Abstract
Background:
NRG1 gene fusions are rare but potentially actionable oncogenic drivers present in some solid tumors. Details regarding the incidence of these gene rearrangements are lacking. Here, we assessed the incidence of NRG1 fusions across multiple tumor types and described fusion partners.
Methods:
Tumor specimens submitted for molecular profiling at a CLIA-certified genomics laboratory and that underwent fusion testing by anchored multiplex PCR for targeted RNA sequencing were retrospectively identified. The overall and tumor-specific incidence was noted as was the specific fusion partner.
Results:
Out of 21,858 tumor specimens profiled from September 2015 to December 2018, 41 cases (0.2%) harbored an NRG1 fusion. Multiple fusion partners were identified. Fusion events were seen across tumor types. The greatest incidence was in non-small cell lung cancer (25), though this represented only 0.3% of non-small cell lung cancer cases tested. Other tumor types harboring an NRG1 fusion included gallbladder cancer, renal cell carcinoma, bladder cancer, ovarian cancer, pancreatic cancer, breast cancer, neuroendocrine tumor, sarcoma, and colorectal cancer.
Conclusion:
NRG1 fusions can be detected at a low incidence across multiple tumor types with significant heterogeneity in fusion partner.
Keywords: NRG1, Neuregulin-1, gene fusions, NSCLC, RNA-sequencing
Introduction:
Appropriate management of advanced non-small cell lung cancer (NSCLC) is guided by the presence or absence of specific molecular drivers. The identification of activating genomic alterations in EGFR, ALK, ROS1 or BRAF not only provides insight into the underlying biology but also directs initial and subsequent therapeutic decisions (1–5). It is now standard of care to search for these mutations and fusions in all patients with non-squamous NSCLC (6). It has also become clear that some molecular drivers will serve as therapeutic targets across multiple tumor types (7), including the tumor agnostic approval of larotrectinib for tumors with a gene fusion in NTRK1, NTRK2, or NTRK3 (8). As our understanding of cancer grows increasingly sophisticated, additional drivers have surfaced that may have a similar impact on evolving treatment paradigms.
Neuregulin-1 (NRG1) gene fusions are an emerging, potentially actionable oncogenic driver (9). NRG1 fusions can promote pathologic signaling via MAPK and other canonical pathways (10). When NRG1 fusions are present, targeting ERBB2 and ERBB3 has been an effective treatment strategy in vitro. Recently, clinical responses to tyrosine kinase inhibitors and monoclonal antibodies have also been reported (9,11–13).
The interest in evaluating the prevalence of NRG1 fusions has increased given the potential therapeutic implications of this genetic alteration. Since the original description of the CD74-NRG1 gene fusion in invasive mucinous lung adenocarcinoma, detection has been noted in other tumor types, both de novo and as a resistance mechanism in ALK rearranged NSCLC (9,14–16). Here, we report the incidence and characteristics of NRG1 fusions across a variety of tumor types based on a large molecular profiling experience.
Methods:
Patient Cohort
An institutional review board (IRB)-approved, retrospective assessment of a de-identified molecular profiling database was surveyed for solid tumors that underwent fusion testing. From a cohort including all cases submitted to a CLIA-certified laboratory (Caris Life Sciences, Phoenix, AZ) for comprehensive genomic profiling from September 2015 to December 2018, all unique cases that underwent successful fusion testing for targeted RNA sequencing were identified. Additionally, all histologic characteristics were reviewed by a board-certified pathologist (Z.G.).
Gene Fusion Detection
Prior to any molecular analysis, H&E-stained sections of formalin-fixed paraffin-embedded (FFPE) tumor tissue were manually assessed by board-certified pathologists for tumor cell populations and harvested using manual microdissection to enrich the sample to at least 20% tumor nuclei. Anchored multiplex PCR was performed for targeted RNA sequencing using the ArcherDx fusion assay (Archer FusionPlex Solid Tumor panel). RNA sequencing was performed on mRNA that was isolated and reverse transcribed into complementary DNA from FFPE tumor tissues. Unidirectional gene-specific primers were used to enrich for target regions, followed by Next-Generation sequencing (Illumina MiSeq platform). Targets included 52 genes, and the full list can be found at http://archerdx.com/fusionplex assays/solid-tumor (accessed 12/27/18). Reads that were matched to a database of known fusions and other oncogenic isoforms (Quiver database, ArcherDx), as well as those novel isoforms or fusions with high reads (>10% of total reads) and high confidence after bioinformatic filtering, were analyzed. Samples with less than 4,000 unique RNA reads were reported as indeterminate and excluded from analysis. All NRG1 transcript variants were investigated whereby splice junctions were analyzed using the UCSC genome browser to predict the likelihood of the mRNA transcript to encode a functional protein (17). The detection sensitivity of the assay allows for detection of a fusion that is present in at least 10% of the cells in the samples tested.
Frame Retention Prediction
NRG1 fusions were predicted to be (1) in-frame variants, (2) out of frame variants of unknown significance or (3) translated variants where exon 2 of NRG1 is spliced to upstream non-coding exons with confirmed presence of internal initiation sites, (e.g. methionine codon) (17,18). Inclusion of these variants was based on the retention of the EGF-like domain of NRG1, the functional domain which facilitates its oncogenic potential (19).
Next Generation Sequencing
Next-Generation Sequencing (NGS) was performed on isolated genomic DNA using the Illumina NextSeq platform. A custom-designed SureSelect XT assay was used to enrich 592 whole-gene targets (Agilent Technologies, Santa Clara, CA). All variants were detected with > 99% confidence based on allele frequency and amplicon coverage, with an average sequencing depth of coverage of > 500 and an analytic sensitivity of 5%. For variant classification, variants of genes that were pre-determined for their cancer-related and clinical significance were interpreted by board-certified molecular geneticists and categorized as pathogenic, presumed pathogenic, variant of unknown significance, presumed benign, or benign according to ACMG (American College of Medical Genetics and Genomics) standards. Only pathogenic or presumed pathogenic mutations were considered deleterious and included for assessment of co-mutation patterns with NRG1-fusion positive cases.
Immunohistochemistry (IHC)
IHC was performed using commercially available detection kits and automated staining techniques (Benchmark XT, Ventana, Tucson, AZ; and AutostainerLink 48, Dako, Carpinteria, CA). Primary antibodies tested: Her2/neu (4B5, Ventana), pan-TRK (C17F1, Cell Signaling) and ALK (D5F3, Ventana). Cutoffs for positive staining: (3) pan-TRK, ≥1+ and ≥1% of cells, (4) Her2, ≥3+ and ≥ 10% and (5) ALK, ≥3+ and ≥ 10%.
Results:
Sample population
From September 2015 to December 2018, a total of 21,858 tumor specimens from unique patients were successfully evaluated. The tumor types included NSCLC (n=9592), glioma (n=1997), colorectal cancer (n=1690), breast cancer (n=1106), bladder cancer (n=945), ovarian cancer (n=686), sarcoma (n=627), pancreatic adenocarcinoma (n=623), gallbladder cancer (n=580), other gynecological malignancies (e.g. uterine, cervical, vulvar; n=524), melanoma (n=360), prostate cancer (n=261), gastric adenocarcinoma (n=239), head and neck squamous cell carcinoma (n=236), thyroid cancer (n=219), renal cell carcinoma (n=211), neuroendocrine tumors (n=203), esophageal cancer (n=202), small cell lung cancer (n=107), extrahepatic bile duct cancer (n=98), small bowel cancer (n=98), gastrointestinal stromal tumor (n=83), hepatocellular carcinoma (n=83), thymic cancer (n=31), testicular cancer (n=25), and other malignancies (n=1032).
Incidence
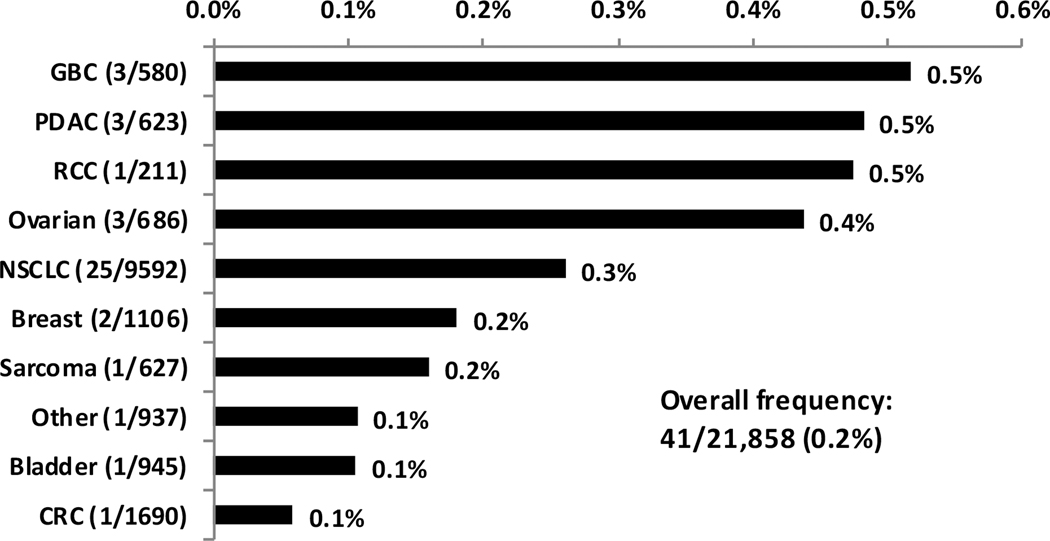
The incidence of NRG1 fusions in the entire tested population was 0.2% (41/21,858). Incidence varied by tumor type (Figure 1): 0.5% gallbladder cancer (3/580), 0.5% pancreatic cancer (3/623), 0.5% renal cell carcinoma (1/211), 0.4% ovarian cancer (3/686), 0.3% non-small cell lung cancer (25/9592), 0.2% breast cancer (2/1106), 0.2% sarcoma (1/627), 0.1% bladder cancer (1/945) and 0.1% colorectal cancer (1/1690). The remaining identified NRG1 fusion was in a patient with a neuroendocrine tumor of the nasopharynx. Table 1 describes the characteristics of the 41 patients found to have an NRG1 fusion. The most common histologic subtype was adenocarcinoma (70%), of which 24% were classified as mucinous adenocarcinoma and another 8% had a mixed histology with a mucinous component (Figure S1). The majority of cases were stage IV at the time of fusion detection. NRG1 fusion events were more frequently identified in females (66%) versus males, and most specimens were procured from the primary site (68%) compared to a distant metastasis (32%). In the total cohort, 51% (11228/21858) of patients were females and 59% (12798/21858) of specimens profiled were from primary sites.
Figure 1.
Rate of NRG1 fusions by tumor type. The tumor type with NRG1 fusion in the other category is a neuroendocrine tumor of the nasopharynx. Abbreviations: GBC, gallbladder cancer (cholangiocarcinoma); PDAC, pancreatic ductal adenocarcinoma; RCC, renal cell carcinoma; NSCLC, non-small cell lung cancer; CRC, colorectal cancer.
Table 1.
Patient and Tumor Characteristics for NRG1 Fusion Positive Cases.
| NSCLC | Ovarian Cancer | Breast Cancer | GI Cancersa | GU Cancersb | Otherc | Overall | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total, n | 25 | 3 | 2 | 7 | 2 | 2 | 41 | |||||||
| Median Age, range | 71 | 52–90 | 53 | 47–69 | 44 | 38–49 | 46 | 37–68 | 61 | 58–63 | 59 | 36–81 | 68 | 36–90 |
| Sex, n, % | ||||||||||||||
| Male | 8 | 32% | - | - | - | - | 3 | 43% | 1 | 50% | 2 | 100% | 14 | 34% |
| Female | 17 | 68% | 3 | 100% | 2 | 100% | 4 | 57% | 1 | 50% | - | - | 27 | 66% |
| Group Stage, time of biopsy, n, % | 22 | 3 | 2 | 7 | 2 | - | 36 | |||||||
| I | 1 | 5% | - | - | - | - | - | - | - | - | - | - | 1 | 3% |
| II | 3 | 14% | - | - | - | - | - | - | - | - | - | - | 3 | 8% |
| III | 6 | 27% | - | - | - | - | - | - | - | - | - | - | 6 | 17% |
| IV | 12 | 54% | 3 | 100% | 2 | 100% | 7 | 100% | 2 | 100% | - | - | 26 | 72% |
| Histology, n, % | ||||||||||||||
| Adenocarcinoma, | 29 | 70% | ||||||||||||
| Papillary | 1 | 4% | - | - | - | - | 1 | 14% | - | - | - | - | - | - |
| Mucinous | 6 | 24% | - | - | - | - | - | - | - | - | - | - | - | - |
| Acinar | 2 | 8% | - | - | - | - | - | - | - | - | - | - | - | - |
| Mixedd | 3 | 12% | - | - | - | - | - | - | - | - | - | - | - | - |
| Poorly differentiated | 2 | 8% | - | - | 1 | 50% | - | - | 1 | 50% | - | - | - | - |
| NOSe | 8 | 32% | - | - | 1 | 50% | 6 | 86% | - | - | - | - | - | - |
| Squamous cell carcinoma | 2 | 8% | - | - | - | - | - | - | - | - | - | - | 2 | 50% |
| Serous carcinoma | - | - | 2 | 67% | - | - | - | - | - | - | - | - | 2 | 5% |
| Otherf | 1 | 4% | 1 | 33% | - | - | - | - | 1 | 50% | 2 | 100% | 5 | 20% |
| Specimen Site, n, % | ||||||||||||||
| Primary | 20 | 80% | 3 | 100% | - | - | 3 | 43% | 1 | 50% | 1 | 50% | 28 | 68% |
| Distant Metastasis | 5 | 20% | - | - | 2 | 100% | 4 | 57% | 1 | 50% | 1 | 50% | 13 | 32% |
pancreatic ductal adenocarcinoma; gallbladder cancer (cholangiocarcinoma) and colorectal cancer; GU, genitourinary
renal cell carcinoma, urothelial bladder cancer
soft tissue sarcoma of the extremity/trunk, neuroendocrine tumor of the nasopharynx
mixed histology (two patients with acinar, clear cell and mucinous components and one patient with adenosquamous features)
NOS, not otherwise specified
Other, pleomorphic carcinoma or sarcoma, carcinosarcoma, clear cell carcinoma or neuroendocrine tumor. Abbreviations: NSCLC, non-small cell lung cancer; GI, gastrointestinal.
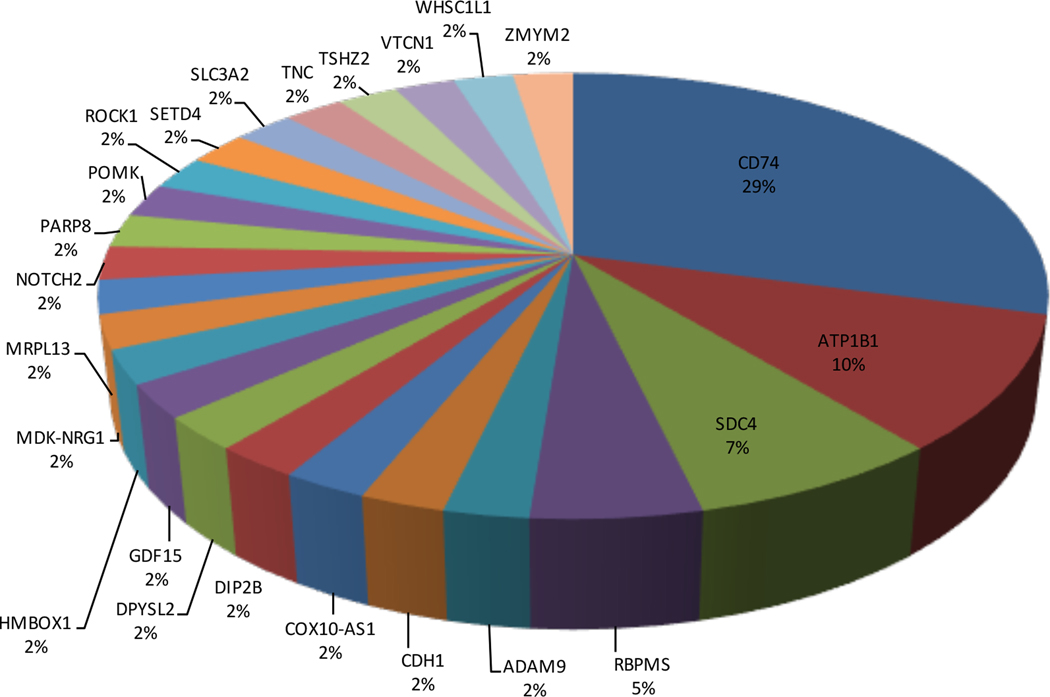
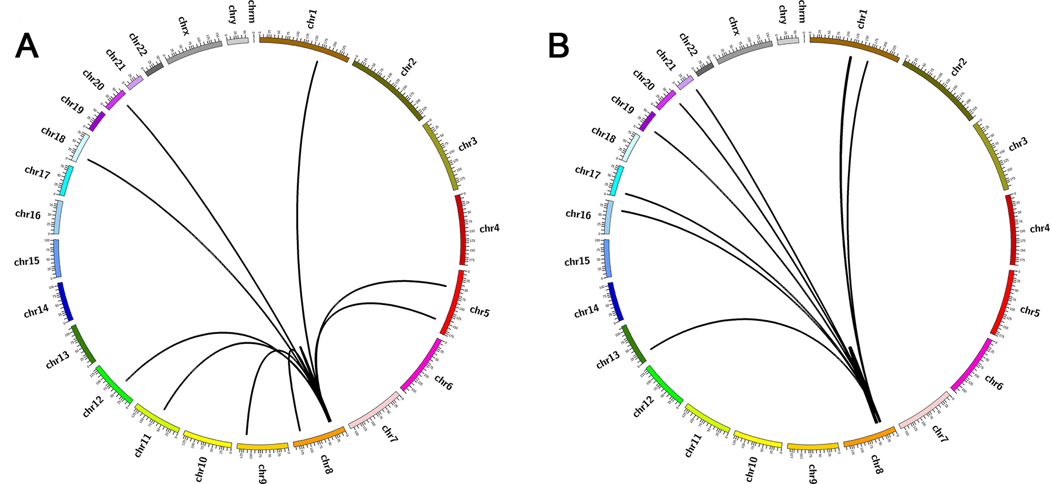
Fusion partners
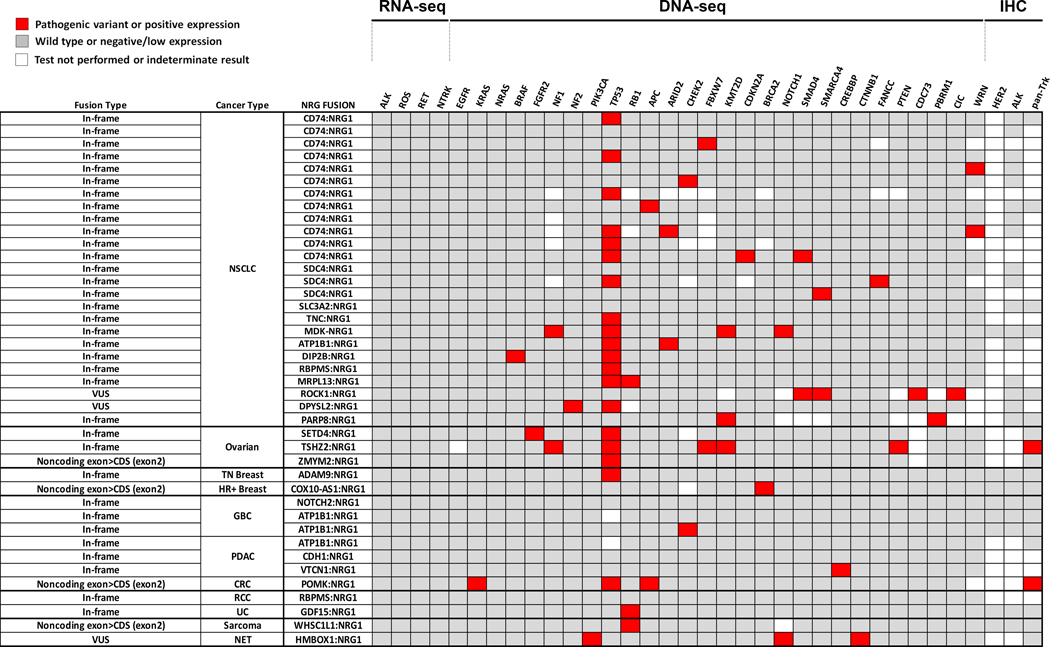
The specific fusion partners were also diverse within and across malignancies (Table S1; Figures 2–5, Figure S2). In NSCLC, CD74 was the most common fusion partner (n=12), but other detected partners in NSCLC cases included SDC4 (n=3), SLC3A2 (n=1), TNC (n=1), MDK (n=1), ATP1B1 (n=1), DIP2B (n=1), RBPMS (n=1), MRPL13 (n=1), ROCK1 (n=1), DPYSL2 (n=1), and PARP8 (n=1). In the other malignancies, the identified fusion partners were as follows: SETD4, TSHZ2 and ZMYM2 in ovarian cancer; ADAM9 and COX10-AS1 in breast cancer; ATP1B1, CDH1 and VTCN1 in pancreatic cancer; NOTCH2 and ATP1B1 (n=2) in gall bladder cancer; POMK in colorectal cancer; RBPMS in renal cell carcinoma; GDF15 in urothelial bladder cancer and WHSC1L1 in sarcoma and HMBOX1 in neuroendocrine tumor of the nasopharynx. Of the 41 NRG1 fusions identified, 34 were in-frame, 3 were out of frame variants of unknown significance, and 4 were translated variants.
Figure 2.
Genomic features observed in NRG1-fusion positive solid tumors. Oncoprint plot illustrating co-occurrence of driver events, genes with any pathogenic variant detected in the cohort and other clinically relevant protein markers. Each NRG1-fusion positive sample corresponds to one row in the table: frame prediction of the fusion, cancer type and fusion partner are provided. Fill of boxes correlate with gene/protein status: (1) red, pathogenic variant detected or positive expression, (2) grey, wild type or low/negative expression and (3) white, test was not performed, or indeterminate. Pathogenic variants in oncogenes were rare, but at least one mutation in tumor suppressor genes including TP53 occurred in all but nine samples. Abbreviations: NSCLC, non-small cell lung cancer, TN (triple-negative) breast, HR+ (hormone receptor positive) breast, GBC, gallbladder cancer (cholangiocarcinoma); PDAC, pancreatic ductal adenocarcinoma; CRC, colorectal cancer; RCC, renal cell carcinoma; UC (urothelial bladder cancer); NET (neuroendocrine tumor of the nasopharynx); VUS, fusion variant of unknown significance; CDS, coding sequence.
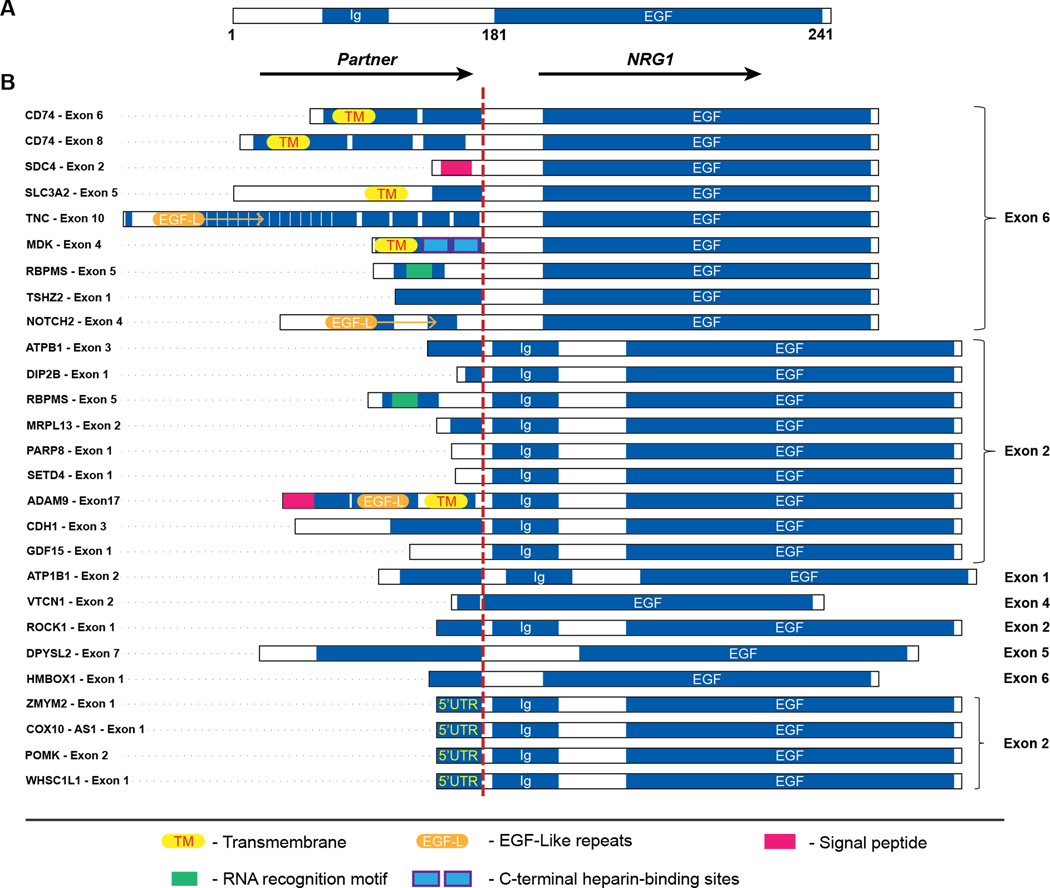
Figure 5.
Schematic diagram of NRG1 fusion variants in solid tumors. A. Genomic structure of wild type NRG1; B. Fusion variants identified with 5’ partners joined to 3’ NRG1. Bars depict the predicted functional domains (not shown to scale) of interest and red dashed line indicates fusion breakpoints. The EGF domain is preserved in all fusion variants.
Co-occurrence with other genetic aberrations
NRG1 fusions were mutually exclusive with oncogenic alterations in EGFR, KRAS, ALK, ROS1, and RET (Figure 2). One case co-occurred with a BRAF G466A mutation, one with a KRAS G12D mutation and three with NF1 or NF2 mutations (NF1,Q616fs, NSCLC and c.204+1G>T, ovarian; NF2 H242fs, NSCLC). Most cases (n=30) also demonstrated concurrent mutations in tumor suppressor genes, including TP53.
Survival
Limited survival analysis is shown in Figure S3 for patients with full annotation (n=7). Median survival for the entire cohort was 638 days and varied by tumor type, though analysis is limited by the small sample size.
Discussion:
NRG1 gene fusions represent a novel oncogenic driver across cancer types. These rare genomic events can generate proteins that retain the extracellular EGF-like domain of NRG1 and the transmembrane domain of the specific fusion partner. These proteins then serve as ligands for ERBB3 (HER3) and ERBB4 (HER4) receptors (10). ERBB3 can then be activated through juxtacrine signaling from the EGF-like domain and autocrine signaling of secreted NRG1 (19). Subsequent heterodimerization of ERBB3 with ERBB2 activates downstream signaling important in tumorigenesis mediated by pathways including ERK, PI3K, AKT and NFkB, described in cell models (9,19).
In this report, we retrospectively analyzed over 21,000 specimens after RNA sequencing using the ArcherDx platform to detect NRG1 fusions. As previously reported, our study confirmed the occurrence of NRG1 fusions in NSCLC, breast cancer, cholangiocarcinoma, ovarian cancer, and pancreatic cancer with a low overall incidence. Here, we also detected NRG1 fusions in colorectal cancer, sarcoma, and a neuroendocrine tumor of the nasopharynx, which had not been previously reported. In this report, the majority of these tumors (70%) were adenocarcinoma. NRG1 fusions in NSCLC had been described more frequently in the invasive mucinous adenocarcinoma subtype; in this series, 32% (8/25) of the NRG1+ NSCLC cases had a mucinous histology or a mucinous component (Table 1). The use of broad molecular profiling in this series was based on clinician discretion and may be influenced by patient and tumor characteristics. Thus, the actual incidence may not be entirely representative of the general population. Despite these shortcomings, the detection of such rare genetic alterations across different tumor types supports broader use of next-generation sequencing.
The specific NRG1 fusion partners are variable within and across tumor types (11–15,20). Several novel fusion partners detected in this report include TNC, MRPL13, MDK and DIP2B in NSCLC. Previous reports suggest fusion partners may influence localization of NRG1 to the plasma membrane (20), though the exact significance remains unclear, and the variety of partners observed may introduce challenges for widespread detection efforts.
Splice junctions of all candidate NRG1 fusions were analyzed to predict likelihood to encode functional proteins. Most were predicted to be in-frame; however, a recurrent novel fusion class was identified whereby exon 2 of NRG1 is spliced to upstream non-coding exons of fusion partner genes. In each of these cases (n=4; Table S1), a codon encoding for methionine is present a short distance into exon 2 of NRG1 that could potentially act as a translation initiation codon; if functional, the fusion partner could be providing the promoter for a likely N-terminal truncated version of NRG1. These observations are consistent with similar studies where NRG1 fusion variants included chimeric proteins and cases where expression of NRG1 is controlled by the promoter of the 5’ partner (21). Alternative methodologies are needed to confirm expression of the transcript s identified in this study to determine their significance.
Additional studies describing NRG1 fusions suggest these events are mutually exclusive with other known molecular drivers (14). This was consistent with the findings in this report. Specifically, all NSCLC cases were ALK, ROS, RET fusion-negative and KRAS wild type, and all pancreatic adenocarcinomas were KRAS wild type. The exception was one colorectal cancer case that also harbored a KRAS G12D mutation. The remainder of the cases studied harbored several pathogenic variants in tumor suppressor genes including TP53 and DNA damage and response genes (CHEK2, BRCA2, WRN).
NRG1 fusions are detected in a variety of tumor types. In 2014, Fernandez-Cuesta and colleagues first described the CD74-NRG1 gene fusion in five female never-smokers whose tumors lacked known activating mutations (10). As comprehensive molecular profiling and RNA sequencing has become more prevalent, NRG1 fusions have been detected in a variety of other tumor types, including breast, ovarian, and pancreatic cancer (14,15). Analysis of MSK-IMPACT dataset including next-generation sequencing and the MSK solid fusion assay identified ten patients with NRG1 fusions (out of 17,485 tested): seven in lung adenocarcinoma, two in pancreatic cancer, and one in breast cancer. Further analysis with RNA sequencing revealed additional fusions in other tumor types including ovarian cancer, uterine carcinosarcoma, renal clear cell carcinoma, prostate cancer, and head and neck cancer (9).
As NRG1 alterations activate the ERBB2/ERBB3 signaling pathway, targeted treatment with inhibitors of this pathway is an appealing therapeutic strategy. Dual targeting of ERBB2 and ERBB3 has also been evaluated in preclinical models (22,23). Afatinib, a pan-ERBB inhibitor, was successfully utilized in this manner, and several patients with tumor harboring an NRG1 fusion achieved durable benefit with afatinib (11–13). Response to an ERBB3 monoclonal antibody, GSR2849330, has also been reported (9). Combining an ERBB3 monoclonal antibody and an EGFR tyrosine kinase inhibitor was also effective in a small case series (24). Prospective studies are needed to define the role of targeted therapy for patients with tumors harboring NRG1 fusions, but these data suggest that NRG1 fusions represent a novel potential target across many tumor types that warrant further study.
Supplementary Material
Figure S1. H&E demonstrating mucinous histology. A, CD74-NRG1 lung mucinous bronchoalveolar carcinoma; B, DIP2B-NRG1 lung mucinous colloid tumor
Figure S2. Diagram showing the variety and proportion of 5’ partners by tumor type.
Figure S3. Kaplan-Meier curves for a small cohort of patients with NRG1 fusion positive solid tumors. Vertical tick marks indicate right censored data. Numbers in box indicate median survival time in days (t). Whole cohort shown in green (n = 7, deaths = 5, t = 638 days). Cohorts by lineage shown in orange (lung; n = 3, deaths = 3, t = 200), pink (soft tissue tumors; n = 1, deaths = 1, t = 733) and blue (pancreatic; n = 2, deaths = 1, t = 638). Colorectal not shown; n = 1, deaths = 0, t not reached).
Figure 3.
NRG1 fusion partners. Pie chart showing the proportion and variety of fusion partners for NRG1.
Figure 4.
Circos plot of depicting NRG1 fusion genes and partners from Table S1. NRG1 and partners in (A) NSCLC and (B) all other tumors
Significance:
NRG1 fusions are potentially actionable genomic events seen in various tumor types. While there are reports of therapeutic efficacy with agents that target Erb-B2/Erb-B3, little is known about the characteristics of these fusions. Here, we report the incidence of NRG1 fusions in a large cohort of solid tumors that underwent RNA sequencing. NRG1 fusions were detected at a low incidence across many solid tumor types. Multiple fusion partners were identified, which will influence the development of strategies to detect these events on a large scale.
Acknowledgments
The authors thank Alfredo Moreno for support designing the figures and Michele Saul for the analysis of survival data.
Financial Support: The authors received no specific funding for this work.
Footnotes
Conflict of Interest Statement: S. Jonna reports no competing interests. R.A. Feldman, J. Swensen, Z. Gatalica and W.M. Korn are employees of Caris Life Sciences. W.M. Korn reports consulting/advisory role from Merrimack and Merck Sharp & Dohme, stock/ownership interests with OncoCyte, has received honoraria from Genentech/Roche and institution-associated funding from Merrimack. H. Borghaei reports consulting/advisory role from Bristol-Myers Squibb, Lilly, Celgene, Genentech, Pfizer, Boehringer Ingelheim, EMD Serono, Trovagene, Novartis, Merck, AstraZeneca, Genmab, Regeneron, Contargia AB, BioNTech AG, Abbvie, received honoraria from Bristol-Myers Squibb, Celgene, Axiom Biotechnologies and institution-associated research funding from Millennium, Merck, Celgene, Bristol-Myers Squibb and Lilly. P.C. Ma reports association with the speakers’ bureau for Merck, Takeda, Bristol-Myers Squibb, stock/ownership from Cymeta Biopharmaceutical and institution-associated research funding from Pfizer, MedImmune, AstraZeneca, Bristol-Myers Squibb, Loxo, Xcovery, Abbvie, EpicentRx, Tesaro, Boehringer Ingelheim, OncoMed, CBT Pharmaceuticals, Merck and Cymeta Biopharmaceutical. J. Nieva reports consulting/advisory role with AstraZeneca, Genentech/Roche and Western Oncolytics, stock/ownership in Epic Sciences and research funding from Merck. A. Spira reports institution-associated research funding from Roche, AstraZeneca, Boehringer Ingelheim, Astellas Pharma, MedImmune, Novartis, Newlink Genetics, Incyte, Abbvie, Ignyta, LAM Therapeutics, Trovagene, Takeda, Macrogenics and CytomX Therapeutics. A. Vanderwalde reports consulting/advisory role with Bristol-Myers Squibb, AstraZeneca, Genentech and Caris Life Sciences, has received honoraria from AstraZeneca and institution-associated research funding from Amgen, Merck, Genentech/Roche, Millennium, AstraZeneca, Polynoma, Lilly, Bristol-Myers Squibb and Amgen. A. Wozniak reports consulting/advisory role with Boehringer Ingelheim, AstraZeneca, ARIAD, Coherus Biosciences, Array BioPharma, Hospira, Quintiles, BeyondSpring Pharmaceuticals, WCCT Global, Epic, Huron Consulting, HUYA Bioscience International and Takeda and has received research funding from Boehringer Ingelheim. E.S. Kim reports consulting/advisory role with Lilly, AstraZeneca, Boehringer Ingelheim, Pfizer, Merck and Takeda, has received honoraria from Lilly, AstraZeneca, Boehringer Ingelheim, Pfizer, Merck and Takeda and research funding from Boehringer Ingelheim, Lilly, Merck, Ignyta and Genentech/Roche. S.V. Liu reports consulting/advisory role with Apollomics, Boehringer-Ingelheim, G1 Therapeutics, Genentech/Roche, Ignyta, Guardant 360, Inivata, Janssen, Pfizer, Lilly, Merck, Taiho Pharmaceutical, Bristol-Myers Squibb, AstraZeneca, Takeda, HERON and Regeneron and has received research funding from Genentech/Roche, Pfizer, Threshold Pharmaceuticals, Clovis Oncology, Corvus Pharmaceuticals, Esanex, Bayer, OncoMed, Merck, Lycera, AstraZeneca, Ignyta, Molecular Partners, Blueprint Medicines, Lilly and Rain Therapeutics.
References:
- 1.Mok TS, Wu Y-L, Ahn M-J, Garassino MC, Kim HR, Ramalingam SS, et al. Osimertinib or Platinum-Pemetrexed in EGFR T790M-Positive Lung Cancer. N Engl J Med. 2017;376:629–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hida T, Nokihara H, Kondo M, Kim YH, Azuma K, Seto T, et al. Alectinib versus crizotinib in patients with ALK-positive non-small-cell lung cancer (J-ALEX): an open-label, randomised phase 3 trial. Lancet. 2017;390:29–39. [DOI] [PubMed] [Google Scholar]
- 3.Solomon BJ, Mok T, Kim D-W, Wu Y-L, Nakagawa K, Mekhail T, et al. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N Engl J Med. 2014;371:2167–77. [DOI] [PubMed] [Google Scholar]
- 4.Planchard D, Smit EF, Groen HJM, Mazieres J, Besse B, Helland Å, et al. Dabrafenib plus trametinib in patients with previously untreated BRAFV600E-mutant metastatic non-small-cell lung cancer: an open-label, phase 2 trial. Lancet Oncol. 2017;18:1307–16. [DOI] [PubMed] [Google Scholar]
- 5.Mayekar MK, Bivona TG. Current Landscape of Targeted Therapy in Lung Cancer. Clin Pharmacol Ther. 2017;102:757–64. [DOI] [PubMed] [Google Scholar]
- 6.Lindeman NI, Cagle PT, Aisner DL, Arcila ME, Beasley MB, Bernicker EH, et al. Updated Molecular Testing Guideline for the Selection of Lung Cancer Patients for Treatment With Targeted Tyrosine Kinase Inhibitors. The Journal of Molecular Diagnostics. 2018;20:129–59. [DOI] [PubMed] [Google Scholar]
- 7.Liu SV, Macke LA, Colton BS, Imran SS, Christiansen J, Chow-Maneval E, et al. Response to Entrectinib in Differentiated Thyroid Cancer With a ROS1 Fusion. JCO Precision Oncology. 2017;1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Drilon A, Laetsch TW, Kummar S, DuBois SG, Lassen UN, Demetri GD, et al. Efficacy of Larotrectinib in TRK Fusion-Positive Cancers in Adults and Children. N Engl J Med. 2018;378:731–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Drilon A, Somwar R, Mangatt BP, Edgren H, Desmeules P, Ruusulehto A, et al. Response to ERBB3-Directed Targeted Therapy in NRG1-Rearranged Cancers. Cancer Discov. 2018;8:686–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fernandez-Cuesta L, Plenker D, Osada H, Sun R, Menon R, Leenders F, et al. CD74-NRG1 fusions in lung adenocarcinoma. Cancer Discov. 2014;4:415–22. [DOI] [PubMed] [Google Scholar]
- 11.Gay ND, Wang Y, Beadling C, Warrick A, Neff T, Corless CL, et al. Durable Response to Afatinib in Lung Adenocarcinoma Harboring NRG1 Gene Fusions. J Thorac Oncol. 2017;12:e107–10. [DOI] [PubMed] [Google Scholar]
- 12.Jones MR, Lim H, Shen Y, Pleasance E, Ch’ng C, Reisle C, et al. Successful targeting of the NRG1 pathway indicates novel treatment strategy for metastatic cancer. Ann Oncol. 2017;28:3092–7. [DOI] [PubMed] [Google Scholar]
- 13.Cheema PK, Doherty M, Tsao M-S. A Case of Invasive Mucinous Pulmonary Adenocarcinoma with a CD74-NRG1 Fusion Protein Targeted with Afatinib. J Thorac Oncol. 2017;12:e200–2. [DOI] [PubMed] [Google Scholar]
- 14.Heining C, Horak P, Uhrig S, Codo PL, Klink B, Hutter B, et al. NRG1 Fusions in KRAS Wild-Type Pancreatic Cancer. Cancer Discov. 2018;8:1087–95. [DOI] [PubMed] [Google Scholar]
- 15.Huang H-E, Chin S-F, Ginestier C, Bardou V-J, Adélaïde J, Iyer NG, et al. A recurrent chromosome breakpoint in breast cancer at the NRG1/neuregulin 1/heregulin gene. Cancer Res. 2004;64:6840–4. [DOI] [PubMed] [Google Scholar]
- 16.McCoach CE, Le AT, Gowan K, Jones K, Schubert L, Doak A, et al. Resistance Mechanisms to Targeted Therapies in ROS1+ and ALK+ Non-small Cell Lung Cancer. Clin Cancer Res. 2018;24:3334–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kent WJ, Sugnet CW, Furey TS, Roskin KM, Pringle TH, Zahler AM, et al. The human genome browser at UCSC. Genome Res. 2002;12:996–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Panigrahi P, Jere A, Anamika K. FusionHub: A unified web platform for annotation and visualization of gene fusion events in human cancer. PLoS ONE. 2018;13:e0196588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wen D, Suggs SV, Karunagaran D, Liu N, Cupples RL, Luo Y, et al. Structural and functional aspects of the multiplicity of Neu differentiation factors. Mol Cell Biol. 1994;14:1909–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Murayama T, Nakaoku T, Enari M, Nishimura T, Tominaga K, Nakata A, et al. Oncogenic Fusion Gene CD74-NRG1 Confers Cancer Stem Cell-like Properties in Lung Cancer through a IGF2 Autocrine/Paracrine Circuit. Cancer Res. 2016;76:974–83. [DOI] [PubMed] [Google Scholar]
- 21.Dhanasekaran SM, Balbin OA, Chen G, Nadal E, Kalyana-Sundaram S, Pan J, et al. Transcriptome meta-analysis of lung cancer reveals recurrent aberrations in NRG1 and Hippo pathway genes. Nat Commun. 2014;5:5893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jo JY, Shin DH, Han J-Y. Abstract 3989: Dual targeting of ErbB2/ErbB3 for treatment of SCL3A2-NRG1-mediated lung cancer. Cancer Research. 2018;78:3989–3989. [Google Scholar]
- 23.Shin DH, Jo JY, Han J-Y. Dual Targeting of ERBB2/ERBB3 for the Treatment of SLC3A2-NRG1-Mediated Lung Cancer. Mol Cancer Ther. 2018;17:2024–33. [DOI] [PubMed] [Google Scholar]
- 24.Kim HS, Han J-Y, Shin DH, Lim KY, Lee GK, Kim JY, et al. EGFR and HER3 signaling blockade in invasive mucinous lung adenocarcinoma harboring an NRG1 fusion. Lung Cancer. 2018;124:71–5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. H&E demonstrating mucinous histology. A, CD74-NRG1 lung mucinous bronchoalveolar carcinoma; B, DIP2B-NRG1 lung mucinous colloid tumor
Figure S2. Diagram showing the variety and proportion of 5’ partners by tumor type.
Figure S3. Kaplan-Meier curves for a small cohort of patients with NRG1 fusion positive solid tumors. Vertical tick marks indicate right censored data. Numbers in box indicate median survival time in days (t). Whole cohort shown in green (n = 7, deaths = 5, t = 638 days). Cohorts by lineage shown in orange (lung; n = 3, deaths = 3, t = 200), pink (soft tissue tumors; n = 1, deaths = 1, t = 733) and blue (pancreatic; n = 2, deaths = 1, t = 638). Colorectal not shown; n = 1, deaths = 0, t not reached).