Abstract
Introduction
Vulvodynia is a chronic pain condition with potential associated factors, including musculoskeletal and psychosocial components.
Aim
This study explores the prevalence of pain-related anxiety and depression in women with provoked vestibulodynia with associated overactive pelvic floor muscle dysfunction (PVD-PFD).
Methods
A retrospective chart review of 352 women presenting to 2 urban vulvovaginal specialty clinics over the course of a year was conducted. Women presenting for initial evaluation completed validated questionnaires for pain-related anxiety and depression. Women who completed these questionnaires with a diagnosis of PVD-PFD independently confirmed by a women's health physical therapist were included in analysis. Information on previously attempted treatments was gathered.
Main Outcome Measures
Pain-related anxiety was measured with the Pain Anxiety Symptoms Scale-20 and depression with the Patient Health Questionnaire 8.
Results
Of 79 women with confirmed PVD-PFD, 22% met criteria for pain-related anxiety alone, 4% for depression alone, and 27% for both pain-related anxiety and depression, with a significant association between anxiety and depression (χ2 (1) = 21.44, P < .0005, phi = 0.521). There was also a significant association between anxiety and/or depression and whether prior treatment was attempted (χ2 (2) = 6.81, P = .03, phi = 0.294).
Conclusion
The study found that 49% of women with PVD-PFD experienced pain-related anxiety, with or without depression. In addition, there was a statistically significant association between attempts at prior treatment and greater pain-related anxiety and depression. This is the first study to report a rate of pain-related anxiety specifically in women with PVD-PFD. These findings are consistent with studies showing elevated pain-related anxiety in other chronic musculoskeletal conditions, including lower back pain and fibromyalgia.
Govind V, Krapf JM, Mitchell L, et al. Exploring Pain-Related Anxiety and Depression in Female Patients With Provoked Vulvodynia With Associated Overactive Pelvic Floor Muscle Dysfunction. J Sex Med 2020;8:517–524.
Key Words: Vulvodynia;, Pain-Related Anxiety, Depression, Pelvic Floor Muscle Dysfunction
Introduction
Vulvodynia is an idiopathic, chronic vulvar pain condition with potential associated factors, including musculoskeletal, nerve-related, and psychosocial components. The most recent consensus guideline on terminology and classification of vulvar pain defines vulvodynia as vulvar pain lasting at least 3-month duration without an identifiable cause but which may have potential associated factors. Musculoskeletal conditions, specifically pelvic floor overactivity, is cited as one of these associated factors that may be used to characterize women with vulvodynia.1 In 2015, the Fourth International Consultation on Sexual Medicine convened an expert committee to evaluate and redefine assessment and treatment strategies for vulvodynia. As part of these guidelines, the society recommended psychological interventions and pelvic floor physical therapy for the management of vulvodynia.2
Women with vulvodynia often experience tenderness of the pelvic floor muscles related to inflammation, changes in perfusion, shortening of the muscles, and hypoxia.2 Studies have indicated that women with vulvar pain on contact and localized to the vulvar vestibule, or provoked vestibulodynia (PVD) (formerly referred to as vulvar vestibulitis syndrome), may have an increase in pelvic floor muscle tone, termed “overactive pelvic floor muscle dysfunction.”2,3 Overactive pelvic floor muscle dysfunction has been associated with increased pain intensity in women with PVD.3, 4, 5, 6, 7, 8 In addition, pain-related anxiety is also positively correlated with pain intensity in PVD.4 Pain-related anxiety is believed to be key factor in chronic musculoskeletal pain conditions and more prevalent in individuals with a history of anxiety and depression.9
It is well reported that women with vulvodynia in general are more likely to experience psychological distress, including anxiety and/or depression.10, 11, 12, 13, 14, 15, 16, 17 A relatively large case-control study16 of women with and without vulvodynia demonstrated that vulvar pain was significantly more likely in women with preexisting anxiety and/or depression. However, in this study, only 56 of 177 (32%) vulvodynia patients included in the analysis were confirmed as having vulvodynia based on a pelvic examination.16 It is not known what percentage of these women had PVD. In almost all of the studies that have focused on PVD, the contribution of pelvic floor dysfunction to pain was not evaluated.11,13, 14, 15 In addition, only 1 study17 used a validated questionnaire to assess pain-related anxiety, the specific form of anxiety related to chronic pain.18
The aim of this study was to determine the prevalence of pain-related anxiety and depression in patients with a diagnosis of vestibulodynia with associated overactive pelvic floor dysfunction (PVD-PFD). Furthermore, the role of previous treatments in the rate of pain-related anxiety and depression was explored.
Methods
The study was conducted at 2 outpatient gynecology clinics specializing in female pelvic pain in large metropolitan areas. A retrospective chart review was conducted of all new patients presenting for vulvovaginal pain consultation over the course of 1 year (January 1, 2017 through December 31, 2017). Approval for retrospective chart review was obtained from Advarra IRB Pro00025298. New patients completed validated questionnaires for pain-related anxiety and depression before their consultation appointments. All patients signed a waiver allowing deidentified data to be included in a research study. Women with a diagnosis of PVD-PFD who subsequently had independent confirmation of their PFD diagnosis by a women's health physical therapist and had completed the questionnaires for pain-related anxiety and depression were included in the study analysis.
The patients were diagnosed with PVD-PFD based on a complete medical history and pelvic examination with a cotton-swab test and evaluation of the pelvic floor muscles. Adult women who reported dyspareunia and/or pelvic burning symptoms, demonstrated localized, provoked pain (greater than 5 of 10 on a 1–10–point pain scale) of the posterior vestibule (between 4 and 8 o'clock), had tense and tender pelvic floor muscles (including the puborectalis, pubococcygeus, iliococcygeus, and/or transverse perinei muscles) on examination as determined by the clinician, and did not have other causes of vulvar pain met diagnostic criteria for inclusion.2,4 All women diagnosed with PVD-PFD in this study had a diagnosis of overactive pelvic floor muscle dysfunction, as evidenced by elevated tone of the puborectalis, pubococcygeus, iliococcygeus, and/or transverse perinei muscles on examination of the pelvic floor confirmed by a women's health physical therapist.
The Pain Anxiety Symptoms Scale-20 (PASS-20) was used to evaluate pain-related anxiety in women with PVD-PFD.19 The PASS-20, which is a shortened form of the 40-question PASS, is one of the most frequently used measures of pain-related anxiety in research and clinical practice.18,20 This tool has been validated in chronic pain populations, including patients with chronic lower back pain and fibromyalgia.21,22 It is also included as one of the main instruments to measure emotional function in women with vulvodynia.20 This validated self-report questionnaire assesses 4 components of pain-related anxiety, including cognitive anxiety, fear of pain, escape and avoidance behaviors, and physiological anxiety. Each of the 20 items is rated on a 6-point Likert scale ranging from 0 (never) to 5 (always). Adding the subscales provides a score that is a general measure of pain-related anxiety. Scores greater than 30 indicate potentially maladaptive levels of pain-related anxiety, and this increases risk for chronic pain.18
The Patient Health Questionnaire 8 (PHQ-8) was used to evaluate depression.23 This well-known depression-screening tool is a listed assessment measurement in the evaluation of vulvodynia.2 Each of the 8 items on interest, feeling, sleep, energy, appetite, concentrating, and movement are rated on a 4-point Likert scale, with 0 indicating “not at all,” 1 “several days,” 2 “more than half the days,” and 3 “nearly every day.” The clinically significant depression cutoff score is defined as total score greater or equal to 10, which corresponds to moderate depression.23,24
Statistics
The PASS-20 total score and PHQ-8 score were calculated for each participant. Pain-related anxiety was recorded as “0” if total PASS-20 score was less than or equal to 30 and “1” if PASS-20 score was greater than 30. Depression was recorded as “0” if total PHQ-8 score was less than 10 and “1” if PHQ-8 was greater or equal to than 10. Patient subjective history regarding previously attempted treatments including anxiolytics, antidepressants, counseling, pelvic floor physical therapy, botulinum toxin injections, or diazepam suppositories was recorded.
Data were analyzed using SPSS 24.0 statistical software. Summary statistics were calculated for PASS-20 and PHQ-8 total scores. Chi-square test of independence was performed between pain-related anxiety and depression. Chi-square test of association performed between whether prior treatment was attempted and whether patient had pain-related anxiety and/or depression. Phi value was calculated to determine strength of association. A P-value of less than 0.05 was considered significant.
Results
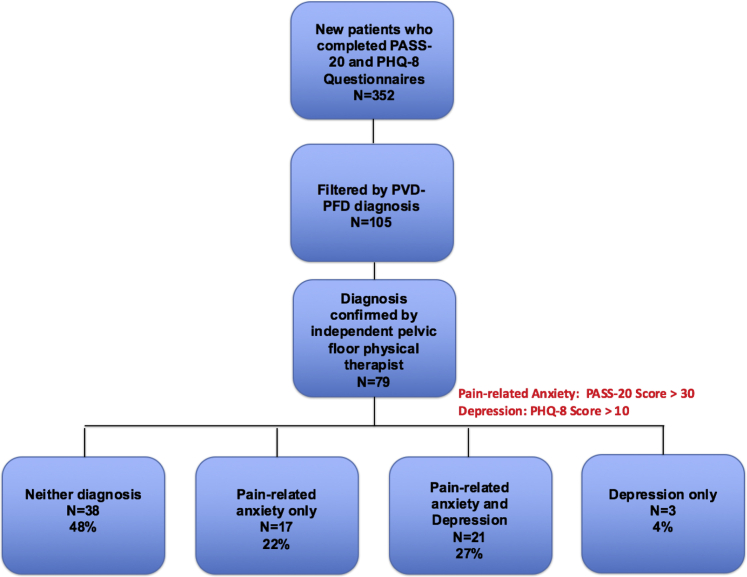
A total of 352 patient charts were reviewed. 79 women were included in the analysis (Figure 1). As shown in Table 1, women with confirmed PVD-PFD had a mean pain-related anxiety (PASS-20) score of 33.53 (SD = 19.68) and a mean depression (PHQ-8) score of 7.57 (standard deviation = 6.77). Of 79, 17 (22%) women met criteria for pain-related anxiety alone, 3 (4%) women for depression alone, and 21 (27%) women for both anxiety and depression. There was a statistically significant association between anxiety and depression in women with PVD-PFD χ2(1) = 21.44, P < .0005, phi = 0.521 (Table 2).
Figure 1.
Observed anxiety and depression in new patients with vulvodynia with associated overactive pelvic floor muscle dysfunction. 79 patients with PVD-PFD completed PASS-20 and PHQ-8 questionnaires. The cutoff score for pain-related anxiety was PASS-20 score greater than 30. The cutoff score for depression was PHQ-8 score greater than 10. The cutoff scores identified 17 (22%) patients with pain-related anxiety, 3 (4%) patients with depression, and 21 (27%) patients with pain-related anxiety and depression. PASS-20 = Pain Anxiety Symptoms Scale-20; PHQ-8 = Patient Health Questionnaire 8; PVD-PFD = provoked vestibulodynia with associated overactive pelvic floor muscle dysfunction.
Table 1.
Summary Statistics
| Questionnaire | Sample size | Minimum | Maximum | Mean | Standard deviation |
|---|---|---|---|---|---|
| PHQ-8 | 79 | 0 | 24 | 7.57 | 0.76 |
| PASS-20 | 79 | 0 | 85 | 33.53 | 2.21 |
79 patients with provoked vestibulodynia with associated overactive pelvic floor muscle dysfunction completed questionnaires. The maximum possible PHQ-8 score is 30 with a depression cutoff score of 10. PHQ-8 scores ranged from 0 to 24 with mean 7.57 and standard deviation 0.76 points. Maximum possible PASS-20 score is 100 with pain-related anxiety cut-off score of 30. PASS-20 scores ranged from 0 to 85 with mean 33.53 and standard deviation 2.21 points.
PASS-20 = Pain Anxiety Symptoms Scale-20; PHQ-8 = Patient Health Questionnaire 8.
Table 2.
Data for chi-square test of Association
| Depression |
|||
|---|---|---|---|
| No | Yes | Total | |
| Anxiety | |||
| No | |||
| Count | 38 | 3 | 41 |
| Expected | 28.5 | 12.5 | 41 |
| % within anxiety | 92.7 | 7.3 | 100 |
| % within depression | 69.1 | 12.5 | 51.9 |
| % total | 48.1 | 3.8 | 51.9 |
| Yes | |||
| Count | 17 | 21 | 38 |
| Expected | 26.5 | 11.5 | 38 |
| % within anxiety | 44.7 | 55.3 | 100 |
| % within depression | 30.9 | 87.5 | 48.1 |
| % total | 21.5 | 26.6 | 48.1 |
| Total | |||
| Count | 55 | 24 | 79 |
| Expected | 55 | 24 | 79 |
| % within anxiety | 69.6 | 30.4 | 100 |
| % within depression | 100 | 100 | 100 |
| % total | 69.6 | 30.4 | 100 |
| Chi square tests | Value | Df | Asymptotic significance (2-sided) | Exact significance (2-sided) | Exact significance (1-sided) |
|---|---|---|---|---|---|
| Pearson chi square | 21.435∗ | 1 | 0.000 | ||
| Continuity correction | 19.228 | 1 | 0.000 | ||
| Likelihood ratio | 23.297 | 1 | 0.000 | ||
| Fischer's exact test | 0.000 | 0.000 | |||
| Linear-by-linear association | 21.164 | 1 | 0.000 |
| Symmetric measures | Value | Approximate significance | |
|---|---|---|---|
| Nominal by nominal | Phi | 0.521 | 0.000 |
| Cramer's V | 0.521 | 0.000 | |
A chi-square test of association was conducted between anxiety and depression diagnoses. All expected cell frequencies were greater than 5. There was a statistically significant association between anxiety and depression within the patients, ˕χ2(1) = =21.435, P < 0.0005. There was a very strong association between anxiety and depression in these patients, phi = =0.521, P < 0.0005.
0 cells (0.0%) have expected count less than 5. The minimum expected count is 5.32.
When examining treatments for affective disorder in this population, 49% of women had previously used anxiolytics and/or antidepressants and 22% had participated in counseling. In regard to treatments for pelvic pain, 43% had previously engaged in physical therapy, 37% had used diazepam suppositories, and 18% had undergone off-label pelvic floor (levator ani) botulinum toxin injections. In regard to prior treatments, 28% of women attempted 1 treatment, 17% attempted 2, 13% attempted 3, 13% attempted 4, and 4% of women attempted 5 prior treatments (Table 3). There was a statistically significant association between anxiety and/or depression and whether prior treatment was attempted χ2 (2) = 6.81, P = .03, phi = 0.294 (Table 4).
Table 3.
Prior treated patient subjective regarding prior treatments was recorded
| Prior treatments | Psychotropics | Counseling | Physical therapy | Diazepam suppositories | Botulinum injections |
|---|---|---|---|---|---|
| % of patients | 49 | 22 | 43 | 37 | 18 |
| # Prior treatments | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| % of patients | 28 | 17 | 13 | 13 | 4 |
Table 4.
Data for Chi-square test of Independence
| Prior treatment attempted |
|||
|---|---|---|---|
| No | Yes | Total | |
| Psychological disorder diagnoses | |||
| None | |||
| Count | 15 | 23 | 38 |
| Expected Count | 10.1 | 27.9 | 38 |
| % within number of psychological diagnoses | 39.5 | 60.5 | 100 |
| % within prior treatment attempted | 71.4 | 39.7 | 48.1 |
| % total | 19 | 29.1 | 48.1 |
| Adjusted residual | 2.5 | −2.5 | |
| 1 | |||
| Count | 4 | 16 | 20 |
| Expected count | 5.3 | 14.7 | 20 |
| % within number of psychological diagnoses | 20 | 80 | 100 |
| % within prior treatment attempted | 19 | 27.6 | 25.3 |
| % total | 5.1 | 20.3 | 25.3 |
| Adjusted residual | −0.8 | 0.8 | |
| Both | |||
| Count | 2 | 19 | 21 |
| Expected count | 5.6 | 15.4 | 21 |
| % within number of psychological diagnoses | 9.5 | 90.5 | 100 |
| % within prior treatment attempted | 9.5 | 32.8 | 26.6 |
| % total | 2.5 | 24.1 | 26.6 |
| Adjusted residual | −2.1 | 2.1 | |
| Total | |||
| Count | 21 | 58 | 79 |
| Expected count | 21 | 58 | 79 |
| % within number of psychological diagnoses | 26.6 | 73.4 | 100 |
| % within prior treatment attempted | 100 | 100 | 100 |
| % total | 26.6 | 73.4 | 100 |
| Chi-square tests | Value | Df | Asymptotic significance (2-sided) |
|---|---|---|---|
| Pearson Chi-square | 6.811∗ | 2 | 0.033 |
| Likelihood Ratio | 7.284 | 2 | 0.026 |
| Linear-by-linear Association | 6.575 | 1 | 0.01 |
| Symmetric measures | Value | Approximate significance | |
|---|---|---|---|
| Nominal by nominal | Phi | 0.294 | 0.033 |
| Cramer's V | 0.294 | 0.033 | |
A chi square test of independence was conducted between number of psychological diagnoses and whether prior treatment was attempted by the patient. All expected cell frequencies were greater than 5. There was a statistically significant association between number of psychological diagnoses and whether prior treatment was attempted by the patient, χ2 (2) = 6.811, P = .033. There was a very strong association between number of psychological diagnoses and whether prior treatment was attempted, phi = 0.294, P = .033
0 cells (0.0%) have expected count less than 5. The minimum expected count is 5.32.
Discussion
This study was conducted to explore the prevalence of pain-related anxiety and depression in women with PVD-PFD. We found that 49% of women with PVD-PFD experienced pain-related anxiety, with or without depression. In addition, there was a statistically significant association between attempt at prior treatment and greater pain-related anxiety and depression.
This is the first study to report a rate of pain-related anxiety in women with vestibulodynia with associated overactive pelvic floor muscle dysfunction. These findings are consistent with studies showing a correlation between pain-related anxiety and chronic pain, especially musculoskeletal conditions such as lower back pain and fibromyalgia.18,21,22,25,26 However, the prevalence of pain-related anxiety in these specific chronic pain populations is not clear. Although the rate of pain-related anxiety in women in general is not known, those without chronic pain demonstrate a lower mean pain-related anxiety score (24.0) than mean scores of samples with chronic pain (38.6).25,26
Researchers have explored the cycle of pain-related anxiety and the role of anxiety sensitivity to the development of chronic pain. Stimulation of pain receptors (nociceptors) leads humans to attribute meaning to unpleasant sensations. Acute pain results in behavioral restriction and avoidance, followed by a gradual increase in activity as pain sensations lessen. Acute pain-related sensations may also be interpreted as catastrophic, leading to increased pain-related anxiety, avoidance, and compulsions, which promote and maintain limitations on activity and the pain sensation itself.27 For patients with anxiety disorders, the pain sensation more quickly triggers avoidance and compulsions, which increase anxiety and further promote the fear-anxiety-avoidance cycle. This is believed to play a role in the development and maintenance of chronic pain and pain-related anxiety.22,28
There may be a larger anxiety and depression component when the cause of chronic pain is unknown. Studies have found that women with vulvodynia were more likely to experience anxiety compared with women with other vulvar pathology with an identified physical cause.10,14 The measures of anxiety and depression in this study were assessed before consultation and diagnosis of overactive pelvic floor muscle dysfunction. It would be interesting to evaluate how treatment affects rates of pain-related anxiety. In a small prospective study, 13 women with PVD were treated with pelvic floor physical therapy and then assessed for symptomatic improvement and pain-related anxiety. After treatment, the women had lower pain ratings during pelvic examination, decreased pain with intercourse, and improved overall sexual function. The treated women also had significantly less pain-related anxiety and pain catastrophizing, although measures of their mental health in general did not improve.17 These results support the idea that pain-related anxiety differs from other anxiety disorders and mood disorders. Future research should explore this concept further in women with PVD and overactive pelvic floor dysfunction.
Another factor that may play a role in pain-related anxiety and depression in the setting of vulvodynia is the number of attempted and failed treatments. This study found that women who arrived for consultation after failed treatments showed higher rates of pain-related anxiety and depression. Many different treatments are tried in the setting of vulvodynia. Oftentimes, these treatments are not directed by determining the cause of vulvar pain. Treatment options vary widely between systemic antidepressants and anticonvulsants to topical preparations to pelvic floor physical therapy to surgical interventions. Determining a dermatologic, neural, muscular, or hormonal cause of vulvar pain in a stepwise approach often focuses treatment modalities. This prevents a “shotgun” approach that often leads to treatment failures. It is unclear whether multiple treatment approaches contribute to increased pain-related anxiety and depression or whether the psychological component contributes to perceived treatment failure.
The present study was not designed to determine cause-effect relationships between PVD-PFD and anxiety or depression. Studies that have explored this relationship indicate that preexisting anxiety and depression play a role in the development and maintenance of vulvodynia. In a community-based epidemiologic study of 240 case-control pairs of women with and without vulvodynia, vulvar pain was 4 times more likely in women with preexisting anxiety and/or depression. In addition, data indicate that vulvodynia causes a greater likelihood of both new and recurrent onset of anxiety and mood disorder symptoms.16 However, this relatively large epidemiologic study has the limitation of including women with vulvar pain by interview, without confirmatory examination for a majority of the participants. In addition, the previous study evaluated general anxiety and not pain-related anxiety, which may have a different mechanism in chronic pain.
Although a temporal relationship and causation cannot be determined, the present study has the strength of only including women with a diagnosis of PVD with associated overactive pelvic floor dysfunction, confirmed by both a physician and pelvic floor physical therapist. Another strength of this study is the use of validated questionnaires for pain-related anxiety and depression. A weakness of the present study is lack of data on preexisting anxiety and mood disorders, other chronic pain conditions, as well as components of chronic pain, including duration of disease and other demographic factors. These factors may play a role in pain characteristics and seeking previous treatment.29
Conclusion
Determining the prevalence of pain-related anxiety and depression in women with PVD-PFD is the first step in optimizing treatment. Research shows that pain-related anxiety plays a role in exacerbating and prolonging chronic pain symptoms, especially in individuals with antecedent anxiety and mood disorders. Identifying overactivity of the pelvic floor muscles as a cause or contributing factor to PVD may help alleviate pain-related anxiety by lessening the fear of the unknown and reducing catastrophizing tendencies. In addition, it is essential to identify and manage pain-related anxiety, as well as baseline anxiety and mood disorders. Cognitive behavioral therapy is the most commonly used and researched psychological treatment modality available. A multidisciplinary combination of pelvic floor physical therapy, psychological intervention, and medical adjuncts for pelvic floor relaxation may provide a good starting point for treatment of PVD-PFD.
Statement of authorship
Category 1
-
(a)Conception and Design
- Vaishnavi Govind; Jill M. Krapf; Leia Mitchell; Karissa Barela; Hillary Tolson; Jaqueline Casey; Andrew T. Goldstein
-
(b)Acquisition of Data
- Vaishnavi Govind; Jill M. Krapf; Leia Mitchell; Karissa Barela; Hillary Tolson; Jaqueline Casey; Andrew T. Goldstein
-
(c)Analysis and Interpretation of Data
- Vaishnavi Govind; Jill M. Krapf; Leia Mitchell; Karissa Barela; Hillary Tolson; Jaqueline Casey; Andrew T. Goldstein
Category 2
-
(a)Drafting the Article
- Vaishnavi Govind; Jill M. Krapf; Leia Mitchell; Karissa Barela; Hillary Tolson; Jaqueline Casey; Andrew T. Goldstein
-
(b)Revising It for Intellectual Content
- Vaishnavi Govind; Jill M. Krapf; Leia Mitchell; Karissa Barela; Hillary Tolson; Jaqueline Casey; Andrew T. Goldstein
Category 3
-
(a)Final Approval of the Completed Article
- Vaishnavi Govind; Jill M. Krapf; Leia Mitchell; Karissa Barela; Hillary Tolson; Jaqueline Casey; Andrew T. Goldstein
Footnotes
Conflict of Interest: The authors report no conflicts of interest.
Funding: None.
References
- 1.Bornstein J., Goldstein A.T., Stockdale C.K. 2015 ISSVD, ISSWSH, and IPPS consensus terminology and classification of persistent vulvar pain and vulvodynia. J Sex Med. 2016;13:607. doi: 10.1016/j.jsxm.2016.02.167. [DOI] [PubMed] [Google Scholar]
- 2.Goldstein A.T., Pukall C.F., Brown C. Vulvodynia: assessment and treatment. J Sex Med. 2016;13:572. doi: 10.1016/j.jsxm.2016.01.020. [DOI] [PubMed] [Google Scholar]
- 3.Thibault-Gagnon S., Morin M. Active and passive components of pelvic floor muscle tone in women with provoked vestibulodynia: a perspective based on a review of the literature. J Sex Med. 2015;12:2178. doi: 10.1111/jsm.13028. [DOI] [PubMed] [Google Scholar]
- 4.Morin M., Binik Y.M., Bourbonnais D. Heightened pelvic floor muscle tone and altered contractility in women with provoked vestibulodynia. J Sex Med. 2017;14:592–600. doi: 10.1016/j.jsxm.2017.02.012. [DOI] [PubMed] [Google Scholar]
- 5.Morin M., Bergeron S., Khalifé S. Morphometry of the pelvic floor muscles in women with and without provoked vestibulodynia using 4D ultrasound. J Sex Med. 2014;11:776–785. doi: 10.1111/jsm.12367. [DOI] [PubMed] [Google Scholar]
- 6.Gentilcore-Saulnier E., McLean L., Goldfinger C. Pelvic floor muscle assessment outcomes in women with and without provoked vestibulodynia and the impact of a physical therapy program. J Sex Med. 2010;7:1003–1022. doi: 10.1111/j.1743-6109.2009.01642.x. [DOI] [PubMed] [Google Scholar]
- 7.Reissing E.D., Brown C., Lord M.J. Pelvic floor muscle function in women with vulvar vestibulitis syndrome. J Psychosom Obstet Gynaecol. 2005;26:107–113. doi: 10.1080/01443610400023106. [DOI] [PubMed] [Google Scholar]
- 8.Benoit-Piau J., Bergeron S., Brassard A. Fear-avoidance and pelvic floor muscle function are associated with pain intensity in women with vulvodynia. Clin J Pain. 2018;34:804. doi: 10.1097/AJP.0000000000000604. [DOI] [PubMed] [Google Scholar]
- 9.Carleton R.N., Abrams M.P., Asmundson G.J. Pain-related anxiety and anxiety sensitivity across anxiety and depressive disorders. J Anxiety Disord. 2009;23:791. doi: 10.1016/j.janxdis.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 10.Stewart D.E., Reicher A.E., Gerulath A.H. Vulvodynia and psychological distress. Obstet Gynecol. 1994;84:587. [PubMed] [Google Scholar]
- 11.Nylanderlundqvist E., Bergdahl J. Vulvar vestibulitis: evidence of depression and state anxiety in patients and partners. Acta Derm Venereol. 2003;83:369. doi: 10.1080/00015550310003764. [DOI] [PubMed] [Google Scholar]
- 12.Arnold L.D., Bachmann G.A., Rosen R. Assessment of vulvodynia symptoms in a sample of US women: a prevalence survey with a nested case control study. Am J Obstet Gynecol. 2007;196:128. doi: 10.1016/j.ajog.2006.07.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Granot M., Lavee Y. Psychological factors associated with perception of experimental pain in vulvar vestibulitis syndrome. J Sex Marital Ther. 2005;31:285. doi: 10.1080/00926230590950208. [DOI] [PubMed] [Google Scholar]
- 14.Wylie K., Hallam-Jones R., Harrington C. Psychological difficulties within a group of patients with vulvodynia. J Psychosom Obstet Gynecol. 2004;25:257. doi: 10.1080/01674820400024463. [DOI] [PubMed] [Google Scholar]
- 15.Masheb R.M., Wang E., Lozano C. Prevalence and correlates of depression in treatment-seeking women with vulvodynia. J Obstet Gynecol. 2005;25:786. doi: 10.1080/01443610500328199. [DOI] [PubMed] [Google Scholar]
- 16.Khandker M., Brady S.S., Vitonis A.F. The influence of depression and anxiety on risk of adult onset vulvodynia. J Womens Health. 2011;20:1445. doi: 10.1089/jwh.2010.2661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goldfinger C., Pukall C.F., Thibault-Gagnon S. Effectiveness of cognitive-behavioral therapy and physical therapy for provoked vestibulodynia: a randomized pilot study. J Sex Med. 2016;13:88. doi: 10.1016/j.jsxm.2015.12.003. [DOI] [PubMed] [Google Scholar]
- 18.Abrams M.P., Carleton R.N., Asmundson G.J. An exploration of the psychometric properties of the PASS-20 with a nonclinical sample. J Pain. 2007;8:879. doi: 10.1016/j.jpain.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 19.McCracken L.M., Dhingra L. A short version of the Pain Anxiety Symptoms Scale (PASS-20): preliminary development and validity. Pain Res Manag. 2002;7:45. doi: 10.1155/2002/517163. [DOI] [PubMed] [Google Scholar]
- 20.Ventolini G. Measuring treatment outcomes in women with vulvodynia. J Clin Med Res. 2011;3:59. doi: 10.4021/jocmr526w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Coons M.J., Hadjistavropoulos H.D., Asmundson G.J.G. Factor structure and psychometric properties of the Pain Anxiety Symptoms Scale-20 in a community physiotherapy clinic sample. Eur J Pain. 2004;8:511. doi: 10.1016/j.ejpain.2003.11.018. [DOI] [PubMed] [Google Scholar]
- 22.Roelofs J., McCracken L., Peters M.L. Psychometric evaluation of the pain anxiety symptoms scale (PASS) in chronic pain patients. J Behav Med. 2004;27:167. doi: 10.1023/b:jobm.0000019850.51400.a6. [DOI] [PubMed] [Google Scholar]
- 23.Kroenke K., Spitzer R.L. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann. 2002;32:509. [Google Scholar]
- 24.Kroenke K., Strine T.W., Spitzer R.L. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114:163. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 25.McCracken L.M., Faber S.D., Janeck A.S. Pain-related anxiety predicts non-specific physical complaints in persons with chronic pain. Behav Res Ther. 1998;36:621–630. doi: 10.1016/s0005-7967(97)10039-0. [DOI] [PubMed] [Google Scholar]
- 26.Zvolensky M.J., Goodie J.L., McNeil D.W. Anxiety sensitivity in the prediction of pain-related fear and anxiety in a heterogeneous chronic pain population. Behav Res Ther. 2001;39:683–696. doi: 10.1016/s0005-7967(00)00049-8. [DOI] [PubMed] [Google Scholar]
- 27.Asmundson G.J., Wright K.D. Biopsychosocial approaches to pain. In: Hadjistavropoulos T., Craig K.D., editors. Psychological perspectives. Lawrence Erlbaum Associates, Inc; Mahwah, NJ: 2004. pp. 35–57. [Google Scholar]
- 28.Asmundson G.J., Vlaeyen J.W., Vlaeyen J.W., editors. Understanding and treating fear of pain. Oxford University Press; USA: 2004. [Google Scholar]
- 29.Lester R.A.1, Brotto L.A.2, Sadownik L.A.2. Provoked vestibulodynia and the health Care Implications of Comorbid pain conditions. J Obstet Gynaecol Can. 2015 Nov;37:995–1005. doi: 10.1016/s1701-2163(16)30049-4. [DOI] [PubMed] [Google Scholar]