Abstract
Background
During the COVID-19 outbreak, healthcare professionals (HCP) are at the frontline of clinical management and at increased risk for infection. The SARS-CoV-2 seroprevalence of oncological HCP and their patients has significant implications for oncological care.
Methods
HCP and patients with cancer at the Division of Oncology, Medical University of Vienna were included between 21 March and 4 June and tested for total antibodies against SARS-CoV-2 employing the Roche Elecsys Anti-SARS-CoV-2 immunoassay. Reactive samples were confirmed or disproved by the Abbott SARS-CoV-2 IgG test. Additionally, a structured questionnaire regarding basic demographic parameters, travel history and COVID-19-associated symptoms had to be completed by HCP.
Results
146 subjects (62 HCP and 84 patients with cancer) were enrolled. In the oncological HCP cohort, 20 (32.3%) subjects were medical oncologists, 28 (45.2%) nurses at our ward and 14 (22.6%) fulfil other functions such as study coordinators. In the patient cohort, most individuals are on active anticancer treatment (96.4%). 26% of the HCP and 6% of the patients had symptoms potentially associated with COVID-19 since the end of February 2020. However, only in 2 (3.2%) HCP and in 3 (3.6%) patients, anti-SARS-Cov-2 total antibodies were detected. The second assay for anti-SARS-Cov-2 IgG antibodies confirmed the positive result in all HCP and in 2 (2.4%) patients, suggesting an initial assay’s unspecific reaction in one case. In individuals with a confirmed test result, an active COVID-19 infection was documented by a positive SARS-CoV-2 RNA PCR test.
Conclusion
Specific anti-SARS-CoV-2 antibodies were found solely in persons after a documented SARS-CoV-2 viral infection, thus supporting the test methods’ high sensitivity and specificity. The low prevalence of anti-SARS-CoV-2 antibodies in our cohorts indicates a lack of immunity against SARS-CoV-2. It highlights the need for continued strict safety measures to prevent uncontrolled viral spread among oncological HCPs and patients with cancer.
Keywords: seroprevalence, SARS-COV-2, healthcare professionals, COVID-19
Significance of this study.
What is already known about this subject?
The SARS-CoV-2 seroprevalence is low in the general population.
The antibody response rates against SARS-CoV-2 in patients with cancer receiving anticancer therapies are less pronounced.
The SARS-CoV-2 seropositivity rate in oncological healthcare workers has not been investigated so far.
What does this study add?
Although the 26% of the oncological healthcare workers reported symptoms potentially associated with COVID-19, only a minority had specific anti-SARS-Cov-2 antibodies.
The prevalence of anti-SARS-CoV-2 antibodies in oncological healthcare workers and patients with cancer is low and indicates a lack of immunity against SARS-CoV-2.
How might this impact on clinical practice?
Although the strict measures of containment are gradually rolled back worldwide, there is continued need for strict safety measures at cancer centres to prevent uncontrolled viral spread among oncological healthcare professionals and patients with cancer.
Introduction
On 12 December 2019, a patient suffering from novel pneumonia of unknown aetiology was hospitalised in Wuhan, Hubei Province, China.1 Subsequently, SARS-CoV-2 was identified as the underlying causative pathogen.1 SARS-CoV-2 infection, however, results in a heterogeneous symptom complex coined COVID-19. COVID-19 comprises dyspnoea, fever, cough, olfactory disorders and pneumonia and the fatal severe acute respiratory distress syndrome, although mild and asymptomatic courses have been described.2 3 SARS-CoV-2 rapidly spread worldwide within a few weeks, which poses a major challenge for healthcare systems. Thus, WHO declared that COVID-19 is a ‘public health emergency of international concern’.4 Until June 2020, approximately 422 000 deaths and 7 500 000 cases were announced by WHO.5
Notably, patients with malignancies might be among the most threatened patient populations since most of them are heavily immunosuppressed due to their underlying disease, their treatment or both. Thus, they are highly susceptible to severe complications if infected with SARS-CoV-2. In an early report from China, the COVID-19 mortality rate was 2% in the general population and 6% in patients with cancer.6 Additionally, a very recent study from the UK showed that 52% of the patients with cancer suffer from mild symptoms. Mortality is driven by age, gender and comorbidities rather than by tumour type or anticancer treatment.7
Likewise, healthcare professionals (HCP), who are at the frontline of the disease and confronted with a growing number of SARS-CoV-2-positive patients, are highly vulnerable to COVID-19 infection.8 Personal protective equipment (PPE) is the primary strategy to prevent disease transmission within the healthcare setting. PPE refers to several tools for protecting skin, mucous membranes, airways and clothing from infectious agents. Nevertheless, and according to a recent report, approximately 9% of the Italian HCP were infected with SARS-CoV-2.8 This is particularly critical, as it decreases the number of healthcare workers available and increases the risk of infection in other healthcare workers and patients. In Wuhan, 41% of the confirmed COVID-19 cases resulted from hospital-related transmission.6
The current gold standard confirming current SARS-CoV-2 infection is—as recommended by the Center for Disease Control—the collection of nasopharyngeal swabs followed by SARS-COV-2 RNA detection using reverse-transcription PCR (RT-PCR). However, false-negative test results have been reported early in the course of an infection.9 10
Serological tests detecting IgG and IgM antibodies against SARS-CoV-2 might be of particular use in this setting.11 They confirm positive RT-PCR test results and are easy to perform while reducing the heterogeneity compared with nasopharyngeal specimens. More importantly, a serological test could capture previous asymptomatic infections and help to assess the immune status of a subject and finally estimate herd immunity.12 Worldwide, several countries are going to ease the restriction measurements after the initial COVID-19 wave faded away. However, the SARS-CoV-2 seroprevalence is still low in the population, and herd immunity has not been developed.13
Likewise, the SARS-CoV-2 seroprevalence of oncological HCP and their patients is currently unknown but has significant implications for oncological care and policymakers. Therefore, this study aimed to perform serological testing and evaluate SARS-CoV-2 antibody levels in both oncological HSP and patients with cancer irrespective of COVID-19 symptoms in a large tertiary care hospital after implementation of institutional safety measures.
Methods
The present study is a mixed retrospective/prospective cohort study with the enrolment date used to collect retrospective data and start the prospective seroprevalence branch in HCP.
Healthcare staff cohort
The study population comprises nurses, nurse technicians, attending physicians, medical oncologists, physical therapists, nurse practitioners, environmental service workers, administrative staff and dietitians working at the Division of Oncology, Medical University of Vienna, Austria, during the COVID-19 pandemic between 1 April and 4 June 2020.
HCP participating in the study were asked to sign an informed consent and fill in a structured questionnaire. It queried data regarding basic demographic parameters (age, gender and profession), working environment, travel history in the last 6 weeks place of residence, known contact with a COVID-19-positive person, the environment of contact with a COVID-19-positive person, the necessity of quarantine, duration of quarantine, positive SARS-CoV-2 test in the past, the necessity of inpatient treatment, experienced symptoms and about their general experience of COVID-19 pandemic.
Patient cohort
We retrospectively collected baseline, clinical and treatment data of all patients, who consented to participate in our biobanking programme and were both routinely tested for SARS-CoV-2 and for whom archival serum was available in our biobank facility between 21 March and 4 June 2020 at the Division of Oncology, Medical University of Vienna, Vienna, Austria by chart review.
From 21 March 2020, nasal or pharyngeal respiratory swabs were routinely taken of each patient presenting at our department, unless a negative SARS-Cov-2 test result within the past 2 weeks was on file. In case of symptoms indicating a respiratory infection and before medical interventions with a high risk of transmission, the SARS-CoV-2 test was repeated in a shorter interval.
Seroprevalence and SARS-CoV-2 testing
All tests were performed at the Department of Laboratory Medicine, Medical University of Vienna, Vienna, Austria. Blood samples were processed and stored by the Medical University of Vienna Biobank facility according to standard operating procedures in an ISO 9001:2015 certified environment, as published previously.14
Total antibodies (including IgG, IgM and IgA) against SARS-CoV-2 were detected using the Roche Elecsys Anti-SARS-CoV-2 immunoassay (Roche Diagnostics, Rotkreuz, Switzerland) on a Cobas e801 analyzer (specificity >99%). In this electrochemiluminescence test, circulating SARS-CoV-2-specific antibodies are sandwiched between biotinylated and ruthenylated recombinant nucleocapsid (N) antigens from SARS-CoV-2. The biotinylated antigen attaches the immunocomplex to streptavidin-coated microparticles, which are subsequently magnetically captured. Any unbound antigens are removed. Applying a voltage induces electrochemiluminescence in the ruthenium particle attached to the second antigen. The emitted light, whose intensity corresponds to the amount of captured antibodies, is detected by a photomultiplier. A cut-off index >1 is regarded as positive.
In the case of positivity, a second test for IgG antibodies was performed to confirm the results. IgG antibodies against SARS-CoV-2 were detected through chemiluminescent microparticle immunoassay technology using the Abbott SARS-CoV-2 IgG test on the Abbott ARCHITECT i2000sr platform (Abbott Laboratories, Illinois, USA). In this immunoassay, IgG antibodies to SARS-CoV-2 present in the sample bind to antigen-coated microparticles. Applying IgG acridinium labelled conjugate a chemiluminescent reaction is measured as a relative light unit (RLU). The RLUs detected by the system optics have a direct relationship to the amount of IgG antibodies in the sample. Using a calibrator, the samples RLU values are reflected in the calculated index (S/C). An index (S/C) >1.4 is regarded as positive.
Testing for the presence of SARS-CoV-2 RNA in respiratory specimens was done RT-PCR. RT-PCR analysis was either performed using a CE/IVD validated workflow (Cobas SARS-CoV-2 assay on the Roche Cobas 6800 platform; Abbott RealTime SARS-CoV-2 assay on the Abbott m2000 platform) or using a validated RT-PCR workflow according to Corman et al.15
Statistical analysis
Statistical analysis was performed using the SPSS V.26 software package (SPSS, Chicago, Illinois, USA). Continuous variables were presented as median and range. Categorical variables were summarised using percentages and counts. The 95% two-sided CIs of the seroprevalence were calculated from binomial probabilities using Clopper-Pears methods. For comparisons of seroprevalence status between HCP and patients, cross-tabulation and χ2 (at a two-sided significance level of 0.05) analysis was performed.
Results
Healthcare staff cohort
Sixty-two subjects were enrolled. The baseline characteristics of the HCP study population are depicted in table 1. The median age was 41 (23–59) years, and most of the participants were female (44; 71%). While only a minority of the participants were active smokers (5; 8.1%), 77% of the subjects were non-Viennese residents and, therefore, commuters (either by public transport or by car). Twenty-nine (46.8%) subjects self-reported a travel history abroad during the last 6 months. Twenty (32.3%) subjects were medical oncologists, 28 (45.2%) nurses and 14 (22.6%) fulfil other functions such as study coordinators; 62.9% (n=39) work at our day clinic or the inpatient ward and are in prolonged and close contact with patients with cancer.
Table 1.
HCP characteristics
| Characteristics | Number of subjects (%) |
| Sex | |
| Male | 18 (29%) |
| Female | 44 (71%) |
| Smoking status | |
| Never smoker | 46 (74.2%) |
| Smoker | 5 (8.1%) |
| Former smoker | 11 (17.7%) |
| Median age (range), years | 41 (23–59) |
| Profession | |
| Medical oncologists | 20 (32.2%) |
| Nurses | 28 (45.2%) |
| Other | 14 (22.6%) |
| Work environment | |
| Day unit/inpatient ward | 39 (62.9%) |
| Outpatient clinic | 16 (25.8%) |
| Other | 7 (11.3%) |
| Residence in Vienna | |
| No | 47 (77.0%) |
| Yes | 28 (23.0%) |
| Not evaluable | 1 |
| Single person household | |
| No | 42 (67.7%) |
| Yes | 20 (32.3%) |
HCP, healthcare professional.
As for risk factors for COVID-19 infections, HCP reported living together with family members in 42 (67.7%) of the cases (table 2). A family member’s quarantine due to a potential COVID-19 infection was issued for five (8.2%) members of the HCP. Interestingly, 26% of the HCPs had symptoms potentially associated with a COVID-19 infection such as fever or cough since the end of February 2020, and seven were in contact with a patient who had a confirmed COVID-19 infection. Likewise, seven subjects (11.3%) had to undergo home quarantine. Routine nasal or pharyngeal respiratory swabs for COVID-19 screening were taken in 46 (75.4%) HCPs (table 2).
Table 2.
COVID-19-associated risk factors in HCP
| Characteristics | Number of patients (%) |
| Sex | |
| Male | 43 (51.2%) |
| Female | 41 (48.8%) |
| Cancer type | |
| Lung cancer | 29 (34.5%) |
| Head and neck cancer | 9 (10.7%) |
| Renal cell cancer | 1 (1.2%) |
| Bladder cancer | 1 (1.2%) |
| Breast cancer | 10 (11.9%) |
| Mesothelioma | 1 (1.2%) |
| Colorectal cancer | 3 (3.6%) |
| Pancreatic cancer | 7 (8.3%) |
| Oesophageal cancer | 2 (2.4%) |
| Gastric cancer | 2 (2.4%) |
| Glioblastoma | 2 (2.4%) |
| Cancer of unknown primary | 6 (7.1%) |
| Cholangiocellular carcinoma | 1 (1.2%) |
| Hepatocellular carcinoma | 2 (2.4%) |
| Sarcoma | 6 (7.1%) |
| Glioma low grade | 1 (1.2%) |
| Neuroendocrine carcinoma | 1 (1.2%) |
| Median age (range), years | 61 (18–86) |
| Type of cancer therapy | |
| No anticancer therapy | 3 (3.6%) |
| Immunotherapy | 23 (27.4%) |
| Chemotherapy | 27 (31.1%) |
| Targeted therapy | 1 (1.2%) |
| Chemotherapy plus targeted therapy | 11 (13.1%) |
| Immunotherapy plus targeted therapy | 3 (3.6%) |
| Immunotherapy plus chemotherapy | 16 (19%) |
| Palliative setting | |
| No | 10 (11.9%) |
| Yes | 74 (88.1%) |
| Outpatient treatment | |
| No | 47 (77.0%) |
| Yes | 28 (23.0%) |
HCP, healthcare professional.
However, only in two (3.2%; 95% CI 0.4% to 11.2%) individuals, serum anti-SARS-Cov-2 antibodies were detected (figure 1A). Quantitative serological raw data of all subjects tested are shown in figure 2. A second antibody assay was subsequently performed as described above and confirmed positivity in both individuals, showing an index (S/C) of 3.92 and 5.65. For these subjects, an active COVID-19 infection was documented by a positive SARS-CoV-2 RNA PCR test as well. No anti-SARS-Cov-2 antibodies could be detected in any asymptomatic HCPs.
Figure 1.
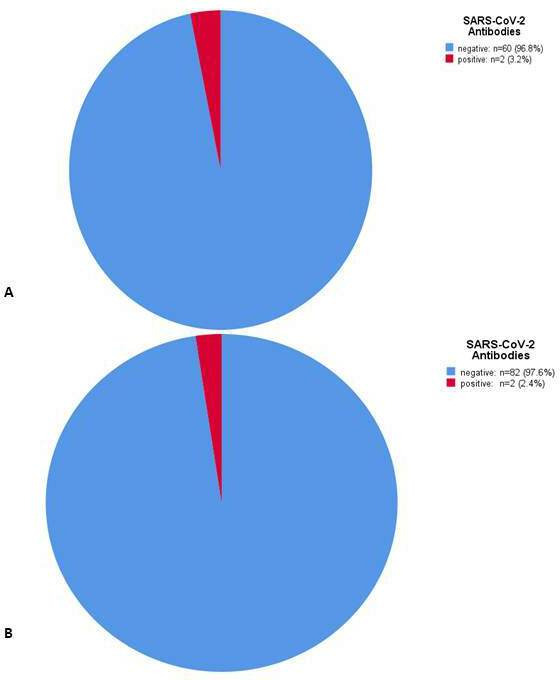
Number of confirmed seropositive healthcare professional (HCP) (A) and number of seropositive patients (B).
Figure 2.
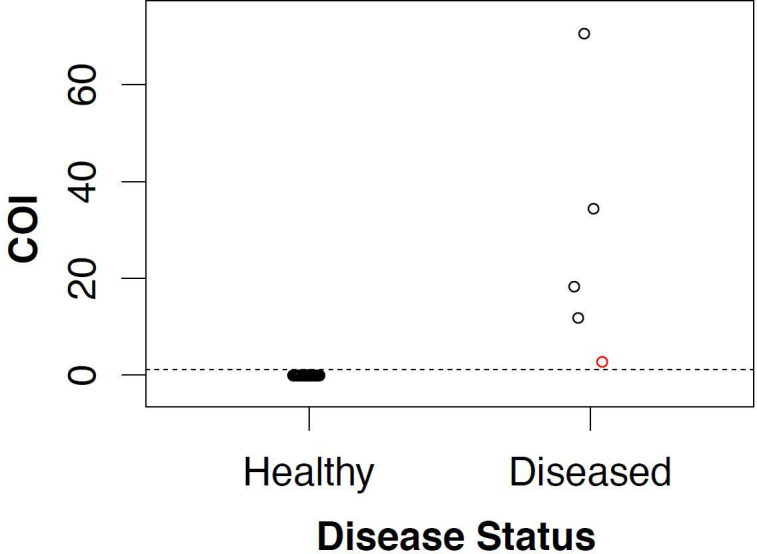
Cut-off index (COI) of seronegative and healthy individuals (left) and of seropositive individuals (right). The red circle indicates the COI of the false positive patient.
Patient cohort
A total of 43 male and 41 female patients (median age 61 years) with active cancer undergoing treatment at our Department were included in this analysis. The most common primary tumour sites included lung cancer (29; 34.5%), breast cancer (10; 11.9%), head and neck cancer (9; 10.7%), pancreatic cancer (7; 8.3%), sarcoma (6; 7.1%) and cancer of unknown primary (6; 7.1%). The majority of patients received either chemotherapy (27; 31.1%), immunotherapy (23; 27.4%), a combination of both (16; 19%) or chemotherapy plus targeted therapy (11; 13.1%). Systemic therapy was mainly given in a palliative intent in 74 (88.1%) patients (table 3).
Table 3.
Patient characteristics
| Characteristics | Number of patients (%) |
| SARS-COV-2 test performed | |
| No | 0 |
| Yes | 84 (100%) |
| SARS-COV-2 test result | |
| Positive | 2 (2.4%) |
| Negative | 82 (97.6%) |
| Median number of SARS-COV-2 tests | 2 (range 1–5) |
| COVID-19-associated symptoms | |
| No | 79 (94.0%) |
| Yes | 5 (6.0%) |
During the observation period, a minority of the patients (6; 6.0%) reported COVID-19-associated symptoms (table 4). In all 84 patients, at least one nasal or pharyngeal respiratory swab for COVID-19 screening was performed (median 2; range 1–5). Two (2.4%) patients were tested positive for COVID-19 infection, and 82 (97.6%) patients were negative.
Table 4.
COVID-19 tests and associated risk factors in patients with cancer
| Characteristics | Number of patients (%) |
| SARS-COV-2 test performed | |
| No | 0 |
| Yes | 84 (100%) |
| SARS-COV-2 test result | |
| Positive | 2 (2.4%) |
| Negative | 82 (97.6%) |
| Median number of SARS-COV-2 tests | 2 (range 1–5) |
| COVID-19-associated symptoms | |
| No | 79 (94.0%) |
| Yes | 5 (6.0%) |
Initially, serum anti-SARS-Cov-2 antibodies were at first detected in three (3.6%) patients. Interestingly, in one patient, the second assay did not confirm the positive result, suggesting an initial assay’s unspecific reaction. Therefore, only two (2.4%; 95% CI 0.3% to 8.3%) patients could be considered seropositive for anti-SARS-Cov-2 antibodies (figure 1B).
A not statistically significant association was found between seroprevalence in HCP and in patients with cancer treated as determined by the χ2 test (p=0.75).
Discussion
The number of patients hospitalised with COVID-19 and the SARS-CoV-2 infection rates, in general, are currently at a comparably low level in Austria and many countries throughout Europe. Therefore, the strict measures of containment are gradually rolled back worldwide, although the general population’s immunological state is widely unknown. In this study, we show that the SARS-CoV-2 seroprevalence in oncological HCP and patients with cancer is still low, and anti-SARS-CoV-2 antibodies were detected solely in persons after a documented SARS-CoV-2 viral infection. These findings support the policy of continuous and strict safety measures for critical infrastructure such as hospitals despite declining COVID-19 cases to prevent uncontrolled viral spread among oncological HCPs and patients with cancer.
A recent Chinese study showed that in Wuhan, which was the epicentre of the COVID-19 pandemic, the seropositivity rates varied between 3.2% and 3.8%,16 especially HCP and patients undergoing haemodialysis, with more regular hospital visits, had a higher seropositivity rate.16 Interestingly, with an increasing geographical distance from the epicentre, the seroprevalence was lower, and only 2.5% of the HCP developed SARS-CoV-2 IgG or IgM antibodies.16 Of note, only 19 of 23 patients, who had a positive SARS-CoV-2 RT-PCR test, developed SARS-CoV-2 IgG antibodies. Similarly, a population-based Swiss study conducted in 5000 individuals in Geneva, estimated the seroprevalence in the general population between 4.8% and 10.8% depending on the age group.13 Finally, a study performed in the USA reported a 4.65% seroprevalence in Los Angeles county.17 Despite the limited sample size of our study population, the results of the above are consistent with our findings: the SARS-CoV-2 seroprevalence was 3.2% (95% CI 0.4% to 11.2%) in HCP, which represented a younger population with a median age of 41 years and 2.4% (95% CI 0.3% to 8.3%) in the older patient population.
However, in contrast to the Chinese study, we did not find a discrepancy between seropositivity and a positive SARS-CoV-2 RT-PCR test, since both healthcare workers and patients were diagnosed with COVID-19 infection by RT-PCR and developed consistently anti-SARS-CoV-2 IgG. This observation has to be interpreted with caution since it is well known that seroconversion after symptom onset occurs within several days, and the sensitivity of serological assays is below 30% within the first week of a COVID-19 infection.18 Apart from that, it has to be noted that multiple serological assays for antibody detection have been developed and employed in different studies. This fact impairs the comparability of the different studies.12 18 In our analysis, we selected a validated and Emergency Use Authorisation Food and Drug Administration-approved total antibody electrochemiluminescence assay and confirmed positive results with an IgG-specific chemiluminescent microparticle immunoassay to rule out false-positive results.
It seems evident that the role of serological assays is rather the identification of previous COVID-19 infections, since asymptomatic COVID-19 courses are well documented than the initial diagnosis. A study evaluating the SARS-CoV-2 seroconversion among passengers quarantined after disembarking a cruise ship reported that six out of nine patients with either positive serology or SARS-CoV-2 RT-PCR test remained asymptomatic.19 While the incidence of asymptomatic cases reported in different studies varies widely between 1.6% and >50% dependent on the general testing rates and the methodology employed, there is consensus that asymptomatic patients can spread the disease.20 Additionally, it was demonstrated that asymptomatic individuals exhibited a weaker immune response and had lower levels of neutralising IgG antibodies.21 Moreover, 40% of these patients became seronegative for IgG, while 12.9% of the symptomatic group became negative for IgG in the early convalescent phase.21
Surprisingly, no asymptomatic seropositive HCP was detected in our analysis.
On the contrary, although 26% of the HCP reported symptoms potentially associated with COVID-19, only a minority was seropositive and COVID-19 positive, as stated above. Furthermore, seven HCP were exposed to a patient who had a confirmed COVID-19 infection, which has been associated with a higher seroprevalence.22
As reported very recently, the prevalence of COVID-19 infections in patients with cancer treated at our Department was 0.4% (4/1016). At the time of testing, all four SARS-CoV-2-positive patients were asymptomatic.23 Two of those patients were included in our analysis for seroprevalence as well. Since it has been shown previously that the antibody response rates in patients with cancer receiving anti-cancer therapies are less pronounced, it might be reasonable to think that asymptomatic patients with cancer do not develop detectable antibody responses and remain seronegative, which was not the case in our analysis.24
Of note, the COVID-19 prevalence in patients without cancer, who presented at our hospital with potential COVID-19-related symptoms was 6.7%.23 The odds to be infected with SARS-CoV-2 as a patient without cancer was about 18 times higher than in the cancer cohort.23 Although the reason of this finding is unclear, it is tempting to speculate and supported by the low SARS-CoV-2 seroprevalence rates we detected in this analysis that patients with cancer and their caregivers make greater efforts to protect themselves from COVID-19 compared with the general public.
The COVID-19 outbreak had a major impact on treatment patterns and cancer care in general. Multiple recommendations on this topic have been published so far.25–27 The majority of those guidelines/surveys advocate for treatment modifications such as extending the cycles of immunotherapy administrations, simplification of radiotherapy duration or implementing telemedicine procedures.27–30 However, the importance of regular testing of both oncological HCP and patients with cancer is rarely stressed.
In addition to the measures mentioned above, HCP and patients with cancer undergo biweekly COVID-19 screening by RT-PCR at our Department irrespective of symptoms.
The low prevalence of anti-SARS-CoV-2 antibodies in our cohorts indicates a lack of immunity against SARS-CoV-2. It highlights the need for continued strict safety measures to prevent uncontrolled viral spread among oncological HCPs and patients with cancer.
Acknowledgments
The authors are grateful for the administrative support of Ms Cornelia Lhotak.
Footnotes
Contributors: TF, ASB, HH, LS, MP and ST designed the research. TP and RS performed laboratory tests, TF, ASB, HH, MP and ST analysed the data. TF, ASB and ST wrote the main manuscript and all authors reviewed and commented on the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: TF has received honoraria for lectures, consultation or advisory board participation from the following for-profit companies: Bristol-Myers Squibb, Novartis, Roche, Sanofi, Merck Sharp & Dome, Merck Darmstadt, Amgen, Böhringer-Ingelheim, Accord, AstraZeneca. The following for-profit companies have supported clinical trials and contracted research conducted by TF with payments made to his institution: Bristol-Myers Squibb, Merck Sharp & Dome, Roche, Merck Darmstadt. ASB has research support from Daiichi Sankyo (≤€10 000), Roche (>€10 000) and honoraria for lectures, consultation or advisory board participation from Roche, Bristol-Meyers Squibb, Merck, Daiichi Sankyo (all <€5000) as well as travel support from Roche, Amgen and AbbVie. ASB has research support from Daiichi Sankyo (≤€10 000), Roche (>€10 000) and honoraria for lectures, consultation or advisory board participation from Roche, Bristol-Meyers Squibb, Merck, Daiichi Sankyo (all <€5000) as well as travel support from Roche, Amgen and AbbVie. MP has received honoraria for lectures, consultation or advisory board participation from the following for-profit companies: Bayer, Bristol-Myers Squibb, Novartis, Gerson Lehrman Group (GLG), CMC Contrast, GlaxoSmithKline, Mundipharma, Roche, BMJ Journals, MedMedia, AstraZeneca, AbbVie, Lilly, Medahead, Daiichi Sankyo, Sanofi, Merck Sharp & Dome, Tocagen. The following for-profit companies have supported clinical trials and contracted research conducted by MP with payments made to his institution: Böhringer-Ingelheim, Bristol-Myers Squibb, Roche, Daiichi Sankyo, Merck Sharp & Dome, Novocure, GlaxoSmithKline, AbbVie. GH, TP, RS, JB, HCP, JK, FM, LS, AMS, AS, SW and ST have nothing to disclose.
Patient consent for publication: Not required.
Ethics approval: The study was performed in accordance with the Declaration of Helsinki and good clinical practice guidelines and was approved by the local ethics committee (#1296/2020 and #1394/2020).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available on reasonable request; 0000-0002-8241-8317 thorsten.fuereder@meduniwien.ac.at.
References
- 1.Wu F, Zhao S, Yu B, et al. A new coronavirus associated with human respiratory disease in China. Nature 2020;579:265–9. 10.1038/s41586-020-2008-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gosain R, Abdou Y, Singh A, et al. COVID-19 and cancer: a comprehensive review. Curr Oncol Rep 2020;22:53. 10.1007/s11912-020-00934-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guan W-J, Ni Z-Y, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382:1708–20. 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wu D, Wu T, Liu Q, et al. The SARS-CoV-2 outbreak: what we know. Int J Infect Dis 2020;94:44–8. 10.1016/j.ijid.2020.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO WHO coronavirus disease (COVID-19) Dashboard, 2020. Available: https://covid19.who.int/
- 6.Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA 2020. [DOI] [PubMed] [Google Scholar]
- 7.LYW L, Cazier JB, Starkey T, et al. COVID-19 mortality in patients with cancer on chemotherapy or other anticancer treatments: a prospective cohort study. The Lancet 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anelli F, Leoni G, Monaco R, et al. Italian doctors call for protecting healthcare workers and boosting community surveillance during covid-19 outbreak. BMJ 2020;368:m1254. 10.1136/bmj.m1254 [DOI] [PubMed] [Google Scholar]
- 9.Kucirka LM, Lauer SA, Laeyendecker O, et al. Variation in false-negative rate of reverse transcriptase polymerase chain reaction-based SARS-CoV-2 tests by time since exposure. Ann Intern Med 2020;173:262–7. 10.7326/M20-1495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Loeffelholz MJ, Tang Y-W. Laboratory diagnosis of emerging human coronavirus infections - the state of the art. Emerg Microbes Infect 2020;9:747–56. 10.1080/22221751.2020.1745095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guo L, Ren L, Yang S, et al. Profiling early humoral response to diagnose novel coronavirus disease (COVID-19). Clin Infect Dis 2020;71:778–85. 10.1093/cid/ciaa310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kontou PI, Braliou GG, Dimou NL, et al. Antibody tests in detecting SARS-CoV-2 infection: a meta-analysis. Diagnostics 2020;10:319. 10.3390/diagnostics10050319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stringhini S, Wisniak A, Piumatti G, et al. Seroprevalence of anti-SARS-CoV-2 IgG antibodies in Geneva, Switzerland (SEROCoV-POP): a population-based study. Lancet 2020;396:313–9. 10.1016/S0140-6736(20)31304-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haslacher H, Gerner M, Hofer P, et al. Usage data and scientific impact of the prospectively established fluid BioResources at the hospital-based MedUni Wien Biobank. Biopreserv Biobank 2018;16:477–82. 10.1089/bio.2018.0032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Corman VM, Landt O, Kaiser M, et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Eurosurveillance 2020;25 10.2807/1560-7917.ES.2020.25.3.2000045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xu X, Sun J, Nie S, et al. Seroprevalence of immunoglobulin M and G antibodies against SARS-CoV-2 in China. Nat Med 2020. [DOI] [PubMed] [Google Scholar]
- 17.Sood N, Simon P, Ebner P, et al. Seroprevalence of SARS-CoV-2-Specific antibodies among adults in Los Angeles County, California, on April 10-11, 2020. JAMA 2020;323:2425–7. 10.1001/jama.2020.8279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deeks JJ, Dinnes J, Takwoingi Y, et al. Antibody tests for identification of current and past infection with SARS-CoV-2. Cochrane Database Syst Rev 2020;6:Cd013652. 10.1002/14651858.CD013652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hung IF-N, Cheng VC-C, Li X, et al. SARS-CoV-2 shedding and seroconversion among passengers quarantined after disembarking a cruise SHIP: a case series. Lancet Infect Dis 2020. 10.1016/S1473-3099(20)30364-9. [Epub ahead of print: 12 Jun 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gao Z, Xu Y, Sun C, et al. A systematic review of asymptomatic infections with COVID-19. J Microbiol Immunol Infect 2020. 10.1016/j.jmii.2020.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Long Q-X, Tang X-J, Shi Q-L, et al. Clinical and immunological assessment of asymptomatic SARS-CoV-2 infections. Nat Med 2020;26:1200–4. 10.1038/s41591-020-0965-6 [DOI] [PubMed] [Google Scholar]
- 22.Chen Y, Tong X, Wang J, et al. High SARS-CoV-2 antibody prevalence among healthcare workers exposed to COVID-19 patients. J Infect 2020;81:420–6. 10.1016/j.jinf.2020.05.067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Berghoff AS. SARS-CoV-2 testing in 1016 consecutive cancer patients treated at a tertiary care hospital during the COVID-19 pandemic. J Clin Oncol 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Solodky ML, Galvez C, Russias B, et al. Lower detection rates of SARS-COV2 antibodies in cancer patients versus health care workers after symptomatic COVID-19. Annals of oncology : official journal of the European Society for Medical Oncology / ESMO 2020. (published Online First: 2020/05/04). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ueda M, Martins R, Hendrie PC, et al. Managing cancer care during the COVID-19 pandemic: Agility and collaboration toward a common goal. Journal of the National Comprehensive Cancer Network 2020;18:366–9. 10.6004/jnccn.2020.7560 [DOI] [PubMed] [Google Scholar]
- 26.Poggio F, Tagliamento M, Di Maio M, et al. Assessing the impact of the COVID-19 outbreak on the attitudes and practice of Italian oncologists toward breast cancer care and related research activities. JCO Oncology Practice 2020:Op2000297:OP.20.00297 (published Online First: 2020/06/24). 10.1200/OP.20.00297 [DOI] [PubMed] [Google Scholar]
- 27.Lambertini M, Toss A, Passaro A, et al. Cancer care during the spread of coronavirus disease 2019 (COVID-19) in Italy: young oncologists’ perspective. ESMO Open 2020;5:e000759 10.1136/esmoopen-2020-000759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Aeppli S, Eboulet EI, Eisen T, et al. Impact of COVID-19 pandemic on treatment patterns in metastatic clear cell renal cell carcinoma. ESMO Open 2020;5:e000852 10.1136/esmoopen-2020-000852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Meattini I, Franco P, Belgioia L, et al. Radiation therapy during the coronavirus disease 2019 (covid-19) pandemic in Italy: a view of the nation’s young oncologists. ESMO open 2020;5(2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tagliamento M, Spagnolo F, Poggio F, et al. Italian survey on managing immune checkpoint inhibitors in oncology during COVID‐19 outbreak. Eur J Clin Invest 2020;12:e13315 10.1111/eci.13315 [DOI] [PMC free article] [PubMed] [Google Scholar]


