Abstract
Introduction
Smartphone-delivered healthcare interventions allow patients to access services on demand when needed, improving motivation and compliance. However, the use of mobile health apps has been scarcely explored in sexual medicine.
Aim
To evaluate the effects of integrating psychological treatment for premature ejaculation (PE) with a mobile coaching app that offers therapeutic exercises on the patient’s smartphone.
Methods
This study comprised 35 heterosexual men with primary psychogenic PE (mean age 34 years, standard deviation = 9.15). All patients entered a cycle of 15 sessions of psychodynamic psychotherapy integrating behavioral therapy, each lasting about 45 minutes. The patients were randomly assigned to 2 groups, each of which performed daily homework exercises (physiotherapy exercises for reinforcing the pelvic floor muscles and cognitive exercises for distancing from sexual failure.) The first group (15 patients) received verbal and printed instructions only (treatment as usual—TAU), whereas the second group (17 patients) experienced the exercises with guidance from the mobile app (app). In both groups, the exercises started after the seventh session. Patients were advised to perform the exercises 3 times a day for 3 months.
Main Outcome Measures
The primary outcome measures were the Premature Ejaculation Diagnostic Tool and the Premature Ejaculation Profile.
Results
Analysis of the data revealed significant pre-post improvements in Premature Ejaculation Diagnostic Tool and Premature Ejaculation Profile scores for the app group compared with those of the TAU group (P < .01). The frequency of patients with no-PE condition for the app group after treatment was significantly higher than the frequency of patients with no-PE condition for the TAU group (P < .001).
Conclusion
Results suggest that a mobile coaching app performs better than TAU in improving both the behavioral skills of ejaculatory delay and sexual self-confidence within a psychological treatment for PE. Future studies should collect follow-up data and explore the potential of mobile coaching apps in combined pharmacotherapy and psychotherapy interventions.
Optale G, Burigat S, Chittaro L. et al. Smartphone-Based Therapeutic Exercises for Men Affected by Premature Ejaculation: A Pilot Study. J Sex Med 2020;8:461–471.
Key Words: Premature Ejaculation, Smartphone, App, Mobile, Coaching, Psychotherapy
Introduction
The International Society for Sexual Medicine defines premature ejaculation (PE) as (i) a male sexual dysfunction characterized by ejaculation that always, or nearly always, occurs within 1 minute of vaginal penetration from the first sexual experience (lifelong type) or (ii) a clinically significant reduction in latency time, often to about 3 minutes or less (acquired type). PE is characterized by the inability to delay ejaculation on all or nearly all vaginal penetrations, resulting in negative personal consequences.1 In addition to being a very frequent sexual dysfunction,2,3 PE has negative consequences both on personal general well-being and on the quality of life of couples in an existing relationship.4, 5, 6
Various psychotherapeutic treatments that integrate psychodynamic, behavioral, and cognitive approaches are available for PE. These are based on the hypothesis that the dysfunction has emotional origins. The guiding approach of these treatments is to learn to control ejaculation both physically and mentally, while understanding the meaning of the symptoms and the context in which they occur.7 These treatments can also be integrated with pharmacotherapy, including local anesthetics8 and/or selective serotonin reuptake inhibitors (SSRIs) that target the depressive psychopathology involved in the disease.9,10
However, therapeutic dropout still occurs,10, 11, 12 even with the pharmacologic use of dapoxetine (the first and only selective serotonin reuptake inhibitor licensed for the treatment of PE). Dropout is likely due to reasons such as an apparent complete absence of effects, an effect that is lower than the patient’s expectations, or a temporary loss of interest in sex because of relational issues with the partner or the side effects of antidepressant drugs.12,13
To improve the outcomes of psychotherapeutic treatments for PE, coaching is also used.7 Coaching interventions typically target resistance to medical interventions that leads to premature discontinuation. Sources of resistance can be emotional, the target of the coaching is to reduce or eliminate performance anxiety; cognitive, the target is to address the psychosocial obstacles that emerge after the onset of the dysfunction; and/or physical, the target is to counter atrophy of the ischiocavernosus muscle.14
However, effective coaching requires time and practice. By providing patients with a technological tool aimed at overcoming these barriers, clinicians are likely to significantly increase the effectiveness of treatment interventions. As stated by Garcia-Cruz et al15 in their analysis of the use of digital technology related to men’s sexual disorders, the revolution of digital technologies constitutes a new setting for the patient-physician relationship and provides patients with a scenario of privacy and universal access to a vast amount of information.
Specifically, mobile health apps can be used to support individuals in managing their own coaching practice, allowing access to needed services on demand and thus improving motivation and compliance.16
The objective of our study is to determine the effects of integrating psychological treatment for PE with a mobile coaching app that offers therapeutic exercises on the patient’s smartphone. Previous controlled studies using mental health apps17,18 suggest that this technological adjunct could stimulate the patient to engage with and scrupulously perform the prescribed therapeutic exercises. Moreover, by using a smartphone app, the patient can regularly repeat the therapy in a setting of complete privacy,18 which may also help develop selective attention and lay the basis, via mental elaboration, for the internalization of this knowledge.
Starting from the aforementioned premises, this article will explore the following 2 hypotheses:
-
(i)
The use of a mobile coaching app within psychodynamic psychotherapy integrating behavioral therapy will improve the behavioral skills of ejaculatory control;
-
(ii)
The use of a mobile coaching app within psychodynamic psychotherapy integrating behavioral therapy will improve sexual self-confidence.
Material and methods
Participants were recruited from patients who presented to the Male and Female Sexual Dysfunctions clinic of the Regione Veneto, ASL 3, Mestre-Venezia, Italy, between January 2015 and December 2017. The study protocol was approved by the Ethical Committee of the Public Health Service of the Regione Veneto, ASL 3.
Inclusion criteria were the following: 18 years of age or older, meets the diagnostic criteria for lifelong-type PE, lack of comorbidities (including diabetes, cardiovascular disease, and hypertension), stable partner in a heterosexual relationship for at least 3 months, active involvement of the partner in the therapy, and availability of an Android smartphone. Patients with a short frenulum, phimosis, erectile dysfunction, chronic prostatitis, or having been previously treated for PE were not included in the study.
All participants signed a generic consent form required by the Public Health Service of the Regione Veneto, ASL 3, and a specific consent form for the psychodynamic psychotherapy used in the study. Participants who were included in the app group were also required to sign an additional consent form about app data collection.
The following tools were used to perform clinical diagnosis and evaluate sexual health during the study:
-
(i)
The 15-question International Index of Erectile Function (IIEF-15) questionnaire19 is a validated, multidimensional, self-administered tool for the clinical assessment of erectile dysfunction. Questions examine 5 domains of male sexual function (erectile function, orgasmic function, sexual desire, intercourse satisfaction, and overall satisfaction) and are scored on a 0–5 scale;
-
(ii)
The 5-question Premature Ejaculation Diagnostic Tool (PEDT)20 is a short validated self-report measure that facilitates the diagnosis of PE. PEDT questions are related to the characteristics of the ejaculation process (control, frequency, minimal sexual stimulation, distress, and interpersonal difficulty) and are answered on a 5-point Likert-type scale. A PEDT score of ≥9 indicates PE or possible PE;
-
(iii)
The 4-question Premature Ejaculation Profile (PEP)21 is a short validated self-report measure to monitor outcomes of men with PE. PEP questions assess sense of control over ejaculation, distress related to PE, interpersonal difficulty, and satisfaction with sexual intercourse and are answered on a 5-point Likert-type scale. A PEP score of ≤8 indicates PE;
-
(iv)
The intravaginal ejaculatory latency time (IELT)22 is the time taken by a man to ejaculate during vaginal penetration. The IELT was considered pathologic, in accordance with criteria A of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition,23 if the participant ejaculated in less than 1 minute as confirmed by the partner. The IELT has been used at enrollment only to avoid increasing performance anxiety in the couple.
-
(v)
The ten-question Rosenberg self-esteem scale24,25: a validated scale that measures global self-worth by measuring both positive and negative feelings about the self. The Rosenberg self-esteem scale was administered only at enrollment to evaluate self-esteem. Subjects were excluded with a score <15.
-
(vi)
The twelve-question Italian questionnaire for anxiety disorders26 is a validated screening tool for anxiety symptoms. Subjects were excluded with a score of ≥ 6.
-
(vii)
The thirteen-question Italian questionnaire for depression26 is a validated screening tool for depressive symptoms. Subjects were excluded with a score of ≥ 6.
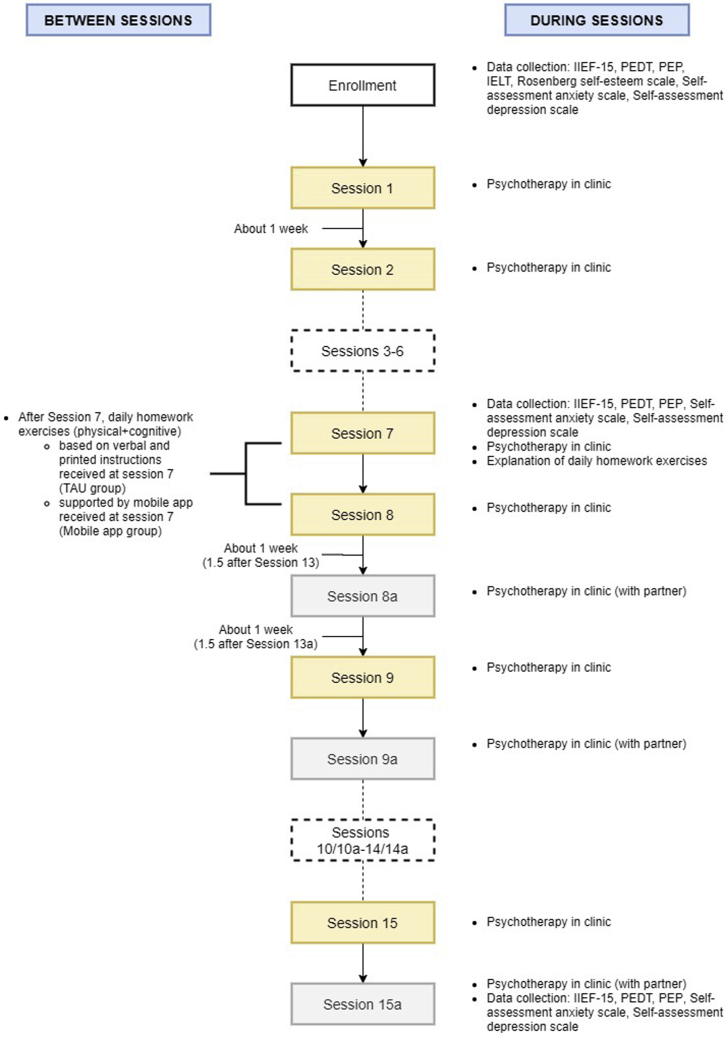
All patients entered a previously validated 15-session cycle (see Figure 1) of psychodynamic psychotherapy integrating behavioral therapy through the use of virtual reality.27,28 Each session lasted about 45 minutes. The therapy targets the multifactorial concept of sexual identity, seen as the outcome of a dynamic fusion of the biological/physical, psychological, and social components of the self. The dynamic aspect involves the possibility that one of the embodied columns of sexual identity (erection, penetration, and ejaculation) may be wounded or even destroyed. In such cases, the focus of psychodynamic therapy is to rebuild them through an embodiment process: the integration of various aspects of self (sensory, affective, and mental) within the structure of the physical body of the person.29 To support this process, the use of virtual reality enables the patient to quickly develop memories and emotions using the body as a channel of expression. These memories and emotions are then worked through with the psychotherapist at the end of the session, with the goal of identifying and addressing blockages that may happen on an emotional and/or cognitive level. As the patient becomes aware that the causes of his sexual dysfunction can be identified and modified in the virtual reality experience, he acquires further means of taking part in the healing process, under the therapist’s guidance.
Figure 1.
Session diagram with indication of the activities carried out during sessions and between sessions. IELT = intravaginal ejaculatory latency time; IIEF-15 = 15-question International Index of Erectile Function; PEDT = Premature Ejaculation Diagnostic Tool; PEP = Premature Ejaculation Profile; TAU = treatment as usual.
Using this approach, treatment aims at allowing the patient to acquire greater control over levels of arousal and ejaculation times. Morevover, it tries to rebuild the patient’s self-esteem, which translates into greater confidence during sexual intercourse, thereby reducing anxiety, causing increased ejaculation latency times, and offering the possibility of greater ease of penetration.
The first 8 sessions were held once a week, the next 5 sessions once every 2 weeks, and the remaining 2 sessions once every 3 weeks, over a minimum of about 25 weeks (see Figure 1). 8 additional Bis sessions (sessions 8a-9a-10a-11a-12a-13a-14a-15a) were held with the sexual partner, after the eighth session, to identify any dysfunctional relationship elements, such as collusion, hostility, sadness, anxiety, anger, or dissatisfaction.
Using simple randomization (randomization based on a single sequence of random assignments30), the patients were divided into 2 groups and were asked to perform daily homework exercises (physiotherapy exercises for reinforcing the pelvic floor muscles and cognitive exercises for distancing from sexual failure), starting after the seventh session.
The first group (15 patients, treatment as usual [TAU]) was given verbal and printed instructions on how to perform (i) 2 physical exercises for strengthening the muscles of the pelvic floor and (ii) 2 mental-distancing exercises that involved copying specific sex-related self-esteem sentences (see Table 1) on a sheet of paper and then erasing them. Participants were advised to perform these activities 3 times a day (a total of 12 exercises) for 3 months.
Table 1.
The sex-related self-esteem sentences used by the app in the mental distancing exercises
| Sex-related self-esteem sentences |
|---|
| I cannot control my ejaculation |
| If I do not satisfy her sexually, she will leave me |
| I am a sexually inadequate male |
| I feel judged by her |
| She does not need me |
| I do not feel worthy of having her |
| I think I am of little sexual worth |
The second group (17 patients, App) started using a mobile coaching app on their Android smartphones. The app guided the patients through the execution of the 2 physical exercises and 2 mental-distancing exercises. A detailed description of the app is provided in the following paragraph. As for the first group, participants were advised to perform the activities with the support of the app 3 times a day for 3 months.
The mental distancing exercises take inspiration from mindfulness techniques,31, 32, 33, 34 which have been found to provide positive effects not only on general mental health in healthy subjects35 but also on patients with depressive disorder,36 anxiety,37 and post-traumatic stress disorder.38
Clinical assessments (including the filling out of questionnaires) were made at enrollment, at the start of the app cycle (scheduled after the seventh session of psychotherapy), and at the end of the psychotherapeutic cycle.
The Mobile Coaching App
The mobile coaching app supports users in carrying out 10-minute training sessions that comprise 2 physical exercises and 2 mental-distancing exercises. Each training session requires users to carry out the 4 exercises in alternating fashion: first, a physical exercise; then, a mental-distancing exercise, another physical exercise; and finally, another mental-distancing exercise.
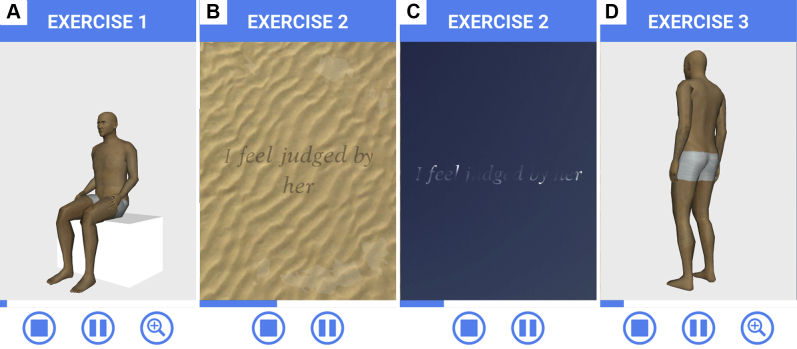
The first exercise in a training session is a physical exercise that requires the user to contract and relax his abdominal muscles 10 times in about 2 minutes. The app guides the user in the correct execution of the exercise through a voice-over that provides verbal instructions and an animated 3-dimensional “avatar” that visually demonstrates the actions to be followed (Figure 2A).
Figure 2.
Example app screens for the training exercises: contraction of the abdomen (A), dissolving sentences written underwater (B), dissolving sentences written as vapor trails (C), contraction of the glutei (D).
Buttons at the bottom of the screen allow the user to quit the exercise, pause/resume it, or zoom in and out on the avatar.
The second exercise in the session requires the user to delete sex-related self-esteem sentences (7 different sentences in 7 days, see Table 1) by repeatedly sliding a fingertip on the smartphone touch screen. During the first week, the app displays sentences as if they were written in ink on a sandy floor underwater, and the user can create waves with his finger to progressively dissolve each sentence (Figure 2B). During the second week, sentences are displayed as vapor trails in the sky, and the user can dissolve them by moving his finger on the screen (Figure 2C). As in the physical exercises, a voice-over provides instructions on how to correctly carry out the mental-distancing exercises.
The third exercise in the session requires the user to contract and relax his gluteus muscles 10 times in about 3 minutes. The app guides the user through the correct execution of the exercise through a voice-over and an animated 3-dimensional “avatar” that visually demonstrates the actions to perform (Figure 2D).
The fourth and final exercise in the session is a repetition of the previous mental-distancing exercise. At the end of this exercise, the user is informed of the number of sessions he still needs to complete during the day to reach 3 sessions per day.
The app captures anonymous usage data and sends it to a secure remote server for storage and later analysis. Captured data consist of the start and end date and time of each exercise as well as the date and time of each additional pausing, resuming, and stopping action performed by users in the app.
Statistics
Fisher’s exact test was used to compare the frequency of patients with PE in the 2 groups after treatment.
To analyze questionnaire data, we used the nonparametric Aligned Rank Transform for a mixed-design model,39 with the treatment group as between-subjects variable (levels: TAU, App) and time as within-subjects variable (levels: enrollment, session 7, and session 15a). The nonparametric Aligned Rank Transform procedure can be used to analyze data that lack homogeneity of variance, as were found in our case with Levene’s test. The post hoc analysis of main effects in case of no interaction between treatment group and time was performed with the adjusted Tukey’s honestly significant difference method. In case of interaction between treatment group and time, the post hoc analysis of simple effects was performed with Wilcoxon signed-rank tests for the within-subjects variable and with Mann-Whitney U tests for the between-subjects variable. In both cases, correction for multiple comparisons was performed using Holm’s sequential Bonferroni procedure.40
Finally, partial correlations were run to find relationship between PEDT and PEP scores at session 15a and app usage measures (number of training sessions and number of app usage days), while controlling for PEDT and PEP scores at session 7.
For all statistical tests, the significance level (p) was 0.05. All data were analyzed with R version 3.4.0 (R Foundation for Statistical Computing; Vienna, Austria).
Results
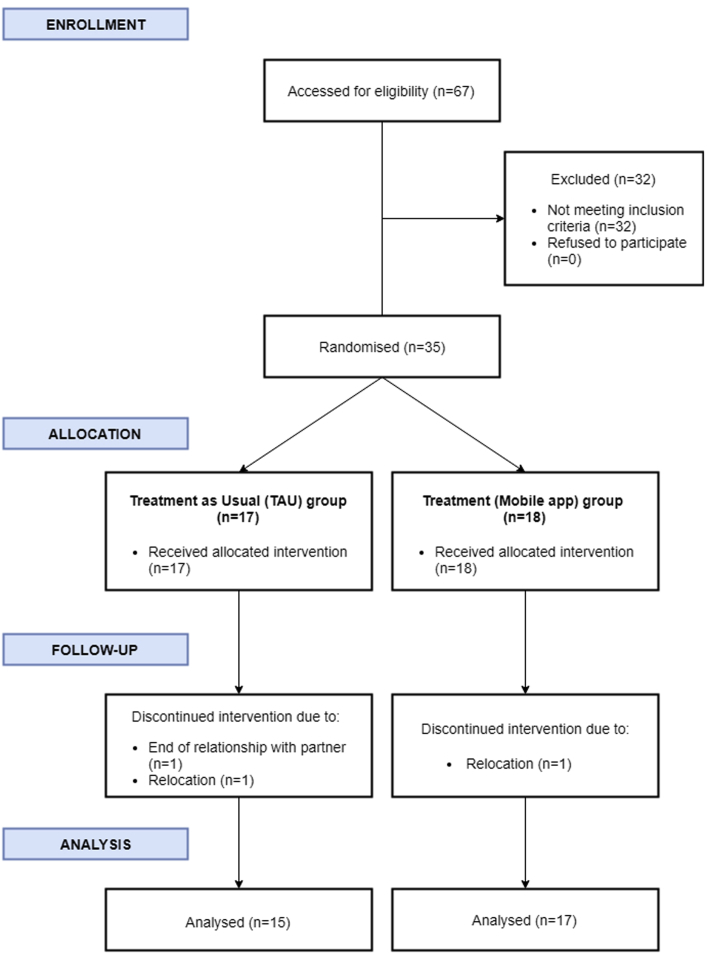
Of the 35 participants who were included in the study (age, M = 34 years, standard deviation [SD] = 9.15), 32 (17 in the app group and 15 in the TAU group) maintained sexual activity with the same partner until the end of the study (Figure 3). 3 patients (1 in the app group and 2 in the TAU group) interrupted the therapeutic cycle before the seventh session for personal reasons (transfer to a different city or end of the relationship with the partner). All participants were Caucasian and had similar characteristics in terms of sociocultural level and relationship duration (>1 year). The following results concern the 32 patients who participated in the study until its end.
Figure 3.
Consort flowchart for the study.
Questionnaire Data
We found a statistically significant difference between the app group and TAU group in the frequency of patients with no-PE condition (PEDT score < 9) at session 15a, with a higher frequency of patients with no-PE condition in the app group (Table 2).
Table 2.
Frequency of patients with PE condition vs patients with no-PE condition at the end of the psychotherapeutic cycle (Session 15a)
| Patients with PE condition |
Patients with no-PE condition |
P Value | |
|---|---|---|---|
| Number (%) | Number (%) | ||
| TAU group | 10 (66.66) | 5 (33.33) | <.001∗,† |
| App group | 1 (5.88) | 16 (94.12) |
Classification based on PEDT scores: PEDT score ≥9 indicates PE or possible PE, PEDT score < 9 indicates no-PE.
PE = premature ejaculation; PEDT = Premature Ejaculation Diagnostic Tool; TAU = treatment-as-usual.
P < .05.
Fisher's exact test.
Analysis of PEDT scores (Table 3) revealed a main effect of treatment group, a main effect of time, and an interaction effect (Table 4). In the post hoc analysis, we found (i) a statistically significant difference between app group and TAU group at session 15a (P < .01), with lower PEDT scores for the app group; (ii) a statistically significant decrease in PEDT score between enrollment and session 7 (P < .05), between session 7 and session 15a (P < .01), and between enrollment and session 15a (P < .01) for the app group; and (iii) a statistically significant decrease in PEDT scores between enrollment and session 15a (P < .01) for the TAU group.
Table 3.
Descriptive statistics of dependent variables PEDT score, PEP score, IIEF-15 subscale scores, anxiety score, depression score for the 2 treatment groups (TAU, App) at 3 different times during the psychotherapeutic cycle (enrollment, session 7, session 15a)
| TAU group |
App group |
|||||
|---|---|---|---|---|---|---|
| Enrollment |
Session 7 |
Session 15a |
Enrollment |
Session 7 |
Session 15a |
|
| Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | |
| PEDT score | 19 (4) | 17 (3.5) | 15 (10) | 18 (5) | 16 (5) | 5 (2) |
| PEP score | 4 (2.5) | 4 (4) | 6 (6.5) | 4 (3) | 5 (2) | 12 (2) |
| IIEF-15 EF score | 29 (1.5) | 29 (1.5) | 29 (2) | 29 (2) | 29 (3) | 30 (2) |
| IIEF-15 IS score | 7 (3.5) | 8 (4.5) | 10 (3.5) | 7 (3) | 7 (3) | 11 (0) |
| IIEF-15 OF score | 10 (0.5) | 10 (0) | 10 (0) | 10 (0) | 10 (0) | 10 (0) |
| IIEF-15 SD score | 7 (2) | 7 (1.5) | 7 (2) | 8 (3) | 7 (2) | 8 (1) |
| IIEF-15 OS score | 4 (2) | 5 (3.5) | 4 (6) | 4 (3) | 4 (3) | 8 (1) |
| Anxiety score | 2 (1) | 2 (1.5) | 2 (1.5) | 1 (2) | 1 (2) | 0 (2) |
| Depression score | 3 (3) | 2 (4) | 1 (1.5) | 1 (3) | 1 (2) | 0 (1) |
Possible score ranges: PEDT (0–20), PEP (0–16), IIEF-15 EF (0–30), IIEF-15 IS (0–15), IIEF-15 OF (0–10), IIEF-15 SD (0–10), IIEF-15 OS (0–10), Anxiety (0–12), Depression (0–13).
EF = Erectile Function; IIEF = International Index of Erectile Function; IQR = interquartile range; IS = Intercourse Satisfaction; OF = Orgasmic Function; OS = Overall Satisfaction; PEDT = Premature Ejaculation Diagnostic Tool; PEP = Premature Ejaculation Profile; SD = Sexual Desire; TAU = treatment-as-usual.
Table 4.
Effects of treatment group and time on dependent variables PEDT score, PEP score, IIEF-15 subscale scores, anxiety score, depression score
| Group |
Time |
Group∗time |
||||
|---|---|---|---|---|---|---|
| F (1, 30) | P value | F (2, 60) | P value | F (2, 60) | P value | |
| PEDT score | 19.03 | <.001∗,† | 97.30 | <.001∗,† | 13.87 | <.001∗,† |
| PEP score | 9.61 | <.01∗,† | 64.43 | <.001∗,† | 14.07 | <.001∗,† |
| IIEF-15 EF score | 0.06 | .81† | 1.04 | .36† | 2.67 | .08† |
| IIEF-15 IS score | 0.00 | .98† | 25.64 | <.001∗,† | 6.18 | <.01∗,† |
| IIEF-15 OF score | 0.08 | .78† | 1.97 | .15† | 1.07 | .35† |
| IIEF-15 SD score | 2.84 | .10† | 1.41 | .25† | 0.37 | .69† |
| IIEF-15 OS score | 1.04 | .32† | 19.00 | <.001∗,† | 12.35 | <.001∗,† |
| Anxiety score | 1.60 | .22† | 2.11 | .13† | 0.77 | .47† |
| Depression score | 2.25 | .14† | 14.01 | <.001∗,† | 0.57 | .57† |
The table shows main effects (group, time) and interaction (group∗time). Headings of F columns show the degrees of freedom for the considered effect.
EF = Erectile Function; IIEF = International Index of Erectile Function; IS = Intercourse Satisfaction; OF = Orgasmic Function; OS = Overall Satisfaction; PEDT = Premature Ejaculation Diagnostic Tool; PEP = Premature Ejaculation Profile; SD = Sexual Desire.
P < .05.
2-way factorial ANOVA of Aligned Rank Transformed data.
Analysis of PEP scores (Table 3) revealed a main effect of treatment group, a main effect of time, and an interaction effect (Table 4). In the post hoc analysis, we found (i) a statistically significant difference between app group and TAU group at session 15a (P < .01), with higher PEP scores for the app group, and (ii) a statistically significant increase in PEP scores between session 7 and session 15a (P < .01) and between enrollment and session 15a (P < .01) for the app group.
Analysis of the IIEF-15 subscales scores (Table 3) revealed significant effects for Intercourse Satisfaction (IS) and Overall Satisfaction (OS).
For the IS subscale, we found no main effect of treatment group, a main effect of time, and an interaction effect (Table 4). Post hoc analysis revealed a statistically significant increase in IS scores between session 7 and session 15a (P < .05) and between enrollment and session 15a (P < .05) for the app group.
For the OS subscale, we found no main effect of treatment group, a main effect of time, and an interaction effect (Table 4). Post hoc analysis revealed (i) a statistically significant difference between the app group and TAU group at session 15a (P < .05), with higher OS scores for the app group, and (ii) a statistically significant increase in OS scores between session 7 and session 15a (P < .01) and between enrollment and session 15a (P < .01) for the app group.
Finally, analysis of the psychological variables (Table 3) revealed a main effect of time in the depression questionnaire (Table 4): there was a statistically significant decrease in the depression score between session 7 and session 15a (P < .001) and between enrollment and session 15a (P < .001) for both the app and TAU groups.
App Usage Data
The number of app training sessions ranged from 15 to 269 (M = 94.93, SD = 72.73), the number of app use days ranged from 8 to 102 (M = 45.07, SD = 27.97), and the number of daily app sessions was on average 2 (SD = 0.51). Partial correlation analysis revealed small-to-moderate correlation coefficients between PEDT and PEP scores at session 15a and app use data (Table 5). However, the effects did not reach statistical significance.
Table 5.
Partial correlation of app use data (number of training sessions, app use days) with PEDT and PEP scores at the end of the psychotherapeutic cycle (session 15a), while controlling for PEDT and PEP scores at the start of the app use period (session 7)
| Number of training sessions | App use days | |
|---|---|---|
| PEDT score (Session 15a) | ||
| r | 0.175 | 0.277 |
| P | .58 | .36 |
| PEP score (Session 15a) | ||
| r | −0.403 | −0.417 |
| P | .17 | .16 |
PEDT = Premature Ejaculation Diagnostic Tool; PEP = Premature Ejaculation Profile; r = Pearson's correlation coefficient.
Discussion
A systematic review of behavioral therapies for PE management that included 10 randomized controlled trials found limited evidence that such therapies significantly improve IELT and other outcomes compared with waitlist.41 However, there seems to be a close link between the effectiveness of cognitive behavioral therapy, one of the most used psychotherapy approaches for PE, and the patient’s diligent performance of the prescribed exercises—“homework assignments”—between therapeutic sessions.42
In this study, we sought to investigate whether the use of a mobile coaching app that offers therapeutic exercises on the patient’s smartphone can improve the efficacy of a clinically validated psychodynamic psychotherapy integrating behavioral therapy.27,28
The most significant result of the study was that PEDT and PEP scores in the group using the mobile coaching app were significantly better at the end of the treatment than PEDT and PEP scores in the TAU group. Moreover, the frequency of patients with a PEDT score smaller or equal to 9 at the end of the treatment, indicating a man does not have PE, was remarkably higher in the app group than in the TAU group. The additional effects we found for the IIEF-15 IS and OS subscales and for depression scores further highlight the advantages of the app condition.
These results suggest that the availability of an app supporting patients in the therapeutic exercises produces better outcomes in the long run, in both PE and its psychological correlates. By being always available on demand when the patient feels he needs it, the app becomes a trusted tool that leads to improved motivation and compliance. It encourages the patient to regularly conduct the different exercises and to reflect on the presented experiences, thus integrating PE counseling exercises into daily routines more than traditional verbal and printed instructions ever could. This integration is likely to help the patient rapidly change the negative self-schemas that are activated in response to negative sexual events.43, 44, 45 Research has incontrovertibly established that task-oriented training improves the learning of the trained skill.46 The mobile app’s avatar-guided repetition of physical exercises simplifies exercise execution, leading to improved functionality of the muscles of the pelvic floor, which play an important role in controlling the functionality of sexual activity.47 The constant repetition of visual and motor experiences prompted by the app and performed in complete privacy may facilitate the internalization of positive mental associations of sexual performance in contrast with the negative schemas that hinder patients suffering from PE. The mental exercise component of the mobile app may encourage the patient with PE to distance himself from thoughts of sexual failure through elimination of negative expressions. The app is a means by which images and thoughts can be reworked through cognitive processes that are stimulated by this technological adjunct, with the end goal of increasing patient awareness and thus having greater beneficial results.
The lack of statistical significance for the small-to-moderate correlations between PEDT and PEP scores and app usage data might have been influenced by the relatively low number of participants, but might also suggest that the app had a positive effect on participants not only by supporting them in carrying out the exercises but also because of its mere availability. Having an easy to access and easy to use tool always at their disposal thus might have helped participants.
Overall, the proposed counseling app appears to improve PE therapeutic interventions in the daily lives of patients, helping them to overcome barriers in planning and conducting counseling exercises and, in the end, increasing the effectiveness of clinically validated psychotherapeutic treatments for PE.
A possible limitation of this study is its sample size. However, sample size analysis revealed that we had a large enough sample size to identify a significant difference between the 2 groups. We also exceeded the recommendation by Julious,48 who suggests a minimum sample size of 12 subjects per group for pilot studies.
A second limitation of this study concerns the absence of another group with a different psychotherapeutic approach. However, it is difficult to imagine a group using the app without psychotherapeutic integration, which would also be unethical. Further limitations are that the study protocol did not include a questionnaire designed for partners of men with PE and that group assignment was not blinded to the psychotherapist. Psychosocial factors (eg, whether the partner was new to the participant, whether multiple partners were involved in a committed relationship, how long participants were not having sexual activity, position during sex) could also be confounding factors that may have influenced the final outcome of the study.49 Finally, the study did not include the acquisition of long-term follow-up data.
Conclusions
To the best of our knowledge, this is the first PE study including an app in the clinical protocol. The results of this pilot study support the clinical feasibility of a mobile coaching app that offers therapeutic exercises on the patient’s smartphone. Moreover, collected data suggest that using the app leads to better results than a TAU approach in improving both the behavioral skills of ejaculatory control and sexual self-confidence within a previously validated psychotherapy treatment for PE. Specifically, the app group improved more than the TAU group both in terms of the PEDT and the PEP clinical outcomes.
One possible interpretation of the results is that the support received through the coaching app makes it easier to understand and comply with the prescribed exercises compared to the verbal and printed instructions used in TAU, thus leading to stronger beneficial effects. It is also possible that the mere availability of the app had a positive effect on patients.
This pilot study has limitations, including small initial sample size, a non-blinded group assignment and the lack of follow-up data. These factors will need to be addressed in further, larger studies able to assess the long-term efficacy of the approach and to explore the potential of mobile coaching apps in combined pharmacotherapy and/or psychotherapy interventions.
Statement of authorship
Category 1
-
(a)Conception and Design
- Gabriele Optale; Stefano Burigat; Luca Chittaro; Giuseppe Riva
-
(b)Acquisition of Data
- Gabriele Optale
-
(c)Analysis and Interpretation of Data
- Gabriele Optale; Stefano Burigat; Luca Chittaro
Category 2
-
(a)Drafting the Article
- Gabriele Optale; Stefano Burigat; Luca Chittaro; Giuseppe Riva
-
(b)Revisiting It for Intellectual Content
- Gabriele Optale; Stefano Burigat; Luca Chittaro; Giuseppe Riva
Category 3
-
(a)Final Approval of the Complete Article
- Gabriele Optale, Stefano Burigat, Luca Chittaro, Giuseppe Riva
Footnotes
Conflicts of Interest: The authors report no conflicts of interest.
Funding: None.
References
- 1.Althof S.E., McMahon C.G., Waldinger M.D. An update of the International Society of Sexual Medicine’s guidelines for the diagnosis and treatment of premature ejaculation (PE) J Sex Med. 2014;11:1392–1422. doi: 10.1111/jsm.12504. [DOI] [PubMed] [Google Scholar]
- 2.Porst H., Montorsi F., Rosen R.C. The premature ejaculation prevalence and attitudes (PEPA) survey: prevalence, comorbidities, and professional help-seeking. Eur Urol. 2007;51:816–824. doi: 10.1016/j.eururo.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 3.Saitz T.R., Serefoglu E.C. The epidemiology of premature ejaculation. Transl Androl Urol. 2016;5:409–415. doi: 10.21037/tau.2016.05.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rosen R.C., Althof S. Impact of premature ejaculation: the psychological, quality of life, and sexual relationship consequences. JSM. 2008;5:1296–1307. doi: 10.1111/j.1743-6109.2008.00825.x. [DOI] [PubMed] [Google Scholar]
- 5.Rowland D.L., Patrick D.L., Rothman M. The psychological burden of premature ejaculation. J Urol. 2007;177:1065–1070. doi: 10.1016/j.juro.2006.10.025. [DOI] [PubMed] [Google Scholar]
- 6.Symonds T., Roblin D., Hart K. How does premature ejaculation impact a man’s life? J Sex Marital Ther. 2003;29:361–370. doi: 10.1080/00926230390224738. [DOI] [PubMed] [Google Scholar]
- 7.Althof E.S. Psychological treatment strategies for rapid ejaculation: rationale, practical aspects, and outcome. World J Urol. 2005;23:89–92. doi: 10.1007/s00345-004-0489-6. [DOI] [PubMed] [Google Scholar]
- 8.Martyn-St James M., Cooper K., Ren K. Topical anaesthetics for premature ejaculation: a systematic review and meta-analysis. Sex Health. 2016;13:114–123. doi: 10.1071/SH15042. [DOI] [PubMed] [Google Scholar]
- 9.Waldinger M.D., Hengeveld M.W., Zwinderman A.H. Effect of SSRI antidepressants on ejaculation: a double-blind, randomized, placebo-controlled study with fluoxetine, fluvoxamine, paroxetine, and sertraline. J Clin Psychopharmacol. 1998;18:274–281. doi: 10.1097/00004714-199808000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Park H.J., Park N.C., Kim T.N. Discontinuation of dapoxetine treatment in patients with premature ejaculation: a 2-year prospective observation study. Sex Med. 2017;5:e99–e105. doi: 10.1016/j.esxm.2017.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salonia A., Rocchini L., Pellucchi F. Ejaculatory disorders: acceptance of and discontinuation rate from paroxetine treatment in patients with lifelong premature ejaculation. J Sex Med. 2009;6:2868–2877. doi: 10.1111/j.1743-6109.2009.01404.x. [DOI] [PubMed] [Google Scholar]
- 12.Mondaini N., Fusco F., Cai T. Dapoxetine treatment in patients with lifelong premature ejaculation: the reasons of a “Waterloo”. Urology. 2013;82:620–624. doi: 10.1016/j.urology.2013.05.018. [DOI] [PubMed] [Google Scholar]
- 13.Gelenberg A.J., Delgado P., Nurnberg H.G. Sexual side effects of antidepressant drugs. Curr Psychiatry Rep. 2000;2:223–227. doi: 10.1007/s11920-996-0012-4. [DOI] [PubMed] [Google Scholar]
- 14.Lavoisier P., Roy P., Dantony E. Pelvic-floor muscle rehabilitation in erectile dysfunction and premature ejaculation. Phys Ther. 2014;94:1731–1743. doi: 10.2522/ptj.20130354. [DOI] [PubMed] [Google Scholar]
- 15.García-Cruz E., Romero-Otero J., Fode M. The digital environment in men’s sexual disorders: a systematic review. Actas Urol Esp. 2018;42:365–374. doi: 10.1016/j.acuro.2017.05.008. [DOI] [PubMed] [Google Scholar]
- 16.Neary M., Schueller S.M. State of the field of mental health apps. Cog Behav Pract. 2018;25:531–537. doi: 10.1016/j.cbpra.2018.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miloff A., Marklund A., Carlbring P. The challenger app for social anxiety disorder: new advances in mobile psychological treatment. Internet Interv. 2015;2:382–391. [Google Scholar]
- 18.Lyons E.J., Lewis Z.H., Mayrsohn B.G. Behavior change techniques Implemented in Electronic Lifestyle activity monitors: a systematic content analysis. J Med Internet Res. 2014;16:e192. doi: 10.2196/jmir.3469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rosen R.C., Riley A., Wagner G. The International Index of Erectile Function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–830. doi: 10.1016/s0090-4295(97)00238-0. [DOI] [PubMed] [Google Scholar]
- 20.Symonds T., Perelman M.A., Althof S. Development and validation of a premature ejaculation diagnostic tool. Eur Urol. 2007;52:565–573. doi: 10.1016/j.eururo.2007.01.028. [DOI] [PubMed] [Google Scholar]
- 21.Patrick D.L., Giuliano F., Ho K.F. The Premature Ejaculation Profile: validation of self-reported outcome measures for research and practice. BJU Int. 2009;103:358–364. doi: 10.1111/j.1464-410X.2008.08041.x. [DOI] [PubMed] [Google Scholar]
- 22.Waldinger M.D., Quinn P., Dilleen M. A multinational population survey of intravaginal ejaculation latency time. J Sex Med. 2005;2:492–497. doi: 10.1111/j.1743-6109.2005.00070.x. [DOI] [PubMed] [Google Scholar]
- 23.Dsm – 5, diagnostic and statistical Manual of mental disorders – 5. American Psychiatric Publishing; Washington, DC: 2013. p. 443. [Google Scholar]
- 24.Rosenberg M. Princeton University Press; Princeton, NJ: 1965. Society and adolescent self-image. [Google Scholar]
- 25.Prezza M., Trombaccia F.R., Armento L. La scala dell’autostima di Rosenberg: traduzione e validazione italiana. Bollettino di Psicologia Applicata. 1997;223:35–44. [Google Scholar]
- 26.Cassano G.B., Cecconi D. Questionari di autovalutazione per i disturbi d’ansia e depressione. Quaderni Italiani di Psichiatria. 1995;XIV:86–108. [Google Scholar]
- 27.Optale G., Munari A., Nasta A. Multimedia and virtual reality techniques in the treatment of male erectile disorders. Int J Impot Res. 1997;9:197–203. doi: 10.1038/sj.ijir.3900316. [DOI] [PubMed] [Google Scholar]
- 28.Optale G., Munari A., Nasta A. Virtual environments in the treatment of impotence and premature ejaculation. CyberPsychol Behav. 1998;1:213–216. [Google Scholar]
- 29.Bloom K. Routledge; 2018. The embodied self: Movement and psychoanalysis. [Google Scholar]
- 30.Suresh K. An overview of randomization techniques: an unbiased assessment of outcome in clinical research. J Hum Reprod Sci. 2011;4:8–11. doi: 10.4103/0974-1208.82352. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 31.Chittaro L., Vianello A. Computer-supported mindfulness: evaluation of a mobile thought distancing application on naive meditators. Int J Human-Computer Stud. 2014;72:337–348. [Google Scholar]
- 32.Chittaro L., Vianello A. Mobile mindfulness and user’s worry: a qualitative study of using a smartphone app for distancing from negative thoughts. Interacting Comput. 2016;28:695–717. [Google Scholar]
- 33.Kabat-Zinn J. Delta; New York: 1990. Full catastrophe living: using the wisdom of your body and mind to face stress, pain, and illness. [Google Scholar]
- 34.Williams M., Teasdale J., Segal Z. The Guilford Press; New York: 2007. The mindful way through depression. [Google Scholar]
- 35.Chiesa A., Serretti A. Mindfulness-based stress reduction for stress management in healthy people: a review and meta-analysis. J Altern Complement Med. 2009;15:593–600. doi: 10.1089/acm.2008.0495. [DOI] [PubMed] [Google Scholar]
- 36.Piet J., Hougaard E. The effect of mindfulness-base cognitive therapy for prevention of relapse in recurrent major depressive disorder: a systematic review and meta-analysis. Clin Psychol Rev. 2011;31:1032–1040. doi: 10.1016/j.cpr.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 37.Grossman P., Niemann L., Schmidt S. Mindfulness-based stress reduction and health benefits: a meta-analysis. J Psychosom Res. 2004;57:35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- 38.Bormann J.E., Oman D., Walter K.H. Mindful attention increases and mediates psychological outcomes following mantram repetition practice in veterans with posttraumatic stress disorder. Med Care. 2014;52:S13–S18. doi: 10.1097/MLR.0000000000000200. [DOI] [PubMed] [Google Scholar]
- 39.Wobbrock J.O., Findlater L., Gergle D. Proc. Of the SIGCHI Conference on Human factors in Computing Systems. ACM Press; 2011. The aligned rank transform for nonparametric factorial analyses using only ANOVA procedures; pp. 143–146. [Google Scholar]
- 40.Holm S. A simple sequentially rejective multiple test procedure. Scand J Stat. 1979;6:65–70. [Google Scholar]
- 41.Cooper K., Martyn-St James M., Kaltenthaler E. Behavioral therapies for management of premature ejaculation: a systematic review. Sex Med. 2015;3:174–188. doi: 10.1002/sm2.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McCabe M.P. Evaluation of a cognitive behaviour therapy program for people with sexual dysfunction. J Sex Marital Ther. 2001;27:259–271. doi: 10.1080/009262301750257119. [DOI] [PubMed] [Google Scholar]
- 43.Nobre P.J., Pinto-Gouveia J. Questionnaire of cognitive schema activation in sexual contest: a measure to assess cognitive schemas activated in unsuccessful sexual dysfunctions. J Sex Res. 2009;46:1–13. doi: 10.1080/00224490902792616. [DOI] [PubMed] [Google Scholar]
- 44.Quinta Gomes A.L., Nobre P.J. Early maladaptive schemas and sexual dysfunction in men. Arch Sex Behav. 2012;41:311–320. doi: 10.1007/s10508-011-9853-y. [DOI] [PubMed] [Google Scholar]
- 45.Peixoto M., Nobre P.J. Macho beliefs moderate the association between negative sexual episodes and activation of incompetence schemas in sexual context, in gay and heterosexual men. J Sex Med. 2017;14:518–525. doi: 10.1016/j.jsxm.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 46.Wressle E., Eeg-Olofsson A.M., Marcusson J. Improved client participation in the rehabilitation process using a client-centred goal formulation structure. J Rehabil Med. 2002;34:5–11. doi: 10.1080/165019702317242640. [DOI] [PubMed] [Google Scholar]
- 47.Shafik A. The role of the elevator ani muscle in evacuation, sexual performance and pelvic floor disorders. Int Urogynecol J Pelvic Floor Dysfunct. 2000;11:361–376. doi: 10.1007/pl00004028. [DOI] [PubMed] [Google Scholar]
- 48.Julious S.A. Sample size of 12 per group rule of thumb for a pilot study. Pharmaceut Statist. 2005;4:287–291. [Google Scholar]
- 49.Yusof F., Sidi H., Das S. Understanding the pathophysiology of premature ejaculation: bridging the link between pharmacological and psychological interventions. Curr Drug Targets. 2018;19:856–864. doi: 10.2174/1389450117666161215161108. [DOI] [PubMed] [Google Scholar]