Abstract
Background:
Antibiotics are the most frequently used medicines worldwide with most of the countries defining these as prescription-only medicines. Though, dispensing non-prescribed antibiotics represent one of the chief causal factors to the irrational use of antibiotics that paves the way to the development of antimicrobial resistance.
Objective:
We aimed at describing the practices and the enablers for non-prescribed antibiotic dispensing in Maputo city, Mozambique.
Methods:
A qualitative study was conducted, between October 2018 and March 2019, in nine private pharmacies randomly selected across Maputo city. Eighteen pharmacists were contacted and seventeen enrolled through snowball sampling. In-depth interviews were conducted, audiotaped, and transcribed verbatim. Transcripts were coded and analysed though thematic analysis with guidelines from Braun and Clark. The Consolidated Criteria for Reporting Qualitative Studies (COREQ) checklist by (Tong, 2007) was performed.
Results:
Out of seventeen, fifteen pharmacists admitted non-prescribed dispensing of antibiotics. Common antibiotic dispensing practices included; dispensing without prescription, without asking for a brief clinical history of patients, without clear explanation of the appropriate way of administering, without advising on the side effects. Reasons for non-prescribed antibiotic dispensing are linked to patients’ behaviour of demanding for non-prescribed antibiotics, to the patients expectations and beliefs on the healing power of antibiotics, to the physicians’ prescribing practices. Other reasons included the pressure for profits from the pharmacy owners, the fragile law enforcement, and absence of accountability mechanisms.
Conclusions:
The practices of non-prescribed antibiotic dispensing characterize the ‘daily life’ of the pharmacists. On the one hand, the patient’s demand for antibiotics without valid prescriptions, and pharmacist’s wish to assist based on their role in the pharmacy, the pressure for profits and on the understanding of the larger forces driving the practices of self-medication with antibiotics - rock. On the other hand, pharmacists are aware of the legal status of antibiotics and the public health consequences of their inappropriate dispensing practices and their professional and ethical responsibility for upholding the law - hard place. Highlighting the role of pharmacists and their skills as health promotion professionals is needed to optimizing antibiotic dispensing and better conservancy in Mozambique.
Keywords: Anti-Bacterial Agents, Self Medication, Prescriptions, Pharmacists, Professional Practice, Pharmacies, Drug Resistance, Bacterial, Motivation, Law Enforcement, Public Health, Qualitative Research, Mozambique
INTRODUCTION
The growth of antimicrobial resistance has prompted calls to reduce unnecessary antibiotic use, improving treatment protocols to maximize the lifespan of these drugs.1,2 In many countries including Mozambique, antibiotics are prescription-only-medicines.3-6 Though, antibiotics are frequently accessed without prescription mainly in resource-constrained settings, paving the way to the practices of self-medication with antibiotics.7-9 These practices result from a complex interaction between several factors notably; health care providers’ prescribing practices, pharmacists’ dispensing practices, health care facilities’ conditions, individuals’ and communities’ beliefs on the healing power of antibiotics, health-seeking behaviours, individual responsibility for one’s own health, patients’ expectations, previous experience with antibiotics, and individuals’ self-care practices.5,7,8,10-13 Nonetheless, incorrect diagnosis, incorrect therapeutic choice, inappropriate drug and dose selections, and insufficient treatment duration, frequently accompanied the non-prescribed utilization of antibiotics adding risks to individuals’ health.4,5,7,14,15
The World Health Organization (WHO) recognizes the inappropriate use of antibiotics as an important driving force behind the rise of antimicrobial resistance rates both at hospital and community levels especially within the low and middle-income countries (LMICs), were the burden of infectious disease is high.9,11 Moreover, evidence of the magnitude of inappropriate use of antibiotics in human health and the subsequent increase in antimicrobial resistance are well documented.4,18-27 According to the WHO, it has been estimated that more than 50% of the antibiotics worldwide are sold without medical prescription.9,28 In addition, high resistance rates are noted in communities where antibiotic sales without prescription are common practices.6
Pharmacies often serve as the first and the last point of contact for the patients in the healthcare-seeking chain.26 The expansion of the pharmaceutical industry globally has led to the rapid growth of pharmacies in urban and peri-urban areas of many resource-constrained countries.25,26,29 While this expansion provides previously underserved populations with access to professional advice and medicines, at these pharmacies, medicine sales are largely driven by the aggressive marketing of pharmaceutical companies offering attractive incentive schemes, bonuses, and gifts for increased sales.29 Pharmacists are ideally positioned as front line health care providers to limit indiscriminate antibiotic use and promote safe and effective administration of these medications.30 The public practices of self-medication with antibiotics and the pharmacists’ practices of non-prescribed antibiotic dispensing has been extensively investigated all over the world.1,5,6,10,13,16,17,26,31-47 Unfortunately, evidence report that the practices of self-medication and the inappropriate utilization of antibiotics are in the majority of the cases, connected to the pharmacists’ frequent and unsuitable antibiotics dispensing practices, to the weak compliance and the fragile law enforcements.16,17,30,40,48,49
Published evidence suggests inappropriate dispensing practices with the public frequently acquiring non-prescribed antibiotics from the private pharmacies.11,50-52 While the pharmacist’s compliance and their appropriate dispensing practices are vital to enable the suitable utilization of antibiotics amongst the public, studies documenting antibiotic dispensing practices are to date non-existent in the Mozambican context.
The use of a qualitative analytic approach to describe the practices and reasons for non-prescribed antibiotic dispensing by pharmacists provides a first-hand and frank account of the drivers underlying this practice. An evidence-based understanding of pharmacists’ practices and enablers will contribute to the development of appropriate public health interventions. These evidence are also relevant for closing the gap between what pharmacists know they should be doing concerning prescription-only medicines and the non-prescribed antibiotic dispensing practices dynamics and reality. This study thus, aimed at describing the practices and the enablers for non-prescribed antibiotic dispensing by the pharmacists in Maputo city, Mozambique.
METHODS
Study design and setting
A descriptive qualitative study was conducted to develop an understanding of the practices of non-prescribed antibiotic dispensing among pharmacists working in private pharmacies in different socioeconomic areas of Maputo city, the capital of Mozambique. Only private pharmacies in Maputo city were included since the public pharmacies are run by state-related entities that strictly enforce prescription-only dispensing of antibiotics. Private pharmacies are registered within the Ministry of Health, are owned by individuals with a license to run the pharmacy and dispense medicines. The National Direction of Pharmacy at the Ministry of Health provided a list that indicated that by September 2018, there were registered 451 private pharmacies, 150 of which based in Maputo city. Registered private pharmacies were categorized according to the socioeconomic status (high, middle, and low) of their location (area) in the city. Using the Excel random number function three pharmacies were randomly selected from each socioeconomic area (n=9).
Study participants
In this study, we purposively enrolled pharmacists provided they were working in one of the Maputo city private pharmacies for at least twelve months before the study. The room/office was private enough to guarantee a conversation without any interruptions. In Mozambique, pharmacists are entitled to a variety of pharmaceutical activities from the preparation and supply to the distribution of medicines, chemicals, and dietary products. Pharmacists are also entitled to dispense and deliver prescription-only drugs; verify the authenticity of prescriptions and advise patients regarding the safe and storage of medicines, potential drug interactions, the side effects, and management of pharmacies.57 In this study, we adopted the term pharmacist to refer to the pharmacy professionals, their enrolment was based on the fact that they were working in Maputo city private pharmacies for at least twelve months before the study.
Study sampling and recruitment methods
A modified snowball sampling technique was employed to recruit pharmacists. The first three pharmacists from each socioeconomic area were recruited by telephone based on the information provided by the National Direction of Pharmacy. We then asked each pharmacist to identify at least two other pharmacists working in the identified pharmacies. We contacted eighteen pharmacists in total, seventeen of whom agreed to participate and were enrolled provided they were not the owners of the pharmacies and not member of the pharmacy board. This was to ensure that enrolled pharmacists were working directly with the public directly dispensing various pharmaceutical products and antibiotics with or without prescriptions.
Ethics approval
Written informed consent was read and signed by participants before starting the interview. Participants also signed the informed consent to audio record the interviews. Although we used names to identify and then contact pharmacists, their names, the names and the address of the pharmacies they worked in, were concealed to guarantee confidentiality and anonymity. Pharmacists were assured that no data leading to their identification or place of work would be published in any form. Ethical clearance was sought and obtained both at the University of KwaZulu-Natal and the National Bioethics Health Committee of Mozambique under the numbers HSS/0142/08D and 376/CNBS/18, respectively.
Data collection process and study tools
The primary data collection method used in this study was face-to-face semi-structured interviewing with open-ended questions. Semi-structured interviewing has defined goals and guidelines to enable systematic data collection while offering flexibility to change the sequences of the questions. The interview guide was based on the objectives of the study and consisted on demographic information (e.g. age, gender, years of professional experience). It also included questions regarding dispensing practices and reasons for non-prescribed antibiotic dispensing, the perceptions of pharmacists regarding patients’ attitudes and behaviours towards antibiotics use, compliance with the regulations and guidelines for antibiotic dispensing and the pharmacists suggestions to improve the current scenario. The interview guide included a definition of self-medication with antibiotics. Self-medication with antibiotics was defined as the circumstances wherein the customer requests, purchases, and administers an antibiotic without prescription to themselves or a child. Two focus group discussion sessions were planned for this study, however of the 17 enrolled, 15 pharmacists refused to participate in the focus group fearing reprisals and losing the job post at the pharmacy. Only two pharmacists consented to participate in the focus groups. Consequently, this data gathering method was dropped off due to the limited number of participants.
Since 11 pharmacists were simultaneously working in public and private pharmacies (performing day shift in public hospital or health care centre pharmacy and night and weekend shifts in the private pharmacy), interviews sessions occurred in private rooms of the public health facilities in a day and time identified by the pharmacists. The remaining six interviews of the pharmacists working exclusively for private pharmacies, occurred in a private room arranged by the researcher (upon agreement with the participant) provided the best time for the pharmacists. None of the interviews sessions occurred at the private pharmacy where the pharmacist worked, since pharmacists feared reprisals from the pharmacy owners. The room/office chosen either by the pharmacists or by the researcher was private, all the interviews settings were calm and appropriated, with interviews occurring between 16.30 p.m. and 18 p.m., after day labour hours (7.30 a.m. - to 15.30 p.m.). A small thank you gift of a USB drive (costing approximately 25 USD) was given to participants at the end of the interview session. Interview lasted between 15 to 38 minutes. Saturation, which was determined by the redundancy of data, occurred after 13 in-depth interviews; nevertheless, we continued with the remaining four interviews due to the already scheduled interviews and participants’ availability and willing to participate. These interviews also served to confirm the saturation.
Data management and analysis
The in-depth interviews were audio-recorded in Portuguese, transcribed verbatim, and translated into English. The transcriptions were subsequently checked against the audios by the interviewer. To check the accuracy of the translation, two randomly selected records were translated and then back-translated into Portuguese by a bi-lingual researcher. Data were analysed using thematic analysis, a method of analysis that aims to identify analyse and report repeated patterns of meaning (or “themes”) within a data set.59 A constant comparison approach was used with researchers reviewing and taking notes at the end of each interview session. The first two authors read and familiarised themselves with the transcripts and coded independently and later discussed the codes. Following the discussion of the codes, the first author summarized the first two authors’ codes and shared with the second and third author for further discussions and agreements. During coding, a selection of transcripts was read line by line, and initial labels or ‘codes’ applied to each passage that described the essential meaning of the data within. The coding tree included the main questions, the answers of participants, and the extracted themes and subthemes. This process allowed for the identification of potential themes that the researcher had not yet captured at the same time that tackled the validity of the codes.
The guidelines outlined by Braun and Clarke were the basis for performing the thematic analyses as a flexible technique that enabled the researcher to determine themes in several ways. Braun and Clarke guidelines follow the steps below; I) familiarising with the data; ii) generating initial codes; iii) searching for themes; iv) reviewing themes; v) defining and naming themes; and vi) producing the report.59,61 NVivo version 12 was used to store and retrieve the data.
Reflexivity is vital to promote the honesty and transparency of the research process aiming at improving the quality of research, therefore, we used a reflection diary and a constant process of self-awareness and self-reflection. Prior to the data collection sections, the researchers and research assistants undertook refreshing training in qualitative data collection and consulted the study advisor/supervisor before and after each data collection stage and during the analysis of the data. The Consolidated Criteria for Reporting Qualitative Research COREQ-Tong (2007) was performed.
RESULTS
The results of the study are presented below with sociodemographic characteristics of the participants followed by the themes and subthemes emerged, and the most relevant quote from participants. A summarized figure with the practices and reasons for non-prescribed antibiotic dispensing is presented (Figure 1).
Figure 1. Non-prescribed antibiotic dispensing.
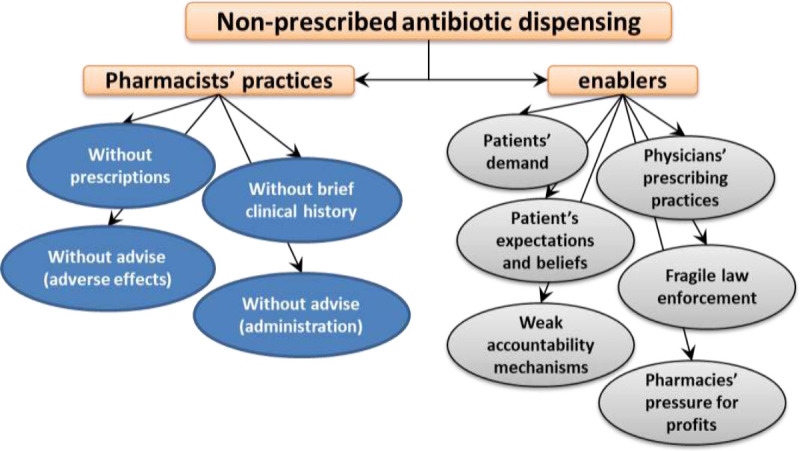
Table 1 shows the sociodemographic characteristics of the interviewed pharmacists with variation in age, gender and years of professional experience. The pharmacists’ main age was 36 years old, with the majority being male (n=11) and more than half of the pharmacists having between five to fifteen years of professional experience.
Table 1. Socio-demographic characteristics of the pharmacists.
| Participants | Age | Gender | Professional experience |
|---|---|---|---|
| Pharmacist 1 | 24 | Male | 2 years |
| Pharmacist 2 | 36 | Male | 3 years |
| Pharmacist 3 | 39 | Female | 5 years |
| Pharmacist 4 | 38 | Male | 6 years |
| Pharmacist 5 | 45 | Male | 15 years |
| Pharmacist 6 | 43 | Female | 11 years |
| Pharmacist 7 | 24 | Male | 2 years |
| Pharmacist 8 | 36 | Male | 8 years |
| Pharmacist 9 | 35 | Female | 11 years |
| Pharmacist 10 | 38 | Female | 4 years |
| Pharmacist 11 | 24 | Male | 2 years |
| Pharmacist 12 | 25 | Male | 2 years |
| Pharmacist 13 | 45 | Female | 3 years |
| Pharmacist 14 | 47 | Male | 9 years |
| Pharmacist 15 | 37 | Female | 5 years |
| Pharmacist 16 | 33 | Male | 7 years |
| Pharmacist 17 | 37 | Female | 10 years |
Non-prescribed antibiotic dispensing and the practice of self-medication
All pharmacists defined self-medication with antibiotics correctly and considered themselves well informed about the country’s legal status of prescription-only medicines. All expressed their dispensing practices were not always optimal and were aware of the risks of dispensing prescription-only medicines without a prescription. However, two pharmacists reported seeing colleagues dispensing without prescription but did not admit themselves endorsing non-prescribed antibiotic dispensing even in the face of potential sanction from pharmacy owners:
“I don’t dispense prescription-only medicines without prescriptions in any circumstances, that’s why I’m always changing the pharmacy. Some owners don’t appreciate that.” (Pharmacist 3).
“ If no prescription is seen, I don’t dispense. I’m old school, in a normal situation you and the pharmacy should be fined.” (Pharmacist 5).
In contrast, fifteen pharmacists admitted dispensing antibiotics without prescription. These pharmacists stressed self-medication with antibiotic is a common practice with people frequently requesting non-prescribed antibiotics:
“(…) nowadays it is impressive, in 10 clients, you only find 3 with prescriptions…the pharmacy is like a supermarket at some point (laughs)” (Pharmacist 1).
“We frequently sell analgesics, antibiotics, and antihistamines, every single day we sell the majority without prescriptions…let me say in four clients only one may handle the prescription.” (Pharmacists 2).
One pharmacist mentioned what he called a “never seen before” era of intense antibiotic consumption with patients and physicians, requesting and prescribing a lot of antibiotics respectively:
“I regret to say this (silence) I’m almost 12 years’ experience working with pharmacies and I’ve never experienced these high levels of self-medication practices. Anti-inflammatory and antibiotics are too much used nowadays, people can buy 5 or 10 tablets for one or 3 days. Doctors are also just prescribing antibiotics, seriously (lower voice).” (Pharmacist 9).
Pharmacist’s self-perceived role at the pharmacy
The pharmacists stated their main role is dispensing medicines rationally and responsibly. Dispensing drugs was defined as consistently and responsibly preparing, packaging, labelling, recording, and transferring drugs to a patient or intermediary who is responsible for the administration of the drug.
Pharmacists described their roles primarily as more selling than dispensing drugs suggesting that in most cases, patients know what they want, and they hand over the medicines without asking for a prescription or for health information related to the medicine:
“Well, I can say I’m more selling than dispensing medicines, the clients come, and request and I just give them what they want.” (Pharmacist 11).
“ (…) the person comes to me and says I need cotrimoxazole, 20 tablets, there are no prescriptions on his hands. Should I ask why or what for? (silent). I don’t think so, people come to the pharmacy knowing very well what they want…” (Pharmacist 7).
Practices of non-prescribed antibiotic dispensing
Requesting for a valid prescription: Valid prescription was defined as the original script signed by the prescriber within not more than seven days. To access the practice of requesting valid prescriptions, pharmacists were presented the following probing question: If a customer comes to your pharmacy and requests a certain antibiotic what is the first question you ask and what do you do next? Of the seventeen pharmacists, two responded they would first request the doctor’s prescription:
“First thing…clients need to show up the doctor’s prescription… if I don’t see I would ask for it and nothing else, would do without.” (Pharmacist 3).
“Well, I need to ask about the doctors’ paper (scripts) otherwise how should I know the type/class, quantity, dosage of that antibiotic?” (Pharmacist 5).
The majority of pharmacist said they would dispense the antibiotic after questioning the customer the following:
“I would ask what health problems the customer intends to deal with?” (Pharmacist 1).
“I would ask what age the patient is (…)” (Pharmacist 6).
“I ask what the antibiotic is for and dispense it “ (Pharmacist 4).
“I would ask the quantity of the antibiotics, for how many days” (Pharmacist 8).
Instructing patients on the intake of the antibiotic and safety issues
We assessed non-prescribed antibiotic dispensing practices by questioning if pharmacists ask for a brief clinical history of the patients; if they instruct patients on how they should take the antibiotic; and if they counselled on safety-related information and on the importance of completing the course of antibiotics, two responded:
“…although I should do, I don’t ask about allergy when clients come and request, I assume they know the antibiotic and have taken at least once.” (Pharmacist 4).
“We don’t pay attention to the customer, it works like this; the customer arrives and requests, pharmacist dispenses and full stop.” (Pharmacist 8).
Why dispensing non-prescribed antibiotics?
Five subthemes emerged under this theme, namely; the customer’s behaviour and beliefs on the curative power of antibiotics; the physicians’ prescribing practices; the run for pharmacy profits, the law enforcement, and the accountability mechanisms.
Patients’ behaviour and beliefs on the curative power of antibiotics: According to pharmacists, patients are increasingly using pharmacies as their first point of contact when seeking health care. This trend influences pharmacists dispensing practices particularly because, many patients believe “antibiotics cure everything”. Questioned what they perceive as the main reasons for self-medication with antibiotics, pharmacists responded as illustrated:
“Clients’ behaviour is something else, I don’t know how to classify, people think they don’t need doctors, the person has fever and cough or pain, comes to the pharmacy instead of going to the health care centre, there is a concerning behaviour of self-medication…” (Pharmacist 11).
“(…) for cough, people want antibiotics, for pain somewhere, antibiotics, toothache, antibiotics, they believe antibiotics cure everything!” (Pharmacist 8).
Physicians’ prescribing practices: Some pharmacists believe, by frequently prescribing the same or similar antibiotics for different health conditions and for different patients, physicians are influencing patients’ decisions to by-pass medical services and indulge in self-medication with antibiotics. Because patients tend to share experiences with others, according to pharmacists, physicians practices may lead patients to make use of the medical information and think they could always use these antibiotics for any other self-diagnosed diseases and directly request these non-prescribed antibiotics from the pharmacies. Additionally, pharmacists believe physicians are over prescribing antibiotics:
“People share information of health experiences, medications and even prescriptions, I think they pay attention to what has been prescribed, what cured this or that and later they make use of that information”. (Pharmacist 17).
“Nowadays doctors and nurses just prescribe antibiotics, for anything even viral infections they send patients to by amoxicillin, a sore throat, azithromycin, for a simple cough, cotrimoxazole. It is now trending or fancy prescribing these things. I’m not sure they all need antibiotic treatment and most of the time very potent ones” (Pharmacist 3).
The run for pharmacy profits: The respondents stressed concerns regarding the pharmacy owner’s pressure and demand for profits added to their own need for a salary income as an influencing factor for non-prescribed antibiotic dispensing practices. Pharmacists reported some of their employers give attractive incentives to the pharmacist selling the most medicines per month which is contrary to the optimal dispensing practice guidelines:
“ Antibiotics are the most sold medicines, so there is no point in working in a pharmacy and not selling antibiotics without prescription, you end up fired. The owner wants profits and I need the salary.” (Pharmacist 16).
“ If you don’t sell antibiotics, analgesics, and anti-inflammatory drugs, you are doing nothing, I have colleagues who earn selling bonus of over their salaries because they made profits. The first thing the owner says when you are offered the job vacancy: here we sell medicines, so make sure you sell…they want profits just that, we need job.” (Pharmacist 8).
Law enforcement and accountability mechanisms: Although participants admitted their dispensing practices are suboptimal, they believed the problem would be easily solved if compliance and accountability measures were enforced. This, according to the participants, would educate owners, pharmacists, and clients regarding the optimal use and would slowly eradicate the practices of self-medication with antibiotic and non-prescribed antibiotic dispensing. Two participants suggested:
“Health authorities should visit pharmacies more often and see what is happening around us, if only one or two owners receive a huge fine by the authorities this would be known by others and would stop. I think authorities must do this.” (Pharmacist 10).
“We, pharmacists, know all the consequences of non-prescribed antibiotic dispensing, we know. But when you get to the position at the pharmacy as a magic trick you tend to forget all in the name of the owner’s profits and to protect your month-end and job post.” (Pharmacist 6).
Pharmacists suggestions for improving the rational use of antibiotics
Challenge the culture of self-medication, raise awareness and educate patients: Enforcing compliance to the standard guidelines dispensing antibiotics at the pharmacy level is a priority action for changing the culture of self-medication, according to the pharmacists. One stated:
“People should be told and educated that the pharmacist is not a doctor and a pharmacy is not a health care centre, maybe it would be good to explain to them our roles in the pharmacy, so they stop pressing us and change behaviour.” (Pharmacist 7).
One pharmacist also stressed the need to start education at the household level considering the strong influence family members have in the health-seeking behaviour:
“ educating people on what is a pharmacy, how to use medicines properly, when to go to a pharmacy, this should start at home, with the family”(Pharmacist 12).
Strengthen law enforcement and control: Enforcing the law and control the level of guidelines compliance are necessary to ensure medicines are dispensed for health benefits and not exclusively for pharmacy profits. Pharmacists added that consistent and persistent law enforcement and accountability measures would prevent pressure and irrational dispensing. The quote below illustrates:
“ We know the inspection is there, people are there for this work, but I don’t see them working properly, they should be consistent to implement the law and sue non-complaints owners with expensive fees.” (Pharmacist 10).
Establish a Pharmacy Profession Association: The interviewed pharmacists were not aware of the existence of the Pharmacist’s Professional Association in country, which participants regarded as a gap for better address the profession challenges and maximize the skills. For the majority of pharmacists, the establishment of a Pharmacy Professionals Association would be beneficial to organize the collective voice in calling for implementation of standard guidelines addressing the multiple issues regarding medicine use including non-prescribed antibiotic dispensing and indirectly, the profit margin pursuit of some pharmacy owners. Two pharmacists said:
“We need to be more organized as pharmacy professionals, only this would help us addressing the challenges and barriers we face during activities”. (Pharmacist 9).
“(…) If there was an association among pharmacy professionals, the pharmacy owner would behave better, that would work as a controlling body that protects the professionals.” (Pharmacist 12).
Pharmacy and pharmacists awareness activities: As a platform to promote the work, skills and roles of pharmacists and emphasise the role and importance of this service in the health care chain, some pharmacists suggested having an annual pharmacy awareness week. This would demonstrate a variety of activities focused on highlighting the positive role of pharmacists, improving prescribing practices, and promoting the rational use of medicines among prescribers, patients, and pharmacists:
“ If we could just have one month or a week annually for celebrating the pharmacists and having those health fairs to raise awareness and educate more people including doctors to understand the need to prescribe properly, that would be good, people would also get to know our roles…”(Pharmacist 8).
“ I see this situation improving, like if we had a national pharmacy awareness week or one day with a lot of campaigns focused on the community but also the prescribers and the pharmacists themselves. Without an professional association to fight for this, it can be complex, I’m not saying impossible, but this would work better if we put it as an association” (Pharmacist 17).
DISCUSSION
While high-income countries are moving towards a more controlled antibiotic and medicine use, some low-income countries may be moving in the opposite direction. This study sought to describe the practices and reasons for non-prescribed antibiotic dispensing by pharmacists from private pharmacies in Maputo city using a qualitative approach and insight from the pharmacists themselves. Unsuitable dispensing of antibiotics poses an urgent public health threat especially for the resource constrained countries where fragile health care systems are faced with high burden of infectious diseases that need antibiotics to be rationally used and available.
Studies have reported the non-prescription sale and utilization of antibiotics as one of the major reasons for increasing irrational antibiotic consumption which paves the way to the emergence of antimicrobial resistance.26,56,62-64 Mozambican health authorities and partners have emphasized the urgent need for better use of antibiotics at all levels to reduce inappropriate antibiotic consumption and contain antimicrobial resistance.3 To date, research investigating pharmacists’ non-prescribed antibiotic dispensing practices in Mozambique is non-existent. The findings will contribute to generating evidence-based information to help developing appropriate interventions to mitigate the practices of self-medication with antibiotics and of dispensing of prescription-only medicine such as antibiotics, without professional oversight.
Pharmacists’ non-prescribed antibiotic dispensing practices
The pharmacists in this study could not deny their non-prescribed antibiotic dispensing as “daily practices”. Also the illegality of the practice is well acknowledged, however, these non-prescribed antibiotics dispensing practices are at the same time suggestive of a high-pitched magnitude of self-medication with antibiotics. In other settings, pharmacists that admitted their illegal and irresponsible dispensing practices of antibiotics were noticed.16,17,25,26,37
Despite being the first and last point of contact in the health-seeking chain, pharmacists perceived their role as primarily drug sellers than drug dispensers, with a limited health advisory role. To this is added the fact that the advisory role regarding the safety of antibiotics was absent in most of the non-prescribed antibiotic dispensing events, leaving patients purchasing these medicines at their own risks. When not requesting for a valid antibiotic prescription, not explaining the side effects and all the relevant information regarding the antibiotic being purchased, pharmacists’ found themselves practicing more as sellers of drugs than as drug dispensers health care professionals. This suggests poor dispensing practices which may determine the underestimation of the pharmacy profession.
According to Fang et al., (2013), in high-income countries the status of pharmacists are well established and pharmacy health care services are considered integral to health care chain.65 On the other hand, Azhar et al., (2009), pointed to the emergent status of the pharmacist in LMICs, where their roles are limited to drug manufacturing, procurement, dispensing and storage.66 In addition, pharmacists in LMICs have a minimal involvement in providing patient care related services and in promoting initiatives related to rational use of medicines, promoting self-testing and monitoring health, such as rapid testing malaria and other non-communicable diseases and quick point of care diagnosis for chronic diseases, for example.67,68
As pharmacists regarded themselves as mere drug sellers and dispensers, the opportunity should be grasped to include pharmacists in designing refreshing trainings, health promotion fairs, counselling events, awareness day or week, and campaigns towards emphasizing the need to rationally use the medicines, promote the image of pharmacists and their role in the health care chain. These actions would contribute to retell the pharmacist’s roles in promoting the adequate use of antibiotics and influence behaviour change either at the community or at the health care system level. Furthermore, studies have shown positive impact and significant improvement in the quality use of antibiotics with the inclusion of pharmacists in different health promotion activities and health care settings of middle and high- income countries.69-71
Pharmacists non-prescribed antibiotic dispensing enablers
Pharmacy clients’ behaviour
Rodrigues (2020), has disclosed that self-medication with antibiotics are practices that do not always follow biomedical recommendations of rational use, rather, individuals are actively engaged in therapeutic processes, that emphasises self-reliance and individual responsibility for one’s own health.5 Furthermore, authors have pointed out that self-medication practices are entrenched not only to the individual’s previous successful experiences with antibiotics but also to the interplay of the knowledge and expectations of prescribers and patients, and to the individuals and public beliefs on the healing power of antibiotics.12,13,23,31,32,72-74 However, studies also suggested the behaviour behind the practices of seeking non-prescribed antibiotics are also influenced by the characteristics of the health care system and by the pharmacy regulatory environment.9,28 These experiences are then part of the process of social construction of the health care centre, the pharmacy, the pharmacists, the medicines and antibiotics in particular, knowledge which are shared with the people from the social group (family members, neighbours, and friends). Previous studies have reported how participants have taken advantage of previous experiences, past prescriptions and leftovers antibiotics to self-treat new sickness events.5,7,31,47,75 These two factors – the use of medical information and or knowledge gained from past sickness events and the sharing of medical and health information among individuals and groups – pave the way to expand the practices of self-treatment of self-diagnosed diseases which is largely done by approaching the pharmacy and request/purchase antibiotics previously used rather than consulting a physician.
This set of factors affect individual’s intention, attitudes and behaviours driving their demand for non-prescribed antibiotics. It is therefore, important to contextually examine the sociocultural, economic and political contingencies that may influence the needs for antibiotics by consider the individual’s rationales as integrant part of the solution.5 Also, engage with all different enablers and actors to tackle the behaviour and the misconceptions about antibiotics by illustrating the disadvantages, the risks and the consequences of self-medication with antibiotics and educate pharmacy clients to improve antibiotic use could be useful.
Physicians’ prescribing practices
Pharmacists in this study believe physicians’ prescribing practices influence and contribute to increase self-medication with antibiotics. These prescribing practices include - overprescribing and or frequently prescribing the same antibiotics for different health conditions, quick antibiotic prescribing, blind or needless prescribing, poor communication with patients regarding the prescribed antibiotic and its side effects. Although published evidence regarding antibiotic prescription rates and patterns for outpatients in Mozambique are scarce. One unpublished study by Mamade et al., (2019) shows suboptimal oral antibiotics prescription with high proportion of antibiotics such us amoxicillin, cotrimoxazole and metronidazole being prescribed for outpatients in Maputo Central Hospital.76 While studies have reported inappropriate and high rates of antibiotic prescription in other settings evidence shows that the most prescribed antibiotics are at the same time, the most requested non-prescribed antibiotics, with antibiotics such amoxicillin, amoxicillin with clavulanic acid, metronidazole and cotrimoxazole being in the top of the list.5,48,79,80 The patients’ expectations for antibiotics prescriptions are one of the causes of pressure for physicians to prescribe.77 Pharmacists, therefore, criticise the physicians for contributing to strengthen the public belief that antibiotics are effective and quick to treat all diseases.23 Moreover, because medicines are seem as commodities and precious goods, and patients are not active recipients of health care, the individual’s adjust, make considerations and use the accumulated and constructed health information gained thanks to their experiences and their interactions with previously prescribed or used medicines, with health care providers and prescribers.5,31,79 Patients tend to recall the bad or good previous experiences with sickness events, the healing process, the therapeutic itinerary adopted and the prescribed medications and their sources to socially construct the need for antibiotic and or make decision to demand for it. Despite studies reporting the huge pressure physicians receive from patients to prescribe antibiotics, strategies to involve physicians and warn about the patients expectations for antibiotics are needed. Additionally, physicians should be alerted to be more vigilant to their prescribing practices, giving specially attention and explanation to the patients, mainly those in needs for antibiotic prescriptions, explaining and clarifying the utility, the effect on that specific health condition healing process, the side effects and the care patients ought to have while using the prescribed antibiotic. These actions together would be useful to discourage patients to misuse the health information and control their expectations for antibiotic prescriptions.
Pharmacies’ run for profits
Consistent with previous studies, our study findings reveal the influence of the proliferation of pharmacies and inter-pharmacy competitiveness on the irrational dispensing of antibiotics.16,26 The run for profits linked to the aggressive marketing strategies with incentives for pharmacists to increase the sales and the pressure to meet financial targets contributes to the suboptimal and unethical antibiotic dispensing within the pharmacies. To this is added the absence of robust law enforcement and accountability mechanisms to penalize the non-compliant pharmacies and pharmacists. The patients, therefore, have no difficulties accessing and requesting non-prescribed antibiotic. A study conducted in Nigeria reported limited controls on the sales or advertisement of antibiotics that created opportunities for misinformation and misperceptions on the antibiotic utilization and conservancy which exacerbated improper antibiotic use.54 In Mozambique, the proliferation of pharmacists within the city and suburbs is noticeable, leading to competition and to poor practices of dispensing medicines and antibiotics.3 Multi-layer robust law enforcement that targets pharmacists and pharmacies by prosecuting, punishing, and finning the non-compliant pharmacists added to the cancellation of the registration and operation license would be useful. Implementing these measures would highly contribute to discourage non-prescribed antibiotic dispensing and enabling good dispensing practices concomitant to discouraging self-medication with antibiotics.
Pharmacists’ suggestions to improve the scenario
Towards the improvement of the situation, pharmacists suggested interventions at three levels namely:
1) at the pharmacy profession level
The Pharmacy Professional Association in Mozambique was officially created in December 2014, and the first national conference only happened in November 2018. However, at the time of this study, very little dissemination, awareness and other activities regarding this association had happened so far. This may be the reason interviewed pharmacists were not aware of the existence of the organization, therefore, the participants advocated for the establishment of a Pharmacy Professional Association to champion their collective professional interests and provide a national platform for addressing the multiple challenges and dilemmas pharmacists face in their duties, particularly regarding the dispensing practices. Increasing the professional association visibility and activities among the pharmacists would be helpful to be aware of the dynamics of the profession and effectively address the challenges pharmacists face. Additionally, the study participants are aware of the existence of the world antibiotic awareness week in November every year, where a global campaign aimed at increasing awareness of antibiotic resistance and to encourage best practices among the general public, health workers and policy makers. However, the establishment of a national annual pharmacy awareness week or day, with a variety of activities focused on highlighting the positive role of pharmacists, improving prescribing practices, and promoting the rational use of medicines among prescribers, patients’ and pharmacists were suggested as a platform towards appropriate antibiotic use and conservancy. Concordant findings were reported in India, in study where pharmacists considered the institution of an awareness day as a good attempt to improve knowledge.26
2) at the policy level
The participants believe health authorities, law enforcement institutions, policy makers and pressure groups ought to work together to improve supervision, monitor and publicly apply heavy penalties to non-compliant pharmacies and pharmacists to discourage the practice. In Mozambique prescription-only medicines regulations and guidelines are embedded in the Drug Law number 12/2017. Despite establishing penalties for the non-complaints, to date no strong penalties were publicly applied to pharmacies dispensing prescription-only medicines. This may explain why, no pharmacy has been penalised for non-prescription antibiotic dispensing. Publicly applied penalties would have an impact on decreasing the non-prescription dispensing of antibiotics and other prescription-only medicines. Moreover, studies in other countries have shown that implementation of enforcement measures guided by the existing laws and guidelines for prescribing and dispensing antibiotics has led to a decrease in over consumption of antibiotics.70,80-82
3) at community level
Pharmacists advocate for public health and health promotion professionals to constantly raise awareness and intensively highlight the risks and consequences of practicing self-medication by tackling the knowledge gaps and the misapprehensions, while increasing awareness campaigns motivating the community to monitor and report the non-compliant pharmacists/pharmacies. Interventions targeted at enhancing behaviour are more likely to be effective. However, for health policies to be more effective and acceptable, strategies to raise awareness and promote the better use of health care services should consider health-seeking behaviour and its social, economic and political determinants as an integrant parts of the prevention, treatment and healing process.
Finally, this study sheds light on significant issues to be addressed in order to enhance the appropriate utilization of antibiotics. Concordant with Al-Kubaisi et al., (2018) the study has revealed that the weak knowledge, the expectations and misapprehensions of antibiotics by the public are enhanced in patients by both the pharmacists who dispense antibiotics without prescriptions and by the physicians who quickly and blindly prescribe antibiotics to their patients.13 While increasing awareness regarding the appropriate antibiotic use and conservancy among pharmacy clients’ and communities is paramount, elevating the advisory role of the pharmacist in delivering patient-centred services of health promotion, infection control, prudent antibiotic utilization, and nutrition are important health education strategies for better antibiotic utilization and conservancy in Mozambique.65,67
Limitations
This study presents a comprehensive summary of the phenomena of non-prescribed antibiotic dispensing practices in Maputo city, Mozambique. Notwithstanding the inclusion of pharmacies from the three socio-economic areas of the city, the sample size of pharmacies and pharmacists represents a limitation since the findings of this study are not representative of all pharmacies and pharmacists in the city. Additionally, having some participants giving short answers, feeling embarrassed and skipping questions of the interview guide constituted another study limitation as it reduced the response rate. Moreover, the tools of this study could be improved if focus group discussions with pharmacists could be performed to capture the opinions of pharmacists in a group and compare them to the ones from the individual interviews. Further research involving larger samples, qualitative, ethnographic, observational, and quantitative studies concerning the dispensing practices, the barriers for better compliance and challenges pharmacists face would provide an expanded knowledge base for the development of interventions for a national roll-out.
CONCLUSIONS
This study revealed knowledge regarding the non-prescribed antibiotic dispensing practices and enablers within the private pharmacies in Maputo city. Antibiotic dispensing was widespread with precarious, unsafe, irresponsible, suboptimal, and unethical practices. Pharmacists are troubled by non-prescribed antibiotic and self-medication practices, perceiving themselves as being caught between the rock and a hard place. On the one hand, the patient’s requests for antibiotics without valid prescriptions, and pharmacists’ desire to assist based on their role in the pharmacy, the pressure for profits and an understanding of the larger forces driving the practices of self-medication with antibiotics - rock. On the other hand, pharmacists’ knowledge of the legal status of antibiotics and the public health consequences of their inappropriate dispensing and their professional and ethical responsibility for upholding this law - hard place. Understanding the dynamics and the complex nuances associated with self-medication with antibiotics of patients and the non-prescribed antibiotic dispensing practices of pharmacists is relevant to generate evidence-based information. These would be useful for designing impactful and contextual strategies towards strengthening health promotion and awareness-raising towards antibiotic stewardship and conservancy in-country. Also, a top-down approach from the regulators is needed to ameliorate the run for profits from the pharmacy owners, removing pressure and enhancing good dispensing practices of pharmacists and discouraging non-compliant pharmacists.
ACKNOWLEDGMENTS
The ISCISA, the NORHED Project, and University of KwaZulu Natal (UKZN) are acknowledged for the incentive and provision of resources for this review. The UKZN College of Health Sciences, School of Nursing, and Public Health are acknowledged for the provision of research methodology courses as well as manuscript writing workshops. António Tovela is acknowledged for the language writing contributions.
Footnotes
CONFLICT OF INTEREST
The authors declare that they have no competing interests.
FUNDING
This study was partially funded by ISCISA via the NORHED Project Grant and by the CHS-UKZN throughout a PhD scholarship awarded to the first author. ISCISA, NORHED and UKZN had no role in the study design, data collection and analysis, decision to publish or even preparation of the manuscript.
Contributor Information
Neusa F. Torres, Higher Institute for Health Sciences (ISCISA). Maputo (Mozambique). torresneusa@gmail.com
Vernon P. Solomon, MSc (Clin Psychol). Discipline of Pharmaceutical Sciences School of Health Sciences, University of KwaZulu Natal. Durban (South Africa). vernonsolomon@gmail.com
Lyn E. Middleton, Phd (Nurs & Educ). Discipline of Pharmaceutical Sciences, School of Health Sciences, University of KwaZulu Natal. Durban (South Africa). lynelizabethmiddleton@gmail.com
References
- 1.Auta A, Hadi MA, Oga E, Adewuyi EO, Abdu-Aguye SN, Adeloye D, Strickland-Hodge B, Morgan DJ. Global access to antibiotics without prescription in community pharmacies:A systematic review and meta-analysis. J Infect. 2019;78(1):8–18. doi: 10.1016/j.jinf.2018.07.001. [DOI] [PubMed] [Google Scholar]
- 2.Lipsitch M, Samore MH. Antimicrobial use and antimicrobial resistance:a population perspective [published correction appears in Emerg Infect Dis 2002 May; 8(5):540] Emerg Infect Dis. 2002;8(4):347–354. doi: 10.3201/eid0804.010312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sigaúque B, Sevene E. Situations analysis and recomendations:Antibiotic use and resistance in Mozambique. [accessed Aug 9 2020]; Available at:https://cddep.org/wp-content/uploads/2017/08/sitan_booklet_a4.pdf .
- 4.World Heath Organization Assessing on-prescription and inappropriate use of antibiotics:report on survey. Geneva: WHO; 2019. [Google Scholar]
- 5.Rodrigues CF. Self-medication with antibiotics in Maputo, Mozambique:practices, rationales and relationships. Palgrave Commun. 2020;6(1):1–12. doi: 10.1057/s41599-019-0385-8. [DOI] [Google Scholar]
- 6.Morgan DJ, Okeke IN, Laxminarayan R, Perencevich EN, Weisenberg S. Non-prescription antimicrobial use worldwide:a systematic review. Lancet Infect Dis. 2011;11(9):692–701. doi: 10.1016/s1473-3099(11)70054-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sambakunsi CS, Småbrekke L, Varga CA, Solomon V, Mponda JS. Knowledge, attitudes and practices related to self-medication with antimicrobials in Lilongwe, Malawi. Malawi Med J. 2019;31(4):225–232. doi: 10.4314/mmj.v31i4.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Foster EK, Bandawe CR. How much do patients in Blantyre, Malawi know about antibiotics and other prescription only medicines? Malawi Med J. 2014;26(1):12–15. [PMC free article] [PubMed] [Google Scholar]
- 9.World Heath Organization Antimicrobial. Resistance:Global Report on Surveillance. Geneva: WHO; 2014. [Google Scholar]
- 10.Mate I, Come CE, Gonçalves MP, Cliff J, Gudo ES. Knowledge, attitudes and practices regarding antibiotic use in Maputo City, Mozambique. PLoS One. 2019;14(8):e0221452. doi: 10.1371/journal.pone.0221452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Torres NF, Chibi B, Middleton LE, Solomon VP, Mashamba-Thompson TP. Evidence of factors influencing self-medication with antibiotics in low and middle-income countries:a systematic scoping review. Public Health. 2019;168:92–101. doi: 10.1016/j.puhe.2018.11.018. [DOI] [PubMed] [Google Scholar]
- 12.Zajmi D, Berisha M, Begolli I, Hoxha R, Mehmeti R, Mulliqi-Osmani G, Kurti A, Loku A, Raka L. Public knowledge, attitudes and practices regarding antibiotic use in Kosovo. Pharm Pract (Granada) 2017;15(1):827. doi: 10.18549/pharmpract.2017.01.827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Al-Kubaisi KA, De Ste Croix M, Vinson D, Sharif SI, Abduelkarem AR. What drives using antibiotic without prescriptions?A qualitative interview study of university students in United Arab Emirates. Pharm Pract (Granada) 2018;16(2):1172. doi: 10.18549/pharmpract.2018.02.1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jakupi A, Raka D, Kaae S, Sporrong SK. Culture of antibiotic use in Kosovo - an interview study with patients and health professionals. Pharm Pract (Granada) 2019;17(3):1540. doi: 10.18549/pharmpract.2019.3.1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mansour H, Feghali M, Saleh N, Zeitouny M. Knowledge, practice and attitudes regarding antibiotics use among Lebanese dentists. Pharm Pract (Granada) 2018;16(3):1272. doi: 10.18549/pharmpract.2018.03.1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bahnassi A. A qualitative analysis of pharmacists'attitudes and practices regarding the sale of antibiotics without prescription in Syria. J Taibah Univ Med Sci. 2015;10(2):227–233. doi: 10.1016/j.jtumed.2014.09.001. [DOI] [Google Scholar]
- 17.Bahnassi A. Pharmacists Views and Practices in Regard to Sales of Antibiotics Without a Prescription in Madinah, Saudi Arabia. J Patient Saf. 2016;12(3):159–164. doi: 10.1097/pts.0000000000000087. [DOI] [PubMed] [Google Scholar]
- 18.Ahmad A, Patel I, Mohanta G, Balkrishnan R. Evaluation of self medication practices in rural area of town sahaswan at northern India. Ann Med Health Sci Res. 2014;4(Suppl 2):S73–S78. doi: 10.4103/2141-9248.138012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sawalha AF. A descriptive study of self-medication practices among Palestinian medical and nonmedical university students. Res Social Adm Pharm. 2008;4(2):164–172. doi: 10.1016/j.sapharm.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 20.Abdulraheem IS, Adegboye A, Fatiregun AA. Self-medication with antibiotics:empirical evidence from a Nigerian rural population. Br J Pharm Res. 2016;11(5):1–13. doi: 10.9734/BJPR/2016/25268. [DOI] [Google Scholar]
- 21.Afolabi AO. Factors influencing the pattern of self-medication in an adult Nigerian population. Ann Afr Med. 2008;7(3):120–127. doi: 10.4103/1596-3519.55666. [DOI] [PubMed] [Google Scholar]
- 22.Al-Hamad A. Over-the-counter delivery of antibiotics:are we sending the right message? Am J Infect Control. 2012;40(1):81–82. doi: 10.1016/j.ajic.2011.08.011. [DOI] [PubMed] [Google Scholar]
- 23.Alhomoud F, Aljamea Z, Basalelah L. “Antibiotics kill things very quickly”- consumers'perspectives on non-prescribed antibiotic use in Saudi Arabia. BMC Public Health. 2018;18(1):1177. doi: 10.1186/s12889-018-6088-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alkhatatbeh MJ, Alefan Q, Alqudah MA. High prevalence of self-medication practices among medical and pharmacy students:a study from Jordan. Int J Clin Pharmacol Ther. 2016;54(5):390–398. doi: 10.5414/cp202451. [DOI] [PubMed] [Google Scholar]
- 25.Belkina T, Duvanova N, Karbovskaja J, Tebbens JD, Vlcek J. Antibiotic use practices of pharmacy staff:a cross-sectional study in Saint Petersburg, the Russian Federation. BMC Pharmacol Toxicol. 2017;18(1):11. doi: 10.1186/s40360-017-0116-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kotwani A, Wattal C, Joshi PC, Holloway K. Irrational use of antibiotics and role of the pharmacist:an insight from a qualitative study in New Delhi, India. J Clin Pharm Ther. 2012;37(3):308–312. doi: 10.1111/j.1365-2710.2011.01293.x. [DOI] [PubMed] [Google Scholar]
- 27.Mshana SE, Matee M, Rweyemamu M. Antimicrobial resistance in human and animal pathogens in Zambia, Democratic Republic of Congo, Mozambique and Tanzania:an urgent need of a sustainable surveillance system. Ann Clin Microbiol Antimicrob. 2013;12:28. doi: 10.1186/1476-0711-12-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.World Health Organization. The evolving threat of antimicrobial resistance, Options for action. Geneve: WHO; 2012. [Google Scholar]
- 29.Kamat VR, Nichter M. Pharmacies, self-medication and pharmaceutical marketing in Bombay, India. Soc Sci Med. 1998;47(6):779–794. doi: 10.1016/s0277-9536(98)00134-8. [DOI] [PubMed] [Google Scholar]
- 30.Black E, Cartwright A, Bakharaiba S, Al-Mekaty E, Alsahan D. A qualitative study of pharmacists'perceptions of, and recommendations for improvement of antibiotic use in Qatar. Int J Clin Pharm. 2014;36(4):787–794. doi: 10.1007/s11096-014-9960-7. [DOI] [PubMed] [Google Scholar]
- 31.Aponte-González J, González-Acuña A, Lopez J, Brown P, Eslava-Schmalbach J. Perceptions in the community about the use of antibiotics without a prescription:Exploring ideas behind this practice. Pharm Pract (Granada) 2019;17(1):1394. doi: 10.18549/pharmpract.2019.1.1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aslam A, Gajdács M, Zin CS, Binti Abd Rahman NS, Ahmed SI, Jamshed SQ. Public Awareness and Practices towards Self-Medication with Antibiotics among the Malaysian Population: A Development of Questionnaire and Pilot-Testing. . Antibiotics (Basel) 2020;9(2):97. doi: 10.3390/antibiotics9020097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Berzanskyte A, Valinteliene R, Haaijer-Ruskamp FM, Gurevicius R, Grigoryan L. Self-medication with antibiotics in Lithuania. Int J Occup Med Environ Health. 2006;19(4):246–253. doi: 10.2478/v10001-006-0030-9. [DOI] [PubMed] [Google Scholar]
- 34.Bilal M, Haseeb A, Khan MH, Arshad MH, Ladak AA, Niazi SK, Musharraf MD, Manji AA. Self-Medication with Antibiotics among People Dwelling in Rural Areas of Sindh. J Clin Diagn Res. 2016;10(5):OC08–OC13. doi: 10.7860/jcdr/2016/18294.7730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brata C, Fisher C, Marjadi B, Schneider CR, Clifford RM. Factors influencing the current practice of self-medication consultations in Eastern Indonesian community pharmacies:a qualitative study. BMC Health Serv Res. 2016;16:179. doi: 10.1186/s12913-016-1425-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Elong Ekambi GA Okalla, Ebongue C, Penda IC, Nnanga Nga E, Mpondo Mpondo E, Eboumbou Moukoko CE. Knowledge, practices and attitudes on antibiotics use in Cameroon:Self-medication and prescription survey among children, adolescents and adults in private pharmacies. PLoS One. 2019;14(2):e0212875. doi: 10.1371/journal.pone.0212875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Emeka PM, Al-Omar MJ, Khan TM. A qualitative study exploring role of community pharmacy in the irrational use and purchase of nonprescription antibiotics in Al Ahsa. Eur J Gen Med. 2012;9(4):230–234. doi: 10.29333/ejgm/82436. [DOI] [Google Scholar]
- 38.Gajdács M, Paulik E, Szabó A. Knowledge, Attitude and Practice of Community Pharmacists Regarding Antibiotic Use and Infectious Diseases:A Cross-Sectional Survey in Hungary (KAPPhA-HU) Antibiotics (Basel) 2020;9(2):41. doi: 10.3390/antibiotics9020041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Grigoryan L, Germanos G, Zoorob R, Juneja S, Raphael JL, Paasche-Orlow MK, Trautner BW. Use of Antibiotics Without a Prescription in the U.S. Population:A Scoping Review. Ann Intern Med. 2019;171(4):257–263. doi: 10.7326/m19-0505. [DOI] [PubMed] [Google Scholar]
- 40.Hadi MA, Karami NA, Al-Muwalid AS, Al-Otabi A, Al-Subahi E, Bamomen A, Mohamed MM, Elrggal ME. Community pharmacists'knowledge, attitude, and practices towards dispensing antibiotics without prescription (DAwP):a cross-sectional survey in Makkah Province, Saudi Arabia. Int J Infect Dis. 2016;47:95–100. doi: 10.1016/j.ijid.2016.06.003. [DOI] [PubMed] [Google Scholar]
- 41.Heidarifar R, Koohbor M, Kazemian Mansourabad M, Mikaili P, Sarahroodi S. Selfmedication with Antibiotics among Iranian Population in Qom State. J Sci Innov Res. 2013;2(4):785–789. [Google Scholar]
- 42.Horumpende PG, Sonda TB, van Zwetselaar M, Antony ML, Tenu FF, Mwanziva CE, Shao ER, Mshana SE, Mmbaga BT, Chilongola JO. Prescription and non-prescription antibiotic dispensing practices in part I and part II pharmacies in Moshi Municipality, Kilimanjaro Region in Tanzania:A simulated clients approach. PLoS One. 2018;13(11):e0207465. doi: 10.1371/journal.pone.0207465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Israel EU, Emmanuel EG, Sylvester EG, Chukum E. Self-medication with antibiotics amongst civil servants in Uyo, Southern Nigeria. J Adv Med Pharm Sci. 2015;2(3):89–97. doi: 10.9734/JAMPS/2015/15147. [DOI] [Google Scholar]
- 44.Khan RA. Self-medication with antibiotics:Practices among Pakistani students in Sweden and Finland. [accessed May 9 2020]. Available at:http://www.diva-portal.org/smash/record.jsf?pid=diva2%3A452461 .
- 45.Llor C, Cots JM. Dispensing of antibiotics without a medical prescription and communication skills of pharmacists. Aten Primaria. 2013;45(9):496–497. doi: 10.1016/j.aprim.2013.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ngigi C.K, Mwagiru P, Wala J. Self-Medication with antibiotics prior to seeking treatment among adult patients attending outpatient department at Gatundu Sub-County Hospital, Kiambu county, Kenya. Imp J Interdiscip Res. 2016;2(8):609–616. [Google Scholar]
- 47.Torres NF, Solomon VP, Middleton LE. Patterns of self-medication with antibiotics in Maputo City:a qualitative study. Antimicrob Resist Infect Control. 2019;8:161. doi: 10.1186/s13756-019-0618-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Miller R, Goodman C. Performance of retail pharmacies in low- and middle-income Asian settings:a systematic review. Health Policy Plan. 2016;31(7):940–953. doi: 10.1093/heapol/czw007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shet A, Sundaresan S, Forsberg BC. Pharmacy-based dispensing of antimicrobial agents without prescription in India:appropriateness and cost burden in the private sector. Antimicrob Resist Infect Control. 2015;4:55. doi: 10.1186/s13756-015-0098-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.The Center For Disease Dynamics, Economics &Policy. Situations Analysis and recomendations:Antibiotic Use and Resistance in Mozambique. [accessed May 9 2020]. Available at:https://cddep.org/wp-content/uploads/2017/06/moz_sitan_4_page_brochure_b_1-1.pdf .
- 51.Centro de Integridade Pública. A falta de medicamentos estátambém associada a precariedade no funcionamento da logística farmacêutica no sistema público de saúde. Maputo: CIP; 2015. [Google Scholar]
- 52.Município de Maputo. [Informal drug sales in Maputo city, causes and consequences for publis health] [accessed May 9 2020]. Available at:https://www.medicusmundimozambique.org/files/2018/02/Venta_Med_Maputo.pdf .
- 53.Zahreddine L, Hallit S, Shakaroun S, Al-Hajje A, Awada S, Lahoud N. Knowledge of pharmacists and parents towards antibiotic use in pediatrics:a cross-sectional study in Lebanon. Pharm Pract (Granada) 2018;16(3):1194. doi: 10.18549/pharmpract.2018.03.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sapkota AR, Coker ME, Rosenberg Goldstein RE, Atkinson NL, Sweet SJ, Sopeju PO, Ojo MT, Otivhia E, Ayepola OO, Olajuyigbe OO, Shireman L, Pottinger PS, Ojo KK. Self-medication with antibiotics for the treatment of menstrual symptoms in Southwest Nigeria:a cross-sectional study. BMC Public Health. 2010;10:610. doi: 10.1186/1471-2458-10-610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Widayati A, Suryawati S, de Crespigny C, Hiller JE. Self medication with antibiotics in Yogyakarta City Indonesia:a cross sectional population-based survey. BMC Res Notes. 2011;4:491. doi: 10.1186/1756-0500-4-491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kalungia AC, Burger J, Godman B, Costa JO, Simuwelu C. Non-prescription sale and dispensing of antibiotics in community pharmacies in Zambia. Expert Rev Anti Infect Ther. 2016;14(12):1215–1223. doi: 10.1080/147∑0.2016.1227702. [DOI] [PubMed] [Google Scholar]
- 57.Ministerio Da Saúde. [Cirriculum of Pharmacy Technicians] Moçambique: MdS; 2007. [Google Scholar]
- 58.Clarke V, Braun V. Teaching thematic analysis:Overcoming challenges and developing strategies for effective learning. Psychologist. 2013;26(2):120–123. [Google Scholar]
- 59.Braun V, Clarke V, Hayfield N, Terry G. Thematic Analysis. In: Liamputtong P, editor. Handbook of Research Methods in Health Social Sciences. Singapore: Springer; 2019. [Google Scholar]
- 60.Braun V, Clarke V. Thematic analysis. In: Cooper H, Camic PM, Long DL, Panter AT, Rindskopf D, Sher KJ, editors. APA handbooks in psychology. APA; Washington, DC: 2012. [Google Scholar]
- 61.Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis:Striving to meet the trustworthiness criteria. Int J Qual Methods. 2017;16(1):1609406917733847. doi: 10.1177/1609406917733847. [DOI] [Google Scholar]
- 62.Hawkey PM, Jones AM. The changing epidemiology of resistance. J Antimicrob Chemother. 2009;64(suppl 1):i3–i10. doi: 10.1093/jac/dkp256. [DOI] [PubMed] [Google Scholar]
- 63.Gebretekle GB, Serbessa MK. Exploration of over the counter sales of antibiotics in community pharmacies of Addis Ababa, Ethiopia:pharmacy professionals'perspective. Antimicrob Resist Infect Control. 2016;5:2. doi: 10.1186/s13756-016-0101-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Yakimova Y. Pharmacists'knowledge of the safety of antibiotics for systemic use. Int J Risk Saf Med. 2015;27(Suppl 1):S11–S12. doi: 10.3233/jrs-150670. [DOI] [PubMed] [Google Scholar]
- 65.Fang Y, Yang S, Zhou S, Jiang M, Liu J. Community pharmacy practice in China:past, present and future. Int J Clin Pharm. 2013;35(4):520–528. doi: 10.1007/s11096-013-9789-5. [DOI] [PubMed] [Google Scholar]
- 66.Azhar S, Hassali MA, Ibrahim MI, Ahmad M, Masood I, Shafie AA. The role of pharmacists in developing countries:the current scenario in Pakistan. Hum Resour Health. 2009;7:54. doi: 10.1186/1478-4491-7-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Parthasarathi G, Ramesh M, Nyfort-Hansen K, Nagavi BG. Clinical pharmacy in a South Indian teaching hospital. Ann Pharmacother. 2002;36(5):927–932. doi: 10.1345/aph.1a223. [DOI] [PubMed] [Google Scholar]
- 68.Basak SC, van Mil JW, Sathyanarayana D. The changing roles of pharmacists in community pharmacies:perception of reality in India. Pharm World Sci. 2009;31(6):612–618. doi: 10.1007/s11096-009-9307-y. [DOI] [PubMed] [Google Scholar]
- 69.Magedanz L, Silliprandi EM, dos Santos RP. Impact of the pharmacist on a multidisciplinary team in an antimicrobial stewardship program:a quasi-experimental study. Int J Clin Pharm. 2012;34(2):290–294. doi: 10.1007/s11096-012-9621-7. [DOI] [PubMed] [Google Scholar]
- 70.Sakeena MHF, Bennett AA, McLachlan AJ. Enhancing pharmacists'role in developing countries to overcome the challenge of antimicrobial resistance:a narrative review. Antimicrob Resist Infect Control. 2018;7:63. doi: 10.1186/s13756-018-0351-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Brink AJ, Messina AP, Feldman C, Richards GA, Becker PJ, Goff DA, Bauer KA, Nathwani D, van den Bergh D Netcare Antimicrobial Stewardship Study Alliance. Antimicrobial stewardship across 47 South African hospitals:an implementation study. Lancet Infect Dis. 2016;16(9):1017–1025. doi: 10.1016/s1473-3099(16)30012-3. [DOI] [PubMed] [Google Scholar]
- 72.Norris P, Chamberlain K, Dew K, Gabe J, Hodgetts D, Madden H. Public Beliefs about Antibiotics, Infection and Resistance:A Qualitative Study. Antibiotics (Basel) 2013;2(4):465–476. doi: 10.3390/antibiotics2040465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Napolitano F, Izzo MT, Di Giuseppe G, Angelillo IF. Public knowledge, attitudes, and experience regarding the use of antibiotics in Italy. PLoS One. 2013;8(12):e84177. doi: 10.1371/journal.pone.0084177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.PavydėE Veikutis V, Mačiulienė A, Mačiulis V, Petrikonis K, Stankevičius E. Public Knowledge, Beliefs and Behavior on Antibiotic Use and Self-Medication in Lithuania. Int J Environ Res Public Health. 2015;12(6):7002–7016. doi: 10.3390/ijerph120607002. Published 2015 Jun 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Anghel IB, Craciun C. Self-Medication with over-the-counter drugs and antibiotics in Romanian consumers:A qualitative study. Cogn Brain Behav. 2013;17(3):215–235. [Google Scholar]
- 76.Mamade S, Suleman F, Smabrekke L. Antibiotic prescription patterns for outpatients at a Central Hospital in Maputo city, Mozambique [Masters Dissertation], School of Pharmaceutical Sciences, University of KwaZulu Natral. 2019 [Google Scholar]
- 77.Yates TD, Davis ME, Taylor YJ, Davidson L, Connor CD, Buehler K, Spencer MD. Not a magic pill:a qualitative exploration of provider perspectives on antibiotic prescribing in the outpatient setting. BMC Fam Pract. 2018;19(1):96. doi: 10.1186/s12875-018-0788-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Yaacoub SG, Koyess V, Lahoud N, Rahme D, Francis N, Saleh N, Maison P. Antibiotic prescribing for acute uncomplicated cystitis in Lebanese community pharmacies using a simulated patient. Pharm Pract (Granada) 2019;17(4):1604. doi: 10.18549/pharmpract.2019.4.1604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.van der Geest S, Whyte SR. The charm of medicines:metaphors and metonyms. Med Anthropol Q. 1989;3(4):345–367. [Google Scholar]
- 80.Chalker J, Ratanawijitrasin S, Chuc NT, Petzold M, Tomson G. Effectiveness of a multi-component intervention on dispensing practices at private pharmacies in Vietnam and Thailand--a randomized controlled trial. Soc Sci Med. 2005;60(1):131–141. doi: 10.1016/j.socscimed.2004.04.019. [DOI] [PubMed] [Google Scholar]
- 81.Finch RG, Metlay JP, Davey PG, Baker LJ International Forum on Antibiotic Resistance colloquium. Educational interventions to improve antibiotic use in the community:report from the International Forum on Antibiotic Resistance (IFAR) colloquium. Lancet Infect Dis. 2002;2004;4(1):44–53. doi: 10.1016/s1473-3099(03)00860-0. [DOI] [PubMed] [Google Scholar]
- 82.Kozman D, Schuttner L, Chunda L, Tymchuk C. Educational intervention to improve antibiotic knowledge at Kamuzu Central Hospital, Malawi. Lancet Glob Health. 2018;6(special):S43. doi: 10.1016/S2214-109X(18)30172-4. [DOI] [Google Scholar]


