To the Editor,
As the world battles the coronavirus disease 2019 (COVID-19) pandemic, wading through the deluge of published COVID-19 research has become a challenge for clinicians. Despite a strong push for the practice of evidence-based medicine over the past decades, a search of COVID-19 literature in recent months paints a different picture. The use of hydroxychloroquine has been the ‘poster child’ for the importance of conducting randomized controlled trials (RCTs), initially showing promise in uncontrolled studies [1] and even being recommended by governmental leaders, only to later show no benefit in RCTs [2]. Similarly, many observational studies have reported on risk factors for COVID-19. A recent genome-wide association analysis (GWAS) has implicated that blood group A patients had a higher risk of severe COVID-19 than other blood types [3], while other studies have found associations between vitamin D levels/latitude, and Bacille de Calmette et Guérin (BCG) vaccine and mortality to COVID-19 [4]. Based on the results of these studies, shall we tell our blood group A patients to stay home or tell everyone to take vitamin D or get vaccinated with BCG? What are the mechanisms underlying these relationships? Although blood group antigens are known to play a role in infections, the results of the recent GWAS study may have been influenced by the control group comprising blood donors and the lack of adjustment for comorbidities [5]. Low vitamin D levels have often been associated with a higher risk of infections, but vitamin D supplementation has not been shown to prevent respiratory infections among adults with low vitamin D levels [6]. The BCG vaccine is thought to provide broad protection against other infections, but a recent study showed no difference in rates of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection among vaccinated or unvaccinated adults [7]. Overall, evidence supporting a causal relationship between blood types, vitamin D and BCG vaccine and COVID-19 risk are scant.
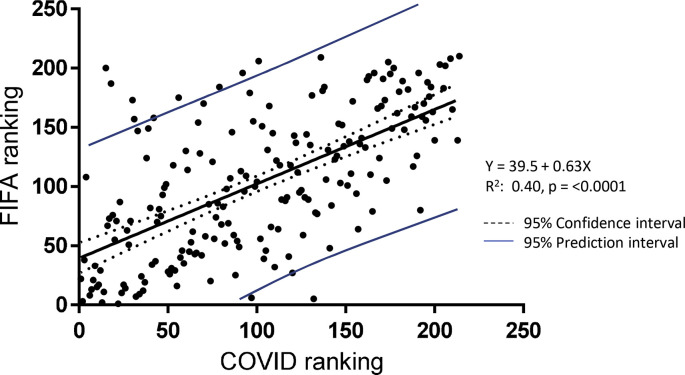
The ‘big data’ and ‘real-world data’ movements have gained an increasing foothold in the pages of high-impact journals during the pandemic, but it is important to remember that correlation does not equal causation. To further demonstrate our point, we studied the correlation between the global ranking of the Fédération Internationale de Football Association (FIFA) and the ranking of COVID-19 cases by country (Fig. 1 ). A ranking of countries based on the highest total number COVID-19 cases was calculated on 16 June 2020 based on data from the open-source ‘World-O-Meter’ online data repository [5]. The FIFA ranking is a point-based system derived by adding points a national football team gains from playing international matches over the period of the last 4 years. Points are given for the outcome of the match, the importance of the match and the strength of the opposing team. We found a strong positive correlation between a country's FIFA ranking and their COVID-19 ranking (R 2 = 0.40, p < 0.0001). This association was stronger than those of the prevalence of diabetes or obesity with COVID-19 risk (data not shown). Indeed, multiple football players in the Premier League, Serie A, La Liga, etc., have been reported to test positive for SARS-CoV-2 since the beginning of COVID-19 pandemic. Does this mean that people who are skilled in playing football are at increased risk of catching SARS-CoV-2 or of spreading it? Or does COVID-19 make you a better football player? This is unlikely to be the correct conclusion to draw from these findings. However, there might be alternative explanations. The mass gatherings at football stadiums early in the pandemic may have contributed to the spread of SARS-CoV-2 or the cross-border travel of the supporters during the UEFA Champions League may have spread it to multiple European countries. Or is it possible that SARS-CoV-2 spreads among the guests in the football pubs where the supporters got drunk without social distancing and face coverings? These latter explanations appear more reasonable than the former, but no matter how strong correlation does not equal causation.
Fig. 1.
Scatterplot showing the association between national football team FIFA ranking and the respective country's COVID-19 ranking based on total confirmed COVID-19 cases. There was a strong correlation between the two rankings (R2 0.40, p < 0.0001).
While much of the published COVID-19 observational research has been fuelled by genuine scientific curiosity, we must not let our desperate effort to identify at-risk populations and effective treatments erase our appreciation of the well-established hierarchy of evidence. Instead, we should not forget that outcomes of observational studies are only hypothesis forming, allowing closer examination of the situation to identify whether a true causation can be established between the two variables.
Transparency Declaration
The authors report no external funding associated with the present work. All authors have no conflicts of interest directly relevant to the content of this article.
Author contributions
A.F.: writing of original draft. T.S.: conceptualization (equal); editing and approval of final draft. A.S.: conceptualization; methodology; writing, review and editing.
Editor: L. Leibovici
References
- 1.Gautret P., Lagier J.C., Parola P., Hoang V.T., Meddeb L., Mailhe M. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. 2020;56:105949. doi: 10.1016/j.ijantimicag.2020.105949. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 2.Tang W., Cao Z., Han M., Wang Z., Chen J., Sun W. Hydroxychloroquine in patients with mainly mild to moderate coronavirus disease 2019: open label, randomised controlled trial. BMJ. 2020;369:m1849. doi: 10.1136/bmj.m1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ellinghaus D., Degenhardt F., Bujanda L., Buti M., Albillos A., Invernizzi P. Genomewide association study of severe Covid-19 with respiratory failure. N Engl J Med. 2020 doi: 10.1056/NEJMoa2020283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rhodes J.M., Subramanian S., Laird E., Kenny R.A. Letter: low population mortality from COVID-19 in countries south of latitude 35 degrees north supports vitamin D as a factor determining severity – authors’ reply. Aliment Pharmacol Ther. 2020 doi: 10.1111/apt.15777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Worldometer COVID-19 coronavirus pandemic. 2020. https://www.worldometers.info/coronavirus/ [Google Scholar]
- 6.Camargo C.A., Sluyter J., Stewart A.W., Khaw K.T., CLawes C.M.M., Toop L. Effect of monthly high-dose vitamin d supplementation on acute respiratory infections in older adults: a randomized controlled trial. Clin Infect Dis. 2020;71:311–317. doi: 10.1093/cid/ciz801. [DOI] [PubMed] [Google Scholar]
- 7.Hamiel U., Kozer E., Youngster I. SARS-CoV-2 rates in BCG-vaccinated and unvaccinated young adults. JAMA. 2020 doi: 10.1001/jama.2020.8189. [DOI] [PMC free article] [PubMed] [Google Scholar]