Abstract
Background
Ginsenoside Rh2 (GRh2) is a characterized component in red ginseng widely used in Korea and China. GRh2 exhibits a wide range of pharmacological activities, such as anti-inflammatory, antioxidant, and anticancer properties. However, its effects on Toxoplasma gondii (T. gondii) infection have not been clarified yet.
Methods
The effect of GRh2 against T. gondii was assessed under in vitro and in vivo experiments. The BV2 cells were infected with tachyzoites of T. gondii RH strain, and the effects of GRh2 were evaluated by MTT assay, morphological observations, immunofluorescence staining, a trypan blue exclusion assay, reverse transcription PCR, and Western blot analyses. The in vivo experiment was conducted with BALB/c mice inoculated with lethal amounts of tachyzoites with or without GRh2 treatment.
Results and conclusion
The GRh2 treatment significantly inhibited the proliferation of T. gondii under in vitro and in vivo studies. Furthermore, GRh2 blocked the activation of microglia and specifically decreased the release of inflammatory mediators in response to T. gondii infection through TLR4/NF-κB signaling pathway. In mice, GRh2 conferred modest protection from a lethal dose of T. gondii. After the treatment, the proliferation of tachyzoites in the peritoneal cavity of infected mice markedly decreased. Moreover, GRh2 also significantly decreased the T. gondii burden in mouse brain tissues. These findings indicate that GRh2 exhibits an anti–T. gondii effect and inhibits the microglial activation through TLR4/NF-κB signaling pathway, providing the basic pharmacological basis for the development of new drugs to treat toxoplasmic encephalitis.
Keywords: Ginsenoside Rh2, Microglia, TLR4, Toxoplasma gondii, Toxoplasmic encephalitis
1. Introduction
The parasite Toxoplasma gondii (T. gondii) causes an opportunistic infection, which rarely causes severe symptoms in immunocompetent individuals [1]; however, immunocompromised individuals infected with T. gondii may lead to life-threatening toxoplasmic encephalitis (TE) from primary or recrudescent infection [2], [3]. Activated microglia may produce an abundance of tumor necrosis factor α (TNF-α) and inducible nitric oxide synthase (iNOS), ultimately leading to neuronal apoptosis and a more severe case of TE [3]. TE is currently treated with a combination of pyrimethamine, sulfadiazine, and leucovorin [4]. However, these treatments may be associated with toxic complications that usually lead to a gradual dose-related bone marrow depression [5]. Therefore, developing effective and nontoxic drugs to treat TE is critical.
Ginseng (Panax ginseng Meyer), which has been used as a traditional tonic and medicine for thousands of years in Asia [6], has been reported to have an adaptogenic effect on endocrine, immune, cardiovascular, and central nervous systems (CNS) [7]. In China, ginseng can be used to treat asthenia syndromes related to the qi and blood and regulate immune functions. In “Shennong Bencaojing”, which was written about 2000 years ago, ginseng was listed as the best tonic because it was nontoxic and could eliminate evil qi (e.g., pathogens and diseases). The textbook of “Bencaojingjie” includes the following statement: “Ginseng benefits qi, and when qi is sufficient, evil cannot remain, so evil qi can be eliminated”. The ginsenoside Rh2 (GRh2) is a characterized component in red ginseng used extensively in Korea and China [8] and has various potent biological functions, including anti-inflammatory [9] and antioxidant [10] activities and preventing neurodegenerative diseases [11]. Previous studies revealed that GRh2 significantly inhibited the lipopolysaccharide (LPS)-induced activation of BV2 cells and decreased the production of the inflammatory mediators via modulating the transforming growth factor-β1/Smad pathway [8]. Thus, GRh2 helps to modulate immune responses and inflammation. Although it was reported that ginseng stem-and-leaf saponins along with recombinant T. gondii–derived heat shock protein 70 (T.g.HSP70) [12] or ginsenoside Re and recombinant T. gondii rhoptry protein 18 [13] elicited substantial immune responses and increased the survival rate of T. gondii-infected mice, the potential protective effects of GRh2 against toxoplasmosis have not been examined.
In this study, we have verified the effects of GRh2 on T. gondii infection for the first time by conducting in vitro and in vivo studies focusing on the BV2 cells and mouse brains. Our results demonstrate that GRh2 inhibits T. gondii proliferation and attenuates microglial activation and neuroinflammation through the toll-like receptor 4 (TLR4)/nuclear factor-kappa B (NF-κB) signaling pathway. These results would provide a rationale for the development of GRh2 as an attractive new target for the treatment of TE.
2. Materials and methods
2.1. Cell culture and materials
The BV2 cells (ATL03001, ICLC, Genova, Italy), a murine microglial cell line, were cultured in Dulbecco's modified Eagle's medium supplemented with 10% heat-inactivated fetal bovine serum (Gibco, NY, USA) and 1% penicillin/streptomycin (Invitrogen, CA, USA) with 5% CO2 at 37°C. GRh2 used in our experiments was 20(S)-ginsenoside Rh2, purchased from Shanghai YuanYe Biotechnology Co., Ltd. (Shanghai, China) with purity of at least 98% in high performance liquid chromatography (HPLC) analysis. Sulfadiazine (SD) or sulfadiazine sodium (SD-Na), which is commonly used to treat human toxoplasmosis, served as a control drug. Dimethyl sulfoxide (DMSO), SD, and SD-Na were purchased from Sigma-Aldrich (St. Louis, MO, USA). GRh2 and SD for in vitro study were dissolved in 0.1% DMSO. GRh2 and SD-Na for in vivo study was suspended in 0.5% carboxymethyl cellulose sodium (CMC-Na) (Sangon Biotech Co., Ltd., Shanghai, China) and deionized water, respectively.
2.2. Mice and T. gondii maintenance
Female BALB/c mice (6–8 weeks old, weighing 18–22 g) were purchased from Experiment Center, Yanbian University (SPF, SCXK (J) 2017-0003, Jilin, China). The virulent RH strain of T. gondii were provided from Chiba University, Japan and maintained by serial intraperitoneal passage in BALB/c mice. All mice were housed in a central animal care facility in a temperature- (23 ± 1°C), humidity-, and atmosphere-controlled room with unrestricted access to food and water and were allowed to adapt to their new environment for at least 7 days before experiments. The experiment was carried out in accordance with the guidelines of the Animal Care Committee of Yanbian University (resolution number, 201501022).
2.3. MTT assay
The cell viability was measured by the MTT 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl-tetrazolium bromide assay. Briefly, the BV2 cells were seeded in 96-well microplates at a density of 1 × 104 cells/well/200 μL with 5% CO2 at 37°C until confluency and then treated with different concentrations (5, 10, 20 and 40 μM) of GRh2. After 24 h of treatment, cells were incubated with 5 mg/mL MTT for 3 h under the same conditions of the culture in the incubator at 37°C, 5% CO2. The formazan crystals were dissolved in DMSO, and the optical density was measured at 570 nm with a Multiskan GO (Thermo Electron Co., Marietta, OH, USA).
2.4. Microscopic observation of parasites and host cells under different infection ratio and culture time
The BV2 cells were seeded in 6-well plates at a density of 8 × 104/well until confluency and then infected with T. gondii tachyzoites at different densities (the ratio of parasite:host cell number = 1:1, 5:1, and 10:1). After 4 hours, the morphological changes of T. gondii–infected and T. gondii–uninfected BV2 cells were comparatively observed under an inverted fluorescence microscope (Olympus IX83, Olympus Corporation, Tokyo, Japan).
Next, the BV2 cells seeded as mentioned previously were infected with T. gondii at the ratio of tachyzoite:cell = 5:1. After 4 hours, T. gondii–infected BV2 cells were washed with medium to remove extracellular parasites and incubated with 0.1% DMSO for 24, 36, and 48 h. Then, their morphological changes were comparatively observed with uninfected cells cultured at same conditions under the inverted fluorescence microscope.
2.5. Anti–T. gondii activity of GRh2 in vitro
2.5.1. Parasite survival
To investigate the direct inhibition effect of GRh2 against tachyzoites, free tachyzoites were in vitro cocultivated directly with GRh2 (10 or 20 μM) and SD (100 μg/mL) in a 96-well U microplate at a density of 1 × 105 or 1 × 106/well. After 36 h treatment, the tachyzoites were collected and stained by trypan blue, and numbers of stained tachyzoites were counted under the Motic AE2000 inverted biological microscope (Motic China Group Co., China). The T. gondii inhibition rate = (T. gondii numbers in culture medium with DMSO – T. gondii numbers in medium with GRh2 or SD)/T. gondii numbers in culture medium with DMSO × 100%.
2.5.2. Microscopic observation of parasite and host cell
To detect the effect of GRh2 on intracellular and extracellular T. gondii, the confluent BV2 monolayers seeded as mentioned previously were infected with T. gondii at the ratio of tachyzoite:cell = 5:1 for 4 h. After removing extracellular parasites, the BV2 cells were incubated with GRh2 (10 or 20 μM) and SD (100 μg/mL). After 36 h treatment, the morphological changes of T. gondii–infected BV2 cells were observed under the inverted fluorescence microscope. Then, cells were collected and stained by trypan blue to count the stained BV2 cells and tachyzoites under the inverted biological microscope.
2.5.3. Reverse transcription PCR
Furthermore, the effects of GRh2 on mRNA expression of T. gondii–specific antigens (SAG1 and T.g.HSP70) were examined by RT-PCR. Glyceraldehyde 3-phosphate dehydrogenase (GAPDH) was used as an internal control. Total RNA from the cell pellets were extracted by using Eastep® Super Total RNA Extraction and reverse transcribed with cDNA Reverse Transcription Kits (Promega Biological Products Co., Ltd., Shanghai, China). The PCR was performed using the following primers: for SAG1, forward (5′-TCGGATCCCCTCTTGTTGC-3′) and reverse (5′-CTCCAGTTTCACGGTACAGT-3′); for T.g.HSP70, forward (5′-GCGAAGTTGTGTTGGTTG-3′) and reverse (5′-GCTCTTTCCGGTGGACT-3′); and for GAPDH, forward (5′-ACCACAGTCCATGCCATCAC-3′) and reverse (5′-TCCACCACCCTGTTGCTGTA-3′). The PCR products were resolved on 1% agarose gel by electrophoresis and then labeled using ethidium bromide (10 mg/mL). The expression levels of SAG1 and T.g.HSP70 mRNAs were calculated from the densities of their RT-PCR products using the following formula: mRNA expression = SAG1 or T.g.HSP70 mRNA/GAPDH mRNA
2.6. The survival analysis of GRh2 in T. gondii–infected mice
Female BALB/c mice were randomly divided into 4 groups (10 animals/group): the negative control group (CN, infection, and vehicle), GRh2 groups (infection and GRh2 treatment with two different doses of GRh2, i.e. 50 mg/kg and 100 mg/kg), and SD-Na group (infection and 100 mg/kg SD-Na treatment). All the mice were intraperitoneally (i.p.) injected with 1 × 105 tachyzoites. Four hours after infection, the mice were orally administered with 0.2 mL of 0.5% CMC-Na, GRh2 (50 and 100 mg/kg/day) and SD-Na, respectively, once daily for 6 days. The mice were observed every day, and their survival rate was calculated for 10 days.
2.7. Anti–T. gondii activity of GRh2 in vivo
2.7.1. Tachyzoites proliferation in peritoneal cavity
As described previously, female BALB/c mice were randomly assigned into 4 groups (10 animals/group): N group (neither infected nor treated), CN group, GRh2 group, and SD-Na group. Except the N group, mice were i.p. infected with 1 × 105 tachyzoites. Four hours after infection, the infected mice were orally administered with 0.2 mL of 0.5% CMC-Na, 100 mg/kg/day GRh2, and 100 mg/kg/day SD-Na for 6 days and the mice were carefully observed daily for the clinical symptoms of CNS injury until 6 days post-infection, that is, before the death. At the last day, blood and brain tissues were collected from all mice of the 4 groups for subsequent experiments. Peritoneal contents were collected for examining peritoneal T. gondii proliferation.
2.7.2. Quantitative competitive PCR
To quantify the T. gondii burden in the brain of each mouse, a 10-mg brain tissue sample taken from each mouse in the respective groups was digested and genomic DNA (gDNA) templates were extracted by using Wizard® SV Genomic DNA Purification System (Promega Co., Madison, USA) following the instructions of the manufacturer. One μg of gDNA extracted from the brain tissue was coamplified with a constant concentration of competitor (truncated SAG1 DNA) using the aforementioned SAG1 primers. The PCR products were electrophoretically separated by the aforementioned methods, and the ratio to competitor (T/C) SAG1 DNA subsequently amplified was measured with an IPLab Gel densitometer (Signal Analytical Co., Vienna, VA., USA). The number of T. gondii was calculated as described previously [14]. Three mice were used for each experimental group.
2.8. Nissl's staining
The mice were deeply anaesthetized with pentobarbital sodium and perfused transcardially with 4% paraformaldehyde in 0.01-M phosphate buffer 24 h after the last session. The brains were removed and fixed for 24 h, then dehydrated with 30% sucrose solution. After that, coronal brain sections were cut at 8 μm with a freezing microtome (CM1900; Leica Microsystems, Wetzlar, Germany) and collected serially. The selected brain sections were stained with Nissl's staining [1% cresyl violet (Xi 'an Hat Biotechnology Co., Ltd., China)] solution at 50°C and then dehydrated through a graded alcohol series (70%, 80%, 90%, and 100%). Then the sections were washed with xylene and covered with a coverslip. Images were examined with the inverted fluorescence microscope and count neuron numbers in the cortex and hippocampus.
2.9. Immunofluorescence staining
The BV2 cells (2 × 105/well) were cultivated and infected with T. gondii (tachyzoite:cell = 5:1) as described previously but on coverslips. Moreover, murine peritoneal exudate cells (PECs) were seeded in a μ-slide 8-well microscopy chamber (Ibidi Co., Martinsried, Germany) at a density of 2 × 105/well. After 36 h, the released tachyzoites from the cells or PECs were fixed with methanol for 30 min onto coverslips or μ-slide 8 well. The cells were permeabilized with 0.2% Triton X-100 in PBS at 4°C for 15 min. Next, the cells were incubated with PBS containing 5% BSA for 30 min and then incubated with the primary antibody against T. gondii (ViroStat Inc., Portland, MA, USA) or NF-κB p65 (Abcam Inc., Cambridge, MA, USA) at 4°C overnight. On the second day, the cells were incubated with Alexa Fluor® 488 donkey anti-rabbit IgG (H+L) (Abcam, Cambridge, MA, USA) for 30 min at room temperature, followed by DAPI (Roche Applied Science, Mannheim, Germany) staining for 30 min before observation. The staining was examined using the inverted fluorescence microscope. The T. gondii or NF-κB p65 protein showed color in green and the nuclei showed in blue. The merged images were conducted using ImageJ software (Wayne Rasband National Institutes of Health, Bethesda, MD, USA) to show colocalization (cyan fluorescence).
2.10. Immunohistochemical staining
The frozen brain tissue sections of cortex from mice were used for double labeling of TLR4 or phospho-NF-κB p65 (p-NF-κB p65) and Iba-1. Sections were fixed in methanol 20 min, washed in PBS, blocked with PBS containing 2% goat serum and 0.3% Triton X-100 at room temperature for 1 h and then followed by incubation with primary antibody specific for Iba-1, TLR4, and p-NF-κB p65 which were purchased from Abcam Inc. (Cambridge, MA, USA) at 4°C overnight. Sections were washed in PBS. Subsequently, the sections were incubated for 1 h at room temperature with Alexa Fluor® 488 donkey anti-goat IgG (H+L) (Thermo Fisher Scientific, USA) for Iba-1 and with Alexa Fluor® 594 donkey anti-rabbit IgG (H+L) (Thermo Fisher Scientific, USA) for TLR4 or p-NF-κB p65. Finally, the sections were stained with DAPI and analyzed with the inverted fluorescence microscope.
2.11. Enzyme-linked immunosorbent assay
Nitric oxide (NO) production in the culture supernatants of BV2 cells and serum of mice was determined using mouse NO ELISA Kit (MLBIO, China) as per the manufacturer's instructions.
2.12. Western blot analysis
Total proteins were extracted from mouse brain tissues (20 mg) or the cell pellets using the RIPA lysis buffer (Solarbio, Beijing, China) following the manufacturer's instructions. The protein concentrations were measured at 562 nm using the bicinchoninic acid (BCA) protein assay kit (BestBio, Shanghai, China). Equal amounts of protein were loaded onto sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and transferred to a polyvinylidene difluoride membrane (Millipore, Bedford, MA, USA). The membrane was blocked with 5% skim milk and then incubated with the corresponding antibody. Antibodies for TLR4, MyD88, NF-κB p65, TNF-α, and β-actin were purchased from Cell Signaling Technology (Beverly, MA, USA). Antibodies for TRIF, p-NF-κB p65, IκBα, phospho-IκBα (p-IκBα), Iba-1, iNOS, and Interferon-γ (IFN-γ) were purchased from Abcam Inc. (Cambridge, MA, USA). After the membranes were washed with 1 × PBS containing 0.05% Tween-20, they were incubated with horseradish peroxidase–conjugated secondary antibody purchased from Proteintech Group (Chicago, IL, USA) at room temperature for 1 h. After repeating the washing step, protein bands were visualized using the ECL Western Blot analysis kit (Millipore Co., Billerica, MA, USA).
2.13. Statistical analysis
All data were expressed as the mean ± standard deviation (SD). A comparison of the results was performed by one-way analysis of variance (ANOVA) and Tukey's multiple comparison tests (Graphpad Software, Inc., San Diego, CA, USA). Statistic differences on the survival of mice were analyzed by Kaplan–Meier (log rank test). Statistically significant differences between groups were defined as p < 0.05.
3. Results
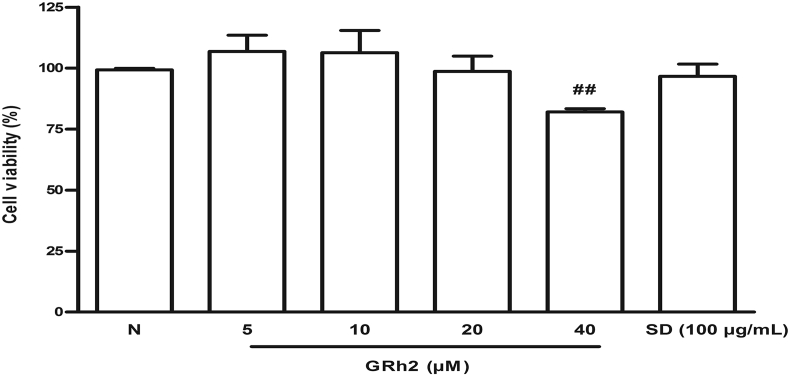
3.1. Effect of GRh2 on cell viability
Before investigating the effects of GRh2 on T. gondii proliferation, we first assayed its cytotoxicity by treating BV2 cells with GRh2 at various concentrations (5, 10, 20, and 40 μM) and SD (100 μg/mL) for 24 h and then performed the MTT assay. At concentrations below 20 μM, GRh2 was not cytotoxic and rather enhanced the proliferation of BV2 cells. In contrast, at 40 μM, GRh2 decreased cell viability to 82.64% (p < 0.01 vs. N group). In addition, the SD (100 μg/mL) treatment did not adversely affect cell viability (Fig. 1). Thus, we concluded that the viability of BV2 cells was not inhibited by GRh2 at concentrations below 20 μM.
Fig. 1.
GRh2 cytotoxicity in BV2 cells. BV2 cells treated with GRh2 (5–40 μM) or SD (100 μg/mL) for 24 h and the cell viability was measured using the MTT assay. Three independent experiments were conducted in triplicate, and data were expressed as the mean ± standard deviation. ##p < 0.01 vs. N group. SD, sulfadiazine.
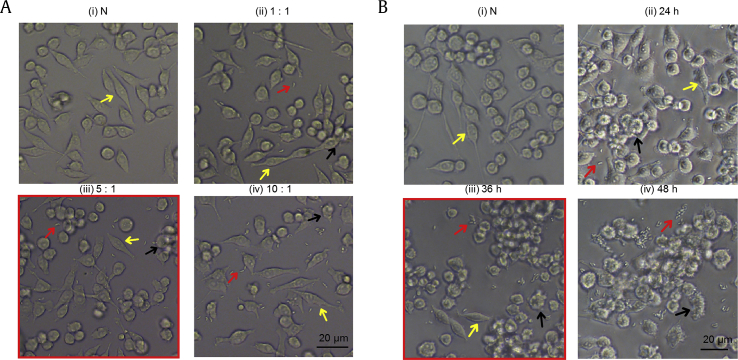
3.2. The interaction between tachyzoites and BV2 cells
Before the in vitro study of T. gondii infection, we have determined the infection ratio of T. gondii vs. BV2 cell numbers. As shown in Fig. 2A, morphology of uninfected BV2 cells (N) was intact with normal growth after the 4-h cell culture. When BV2 cells were infected at the ratio of parasite:host = 1:1, a small number of extracellular tachyzoites were observed; while the BV2 cells were unaffected, they were of the similar appearance with the N groups. When the infection ratio was 5:1, the opportunity of tachyzoites' invasion increased and most BV2 cells were infected. On the other hand, when the infection ratio was 10:1, almost all BV2 cells were infected, while many extracellular tachyzoites still existed and some host cells began to rupture by proliferated tachyzoites. Therefore, we have decided to infect BV2 cells at the ratio of parasite:host = 5:1 for the subsequent experiments.
Fig. 2.
Microscopic observation of tachyzoites and BV2 cells. (A) BV2 cells cocultured with different parasites ratio. (i) Normal BV2 cells without T. gondii infection. (ii) The parasite:host ratio was 1:1. (iii) The parasite:host ratio was 5:1. (iv) The parasite:host ratio was 10:1. (B) BV2 cells cocultured with different infection duration. (i) Normal BV2 cells. (ii) For 24-h culture. (iii) For 36-h culture. (iv) For 48-h culture. The red arrow indicated T. gondii tachyzoite, the black arrow indicated the sensitized cell, and the yellow arrow indicated the normal cell.
Then, we have tested the duration of BV2 cell culture with T. gondii at the infection ratio of parasite:host = 5:1. As shown in Fig. 2B, only a small number of extracellular tachyzoites were observed at 24-h infection. On the other hand, at 36-h infection, BV2 cells swelled because of intracellular T. gondii proliferation and some cells began to rupture which resulted in the release of tachyzoites outside of cells. When cultured for 48 h, almost all host cells were destroyed and tachyzoites could not survive anymore without new host cells. Thus, the appropriate duration of BV2 cell infection was considered 36 h.
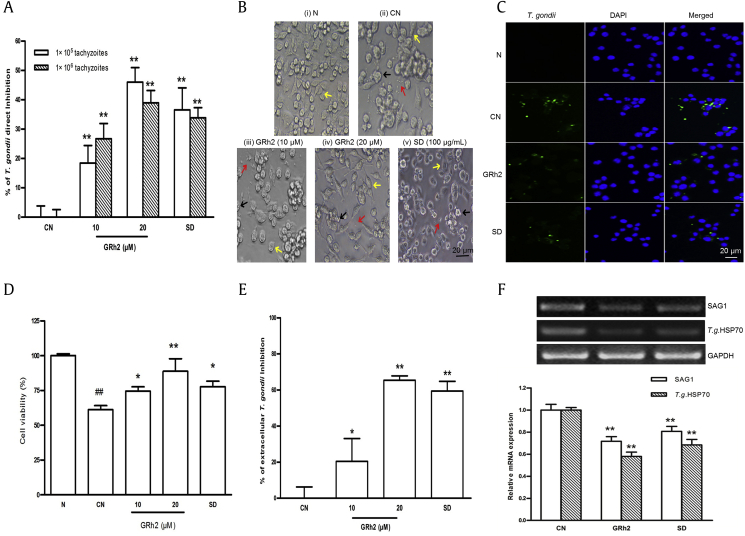
3.3. Effects of GRh2 on in vitro T. gondii infection
First, we examined the direct inhibition effect of GRh2 against tachyzoites by adding GRh2 to free tachyzoites culture for 36 h in the absence of host cells. As shown in Fig. 3A, the direct inhibition rates on 1 × 105 and 1 × 106 tachyzoites by 10 μM GRh2 were 18.42 ± 5.46% and 26.75 ± 5.20%, respectively, those by 20 μM GRh2 were 46.02 ± 4.53% and 38.96 ± 4.20%, respectively, and those by 100 μg/mL SD were 36.56 ± 6.84% and 33.87 ± 3.44%, respectively. These rates with 10 or 20 μM GRh2 or 100 μg/mL SD treatment differed significantly from those of the CN group (p < 0.01, p < 0.01, and p < 0.01, respectively, for both tachyzoites number).
Fig. 3.
The inhibition effects of GRh2 against T. gondii in the in vitro infection study. (A) Direct inhibition rate on tachyzoites. (B) Morphological characteristics during a microscopy analysis. The red arrow indicated T. gondii tachyzoite, the black arrow indicated the sensitized cell, and the yellow arrow indicated the normal cell. (C) Immunofluorescence of T. gondii–infected BV2 cells. The T. gondii was indicated in green, whereas the DAPI stain (blue) indicated the location and size of nuclei. (D) and (E) The living host cells viability and extracellular T. gondii inhibition rate. (F) RT-PCR analysis for determining SAG1 and T.g.HSP70 mRNA expression in the BV2 cells. Three independent experiments were conducted in triplicate, and data were expressed as the mean ± standard deviation. ##p < 0.01 vs. N group; ∗p < 0.05 and ∗∗p < 0.01 vs. CN group. RT-PCR, reverse transcription PCR; SD, sulfadiazine.
Next, effects of GRh2 on T. gondii–infected BV2 cells were tested. The T. gondii–infected BV2 cells were washed to remove extracellular parasites before starting the treatment with GRh2 and SD as mentioned in the methods. After 36 h treatment, the morphological changes of the infected BV2 cells and the extracellular release of tachyzoites were examined. In the CN group, tachyzoites from the ruptured cells were detected in the medium and only a few intact cells remained. Conversely, in the treated groups, most of the host cells remained intact and fewer tachyzoites were released into the medium. The 20-μM GRh2 treatment resulted in the fewest extracellular and intracellular tachyzoites that appeared to cease developing (Fig. 3B). Furthermore, the expression of a tachyzoite-specific antigen was investigated based on immunofluorescence staining with an anti–T. gondii antibody. In the CN group, T. gondii tachyzoites were detected much more both intracellularly and extracellularly. However, in the treated group, tachyzoites expression was sparse (Fig. 3C).
The viability of BV2 cells in the CN group was only 61.18 ± 2.90% of that of the N group. However, after the treatment with 10 or 20 μM GRh2 or 100 μg/mL SD, the viability of BV2 cells significantly increased to 74.53 ± 3.08%, 88.80 ± 9.05%, and 77.75 ± 3.92%, respectively. These were different from the CN group (p < 0.05, p < 0.01, and p < 0.05, respectively) (Fig. 3D). When treated with 10 or 20 μM GRh2 or 100 μg/mL SD, the inhibition rate of extracellular T. gondii in infected BV2 cells was 22.85 ± 12.49%, 65.08 ± 2.92%, and 63.40 ± 3.06%, respectively. These results also differed significantly from that of the CN group (p < 0.05, p < 0.01, and p < 0.01, respectively) (http://parasitol.kr/journal/view.php?doi=10.3347/kjp.2016.54.2.139 Fig. 3E). Since inhibitory effects of GRh2 against T. gondii were greater at higher dose, the follow-up experiments were conducted with 20-μM GRh2.
To determine whether GRh2 inhibited intracellular T. gondii, we further examined the inhibitory effect of GRh2 on the expression of tachyzoite-specific SAG1 and T.g.HSP70 mRNA in T. gondii-infected BV2 cells. We found that the levels of SAG1 and T.g.HSP70 mRNA expression in T. gondii-infected BV2 cells were considerably much lower in the treatment groups (GRh2 and SD) than in the CN group (p < 0.01 and p < 0.01, respectively, for SAG1 and T.g.HSP70) (Fig. 3F).
Taken together, these results indicated that GRh2 and SD could efficiently inhibit both extracellular and intracellular T. gondii proliferation in BV2 cells.
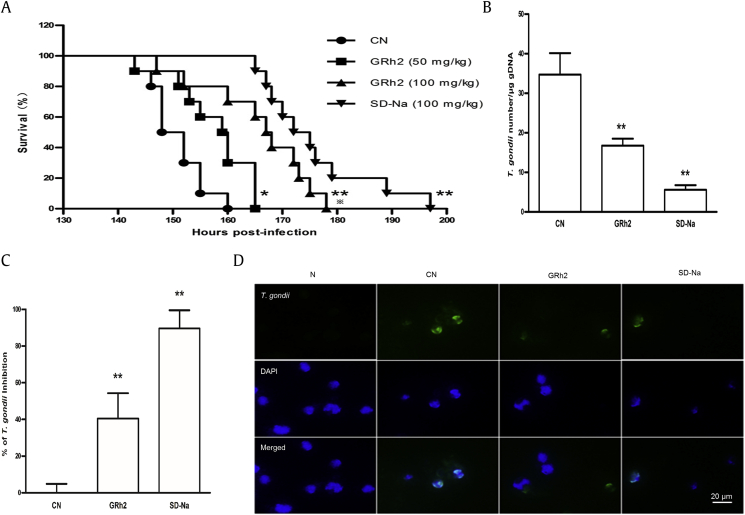
3.4. Effects of GRh2 on in vivo T. gondii infection
To further evaluate the effect of GRh2 on T. gondii, we performed in vivo experiments. First, we examined the effect of GRh2 on the survival of T. gondii–infected mice (Fig. 4A). The mice in the CN group began dying at 143 h after the infection, and all mice died within 160 h. However, in the GRh2 (50 mg/kg), GRh2 (100 mg/kg), and SD-Na (100 mg/kg) groups, the mice began dying at 143 h, 152 h, and 165 h after the infection, respectively, and all mice died within 165 h, 178 h and 197 h, respectively. The survival time of mice treated with GRh2 (50 mg/kg), GRh2 (100 mg/kg), and SD-Na (100 mg/kg) was 157.60 ± 7.17 h, 165.70 ± 10.05 h, and 175.80 ± 10.21 h, respectively. These survival times were significantly different from the CN group (150.70 ± 5.06 h) (p < 0.05, p < 0.01 and p < 0.01, respectively). Thus, treatments with GRh2 and SD-Na significantly prolonged survival, although the drug treatments did not prevent the mice from dying. Because 100 mg/kg GRh2 had a greater effect than 50 mg/kg GRh2 (p < 0.05), 100 mg/kg GRh2 and 100 mg/kg SD-Na were used for the subsequent experiments.
Fig. 4.
Anti–T. gondii activity of GRh2 in BALB/c mice. (A) Treatment effects on the survival of T. gondii–infected BALB/c mice. (B) QC-PCR analysis for determining T. gondii abundance in the brain. (C) Tachyzoites inhibition rate in the peritoneal cavity. (D) Immunofluorescence of T. gondii–infected PECs. The T. gondii was indicated in green, whereas the DAPI staining (blue) indicated the location and size of nuclei. Three independent experiments were conducted in triplicate, and data were expressed as the mean ± standard deviation. ∗p < 0.05 and ∗∗p < 0.01 vs. CN group. QC-PCR, quantitative competitive PCR; SD-Na, sulfadiazine sodium; gDNA, genomic DNA.
Next, the abundance of T. gondii tachyzoites was significantly greater in the brains of mice in the CN group (34.75 ± 5.42/μg gDNA) than in the brains of mice in the GRh2 (16.76 ± 1.76/μg gDNA) and SD-Na (5.6 ± 1.15/μg gDNA) groups (p < 0.01 and p < 0.01, respectively) (Fig. 4B). Meanwhile, the average inhibition of T. gondii in the peritoneal cavity of mice was 40.52 ± 13.73% in the GRh2 group and 89.64 ± 9.92% in the SD-Na group, respectively, and these values were significantly different from the inhibition observed in the mice of the CN group (p < 0.01 and p < 0.01, respectively) (Fig. 4C). Moreover, the abundance of T. gondii tachyzoites in PECs was investigated by immunofluorescence. The fluorescent signal representing tachyzoites was detected intracellularly and extracellularly in the CN group, whereas it was sparse in the treated groups, especially in the GRh2 group (Fig. 4D). These results implied that GRh2 could efficiently play against acute T. gondii infection under in vivo conditions.
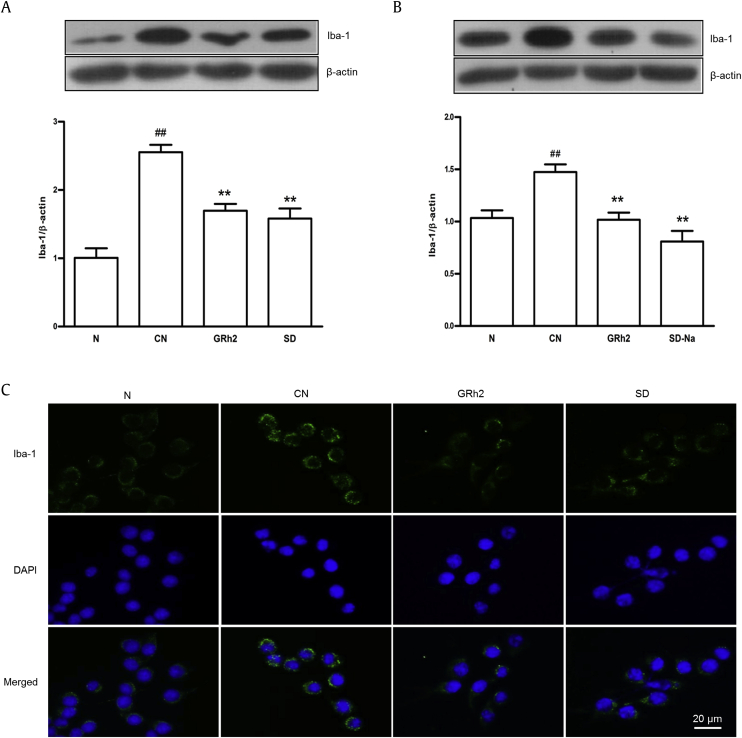
3.5. Effects of GRh2 on microglial activation
To investigate the effects of GRh2 on the microglial activation, we used Western blot analysis to examine the production of Iba-1 (a microglia-specific marker) in T. gondii–infected BV2 cells (Fig. 5A) and mouse brain tissues (Fig. 5B). Our analyses revealed that Iba-1 production in BV2 cells and mouse brain tissues was significantly higher in the CN group than in the N group (p < 0.01). Treatments with GRh2 and SD (SD-Na) resulted in similar significant decreases to the Iba-1 abundance in BV2 cells and brain tissues (p < 0.01, p < 0.01) relative to the amount in the CN group (Figs. 5A, 5B). Furthermore, immunofluorescence staining results revealed that the GRh2 or SD treatment inhibited Iba-1 expression compared with the CN group (Fig. 5C). These results suggested that GRh2 and SD (SD-Na) inhibited the excessive activation of microglia induced by T. gondii infection.
Fig. 5.
The effects of GRh2 on antimicroglia activation after T. gondii infection. Western blot analysis of Iba-1 protein expression in (A) BV2 cells and (B) mouse brain tissues. (C) The effects of GRh2 on Iba-1expression in T. gondii–infected BV2 cells by immunofluorescence assay. Three independent experiments were conducted in triplicate, and data were expressed as the mean ± standard deviation. #p < 0.01 vs. N group; ∗∗p < 0.01 vs. CN group. SD, sulfadiazine; SD-Na, sulfadiazine sodium.
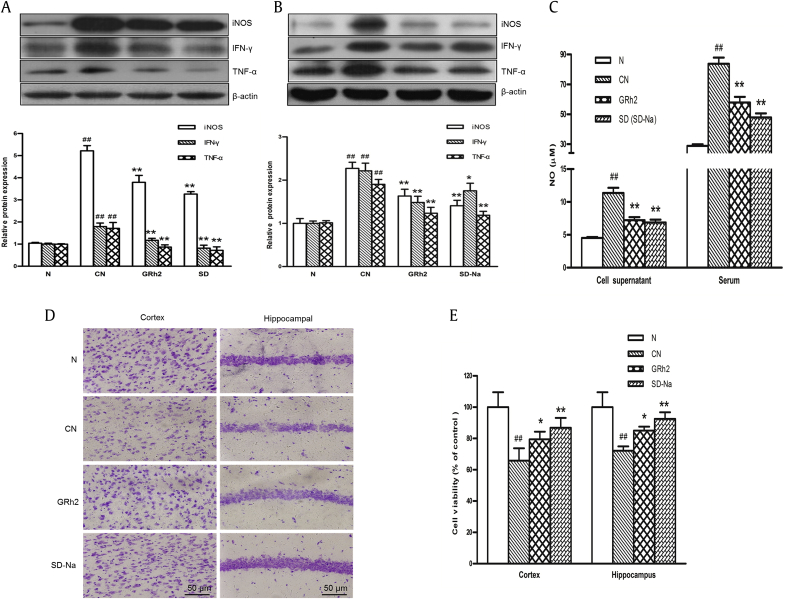
3.6. Effects of GRh2 on the production of inflammatory mediators and the neuronal injury
Activated microglia contributed to the production of inflammatory mediators that directly or indirectly mediate neuronal death [3]. In this study, we analyzed the inflammatory mediators produced by activated BV2 cells and mouse brain tissues challenged with tachyzoites. Western blot analysis indicated that the production of iNOS, IFN-γ, and TNF-α was significantly elevated in BV2 cells (Fig. 6A) and mouse brain tissues (Fig. 6B) after the parasite infection (p < 0.01 vs. N group). The GRh2 and SD (SD-Na) treatment during the T. gondii infection notably restricted the release of iNOS, IFN-γ, and TNF-α from activated microglia under in vitro and in vivo conditions (Figs. 6A, 6B). And the T. gondii infection induced a significant increase in NO production, as indicated by the amount of nitrite that accumulated in the culture supernatants of BV2 cells and in mice serum (Fig. 6C) (p < 0.01 and p < 0.01, respectively, vs. N group). A considerable suppression of NO production in BV2 cells and mice serum was induced by GRh2 and SD (SD-Na) (p < 0.01 and p < 0.01, respectively, vs. CN group) (Fig. 6C).
Fig. 6.
The effects of GRh2 on inflammatory mediator production and neuronal morphology after T. gondii infection. Western blot analysis was completed to analyze iNOS, IFN-γ, and TNF-α expression in (A) BV2 cells and (B) mouse brain tissues. (C) The nitrite concentration was determined for the BV2 cells culture supernatants or mice serum based on the ELISA. (D) and (E) Neuronal morphology and density in the cortex and hippocampus by Nissl staining. Three independent experiments were conducted in triplicate, and data were expressed as the mean ± SD. ##p < 0.01 vs. N group; ∗∗p < 0.01 vs. CN group. IFN-γ, Interferon-γ; iNOS, inducible nitric oxide synthase; TNF-α, tumor necrosis factor α; ELISA, enzyme-linked immunosorbent assay.
In addition, we examined neuronal morphology and density in the cortex and hippocampus by Nissl staining. The CN group displayed signs of significant neuronal damage in the cortex and hippocampus. However, treatment with GRh2 or SD-Na increased the number of normal-looking neurons in the T. gondii infection mice (Fig. 6D). The T. gondii infection group had a lower surviving cell density in the cortex and hippocampus than the N group (p < 0.01, p < 0.01, respectively). The treatment with GRh2 or SD-Na groups had a higher cell density in the cortex and hippocampus than the CN group (p < 0.05 and p < 0.01, respectively, for cortex and hippocampus) (Fig. 6E). Taken together, these results suggested that GRh2 and SD-Na increased neuronal viability in the brain of mice with T. gondii infection.
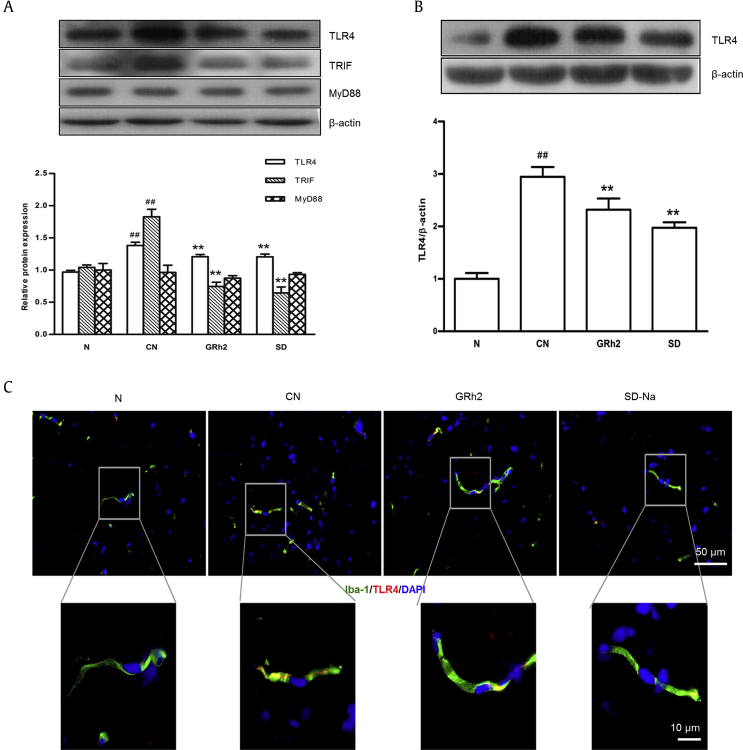
3.7. Effects of GRh2 on the TLR4, TRIF, and MyD88 expression
To further investigate whether a GRh2 treatment affects the T. gondii–induced TLR4 signaling pathway, we completed Western blot analysis to examine TLR4-mediated protein expression in BV2 cells (Fig. 7A) and mouse brain tissues (Fig. 7B). As expected, the TLR4 expression was significantly higher in the BV2 cells and brain tissues of mice infected with T. gondii than in the uninfected N group (p < 0.01) (Figs. 7A, 7B). We examined MyD88 and TRIF expression in T. gondii–infected or T. gondii–uninfected BV2 cells. Western blot analysis indicated that TRIF expression was significantly higher in the CN group than in the N group (p < 0.01). In addition, the TRIF expression was significantly lower in the GRh2 and SD groups than in the CN group (p < 0.01 and p < 0.01, respectively). In contrast, the abundance of MyD88 was unaffected by the T. gondii infection or a treatment with GRh2 or SD (Fig. 7A). These results suggested that GRh2 could inhibit the TLR4/TRIF signal cascade induced in T. gondii–infected BV2 cells. Next, to examine the TLR4 expression in the microglia of cortex of the infected mice with or without GRh2 and SD-Na treatment, we assessed expression levels of Iba-1 and TLR4 in the cortex by immunohistochemical double labeling. As shown in Fig. 7C, TLR4 was highly expressed by microglia in the cortex of T. gondii–infected mice, and its expression was effectively inhibited by GRh2 and SD-Na treatment.
Fig. 7.
The effects of GRh2 on TLR4-mediated signal after T. gondii infection. Western blot analysis was completed to analyze (A) the TLR4, TRIF, and MyD88 expression in BV2 cells and (B) the TLR4 expression in mouse brain tissues. (C) Immunohistochemical double labeling for TLR4 (red) and Iba1 (green) in the cortex. The areas in the square were shown below at higher magnification. Three independent experiments were conducted in triplicate, and data were expressed as the mean ± standard deviation. ##p < 0.01 vs. N group; ∗∗p < 0.01 vs. CN group. SD-Na, sulfadiazine sodium.
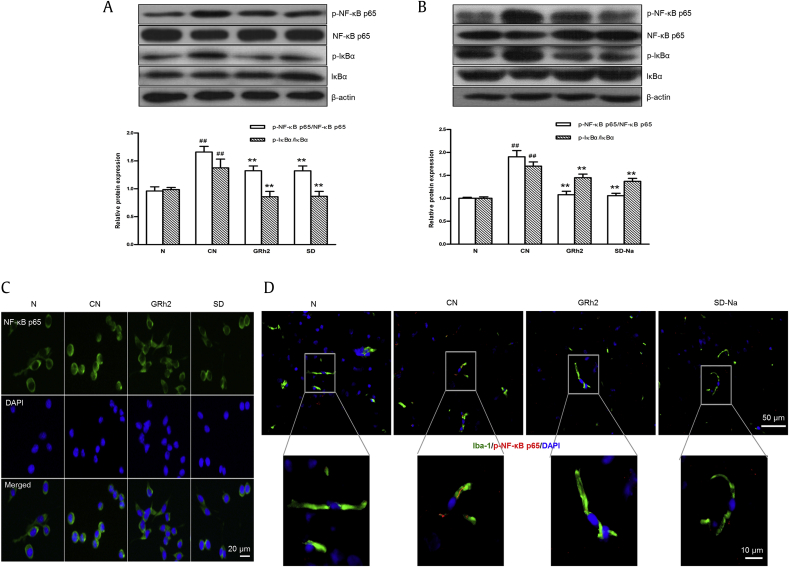
3.8. Effects of GRh2 on the IκBα degradation and NF-κB p65 nuclear translocation
We investigated whether GRh2 affected on the NF-κB signaling pathway by conducting Western blot and immunofluorescence analyses of BV2 cells and mouse brain. A comparison of the uninfected N group and the CN group suggested that the T. gondii infection increased the degradation of cytosolic IκBα and the nuclear translocation of NF-κB p65 of BV2 cells (Fig. 8A) and mouse brain (Fig. 8B). However, the GRh2 or SD (SD-Na) treatment significantly attenuated the infection-induced phosphorylation of IκBα and NF-κB p65 relative to the corresponding levels in the CN group (p < 0.01 and p < 0.01, respectively) (Figs. 8A, 8B). Furthermore, the immunofluorescence staining of BV2 cells revealed that the GRh2 or SD treatment inhibited the nuclear translocation of NF-κB p65 compared to the CN group (Fig. 8C). Moreover, the expression levels of Iba-1 and p-NF-κB p65 and the effects of GRh2 and SD-Na treatment were assessed in the microglia of the cortex by immunohistochemical double labeling. As shown in Fig. 8D, p-NF-κB p65 was highly expressed by microglia in the cortex of T. gondii–infected mice, and GRh2 or SD-Na could inhibit their expression.
Fig. 8.
The effects of GRh2 on IκBα degradation and NF-κB p65 nuclear translocation after T. gondii infection. Western blot analysis was completed to analyze NF-κB p65, p-NF-κB p65, IκBα, and p-IκBα expression in (A) BV2 cells and (B) mouse brain. (C) Representative confocal microscopic images showing labeling for Iba-1 (green) in the BV2 cells. (D) Immunohistochemical double labeling for p-NF-κB p65 (red) and Iba1 (green) in the cortex. The areas in the square were shown below at higher magnification. Three independent experiments were conducted in triplicate, and data were expressed as the mean ± standard deviation. ##p < 0.01 vs. N group; ∗∗p < 0.01 vs. CN group. SD, sulfadiazine; SD-Na, sulfadiazine sodium.
4. Discussion
In immunocompromised individuals, the toxoplasmosis is supposed to occur in acute form and causes acute TE [15]. In humans, proliferating tachyzoites have been detected in glial cells in a patient who developed TE [16]. However, relatively little is known about the precise molecular mechanisms underlying the inflammation associated with the CNS. The present study is the first to demonstrate the effects of GRh2 against T. gondii–induced inflammatory mechanisms in TE through TLR4/NF-κB signaling pathway.
In our in vivo experiment, we assessed the effects of GRh2 on the acute phase of toxoplasmosis in female BALB/c mice infected with the tachyzoites of the highly virulent type I T. gondii RH strain. We found that the GRh2 markedly improved the clinical neurological symptoms of CNS such as ataxia or paraplegia in T. gondii infected mice and considerably decreased the T. gondii loads in the PECs and brain. Meanwhile, GRh2 extended the survival of mice infected with a lethal dose of virulent tachyzoites in a dose-dependent manner. Most importantly, neuroinflammation and neuron damages were markedly improved after the treatment with GRh2 or SD-Na. These results have proved that GRh2 exhibits effective anti–T. gondii and antineuroinflammatory activities which protect neuron injuries.
Type I strain tachyzoites have a tendency to grow more aggressively than type II and III strains in host cells, and the aggressiveness might contribute to the development of TE and other psychiatric disorders such as schizophrenia [17], whereas the blood–brain barrier would protect rapid distribution of tachyzoites into the brain [18]. The type I RH strain tachyzoites are 100% lethal to mice and do not convert to bradyzoites (i.e., do not form cysts). Therefore, the survival has not been rescued even by the positive control, and extension of the survival is meaningful. On the other hand, other T. gondii strains which convert from tachyzoites to bradyzoites (i.e., cyst formation) can chronically live inside of the brain, muscle, or other organs in hosts during the life of hosts. Preliminary experiments revealed that infection with 1 × 105 tachyzoites of RH strain was suitable to analyze murine brain changes because less number of zoites failed to induce 100% detection of T. gondii SAG1 gene and inflammatory histopathological changes in the brain (data not shown). Moreover, female mice are considered more susceptible to T. gondii infection than male mice. Sex-related differences in the prevalence of clinical toxoplasmosis were probably due to the effect of female hormones on the immune system [19].
Microglia are resident macrophages of the brain and represent the first line of immune defense in the CNS [20]. The BV2 cells, an immortalized murine microglial cell line derived from raf/myc-immortalized murine neonatal microglia, are the most frequently used as a substitute for primary microglia [21]. Therefore, we used BV2 cells to detect T. gondii proliferation under in vitro experiment. The SAG1 is a major surface antigen of T. gondii tachyzoites and is one of the main targets of the host immune response [22]. In addition, T.g.HSP70, which influences the virulence of T. gondii tachyzoites, is highly expressed during the lethal stage of acute toxoplasmosis [23]. Thus, as tachyzoite-specific markers, SAG1 and T.g.HSP70 are useful to detect the proliferation of T. gondii tachyzoites. Our study shows the decrease of SAG1 and T.g.HSP70 mRNA levels in T. gondii–infected BV2 cells by GRh2, indicating that the GRh2 treatment effectively eliminates intracellular T. gondii activity in BV2 cells.
T. gondii growth is the result of repeated cycles of host cell invasion, replication, and egress [24]. Infection of microglia induces hypermotility and enhances their transmigration, implying that microglia may represent a possible mechanism for parasite dissemination in the brain of host [25]. This association may contribute to substantial changes in morphology and confluence observed in T. gondii–infected BV2 cells. However, in the present study, GRh2 decreased the number of T. gondii tachyzoites in BV2 cells in a dose-dependent manner, and the microglia seemed to remain metabolically active and viable. In addition, the number of GRh2-treated BV2 cells significantly increased in a dose-dependent manner. These results imply that GRh2 protects host cells from an invasion by T. gondii as well as the subsequent proliferation. Thus, GRh2 can effectively disrupt T. gondii infections and has a protective effect on the host cells.
Encephalitis is the most serious consequence of hosts by T. gondii-infection [26]. Microglia are extremely sensitive to brain microenvironment stimuli and respond to pathogen or tissue damage by altering their morphology and phenotype [3]. T. gondii infection promotes the migration and activation of microglia in the brain of hosts [26], and the resulting activated microglia contribute to neuronal damage via the release of excessive inflammatory mediators [3], [27]. GRh2 has been reported to inhibit LPS-induced cell activation and decrease the excessive production of proinflammatory cytokines in a murine macrophage cell line [28].
In the present study, the enhanced Iba-1 expression and the excessive IFN-γ, TNF-α, and iNOS expression in T. gondii–infected BV2 cells and mouse brain tissues were significantly inhibited by GRh2 treatment. Thus, we confirmed that GRh2 could attenuate the activation of microglia and restrict the production of excessive inflammatory mediators.
Toxoplasmic encephalitis is regulated by complex interconnected signaling networks including TLRs which form a major family of pathogen-associated molecular patterns [29]. Earlier study reported that the expression of TLR4 was upregulated in the brain tissues of rats chronically infected with the T. gondii, resulting in inflammation and brain injuries [30], [31]; however, the underlined mechanisms remain unclear. On the other hand, we have reported that T.g.HSP70 is an agonist of TLR2 and TLR4, and T.g.HSP70 stimulates B cell and bone marrow–derived DC in mice via the TLR4/TRIF pathway [32], [33].
Furthermore, we confirmed that T.g.HSP70-induced anaphylactic reactions in T. gondii–infected mice occurred via the TLR4/MyD88 signaling pathway [34], [35]. Moreover, T. gondii reportedly activates NF-κB, thereby upregulating the expression of antiapoptotic genes and promoting a localized phosphorylation of IκB, which reflects the ability of parasites to regulate the NF-κB cascade [36]. Another study concluded that T. gondii excretory/secretory antigens suppress the secretion of inflammatory mediators by inhibiting the TLR-induced activation of NF-κB [37]. Furthermore, the infection of rat intestinal epithelial cells by T. gondii sporozoites primarily results in upregulated expression of genes associated with TNF-α signaling via NF-κB [38].
In this study, we infected BV2 cells and mouse brains with tachyzoites from a virulent RH strain and subsequently analyzed the changes in the major proteins related to TLR4/NF-κB signaling. The RH tachyzoites promoted the activities of TLR4, TRIF, p-NF-κB p65, and p-IκBα but not MyD88. We also observed that GRh2 downregulated the expression of genes encoding these proteins, but not the MyD88. These findings are consistent with the results of other studies in which macrophage responses to the RH strain occurred independently of MyD88 [39], [40], [41].
However, although previous reports speculated the virulence of T.g.HSP70 in murine toxoplasmosis via modulation of host NF-κB and NO [42], [43], the activation of microglia directly induced by live T. gondii tachyzoites through the TLR4/NF-κB signaling pathway remains poorly characterized. Following our results, it would be possible to speculate that the T.g.HSP70 from live tachyzoites may contribute to TLR4 signaling in T. gondii–infected microglia, while precise mechanisms remain to be analyzed in a future study. Therefore, in TE, the modulation of TLR4 signaling involving TRIF, IκBα, and NF-κB may represent the molecular mechanism underlying the beneficial effects of GRh2 on inflammatory mediators and microglial activation.
By the basis of the “traditional Chinese medicine” theory regarding the balance between yin and yang, we propose that parasite-induced increases in inflammatory mediator production lead to an imbalance in the yin and yang of the host, ultimately resulting in acute toxoplasmosis. The results of our experiments suggest that GRh2 can regulate the excessive immune responses in T. gondii–infected microglia, inhibit neuroinflammation, decrease the abundance of T. gondii in the brain, and increase the survival rate of infected mice. Hence, we speculate that the ability of ginseng to invigorate the immune system and antipathogenic factors is retained by GRh2 to maintain the balance between yin and yang and ultimately protect the host from T. gondii infection.
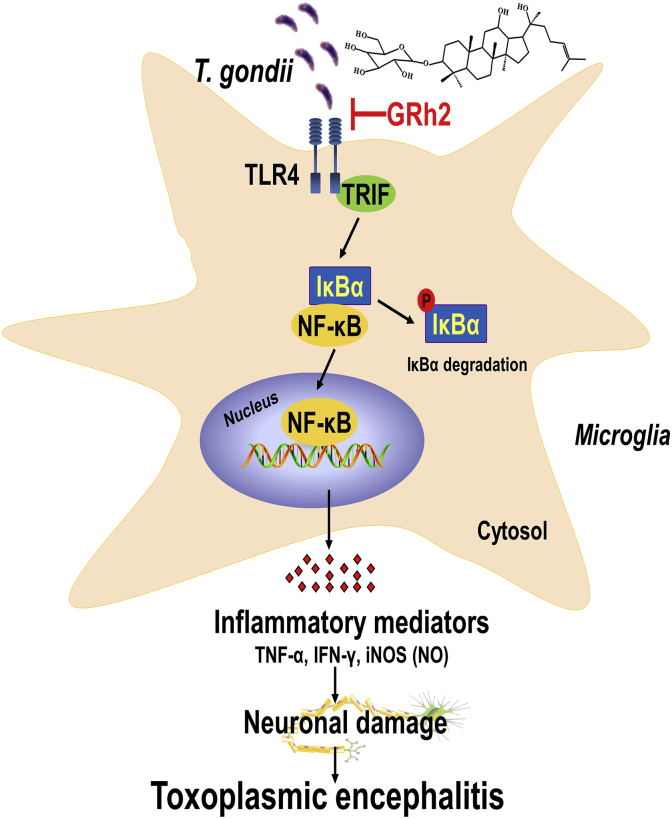
To the best of our knowledge, this is the first study that reveals GRh2 inhibits the proliferation of T. gondii and the excessive production of inflammatory mediators [e.g., IFN-γ, TNF-α, and iNOS (NO)] in activated microglia via the TLR4/NF-κB signaling pathway under in vitro and in vivo studies (Fig. 9). Our findings represent the first pharmacological evidence that GRh2 is an attractive new target for the treatment of TE.
Fig. 9.
A proposed mechanism of GRh2 against TE by attenuating microglial activation via TLR4/NF-κB signaling pathway. TE, toxoplasmic encephalitis; IFN-γ, Interferon-γ; iNOS, inducible nitric oxide synthase; TNF-α, tumor necrosis factor α.
Conflicts of interest
The authors declare no conflicts of interest.
Declaration of transparency and scientific rigor
This declaration acknowledges that this article adheres to the principles for transparent reporting and scientific rigor of preclinical research recommended by funding agencies, publishers, and other organizations engaged with supporting research.
Acknowledgments
This work was supported by the grants from the National Natural Science Foundation of China (81660344 and 81260251). This work was partially supported by Jilin Province Science and Technology Development Plan item (20190201149JC).
Contributor Information
Juan Ma, Email: majuan@ybu.edu.cn.
Lian-Xun Piao, Email: lxpiao@ybu.edu.cn.
References
- 1.Dubey J.P., Jones J.L. Toxoplasma gondii infection in humans and animals in the United States. Int J Parasitol. 2008;38:1257–1278. doi: 10.1016/j.ijpara.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 2.Zhang J.L., Si H.F., Shang X.F., Zhang X.K., Li B., Zhou X.Z., Zhang J.Y. New life for an old drug: In vitro and in vivo effects of the anthelmintic drug niclosamide against Toxoplasma gondii RH strain. Int J Parasitol Drugs Drug Resist. 2018;9:27–34. doi: 10.1016/j.ijpddr.2018.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang Y.H., Chen H., Chen Y., Wang L., Cai Y.H., Li M., Wen H.Q., Du J., An R., Luo Q.L. Activated microglia contribute to neuronal apoptosis in Toxoplasmic encephalitis. Parasit Vectors. 2014;7:372. doi: 10.1186/1756-3305-7-372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Connolly M.P., Goodwin E., Schey C., Zummo J. Toxoplasmic encephalitis relapse rates with pyrimethamine-based therapy: systematic review and meta-analysis. Pathog Glob Health. 2017;111:31–44. doi: 10.1080/20477724.2016.1273597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ben-Harari R.R., Goodwin E., Casoy J. Adverse event profile of pyrimethamine-based therapy in toxoplasmosis: a systematic review. Drugs R D. 2017;17:523–544. doi: 10.1007/s40268-017-0206-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim Y.S., Woo J.Y., Han C.K., Chang I.M. Safety analysis of Panax ginseng in randomized clinical trials: a systematic review. Medicines. 2015;2:106–126. doi: 10.3390/medicines2020106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hu J.N., Xu X.Y., Li W., Wang Y.M., Liu Y., Wang Z., Wang Y.P. Ginsenoside Rk1 ameliorates paracetamol-induced hepatotoxicity in mice through inhibition of inflammation, oxidative stress, nitrative stress and apoptosis. J Ginseng Res. 2019;43:10e19. doi: 10.1016/j.jgr.2017.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vinoth Kumar R., Oh T.W., Park Y.K. Anti-inflammatory effects of ginsenoside-Rh2 Inhibits LPS-induced activation of microglia and overproduction of inflammatory mediators via modulation of TGF-β1/Smad pathway. Neurochem Res. 2016;41:951–957. doi: 10.1007/s11064-015-1804-x. [DOI] [PubMed] [Google Scholar]
- 9.Li L.C., Piao H.M., Zheng M.Y., Lin Z.H., Choi Y.H., Yan G.H. Ginsenoside Rh2 attenuates allergic airway inflammation by modulating nuclear factor-κB activation in a murine model of asthma. Mol Med Rep. 2015;12:6946–6954. doi: 10.3892/mmr.2015.4272. [DOI] [PubMed] [Google Scholar]
- 10.Park H.M., Kim S.J., Mun A.R., Go H.K., Kim G.B., Kim S.Z., Jang S.I., Lee S.J., Kim J.S., Kang H.S. Korean red ginseng and its primary ginsenosides inhibit ethanol-induced oxidative injury by suppression of the MAPK pathway in TIB-73 cells. J Ethnopharmacol. 2012;141:1071–1076. doi: 10.1016/j.jep.2012.03.038. [DOI] [PubMed] [Google Scholar]
- 11.Kim K.H., Lee D., Lee H.L., Kim C.E., Jung K., Kang K.S. Beneficial effects of Panax ginseng for the treatment and prevention of neurodegenerative diseases: past findings and future directions. J Ginseng Res. 2018;42:239–247. doi: 10.1016/j.jgr.2017.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhuo X.H., Sun H.C., Wang S.H., Guo X.L., Ding H.J., Yang Y., Shan Y., Du A.F. Ginseng stem-and-leaf saponin (GSLS)-enhanced protective immune responses induced by Toxoplasma gondii heat shocked protein 70 (HSP70) against toxoplasmosis in mice. J Parasitol. 2017;103:111–117. doi: 10.1645/16-54. [DOI] [PubMed] [Google Scholar]
- 13.Qu D., Han J., Du A. Enhancement of protective immune response to recombinant Toxoplasma gondii ROP18 antigen by ginsenoside Re. Exp Parasitol. 2013;135:234–239. doi: 10.1016/j.exppara.2013.07.013. [DOI] [PubMed] [Google Scholar]
- 14.Luo W., Aosai F., Ueda M., Yamashita K., Shimizu K., Sekiya S., Yano A. Kinetics in parasite abundance in susceptible and resistant mice infected with an avirulent strain of Toxoplasma gondii by using quantitative competitive PCR. J Parasitol. 1997;83:1070–1074. [PubMed] [Google Scholar]
- 15.Sudan V., Tewari A.K., Singh H., Singh R. Pathobiology of human RH strain induced experimental toxoplasmosis in murine model. J Parasit Dis. 2016;40:840–844. doi: 10.1007/s12639-014-0589-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Powell H.C., Gibbs C.J., Jr., Lorenzo A.M., Lampert P.W., Gajdusek D.C. Toxoplasmosis of the central nervous system in the adult. Electron microscopic observations. Acta Neuropathol. 1978;41:211–216. doi: 10.1007/BF00690438. [DOI] [PubMed] [Google Scholar]
- 17.Carruthers V.B., Suzuki Y. Effects of Toxoplasma gondii infection on the brain. Schizophr Bull. 2007;33:745–751. doi: 10.1093/schbul/sbm008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.El Temsahy M.M., El Kerdany E.D., Eissa M.M., Shalaby T.I., Talaat I.M., Mogahed N.M. The effect of chitosan nanospheres on the immunogenicity of Toxoplasma lysate vaccine in mice. Parasit Dis. 2016;40:611–626. doi: 10.1007/s12639-014-0546-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dubey J.P. 2nd ed. CRC Press; Boca Raton: 2010. Toxoplasmosis of animals and humans. [Google Scholar]
- 20.Yuan Y., Rangarajan P., Kan E.M., Wu Y., Wu C., Ling E.A. Scutellarin regulates the Notch pathway and affects the migration and morphological transformation of activated microglia in experimentally induced cerebral ischemia in rats and in activated BV-2 microglia. J Neuroinflammation. 2015;12:11. doi: 10.1186/s12974-014-0226-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Henn A., Lund S., Hedtjärn M., Schrattenholz A., Pörzgen P., Leist M. The suitability of BV2 cells as alternative model system for primary microglia cultures or for animal experiments examining brain inflammation. ALTEX. 2009;26:83–94. doi: 10.14573/altex.2009.2.83. [DOI] [PubMed] [Google Scholar]
- 22.Mineo J.R., Kasper L.H. Attachment of Toxoplasma gondii to host cells involves major surface protein, SAG-1 (P30) Exp Parasitol. 1994;79:11–20. doi: 10.1006/expr.1994.1054. [DOI] [PubMed] [Google Scholar]
- 23.Moroda M., Takamoto M., Iwakura Y., Nakayama J., Aosai F. Interleukin-17A-deficient mice are highly susceptible to Toxoplasma gondii infection due to excessively induced T. gondii HSP70 and interferon gamma production. Infect Immun. 2017;85 doi: 10.1128/IAI.00399-17. e00399–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alomar M.L., Rasse-Suriani F.A., Ganuza A., Cóceres V.M., Cabrerizo F.M., Angel S.O. In vitro evaluation of β-carboline alkaloids as potential anti-Toxoplasma agents. BMC Res Notes. 2013;6:193. doi: 10.1186/1756-0500-6-193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Harker K.S., Ueno N., Lodoen M.B. Toxoplasma gondii dissemination: a parasite's journey through the infected host. Parasite Immunol. 2015;37:141–149. doi: 10.1111/pim.12163. [DOI] [PubMed] [Google Scholar]
- 26.Hwang Y.S., Shin J.H., Yang J.P., Jung B.K., Lee S.H., Shin E.H. Characteristics of infection immunity regulated by Toxoplasma gondii to maintain chronic infection in the brain. Front Immunol. 2018;9:158. doi: 10.3389/fimmu.2018.00158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dellacasa-Lindberg I., Fuks J.M., Arrighi R.B., Lambert H., Wallin R.P., Chambers B., Barragan A. Migratory activation of primary cortical microglia upon infection with Toxoplasma gondii. Infect Immun. 2011;79:3046–3052. doi: 10.1128/IAI.01042-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lian L.H., Jin Q., Song S.Z., Wu Y.L., Bai T., Jiang S., Li Q., Yang N., Nan J.X. Ginsenoside Rh2 downregulates LPS-induced NF-κB activation through inhibition of TAK1 phosphorylation in RAW 264.7 murine macrophage. Evid Based Complement Alternat Med. 2013;2013:646728. doi: 10.1155/2013/646728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Denkers E.Y. Toll-like receptor initiated host defense against Toxoplasma gondii. J Biomed Biotechnol. 2010;2010:737125. doi: 10.1155/2010/737125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhou Y.H., Wang S.S., Yang J., Tao J.P., Xu Y.L., Huang Y.Z., Gao Q. Expression of Toll-like receptor 4 in brain tissue of chronic Toxoplasma gondii infection rats and its effect on brain injury. Zhongguo Xue Xi Chong Bing Fang Zhi Za Zhi. 2012;24:58–61. [PubMed] [Google Scholar]
- 31.Zare-Bidaki M., Hakimi H., Abdollahi S.H., Zainodini N., Arababadi M.K., Kennedy D. TLR4 in Toxoplasmosis; friends or foe? Microb Pathog. 2014;69–70:28–32. doi: 10.1016/j.micpath.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 32.Aosai F., Chen M., Kang H.K., Mun H.S., Norose K., Piao L.X., Kobayashi M., Takeuchi O., Akira S., Yano A. Toxoplasma gondii-derived heat shock protein HSP70 functions as a B cell mitogen. Cell Stress Chaperones. 2002;7:357–364. doi: 10.1379/1466-1268(2002)007<0357:tgdhsp>2.0.co;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Makino M., Uemura N., Moroda M., Kikumura A., Piao L.X., Mohamed R.M., Aosai F. Innate immunity in DNA vaccine with Toxoplasma gondii-heat shock protein 70 gene that induces DC activation and Th1 polarization. Vaccine. 2011;29:1899–1905. doi: 10.1016/j.vaccine.2010.12.118. [DOI] [PubMed] [Google Scholar]
- 34.Fang H., Aosai F., Mun H.S., Norose K., Ahmed A.K., Furuya M., Yano A. Anaphylactic reaction induced by Toxoplasma gondii-derived heat shock protein 70. Int Immunol. 2006;18:1487–1497. doi: 10.1093/intimm/dxl081. [DOI] [PubMed] [Google Scholar]
- 35.Fang H., Mun H.S., Kikumura A., Sayama Y., Norose K., Yano A., Aosai F. Toxoplasma gondii-derived heat shock protein 70 induces lethal anaphylactic reaction through activation of cytosolic phospholipase A2 and platelet-activating factor via Toll-like receptor 4/myeloid differentiation factor 88. Microbiol Immunol. 2008;52:366–374. doi: 10.1111/j.1348-0421.2008.00047.x. [DOI] [PubMed] [Google Scholar]
- 36.Molestina R.E., Payne T.M., Coppens I., Sinai A.P. Activation of NF-kappaB by Toxoplasma gondii correlates with increased expression of antiapoptotic genes and localization of phosphorylated IkappaB to the parasitophorous vacuole membrane. J Cell Sci. 2003;116:4359–4371. doi: 10.1242/jcs.00683. [DOI] [PubMed] [Google Scholar]
- 37.Wang S., Zhang Z., Wang Y., Gadahi J.A., Xie Q., Xu L., Yan R., Song X., Li X. Toxoplasma gondii excretory/secretory antigens (TgESAs) suppress inflammatory cytokine secretion by inhibiting TLR-induced NF-κB activation in LPS-stimulated murine macrophages. Oncotarget. 2017;8:88351–88359. doi: 10.18632/oncotarget.19362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Guiton P.S., Sagawa J.M., Fritz H.M., Boothroyd J.C. An in vitro model of intestinal infection reveals a developmentally regulated transcriptome of Toxoplasma sporozoites and a NF-κB-like signature in infected host cells. PLoS One. 2017;12 doi: 10.1371/journal.pone.0173018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Glaser K.C., Hagos B., Molestina R.E. Effects of Toxoplasma gondii genotype and absence of host MAL/Myd88 on the temporal regulation of gene expression in infected microglia. Exp Parasitol. 2011;129:409–413. doi: 10.1016/j.exppara.2011.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kim L., Butcher B.A., Lee C.W., Uematsu S., Akira S., Denkers E.Y. Toxoplasma gondii genotype determines MyD88-dependent signaling in infected macrophages. J Immunol. 2006;177:2584–2591. doi: 10.4049/jimmunol.177.4.2584. [DOI] [PubMed] [Google Scholar]
- 41.Lee C.W., Sukhumavasi W., Denkers E.Y. Phosphoinositide-3-kinase-dependent, MyD88-independent induction of CC-type chemokines characterizes the macrophage response to Toxoplasma gondii strains with high virulence. Infect Immun. 2007;75:5788–5797. doi: 10.1128/IAI.00821-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dobbin C.A., Smith N.C., Johnson A.M. Heat shock protein 70 is a potential virulence factor in murine Toxoplasma infection via immunomodulation of host NF-κB and nitric oxide. J Immunol. 2002;169:958–965. doi: 10.4049/jimmunol.169.2.958. [DOI] [PubMed] [Google Scholar]
- 43.Mun H.S., Aosai F., Norose K., Piao L.X., Fang H., Akira S., Yano A. Toll-like receptor 4 mediates tolerance in macrophages stimulated with Toxoplasma gondii-derived heat shock protein 70. Infect Immun. 2005;73:4634–4642. doi: 10.1128/IAI.73.8.4634-4642.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]