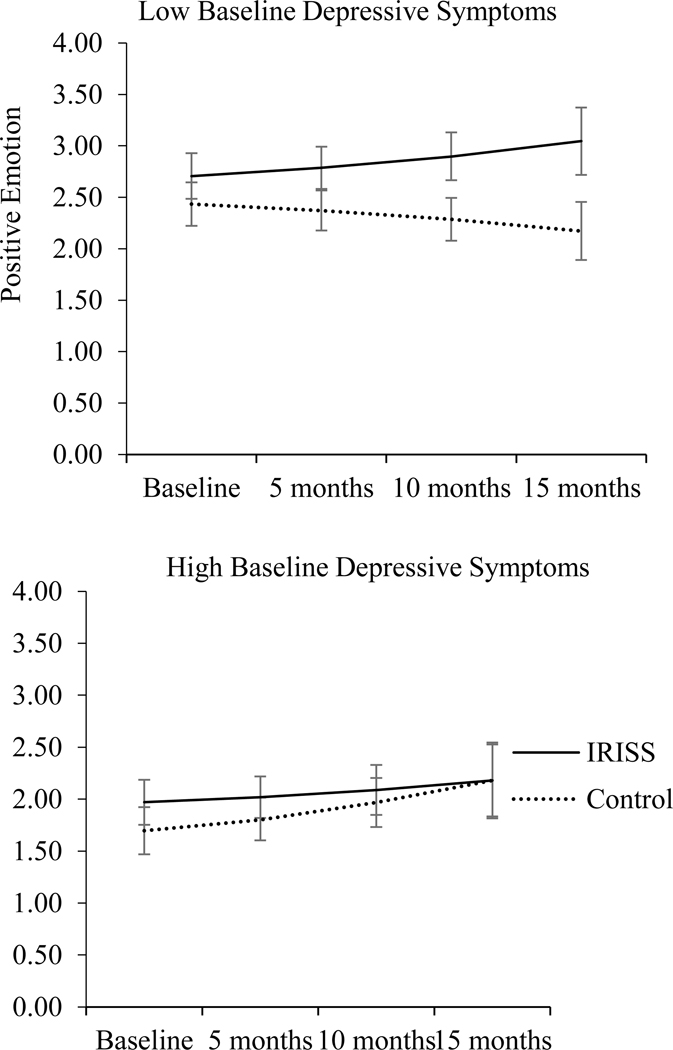
Baseline depression significantly moderated effects on positive emotion (Table 2; Figure 1iii). Participants with low baseline levels of depression showed significant decreases in positive emotion over time in the control condition (B=−0.02, t(100)=−4.54, p<.001), but marginally significant increases in positive emotion in IRISS (B=0.02, t(169)=1.90, p=.059). Among participants with low baseline levels of depression, positive emotion was significantly greater among IRISS vs. control participants at baseline (M=2.71 vs. 2.43, respectively; p=.03); this significant between-group difference grew larger at 5- (M=2.79 vs. 2.37, respectively; p=.001), 10- (M=2.90 vs. 2.29, respectively; p=.001), and 15-months (M=3.05 vs. 2.17, respectively; p=.001) post-diagnosis. In contrast, participants with high baseline levels of depression showed increases in positive emotion over time in the control condition (B=0.03, t(156)=2.98, p=.003), but stable levels of positive emotion in IRISS (B=0.01, t(164)=0.75, p=.45). Positive emotion was significantly higher at baseline among IRISS (M=1.97) vs. control (M=1.70) participants with high baseline levels of depression (p=.03); this difference became non-significant at all subsequent assessments (ps≥.09). None of the other variables significantly moderated intervention effects on positive emotion over time (ps>.13; Table 2).
Table 2.
Moderators of intervention effects on positive emotion and antidepressant use
| Outcome | |||
|---|---|---|---|
| Moderator | Positive Emotion | Antidepressant Use | |
| Moderator × Condition × Time Interaction | Moderator × Condition × Time Interaction (Linear Effect) | Moderator × Condition × Time2 Interaction (Quadratic Effect) |
|
| Age | F(1, 391) = 0.09, p = .76 | χ2 = 3.82, p = .05 | χ2 = 2.22, p = .33 |
| Race/Ethnicity (Minority = 1, White = 0) |
F(1, 415) = 2.33, p = .13 | χ2 = 1.77, p = .18 | χ2 = 6.20, p = .045 |
| Education (College Degree or Higher = 1, Less than College = 0) |
F(1, 407) = 1.25, p = .27 | χ2 = 0.04, p = .85 | χ2 = 6.48, p = .04 |
| Income (High income (≥$30,000) = 1, Low income (<$30,000) = 0) |
F(1, 380) = 0.16, p = .69 | χ2 = 0.04, p = .85 | χ2 = 5.58, p = .06 |
| Baseline Optimism | F(1, 410) = 0.17, p = .68 | χ2 = 0.42, p = .52 | χ2 = 0.01, p = .99 |
| Baseline Depressive Symptoms | F(1, 416) = 6.63, p = .01 | χ2 = 0.04, p = .85 | χ2 = 9.19, p = .01 |
| Perceived Stress | F(1, 366) = 0.20, p = .66 | χ2 = 0.21, p = .65 | χ2 = 13.44, p = .001 |
| Life Events (Total) | F(1, 363) = 0.56, p = .45 | χ2 = 0.09, p = .76 | χ2 = 0.95, p = .62 |
| Life Events (Positive) | F(1, 361) = 0.06, p = .81 | χ2 = 0.69, p = .41 | χ2 = 0.72, p = .70 |
| Life Events (Negative) | F(1, 364) = 0.01, p = .93 | χ2 = 0.02, p = .88 | χ2 = 0.15, p = .93 |
Figure 1.
Positive emotion as a function of intervention condition and baseline depressive symptoms.
Moderation Effects on Antidepressant Use
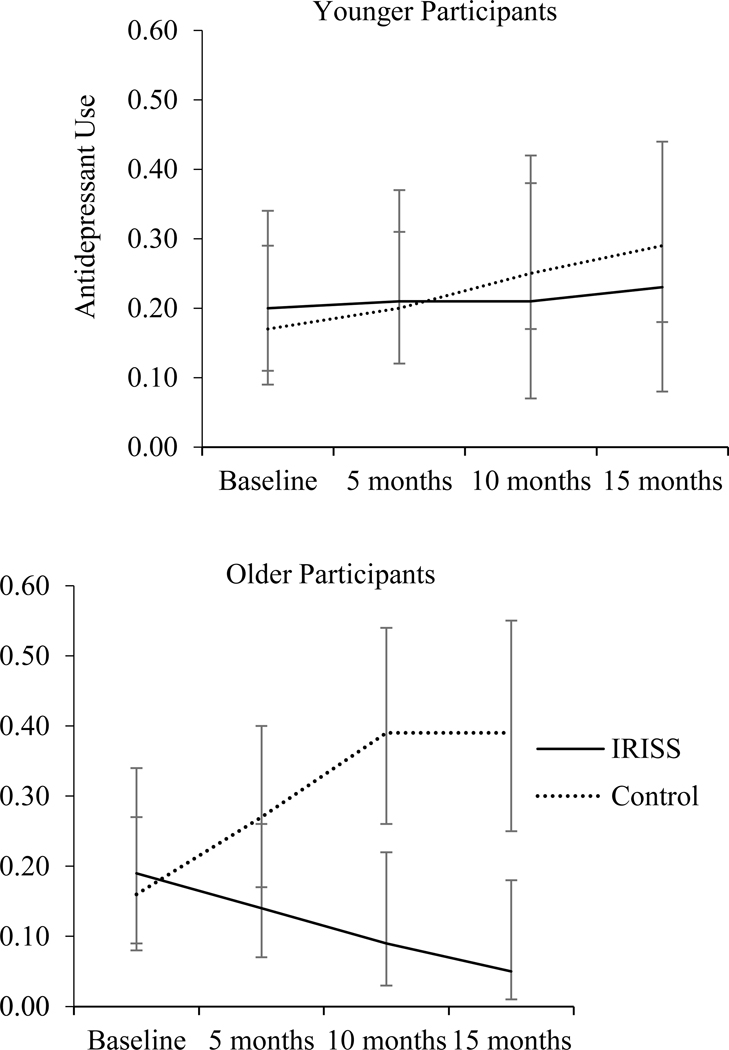
Age significantly moderated intervention effects on antidepressant use (Table 2; Figure 2). Older control participants showed significant linear (B=0.28, χ2=13.99, p<.001) and quadratic (B=−0.01, χ2=10.45, p=.001) increases in antidepressant use over time (p≤.001), whereas older IRISS participants did not (ps≥.078). Antidepressant usage among older participants was significantly lower (ps≤.044) in IRISS (5-months: 14%, 10-months: 9%, 15-months: 5%) vs. control (5-months: 27%, 10-months: 39%, 15-months: 39%). Among younger participants, antidepressant usage did not significantly change over time in either condition (ps>.70), and between-group comparisons were non-significant (ps>.56) at all timepoints.
Figure 2.
Antidepressant use as a function of intervention condition and age.
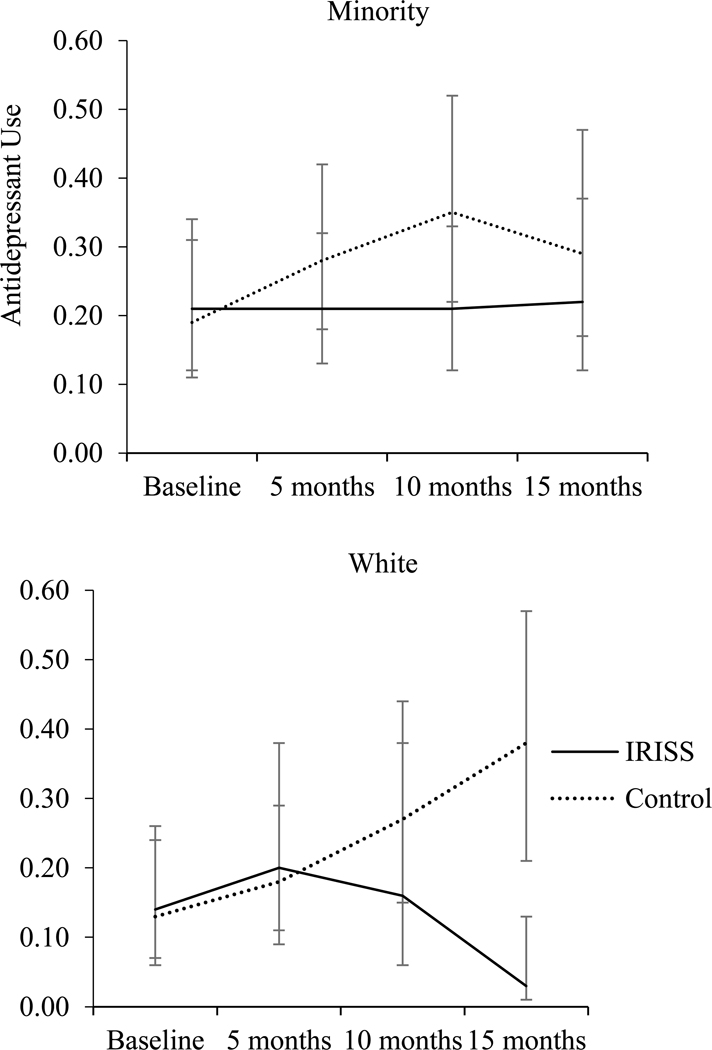
Race/ethnicity significantly moderated intervention effects on antidepressant use (Table 2; Figure 3). Minority participants in the control showed significant linear (B=0.19, χ2=12.37, p<.001) and quadratic (B=−0.009, χ2=12.93, p<.001) increases in antidepressant use over time, whereas minority participants in IRISS showed stable levels of antidepressant use (ps≥.49). Among minority participants, comparisons between IRISS vs. control were non-significant at all assessments (ps>.17). In contrast, antidepressant usage among White participants did not significantly change over time in either condition (ps>.70). Comparison of antidepressant use among White participants in IRISS (3%) vs. control (38%) was significant only at 15-months post-diagnosis (p<.001).
Figure 3.
Antidepressant use as a function of intervention condition and race/ethnicity.
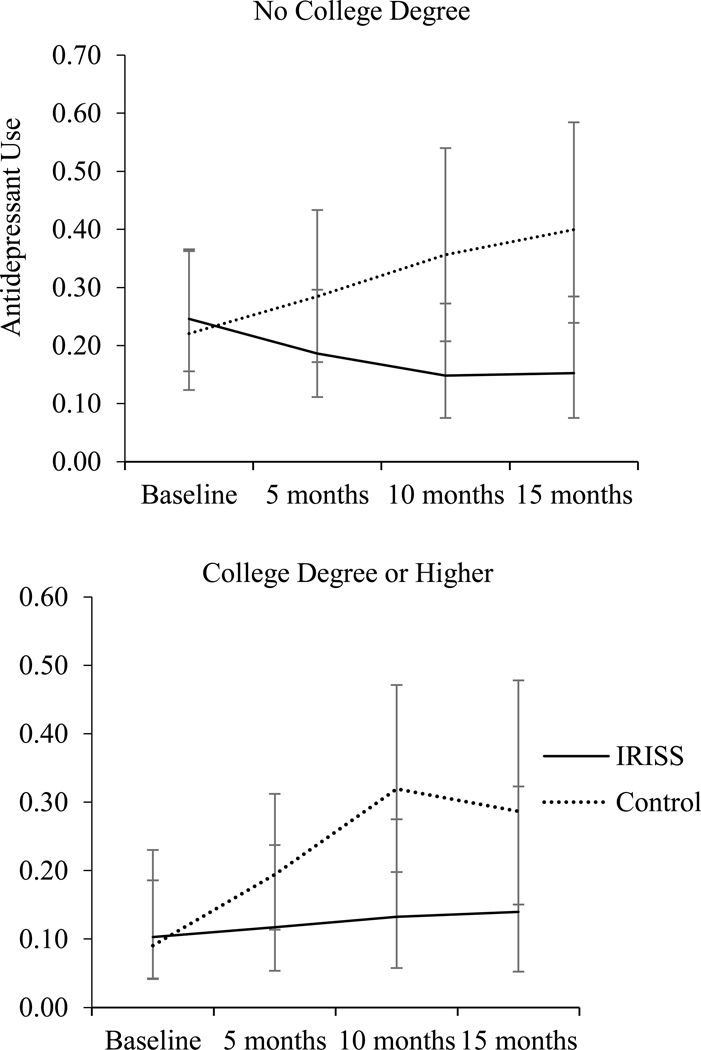
Education significantly moderated intervention effects on antidepressant use (Table 2; Figure 4). College graduates showed significant linear (B=0.31, χ2=13.31, p<.001) and quadratic (B=−0.01, χ2=11.52, p=.001) increases in antidepressant use over time in the control, but stable levels in IRISS (ps≥.598). Antidepressant use among college graduates was significantly lower in IRISS (13%) vs. control participants (32%) only at 10-months (p=.023). In contrast, among participants without a college degree, antidepressant usage did not significantly change over time in either condition (ps>.13). Antidepressant usage was significantly lower in IRISS vs. control participants without a college degree at 10- (15% vs. 36%, respectively; p=.036) and 15-months post-diagnosis (15% vs. 40%, respectively; p=.018), but not at other assessments (p>.21).
Figure 4.
Antidepressant use as a function of intervention condition and education.
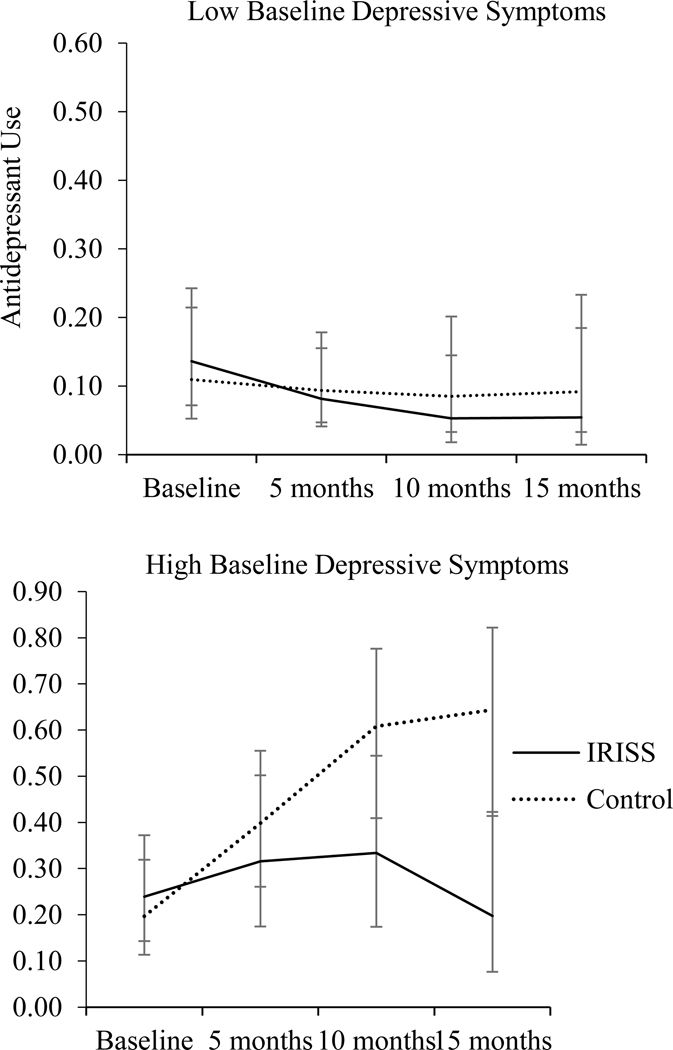
Baseline depression significantly moderated intervention effects on antidepressant use (Table 2; Figure 5). Participants with high baseline levels of depression showed significant linear (B=0.31, χ2=8.54, p=.003) and quadratic (B=−0.01, χ2=12.49, p<.001) increases in antidepressant use over time in the control condition, but not in IRISS (ps≥.35). Among participants with high baseline levels of depression, antidepressant usage was significantly lower among IRISS (10-months: 33%, 15-months: 20%) vs. control (10-months: 61%, 15-months: 64%) at 10- (p=.048) and 15-months (p=.001) post-diagnosis. In contrast, participants with low baseline levels of depression did not show changes in antidepressant use over time in either condition (ps>.10), and between-group comparisons between IRISS vs. control were non-significant at all assessments (ps>.51).
Figure 5.
Antidepressant use as a function of intervention condition and baseline depressive symptoms.
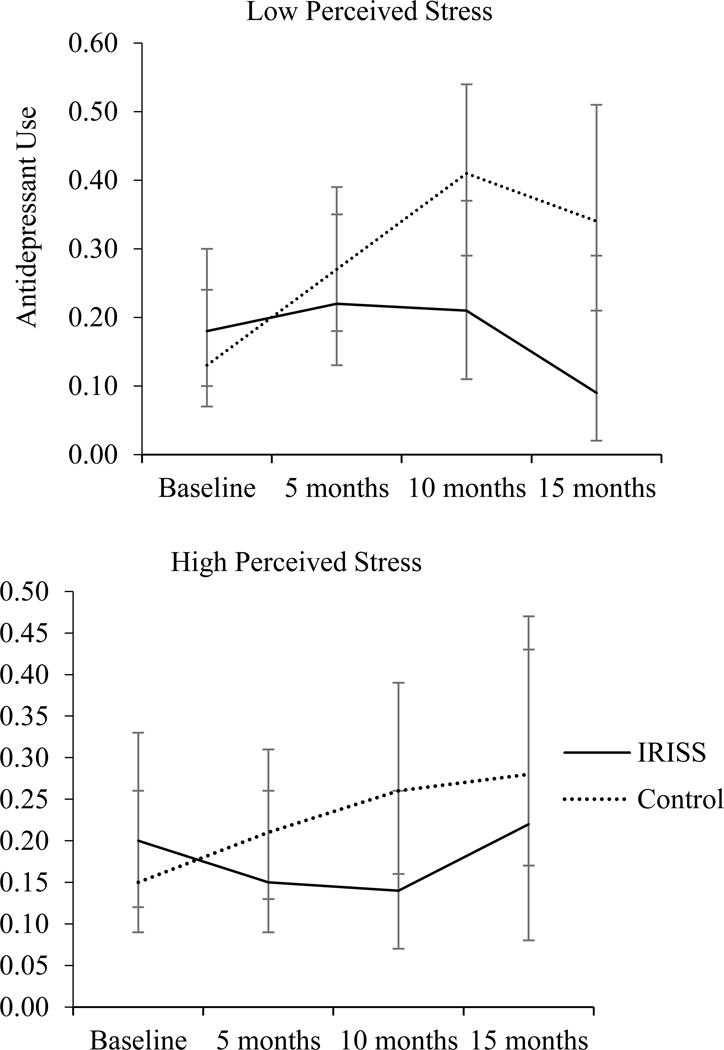
Perceived stress since the last assessment significantly moderated intervention effects on antidepressant use (Table 2; Figure 6). High-stress participants in IRISS showed marginally-significant linear (B=−0.13, χ2=3.40, p=.065) and quadratic (B=0.008, χ2=3.59, p=.058) decreases in antidepressant use over time, while those in the control showed marginally-significant linear (B=0.11, χ2=3.37, p=.067) and significant quadratic (B=0.003, χ2=9.18, p=.002) increases in antidepressant use over time. Between-group comparisons among high-stress participants were non-significant at all assessments (ps≥.11). Among low-stress participants, antidepressant use significantly increased over time in the control (linear effect: B=0.27, χ2=18.59, p<.001; quadratic effect: B=−0.01, χ2=21.90, p<.001), but did not significantly change in IRISS (ps≥.23). Antidepressant use among low-stress participants was significantly lower in IRISS vs. control at 10-months (21% vs. 41%, respectively; p=.03) and 15-months post-diagnosis (9% vs. 34%, respectively; p=.01), but not at other assessments (p>.39). None of the other variables significantly moderated intervention effects on antidepressant use over time (ps>.41; Table 2).
Figure 6.
Antidepressant use as a function of intervention condition and perceived stress.
Discussion
This study addresses an important gap in the literature – identifying who most benefits from PPIs – and provides several advances beyond prior PPI moderator analyses: (1) It focuses on a specific clinical sample, PLWH. (2) The sample includes high proportions of low income/education and racial/ethnic minority participants. (3) This RCT compares a PPI to an active control, rather than waitlist or no additional intervention, as is common in many PPI trials (Bolier et al., 2013; Sin & Lyubomirsky, 2009). (4) It examines outcomes separately, rather than combining distinct indicators into broader categories (e.g., well-being).
Results revealed significant effects of IRISS on antidepressant use among older participants, racial/ethnic minorities, college graduates, and participants with elevated baseline depression and greater perceived stress. Within each of these subgroups, the proportion of participants using antidepressants increased over time in controls, but remained relatively stable, and often significantly lower, in IRISS. Between-group analyses identified significantly lower antidepressant use among IRISS vs. controls at follow-up among White participants, those without a college degree, and those with lower levels of perceived stress.
While antidepressant therapy in PLWH may improve depression, most trials have lacked rigor (Eshun-Wilson et al., 2018). Moreover, PLWH frequently report unwanted side effects of antidepressants, and how these medications affect HIV outcomes remains largely unknown (Eshun-Wilson et al., 2018). Our results suggest that, when antidepressant therapy is contraindicated/undesirable, IRISS provides another possibility for improving emotion regulation, particularly for PLWH who are older, racial/ethnic minorities, college graduates, and those with elevated depression or stress.
Most moderator analyses were non-significant for emotion outcomes, indicating similar effects across subgroups. Two exceptions emerged: income moderated effects on negative emotion,i and baseline depression moderated effects on positive emotion. Whereas positive emotion was relatively stable in IRISS regardless of baseline depression, control participants’ positive emotion changed significantly – but in opposite directions, depending on baseline depression levels – decreasing in controls with lower baseline depression, and increasing in controls with higher baseline depression. This suggests that talking with a sympathetic listener may be detrimental to positive emotion among PLWH with less depression. Conversely, given that antidepressant use also increased over time among controls with higher baseline depression, perhaps the combination of pharmacotherapy and supportive listening is effective for increasing positive emotions in depressed PLWH.
Unlike other medical research (Antoni et al., 2001; Charlson et al., 2014), optimism and life events did not significantly moderate IRISS effects. PPI moderators may not generalize across samples and outcomes. Researchers should examine outcomes separately and investigate clinical characteristics as potential moderators, even when aggregating PPI trials in meta-analyses. Large samples are needed to provide power for examining moderator interactions (e.g., age x gender) (Aldao, 2013).
Limitations
Because IRISS recruited in San Francisco, where cost of living is especially high, and the sample was overwhelmingly male, results may not generalize to other regions or genders. The sample size did not allow us to test moderating effects of separate racial/ethnic groups. Trials enrolling large, diverse samples are needed to better understand how race/ethnicity and gender moderate PPI efficacy.
Most participants received all eight IRISS skills (Moskowitz et al., 2017). We therefore cannot examine differential responses to particular skills. Future studies should examine whether personal characteristics predict greater efficacy of specific PPI techniques – i.e., person-activity fit (Lyubomirsky & Layous, 2013; Proyer et al., 2015).
Conclusions
IRISS meets criteria for a high-quality PPI trial (Bolier et al., 2013) and focuses on PLWH, an important clinical sample. This study thus advances evidence for including PPIs in targeted public health efforts. Results have clinical implications regarding which patients are likely to benefit from PPI: older adults, racial/ethnic minorities, college graduates, individuals with income ≥$30,000, and patients with elevated depression or stress.
Supplementary Material
Acknowledgments
Funding provided by National Institutes of Health (R01-MH087423, K24-MH093225, P30-AI117943) and Third Coast Center for AIDS Research.
Footnotes
To further examine differential effects on emotion, we tested moderator effects on negative emotion; see supplementary materials.
Income was dichotomized using a median split.
In all figures, error bars denote 95% confidence intervals.
Conflicts of interest: None.
References
- Addington EL, Cheung EO, & Moskowitz JT (2018). Positive affect skills may improve pain management in people with HIV. Journal of Health Psychology. Advance online publication. doi: 10.1177/1359105318769355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aldao A (2013). The Future of Emotion Regulation Research: Capturing Context. Perspectives on Psychological Science, 8, 155–172. doi: 10.1177/1745691612459518 [DOI] [PubMed] [Google Scholar]
- Antoni MH, Lehman JM, Kilbourn KM, Boyers AE, Culver JL, Alferi SM, … Carver CS (2001). Cognitive-behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early-stage breast cancer. Health Psychology, 20, 20–32. doi: 10.1037/0278-6133.20.1.20 [DOI] [PubMed] [Google Scholar]
- Bengtson AM, Pence BW, Crane HM, Christopoulos K, Fredericksen RJ, Gaynes BN, … Mugavero MJ (2016). Disparities in Depressive Symptoms and Antidepressant Treatment by Gender and Race/Ethnicity among People Living with HIV in the United States. PloS One, 11. doi: 10.1371/journal.pone.0160738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatia R, Hartman C, Kallen MA, Graham J, & Giordano TP (2011). Persons newly diagnosed with HIV infection are at high risk for depression and poor linkage to care: Results from the Steps Study. AIDS and Behavior, 15, 1161–1170. doi: 10.1007/s10461-010-9778-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolier L, Haverman M, Westerhof GJ, Riper H, Smit F, & Bohlmeijer E (2013). Positive psychology interventions: A meta-analysis of randomized controlled studies. BMC Public Health, 13, 119. doi: 10.1186/1471-2458-13-119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrico AW, & Moskowitz JT (2014). Positive affect promotes engagement in care after HIV diagnosis. Health Psychology, 33, 686–689. doi: 10.1037/hea0000011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS, & Scheier MF (2014). Dispositional optimism. Trends in Cognitive Sciences, 18, 293–299. doi: 10.1016/j.tics.2014.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlson ME, Wells MT, Peterson JC, Boutin-Foster C, Ogedegbe GO, Mancuso CA, … Isen AM (2014). Mediators and moderators of behavior change in patients with chronic cardiopulmonary disease: The impact of positive affect and self-affirmation. Translational Behavioral Medicine, 4, 7–17. doi: 10.1007/s13142-013-0241-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S (1988). Perceived stress in a probability sample of the United States In The social psychology of health (pp. 31–67). Sage Publications, Inc. [Google Scholar]
- Eshun-Wilson I, Siegfried N, Akena DH, Stein DJ, Obuku EA, & Joska JA (2018). Antidepressants for depression in adults with HIV infection. The Cochrane Database of Systematic Reviews, 1, CD008525. doi: 10.1002/14651858.CD008525.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folkman S (1997). Positive psychological states and coping with severe stress. Social Science & Medicine, 45, 1207–1221. doi: 10.1016/S0277-9536(97)00040-3 [DOI] [PubMed] [Google Scholar]
- Fredrickson BL (2013). Positive Emotions Broaden and Build In Devine P & Plant A (Eds.), Advances in Experimental Social Psychology (Vol. 47, pp. 1–53). Academic Press. doi: 10.1016/B978-0-12-407236-7.00001-2 [DOI] [Google Scholar]
- Gaynes BN, O’Donnell J, Nelson E, Heine A, Zinski A, Edwards M, … Pence BW (2015). Psychiatric comorbidity in depressed HIV-infected individuals: Common and clinically consequential. General Hospital Psychiatry, 37, 277–282. doi: 10.1016/j.genhosppsych.2015.03.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hittner EF, Rim KL, & Haase CM (2019). Socioeconomic Status as a Moderator of the Link Between Reappraisal and Anxiety. Emotion, 19, 1478–1479. doi: 10.1037/emo0000539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahneman D, Krueger AB, Schkade DA, Schwarz N, & Stone AA (2004). A survey method for characterizing daily life experience: The day reconstruction method. Science, 306, 1776–1780. doi: 10.1126/science.1103572 [DOI] [PubMed] [Google Scholar]
- Lyubomirsky S, & Layous K (2013). How do simple positive activities increase well-being? Current Directions in Psychological Science, 22, 57–62. doi: 10.1177/0963721412469809 [DOI] [Google Scholar]
- Massey CN, Feig EH, Duque-Serrano L, Wexler D, Moskowitz JT, & Huffman JC (2019). Well-Being Interventions for Individuals with Diabetes: A Systematic Review. Diabetes Research and Clinical Practice, 147, 118–133. doi: 10.1016/j.diabres.2018.11.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moskowitz JT (2003). Positive affect predicts lower risk of AIDS mortality. Psychosomatic Medicine, 65, 620–626. [DOI] [PubMed] [Google Scholar]
- Moskowitz JT, Carrico AW, Cohn MA, Duncan LG, Bussolari C, Layous K, … Folkman S (2014). Randomized controlled trial of a positive affect intervention to reduce stress in people newly diagnosed with HIV; protocol and design for the IRISS study. Open Access Journal of Clinical Trials. doi: 10.2147/OAJCT.S64645 [DOI] [Google Scholar]
- Moskowitz JT, Carrico AW, Duncan LG, Cohn MA, Cheung EO, Batchelder A, … Folkman S (2017). Randomized controlled trial of a positive affect intervention for people newly diagnosed with HIV. Journal of Consulting and Clinical Psychology, 85, 409–423. doi: 10.1037/ccp0000188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moskowitz JT, Cheung EO, Snowberg K, Cotten P, & Dowling GA (2019). Randomized trial of a facilitated online positive emotion regulation intervention for dementia caregivers. Health Psychology, 38, 391–402. doi: 10.1037/hea0000680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- NIH. (2018). Emotional well-being: Emerging insights and questions for future research Report of a roundtable meeting. NCCIH & OBSSR. [Google Scholar]
- Proyer RT, Wellenzohn S, Gander F, & Ruch W (2015). Toward a better understanding of what makes positive psychology interventions work: Predicting happiness and depression from the person × intervention fit in a follow-up after 3.5 years. Applied Psychology. Health and Well-Being, 7, 108–128. doi: 10.1111/aphw.12039 [DOI] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement, 1, 385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- Sarason IG, Johnson JH, & Siegel JM (1978). Assessing the impact of life changes: Development of the Life Experiences Survey. Journal of Consulting and Clinical Psychology, 46, 932–946. [DOI] [PubMed] [Google Scholar]
- Scheier MF, Carver CS, & Bridges MW (1994). Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the Life Orientation Test. Journal of Personality and Social Psychology, 67, 1063–1078. [DOI] [PubMed] [Google Scholar]
- Sin NL, & Lyubomirsky S (2009). Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: A practice-friendly meta-analysis. Journal of Clinical Psychology, 65, 467–487. doi: 10.1002/jclp.20593 [DOI] [PubMed] [Google Scholar]
- Singer JD, & Willett JB (2003). Applied longitudinal data analysis: Modeling change and event occurrence. Oxford University Press. doi: 10.1093/acprof:oso/9780195152968.001.0001 [DOI] [Google Scholar]
- Troy AS, Ford BQ, McRae K, Zarolia P, & Mauss IB (2017). Change the things you can: Emotion regulation is more beneficial for people from lower than from higher socioeconomic status. Emotion, 17, 141–154. doi: 10.1037/emo0000210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zautra AJ, Johnson LM, & Davis MC (2005). Positive affect as a source of resilience for women in chronic pain. Journal of Consulting and Clinical Psychology, 73, 212–220. doi: 10.1037/0022-006X.73.2.212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeger SL, Liang K-Y, & Albert PS (1988). Models for longitudinal data: A generalized estimating equation approach. Biometrics, 44, 1049–1060. doi: 10.2307/2531734 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.