Abstract
Introduction
Endometriosis is a benign gynecological disease with a high disease burden and significant, multifaceted impact on health-related quality of life (HRQoL) and sexual quality of life (SQoL).
Aim
To explore which patient- and disease-specific characteristics were independently associated with SQoL.
Methods
A literature search was carried out to identify characteristics with an evidence-based or hypothesized effect on SQoL. Subsequently, data on HRQoL in women with endometriosis (n = 224), collected between 2013 and 2018 in a prospective longitudinal Dutch cohort study performed in 7 referral centers, were used to perform a cross-sectional cohort study. Data were collected using an online self-administered survey including the validated Endometriosis Health Profile-30. Inclusion criteria were recently diagnosed endometriosis patients or newly referred patients with a clinical diagnosis of endometriosis. Patients were excluded in case of incomplete answers on the SQoL questions. Univariate analyses and multiple linear regression analyses were performed.
Outcomes
SQoL, measured by the 5-item “sexual intercourse” dimension score of the modular Endometriosis Health Profile-30 questionnaire, was the primary outcome with scores ranging from 0 to 100 (0 indicating the best and 100 indicating the worst health status).
Results
Based on a literature search, 29 characteristics potentially associated with SQoL were selected from the survey and included in the analyses. In total, 192 women (mean age 36 years) met the inclusion criteria. The majority of women (86.5%) had had intercourse in the period before completing the survey and the study population showed a mean SQoL score of 47.5 ± 29.6, indicating moderate SQoL. Worse SQoL was independently associated with dyspareunia (P < .001), worse HRQoL (P = .001), severity of dysmenorrhea (P = .017), and unemployed work status (P = .022).
Conclusion
In a cohort of women with endometriosis, worse SQoL was significantly and independently associated with the presence of dyspareunia, more severe dysmenorrhea, worse HRQoL, and unemployed work status.
van Poll M, van Barneveld E, Aerts L, et al. Endometriosis and Sexual Quality of Life. Sex Med 2020;8:532–544.
Key Words: Endometriosis, Sexual Quality of Life, Sexuality, Health-Related Quality of Life, Endometriosis Health Profile-30
Introduction
Endometriosis is a chronic benign gynecological disease. It is defined as the presence of endometrium-like tissue outside the uterine cavity, accompanied by chronic inflammation induced by these ectopic implants.1, 2, 3 Global prevalence of endometriosis is estimated to vary between 2% and 10% in women of reproductive age and up to 50% in women with chronic pelvic pain or fertility problems.2 Endometriosis has a high disease burden4,5 presenting a wide variety of symptoms, including dysmenorrhea, chronic pelvic pain, dyspareunia, dyschezia, dysuria, and subfertility.6
As a result, endometriosis has a significant social and psychological impact, decreasing the patient's quality of life (QoL).7, 8, 9 Affected aspects of life include self-image, private and professional relationships, and sexuality.1,7,10, 11, 12, 13
Several studies have been carried out to evaluate sexual functioning in patients with endometriosis, amongst which the direct impact of dyspareunia has been researched extensively.14, 15, 16, 17, 18, 19 Women with endometriosis and deep dyspareunia have been found to have lower sexual QoL (SQoL), which can present as impaired sexual functioning and decreased satisfaction, which in turn can negatively affect personal relationships.3,10,11,20
Besides dyspareunia, multiple other factors have been identified to contribute to poorer SQoL in women with endometriosis, including depressive symptoms, anxiety, bladder pain syndrome, and heterosexual orientation.15,16,21
A representative measure for the evaluation of SQoL in women with endometriosis is the modular dimension “sexual intercourse” of the Endometriosis Health Profile-30 (EHP-30).22,23 The EHP-30 is a validated questionnaire to measure health-related QoL (HRQoL) in women with endometriosis and it addresses diverse aspects of life, including sexuality.24
The aim of this study is to explore which patient- and disease-specific characteristics are independently associated with SQoL, as measured by one of the dimensions of the EHP-30, in a population of Dutch women with endometriosis. Identifying relevant characteristics that have an influence on SQoL in this population can aid in improving endometriosis consultation addressing sexuality and SQoL.
Material and methods
Study Design
This study is a secondary analysis of a multicenter longitudinal observational study assessing HRQoL in Dutch women with a clinical diagnosis of endometriosis. It aims to explore which patient- and disease-specific characteristics are associated with sexual quality of life (SQoL), which is one of the dimensions of HRQoL. A literature search was conducted to make an inventory of known and potential characteristics of the influence on SQoL. Based on the findings of this literature search, a database search was conducted to explore the influence of specific characteristics associated with SQoL in a Dutch population of women with endometriosis.
Literature Search
A broad search was performed using PubMed in the MEDLINE database with the following free terms: “Endometriosis,” “Sexual quality of life,” “Quality of sex life,” “Sexuality,” “SQoL,” “Sexual life,” “Sex life.” The Medical Subject Headings terms “Endometriosis,” “Quality of life,” “Sex,” and “Sexuality” were added to this search. Titles and abstracts of the resulting 242 hits were screened for eligibility. After screening, 40 relevant articles remained.
Additionally, a search in the Cochrane Library was carried out using the Medical Subject Headings descriptors “Endometriosis” and “Quality of Life.” This search yielded 3 reviews of which only one was relevant to the subject of this study.
Furthermore, of the included articles, reference lists were screened and relevant articles were also included. Full text and English language articles that applied to the subject of this study were read and potential characteristics of the influence on SQoL were identified.
Setting and Participants
The original HRQoL study was carried out in 7 Dutch hospitals, of which 2 are academic hospitals. Ethical approval for this study was obtained from the Ethical Committee of Maastricht University Medical Center+ (azM/UM METC 13-4-034). Eligible women were informed verbally and by information letter about the study. Participants were required to sign an informed consent form before participation in the study.
Women were eligible for the main cohort if they presented at 1 of the gynecological outpatient clinics as a “new endometriosis patient.” This encompassed women with a clinical diagnosis of endometriosis, women with a prior diagnosis of endometriosis who had not undergone new treatment or check-ups for their endometriosis in the preceding year, and women with a second opinion referral status. Clinical diagnosis was made by gynecologists with expertise in the field of endometriosis, based on history, physical examination, and imaging techniques.
For the SQoL analysis, women who underwent subsequent endometriosis surgery during the study period and in whom the diagnosis of endometriosis was rejected were excluded. Furthermore, women were excluded if they did not complete the “sexual intercourse” dimension of the EHP-30 questionnaire or if they scored this dimension to be “not relevant” to them. This was done on the grounds that in these cases a score for the primary outcome, SQoL, could not be calculated.
This SQoL study is the first publication of data from the original HRQoL study, which is still ongoing.
Self-Administered Survey
In the main cohort of the HRQoL study, participants received surveys at fixed time intervals; directly after clinical diagnosis (T0), 6 months after clinical diagnosis (T6), and thereafter annually (T12, T24, T36, T48) in order to assess patient- and disease-specific characteristics and HRQoL during the course of their treatment. For the SQoL analysis, only the survey data from T0 were included.
The self-administered survey comprised 2 parts. The first part pertained to general patient- and disease-specific characteristics to determine the current sociodemographic profile, including questions concerning marital status, education, work, onset of endometriosis complaints and diagnostic pathway, current endometriosis-associated complaints and symptoms, general health and medical history, medication, and fertility. Endometriosis-associated symptoms were measured on a numerical rating scale. Pain intensity was scored on a range from 1 to 10, with 1 representing “no pain at all” and 10 representing “insufferable pain.” The second part of the T0 survey was composed of the Dutch version of the EHP-30; a validated tool to measure the HRQoL in women with endometriosis.22 Validity and reliability of the Dutch version of the EHP-30 have been demonstrated.25,26 Both the core questionnaire of the Dutch EHP-30 as well as the modular questionnaire were presented to the participants.23
Surveys were provided on paper or digitalized. SurveyMonkey (SurveyMonkey Inc, www.surveymonkey.com, San Mateo, CA) was used as a platform to construct the online version of the survey, which was distributed amongst the participants via email. Data from the online survey and on paper responses were exported to create an offline database. In the database, individual study numbers were assigned to every patient, ensuring patient anonymity. All data will be stored for 15 years according to Dutch law.
SQoL and HRQoL
SQoL was measured by the “sexual intercourse” dimension scores (SQoL score) of the EHP-30 modular questionnaire. This dimension encompasses 5 items and assesses the pain experience during or after intercourse, worries about having intercourse because of the pain, avoidance of intercourse because of the pain, feelings of guilt about not wanting to have intercourse, and feelings of frustration due to lack of enjoyment in intercourse. The items concern the effect endometriosis has had on sexual relationships of the participant during the 4 weeks prior to filling in these items. Items are scored on a 5-point Likert scale (0 = “never,” 1 = “rarely,” 2 = “sometimes,” 3 = “often,” 4 = “always”). For the “sexual intercourse” dimension participants have an additional option to qualify an item as “not relevant.” The dimension was calculated on a scale from 0 (indicating the best health status) to 100 (indicating the worst health status). This was done by summing up the scores for each item in the dimension and subsequently dividing this score by the maximum score possible (∑/20×100). In case 1 or more of the items were qualified as “not relevant,” the scale was calculated by omitting those items. No scale could be calculated for the participants who scored all items in the dimension “sexual intercourse” as “not relevant.”23
HRQoL was measured by the score of all EHP-30 core questionnaire dimensions (pain, control and powerlessness, social support, emotional well-being, self-image). Calculations for the HRQoL score were similar to the calculations for the SQoL score.
Statistical Analysis
As assumptions for parametric tests were violated, non-parametric tests were used to assess differences between groups in nominal and categorical characteristics and associations for continuous characteristics, with the SQoL score as a dependent variable.
Differences between 2 independent groups of dichotomous characteristics were tested with the Mann-Whitney U Test. For categorical characteristics with 3 or more independent groups, differences between groups were assessed using the Kruskal-Wallis Test. In case post-hoc analyses were carried out, they were performed using the Mann-Whitney U Test for categorical characteristics with a significant difference between groups. Bonferroni's correction was applied in post-hoc analyses. Relationships between continuous characteristics and the outcome measure were assessed using the Spearman Rank Order Correlation.
Multiple linear regression analysis was used to test if the characteristics with a P value < .250 significantly predicted SQoL scores. For characteristics that were described dichotomously as well as continuously (ie, dyspareunia [yes/no] and dyspareunia severity [numerical rating scale 1–10]), the dichotomous variant was used in the models. Categorical characteristics were not taken into account in this analysis. Multiple linear regression analyses that were carried out were forced entry, stepwise forward, and stepwise backward methods.
Significance level was set at α = 0.05 for all characteristics. Statistical analysis of the data was performed using IBM SPSS Statistics software version 23.0 (IBM Corporation Armonk, NY). Missing values were excluded from all data analyses.
Results
Literature Search: Characteristics (Potentially) Associated with SQoL
The literature search yielded numerous characteristics that might have an influence on SQoL in women with endometriosis (see Appendix, Table A1). Based on this literature search and with the consensus of researchers based on clinical expertise, characteristics potentially associated with SQoL were selected from the T0 survey. These were classified into sociodemographic characteristics, diagnostic characteristics, gynecological and obstetrical characteristics, endometriosis-associated symptoms, treatment characteristics, and overall HRQoL. Altogether, 29 characteristics were selected from the T0 survey (Table 1).
Table 1.
Characteristics of participants (n = 192)
| Characteristic | Mean ± SD or count (%) |
|---|---|
| Sociodemographic | |
| Age (years) | 35.7 ± 7.3 |
| Current marital status (n = 191) | |
| Single | 21 (11.0) |
| Married or registered partnership | 110 (57.6) |
| Committed relationship (cohabiting/LAT) | 57 (29.8) |
| Divorced | 3 (1.6) |
| Highest level of education (n = 192) | |
| Primary education | 1 (0.5) |
| Secondary education | 32 (16.7) |
| Secondary vocational education | 74 (38.5) |
| Higher education | 85 (44.3) |
| Currently working (n = 191) | |
| Yes | 145 (75.9) |
| No | 46 (24.1) |
| Not employed | 7 (15.2) |
| Unable to work due to health complaints | 28 (60.9) |
| Stay at home spouse or partner | 11 (23.9) |
| Diagnostic | |
| Age at first symptoms (years) (n = 191) | 24.3 ± 9.0 |
| Age at diagnosis (years) (n = 191) | 30.9 ± 7.5 |
| Delay in diagnosis (years) (n = 192) | 6.7 ± 7.6 |
| Period since diagnosis (years) (n = 192) | 4.8 ± 5.2 |
| Center of recruitment (n = 192) | |
| Hospital A (academic) | 68 (35.4) |
| Hospital B | 45 (23.4) |
| Hospital C | 37 (19.3) |
| Hospital D (academic) | 6 (3.1) |
| Hospital E | 5 (2.6) |
| Hospital F | 31 (16.1) |
| Hospital G | 0 |
| Gynecological and obstetric | |
| Age at menarche (years) (n = 191) | 12.8 ± 1.4 |
| Menstrual cycle (n = 192) | |
| Yes | 156 (81.3) |
| No | 36 (18.8) |
| Duration of menses in women with cycle (days) (n = 148) | 6.4 ± 3.2 |
| History of pregnancy (n = 192) | |
| Yes | 111 (57.8) |
| No | 81 (42.2) |
| Parity (n = 192) | |
| Parous | 91 (47.4) |
| Nulliparous | 101 (52.6) |
| History of fertility treatment (n = 192) | |
| Yes | 75 (39.1) |
| No | 117 (60.9) |
| Pregnancy wish (n = 191) | |
| Yes | 109 (57.1) |
| No | 82 (42.9) |
| Intercourse in last 3 months (n = 192) | |
| Yes | 166 (86.5) |
| No | 26 (13.5) |
| Endometriosis-associated symptoms | |
| Dysmenorrhea (women with menstrual cycle, n = 156) | |
| Yes | 154 (98.7) |
| No | 2 (1.3) |
| Severity | 7.5 ± 2.0 |
| Frequency (days/cycle) | 5.6 ± 4.9 |
| Abdominal pain between menstrual periods (n = 156) | |
| Yes | 138 (88.5) |
| No | 18 (11.5) |
| Severity | 4.7 ± 2.3 |
| Frequency (days/cycle) | 10.0 ± 8.7 |
| Abdominal pain (women without menstrual cycle, n = 36) | |
| Yes | 31 (86.1) |
| No | 5 (13.9) |
| Severity | 5.0 ± 2.8 |
| Frequency (days/month) | 14.4 ± 10.8 |
| Dyspareunia (intercourse in last 3 months, n = 166) | |
| Yes | 119 (71.7) |
| No | 47 (28.3) |
| Severity | 5.3 ± 1.9 |
| Frequency (n = 119) | |
| Rarely | 3 (2.5) |
| Sometimes | 27 (22.7) |
| Regularly | 47 (39.5) |
| Often | 20 (16.8) |
| Always | 22 (18.5) |
| Dyschezia (n = 192) | |
| Yes | 156 (81.3) |
| No | 36 (18.8) |
| Severity | 5.2 ± 2.3 |
| Frequency (n = 156) | |
| Rarely | 5 (3.2) |
| Sometimes | 34 (21.8) |
| Regularly | 46 (29.5) |
| Often | 24 (15.4) |
| Always | 21 (13.5) |
| Cyclical | 26 (16.7) |
| Dysuria (in total population, n = 192) | |
| Yes | 76 (39.6) |
| No | 116 (60.4) |
| Severity | 4.6 ± 2.4 |
| Frequency (n = 76) | |
| Rarely | 9 (11.8) |
| Sometimes | 26 (34.2) |
| Regularly | 28 (36.8) |
| Often | 11 (14.5) |
| Always | 2 (2.6) |
| Treatment | |
| First ever received treatment (n = 192) | |
| No treatment received yet | 11 (5.7) |
| Hormonal therapy | 78 (40.6) |
| Surgical therapy | 88 (45.8) |
| Hormonal and surgical therapy | 15 (7.8) |
| Currently using hormonal therapy (n = 191) | |
| Yes | 129 (67.5) |
| Progestogens only or in combination with estrogens | 84 (65.1) |
| GnRH analogues | 45 (34.9) |
| No | 62 (32.5) |
| Endometriosis surgery in medical history (n = 192) | |
| Yes | 127 (66.1) |
| No | 65 (33.9) |
| Other surgery in medical history (n = 191) | |
| Yes | 131 (68.6) |
| No | 60 (31.4) |
| Pain medication use (n = 191) | |
| Yes | 155 (81.2) |
| PCM | 120 (77.4) |
| NSAID | 107 (69.9) |
| Opiod | 21 (13.7) |
| No | 36 (18.8) |
| EHP-30 | |
| HRQoL score∗ (n = 185) | 41.8 ± 22.8 |
| 45.6 [37.1] | |
| SQoL score∗ (n = 192) | 47.5 ± 29.6 |
| 50.0 [48.8] | |
EHP-30 = Endometriosis Health Profile-30; GnRH = gonadotropin releasing hormone; HRQoL = health-related quality of life; LAT = living apart together; NSAID = non-steroidal anti-inflammatory drugs; PCM = paracetamol; SQoL = sexual quality of life.
Characteristics are depicted as count with percentage (%) or mean with SD.
Population Selection
Between July 2013 and July 2018, 224 patients provided written informed consent and 223 women were included in the “Quality of life in women with endometriosis: a longitudinal observational study.” Of these 223 eligible women, 14 were excluded for the current study. These women were excluded on the grounds that the primary outcome in the questionnaire was not completed appropriately. Furthermore, 17 women were excluded as they scored the total EHP-30 “sexual intercourse” dimension as “not relevant.” The remaining 192 women were included in the SQoL study. Selection of the study population is illustrated in Figure 1.
Figure 1.
Selection of study population. EHP-30 = Endometriosis Health Profile-30.
Participants
Characteristics of the participants are presented in Table 1. The mean age of the participants in this study was 36 years (with a range of 19–55 years). Approximately 75% of the participants were employed at the time of filling in the survey. The majority of the participants (86.5%) reported having had intercourse in the 3 months prior to filling in the survey. Of the endometriosis-associated symptoms, dysmenorrhea, dyspareunia, and dyschezia were reported by the majority of participants (98.7%, 71.7%, and 81.3%, respectively), while dysuria was reported by only 39.6%. Abdominal pain experienced between menstrual periods and abdominal pain in general in participants without a menstrual cycle were also reported frequently. The mean HRQoL score was 41.8 (with a range of 0–86.7). The mean SQoL score for the total study population (n = 192) was 47.5 (with a range of 0–100).
Comparison of Groups
Results of the univariate analyses for dichotomous and categorical characteristics are displayed in Table 2. Participants suffering from dyspareunia, dysuria, or dyschezia had significantly (P < .05) higher SQoL scores than participants without these endometriosis-associated symptoms.
Table 2.
Differences in SQoL score† between groups for dichotomous and categorical characteristics
| Characteristic | Count | SQoL score |
P value |
|---|---|---|---|
| Median [IQR] | |||
| Sociodemographic | |||
| Current marital status | |||
| Single | 21 | 50.0 [60.0] | .409 |
| Married or registered partnership | 110 | 45.0 [50.0] | |
| Committed relationship (cohabiting/LAT) | 57 | 60.0 [47.5] | |
| Divorced | 3 | 50.0 [N/A] | |
| Highest level of education | |||
| Primary education | 1 | [N/A] | .142 |
| Secondary education | 32 | 55.6 [42.5] | |
| Secondary vocational education | 74 | 50.0 [40.0] | |
| Higher education | 85 | 45.0 [60.0] | |
| Currently working | |||
| Yes | 145 | 45.0 [50.0] | .004∗ |
| No | 46 | 61.3 [36.1] | |
| Not employed | 7 | 60.0 [53.3] | .421 |
| Unable to work due to health complaints | 28 | 63.8 [34.6] | |
| Stay at home spouse or partner | 11 | 60.0 [70.0] | |
| Gynecological and obstetric | |||
| Menstrual cycle | |||
| Yes | 156 | 50.0 [50.0] | .589 |
| No | 36 | 47.5 [53.8] | |
| History of pregnancy | |||
| Yes | 111 | 50.0 [55.0] | .893 |
| No | 81 | 50.0 [55.0] | |
| Parity | |||
| Parous | 91 | 50.0 [45.0] | .424 |
| Nulliparous | 101 | 50.0 [55.0] | |
| History of fertility treatment | |||
| Yes | 75 | 41.7 [53.3] | .152 |
| No | 117 | 55.0 [47.5] | |
| Pregnancy wish | |||
| Yes | 109 | 50.0 [56.7] | .346 |
| No | 82 | 50.0 [41.3] | |
| Intercourse in last 3 months | |||
| Yes | 166 | 50.0 [50.0] | .149 |
| No | 26 | 59.4 [56.8] | |
| Endometriosis-associated symptoms | |||
| Dysmenorrhea | |||
| Yes | 154 | 50.0 [50.0] | .819 |
| No | 2 | 52.5 [N/A] | |
| Abdominal pain between menstrual periods | |||
| Yes | 138 | 50.0 [45.0] | .102 |
| No | 18 | 27.5 [66.6] | |
| Abdominal pain in last 3 months | |||
| Yes | 31 | 45.0 [56.3] | .801 |
| No | 5 | 60.0 [47.5] | |
| Dyspareunia | |||
| Yes | 119 | 60.0 [35.0] | <.001∗ |
| No | 47 | 10.0 [30.0] | |
| Dyschezia | |||
| Yes | 156 | 50.0 [45.0] | .022∗ |
| No | 36 | 27.5 [52.5] | |
| Dysuria | |||
| Yes | 76 | 55.6 [41.3] | .036∗ |
| No | 116 | 45.0 [50.0] | |
| Treatment | |||
| First ever received treatment | |||
| No treatment received yet | 11 | 45.0 [60.0] | .849 |
| Hormonal therapy | 78 | 50.0 [50.0] | |
| Surgical therapy | 88 | 50.0 [52.5] | |
| Hormonal and surgical therapy | 15 | 45.0 [20.0] | |
| Currently using hormonal therapy | |||
| Yes | 129 | 50.0 [50.0] | .467 |
| No | 62 | 52.5 [56.3] | |
| Hormonal therapy use specified | |||
| Progestogens with or without estrogens | 84 | 50.0 [50.0] | .538 |
| GnRH analogue | 45 | 50.0 [47.5] | |
| Endometriosis surgery in medical history | |||
| Yes | 127 | 50.0 [50.0] | .375 |
| No | 65 | 55.0 [50.0] | |
| Other surgery in medical history | |||
| Yes | 131 | 50.0 [55.0] | .506 |
| No | 60 | 52.5 [43.8] | |
| Pain medication use | |||
| Yes | 155 | 50.0 [50.0] | .012∗ |
| No | 36 | 32.5 [56.6] | |
GnRH = gonadotropin releasing hormone; IQR = interquartile range; LAT = living apart together; N/A = not applicable; SQoL = sexual quality of life.
P values were calculated using the Mann-Whitney U Test and the Kruskal-Wallis Test (α < 0.05).
Significant P values.
SQoL score = Endometriosis Health Profile-30: sexual intercourse dimension score. SQoL scores are depicted as median with IQR.
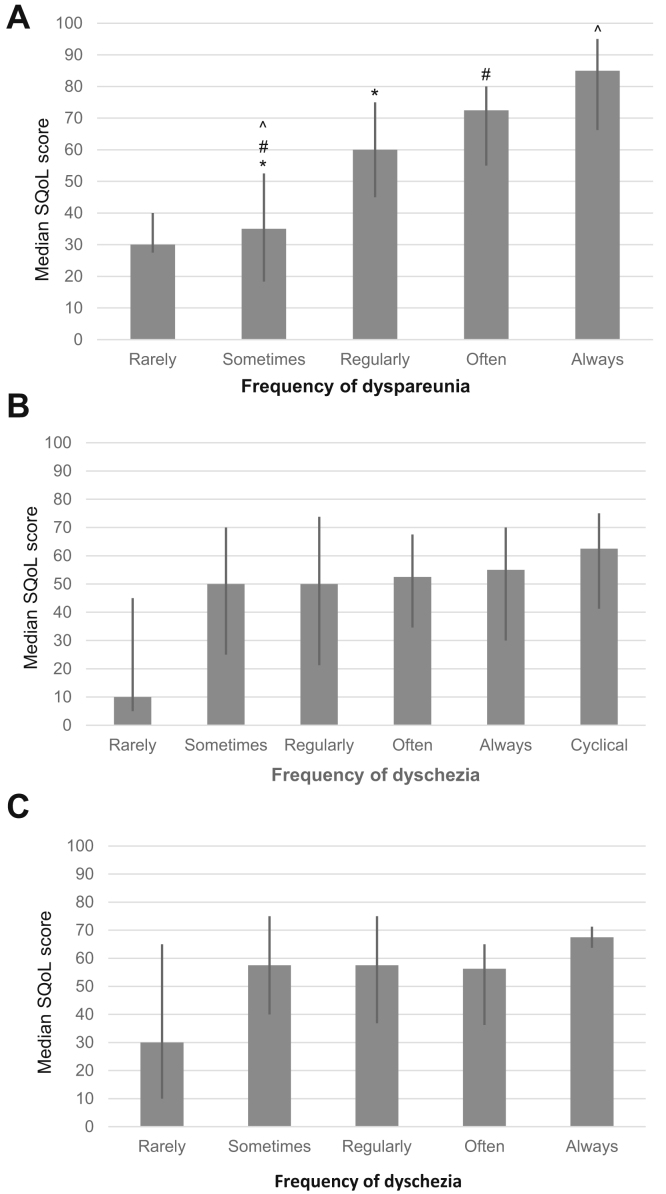
A trend can be seen when plotting SQoL scores for the frequency in which dyspareunia, dyschezia, and dysuria were reported as shown in Figure 2. Here, it seems that higher frequencies in which symptoms are experienced correlate with higher SQoL scores. Although analyses of the frequency in which dyschezia and dysuria were experienced did not show a significant difference in SQoL scores, there was a significant difference in the frequency in which dyspareunia was experienced. Post-hoc analyses showed a significant difference in scores between women who “rarely” experienced dyspareunia and women who “regularly,” “often,” or “always” experienced dyspareunia.
Figure 2.
Sexual quality of life (SQoL) scores, depicted as median with interquartile range, plotted for the experienced frequency of dyspareunia (A), dyschezia (B), and dysuria (C). Significant differences between groups are denoted with (∗), (#), and (ˆ).
Furthermore, participants who were using pain medication had significantly higher SQoL scores.
Participants who were unemployed had significantly higher SQoL scores compared to employed participants. Post-hoc analysis of the three subgroups showed that unemployed participants and stay at home spouses or partners had higher SQoL scores compared to employed participants, though these results were not statistically significant (P = .05 and P = .893, respectively). However, participants who were unable to work due to health complaints had significantly higher SQoL scores (P = .004) compared to employed participants, indicating worse SQoL.
Comparing participants with children and participants with unwanted childlessness did not result in significant differences in SQoL scores (P = .061; respective median SQoL score [IQR] of 50.0 [56.25] and 25.0 [40.0]).
Results of univariate analyses for continuous characteristics potentially associated with SQoL are shown in Table 3. The duration of menses in women with a menstrual cycle, abdominal pain severity, severity of dysmenorrhea, and the number of days on which abdominal pain between menstrual periods was reported showed a significant and positive association with SQoL score, with an increase in SQoL score as the duration, severity, or frequency increased. A positive correlation with SQoL scores was also found for the severity and frequency of abdominal pain in participants without a menstrual cycle. Furthermore, a positive association for dyschezia and HRQoL score with SQoL score was seen for women with and without a menstrual cycle. Severity of dyspareunia showed the largest association with SQoL scores, with an increase in SQoL score as severity of dyspareunia increased.
Table 3.
Correlation between continuous characteristics and SQoL scores†
| Characteristic | Count | Spearman ρ | P value |
|---|---|---|---|
| Sociodemographic | |||
| Age (years) | 191 | −0.016 | .828 |
| Diagnostic | |||
| Age at first symptoms (years) | 191 | 0.016 | .825 |
| Age at diagnosis (years) | 191 | −0.019 | .795 |
| Delay in diagnosis (years) | 192 | 0.022 | .767 |
| Period since diagnosis (years) | 192 | −0.94 | .194 |
| Gynecological and obstetric | |||
| Age at menarche (years) | 191 | 0.079 | .298 |
| Duration of menses in women with cycle (days) | 148 | 0.190 | .020∗ |
| Endometriosis-associated symptoms | |||
| Dysmenorrhea severity (1–10) | 157 | 0.255 | .001∗ |
| Abdominal pain severity between menstrual periods (1–10) | 157 | 0.289 | <.001∗ |
| Abdominal pain frequency between menstrual periods (days) | 156 | 0.269 | .001∗ |
| Abdominal pain severity in participants without a cycle (1–10) | 36 | 0.370 | .026∗ |
| Abdominal pain frequency in participants without a cycle (days) | 34 | 0.403 | .018∗ |
| Dyspareunia severity (1–10) | 118 | 0.571 | <.001∗ |
| Dyschezia severity (1–10) | 156 | 0.195 | .015∗ |
| Dysuria severity (1–10) | 71 | 0.122 | .309 |
| EHP-30 | |||
| HRQoL score | 185 | 0.428 | <.001∗ |
EHP-30 = Endometriosis Health Profile-30; HRQoL = health-related quality of life; SQoL = sexual quality of life.
Significant P values.
SQoL scores = Endometriosis Health Profile-30: sexual intercourse dimension scores. P values were calculated using the Spearman Rank Order Correlation (α < 0.05).
Multiple Linear Regression Analysis
All characteristics in the univariate analysis associated with the SQoL score with a P value below .250 were considered for the multiple linear regression analysis (n = 122). As shown in Table 4, 3 different methods, namely forced entry, stepwise forward, and stepwise backward were performed.
Table 4.
Multiple linear regression using forced entry, stepwise forward, and stepwise backward method (n = 122)
| Forced entry |
Stepwise forward |
Stepwise backward |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| B | Se B | P value | B | Se B | P value | B | Se B | P value | |
| Constant | 5.885 | 10.815 | −3.171 | 8.022 | −1.929 | 8.171 | |||
| Period since diagnosis† | −0.258 | 0.426 | .545 | ||||||
| Duration of menses‡ | −0.489 | 0.567 | .390 | ||||||
| Dysmenorrhea severity§ | 2.877 | 0.966 | .004∗ | 2.254 | 0.932 | .017∗ | 2.893 | 0.952 | .003∗ |
| Dyspareunia‖ | 43.111 | 4.385 | <.001∗ | 38.937 | 4.006 | <.001∗ | 41.895 | 4.109 | <.001∗ |
| History of fertility treatment‖ | 0.375 | 4.094 | .927 | ||||||
| Currently working‖ | −11.014 | 4.555 | .017∗ | −9.916 | 4.261 | .022∗ | −10.343 | 4.202 | .015∗ |
| Dyschezia‖ | −3.548 | 5.005 | .480 | ||||||
| Dysuria‖ | −8.081 | 4.272 | .061 | −8.660 | 4.023 | .033∗ | |||
| Pain medication use‖ | −9.887 | 5.463 | .073 | −8.808 | 5.248 | .096 | |||
| Abdominal pain outside menstruation‖ | −0.882 | 5.698 | .877 | ||||||
| HRQoL score¶ | 0.384 | 0.100 | <.001∗ | 0.302 | 0.088 | .001∗ | 0.376 | 0.092 | <.001∗ |
| Adjusted R2 = 0.558 (P < .001∗) | Adjusted R2 = 0.554 (P < .001∗) | Adjusted R2 = 0.570 (P < .001∗) | |||||||
B = unstandardized beta; EHP-30 = Endometriosis Health Profile-30; HRQoL = health-related quality of life; NRS = numerical rating scale; Se B = standard error for the unstandardized beta.
Significant P values.
Continuous characteristic, in years.
Continuous characteristic, in days.
Continuous characteristic, NRS (1–10).
Dichotomous characteristic, yes or no.
Continuous characteristic, EHP-30 (0–100).
All methods indicated that dyspareunia, a worse HRQoL score, increasing dysmenorrhea severity, and unemployed work status were significantly associated with higher SQoL scores, indicating a worse SQoL. The models accounted for 55.8%, 55.4%, and 57.0% of the variance in SQoL scores, respectively. Dyspareunia made the strongest unique contribution to explain the SQoL score in all the regression models (β = 0.660, β = 0.596, and β = 0.641, respectively).
Only the stepwise backward model identified dysuria (B = −8.660, P = .033) as a significantly associated characteristic with SQoL score. In this model, the presence of dysuria was associated with lower SQoL scores.
Discussion
The aim of the current study was to explore which patient- and disease-specific characteristics are independently associated with SQoL, as measured by the EHP-30 “sexual intercourse” dimension score, in a population of Dutch women with endometriosis.
Mean HRQoL and SQoL scores of our study population indicated an overall moderate health status among these Dutch women with endometriosis.
Univariate analysis showed that participants who were not employed, suffering from dyspareunia, dyschezia, dysuria, or were using pain medication had significantly higher SQoL scores than participants without the above-mentioned characteristics. Concomitantly, prolonged duration of menses, more severe dysmenorrhea, more severe abdominal pain between menstrual periods, more severe abdominal pain for participants without a cycle, more severe dyspareunia and dyschezia, and worse overall HRQoL are associated with higher SQoL scores. In conclusion, these characteristics are associated with significant worse SQoL.
Based on the characteristics with significant associations in univariate analyses, multiple linear regression analyses were performed. These analyses showed that the presence of dyspareunia, unemployed work status, more severe dysmenorrhea, and worse overall HRQoL were significantly and independently associated with worse SQoL after controlling for other relevant factors. The presence of dyspareunia seemed to be the best and strongest predictor of worse SQoL in our analyses.
It is noteworthy that the characteristic of having had intercourse in the 3 months prior to filling in the survey was considered as well but was eliminated in the analyses due to the fact that it was constant to the characteristic of experiencing dyspareunia. Translating this into clinical practice, it is a logical finding as dyspareunia will not be experienced by patients that are not sexually active. Nevertheless, dyspareunia does remain an important reason for patients to refrain from having intercourse, so this finding should be taken into consideration in clinical practice.27
Strengths and Limitations
An important strength of this study is the use of a validated method to measure SQoL in women with endometriosis specifically. To our knowledge, this is one of the few studies to use the “sexual intercourse” dimension of the EHP-30 modular questionnaire as a measure for SQoL in this specific population. Furthermore, the size of the cohort in this study minimizes the statistical margin of error. An additional strength is that data analyzed in this study have been collected prospectively, which limits recall bias to some extent. Thereby, all participants were included on the common ground of being new endometriosis patients in the referral centers where they presented themselves.
A limitation of this study is its cross-sectional nature which does not allow causal relations to be distinguished. Furthermore, a limitation that is imposed by the fact that an existing database was used is the restricted array of potential patient- and disease-specific characteristics influencing SQoL, as the original study aimed to look at HRQoL generally and not SQoL specifically. Prior research suggests that patient-specific characteristics such as depression and depressive symptoms,3,15,28 anxiety,28 and heterosexual orientation21 are significantly associated with worse SQoL or sexual functioning. Thereby, disease-specific characteristics such as stage of endometriosis and referral status were explored to see if they were potential characteristics of influence in previous studies.3,21 These characteristics could not be addressed in the current study, as these items were not part of the T0 survey.
Interpretation
This study confirms previous findings that dyspareunia is independently associated with worse SQoL and contributes to a greater understanding of the importance of this clinical finding in women with endometriosis.21 Furthermore, more severe dysmenorrhea, unemployment, and worse overall HRQoL were associated with worse SQoL in women with endometriosis.
Several studies investigated the impact of dysmenorrhea in women with endometriosis on overall QoL and evidence of these studies suggests that dysmenorrhea mainly has an impact on physical QoL.1,29,30 Nevertheless, the significant association between more severe dysmenorrhea and worse SQoL as indicated by our findings has not been described before. As Soliman et al31 demonstrated previously, EHP-30 scores on all core questionnaire domains were significantly higher for self-reported moderate and severe disease vs mild disease in women with endometriosis. Furthermore, their cross-sectional study indicated that with an increase of symptom severity the impact on HRQoL increases. In combination with our results indicating a positive association between SQoL and HRQoL, a hypothetical explanation might be that more severe dysmenorrhea is more invalidating on all aspects of life, including SQoL.
Our study found an association between unemployment and worse SQoL. This finding requires further research as we are unsure of what the underlying theoretical framework is and what the clinical implications could be. Menstruation-related symptoms in general and endometriosis in particular have a high impact on work-related domains such as absenteeism, presenteeism, and loss in efficiency and productivity of work.32,33 We can theorize that women with endometriosis who are unable to work due to health complaints encounter more severe impairment from their disease than women who are still able to work. This impairment might extend to their intimate relationships and thus be associated with worse SQoL, as our analysis pointed out.
Also, we found that worse HRQoL was associated with worse SQoL. This supports evidence from previous research that indicated that there seems to be a correlation between QoL and sexual functioning in women with endometriosis.15,34
Lastly, we determined whether there were differences in SQoL in women with children vs women with unwanted childlessness, as prior research indicated that childlessness and infertility might have a major impact on sexuality, general psychological well-being, and life satisfaction.35, 36, 37 Our analysis did not render a significant difference between the 2 groups; however, the sample size of women with unwanted childlessness was small (n = 7) as we did not have specific data on infertility itself.
Clinical Applicability and Implications
Our results indicate that in a cohort of Dutch women with endometriosis, dyspareunia, unemployed work status, worse HRQoL, and severity of dysmenorrhea are significantly and independently associated with SQoL, as measured with the “sexual intercourse” dimension of the EHP-30 modular questionnaire. Our evidence suggests that reducing or even eliminating dyspareunia in these women might have a major positive effect on the experienced SQoL; however, based on our cross-sectional data we cannot draw any conclusions on the effect of medical or surgical treatment on SQoL. Surgical, and to a lesser extent pharmacological, treatment of endometriosis with a focus on dyspareunia have been described in the literature.17,38, 39, 40, 41, 42, 43, 44 Conclusions in these studies suggest that surgical treatment of deep infiltrating endometriosis in particular is effective in reducing and even eliminating dyspareunia. Symptom-focused treatment to reduce endometriosis-associated symptoms was previously suggested by De Graaff et al.15 Given that dyspareunia is a strong independent predictor for SQoL in our study, this symptom should be addressed primarily when focusing on SQoL. This is also supported by earlier research from Yong et al45 that describes dyspareunia as particularly harmful because it is usually experienced with every attempt of sexual intercourse, whereas dysmenorrhea typically only is present during a few days of the menstrual cycle. Thereby, research indicates a link between decreased pain intensity and increased QoL.46,47
However, a medical symptom-focused therapy to reduce pain symptoms might not be sufficient to ameliorate SQoL in women with endometriosis. Barbara et al39 reviewed the existing literature on the effect of surgical and pharmacological treatment on female sexual dysfunction and found that even though improvement can be achieved, this treatment might not be a definitive solution. More importantly, in women with endometriosis and a current desire to have children, pharmacological (ie, hormonal) treatment for dyspareunia is not an option. Barbara et al39 proposed that improving global sexual functioning “… should be considered as a major clinical goal of endometriosis treatment,” and not merely reduction of pain. Buggio et al48 highlighted the importance of an integration of psychological-sexological interventions in clinical treatment of endometriosis.
In clinical care, anamnestic information about dyspareunia, employment status, HRQoL, and dysmenorrhea severity might provide hints to the clinician about an association with deteriorated SQoL in these women and in this way aid in addressing the subject of sexuality and SQoL. Vice versa, the 5-item “sexual intercourse” dimension allows for a quick evaluation of SQoL in women with endometriosis and therefore can be implemented easily in clinical care as an aid to address this topic during consultation. Additionally, De Graaff et al demonstrated that depressive symptoms, as measured with the Hospital Anxiety and Depression Scale, were also associated with impaired sexual functioning in women with endometriosis.15 Melis et al49 substantiated this evidence and found that having fewer depressive symptoms was associated with an improvement in sexual functioning and vice versa. Thereby, Yong et al50 indicated the importance of an interdisciplinary approach to dyspareunia in women with endometriosis given the multifactorial origins, including comorbidities such as depression and anxiety. Implementation of a self-administered questionnaire in clinical care containing the “sexual intercourse” domain of the EHP-30 and the Hospital Anxiety and Depression Scale might therefore be a valuable construct to evaluate and address SQoL in women with endometriosis specifically. A suggestion would be to implement this using the Experience Sampling Method.51 The Maastricht University Medical Center+ developed a momentary assessment tool to provide real-time information on, amongst others, HRQoL and SQoL in women with endometriosis in the context of daily life.
Suggestions for Future Research
A suggestion for future research is to conduct a prospective longitudinal cohort study to analyze potential influential patient- and disease-specific characteristics in women with endometriosis on SQoL for causal interpretations to be made.
Other characteristics we would propose to take into consideration in future research are sexual development factors (eg, attitudes toward sexuality during childhood and adulthood, [early life] negative sexual experiences and sexual abuse in childhood and adulthood), communication about sex(uality), and sexual orientation and effect of and on partners, as these characteristics might influence SQoL.12,15,21,52,53 Moreover, the aforementioned characteristics such as depressive symptoms, anxiety, stage of endometriosis, and referral status should be considered.
We would also like to suggest conducting additional research on SQoL in women with endometriosis with the use of the “sexual intercourse” domain of the EHP-30 specifically, as only few studies are known to use this as a measure for SQoL. A promising line of research would be to validate the use of the EHP-30 in women with endometriosis compared to healthy controls with the aim of developing a clinical cut-off score. To the best of our knowledge, a clinical cut-off score to distinguish “normal cases” from “clinical range cases” has not been described for the EHP-30. Establishing a clinical cut-off score for SQoL facilitates the use of self-administered questionnaires as a tool to determine patients in whom sexuality definitely should be addressed. Establishing the clinical range is thereby a necessary construct to perform future research regarding the effects of psychosexological interventions in these women.
Furthermore, future research ascertaining prospective longitudinal designs could focus on the development of a prediction model to predict SQoL scores in women with endometriosis. In clinical care, this might aid in making an estimation for which individual woman sexuality and SQoL should be a topic of priority during consultation.
Conclusion
This study provides evidence that the presence of dyspareunia, unemployed work status, worse HRQoL, and more severe dysmenorrhea are significantly and independently associated with worse SQoL in women with endometriosis. Our recommendation for clinicians is to be aware of these characteristics in endometriosis patients in relation to possible decreased SQoL. Knowledge of the characteristics associated with worse SQoL can aid in addressing this subject more easily during consultation. Vice versa, an additional recommendation would be to implement the use of the 5-item “sexual intercourse” domain of the EHP-30 in common clinical practice to decide in which patients the topic of sexuality should definitely be discussed. A multidisciplinary approach of endometriosis treatment involving psychosexological intervention might be especially helpful in women with dyspareunia and impaired SQoL, although the effectiveness of this treatment requires further research.
Statement of authorship
Mikal van Poll: Conceptualization, Methodology, Formal analysis, Data curation, Writing – original draft. Esther van Barneveld: Writing – review & editing, Supervision. Luca Aerts: Investigation, Data curation. Jacques W.M. Maas: Investigation, Writing – review & editing. Arianne C. Lim: Investigation, Writing – review & editing. Bianca T.A. de Greef: Methodology, Formal analysis, Writing – review & editing. Marlies Y. Bongers: Investigation, Writing – review & editing. Nehalennia van Hanegem: Investigation, Writing – review & editing, Supervision.
Footnotes
Conflict of Interest: The authors report no conflicts of interest.
Funding: None.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.esxm.2020.06.004.
Supplementary Data
References
- 1.De Graaff A.A., D’Hooghe T.M., Dunselman G.A. The significant effect of endometriosis on physical, mental and social wellbeing: results from an international cross-sectional survey. Hum Reprod. 2013;28:2677–2685. doi: 10.1093/humrep/det284. [DOI] [PubMed] [Google Scholar]
- 2.Dunselman G.A., Vermeulen N., Becker C. ESHRE guideline: management of women with endometriosis. Hum Reprod. 2014;29:400–412. doi: 10.1093/humrep/det457. [DOI] [PubMed] [Google Scholar]
- 3.Barbara G., Facchin F., Buggio L. What is known and unknown about the association between endometriosis and sexual functioning: a systematic review of the literature. Reprod Sci. 2017;24:1566–1576. doi: 10.1177/1933719117707054. [DOI] [PubMed] [Google Scholar]
- 4.Klein S., D’Hooghe T.M., Meuleman C. What is the societal burden of endometriosis-associated symptoms? A prospective Belgian study. Reprod Biomed Online. 2014;28:116–124. doi: 10.1016/j.rbmo.2013.09.020. [DOI] [PubMed] [Google Scholar]
- 5.Simoens S., Dunselman G.A., Dirksen C. The burden of endometriosis: costs and quality of life of women with endometriosis and treated in referral centres. Hum Reprod. 2012;27:1292–1299. doi: 10.1093/humrep/des073. [DOI] [PubMed] [Google Scholar]
- 6.Vercellini P., Viganò P., Somigliana E. Endometriosis: pathogenesis and treatment. Nat Rev Endocrinol. 2014;10:261–275. doi: 10.1038/nrendo.2013.255. [DOI] [PubMed] [Google Scholar]
- 7.Culley L., Law C., Hudsen N. The social and psychological impact of endometriosis on women’s lives: a critical narrative review. Hum Reprod Update. 2013;19:625–639. doi: 10.1093/humupd/dmt027. [DOI] [PubMed] [Google Scholar]
- 8.Marinho M.C.P., Magalhaes T.F., Fernandes L.F.C. Quality of life in women with endometriosis: an integrative review. J Womens Health (Larchmt) 2018;27:399–408. doi: 10.1089/jwh.2017.6397. [DOI] [PubMed] [Google Scholar]
- 9.Gallagher J.S., DiVasta A.D., Vitonis A.F. The impact of endometriosis on quality of life in adolescents. J Adolesc Health. 2018;63:766–772. doi: 10.1016/j.jadohealth.2018.06.027. [DOI] [PubMed] [Google Scholar]
- 10.Fritzer N., Haas D., Oppelt P. More than just bad sex: sexual dysfunction and distress in patients with endometriosis. Eur J Obstet Gynecol Reprod Biol. 2013;169:392–396. doi: 10.1016/j.ejogrb.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 11.Di Donato N., Montanari G., Benfenati A. Do women with endometriosis have to worry about sex? Eur J Obstet Gynecol Reprod Biol. 2014;179:69–74. doi: 10.1016/j.ejogrb.2014.05.022. [DOI] [PubMed] [Google Scholar]
- 12.Pluchino N., Wenger J.M., Petignat P. Sexual function in endometriosis patients and their partners: effect of the disease and consequences of treatment. Hum Reprod Update. 2016;22:762–774. doi: 10.1093/humupd/dmw031. [DOI] [PubMed] [Google Scholar]
- 13.Yela D.A., Quagliato I.P., Benetti-Pinto C.L. Quality of life in women with deep endometriosis: a cross-sectional study. Rev Bras Ginecol Obstet. 2020;42:90–95. doi: 10.1055/s-0040-1708091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vercellini P., Meana M., Hummelshoj L. Priorities for endometriosis research: a proposed focus on deep dyspareunia. Reprod Sci. 2011;18:114–118. doi: 10.1177/1933719110382921. [DOI] [PubMed] [Google Scholar]
- 15.De Graaff A.A., Van Lankveld J., Smits L.J. Dyspareunia and depressive symptoms are associated with impaired sexual functioning in women with endometriosis, whereas sexual functioning in their male partners is not affected. Hum Reprod. 2016;31:2577–2586. doi: 10.1093/humrep/dew215. [DOI] [PubMed] [Google Scholar]
- 16.Ferrero S., Esposito F., Abbamonte L.H. Quality of sex life in women with endometriosis and deep dyspareunia. Fertil Steril. 2005;83:573–579. doi: 10.1016/j.fertnstert.2004.07.973. [DOI] [PubMed] [Google Scholar]
- 17.Lukic A., Di Properzio M., De Carlo S. Quality of sex life in endometriosis patients with deep dyspareunia before and after laparoscopic treatment. Arch Gynecol Obstet. 2016;293:583–590. doi: 10.1007/s00404-015-3832-9. [DOI] [PubMed] [Google Scholar]
- 18.Bernays V., Schwartz A.K., Geraedts K. Qualitative and quantitative aspects of sex life in the context of endometriosis: a multicentre case control study. Reprod Biomed Online. 2020;40:296–304. doi: 10.1016/j.rbmo.2019.10.015. [DOI] [PubMed] [Google Scholar]
- 19.Cozzolino M., Magro-Malosso E.R., Tofani L. Evaluation of sexual function in women with deep infiltrating endometriosis. Sex Reprod Healthc. 2018;16:6–9. doi: 10.1016/j.srhc.2017.12.005. [DOI] [PubMed] [Google Scholar]
- 20.Moradi M., Parker M., Sneddon A. Impact of endometriosis on women’s lives: a qualitative study. BMC Womens Health. 2014;14:123. doi: 10.1186/1472-6874-14-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shum L.K., Bedaiwy M.A., Allaire C. Deep dyspareunia and sexual quality of life in women with endometriosis. Sex Med. 2018;6:224–233. doi: 10.1016/j.esxm.2018.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jones G., Jenkinson C., Taylor N. Measuring quality of life in women with endometriosis: tests of data quality, score reliability, response rate and scaling assumptions of the endometriosis health profile questionnaire. Hum Reprod. 2006;21:2686–2693. doi: 10.1093/humrep/del231. [DOI] [PubMed] [Google Scholar]
- 23.Jones G., Jenkinson C., Kennedy S. University of Oxford; Oxford, UK: 2001. The endometriosis health profile user manual–user manual for the EHP-30 and the EHP-5,© 2001 Nuffield Department of Obstetrics & Gynaecology & Health Services Research Unit. [Google Scholar]
- 24.Khong S.Y., Lam A., Luscombe G. Is the 30-item endometriosis health profile (EHP-30) suitable as a self-report health status instrument for clinical trials? Fertil Steril. 2010;94:1928–1932. doi: 10.1016/j.fertnstert.2010.01.047. [DOI] [PubMed] [Google Scholar]
- 25.van de Burgt T.J., Hendriks J.C., Kluivers K.B. Quality of life in endometriosis: evaluation of the Dutch-version endometriosis health profile-30 (EHP-30) Fertil Steril. 2011;95:1863–1865. doi: 10.1016/j.fertnstert.2010.11.009. [DOI] [PubMed] [Google Scholar]
- 26.van de Burgt T.J., Kluivers K.B., Hendriks J.C. Responsiveness of the Dutch endometriosis health profile-30 (EHP-30) questionnaire. Eur J Obstet Gynecol Reprod Biol. 2013;168:92–94. doi: 10.1016/j.ejogrb.2012.12.037. [DOI] [PubMed] [Google Scholar]
- 27.Denny E., Mann C.H. Endometriosis-associated dyspareunia: the impact on women's lives. J Fam Plann Reprod Health Care. 2007;33:189–193. doi: 10.1783/147118907781004831. [DOI] [PubMed] [Google Scholar]
- 28.Friedl F., Riedl D., Fessler S. Impact of endometriosis on quality of life, anxiety, and depression: an Austrian perspective. Arch Gynecol Obstet. 2015;292:1393–1399. doi: 10.1007/s00404-015-3789-8. [DOI] [PubMed] [Google Scholar]
- 29.Oehmke F., Weyand J., Hackethal A. Impact of endometriosis on quality of life: a pilot study. Gynecol Endocrinol. 2009;25:722–725. doi: 10.3109/09513590903159607. [DOI] [PubMed] [Google Scholar]
- 30.Facchin F., Barbara G., Saita E. Impact of endometriosis on quality of life and mental health: pelvic pain makes the difference. J Psychosom Obstet Gynaecol. 2015;36:135–141. doi: 10.3109/0167482X.2015.1074173. [DOI] [PubMed] [Google Scholar]
- 31.Soliman A.M., Coyne K.S., Zaiser E. The burden of endometriosis symptoms on health-related quality of life in women in the United States: a cross-sectional study. J Psychosom Obstet Gynaecol. 2017;38:238–248. doi: 10.1080/0167482X.2017.1289512. [DOI] [PubMed] [Google Scholar]
- 32.Fourquet J., Báez L., Figueroa M. Quantification of the impact of endometriosis symptoms on health-related quality of life and work productivity. Fertil Steril. 2011;96:107–112. doi: 10.1016/j.fertnstert.2011.04.095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schoep M.E., Adang E.M.M., Maas J.W.M. Productivity loss due to menstruation-related symptoms: a nationwide cross-sectional survey among 32 748 women. BMJ Open. 2019;9:e026186. doi: 10.1136/bmjopen-2018-026186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Montanari G., Di Donato N., Benfenati A. Women with deep infiltrating endometriosis: sexual satisfaction, desire, orgasm, and pelvic problem interference with sex. J Sex Med. 2013;10:1559–1566. doi: 10.1111/jsm.12133. [DOI] [PubMed] [Google Scholar]
- 35.Tanaka K., Johnson N.E. Childlessness and mental well-being in a global context. J Fam Issues. 2016;37:1027–1045. [Google Scholar]
- 36.La Rosa V.L., Barra F., Chiofalo B. An overview on the relationship between endometriosis and infertility: the impact on sexuality and psychological well-being. J Psychosom Obstet Gynaecol. 2020;41:93–97. doi: 10.1080/0167482X.2019.1659775. [DOI] [PubMed] [Google Scholar]
- 37.Matasariu R.D., Mihaila A., Iacob M. Psycho-social aspects of quality of life in women with endometriosis. Acta Endocrinol (Buchar) 2017;13:334–339. doi: 10.4183/aeb.2017.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fritzer N., Tammaa A., Salzer H. Dyspareunia and quality of sex life after surgical excision of endometriosis: a systematic review. Eur J Obstet Gynecol Reprod Biol. 2014;173:1–6. doi: 10.1016/j.ejogrb.2013.10.032. [DOI] [PubMed] [Google Scholar]
- 39.Barbara G., Facchin F., Meschia M. When love hurts. A systematic review on the effects of surgical and pharmacological treatments for endometriosis on female sexual functioning. Acta Obstet Gynecol Scand. 2016;96:668–687. doi: 10.1111/aogs.13031. [DOI] [PubMed] [Google Scholar]
- 40.Fritzer N., Hudelist G. Love is a pain? Quality of sex life after surgical resection of endometriosis: a review. Eur J Obstet Gynecol Reprod Biol. 2017;209:72–76. doi: 10.1016/j.ejogrb.2016.04.036. [DOI] [PubMed] [Google Scholar]
- 41.Franck C., Poulsen M.H., Karampas G. Questionnaire-based evaluation of sexual life after laparoscopic surgery for endometriosis: a systematic review of prospective studies. Acta Obstet Gynecol Scand. 2018;97:1091–1104. doi: 10.1111/aogs.13369. [DOI] [PubMed] [Google Scholar]
- 42.Ferrero S., Abbamonte L.H., Giordano M. Deep dyspareunia and sex life after laparoscopic excision of endometriosis. Hum Reprod. 2007;22:1142–1148. doi: 10.1093/humrep/del465. [DOI] [PubMed] [Google Scholar]
- 43.De la Hera-Lazaro C.M., Munoz-Gonzalez J.L., Perez R.O. Radical surgery for endometriosis: analysis of quality of life and surgical procedure. Clin Med Insights Womens Health. 2016;9:7–11. doi: 10.4137/CMWH.S38170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lermann J., Topal N., Renner S.P. Comparison of preoperative and postoperative sexual function in patients with deeply infiltrating endometriosis with and without bowel resection. Eur J Obstet Gynecol Reprod Biol. 2019;239:21–29. doi: 10.1016/j.ejogrb.2019.05.007. [DOI] [PubMed] [Google Scholar]
- 45.Yong P.J., Sadownik L., Brotto L.A. Concurrent deep-superficial dyspareunia: prevalence, associations, and outcomes in a multidisciplinary vulvodynia program. J Sex Med. 2015;12:219–227. doi: 10.1111/jsm.12729. [DOI] [PubMed] [Google Scholar]
- 46.Comptour A., Chauvet P., Canis M. Patient quality of life and symptoms after surgical treatment for endometriosis. J Minim Invasive Gynecol. 2019;26:717–726. doi: 10.1016/j.jmig.2018.08.005. [DOI] [PubMed] [Google Scholar]
- 47.Arcoverde F.V.L., Andres M.P., Borrelli G.M. Surgery for endometriosis improves major domains of quality of life: a systematic review and meta-analysis. J Minim Invasive Gynecol. 2019;26:266–278. doi: 10.1016/j.jmig.2018.09.774. [DOI] [PubMed] [Google Scholar]
- 48.Buggio L., Barbara G., Facchin F. Self-management and psychological-sexological interventions in patients with endometriosis: strategies, outcomes, and integration into clinical care. Int J Womens Health. 2017;9:281–293. doi: 10.2147/IJWH.S119724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Melis I., Litta P., Nappi L. Sexual function in women with deep endometriosis: correlation with quality of life, intensity of pain, depression, anxiety, and body image. Int J Sex Health. 2015;27:175–185. [Google Scholar]
- 50.Yong P.J., Williams C., Bodmer-Roy S. Prospective cohort of deep dyspareunia in an interdisciplinary setting. J Sex Med. 2018;15:1765–1775. doi: 10.1016/j.jsxm.2018.10.005. [DOI] [PubMed] [Google Scholar]
- 51.Kramer I., Simons C.J., Hartmann J.A. A therapeutic application of the experience sampling method in the treatment of depression: a randomized controlled trial. World Psychiatry. 2014;13:68–77. doi: 10.1002/wps.20090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.An overview of healthy childhood sexual development. 2013. https://www.nsvrc.org/publications/an-overview-on-healthy-childhood-sexual-development Available at:
- 53.Richtlijn Seksuele ontwikkeling. Determinanten van seksuele gezondheid. 2014. https://www.ncj.nl/richtlijnen/alle-richtlijnen/richtlijn/?richtlijn=2&rlpag=478 Available at. Accessed October 10, 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.