Abstract
Background
Globally obstetric anesthesia is being done under spinal and epidural than general anesthesia (GA) for most caesarean sections (CSs). This is because GA is associated with failed endotracheal intubation and aspiration of gastric contents. Eventhough general anesthesia is the fastest method for anesthetizing a category 1 cesarean section, it is associated with increased maternal mortality and morbidity. Spinal anesthesia is the preferred regional technique for cesarean section but failure sometimes occurs. To minimize the time factor of spinal anesthesia as well as to avoid the side effects of general anesthesia ‘rapid sequence spinal ‘(RSS) has developed as a novel approach in cases of category one cesarean sections.
Methods
The study was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) protocol. Search engines like PubMed through HINARI, Cochrane database and Google Scholars were used to find high-level evidences that help to draw appropriate conclusions.
Discussion
Neuraxial anesthetic techniques have several advantages which include low risk of aspiration and failed intubation, avoidance of central nervous system (CNS) and respiratory depressant drugs, the ability to maintain a wakeful state of mother enjoying the experience of delivery of baby and also lower incidence of blood loss. ‘Rapid sequence spinal’ described to minimize anesthetic time. This consists of a no-touch spinal technique, consideration of omission of the spinal opioid, limiting spinal attempts, allowing the start of surgery before full establishment of the spinal block, and being prepared for conversion to general anesthesia if there are delays or problems. To do rapid sequence spinal anesthesia safely and timely, cooperative work is mandatory with good team relation for those simultaneous and necessary tasks.
Conclusion
The choice of anesthetic in Cesarean section has long been recognized as one of prime importance, because there are two lives to safeguard instead of one. A balance must be struck between the anesthetic dictated by the general condition of the mother and that suited to the needs of the fetal respiratory system.
Keywords: Rapid sequence spinal anesthesia, Cesarean section, Difficult intubation, Fetal distress
Rationale.
-
➢
To reduce general anesthetic related maternal and neonatal morbidity and mortality
-
➢
To identify and give evidence based anesthetic services for pregnant mothers coming for cesarean delivery
-
➢
To have best possible maternal and neonatal outcome.
1. Background
Internationally, obstetric anesthesia guidelines recommend spinal and epidural over general anesthesia (GA) for most caesarean sections (CSs). The primary reason for recommending regional blocks is the risk of failed endotracheal intubation and aspiration of gastric contents. General anesthesia is the fastest method for anesthetizing a category 1 cs associated with increased maternal mortality and morbidity and Spinal anesthesia is the preferred regional technique for cs but failure sometimes occurs. While regional anesthesia or general anesthesia are both acceptable for cesarean delivery, the use of general anesthesia has become less common in the past few decades. While most cesarean sections are performed under regional anesthesia, general anesthesia should always be considered as it is occasionally necessary [1,2]∗∗,∗∗.
To minimize the time factor of spinal anesthesia as well as to avoid the side effects of general anesthesia ‘rapid sequence spinal ‘(RSS) has developed as a novel approach in cases of category one cesarean sections. Neuraxial anesthetic techniques have several advantages which include low risk of aspiration and failed intubation, avoidance of central nervous system and respiratory depressant drugs, the ability to maintain a wakeful state of mother enjoying the experience of delivery of baby, lower incidence of blood loss, early ambulation and low risk of DVT, early return of gastrointestinal function and short hospital stay length. Amongst the various neuraxial techniques, spinal anesthesia has been popular for cesarean delivery because of ease of administration, effectiveness and faster onset providing dense motor block with minimal drug toxicity to mother and to fetus due to limited placental transfer [1,2]∗∗,∗∗.
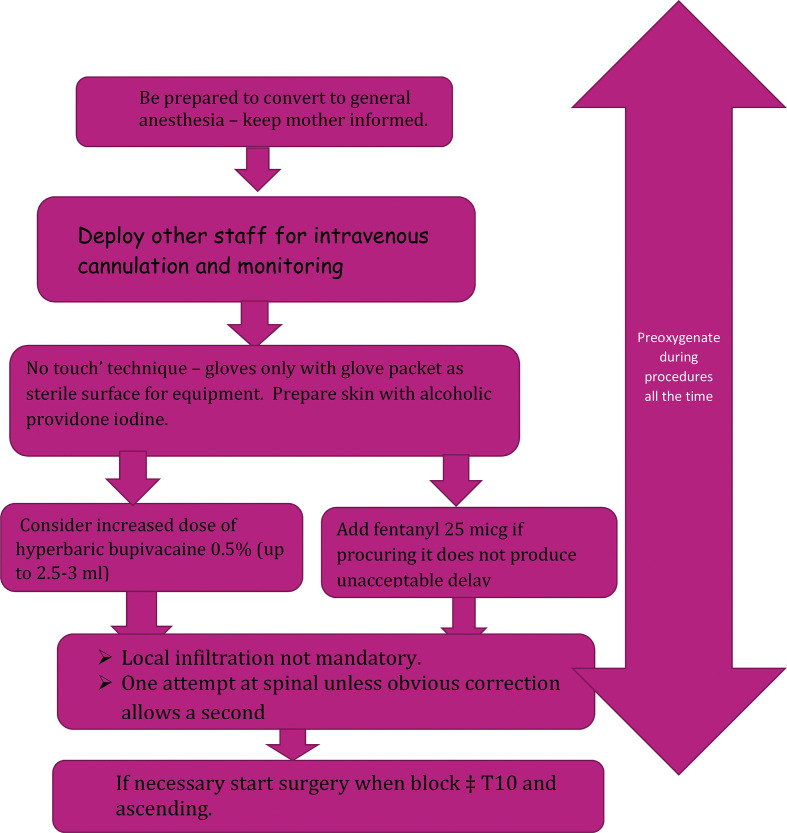
The rapid sequence spinal (RSS), first described in 2003, consists of measures aimed at reducing the time to establish spinal anesthesia in urgent obstetric cases and We all know that category-1 caesarean sections are a challenge and the anesthetic we provide has to be safe, effective and fast. The concept of rapid sequence spinal (RSS) evolved as an alternative to both emergency general anesthesia, which carries risks of several fatal complications and also the conventional spinal anesthesia, which is time consuming. It is actually a conjugation of the two which is based on the principles of performing as fast as possible carrying out only the absolute essential steps thereby cutting the permissible time and on the other hand, limiting the attempts of administering the block or even abandoning it in favor of other alternative techniques as is done during rapid sequence induction including multiple drug exposure during general anesthesia [3,4]∗,∗(see Fig. 1 ).
Fig. 1.
Flow diagram, Rapid sequence Spinal Anesthesia.
2. Justifications
The choice of anesthetic in Cesarean section has long been recognized as one of prime importance, because there are two lives to safeguard instead of one. A balance must be struck between the anesthetic dictated by the general condition of the mother and that suited to the needs of the fetal respiratory system because fetal distress is one of the indications to fasten the delivery process and the diagnosis of fetal distress is based on the fetal heart beats, whether they are fast, slow, irregular and whether there is meconium present during delivery. There have been many reasons to develop and adopt rapid sequence spinal anesthesia for category 1 cesarean section and this can be generally justified by weighing risk and benefits of general and spinal anesthesia. Clinical investigations and reviews done in different countries with time period showed, the death due to g anesthesia related death is high even though spinal anesthesia related deaths decreased [[5], [6], [7]]∗,∗,∗. According to NAP3 (national audit project 3) with met analysis of 141 trials there is 30% reduction of mortality by using CNB compared with general anesthesia [8]∗. To have general understandings of the urgency of cesarean section, every team member have to know the classification. This category was depending on the fetal and maternal conditions for timely operative delivery [9]∗∗.
Category1-requiring immediate delivery within 30 min-a threat to maternal or fetal life (major hemorrhage, profound and persistent fetal bradycardia, prolapsed cord, shoulder dystocia. Category 2-requiring urgent delivery-maternal or fetal compromise that is not immediately life threatening.
Category 3-requiring early delivery-but no maternal or fetal compromise.
Category 4-at a time suited to the woman maternity staff.
Generally those category 1 cesarean sections should be indicated and recommended for rapid sequence spinal (RSS) unless there is absolute contraindication.
3. Methods
This study was carried out in accordance with the Preferred reporting Items for Systematic Reviews and Meta-Analyses. A computerized systematic search of the PubMed, Google Scholar, and Science Direct databases were used to find articles. Prospective observational, interventional studies, meta-analysis, systematic review and audit studies were included in the review using the following MeSH terms: (Spinal Anesthesia OR Neonatal outcome OR Maternal complications) AND Cesarean section AND Anesthesia AND (Rapid sequence spinal Anesthesia OR Rapid sequence Induction OR Failed obstetric intubation) AND perioperative Cardio-respiratory adverse events of neonate. Only those articles written in English language were considered for this review. Furthermore, after comprehensive and in-depth appraisal of literature, evaluation of quality was conducted by categorize them into level 1 (∗ Meta-analysis, systematic review, randomized control trial) level 2 (∗∗ Well designed cohort study) and level 3 (∗∗∗ case reports, commentaries, and expert opinions). Finally, conclusion has drawn based the level of evidences and class of recommendation.
4. Discussion
Difficult air way and intubation risk is more profound in pregnancy and obesity almost double risk when it is compared with other normal patients as it is supported by the systematic review [10]∗. The risk is high in pregnancy because of pregnancy related physiologic and anatomic changes such as large breast, edematous air way and frequent hypoxia, which is due to limited diaphragmatic excursion due to gravid uterus, high oxygen consumption and high risk of aspiration to have standard laryngoscopy by repeated attempts. As this was supported by many evidences previously that here are still risk of difficult intubation, difficult laryngoscopy, failed intubation, regurgitation during intubation trials and aspiration of gastric contents during emergency cesarean section under general anesthesia [11]∗∗. Due to these all factors, difficult and failed intubation after general anesthesia are found to be major contributing factors for the anesthesia related maternal complications [12]. As it is shown in multicenter observational study done on 895 women, the incidence of hypoxemia was 19% and it was significantly associated with difficult and failed intubation during general anesthesia for emergency cesarean section [13]∗∗. Poor airway assessment contributed to poor airway outcomes because of omission, incomplete assessment or a failure to alter the airway management technique in response to findings at assessment. Studies from difficult air way society of united kingdom recommended that, assessment to predict both potential airway difficulty and aspiration risk were equally important and this all were due to inadequate time during category 1 emergency cesarean section cases [14,15]∗.
In addition to this, when we see risk of aspiration during general anesthetic where the risk is higher than normal, consideration should be given to minimizing gastric volume and raising pH of gastric contents and protecting the airway through Rapid Sequence Induction (RSI). Morbidity will arise where the risk of aspiration is not taken into account, the ‘no-risk’ assessment is incorrect or the elements of RSI fail to protect the airway. Cricoid force applied as part of RSI may itself cause problems with intubation and oxygenation, particularly when applied force is excessive or incorrectly applied as it is recommended by clinical reviews of national audit project of royal colleges of anesthetists [[16], [17], [18]]∗.
As it has been described earlier, there is limited time for detail preoperative assessment to predict or stratify the risks and benefits of the procedure. During the brief preoperative assessment, it is must to have consent for all procedures and possible events probably happening in the theatre; such as attempt of rapid sequence spinal anesthesia, urgency of the situation, aims to avoid GA, possibility of conversion to GA if the block fails and mild discomfort/pain during the operation [19]∗∗. So consent should be taken for both spinal and general anesthesia during preoperative patient visit.
The main controversies which have been argued in different centers and literatures was time of anesthesia, time of surgical readiness and emergence; which were found to be significantly shorter during rapid sequence spinal anesthesia than rapid sequence induction of General anesthesia but the incision to delivery time and APGAR score were not significantly different between groups [3,20]∗,∗. Conversely the decision to delivery interval was longer during spinal anesthesia but the low APGAR score and other worse perinatal outcomes were more associated with general anesthesia [[21], [22], [23]]∗∗,∗∗,∗∗. There is study showing longer time of decision to delivery interval than the recommended time (30 min) for category 1-cesarean section and this was more associated with time taken to collect surgical materials), time spent between decision and arrival to the operation theater and time taken from arrival at the operation theater to the immediate start of skin incision [24]∗∗. Neonatal morbidity have been compared for general and spinal anesthesia during emergency cesarean section and the General anesthesia was more associated with low 1-min APGAR score, longer time of hospitalization, higher incidence of morbidity, and lower umbilical blood pH [25]∗.
22 studies from Cochrane review showed that there was significant decrement of blood loss and post-operative pain relief during regional anesthesia than general anesthesia even though other parameters such as recovery times, effects on breastfeeding, effects on the mother-child relationship and length of time before mother feels well enough to care for her baby are not considered [26]∗. Another study showed, improved survival in patients randomized to neuraxial blockade and, found reductions in risk of venous thromboembolism, myocardial infarction, bleeding complications, pneu-monia, respiratory depression, and renal failure [27]∗.
It is known that spinal anesthesia is not without risk eventhough it has been considered for urgent cesarean section and failed block was found to be 6% [28]∗∗∗. Other potential complications of spinal anesthesia were hypotension, backache, headache, bradycardia, nausea and vomiting and urinary retention eventhough its simplicity and absence of severe complications for more than >50% of patients [29] ∗∗.
Nowadays we are suffering with corona virus (covid-19) pandemic. In addition to limited time to assess the airways of pregnant mothers decided for emergent cesarean section with corona virus confirmed, there is risk of disease transmission to do so. As it has been mentioned about higher rates of difficult airway during general anesthesia for cesarean section, the corona virus transmission is very high during any aerosol procedure and the rapid sequence spinal anesthesia is becoming new and novel approach for those patients indicated for cesarean section with category1 indication [30]∗∗. This disease is associated with wide ranges of respiratory compromization which could potentially be affected or aggravated by the drugs during general anesthesia and it is recommended to proceed with rapid sequence spinal anesthesia to prevent the mentioned problems [31]∗.
5. Areas of controversy
Great controversy is timing to attain rapid sequence spinal anesthesia when compared with rapid sequence general anesthesia because of there are some factors for inability to attain rapid sequence spinal anesthesia at intended time. One clinical observational study done in British and other RCT done in India showed that the average time to attain adequate block during spinal anesthesia and optimal time to start surgery in general anesthesia was 6–11min and 5–10 min respectively by having same time duration from decision to arrival of the patient to the theatre, which can vary due to different factors [[32], [33], [34]]∗∗,∗,∗. However this timing cannot be taken in to consideration when we think about risks of unanticipated difficult airway, high risk of aspiration and pulmonary damage, delayed awakening, multidrug exposure of the fetus and other potential morbidities during general anesthesia [[35], [36], [37]]∗∗,∗,∗.
The other controversy is risk of infection compared between normal spinal anesthetic technique with standard antiseptic technique and rapid sequence spinal with single antiseptic application. 3690 patients were received rapid sequence spinal anesthesia with single chlorhexidine in alcohol application with time period between 1991 and 1999 showed no infection so it is safe to practice for those conditions [38]∗. Chlorhexidine in alcohol preparation is not available in the study area. However alcoholic providone iodine has comparable efficacy with chlorhexidine 0.5% in alcohol if used as antiseptic solution for neuraxial blockade and surgical site skin preparation [39,40]∗∗,∗.
6. Conclusion
Neuraxial anesthetic techniques have several advantages which include low risk of aspiration and failed intubation, avoidance of central nervous system (CNS) and respiratory depressant drugs, the ability to maintain a wakeful state of mother enjoying the experience of delivery of baby and also lower incidence of blood loss. ‘Rapid sequence spinal’ described to minimize anesthetic time. This consists of a no-touch spinal technique, consideration of omission of the spinal opioid, limiting spinal attempts, allowing the start of surgery before full establishment of the spinal block, and being prepared for conversion to general anesthesia if there are delays or problems. To do rapid sequence spinal anesthesia safely and timely, cooperative work is mandatory with good team relation for those simultaneous and necessary tasks. The task of IV cannulation most of the time is experienced midwife but anybody from the team members can do so to avoid unnecessary delay. Regarding with dose of local anesthetics, it is recommended that better to use slightly higher doses than usual which is 3 ml of 0.5% hyperbaric bupivacaine or 2.5 ml of 0.5% hyperbaric bupivacaine with 25 μg fentanyl if it readily available. Finally it is possible to convert to general anesthesia if spinal block fails without taking additional time for preoxygenation and general anesthetic preparation because the client was on 100% oxygen as it is shown on flow diagram of the tasks and procedures of it and the drugs were already prepared.
7. Recommendation
Awareness should be created among the team members i.e. obstetric residents, obstetricians, midwifes and assistants in addition to Anesthetists’ should be training about its essential steps and overall objectives.
Department of anesthesiology clinical coordinator and hospital clinical director should be noted for timely and continuous supply of appropriate size and functional spinal needles to avoid repeated attempts during the procedure. Anesthetists should prepare all general anesthetic equipments and drugs at all times in the obstetric operation room. The team should have clear indication for rapid sequence spinal anesthesia and it must never be tried by anesthetic trainees or students.
Ethical approval
The ethical approval was obtained from ethical review committee of University of Gondar with reference uog/102/2019.
Sources of funding
University of Gondar.
Author contribution
This work was carried out in collaboration among all authors. A.F. Agegnehu contributed to the conception, the review and interpreted the literatures based on the level of evidence. A.H. Gebregzi and N.S. Endalew in reviewing preparation of the manuscript. All authors participate in preparation and critical review of the manuscripts. In addition, all authors read and approved the manuscript.
Conflict of interest statement
There is no conflict of interest among the participants of the review article.
Guarantor
Abatneh Feleke Agegnehu (A.F. Agegnehu), Amare Hailekiros Gebregzi (A.H. Gebregzi), Nigussie Simeneh Endalew (N·S. Endalew).
Research registration unique identifying number (UIN)
Reviewregistry955.
Acknowledgments
We would like to acknowledge the Department of Anesthesia for all their support with the study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijso.2020.08.013.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Kinsella S., Girgirah K., Scrutton M. Rapid sequence spinal anaesthesia for category-1 urgency caesarean section: a case series. Anaesthesia. 2010;65(7):664–669. doi: 10.1111/j.1365-2044.2010.06368.x. [DOI] [PubMed] [Google Scholar]
- 2.Algert C.S., Bowen J.R., Giles W.B., Knoblanche G.E., Lain S.J., Roberts C.L. Regional block versus general anaesthesia for caesarean section and neonatal outcomes: a population-based study. BMC Med. 2009;7(1):1–7. doi: 10.1186/1741-7015-7-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhattacharya S., Ghosh S., Chattopadhya U., Saha D., Bisai S., Saha M. Rapid sequence spinal anesthesia versus general anesthesia: a prospective randomized study of anesthesia to delivery time in category-1 caesarean section. Journal of Obstetric Anaesthesia and Critical Care. 2016;6(2):75. [Google Scholar]
- 4.Chiron B., Laffon M., Ferrandiere M., Pittet J.-F., Marret H., Mercier C. Standard preoxygenation technique versus two rapid techniques in pregnant patients. Int J Obstet Anesth. 2004;13(1):11–14. doi: 10.1016/S0959-289X(03)00095-5. [DOI] [PubMed] [Google Scholar]
- 5.Mhyre J.M., Riesner M.N., Polley L.S., Naughton N.N. A series of anesthesia-related maternal deaths in Michigan, 1985–2003. Anesthesiology: The Journal of the American Society of Anesthesiologists. 2007;106(6):1096–1104. doi: 10.1097/01.anes.0000267592.34626.6b. [DOI] [PubMed] [Google Scholar]
- 6.Sobhy S., Zamora J., Dharmarajah K., Arroyo-Manzano D., Wilson M., Navaratnarajah R., et al. Anaesthesia-related maternal mortality in low-income and middle-income countries: a systematic review and meta-analysis. The Lancet Global Health. 2016;4(5):e320–e327. doi: 10.1016/S2214-109X(16)30003-1. [DOI] [PubMed] [Google Scholar]
- 7.Esteves-Pereira A.P., Deneux-Tharaux C., Nakamura-Pereira M., Saucedo M., Bouvier-Colle M.-H., Leal MdC. Caesarean delivery and postpartum maternal mortality: a population-based case control study in Brazil. PloS One. 2016;11(4) doi: 10.1371/journal.pone.0153396. e0153396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thomas G., Cook T. The United Kingdom national audit projects: a narrative review. South Afr J Anaesth Analg. 2016;22(2):38–45. [Google Scholar]
- 9.Maneschi F., Biccirè D., Santangelo G., Perrone S., Scaini A., Cosentino C. Implementation of the four-category classification of cesarean section urgency in clinical practice. A prospective study. Gynecol Obstet Invest. 2017;82(4):371–375. doi: 10.1159/000449159. [DOI] [PubMed] [Google Scholar]
- 10.Workeneh S.A., Gebregzi A.H., Denu Z.A. Magnitude and predisposing factors of difficult airway during induction of general anaesthesia. Anesthesiology research and practice. 2017;2017 doi: 10.1155/2017/5836397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McDonnell N., Paech M., Clavisi O., Scott K., Group A.T. Difficult and failed intubation in obstetric anaesthesia: an observational study of airway management and complications associated with general anaesthesia for caesarean section. Int J Obstet Anesth. 2008;17(4):292–297. doi: 10.1016/j.ijoa.2008.01.017. [DOI] [PubMed] [Google Scholar]
- 12.Alanoğlu Z., Karadağ Erkoç S., Yıldırım Güçlü Ç., Orbey Meço B.C., Baytaş V., Selvi Can Ö., et al. Challenges of obstetric anesthesia: difficult laryngeal visualization. Acta Clin Croat. 2016;55(Supplement 1):68–72. [PubMed] [Google Scholar]
- 13.Bonnet M.-P., Mercier F.J., Vicaut E., Galand A., Keita H., Baillard C., et al. Incidence and risk factors for maternal hypoxaemia during induction of general anaesthesia for non-elective Caesarean section: a prospective multicentre study. Br J Anaesth. 2020 doi: 10.1016/j.bja.2020.03.010. [DOI] [PubMed] [Google Scholar]
- 14.Cook T., Woodall N., Frerk C. 4th National Audit Project of The Royal College of Anaesthetists and The Difficult Airway Society. Reports and Findings; 2011. Major complications of airway management in the United Kingdom; pp. 86–95. [DOI] [PubMed] [Google Scholar]
- 15.Higgs A., McGrath B., Goddard C., Rangasami J., Suntharalingam G., Gale R., et al. Guidelines for the management of tracheal intubation in critically ill adults. Br J Anaesth. 2018;120(2):323–352. doi: 10.1016/j.bja.2017.10.021. [DOI] [PubMed] [Google Scholar]
- 16.Sharp L.M., Levy D.M. Rapid sequence induction in obstetrics revisited. Current Opinion in Anesthesiology. 2009;22(3):357–361. doi: 10.1097/aco.0b013e3283294c4a. [DOI] [PubMed] [Google Scholar]
- 17.de Souza D.G., Doar L.H., Mehta S.H., Tiouririne M. Aspiration prophylaxis and rapid sequence induction for elective cesarean delivery: time to reassess old dogma? Anesth Analg. 2010;110(5):1503–1505. doi: 10.1213/ANE.0b013e3181d7e33c. [DOI] [PubMed] [Google Scholar]
- 18.Morris J., Cook T. Rapid sequence induction: a national survey of practice. Anaesthesia. 2001;56(11):1090–1115. doi: 10.1046/j.1365-2044.2001.01962.x. [DOI] [PubMed] [Google Scholar]
- 19.Jigajinni S, Rajala B, El Sharawi N. The rapid sequence spinal for category 1 caesarean section. [DOI] [PubMed]
- 20.Gurvani R., Chandrakar D.V. Rapid sequence spinal anesthesia vs general anesthesia for category-I urgency caesarean section. International Journal of Innovative Research in Medical Science. 2018;3(1) 1608 to 11- to 11. [Google Scholar]
- 21.Hein A., Thalen D., Eriksson Y., Jakobsson J.G. The decision to delivery interval in emergency caesarean sections: impact of anaesthetic technique and work shift. F1000Research. 2017;6 doi: 10.12688/f1000research.13058.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dunn C.N., Zhang Q., Sia J.T., Assam P.N., Tagore S., Sng B.L. Evaluation of timings and outcomes in category-one caesarean sections: a retrospective cohort study. Indian J Anaesth. 2016;60(8):546. doi: 10.4103/0019-5049.187782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sadiq A.M., Al Aasam S.R., Rahman A., Hassan A.N., Yousif M.G. The effect of type of anesthesia on mother and neonatal health during Cesarean section. J Adv Pharm Educ Res. 2018;8(4):117. [Google Scholar]
- 24.Temesgen M.M., Gebregzi A.H., Kasahun H.G., Ahmed S.A., Woldegerima Y.B. Evaluation of decision to delivery time interval and its effect on feto-maternal outcomes and associated factors in category-1 emergency caesarean section deliveries: prospective cohort study. BMC Pregnancy Childbirth. 2020;20(1):1–11. doi: 10.1186/s12884-020-2828-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Edipoglu I.S., Celik F., Marangoz E.C., Orcan G.H. Effect of anaesthetic technique on neonatal morbidity in emergency caesarean section for foetal distress. PloS One. 2018;13(11) doi: 10.1371/journal.pone.0207388. e0207388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khan Z.H., Eftekhar N., Barrak R.S. General versus spinal anesthesia during caesarean section; A narrative review. Archives of Anesthesiology and Critical Care. 2019;5(1):18–21. [Google Scholar]
- 27.Anderson A., McNaught C., MacFie J., Tring I., Barker P., Mitchell C. Randomized clinical trial of multimodal optimization and standard perioperative surgical care. Br J Surg. 2003;90(12):1497–1504. doi: 10.1002/bjs.4371. [DOI] [PubMed] [Google Scholar]
- 28.Halimi N.N., Basit M., Waqas H.M., Khan M.J., Ilyas M. To determine the frequency of failed spinal anaesthesia during cesarean section. Pak J Surg. 2020;36(1):71–74. [Google Scholar]
- 29.Kazom S.N., Kareem S.M. Complication of spinal anesthesia in caesarean section. Al-Qadisiyah Medical Journal. 2019;15(2):93–103. [Google Scholar]
- 30.Varandas J.S., Dias R., Mendes A.B., Lages N., Machado H. New indication for an old anesthetic technique: could we consider now rapid sequence spinal anesthesia in a COVID-19 time? Reg Anesth Pain Med. 2020 doi: 10.1136/rapm-2020-101572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dabrowska D., Lock G.J. Staying ahead of the curve: modified approach to emergency caesarean section under general anaesthesia in COVID-19 pandemic. Anaesthesiol Reanim. 2020;48(3):174–179. doi: 10.5152/TJAR.2020.280420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mandal A., Sengupta S., Sheet J., Bisui B., Swaika S., Majumder S. Rapid sequence spinal anaesthesia with 11mg and 12.5 mg of hyperbaric bupivacaine for Category 1 caesarean section. Sri Lankan Journal of Anaesthesiology. 2014;22(2) [Google Scholar]
- 33.Dransfield M., Richardson A., Robinson N. Recommending AAGBI antisepsis guidance to other medical professionals. Anaesthesia. 2015;70(3):366. doi: 10.1111/anae.13010. [DOI] [PubMed] [Google Scholar]
- 34.Parsons B., Saha S. Skin antisepsis guidelines–time to rethink the ‘rapid sequence spinal’? Anaesthesia. 2015;70(3):366–367. doi: 10.1111/anae.13025. [DOI] [PubMed] [Google Scholar]
- 35.Ghaffari S., Dehghanpisheh L., Tavakkoli F., Mahmoudi H. The effect of spinal versus general anesthesia on quality of life in women undergoing cesarean delivery on maternal request. Cureus. 2018;10(12) doi: 10.7759/cureus.3715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ramkumar V., Dinesh E., Shetty S.R., Shah A., Kundra P., Das S., et al. All India Difficult Airway Association 2016 guidelines for the management of unanticipated difficult tracheal intubation in obstetrics. Indian J Anaesth. 2016;60(12):899. doi: 10.4103/0019-5049.195482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Solangi S.A., Khaskheli M.S., Siddiqui M.A. Comparison of the effects of general vs spinal anesthesia on neonatal outcome. Anaesth Pain Intensive Care. 2019:18–23. [Google Scholar]
- 38.Hell J., Madamombe T., Cordingly M., Eynon C. Skin antisepsis guidelines–presentation or concentration? Anaesthesia. 2015;70(3):367–368. doi: 10.1111/anae.13026. [DOI] [PubMed] [Google Scholar]
- 39.Adams K. 2018. Best practice policy recommendation for neuraxial anesthesia skin antiseptic solutions. [Google Scholar]
- 40.Springel E.H., Wang X.-Y., Sarfoh V.M., Stetzer B.P., Weight S.A., Mercer B.M. A randomized open-label controlled trial of chlorhexidine-alcohol vs povidone-iodine for cesarean antisepsis: the CAPICA trial. Am J Obstet Gynecol. 2017;217(4):463. doi: 10.1016/j.ajog.2017.05.060. e1-. e8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.