Abstract
Background
With the growing use of telehealth, understanding factors affecting patient follow-up in traditional and telehealth settings is important. Few data exist examining the use of telehealth compared with traditional settings. Bridging this gap is critical to optimizing telehealth use and reducing barriers.
Study Design
This is a retrospective cohort study of return and postoperative (electronic video [eClinic] and traditional) visits from January 2018 to March 2020 at single tertiary care center. There were 12,359 unique first-encounter patients with 903 eClinic and 11,456 traditional visits; 11,547 patients completed visits, while 812 patients did not show up. Multivariable logistic regression modeling was performed to identify factors associated with no-show. County-level mapping was used to identify patterns in no-show rates.
Results
Patients from the eClinic had twice the odds of no-show compared with those from a traditional clinic (p < 0.001). Age was inversely proportional to odds of no-show, with each additional decade associated with a 16% decrease in these odds (p < 0.001). African-American patients had greater odds of no-show compared to Caucasian patients (odds ratio [OR] 2.47; 95% CI 1.95–3.13, p < 0.001). Marital statuses of single and legal separation were associated with higher odds of no-show compared with married marital status (p < 0.001 and p = 0.04, respectively). Minimally invasive and endocrine surgery clinics had lower odds of no-show compared with acute care surgery clinic (p < 0.001 for both). County-level no-show rates demonstrate similar patterns between clinic settings.
Conclusions
Several factors are associated with increased odds of no-show, including the visit being in eClinic. County-level analysis suggests no-show variation is not dependent on geographic location. Understanding these patterns allows for prospective identification of barriers and development of interventions to optimize access and patient care.
Visual Abstract
Telehealth for the perioperative care of surgical patients is rapidly expanding. Although the idea of telehealth itself has been around since the early 20th century, the recent explosion in its use is relatively new.1 , 2 Telehealth grew 53% from 2016 to 2017, outpacing any other place of service, including urgent care centers, according to a dataset of 29 billion private healthcare claims.2 Furthermore, many institutions have expanded telehealth capabilities into several surgical fields including vascular, bariatric, maxillofacial, thoracic, and transplant surgery.3, 4, 5, 6, 7 Several benefits of telehealth have been previously described, including high patient and provider satisfaction and reduced barriers related to travel.8 With the expansion of Medicare coverage to now include telehealth services during the COVID-19 pandemic, there is an anticipated surge in usage as millions of Americans now have insurance coverage for such programs.9
Due to increased use of telehealth programs, their safety and efficacy have been evaluated by several studies. A systematic review demonstrated that telehealthcare can be safe and effective in surgical populations.10 Our group has shown that after uncomplicated emergency surgery, postoperative follow-up in telehealth clinic is equivalent to traditional clinic in terms of safety for selected patients.11 In another study, only 14% of patients who underwent an uncomplicated appendectomy or cholecystectomy clinically benefited from in-person follow-up, with the majority of these postoperative visits consisting of suture, staple, or drain removal.12 Therefore, with appropriate selection, surgical patients can safely be monitored remotely. With the opportunity for high quality care and increased access, telehealth use seems advantageous for patients and providers.
There is a paucity of data on how patient use of a telehealth clinic compares with that of a traditional clinic. Knowledge of these patterns will help institutions identify barriers for patients. It will further guide potential strategies for optimizing care, improving education, and increasing outreach. It will also improve the collective understanding of when telehealth initiatives may fail to improve access.
In this study, we aimed to understand how patient factors affect use of our institution’s surgical telehealth clinic and traditional clinic. Our institution’s surgical telehealth clinic is an electronic clinic (eClinic), and we focused specifically on the visits in this clinic in which patients interact with providers via video. We looked at the risk of no-show in both settings and formed several hypotheses. First, given the assumed convenience of telehealth and lack of barriers related to travel, we hypothesized that eClinic visits would have a lower rate of no-show. Second, we hypothesized that younger patients would be more likely to complete their eClinic visit. Third, we hypothesized that racial disparities and marital status would affect the odds of no-show for all visits. Last, we suspected that counties located far from our hospital would have higher rates of no-show in the traditional clinic compared to eClinic.
Methods
Institutional Review Board approval
The study was part of a quality improvement and assessment project and was approved by our Institutional Review Board according to the quality improvement/assessment classification.
Description of clinics and eClinic criteria
At our institution, we offer patients the opportunity to be evaluated in either a traditional or an eClinic setting for follow-up. Traditional clinic visits are the standard in-person evaluation with a surgical provider (attending, advanced practice provider, or resident). With regard to our institution’s eClinic program, visits completed with a secure video link are the preferred form of follow-up. If the patient does not have the ability to participate in a video visit, this visit may be conducted as a telephone visit based on provider discretion. In this study, with regard to the analysis of eClinic visits, we evaluated only those visits that were completed with the video interface. Therefore, telephone visits were not included in this study.
Appropriateness for follow-up in an eClinic setting is typically determined by the provider. Most patients are candidates for eClinic follow-up; however, broad departmental criteria to determine when a patient should be excluded from eClinic include the following: complications, open wounds requiring in-person management, drains requiring removal, staples or sutures that require removal, pathology results that require in-person discussion, and patient request for an in-person visit.
Patient identification and visit definitions
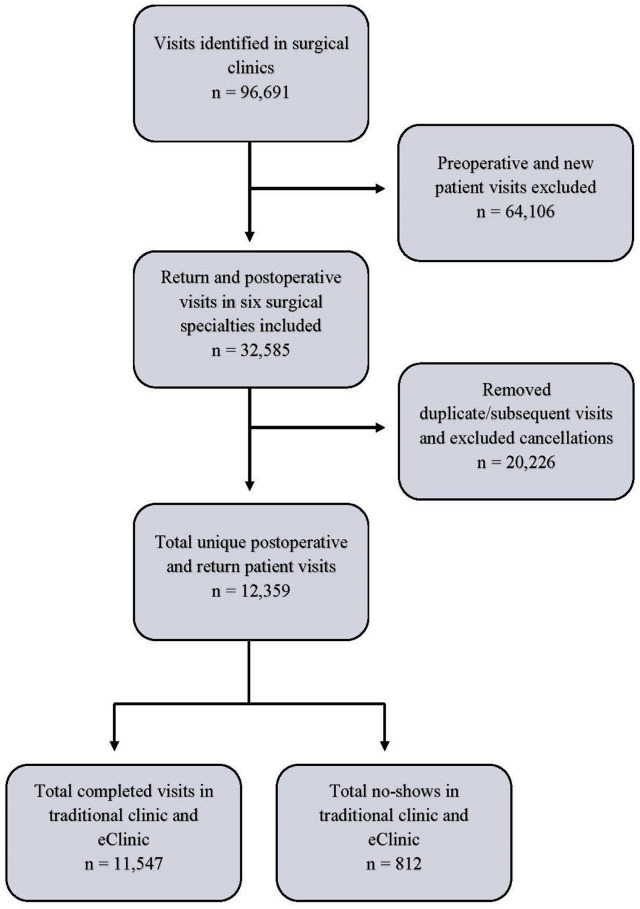
We identified 96,691 surgical patient visits from January 2018 to March 2020 at our institution (Fig. 1 ). These visits encompassed completed, cancelled, and no-show visits. A completed visit signified that the patient was seen by a provider. Cancelled visits were those cancelled by either patient or provider, regardless of subsequent cancellation, no-show, or completion. A no-show visit was when the patient did not show up to the visit, regardless of subsequent visit status or rescheduling. All new patient evaluations were excluded because these visits in eClinic were still being trialed during this period. Therefore, only return and postoperative visits (patients with established care) were included in the final analysis. There were 6 surgical groups conducting return and postoperative appointments in traditional clinic and eClinic: acute care surgery, endocrine surgery, minimally invasive surgery, plastic surgery, hepatopancreaticobiliary surgery, and colorectal surgery. Visits in surgical clinics other than those listed or with other classifications (new patient, procedure, etc) were excluded from the analyses. A total of 32,585 traditional and eClinic visits were ultimately identified. In order to eliminate the effect of duplicate patients with multiple visits, we included only the patient’s first return or postoperative encounter. Given the inability to easily determine the reason for cancellation, we removed all cancelled visits from subsequent analyses. This revealed 12,359 unique patient visits, including 11,547 completed visits and 812 no-show visits (Fig. 1).
Figure 1.
Patient selection flowchart. Our flowchart demonstrates how our final patient study population was established for examining differences in no-show rates.
Retrospective data collection and patient demographics
Using the electronic medical record (Epic), data were extracted from patient visits. Final data included visit status (completed vs no-show), visit type (eClinic vs traditional visit), age, sex, ethnicity, race, year of visit, marital status, need for interpreter, clinic specialty, and residential ZIP code. We used descriptive statistics to detail the clinical and demographic characteristics of the cohort. Student’s t-tests, chi-square tests, or their nonparametric counterparts were used to assess unadjusted associations between patient characteristics and visit status.
Multivariable logistic regression
We used logistic regression modeling to identify patient and clinic factors associated with visit status. Included covariates were patient demographics including age, sex, race, ethnicity, marital status, and need for an interpreter, as well as clinic characteristics such as surgical section of the clinic, visit year, and visit type (eClinic vs traditional). Statistical significance was established at a value of p ≤ 0.05 unless noted otherwise. All analyses were completed using STATA version 16 (Statacorp).
Geographic county heat-mapping
Rates of no-show were aggregated at the county level using ZIP code data from the electronic health records. Stratified rates of no-show for traditional and eClinic visits by county were used to create county-specific heat maps. Counties with no scheduled visits for each visit type were considered missing and labeled as such.
Results
Patient demographics and visit characteristics
There were 11,547 total completed visits, with eClinic representing 6.7% (n = 777) of this cohort; eClinic visits represented 126 of the 812 (15.5%) no-show visits (p < 0.001) (Table 1 ). The average age of patients who completed their visit in both eClinic and traditional clinic was higher than those who did not show up for their visit (p < 0.001). No differences in sex were observed. A higher proportion of African-American patients were identified in the cohort of no-show visits (p < 0.001). A comparison based on the need for an interpreter revealed no differences. Differences were observed between the different surgical subspecialty clinics (p < 0.001) (Table 1). Lastly, differences were noted according to marital status, with married patients representing a higher proportion of completed visits (p < 0.001).
Table 1.
Patient Characteristics
| Characteristic | Completed (n = 11,547) | No show (n = 812) | p Value |
|---|---|---|---|
| Visit type, n (%) | <0.001 | ||
| eClinic | 777 (6.7) | 126 (15.5) | |
| Traditional | 10,770 (93.3) | 686 (84.5) | |
| Hispanic ethnicity | 363 (3.2) | 38 (4.8) | 0.017 |
| Age, y, mean (SD) | 53.8 (16.5) | 45.9 (16.2) | <0.001 |
| Sex, F, n (%) | 6,313 (54.7) | 448 (55.2) | 0.784 |
| Race, n (%) | <0.001 | ||
| Caucasian | 9,557 (87.2) | 568 (75.53) | |
| African-American | 965 (8.8) | 158 (21.0) | |
| Asian | 392 (3.6) | 21 (2.8) | |
| American Indian and Alaskan Native | 8 (0.1) | 0 (0) | |
| Need for interpreter, n (%) | 206 (1.8) | 10 (1.2) | 0.330 |
| Surgical section, n (%) | <0.001 | ||
| Acute care | 2,316 (20.1) | 275 (33.9) | |
| Colorectal | 2,115 (18.3) | 178 (21.9) | |
| Endocrine | 2,985 (25.9) | 101 (12.4) | |
| Hepatopancreaticobiliary | 855 (7.5) | 43 (5.3) | |
| Minimally-invasive | 2,373 (20.55) | 112 (13.8) | |
| Plastic and reconstruction | 902 (7.8) | 103 (12.7) | |
| Year of visit, n (%) | 0.032 | ||
| 2018 | 6,019 (52.1) | 388 (47.8) | |
| 2019 | 4,666 (40.4) | 266 (45.1) | |
| 2020 | 861 (7.5) | 58 (7.1) | |
| Marital status | <0.001 | ||
| Single | 2,701 (30.5) | 290 (49.4) | |
| Married | 5,377 (60.7) | 226 (38.5) | |
| Legally separated | 42 (0.5) | 10 (1.7) | |
| Divorced | 405 (4.6) | 35 (6.0) | |
| Widowed | 341 (3.9) | 26 (4.4) |
Multivariate logistic regression modeling
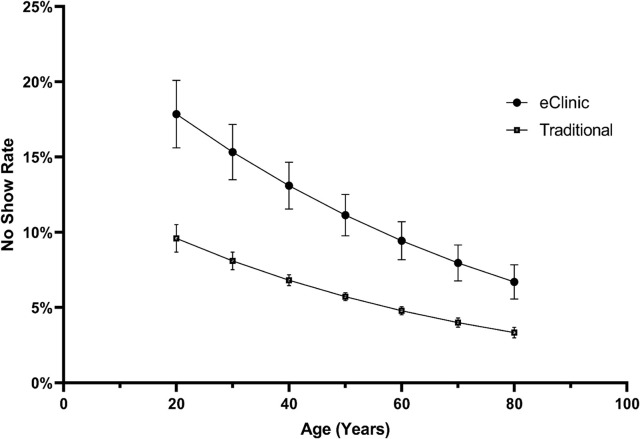
Using a multivariable logistic regression model to assess for confounders, we identified several independently predictive factors for no-shows (Table 2 ). Patients with follow-up in eClinic demonstrated increased odds of no-show compared with patients in traditional clinic (odds ratio [OR] 2.13; 95% CI 1.58–2.89, p < 0.001). No differences were seen according to ethnicity, sex, need for interpreter, or year of visit. There was an inverse relationship between age and odds of no-show (OR 0.84 per decade increase in age; 95% CI 0.79–0.88, p < 0.001), a relationship present for both settings. Predicted probability of no-show for eClinic and traditional visits by age is shown in Figure 2 . Differences in odds of no-show according to race were identified in this multivariable analysis. Patients who identified as African-American (OR 2.47; 95% CI 1.95–3.13, p<0.001) and American Indian/Alaskan Natives (OR 3.29; 95% CI 1.10–9.80, p=0.03) were more likely to not show up for their visit compared with those who identified as Caucasian (Table 2).
Table 2.
Multivariable Logistic Regression Model
| Characteristic | Odds ratio (95% CI) | p Value |
|---|---|---|
| Visit type | ||
| eClinic | 2.13 (1.58–2.89) | <0.001 |
| Hispanic ethnicity | 0.74 (0.39–1.42) | 0.375 |
| Age, per 10-y increase | 0.84 (0.79–0.88) | <0.001 |
| Sex, F | 0.94 (0.78–1.13) | 0.485 |
| Race | ||
| Caucasian | REF | REF |
| African-American | 2.47 (1.95–3.13) | <0.001 |
| Asian | 0.66 (0.37–1.18) | 0.164 |
| American Indian and Alaskan Native | 3.29 (1.10–9.80) | 0.033 |
| Need for interpreter | 0.79 (0.24–2.57) | 0.694 |
| Surgical section | ||
| Acute care | REF | REF |
| Colorectal | 0.93 (0.71–1.23) | 0.624 |
| Endocrine | 0.45 (0.33–0.61) | <0.001 |
| Hepatopancreaticobiliary | 0.89 (0.61–1.32) | 0.572 |
| Minimally invasive | 0.52 (0.39–0.70) | <0.001 |
| Plastic and reconstruction | 1.26 (0.92–1.73) | 0.145 |
| Year of visit | ||
| 2018 | REF | REF |
| 2019 | 1.03 (0.85–1.24) | 0.785 |
| 2020 | 0.81 (0.55–1.19) | 0.286 |
| Marital status | ||
| Single | REF | REF |
| Married | 0.60 (0.48–0.74) | <0.001 |
| Legally separated | 2.30 (1.03–5.17) | 0.043 |
| Divorced | 1.11 (0.75–1.68) | 0.591 |
| Widowed | 1.18 (0.70–2.01) | 0.532 |
Figure 2.
The inverse relationship between age and no-show rate. No-show rates among the younger population is higher than that among the older population for both traditional and eClinic. The eClinic no-show rate in the younger population is almost twice that of the traditional clinic. The y-axis represents marginal predicted probabilities based on the multivariable model described in the text.
A subsequently developed model testing for an interaction effect between race and visit type showed no statistically significant effect for any race category (p > 0.05 for all interaction terms, complete model data not shown). When evaluating the odds of no-show in the different surgical clinics, those with the lowest odds of no-show compared to acute care surgery were endocrine surgery (OR 0.45; 95% CI 0.33–0.61, p < 0.001) and minimally invasive surgery (OR 0.52; 95% CI 0.39– 0.70, p < 0.001). There was no difference in odds of no-show according to the year of the scheduled visit. Marital status was a significant independent predictor of no-show. Married patients, as compared to single patients, had 40% decreased odds of no-show (OR 0.60; 95% CI 0.48–0.74, p < 0.001). Patients identified as legally separated had higher odds of no-show in comparison to single patients (OR 2.30; 95% CI 1.03–5.17, p = 0.04).
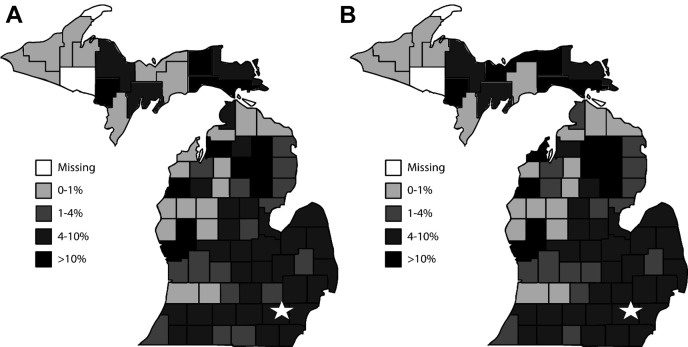
Geographic distribution of no-show visits
Using ZIP code data, a heat map was generated of traditional (Fig. 3A) and eClinic (Fig. 3B) stratified no-show rates in the state of Michigan. Comparison of these patterns revealed that no-show rates in both clinics track similarly across Michigan counties. No discernible pattern is seen relative to the geographic location.
Figure 3.
No-show rates in (A) traditional and (B) eClinic settings for counties in Michigan. There are broad similarities in no-show rates between different counties for traditional clinic and eClinic that do not appear to be dependent on geographic location. The location of our institution is denoted by the star.
Discussion
The benefits of telehealth for surgical specialty and postoperative patient care have been well-described.8 , 10 , 11 While telehealth should improve access for patients, there is a lack of data examining the differences in use patterns between traditional and telehealth visits. We aimed to identify risk factors for patient no-shows at follow-up in our traditional clinic and telehealth eClinic settings in an effort to identify potential targets to optimize care and outreach. These findings have clear implications for institutions in terms of resource use, efficiency, and logistical planning.
Our data indicate several factors associated with increased risk of a patient no-show. Although some of these factors were anticipated, 2 key findings ran contrary to what we expected. For example, we hypothesized that the convenient nature of eClinic would result in a higher completion rate for eClinic visits. Our data, however, suggest that patients are more likely to not show up for these visits, as compared to the traditional visits. Another key finding that differed from our hypotheses was the inverse relationship between no-show rate and age. We originally believed that eClinic no-show rates would be lower among the younger populations. With the assumption that younger patients are more likely to be technically savvy, we thought they would have a greater ability to complete an eClinic visit. However, our data show that younger patients are at greater risk for no-show in both types of clinic settings.
Understanding why patients are less likely to complete their visit is vital to improving patient access to care and for optimizing telehealth infrastructure and processes. Reasons for missing traditional clinic visits have been previously established and include emotional barriers, a perceived disrespect of one’s beliefs and time by the healthcare system, and a lack of understanding of the scheduling system.13 However, a lack of data exists regarding why patients miss their telehealth appointments. Some studies that examined patient preferences regarding telehealth point to areas that may contribute to patient no-show. These include a lack of appropriate privacy to discuss sensitive topics and a concern that the provider would not be able to adequately perform a physical exam virtually.14 It is plausible that these patient attitudes toward telehealth contribute to the no-show rate seen in this study. Additionally, perhaps patients perceive a provider’s recommendation for telehealth follow-up as indicative of the visit being less important to complete since the patient does not need to be seen directly. Overall, continuing to investigate patient attitudes may reveal why patients are more likely to miss their telehealth appointments in comparison to traditional appointments. Future studies may also consider generational analyses to reveal age-specific motivations.
Further focusing on the inverse relationship between age and visit completion, this may reflect generational differences in how healthcare visits are viewed by patients. In a study examining general practitioner attitudes toward patients who miss appointments, younger patients were seen as “lacking respect and responsibility” and “valuing appointments less than older patients.”15 Although one of the aims of telehealth is to improve access, seeing little value in an appointment likely transcends the medium in which the appointment takes place. In other words, younger patients who see little value in a traditional visit may have similar attitudes toward telehealth visits. We suspect this may be particularly true because younger patients are less likely to have significant comorbidities. Additionally, they are more likely to recover from an operation faster without complication, obviating the perceived necessity of a postoperative visit. Optimizing a telehealth clinic should include a brief review of a patient’s overall no-show clinic history. If a younger patient has a history of no-shows in a traditional clinic setting, referral to a telehealth should not be considered a solution to reduce the no-show risk; rather, it would be prudent for the provider to explore these reasons for no-show before referral to telehealth. This may unearth important barriers that need addressing.
Our study revealed differential rates of no-show by clinic specialty. The risk of no-show was lowest for the patients seen in the minimally invasive and endocrine surgery clinics. It is difficult to surmise why this might be, although it is possible that the elective, urgent, or emergent nature of the surgical subspecialty plays a role. Urgent or emergent cases, as are typical in our institution’s acute care surgery service, may be performed by a surgeon with whom the patient does not have a pre-established relationship. We suspect that the relationship formed preoperatively in an elective setting bolsters the likelihood that the patient will follow-up postoperatively. Overall, the exact reason for this effect is unclear and necessitates further studies to determine consistency in different settings across other institutions.
Marital status was also associated with the risk of clinic no-show. Patients who indicated that they were married were less likely to not show up for their visit, independent of other factors. This is consistent with previous studies that have evaluated the positive impact that marriage can have on healthcare, particularly in the elderly.16 Marital status is likely representative of a latent measure of social support. A spouse can hold the patient accountable to complete visits and follow-up their care plan. Additionally, perceived spousal support has been previously shown to be associated with better health.17 Patients who indicate a marital status of single may lack the social support benefits afforded to married patients. Also, people who decide to marry or not may have different priorities that reflect how they make other decisions in their daily lives. Similar to this reasoning, our study revealed that legally separated patients had the highest risk of no-show. Given that legal separation is a stepping-stone in many cases of divorce, it is possible that the acuity of a legal separation is especially disruptive to a patient’s life and social structure. Our findings support the need to screen patients regarding their social support structures. This can be a tool in a physician’s arsenal when trying to risk stratify patients based on their ability to follow-up in clinic and to identify patients who need additional resources.
Our study suggested the presence of racial disparities and associated variation in risk of no-show. We identified a particularly high risk of visit no-show among those who identified as African-American. Importantly, our model suggests that this risk is independent of the other evaluated factors. Our observation is consistent with those from other studies that have identified a number of barriers that this community as well other minority communities encounter, including a distrust in the health system, forgetfulness of the appointment, and a sense that appointments are not helpful.18 Additionally, African-American patients have expressed more concerns than other minority patients in regard to confidentiality, privacy, and the physical absence of the specialist in a telehealth clinic.19 Despite a goal of telehealth to increase access to care, the benefits of telehealth do not necessarily address all these factors. Providers need to acknowledge these contextual barriers in order to optimize care for this community.
Other minority groups may experience barriers to telehealth similarly to African-Americans. One specific barrier could be the decreased access and use of technology, such as the internet, among minorities, persons of low socioeconomic status, and persons with disabilities referred to as the “digital divide.”20 Interpreting our data within the context of available literature suggests that multiple factors contribute to decreased access by minority patients. Dramatically improving access and use of telehealth in these patient populations will require a creative, multifaceted intervention. Screening patients for access to pertinent technology is critical. As part of our telehealth infrastructure, one intervention we are considering at our institution is to have a dedicated social worker to assist populations at risk of encountering barriers to access in an eClinic setting.
Our study sought to understand geographic no-show patterns across the state of Michigan. The geographic heat maps illustrate similar patterns in the frequency of no-show for both eClinic and traditional clinic. In particular, several counties in the Upper Peninsula have high eClinic no-show rates. This is contrary to our hypothesis that patients who live in distant geographic locations relative to our hospital would be the ones most likely to complete eClinic visits. The broad similarities between no-show rates in eClinic and traditional clinic suggest that geographic location does not play a significant role. Future studies examining county-specific data, such as socioeconomic and demographic data, may elucidate trends explaining the similarities noted between no-show rates in both eClinic and traditional clinic.
This study has some limitations that should be acknowledged. First, it was performed at a single center. It is therefore unclear how generalizable these findings are to other health systems that treat different populations. Future studies could be replicated at multiple institutions to determine whether our findings are consistent elsewhere. Additionally, the socioeconomic and geographic makeup vary from state to state, so the results may differ depending on various state-level factors. Another limitation is that this study is an analysis of retrospective data, so it does not incorporate the patient perspective. Future studies should evaluate the patient’s perspective regarding reasons for no-show. Furthermore, due to possible selection bias, there are likely to be inherent differences between the patient populations seen in either clinic setting that we are unable to fully appreciate without more granular data. Also, we were unable to exclude patients who had factors that clearly reduce a patient’s ability to choose (eg presence of drain, staples, or sutures, etc) as we did not have access to these data. Similarly, we were unable to incorporate baseline comorbidities, socioeconomic data, or level of education into our modeling due to limitations in available data. Finally, a limitation in this study is that, while we can detect associations, we are unable to make any definitive conclusions about causality. In order to better define the reasons for these findings in this study, future studies should obtain additional granular information and use a mixed methods research design. Despite these study limitations, our findings are still consistent with previously published literature and provide actionable information for the institutions that are setting up telehealth programs.
Conclusions
Overall, this study offers insights regarding opportunities to improve access for patients in a traditional and telehealth eClinic setting. As part of the quality improvement aspect of this study, we have instituted measures at our institution to identify barriers that patients may encounter when obtaining access to care. First, we emphasize that this information should not be used to exclude patients from being seen in any particular clinic setting. Doing this would institute a systemic barrier that is contrary to the intent of these efforts. Rather, this information should be used to identify patients who require additional assistance or resources to ensure maximal access to care. Patients should be screened for their social support systems, perceptions of the follow-up visit, access to necessary resources, and comfort level with either visit type. Early identification of possible barriers will hopefully improve the chance of follow-up completion in both traditional and telehealth settings.
Author Contributions
Study conception and design: Kemp, Liesman, Brown, Williams, Wilson, Alam
Acquisition of data: Kemp, Liesman, Brown, Wilson
Analysis and interpretation of data: Kemp, Liesman, Brown, Williams, Biesterveld, Wakam, Alam
Drafting of manuscript: Kemp, Liesman, Brown, Williams, Biesterveld, Wakam, Wilson
Critical revision: Kemp, Liesman, Brown, Williams, Alam
Footnotes
Dr Kemp and Daniel Liesman contributed equally to this work and share primary authorship.
Disclosure Information: Nothing to disclose.
References
- 1.Strehle E.M., Shabde N. One hundred years of telemedicine: does this new technology have a place in paediatrics? Arch Dis Child. 2006;91:956–959. doi: 10.1136/adc.2006.099622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.FAIR Health A Multilayered Analysis of Telehealth, A FAIR Health White Paper. July 2019. https://s3.amazonaws.com/media2.fairhealth.org/whitepaper/asset/A%20Multilayered%20Analysis%20of%20Telehealth%20-%20A%20FAIR%20Health%20White%20Paper.pdf Available at:
- 3.Hands L.J., Jones R.W., Clarke M. The use of telemedicine in the management of vascular surgical referrals. J Telemed Telecare. 2004;10(Suppl 1):38–40. doi: 10.1258/1357633042614212. [DOI] [PubMed] [Google Scholar]
- 4.Sudan R., Salter M., Lynch T. Bariatric surgery using a network and teleconferencing to serve remote patients in the Veterans Administration Health Care System: feasibility and results. Am J Surg. 2011;202:71–76. doi: 10.1016/j.amjsurg.2010.06.016. [DOI] [PubMed] [Google Scholar]
- 5.Wood E.W., Strauss R.A., Janus C. Telemedicine consultations in oral and maxillofacial surgery: a follow-up study. J Oral Maxillofac Surg. 2016;74:262–268. doi: 10.1016/j.joms.2015.09.026. [DOI] [PubMed] [Google Scholar]
- 6.Cleeland C.S., Wang X.S., Shi Q. Automated symptom alerts reduce postoperative symptom severity after cancer surgery: a randomized controlled clinical trial. J Clin Oncol. 2011;29:994–1000. doi: 10.1200/JCO.2010.29.8315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McGillicuddy J.W., Gregoski M.J., Weiland A.K. Mobile health medication adherence and blood pressure control in renal transplant recipients: a proof-of-concept randomized controlled trial. JMIR Res Protoc. 2013;2:e32. doi: 10.2196/resprot.2633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Asiri A., AlBishi S., AlMadani W. The use of telemedicine in surgical care: a systematic review. Acta Inform Med. 2018;26(3):201–206. doi: 10.5455/aim.2018.26.201-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alonso-Zaldivar R. “Public health to keep seniors safe at home, Medicare expands telemedicine.” apnews.com. Available at: apnews.com/58e118636f3e39c53370131561127a54. Published March 17, 2020. Accessed March 30, 2020.
- 10.Gunter R.L., Chouinard S., Fernandes-Taylor S. Current use of telemedicine for post-discharge surgical care: a systematic review. J Am Coll Surg. 2016;222:915–927. doi: 10.1016/j.jamcollsurg.2016.01.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nikolian V.C., Williams A.M., Jacobs B.N. Pilot study to evaluate the safety, feasibility, and financial implications of a postoperative telemedicine program. Ann Surg. 2018;268:700–707. doi: 10.1097/SLA.0000000000002931. [DOI] [PubMed] [Google Scholar]
- 12.Chen D.W., Davis R.W., Balentine C.J. Utility of routine postoperative visit after appendectomy and cholecystectomy with evaluation of mobile technology access in an urban safety net population. J Surg Res. 2014;190:478–483. doi: 10.1016/j.jss.2014.04.028. [DOI] [PubMed] [Google Scholar]
- 13.Lacy N.L., Paulman A., Reuter M.D. Why we don’t come: patient perceptions on no-shows. Ann Fam Med. 2004;2:541–545. doi: 10.1370/afm.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Powell R.E., Henstenburg J.M., Cooper G. Patient perceptions of telehealth primary care video visits. Ann Fam Med. 2017;15:225–229. doi: 10.1370/afm.2095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Husain-Gambles M., Neal R.D., Dempsey O. Missed appointments in primary care: questionnaire and focus group study of health professionals. Br J Gen Pract. 2004;54:108–113. [PMC free article] [PubMed] [Google Scholar]
- 16.Iwashyna T.J., Christakis N.A. Marriage, widowhood, and health-care use. Soc Sci Med. 2003;57:2137–2147. doi: 10.1016/s0277-9536(02)00546-4. [DOI] [PubMed] [Google Scholar]
- 17.Ryan L.H., Wan W.H., Smith J. Spousal social support and strain: impacts on health in older couples. J Behav Med. 2014;37:1108–1117. doi: 10.1007/s10865-014-9561-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nwabuo C.C., Dy S.M., Weeks K. Factors associated with appointment non-adherence among African-Americans with severe, poorly controlled hypertension. PLoS One. 2014;9(8) doi: 10.1371/journal.pone.0103090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.George S., Hamilton A., Baker R.S. How Do Low-Income Urban African Americans and Latinos Feel about Telemedicine? A Diffusion of Innovation Analysis. Int J Telemed Appl. 2012;2012:715194. doi: 10.1155/2012/715194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chang B.L., Bakken S., Brown S.S. Bridging the digital divide: reaching vulnerable populations. J Am Med Inform Assoc. 2004;11:448–457. doi: 10.1197/jamia.M1535. [DOI] [PMC free article] [PubMed] [Google Scholar]