Abstract
The ongoing outbreak of the coronavirus disease 2019 (COVID-19) has become an unprecedented threat to public health around the world. The crisis has also brought great challenges to the routine diagnosis and treatment of cancer patients, especially given the urgency and continuity of cancer care. Cancer patients need to be more prudently and individually managed to combat COVID-19. At present, the COVID-19 epidemic in some countries has moved from the outbreak phase to the remission phase. How to preserve high-quality anti-tumor therapy for cancer patients while maintaining strict prevention and control of COVID-19 is a matter of concern. Here, we summarized essential data about COVID-19 and cancer and provided the clinical recommendations for the management of cancer patients during the COVID-19 pandemic based on our practical experience and relevant literatures.
Keywords: COVID-19, cancer patients, clinical management
Introduction
The epidemic of the coronavirus disease 2019 (COVID-19), also known as SARS-CoV-2, has been declared to be a global pandemic by the World Health Organization (WHO). As an emerging infectious disease, it has spread to more than 210 countries since the first confirmed case was reported [1,2]. And as of 10 July, 2020, 12102328 cases and 551046 deaths of COVID-19 have been reported all over the world [3].
After about 4 months of efforts, the epidemic in China has entered the mitigation stage. Currently, the outpatient visits and hospitalization rates in most regions of China have been recovering gradually. At present, the screening and management of asymptomatic individuals has become the main direction in China.
However, as a dynamic and rapidly evolving process, the risk of COVID-19 re-infection should not be underestimated, especially for cancer patients and the corresponding management strategies should be constantly optimized and adjusted. Limited information has been available to describe the considerations for cancer patients requiring hospitalization during the COVID-19 pandemic. In this study, we reviewed essential literatures about COVID-19 and cancer and described how the cancer center of Renmin hospital of Wuhan University has taken measures to ensure the high-quality care for cancer patients while combating the infection of COVID-19, for which we hope our experiences can offer some suggestions to others globally in fight against the epidemic.
Characteristics and challenges of COVID-19
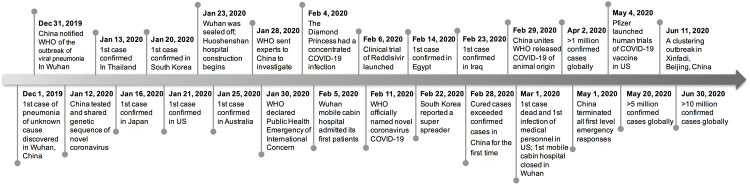
The ongoing expanding COVID-19 has caused a global public health crisis. Here, we summarized the timeline of key events of the COVID-19 from Dec 1, 2019 to Jun 30, 2020 in Figure 1. According to a series of epidemiological reports, the outbreak of COVID-19 began with animal-to-human transmission and followed by continuous spread from person to person [4]. Now, the person-to-person transmission has been confirmed mainly through respiratory droplets and close contact, and fecal-oral transmission has also been reported. The average incubation period for COVID-19 is 5 to 6 days, but can be as long as 14 days, which is the basis for medical observation and quarantine [5].
Figure 1.
Timeline showing key events in the COVID-19 epidemic (December 1, 2019 through June 30, 2020).
Most patients with COVID-19 developed only mild or moderate disease. Fever and cough are the most common clinical symptoms, while anorexia, shortness of breath, myalgias, sore throat, nasal congestion, headache, diarrhea, nausea, vomiting, fatigue, hearing loss and thyroid inflammation are other atypical symptoms that should not be overlooked [6-8]. Advanced age, hypertension, diabetes, heart disease, chronic lung disease and cancer have been reported to be closely associated with severe illness and death of COVID-19 [9]. Although the severity and mortality of COVID-19 is lower than that of Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS), it is the most contagious of the three. Both symptomatic and asymptomatic infected patients have been reported to be contagious [10,11]. People of all ages have no pre-existing immunity to it. Besides, there is so far no specific therapeutics and the promising vaccines are still in clinical trials.
RT-PCR (reverse transcriptase-polymerase chain reaction) serves as a gold standard to diagnose COVID-19. But a negative test does not guarantee against COVID-19 infection [12]. A recently study found that patients with COVID-19 had at least a one-fifth chance of a false negative result during the infection [13]. At last but not least, the mutation of the coronavirus also poses challenges to the spread and control of the epidemic. Two recent studies that have not yet been peer-reviewed come to almost identical conclusion that D614G variant has replaced the original strain from 2019 as the main strain [14,15]. That is just the type of virus mutation that caused the second small outbreak of COVID-19 in Beijing recently, according to the official nucleotide sequencing results. Therefore, the complete prevention and control of COVID-19 is still a long way off.
Cancer patients and COVID-19
Compared with the general population, cancer patients tend to be elderly, immunocompromised, and complicated with basic chronic illness. As susceptible populations, they are considered at theoretically higher risk for COVID-19 infection and severe events (ICUs admission, mechanical ventilation or death) [16]. An earlier study of the epidemiological and clinical characteristics of 72,314 COVID-19 cases in China showed a 5.6% case-fatality rate of COVID-19 in 107 (0.5%) cancer patients [11]. And the odds of COVID-19 progressing into severe illness was reported to be 3.6 times higher for patients with cancer than for those without cancer, a finding consistent with a recent large multicenter cohort study of 13,077 COVID-19 patients in Wuhan (64% vs 32%, OR: 3.61, 95% CI 2.59-5.04, P<0.0001) [17]. According to an Italian report, of the 355 patients who died of COVID-19 in Italy, 20% had a history of active cancer in the past five years [18]. Dai and He et al. further pointed out that cancer patients, especially those with hematological cancer, lung cancer, metastatic cancer (stage IV) or receiving antitumor therapy within 14 days (HR: 4.08, 95% CI 1.09-15.32, P=0.037) had higher risks in all severe outcomes [19,20].
Of the 1575 patients with COVID-19 from our hospital showed that 3.3% were cancer patients, and lung cancer was the most predominant type (19.2%) [21]. Among the 52 cancer patients with COVID-19, 36.5% were severe cases, and the mortality was up to 57.8%. Fever (25%), cough (17.3%) and chest distress (11.5%) were the most common clinical symptoms, while hypertension (51.5%) and diabetes (21.2%) were the most common comorbidities. Typical patchy or ground glass opacity and lymphocytosis were found in more than 75% cases.
Apart from the typical clinical features described above, the particularity and challenges of cancer patients in the era of COVID-19 should not be underestimated. Qu et al. reported a case of lung cancer patient with COVID-19 who developed atypical radiographic features with irregular, diffuse, small ground-glass opacity and partial consolidation on day 10 after infection [22]. Jin et al. reported a patient with hematologic malignancies whose diagnosis of COVID-19 was delayed due to high white blood counts [23]. Besides that, some cancer patients with another viral infection or pulmonary metastasis might be misdiagnosed or never diagnosed because of a false negative serological result. In addition, the frequent hospital visits for periodic reexamination tremendously increased the risk of exposure and cross-infection for cancer patients. Therefore, strengthen the infection control against COVID-19 and reduce the risk of disease progression due to treatment delay in cancer patients are becoming more essential than ever.
Management of COVID-19 in cancer patients
The COVID-19 pandemic has put cancer patients in a dilemma, mainly in terms of the conflict between the disruption or delay of anti-tumor treatment that can lead to disease progression and the risk of COVID-19 infection from risky hospital visits [24]. Is it necessary for cancer patients to risk exposure to COVID-19 for anti-tumor therapy in hospitals? Given the high infectivity of COVID-19, ensuring the safety of patients during the process of cancer care is the basic responsibility of all health care workers. At this particular period of absence of evidence-based cancer care, clinical decisions for each cancer patient often require an individualized assessment by a multidisciplinary team to weigh the risk of morbidity and death from COVID-19 against the expected benefits of cancer treatment [25].
Outpatient management
All cancer patients requiring hospitalization must undergo the first round of COVID-19 risk screening in the outpatient or emergency department, which includes collecting symptoms and signs of COVID-19, asking about history of close contact or exposure, temperature monitoring, chest CT scan, blood routine test, novel coronavirus nucleic acid test (usually nasopharyngeal and oropharyngeal swabs) and serologic test of IgM and IgG immunoglobulin. These requirements also apply to any accompanying person. The specific interpretation and coping strategies of different virological test results of novel coronavirus were presented in Table 1.
Table 1.
Interpretation of different virological test results of COVID-19 and coping strategies
| COVID-19 test results | Interpretation | Optimal treatment strategies |
|---|---|---|
| Nucleic acid test++, IgM+/-, IgG+/- | Confirmed infection | Transfer to a designated hospital |
| Nucleic acid test+, IgM+, IgG+/- | Confirmed infection | Transfer to a designated hospital |
| Nucleic acid test+, IgM-, IgG+/- | Suspected infection or re-positive | Isolation in buffer ward and recheck |
| IgM+, IgG-, Nucleic acid test- | New infection or re-positive | Isolation in buffer ward and recheck |
| IgG+, IgM-, Nucleic acid test- | Previous infection | Recheck and transfer to inpatient ward |
| IgM+, IgG+, Nucleic acid test- | Re-positive or new infection | Isolation in buffer ward and recheck |
| IgM-, IgG-, Nucleic acid test- | No infection | Transfer to impatient ward |
Note: The four-sites nucleic acid test of novel coronavirus mainly includes nasopharyngeal, oropharyngeal, sputum and anal swabs. The serological test includes IgM and IgG antibody. The plus sign indicates a positive result. For the four-sites nucleic acid test, one plus sign (+) represents positive result of one site, two plus signs (++) represent positive results of two or more sites, which are of diagnostic significance combined with the epidemiology and close contact history as well as clinical manifestations.
Fever clinics are specially set up to screen suspicious COVID-19 patients with fever and other typical symptoms. Patients with a history of close contact or have a sojourn history around epidemic foci should be placed in a single isolation unit as soon as possible. Suspected patients with mild to moderate clinical symptoms can be sent to the mobile cabin hospitals for further observation. Patients with only nucleic acid or antibody positive or suspected imaging of diffuse ground-glass or consolidative opacities should continue observation and reexamination, while those confirmed with COVID-19 infection or re-positive should be reported immediately and sent to designated hospitals for isolation and treatment. Beyond that, asymptomatic patients with no abnormal screening results will be transferred to the buffer wards.
For cancer patients requiring continuous intravenous chemotherapy in outpatient settings, oral or subcutaneous therapy may be recommended to reduce the risk of exposure [26]. For example, xeloda or S-1 may be used as an alternative to fluorouracil in maintenance therapy for gastrointestinal tumors. Apatinib and anlotinib are also widely recommended for home care of advanced tumors. There is no evidence to support the use of colony stimulating factors or interleukins to prevent bone marrow suppression during the epidemic. Efficacy evaluation, side effects surveillance and follow-up in outpatient settings should be postponed or minimized and remote online guidance is encouraged, if possible.
Several measures may help reduce nosocomial cross-infection in outpatient settings. Set up special entrance and exit and eye-catching signage with full-time staff to guard. Make an appointment in advance and visit the doctor at the appointed time to avoid long in-hospital waiting. Avoid walking around and touching public goods in the hospital. Avoid or reduce visitation, and if escorts are needed, designate a person. Standard precautions, including hand hygiene (e.g., keep alcohol-based hand sanitizers on hand and use them immediately after touching public door handles) and the use of personal protective equipment and corresponding measures (e.g., wear masks correctly at all times, avoid waiting lists and keep a safe distance of 1.5 meters away from other patients) should be reiterated [27].
Buffer wards management
Buffer wards were established primarily for the second round of risk screening before asymptomatic patient who had been checked out of the outpatient clinic were then diverted to inpatient wards. These wards were reconstructed according to the model of three zones and two channels, namely medical personnel channel and patient channel, clean zone, potential contaminated zone and contaminated zone (Figure 2).
Figure 2.
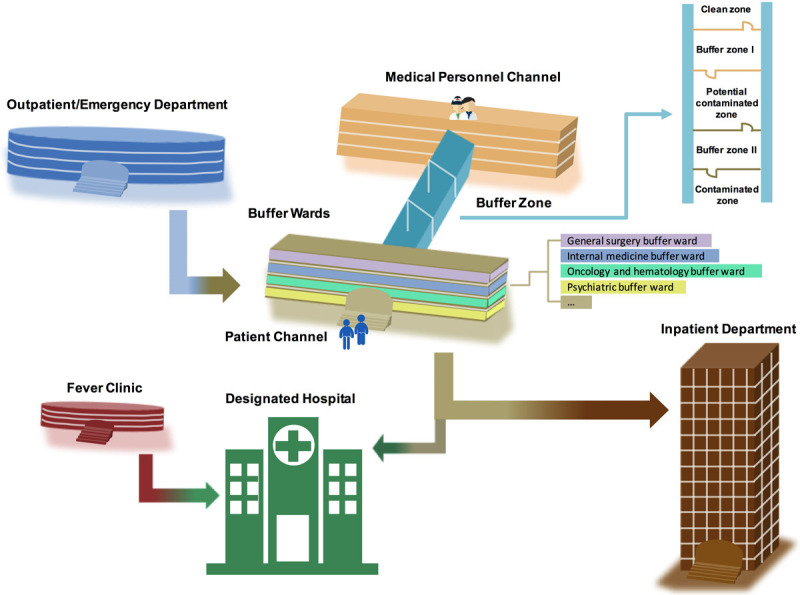
The three-stage admission process for patients requiring hospitalization during the COVID-19 epidemic (Outpatient/Emergency Department-Buffer Wards-Inpatient Department) and the structure installation and subspecialty division of the buffer wards. The buffer system of the buffer wards consists of three zones and two channels, specifically including the medical personnel channel and patient channel, clean zone (office and rest areas for medical personnel), potential contaminated zone and contaminated zone (buffer wards), respectively.
Patients temporarily admitted to the buffer wards should be retested for blood routine, nucleic acid test of nasopharyngeal, oropharyngeal, sputum and anal swabs and serological test of IgM and IgG antibody to exclude COVID-19 infection. Other specialized examinations, such as electrocardiogram (ECG), brain CT scan, myocardial infarction index (cardiac troponin I, cTnI), heart failure index (B-type natriuretic peptide, BNP), biochemical indexes, etc., may also be performed during this transitional period if necessary. All buffer wards are under closed-end management, patients and caregivers are checked in sequence and are not allowed to go in and out at will to reduce cross-infection. A standard 6-occupant ward can only accommodate a maximum of two patients and those previously infected with COVID-19 must be admitted to a separate ward for rigorous medical observation.
Due to the temporary nature of the buffer wards, many specialized drugs and equipment may be inadequate. In order to satisfy the treatment of patients with different needs and improve the efficiency of management, we classified the buffer wards into subspecialties according to the actual situation of the disease admitted. It was mainly divided into 1) comprehensive surgical buffer ward consisting of orthopedics, hepatobiliary and pancreatic surgery, urology, organ transplantation, thoracic and cardiac surgery, head and neck surgery, 2) comprehensive internal medicine buffer ward consisting of cardiology, neurology, respiratory medicine, nephrology, endocrinology and interventional medicine, 3) buffer ward for breast and thyroid and reproductive system diseases, 4) gastrointestinal bleeding related buffer ward, 5) oncology and hematology buffer ward, 6) ophthalmic buffer ward and 7) psychiatric buffer ward. For other specialized emergencies requiring urgent treatment, the physician on duty in the buffer wards may contact a specialist for consultation. In oncology buffer ward, periodic oral chemotherapy, intravenous targeted therapy or immunotherapy may be resumed as appropriate for some eligible patients after assessment by the oncologists.
Public health emergencies usually trigger insurmountable psychological pressure, such as panic disorder, anxiety, depression, insomnia and fear in the general population [28,29]. We observed that most of patients who were eager to receive anti-tumor treatment became more and more anxious in the buffer wards during the waiting process. Psychological crisis intervention, including telephone counseling helplines and online mental health services, became extremely important at that time [30].
Once a confirmed case was found, the patient would be immediately reported and transferred to a designated hospital, while the close contacts would be screened and isolated in a separate ward for another 14-day quarantine. Patients with repeatable negative coronavirus tests may be further transfer to the inpatient department. With the mitigation of the epidemic, most of the buffered wards have now been restored to inpatient wards after thorough sterilization, some buffer wards were still reserved for patients whose screening results were questionable and those who needed urgent treatment but could not wait for screening results.
Inpatient management
Most of the cancer patients that do require hospitalization are usually due to uncontrolled disease progression or complications such as hemoptysis, gastrointestinal bleeding, ileus, and massive pleural or peritoneal effusion [31,32]. For these critically ill patients, symptomatic treatment should be given in emergency department first, and then transferred to the inpatient ward for further therapy after excluding COVID-19 infection in the buffer ward.
It is necessary for cancer patients transferred from the buffer ward to the inpatient ward for another 48 hours of isolation. At least one separate isolation unit should be reserved at the end of each inpatient ward. Temperature monitoring is also a basic requirement in the wards. If a new suspected case appeared during the antitumor treatment, the patient must be transferred to the separate isolation unit for further medical observation. However, once a confirmed case was found, the patient would be immediately reported and transferred to a designated hospital and all the close contacts should receive rigorous medical observation for 14 days and be tested for possible infection. Combined with the actual situation of our hospital, two rounds of intensive risk screening in outpatient and buffer wards ensured that no confirmed COVID-19 cases were detected in our inpatient department. This is just the significance of the establishment of buffer wards.
As for the medical management and therapeutic decision making, a cancer multidisciplinary team consisting of a group of experts will be established through the online platform to conduct individualized analysis and medication guide for each patient [33,34]. The basic principles for management of cancer patients under the COVID-19 epidemic were presented in Table 2. Cancer patients with stable disease (ie without tumor progression or severe complications) were recommended for intravenous administration-free alternatives-oral chemotherapy or targeted drugs at home, which do not require hospitalization. Maintaining chemotherapy and brain irradiation was suggested for metastatic patients. Neoadjuvant chemotherapy with decreased intensity and frequency was recommended to patients who have a locally advanced tumor. For patients scheduled for elective operation, postpone surgery or replace it with interventional or radiation therapy whenever possible until the crisis abates [35,36].
Table 2.
Principles for management of cancer patients with different disease states under the COVID-19 epidemic
| Best alternatives | Indications |
|---|---|
| Chemotherapy | SD: oral chemotherapeutic or targeted drugs at home or temporary break or reduction in the frequency of intravenous maintenance therapy |
| PD: maintain chemotherapy (reduce dose and frequency of administration) | |
| Radiotherapy | SD: temporary break or reduction in the frequency of radiotherapy |
| PD: brain, bone or other metastases irradiation; hypo-fractionated radiotherapy | |
| Urgent palliative radiotherapy: spinal cord compression | |
| Surgery | Elective surgery: postpone surgery or replace it with interventional or preoperative radiation therapy or neoadjuvant chemotherapy |
| Urgent surgery: life-threatening conditions (obstruction, bleeding, perforation...) | |
| Targeted therapy | Oral or intravenous targeted therapy (reduce dose and frequency of administration) |
| Immunotherapy | Conduct online MDT consultations remotely, if possible |
| Periodic intravenous immunotherapy may be resumed as appropriate for some eligible patients after assessment by the MDT |
Note: SD: stable disease; PD: progressive of disease; MDT: multidisciplinary team.
Preoperative radiotherapy has been reported to create conditions and buy the time for delayed surgery. Hypofractionated radiotherapy regimens were more recommended during the epidemic. Considering the closed and public nature of the radiotherapy room and the novel coronavirus activity can last for 72 hours, the implementation of radiotherapy should be cautious [37,38]. The American Society for Radiation Oncology (ASTRO) and Chinese scholars both have recently published practical guidelines on radiotherapy related to COVID-19 [39,40]. Anticancer therapy can lead to systemic immunosuppressive state in cancer patients [24]. So, it is important to note that cancer patients who are actively receiving anticancer therapy are still at high risk of COVID-19 infection and oncologists should always be vigilant during the whole clinical process.
Current status of our hospital and community
At the beginning of the COVID-19 outbreak, a headquarters was immediately established in our hospital to strictly plan and deploy all procedures for the epidemic prevention and control. Affected by the epidemic, the outpatient visits in our hospital in May was only one third that of the same period last year, and the number of inpatients and surgeries was also significantly reduced.
Now, as the epidemic enters a stage of remission, the medical services at our hospital began to gradually return to normal. The eastern branch of our hospital, as a designated hospital for COVID-19 treatment, also fully resumed normal medical services on May 16 after 15 days of complete sterilization. From now on, all patients and their companions can enter the hospital with their health code green, and those who need to be admitted can make an appointment online.
As of 26 April, 2020, Wuhan has achieved zero growth of confirmed and suspected COVID-19 cases for the first time. As the epicenter of the outbreak, Wuhan actively responded to the call for strict prevention and control and performed COVID-19 nucleic acid test for nearly 10 million citizens from May 14 to June 1, 2020. A total of 300 asymptomatic infected individuals were detected, 1,174 close contacts were tracked, and no one was confirmed infection. Currently, all regions of Wuhan City have been declared as low-risk areas.
Besides, from 13 June, the Wuhan Disease Control and Prevention Center tested 34,450 environmental samples from 364 supermarkets, 678 farmer’s markets, 5 aquatic products trading companies and 37 public toilets for consecutive 13 days, all of which were COVID-19 negative. This information means that the transmission of COVID-19 in Wuhan has almost been completely interrupted. At present, each community has no longer adopt closed-off management, residents can scan the two-dimensional code through Alipay or WeChat platform to freely enter and exit their communities, while the temperature monitoring is still mandatory in the entrance.
Discussion
The COVID-19 outbreak posed a great challenge for cancer treatment and patient survival. Given its highly infective nature, adequate prevention is the top priority in the fight against the epidemic. In this review, we addressed some of the current challenges associated with managing cancer patients and provided some recommendations for cancer patients requiring hospitalization in the era of COVID-19 based on our practical experience and relevant literatures. The accumulating evidence suggests that cancer patients are at higher risk of COVID-19 infection and severe events than individuals without cancer. In this scenario, oncologists need to weigh up the balance of risks versus benefits carefully in therapeutic decision making. Consideration of active intervention for cancer patients during the COVID-19 epidemic should be individualized and phased. Minimizing outpatient visits and elective operations during the epidemic outbreak, while encourage admission to hospital and resumption active antitumor treatment under the premise of full self-protection in the epidemic remission stage. Psychological intervention is an evitable issue for all cancer patients, and hand hygiene, self-protection and telemedicine should be highlighted in the prevention and control of COVID-19 and any other infectious diseases in the future.
Although the asymptomatic patients did not play a role in amplifying the spread of the epidemic, close monitoring of them remains a priority. Buffer wards were set up to effectively screen asymptomatic infected patients and those in the incubation period, thus achieving the classification management of patients with different novel coronavirus test results. For cancer patients under different protective conditions, the buffer wards effectively cut off the transmission of the virus and resumed the anti-tumor treatment in a timely and appropriate manner. It has been confirmed that none of the patients admitted to the buffer wards in our hospital were infected with novel coronavirus due to such reasons as close contact. The management model of buffer ward in our hospital is a representative example. At the remission stage of COVID-19 in China, the whole society began to resume work and production. Buffer wards have been adopted in all hospitals in Wuhan, which not only ensured the orderly recovery of anti-tumor treatment, but also strictly limited the source of infection, cut off the route of transmission and effectively blocked the spread of COVID-19.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (No. U1604175), Fundamental Research Funds for the Central Universities of China (2042020kf0110) and National Key R&D Program of China (2018YFC1311300).
Disclosure of conflict of interest
None.
References
- 1.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W China Novel Coronavirus Investigating and Research Team. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW The Northwell COVID-19 Research Consortium. Barnaby DP, Becker LB, Chelico JD, Cohen SL, Cookingham J, Coppa K, Diefenbach MA, Dominello AJ, Duer-Hefele J, Falzon L, Gitlin J, Hajizadeh N, Harvin TG, Hirschwerk DA, Kim EJ, Kozel ZM, Marrast LM, Mogavero JN, Osorio GA, Qiu M, Zanos TP. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323:2052–9. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Coronavirus Disease 2019 (COVID-19) Situation Report-172. 2020
- 4.Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Ren R, Leung KSM, Lau EHY, Wong JY, Xing X, Xiang N, Wu Y, Li C, Chen Q, Li D, Liu T, Zhao J, Liu M, Tu W, Chen C, Jin L, Yang R, Wang Q, Zhou S, Wang R, Liu H, Luo Y, Liu Y, Shao G, Li H, Tao Z, Yang Y, Deng Z, Liu B, Ma Z, Zhang Y, Shi G, Lam TTY, Wu JT, Gao GF, Cowling BJ, Yang B, Leung GM, Feng Z. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS China Medical Treatment Expert Group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang L, Zhu F, Xie L, Wang C, Wang J, Chen R, Jia P, Guan HQ, Peng L, Chen Y, Peng P, Zhang P, Chu Q, Shen Q, Wang Y, Xu SY, Zhao JP, Zhou M. Clinical characteristics of COVID-19-infected cancer patients: a retrospective case study in three hospitals within Wuhan, China. Ann Oncol. 2020;31:894–901. doi: 10.1016/j.annonc.2020.03.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sriwijitalai W, Wiwanitkit V. Hearing loss and COVID-19: a note. Am J Otolaryngol. 2020;41:102473. doi: 10.1016/j.amjoto.2020.102473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brancatella A, Ricci D, Viola N, Sgro D, Santini F, Latrofa F. Subacute thyroiditis after Sars-COV-2 infection. J Clin Endocrinol Metab. 2020;105:dgaa276. doi: 10.1210/clinem/dgaa276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Imam Z, Odish F, Gill I, O’Connor D, Armstrong J, Vanood A, Ibironke O, Hanna A, Ranski A, Halalau A. Older age and comorbidity are independent mortality predictors in a large cohort of 1305 COVID-19 patients in Michigan, United States. J Intern Med. 2020 doi: 10.1111/joim.13119. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zou L, Ruan F, Huang M, Liang L, Huang H, Hong Z, Yu J, Kang M, Song Y, Xia J, Guo Q, Song T, He J, Yen HL, Peiris M, Wu J. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 12.Woloshin S, Patel N, Kesselheim AS. False negative tests for SARS-CoV-2 infection - challenges and implications. N Engl J Med. 2020;383:e38. doi: 10.1056/NEJMp2015897. [DOI] [PubMed] [Google Scholar]
- 13.Kucirka LM, Lauer SA, Laeyendecker O, Boon D, Lessler J. Variation in false-negative rate of reverse transcriptase polymerase chain reaction-based SARS-CoV-2 tests by time since exposure. Ann Intern Med. 2020:M20–1495. doi: 10.7326/M20-1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang L, Jackson CB, Mou H, Ojha A, Rangarajan ES, Izard T, Farzan M, Choe H. The D614G mutation in the SARS-CoV-2 spike protein reduces S1 shedding and increases infectivity. bioRxiv. 2020 [Google Scholar]
- 15.Daniloski Z, Guo X, Sanjana NE. The D614G mutation in SARS-CoV-2 Spike increases transduction of multiple human cell types. bioRxiv. 2020 doi: 10.7554/eLife.65365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xia Y, Jin R, Zhao J, Li W, Shen H. Risk of COVID-19 for patients with cancer. Lancet Oncol. 2020;21:e180. doi: 10.1016/S1470-2045(20)30150-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tian J, Yuan X, Xiao J, Zhong Q, Yang C, Liu B, Cai Y, Lu Z, Wang J, Wang Y, Liu S, Cheng B, Wang J, Zhang M, Wang L, Niu S, Yao Z, Deng X, Zhou F, Wei W, Li Q, Chen X, Chen W, Yang Q, Wu S, Fan J, Shu B, Hu Z, Wang S, Yang XP, Liu W, Miao X, Wang Z. Clinical characteristics and risk factors associated with COVID-19 disease severity in patients with cancer in Wuhan, China: a multicentre, retrospective, cohort study. Lancet Oncol. 2020;21:893–903. doi: 10.1016/S1470-2045(20)30309-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020 doi: 10.1001/jama.2020.4683. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 19.Dai M, Liu D, Liu M, Zhou F, Li G, Chen Z, Zhang Z, You H, Wu M, Zheng Q, Xiong Y, Xiong H, Wang C, Chen C, Xiong F, Zhang Y, Peng Y, Ge S, Zhen B, Yu T, Wang L, Wang H, Liu Y, Chen Y, Mei J, Gao X, Li Z, Gan L, He C, Li Z, Shi Y, Qi Y, Yang J, Tenen DG, Chai L, Mucci LA, Santillana M, Cai H. Patients with cancer appear more vulnerable to SARS-CoV-2: a multicenter study during the COVID-19 outbreak. Cancer Discov. 2020;10:783–791. doi: 10.1158/2159-8290.CD-20-0422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.He W, Chen L, Chen L, Yuan G, Fang Y, Chen W, Wu D, Liang B, Lu X, Ma Y, Li L, Wang H, Chen Z, Li Q, Gale RP. COVID-19 in persons with haematological cancers. Leukemia. 2020;34:1637–1645. doi: 10.1038/s41375-020-0836-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yang F, Shi S, Zhu J, Shi J, Dai K, Chen X. Clinical characteristics and outcomes of cancer patients with COVID-19. J Med Virol. 2020 doi: 10.1002/jmv.25972. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 22.Qu J, Yang R, Song L, Kamel IR. Atypical lung feature on chest CT in a lung adenocarcinoma cancer patient infected with COVID-19. Ann Oncol. 2020;31:825–826. doi: 10.1016/j.annonc.2020.03.001. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jin XH, Zheng KI, Pan KH, Xie YP, Zheng MH. COVID-19 in a patient with chronic lymphocytic leukaemia. Lancet Haematol. 2020;7:e351–e352. doi: 10.1016/S2352-3026(20)30074-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kutikov A, Weinberg DS, Edelman MJ, Horwitz EM, Uzzo RG, Fisher RI. A war on two fronts: cancer care in the time of COVID-19. Ann Intern Med. 2020;172:756–758. doi: 10.7326/M20-1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van de Haar J, Hoes LR, Coles CE, Seamon K, Frohling S, Jager D, Valenza F, de Braud F, De Petris L, Bergh J, Ernberg I, Besse B, Barlesi F, Garralda E, Piris-Gimenez A, Baumann M, Apolone G, Soria JC, Tabernero J, Caldas C, Voest EE. Caring for patients with cancer in the COVID-19 era. Nat Med. 2020;26:665–671. doi: 10.1038/s41591-020-0874-8. [DOI] [PubMed] [Google Scholar]
- 26.Al-Shamsi HO, Alhazzani W, Alhuraiji A, Coomes EA, Chemaly RF, Almuhanna M, Wolff RA, Ibrahim NK, Chua MLK, Hotte SJ, Meyers BM, Elfiki T, Curigliano G, Eng C, Grothey A, Xie C. A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (COVID-19) pandemic: an international collaborative group. Oncologist. 2020;25:e936–e945. doi: 10.1634/theoncologist.2020-0213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cavanagh G, Wambier CG. Rational hand hygiene during the coronavirus 2019 (COVID-19) pandemic. J Am Acad Dermatol. 2020;82:e211. doi: 10.1016/j.jaad.2020.03.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020;33:e100213. doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu X, Luo WT, Li Y, Li CN, Hong ZS, Chen HL, Xiao F, Xia JY. Psychological status and behavior changes of the public during the COVID-19 epidemic in China. Infect Dis Poverty. 2020;9:58. doi: 10.1186/s40249-020-00678-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Duan L, Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry. 2020;7:300–302. doi: 10.1016/S2215-0366(20)30073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.De Simone B, Chouillard E, Di Saverio S, Pagani L, Sartelli M, Biffl WL, Coccolini F, Pieri A, Khan M, Borzellino G, Campanile FC, Ansaloni L, Catena F. Emergency surgery during the COVID-19 pandemic: what you need to know for practice. Ann R Coll Surg Engl. 2020;102:323–332. doi: 10.1308/rcsann.2020.0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Numico G, Cristofano A, Mozzicafreddo A, Cursio OE, Franco P, Courthod G, Trogu A, Malossi A, Cucchi M, Sirotova Z, Alvaro MR, Stella A, Grasso F, Spinazze S, Silvestris N. Hospital admission of cancer patients: avoidable practice or necessary care? PLoS One. 2015;10:e0120827. doi: 10.1371/journal.pone.0120827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Burki TK. Cancer guidelines during the COVID-19 pandemic. Lancet Oncol. 2020;21:629–630. doi: 10.1016/S1470-2045(20)30217-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hanna TP, Evans GA, Booth CM. Cancer, COVID-19 and the precautionary principle: prioritizing treatment during a global pandemic. Nat Rev Clin Oncol. 2020;17:268–270. doi: 10.1038/s41571-020-0362-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Al-Balas M, Al-Balas HI, Al-Balas H. Surgery during the COVID-19 pandemic: a comprehensive overview and perioperative care. Am J Surg. 2020;219:903–906. doi: 10.1016/j.amjsurg.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Diaz A, Sarac BA, Schoenbrunner AR, Janis JE, Pawlik TM. Elective surgery in the time of COVID-19. Am J Surg. 2020;219:900–902. doi: 10.1016/j.amjsurg.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sriwijitalai W, Wiwanitkit V. COVID-19, radiotherapy and cancer. Radiother Oncol. 2020;149:48. doi: 10.1016/j.radonc.2020.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, Tamin A, Harcourt JL, Thornburg NJ, Gerber SI, Lloyd-Smith JO, de Wit E, Munster VJ. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Guckenberger M, Belka C, Bezjak A, Bradley J, Daly ME, DeRuysscher D, Dziadziuszko R, Faivre-Finn C, Flentje M, Gore E, Higgins KA, Iyengar P, Kavanagh BD, Kumar S, Le Pechoux C, Lievens Y, Lindberg K, McDonald F, Ramella S, Rengan R, Ricardi U, Rimner A, Rodrigues GB, Schild SE, Senan S, Simone C, Slotman BJ, Stuschke M, Videtic G, Widder J, Yom SS, Palma D. Practice recommendations for lung cancer radiotherapy during the COVID-19 pandemic: an ESTRO-ASTRO consensus statement. Radiother Oncol. 2020;146:223–229. doi: 10.1016/j.radonc.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wei W, Zheng D, Lei Y, Wu S, Verma V, Liu Y, Wei X, Bi J, Hu D, Han G. Radiotherapy workflow and protection procedures during the Coronavirus Disease 2019 (COVID-19) outbreak: experience of the Hubei Cancer Hospital in Wuhan, China. Radiother Oncol. 2020;148:203–210. doi: 10.1016/j.radonc.2020.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]