Abstract
Objective:
Research Domain Criteria (RDoC) operationalizes a set of basic social dimensions that can be used to deconstruct sources of variation in social impairments across affected individuals, regardless of their diagnostic status. This step is necessary towards the development of etiologically-based and individualized treatments. The main objective of the current investigation was to derive estimations of the RDoC social constructs from the Social Responsiveness Scale (SRS-2).
Method:
Exploratory Structural Equation Modeling (ESEM) and Confirmatory Factor Analysis (CFA) were conducted using individual SRS-2 items from 6 distinct databases (total N= 27953; Mage= 9.55, SD= 3.79; 71.7% male participants) spanning normative (33.8%) and atypical (66.2%) development. The following models were estimated: (1) a 1-factor model; (2) a 3-factor model with separate Attachment and Affiliation (AA), Social Communication (SC), and Understanding of Mental States (UMS) factors, and (3) a 4-factor model where SC was further split into Production of Facial (PFC) and Non-Facial (PNFC) communication.
Results:
The 1-factor solution showed poor fit. The 3-factor solution had adequate fit (comparative fit index [CFI]= .952, Tucker Lewis index [TLI]= .937, root mean square error of approximation [RMSEA]= .054), however, 4-factor solution had superior fit (CFI= .973, TLI= .961, RMSEA= .042) and was robust across age, gender and clinical status.
Conclusion:
To our knowledge, this is the first study examining estimations of the RDoC social constructs from an existing measure. Reported findings show promise for capturing important RDoC social constructs using the SRS-2 and highlight crucial areas for the development of novel dimensional social processing measures.
Keywords: Research Domain Criteria, Social Processes, Neurodevelopmental and Neuropsychiatric Disorders, Variable-Centered, Heterogeneity
Introduction
Disruption of social functioning and difficulties in navigating the complexities of the social world are an early and defining feature of autism spectrum disorder (ASD) and also occur across a wide array of neurodevelopmental, neuropsychiatric and neurodegenerative disorders.1–4 Social impairments persist over time, significantly contributing to poor outcomes for affected individuals and their families and to considerable public health costs.5–8 Social deficits therefore constitute a critical domain for long-term outcomes and an important intervention target. However, there is a striking heterogeneity in the profile of social deficits and strengths across individuals diagnosed with ASD and in their response to treatments.9,10 Noted heterogeneity in social functioning is by no means specific to ASD but is apparent across other neurodevelopmental and neuropsychiatric disorders. Indeed, individuals classified under a range of separate diagnostic categories can exhibit a range of shared social functioning deficits, while those diagnosed with the same disorder can exhibit different deficits.11,12 These limitations of the current diagnostic systems and the lack of accurate characterization of the mechanisms underlying social deficits present an obstacle on the path to precision medicine and the identification of meaningful subgroups that will facilitate the development of more effective and targeted interventions.
A fully dimensional alternative to the categorically based diagnostic systems offered by the National Institute of Mental Health’s (NIMH) Research Domain Criteria (RDoC)11,13 operationalizes an initial set of basic, biologically meaningful dimensions that underpin social functioning. Specified domains include the ability to perceive and interpret social signals, motivation to engage in social interactions and form social bonds, and skills necessary for initiating and maintaining social interactions and relationships. These constructs and are posited to be subserved by a sophisticated, highly connected network of brain regions including amygdala, anterior insula, superior temporal sulcus, ventral and medial prefrontal cortex and the temporo-parietal junction.14–17 Given the complexity of the social processes and the partial mutual dependence of the constituting basic components, even slight deviations in any of the noted social constructs can result in a significant social impairment. Individuals exhibiting diverse phenotypic presentations require varied treatment approaches which will be more or less effective depending on the individual’s profile of strengths and weaknesses across different components of the social phenotype. Therefore the potential utility of the dimensions put forward by the RDoC in deconstructing sources of variation in social impairments across affected individuals, regardless of their diagnostic status, presents a promising and a necessary step towards the development of etiologically-based, individualized treatments.
Despite the significant promise, the translation of the RDoC framework into research and clinical practice has been impeded by the lack of dedicated measures for assessing proposed dimensions. Therefore establishing effective means of capturing and extracting relevant RDoC domains from already collected data, even in a manner that is somewhat suboptimal, can offer an important bridge towards providing initial testing of the explanatory power of this framework. This would also present research and clinical communities with alternative means of assessing key dimensional constructs until measures specifically designed to capture components of functioning across clinical, at risk and normative populations are developed. Recognizing this issue, the NIMH has established a working group to identify existing measures that are able to tap into some of the proposed RDoC constructs.18
One of the measures recommended by the NIMH workgroup18 is the Social Responsiveness Scale (SRS-2).19,20 The SRS-2 is a quantitative measure of social functioning that has previously been used mainly within the context of autism spectrum disorder (ASD) as a measurement of quantitative trait severity, a screening instrument in the general population and diagnostic aid to clinical diagnostic practice, showing good cross-cultural validity.21–23 Relevant to the RDoC framework, the SRS-2 has a good dimensionality and it was designed to cover the four different aspects of social deficits—social awareness, social cognition, social communication and social motivation, in addition to assessing autistic mannerisms. However, the original five factors were not supported in the subsequent studies.21,22,24 Although earlier factor analyses have suggested the unidimensional structure21,22,25,26 more recent and advanced applications of the factor analytic procedures have suggested that unidimensional model shows poor fit27 and that two,24 four,28,29 and five24 factors provide more precise analytical solutions of the SRS-2 structure. Particularly encouraging from the RDoC perspective is a study by Frazier and colleagues24 that has identified several factors including social avoidance, emotion recognition and interpersonal relatedness which bear resemblance to a range of constructs and sub-constructs defined by the RDoC. Although work by Frazier and colleagues offers initial promising insights into the potential utility of the SRS-2, the usefulness of the derived factors is limited by the fact that several potentially distinct constructs are conflated within a single factor, and the identified factors contain items that do not map onto the hypothesized constructs (e.g., “Seems self-confident when interacting with others” and “Is not well coordinated” in the case of emotion recognition and interpersonal relatedness factors, respectively). Therefore, although the SRS-2 holds the potential of approximating some of the RDoC social constructs, further fine-grained factor analytical work in larger and clinically more diverse samples is needed.
Work presented here follows the recommendations from the NIMH workgroup18 and combines an integrative data analysis framework30,31 with advanced variable-centered statistical approaches including confirmatory factor analysis and the exploratory structural equation modeling32,33 to explore the utility of the SRS-2, one of the most commonly used scale to assess social abilities,18 for depicting proposed RDoC social dimensions in a data set an order of magnitude larger than all previous studies, spanning normative and atypical development. We first explore the unidimensional model given that a range of studies still utilize total score following earlier factor analytic studies positing that SRS is best represented as a unitary factor.19 Secondly, we explore the three-factor solution where SRS social and communication items are mapped onto the RDoC constructs of Attachment and Affiliation, Social Communication, and Perception and Understanding of Mental States. Thirdly, we examine a more fine-grained structure where the Social Communication construct was further decomposed into the production of non-facial and facial communication sub-constructs as described in the RDoC framework. Given that previous factor analytical explorations of the SRS that have identified several potential distinct facets captured by this measure, we will compare the fit of these solutions to the best fitting derived RDoC factor solution. Findings from both the general and ASD literature suggest distinct developmental trajectories and gender effects of distinct aspects of social functioning.34,35 In addition, several ASD studies have found association between chronological age and gender with the expression of social deficits captured by the SRS specifically/24,36 Interestingly, a recent study by Wallace and colleagues56 found that while the social-communication abilities measure by the SRS-2 improved with age in a sample of typically developing children, the opposite was observed in children with ASD. Therefore, in addition to exploring the fit and stability of the derived RDoC factor solution across normative and clinical populations, we will also evaluate the effects of age, gender and diagnosis on the expression of identified, distinct RDoC social constructs.
Method
Participants
Data were obtained from six distinct databases: Healthy Brain Network;37 SRS-2 standardization dataset;38 National Database for Autism Research (https://ndar.nih.gov); Simons Simplex Collection;39 Autism Genetic Research Exchange;40 Interactive Autism Research Database (http://iancommunity.org). These datasets include individuals with ASD, their siblings, typically developing and individuals with a range of neurodevelopmental and neuropsychiatric disorders (NDD/NPD). Supplement 1, available online, provides a detailed description of each sample.
All participants or their parent/legal guardian have provided informed consent for participation. Only individuals aged 18 years or younger with SRS-2 (parent report) data were included in this study. The final sample (N= 27953) consisted of predominantly male participants (69.6%), aged 2.04–18.94 years (Mage= 9.55, SD= 3.79). Table 1 presents demographic and diagnostic characteristics separately for each of the databases.
Table 1:
Demographic Characteristics
| Study |
||||||
|---|---|---|---|---|---|---|
| HBN (n= 1301) | SRS Norm (n= 1179) | NDAR (n= 4954) | SSC (n= 5591) | AGRE (n= 2282) | IAN (n= 12646) | |
| Mean age (SD), years | 10.54 (3.17) | 9.06 (4.59) | 9.52 (4.59) | 9.03 (3.56) | 8.34 (3.54) | 9.77 (3.87) |
| Male % | 63 | 48.7 | 78.3 | 68.3 | 68.6 | 69.4 |
| Diagnostic | ||||||
| Groupa | ||||||
| ASD % | 8.2 | 100 | 68.1 | 57.9 | 100 | 64.3 |
| Unaffected | NA | NA | NA | 42.1 | NA | 35.6 |
| Sibling % | ||||||
| TD % | 12.9 | NA | 25.5 | NA | NA | NA |
| NDD/NPD% | 78.9 | NA | 6.4 | NA | NA | 0.1 |
Note: AGRE = Autism Genetic Research Exchange; ASD = autism spectrum disorder; HBN = Healthy Brain Network; IAN = Interactive Autism Research Database; NDAR = National Database for Autism Research; NDD/NPD = neuropsychiatric/neurodevelopmental disorders; SRS Norm = Social Responsiveness Scale standardization dataset; SSC = Simons Simplex Collection; TD = typically developing.
For detailed information on specific diagnoses see Supplement 1, available online.
Measures
The Social Responsiveness Scale (SRS-2) is a 65-item measure designed to index severity in social impairments as well as the presence of repetitive behaviors. Each item is rated on a 4-point Likert scale (from 1= Not True to 4= Almost Always True) with higher scores indicating higher trait severity/atypicality.
Data Analysis
After all six samples were combined, the resulting dataset (N= 27953) was randomly split into initial/construction (Sample 1; n= 14033; Mage= 9.54, SD= 3.79; 69.5% male participants) and validation (Sample 2; n= 13920; Mage= 9.55, SD= 3.80, 69.7% male participants) datasets with the comparable distribution of ASD, NDD/NPD, TD, and unaffected siblings (Sample 1: 59.7% ASD, 24.6% unaffected siblings, 9.4% typically developing, 6.3% NDD/NPD; Sample 2: 60.3% ASD, 24.4% unaffected siblings, 9.3% typically developing, 6% NDD/NPD). SRS items were conceptually mapped onto the overarching RDoC social constructs, as well as onto the more fine-grained social constructs described in the introduction. Seventeen researchers with expertize in social processes across NDD/NPD and TD independently mapped each item against relevant RDoC constructs (for mapping of items against the RDoC constructs see Table S1, available online). For the analyses, each item was mapped onto the specific RDoC construct/subconstruct if there was an agreement across 14 or more experts (>80%). Items that simultaneously sampled absence and atypicality (e.g. item 16 asking whether individual avoids eye contact or has unusual eye contact) or items indicated by the first and senior author, and by research experts, to sample behaviors that could result from a range of distinct processes (e.g., items 36 and 37 measuring individual’s difficulty in relating to adults and peers, respectively) were not included in the analyses given the RDoC emphasis on the importance of assessing basic constructs that do not encompass a range of different processes. Items taping into non-social behaviors/constructs or that had both social and non-social aspects (e.g. items 14, 39, 50, 59 asking whether individual is well coordinated, exhibits narrow range of interests, behaviors such as hand flapping or rocking, and suspicious towards others, respectively) were excluded given the present focus on the RDoC social processes domain. Although item 43 was mapped onto the Attachment and Affiliation construct by 16 experts, it did not load onto any of the constructs in the ESEM analysis (detailed overview provided below). Therefore, final analysis included twenty-six items.
All factor analyses were conducted using MPLUS 8.0.40 Confirmatory factor analysis (CFA) is a dominant approach for validating measurement and construct structure. However, CFA commonly constrains item loading only onto the hypothesized factor which often results in poor fit and biased parameter estimates in psychology and psychiatry research where items are expected to also load onto the non-target factors (constructs).33,41 Therefore, as a primary means for examining SRS RDoC models, we utilized a confirmatory application of a novel analytical framework—Exploratory Structural Equation Modelling (ESEM)32,33 which does not require loadings of items onto non-target factor to be zero. Following the current recommendations,33 we compared statistical indexes of models derived through both ESEM and CFA. Robust maximum likelihood estimator was used. Analyses were also re-run using the polychoric correlations with the weighted least square estimator. Model fit was evaluated using the following fit indices: the Comparative Fit Index (CFI); the Tucker-Lewis Index (TLI); the Root Mean Square Error of Approximation (RMSEA); the Standardized Root Mean Square Residual (SRMR). The following cut-offs were applied: (i) CFI and TLI values > .90 indicating adequate and > .95 excellent fit; (ii) RMSEA and SRSM values of < .08 indicating adequate and < .06 excellent fit, with RMSEA 90% confidence intervals < .08 and the close fit-test with a p value > .05. Fit indices were first evaluated in the initial/construction subsample, and then in the validation subsample to ensure the robustness of the models.
In order to explore age and gender effects on the identified RDoC social factors, factor scores were regressed on age and gender in normative (typically developing and unaffected siblings), ASD and other clinical conditions samples. Regression models were run in SPSS42 and performed with 5000 resamples bootstrapping to provide more robust statistics.43
Results
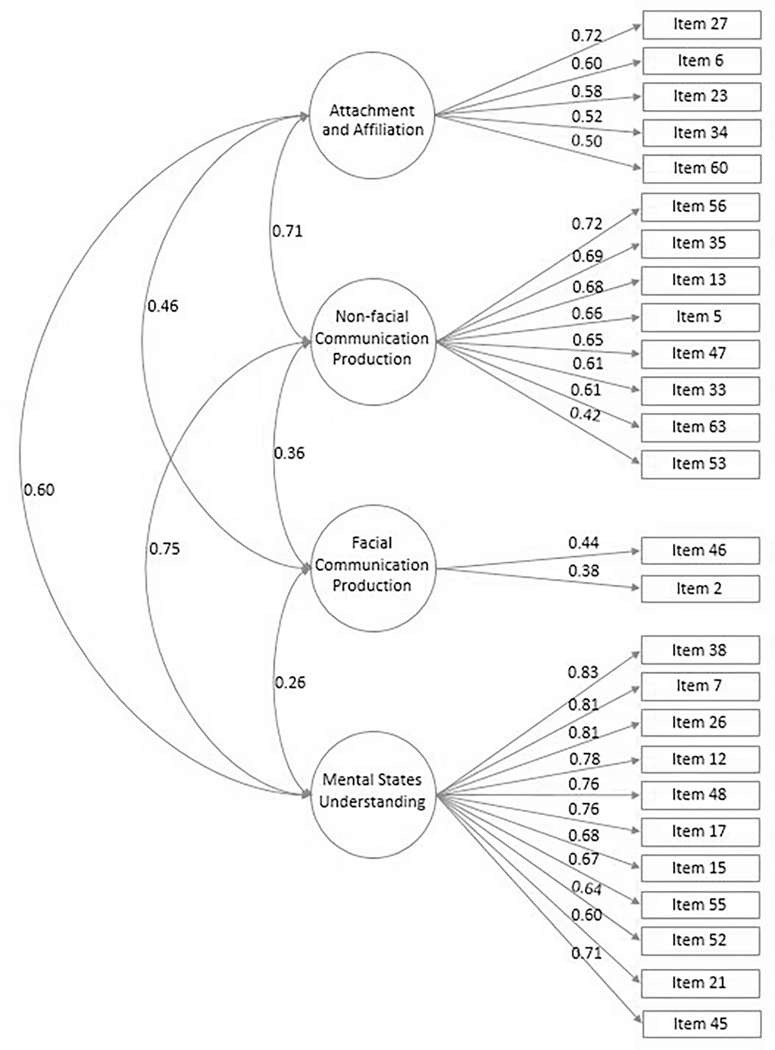
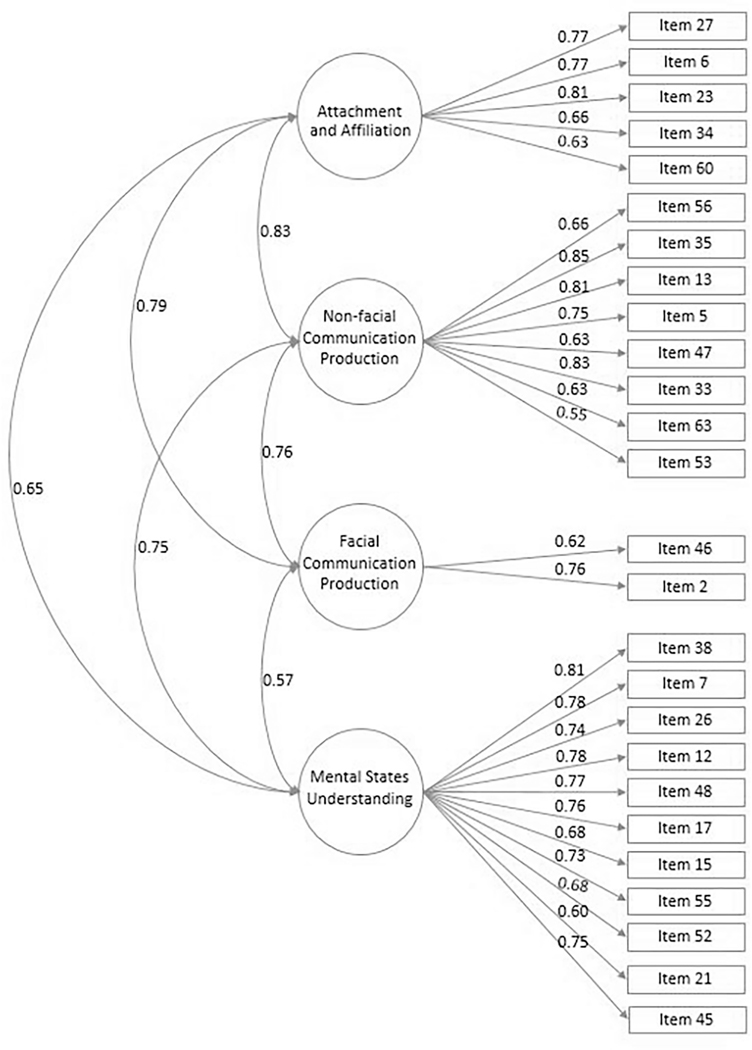
The ESEM and CFA models are presented in Table 2. The unidimensional model had unsatisfactory fit (CFI= .782, TLI= .763, RMSEA= .105). The 4-factor model including Attachment and Affiliation (AA), Production of Facial (PFC) and Non-Facial (PNFC) Communication, and Understanding of Mental States (UMS) had a superior fit to the three-factor model, both when using ESEM (CFI= .973, TLI= .961, RMSEA= .042 vs CFI= .952, TLI= .937, RMSEA= .054) and CFA (CFI= .935, TLI= .928, RMSEA= .058 vs CFI= .927, TLI= 919, RMSEA= .061), across both construction and validation subsamples, and was therefore retained for further exploration. The ESEM framework indicated a more optimal fit and significantly lower factor correlations than CFA (See Figure 1 for ESEM and Figure 2 for CFA for the whole sample). All items loaded onto the hypothesized factor with the following exceptions: item 5 relating to the ability of the individual to recognize when others are trying to take advantage of her/him was originally mapped onto UMS but ESEM suggested it significantly loaded onto the PNFC factor; Item 12 relating to individual’s ability to communicated his/her feelings was originally mapped onto the PNFC factor, but ESEM showed significant loading onto the USM factor instead. Item 56 was originally mapped onto the UMS but ESEM suggested it significantly loaded onto the PNFC factor. The derived 4-factor solution was then compared to the fit of the following SRS-2 factor solutions previously reported in the literature: (i) 2-factor solution derived by Frazier and colleagues24 (Factor 1: social communication and interaction, Factor 2: restricted, repetitive pattern of behavior), 4-factor solutions identified by (ii) Gau and colleagues28 (Factor 1 combining social, communication and repetitive behavior items, Factor 2 mostly repetitive behavior items, Factor 3 social awareness, Factor 4 mostly items related to emotional aspects of behavior) and (iii) Nelson and colleagues29 (social awareness and competence, repetitive behaviors, atypical social communication, and social avoidance), (iv) 5-factor solution by Frazier and colleagues24 (emotion recognition, social avoidance, interpersonal relatedness, insistence on sameness, and repetitive mannerisms). Fit indices of these models are presented in Table 2. As can be seen, 4-factor RDoC solution showed a more optimal fit to the solutions previously reported in the literature.
Table 2:
Summary of Goodness of Fit Statistics for the tested Exploratory Structural Equation Modeling (ESEM) and Exploratory Structural Equation Modeling (ESEM) and Confirmatory Factor Analysis (CFA) and Previous Social Responsiveness Scale (SRS-2) Factor Models
| Model | χ2 | CFI | TLI | RMSEA (90%CI) | SRMR | AIC | BIC | corBIC | |
|---|---|---|---|---|---|---|---|---|---|
| ESEM bUnidimensional | Sample 1 | 44310.956** | .782 | .763 | .105** (.104; .106) | .073 | 847144.962 | 847729.776 | 847481.900 |
| Sample 2 | 43597.869** | .783 | .764 | .105** (.104; .105) | .073 | 844449.582 | 845033.986 | 844786.110 | |
| ESEM 3-Factor | Sample 1 | 9973.876** | .952 | .937 | .054** (.053; .055) | .024 | 812905.882 | 813858.080 | 813454.486 |
| Sample 2 | 9854.900** | .952 | .937 | .055** (.053; .055) | .024 | 810804.614 | 811756.143 | 811352.550 | |
| CFA 3-Factor | Sample 1 | 15088.242** | .927 | .919 | .061** (.060; 062) | .038 | 817928.248 | 818535.555 | 818278.145 |
| Sample 2 | 15094.666** | .926 | .919 | .061** (.061; 062) | .038 | 815952.380 | 816559.261 | 816301.851 | |
| ESEM 4-Factor | Sample 1 | 5638.681** | .973 | .962 | .042 (.041; .043) | .016 | 808616.686 | 809741.330 | 809264.644 |
| Sample 2 | 5674.334** | .973 | .961 | .043 (.042; .044) | .016 | 806670.048 | 807793.901 | 807317.216 | |
| CFA 4-Factor | Sample 1 | 13415.546** | .935 | .928 | .058** (.057; .059) | .034 | 816261.551 | 816891.352 | 816624.408 |
| Sample 2 | 13551.843** | .934 | .926 | 058** (.058; .059) | .035 | 814415.557 | 815044.915 | 814777.971 | |
| Frazier etal.24 | |||||||||
| 2-Factor | |||||||||
| ESEM | Sample 1 | 87013.403** | .856 | .846 | .058** (.058; .059) | .036 | 1960241.939 | 1962151.237 | 1961340.872 |
| Sample 2 | 85065.312** | .857 | .847 | .058** (.058; .058) | .036 | 1960440.831 | 1962348.986 | 1961538.621 | |
| CFA | Sample 1 | 129299.073** | .785 | .778 | .070** (.070; .071) | .058 | 2002403.609 | 2003848.685 | 2003235.350 |
| Sample 2 | 125963.426** | .787 | .780 | .070** (.069; .070) | .058 | 2001214.945 | 2002659.156 | 2002045.821 | |
| Frazier et al.24 | |||||||||
| 5-Factor | |||||||||
| ESEM | Sample 1 | 41039.010** | .934 | .921 | .042 (.041; .042) | .020 | 1914633.546 | 1917913.046 | 1916521.125 |
| Sample 2 | 39007.060** | .936 | .924 | .041 (.040; .041) | .020 | 1914748.579 | 1918026.115 | 1916634.194 | |
| CFA | Sample 1 | 99893.705** | .834 | .828 | .062** (.062; .062) | .061 | 1973016.242 | 1974528.705 | 1973886.769 |
| Sample 2 | 97244.595** | .836 | .830 | .061** (.061; .061) | .059 | 1972514.114 | 1974025.672 | 1973383.736 | |
| Gau et al. 28 | |||||||||
| 4-Factor | |||||||||
| ESEM | Sample 1 | 44867.550** | .923 | .911 | .046 (.046; .047) | .022 | 1789392.526 | 1792043.375 | 1790918.398 |
| Sample 2 | 43078.062** | .925 | .913 | .045 (.045; .046) | .022 | 1788045.859 | 1790694.935 | 1789569.957 | |
| CFA | Sample 1 | 85515.863** | .850 | .844 | .061** (.061; .061) | .042 | 1829704.839 | 1831097.658 | 1830506.568 |
| Sample 2 | 84644.004** | .850 | .844 | .061** (.061; .061) | .042 | 1829275.801 | 1830667.688 | 1830076.598 | |
| Nelson et al29 | |||||||||
| 4-Factor | |||||||||
| ESEM | Sample 1 | 51397.804** | .917 | .905 | .047 (.047; .047) | .023 | 1879686.134 | 1882471.491 | 1881289.311 |
| Sample 2 | 49426.510** | .919 | .907 | .046 (.046; .047) | .023 | 1879627.987 | 1882411.762 | 1881229.582 | |
| CFA | Sample 1 | 108360.927** | .821 | .815 | .065** (.065; 066) | .062 | 1936295.257 | 1937755.323 | 1937135.632 |
| Sample 2 | 106104.523** | .823 | .816 | .065** (.065; 065) | .062 | 1935952.000 | 1937411.237 | 1936791.546 | |
Note: AIC= Akaike Information Criterion; BIC= Bayesian Information Criterion; CFA = Confirmatory Factor; CFI = Comparative Fit Index; corBIC= Sample size adjusted BIC; RMSEA = Root Mean Square Error of Approximation; SRMR = Standardized Root Mean Square Residual; TLI = Tucker-Lewis Index.
p< .01;
p< .001.
Figure 1.
Exploratory Structural Equation Modelling Correlated 4-Factor Solution
Note: Solid lines represent factor loadings and curved lines represent the correlation among factors.
Figure 2.
Confirmatory Factor Analysis (CFA) 4-Factor Solution
Note: Solid lines represent factor loadings and curved lines represent the correlation among factors.
Stability of the derived correlated 4-factor solution was further confirmed across (i) diagnostic group (TD, unaffected siblings, clinical sample), (ii) sex and (iii) age (sample was divided into children aged 2–6, 7–12 and 13–18 years). In addition, a range of SRS-2 items assume child to have a certain level of verbal ability and although the majority of these items were not included in our final 4-factor solution, we have sought to confirm the stability of the derived factor structure separately in subsamples of non-verbal and verbal children. Children were classified as verbal and non-verbal based on the item 1 from the Social Communication Questionnaire (SCQ).58 SCQ data were available for n= 15936 children (12% were non-verbal and 88% verbal). Table 3 shows fit indices across the tested models. A 4-factor solution showed excellent fit across typical and atypical development, age, sex and verbal status and items loadings onto AA, PNFC, PFC and UMS factors were comparable and significant across tested subgroups.
Table 3:
Summary of Goodness of Fit Statistics for the Tested Best Fitting Exploratory Structural Equation Modeling (ESEM) Research Domain Criteria (RDoC) Model Across Normative and Clinical Samples, Age, Gender and Language Level
| χ2 | CFI | TLI | RMSEA (90%CI) | SRMR | AIC | BIC | corBIC | |
|---|---|---|---|---|---|---|---|---|
| Whole Sample | 11059.798** | .973 | .961 | .042 (.042; .043) | .016 | 1615221.613 | 1616449.834 | 1615973.137 |
| Clinical Sample | 8676.615** | .944 | .920 | .046 (.045; .047) | .023 | 1121834.557 | 1123000.033 | 1122523.342 |
| Unaffected Siblings | 2211.598** | .962 | .946 | .036 .035; .038) | .019 | 283218.339 | 284238.039 | 283761.376 |
| Normative Sample | 943.404** | .958 | .939 | .036 (.033; 038) | .021 | 121600.055 | 122471.669 | 121995.082 |
| Feale Sex/Gender | 2914.499** | .976 | .965 | .042 (.041; .044) | .015 | 385413.762 | 386433.008 | 385956.346 |
| Male Sex/Gender | 7658.034** | .965 | .950 | .044 (.043; .045) | .018 | 1064468.165 | 1065629.549 | 1065152.858 |
| Age Group 1a | 3119.032** | .967 | .953 | .044 (.043; .046) | .018 | 401071.695 | 402089.572 | 401612.910 |
| Age Group 2b | 5044.689** | .971 | .958 | .043 (.042; .044) | .017 | 702580.925 | 703683.388 | 703206.706 |
| Age Group 3c | 2380.662** | .973 | .961 | .043 (.041; .044) | .016 | 321368.835 | 322353.218 | 321876.567 |
| No Functional Language | 748.870** | .964 | .949 | .035 (.032; .038) | .020 | 116387.464 | 117216.714 | 116740.167 |
| Functional Language | 5322.038** | .975 | .965 | .042 (.041; .043) | .015 | 766863.586 | 767984.527 | 767507.842 |
Note: AIC= Akaike Information Criterion; BIC= Bayesian Information Criterion; CFA= Confirmatory Factor; CFI= Comparative Fit Index; corBIC= Sample size adjusted BIC; ESEM= Exploratory Structural Equation Modelling; RDoC= Research Domain Criteria; RMSEA= Root Mean Square Error of Approximation; SRMR= Standardized Root Mean Square Residual; TLI= Tucker-Lewis Index.
Group 1: 2–6 years of age.
Group 2: 7–12 years of age.
Group 3: 13–18 years of age.
p< .01;
p< .001
Table 4 shows the effects of age and gender across typically developing, ASD and non-ASD clinical groups. There were significant associations between (i) older age and more severe and PFC scores, (ii) younger age and more severe PNFC and UMS scores, and (iii) female gender and less severe PNFC scores across all groups. Female gender was associated with higher PFC scores in individuals from non-ASD clinical conditions, however, no significant effects for gender on PFC were observed in TD and ASD groups. Conversely, while gender was not significantly associated with AA scores for individuals from non-ASD clinical conditions, both TD and ASD female participants had less severe AA scores. Finally, female participants with ASD had more severe UMS scores, however, the opposite direction of the effect was observed in the other two groups.
Table 4:
Relationship Between Research Domain Criteria (RDoC) Social Responsiveness Scale (SRS-2) Social Constructs with Age and Gender
| β | SE | t | p | BCa 95% CI | |||
|---|---|---|---|---|---|---|---|
| AA | TD | CA | .167 | .001 | 14.269 | <.001 | .007; .009 |
| Sex | −.039 | .052 | −3.343 | .001 | −.274; −.071 | ||
| ASD | CA | .139 | .001 | 17.648 | <.001 | .010; .012 | |
| Sex | −.012 | .073 | −1.469 | .142 | −.249; .036 | ||
| Other Clinical | CA | .196 | .002 | 7.292 | <.001 | .011; .019 | |
| Sex | −.014 | .179 | −.511 | .609 | −.443; .260 | ||
| PNFC | TD | CA | −.112 | .001 | −9.423 | <.001 | −.009; −.006 |
| Sex | −.048 | .077 | −4.024 | <.001 | −.463; −.160 | ||
| ASD | CA | −.039 | .001 | −4.956 | <.001 | −.006; −.003 | |
| Sex | −.020 | .100 | −2.558 | .011 | −.452; −.060 | ||
| Other Clinical | CA | −.115 | .003 | −4.257 | <.001 | −.019; −.007 | |
| Sex | −.109 | .266 | −4.015 | <.001 | −1.592; −.547 | ||
| PFC | TD | CA | .045 | .000 | 3.775 | <.001 | .000; .001 |
| Sex | −.003 | .023 | −.247 | .885 | −.050; .039 | ||
| ASD | CA | .171 | .000 | 21.773 | <.001 | .005; .006 | |
| Sex | .004 | .031 | .520 | .603 | −.044; .077 | ||
| Other Clinical | CA | .192 | .001 | 5.126 | <.001 | .004; .009 | |
| Sex | .088 | .117 | 2.367 | .018 | .047; .507 | ||
| UMS | TD | CA | −.107 | .001 | −9.137 | <.001 | −.016; −.010 |
| Sex | −.096 | .138 | −8.136 | <.001 | −1.397; −.854 | ||
| ASD | CA | −.048 | .001 | −6.103 | <.001 | −.009; −.005 | |
| Sex | .023 | .133 | 2.915 | .004 | .127; .650 | ||
| Other Clinical | CA | −.108 | .004 | −3.963 | <.001 | −.025; −.008 | |
| Sex | −.115 | .366 | −4.244 | <.001 | −2.269; −.834 | ||
Note: AA = Attachment and Affiliation; ASD = autism spectrum disorder; BCa 95% CI= bias-corrected and accelerated 95% confidence internal; CA = Chronological Age; PNFC = Production of Non-Facial Communication; PFC = Production of Facial Communication; TD = typically developing; UMS = Understanding of Mental States.
Discussion
The present study utilized advanced variable-centered statistical approaches to derive estimations of the Research Domain Criteria (RDoC) social constructs and sub-constructs from the Social Responsiveness Scale (SRS-2) in the largest dataset to date spanning both normative and clinical populations. The fine-grained four-factor model reflecting RDoC constructs of Attachment and Affiliation (AA), Production of Facial (PFC) and Non-Facial (PNFC) Communication, and Understanding of Mental States (UMS) showed superior fit across construction and validation subsamples and across clinical, normative and subsample of unaffected siblings of individuals with ASD. The three-factor solution where PFC and PNFC sub-constructs were merged into social communication (resembling solution derived by Frazier et al.24) showed adequate, but less optimal fit. Consistent with Frazier and colleagues and others, the unidimensional model provided a poor fit. Crucially, identified four-factor structure was robust, with excellent fit and very similar loadings of items onto AA, PFC, PNFC, and UMS factors across age, gender, verbal level and typical and atypical development. Finally, the four-factor model showed a more optimal fit to the data when compared to the two-, four and five-factor SRS-2 solutions previously reported in the literature,24,28,29 however, given that our aim was not to identify the best fitting general SRS factor solution but rather to evaluate the ability of the SRS-2 to approximate RDoC social sub-constructs, alternative factor structures, especially in relation to the structure of ASD, are possible and should be used depending on the specific aim and focus of the analysis.
RDoC social constructs and subconstructs captured by the SRS-2 showed a distinct pattern of associations with age and gender, and some of these effects were moderated based on the clinical status. Across both typical and atypical development, female gender was associated with less severe PNFC scores, a finding consistent with the previous literature on higher social interaction skills in female participants, irrespective of the diagnosis.24,34,35 Consistent with the previous literature on social motivation in both ASD and typical development,44 we found that female gender was associated with less severe SRS-2 AA scores across both of these subgroups. We further replicated and extended previous work suggesting that female participants with ASD might show a more severe phenotype in certain aspects of social cognition,24 an opposite pattern to the one seen in typical development.45 Across both typically developing and clinical subsamples, older age was associated with more problems in the affiliation and attachment and production of facial communication, and fewer problems in the production of the non-facial communication and understanding of mental states RDoC constructs as captured by the derived SRS-2 factors. Although these findings are consistent with the general literature suggesting that both social interaction skills and the ability to perceive and interpret social signals become progressively more advanced and sophisticated over time,34,46 it is important to note that given the cross-sectional nature of the data reported here, inferences about the development are necessarily tenuous and some of the observed age effects might be due to the sampling differences across age.24 Detailed longitudinal explorations of these phenomena across both normative and atypical development, and how they mutually interact across sensitive developmental periods in order to produce distinct clinical presentations, is needed in order to further clarify findings reported here. For example, lower levels of affiliative behaviors and social drive over time might occur in individuals who initially had intact desire to interact socially but have faced accumulated negative social experiences due the impairments in other social domains (such as for example ability to understand others’ intentions and read social cues and/or limited social skills). Alternatively, for certain individuals with good UMS and social skills, lack of social drive might just become more apparent over time, as societal expectations increase. Finally, for a subgroup of individuals, the decrease in the desire to socially engage might be a result of additional emerging psychopathology, such as the development of psychotic symptoms and other forms of developing psychopathology, including generalized and social anxiety disorders, as well as depression symptoms.
As suggested by the RDoC, the overall impairments in social functioning and the ability to navigate the social world seen across individuals belonging to a range of diagnostic categories are likely underpinned by distinct areas of weakness, which combined with some preserved (or less impaired) skills, necessitates individually tailored treatment approaches. Therefore, the crucial next step will be to address the question of whether identified social constructs can be used to provide a meaningful characterization of individual clinical cases and to derive predictive profiles in treatment-oriented research. There is a potential for significant synergy between the approach we have taken here and recently developed Natural Language Processing (NLP) algorithms for extracting overarching RDoC domains from the electronic health records.47 More specifically, developed NLP algorithms can be used to sample individuals with general social impairment from large clinical populations, who would then be further profiled at the individual level using the derived SRS-2 RDoC factors. This research pipeline would capitalize on the recommendations for dimensional psychopathology research designs48 and enable identification of clinically useful and biologically valid subtypes that have higher descriptive and predictive power than the current categorical classes.
On a more conceptual level, the proposed structure of the social processes put forward by the RDoC will need to be empirically tested and further refined. For example, the Attachment and Affiliation might be too general given that it encompasses a range of potentially distinct constructs. More specifically, social motivation, which is currently subsumed under the broad attachment and affiliation construct, has been suggested to encompass a range of distinct components including social orienting, interest, approach and social liking.50,51 In addition, RDoC currently draws distinction between the perception of facial and non-facial communication and conceptualizes understanding of mental states as unitary construct, however, in the social cognition literature there is a long standing debate on how best to conceptualize these processes. In fact some experts draw distinction between processing of the low-level and high-level information (e.g. recognition of facial emotion expression vs theory of mind) or between affective and cognitive processing, and others including constructs such as social attribution.52,53 Finally, several models of social processes have highlighted social learning,54 social avoidance,55 or withdrawal,16 and regulation of emotions in social contexts2,57 as important constructs. Therefore, although our study provides very preliminary psychometric evidence for the validity of the attachment and affiliation production of facial and non-facial communication and understanding of mental states constructs, further work integrating multiple measures of social functioning is needed to examine and further refine the RDoC matrix and to arrive at the empirically derived, comprehensive nosology of the social processes across normative and atypical development.
Promising findings from the current study need to be considered in light of several notable limitations. Firstly, although the sample used here spanned normative and different NDD/NPD groups as well as unaffected siblings of individuals with ASD, thus providing a wide variability across social dimensions, the clinical distribution was nevertheless heavily skewed towards the ASD and the findings reported here should be considered predominantly in terms of their relevance to ASD. Therefore future work is needed to further refine derived factors within large non-ASD clinical samples. Secondly, our ability to test RDoC constructs was biased by both the selection of items that were submitted to the ESEM/CFA as well as by the coverage of the instrument itself. More specifically, although the SRS is a quantitative measure that samples a relatively wide range of social behaviors, traits and abilities, it was nevertheless designed in the context of ASD and the coverage of social processes was not rooted in the current conceptual models of social functioning, including the one put forward by the RDoC. As a consequence, in the current analysis, PFC construct is only represented by two items. From a purely psychometric perspective, it has been demonstrated that two, or even single-item indicators can be reliable49,50 and this has been supported by the stability of the PNFC construct across different subgroups in the current analysis. However, from the perspective of clinically, etiologically, and treatment-oriented research, it is clear that additional items capturing different facets of facial communication are essential. Similarly, the PNFC construct does not include important behavioral indicators, such as different types of gestures, and is skewed towards social impairments characteristic of ASD. Further, AA construct does not capture the full range of motivation, attachment and affiliative behavior. Finally, the SRS-2 does not specifically assess reception construct and subconstructs nor does it include items tapping into constructs such as social attribution. Given this, it is important to consider the development of new instruments that will assess the above noted behaviors and dimensions in greater detail. Importantly, future scales should include a balanced number of items to enable a comprehensive assessment of the different dimensions identified in the present investigation. As noted, a number of SRS-2 items require individual to demonstrate a certain level of verbal ability. Although the majority of these items were not included in the RDoC SRS-2 scales we derived here, and identified factor structure was robust across verbal and non-verbal samples, it is clear that this question will need to be more adequately tackled by future new scales. Although the subjective-report unit of analysis is particularly important for clinical practice and affords ecological validity not offered by other measurement modalities, RDoC aims to recast psychopathology in light of impairments in basic biological systems and emphasizes the importance of measuring specific constructs and subconstructs across a spectrum of units of analysis. It will therefore be important for future investigations to span across different units of analyses, including genes, circuits, physiology, and paradigms and provide cross-modal and measurement validation of the factors derived here. Accordingly, performance-based assessment should be developed and included in the process of assessing the different social domains to minimize the known biases and limitations related to the subjective reports. It will also be important to further explore the invariance of social processes factor structure reported here across informants including self-report and teacher/clinician report. Finally, although given the sample size the potential of subject overlap across the data sets to influence findings is minimal, it is important to consider findings reported here in light of this limitation.
Findings presented here have several important theoretical and clinical implications. The purpose of this study was not to arrive at the best fitting general SRS factor solution, and therefore alternative factor structures, especially as it relates to the structure of ASD, are possible. Rather, our focus was to evaluate the ability of SRS, a widely used quantitative measure, to approximate RDoC social sub-constructs and we believe that resultant excellent statistical fit and robustness of the structure across age, gender, verbal ability and clinical status suggest that this aim was achieved thus demonstrating promise of SRS for capturing important RDoC social constructs albeit in a somewhat imprecise way. Therefore, factors derived here present a valuable resource for mapping RDoC constructs across both research and clinical contexts thus providing an important bridge towards initial testing of the explanatory power of the RDoC framework. In addition, a range of robust big data sets that span normative and clinical populations, and include multiple units of analyses, are currently accessible enabling further exploration of the clinical and biological validity of the derived social constructs. Crucial next step for illustrating the potential utility of the RDoC social processes constructs and subconstructs for clinical and etiological research will be to utilize person-centered approaches in order to identify subgroups of individuals with unique constellations of strengths and weakness across distinct components of social processing. Finally, our findings highlight crucial areas for the development of novel, dedicated dimensional measures of social processing.
Supplementary Material
Acknowledgments
The study was supported by grant R03MH111846–01 (Drs. Hardan and Jo) by the National Institute of Mental Health.
Drs. Uljarević, Jo, and Frazier served as the statistical experts for this research.
Glossary
- RH
RDoC and the Social Responsiveness Scale
Footnotes
Disclosure: Dr. Uljarević has received support from the Discovery Early Career Researcher Award from the Australian Research Council (DE180100632). Drs. Frazier, Phillips, Jo, and Hardan and Ms. Littlefield report no biomedical financial interests or potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Mirko Uljarević, Stanford University, CA..
Thomas W. Frazier, Autism Speaks, New York, NY..
Jennifer M. Phillips, Stanford University, CA..
Booil Jo, Stanford University, CA..
Sandy Littlefield, Stanford University, CA..
Antonio Y. Hardan, Stanford University, CA..
References:
- 1.Cotter J, Granger K, Backx R, Hobbs M, Looi CY, Barnett JH4. Social cognitive dysfunction as a clinical marker: A systematic review of meta-analyses across 30 clinical conditions. Neurosci Biobehav Rev. 2018;84:92–99. [DOI] [PubMed] [Google Scholar]
- 2.Happé F, Frith U. Annual research review: Towards a developmental neuroscience of atypical social cognition. J Child Psychol Psychiatry. 2014;55(6):553–7. [DOI] [PubMed] [Google Scholar]
- 3.Henry JD, von Hippel W, Molenberghs P, Lee T, Sachdev PS. Clinical assessment of social cognitive function in neurological disorders. Nat Rev Neurol. 2016;12(1):28–39. [DOI] [PubMed] [Google Scholar]
- 4.Kennedy DP, Adolphs R. The social brain in psychiatric and neurological disorders. Trends Cogn Sci. 2012;16(11):559–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dickerson BC. Dysfunction of social cognition and behavior. Continuum (Minneap Minn). 2015;21(3):660–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dirks MA, Treat TA, Weersing VR. Integrating theoretical, measurement, and intervention models of youth social competence Clin Psychol Rev. 2007;27:327–347. [DOI] [PubMed] [Google Scholar]
- 7.Fett AK, Viechtbauer W, Dominguez MD, Penn DL, van Os J, Krabbendam L. The relationship between neurocognition and social cognition with functional outcomes in schizophrenia: a meta-analysis Neurosci Biobehav Rev. 2011;35:573–588. [DOI] [PubMed] [Google Scholar]
- 8.Huber L, Plötner M, Schmitz J. Social competence and psychopathology in early childhood: a systematic review [published online April 10, 2018]. Eur Child Adolesc Psychiatry. doi: 10.1007/s00787-018-1152-x [DOI] [PubMed] [Google Scholar]
- 9.Vivanti G, Prior M, Williams K, Dissanayake C. Predictors of outcomes in Autism Intervention: Why don’t we know more? Frontiers in Pediatrics. 2014;2:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leekam SR. Social cognitive impairment and autism: What are we trying to explain? Philosophical Transactions of the Royal Society of London Series B Biological Sciences. 2016;371(1686):20150082–20150088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cuthbert B. The RDoC framework: facilitating transition from ICD/DSM to dimensional approaches that integrate neuroscience and psychopathology. World Psychiatry. 2014;13(1):28–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maj M. Why the clinical utility of diagnostic categories in psychiatry is intrinsically limited and how we can use new approaches to complement them. World Psychiatry. 2018;17(2):121–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Insel TR. The challenge of translation in social neuroscience: a review of oxytocin, vasopressin, and affiliative behavior. Neuron. 2010;65:768–779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dunbar RI. The social brain hypothesis and its implications for social evolution Ann Hum Biol. 2009;36:562–572. [DOI] [PubMed] [Google Scholar]
- 15.Adolphs R. The social brain: neural basis of social knowledge. Annu Rev Psychol. 2009;60:693–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Porcelli S, Van Der Wee N, van der Werff S, et al. Social brain, social dysfunction and social withdrawal. Neurosci Biobehav Rev. 2018;S0149–7634(18);30195–7. [DOI] [PubMed] [Google Scholar]
- 17.Van Overwalle F. Social cognition and the brain: a meta-analysis. Hum Brain Mapp. 2009;30(3):829–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Advisory Mental Health Council Workgroup on Tasks and Measures for Research Domain Criteria. Behavioral Assessment Methods for RDoC Constructs. Bethesda, MD; 2016. [Google Scholar]
- 19.Constantino JN, Gruber CP. The Social Responsiveness Scale. Los Angeles, CA: Western Psychological Services;2005. [Google Scholar]
- 20.Constantino JN, & Gruber CP. Social responsive scale manual (2nd ed., SRS-2). Los Angeles, CA: Western Psychological Services;2012. [Google Scholar]
- 21.Wigham S, McConachie H, Tandos J, Le Couteur AS. The reliability and validity of the Social Responsiveness Scale in a UK general child population. Res Dev Disabil.2012;33(3):944–50. [DOI] [PubMed] [Google Scholar]
- 22.Bölte S. Brief Report: the Social Responsivenes s Scale for Adults (SRS-A): initial results in a German cohort. J Autism Dev Disord. 2012;42(9):1998–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kamio Y, Inada N, Moriwaki A, Kuroda M, Koyama T, et al. Quantitative autistic traits ascertained in a national survey of 22 529 Japanese schoolchildren. Acta Psychiatrica Scandinavica. 2013;128:45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Frazier TW, Ratliff KR, Gruber C, Zhang Y, Law PA, Constantino JN. Confirmatory factor analytic structure and measurement invariance of quantitative autistic traits measured by the Social Responsiveness Scale-2. Autism. 2014;18(1):31–44. [DOI] [PubMed] [Google Scholar]
- 25.Constantino JN, Todd RD. Genetic structure of reciprocal social behavior. Am J Psychiatry. 2000; 157:2043–2045. [DOI] [PubMed] [Google Scholar]
- 26.Constantino JN, Gruber CP, Davis S, Hays S, Passante N, Przybeck T. The factor structure of autistic traits. J Child Psychol Psychiatry. 2004; 45:719–726. [DOI] [PubMed] [Google Scholar]
- 27.Duku E, Vaillancourt T, Szatmari P, Georgiades S, Zwaigenbaum L, Smith IM, et al. Investigating the measurement properties of the Social Responsiveness Scale in preschool children with autism spectrum disorders. J Autism Dev Disord. 2013; 43: 860–868. [DOI] [PubMed] [Google Scholar]
- 28.Gau SFS, Liu LT, Wu YY, Chiu YN, Tsai WC. Psychometric properties of the Chinese version of the Social Responsiveness Scale. Res Autism Spectr Disord. 2013; 7: 349–360. [Google Scholar]
- 29.Nelson AT, Lopata C, Volker MA, Thomeer ML, Toomey JA, Dua E. Exploratory factor analysis of SRS-2 teacher ratings for youth with ASD. J Autism Dev Disord. 2016; 46:2905–2915 [DOI] [PubMed] [Google Scholar]
- 30.Curran PJ, Hussong AM. Integrative data analysis: the simultaneous analysis of multiple data sets. Psychol Methods. 2009;14(2):81–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hussong AM, Curran PJ, Bauer DJ. Integrative Data Analysis in Clinical Psychology Research. Annu Rev Clin Psychol. 2013;9:61–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Asparouhov T, Muthén B. Exploratory structuralequation modeling. Struct Equ Model. 2009;16:397–438. [Google Scholar]
- 33.Marsh HW, Morin AJS, Parker P, Kaur G. Exploratory structural equation modeling: an integration of the best features of exploratory and confirmatory factor analysis. Annu Rev Clin Psychol; 2014;10:85–110. [DOI] [PubMed] [Google Scholar]
- 34.Kilford EJ, Garrett E, Blakemore SJ. The development of social cognition in adolescence: An integrated perspective. Neurosci Biobehav Rev. 2016;70:106–120. [DOI] [PubMed] [Google Scholar]
- 35.Lai MC, Lombardo MV, Pasco G, Ruigrok ANV, Wheelwright SJ, Sadek SA, et al. A Behavioral Comparison of Male and Female Adults with High Functioning Autism Spectrum Conditions. PLOS ONE. 2011;6(6):e20835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hus V, Bishop S, Gotham K, Huerta M, Lord C. et al. Factors influencing scores on the social responsiveness scale. J Child Psychol Psychiatry. 2013;54:216–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alexander LM, Escalera J, Ai L, et al. An open resource for transdiagnostic research in pediatric mental health and learning disorders. Sci Data. 2017;4:170181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fischbach GD, Lord C. The Simons Simplex Collection: a resource for identification of autism genetic risk factors. Neuron. 2010;68(2):192–5. [DOI] [PubMed] [Google Scholar]
- 39.Geschwind DH, Sowinski J, Lord C, Iversen P, Shestack J, Jones P, Ducat L, Spence SJ, AGRE Steering Committee. The autism genetic resource exchange: a resource for the study of autism and related neuropsychiatric conditions. Am J Hum Genet. 2001;69:463–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Muthén LK, Muthén BO. Mplus User’s Guide. et al. Los Angeles, CA: Muthén & Muthén; 2007. [Google Scholar]
- 41.Asparouhov T, Muthén B, Morin AJS. Bayesian Structural Equation Modeling with cross-loadings and residual covariances: comments on Stromeyer et al et al. J Manag. 2015;41:1561–1577. [Google Scholar]
- 42.Corp IBM. IBM SPSS statistics for windows (Version 24.0) [Computer Program]. Armonk, NY: IBM Corp; 2016. [Google Scholar]
- 43.Efron B, Tibshirani R. An introduction to the bootstrap. Boca Raton, FL: Chapman & Hall/CRC; 1993. [Google Scholar]
- 44.Sedgewick F, Hill V, Yates R, Pickering L, Pellicano E. Gender differences in the social motivation and friendship experiences of autistic and non-autistic adolescents. J Autism Dev Disord. 2016; 46:1297–1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Christov-Moore L, Simpson EA, Coudé G, Grigaityte K, Iacoboni M, Ferrari PF. Empathy: Gender effects in brain and behavior. Neurosci Biobehav Rev. 2014; 46:604–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Herba C, Phillips M. Annotation: Development of facial expression recognition from childhood to adolescence: behavioural and neurological perspectives. J Child Psychol Psychiatry. 2004; 45(7):1185–1198. [DOI] [PubMed] [Google Scholar]
- 47.McCoy TH, Yu S, Hart KL, et al. High Throughput Phenotyping for Dimensional Psychopathology in Electronic Health Records. Biol Psychiatry. 2018; 83(12):997–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Iacono WG. Achieving Success with the Research Domain Criteria (RDoC): Going beyond the Matrix. Psychophysiology. 2016; 53(3):308–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gosling SD, Rentfrow PJ, Swann WB. A very brief measure of the Big-Five personality domains. J Res Pers. 2003;37(6):504–528. [Google Scholar]
- 50.Strauss GP, Nuñes A, Ahmed AO, Barchard KA, Granholm E, Kirkpatrick B, et al. The latent structure of negative symptoms in schizophrenia. JAMA Psychiatry. 2018; 75(12):1271–1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Uljarević M, Vivanti G, Leekam SR, Hardan AY. Challenges to the social motivation theory of autism: The dangers of counteracting an imprecise theory with even more imprecision. Behavioral and Brain Sciences. 2019. [Google Scholar]
- 52.Green MF, Penn DL, Bentall R, Carpenter WT, Gaebel W, Gur RC, et al. Social Cognition in Schizophrenia: An NIMH Workshop on Definitions, Assessment, and Research Opportunities. Schizophr Bull. 2008;34(6):1211–1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Green MF, Horan WP. Social Cognition in Schizophrenia. Curr Dir Psychol Sci. 2010;19(4):243–8. [Google Scholar]
- 54.Happé F, Cook JL, Bird G. The Structure of Social Cognition: In(ter)dependence of Sociocognitive Processes. Annu Rev Psychol. 2017;68:243–267. [DOI] [PubMed] [Google Scholar]
- 55.Pallathra AA, Calkins ME, Parish-Morris J, Maddox BB, Perez LS, Miller J, et al. Defining behavioral components of social functioning in adults with autism spectrum disorder as targets for treatment. Autism Res. 2018;11(3):488–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wallace GL, Dudley K, Anthony L, Pugliese CE, Orionzi B, Clasen L, et al. Divergence of Age-Related Differences in Social-Communication: Improvements for Typically Developing Youth but Declines for Youth with Autism Spectrum Disorder. J Autism Dev Disord. 2017;47(2):472–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Green MF, Horan WP, Lee J. Social cognition in schizophrenia. Nat Rev Neurosci. 2015;16(10):620–31. [DOI] [PubMed] [Google Scholar]
- 58.Rutter M, Bailey A, Lord C. The social communication questionnaire manual. Los Angeles, CA: Western Psychological Services; 2003. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.