Abstract
Gastric cancer is one of the leading causes of cancer-associated death; however, analysis of its molecular and clinical characteristics has been complicated by its histological and etiological heterogeneity. The present study aimed to estimate somatic mutation profiling in gastric cancer. To do so, targeted next-generation sequencing (NGS) was performed with the Oncomine Focus Assay to compare the clinicopathological characteristics with the mutation profiles in 50 patients with advanced gastric cancer (AGC). Among the 35 hotspot genes and 19 genes for copy number variations (CNVs), 18 single nucleotide variants (SNVs) or small insertions and deletions (14 missense and four frameshift mutations), and 10 amplifications were identified. To examine the association between mutation profiles and clinicopathological characteristics, each element of the clinicopathological characteristics was categorized into three groups: No alteration, PI3K catalytic subunit α (PIK3CA) alterations and alterations other than PIK3CA. Fisher's exact test identified no statistical differences between the clinicopathological characteristics, with the exception of the Tumor-Node-Metastasis (TNM) T stage between the three groups. Cases of AGC with somatic alterations but no PIK3CA exhibited a significant difference in the TNM T stage compared with those with no alterations or PIK3CA alterations (P=0.044). In addition, AGC with PIK3CA alterations was categorized by Lauren's classification to the intestinal type only. The distribution of Lauren's classification in AGC with PIK3CA alterations was statistically different compared with AGC with alterations other than PIK3CA (P=0.028), but not compared with AGC with no alterations (P=0.076). In conclusion, the present study demonstrated a molecular profiling approach that identified potential molecular classifications for gastric cancer and suggested a framework for precision medicine in AGC.
Keywords: next-generation sequencing, somatic alterations, mutation profile, PIK3CA, Oncomine focus assay, advanced gastric cancer
Introduction
Gastric cancer is a major cause of cancer-associated mortality. It ranks as the 5th most common neoplasm and the 3rd most deadly cancer, and was responsible for >1,000,000 new cases with an estimated 783,000 deaths in 2018 (1). However, analysis of the clinical and genetic characteristics of gastric cancer has been complicated by its etiological and histological heterogeneity (2). Etiologically, gastric cancer is often accompanied by infectious agents such as Helicobacter pylori or Epstein-Barr virus, susceptible genetic variants and environmental factors, along with the accumulation of epigenetic and genetic changes (3). Histopathological classification systems such as the Lauren's classification and World Health Organization classification system (4) have limited clinical usefulness as to which classifications unify a clinical correlation with a high validity and practicability in diagnosis and prognostic outcome, making the development of relevant classifiers that can help patient care an urgent priority (5). Thus, molecular classification of gastric cancer has been developed, and candidate drivers and dysregulated pathways of notable subtypes of gastric cancer have been identified (6). Several molecular targeted therapies associated with survival outcomes in other cancer types are currently in clinical research for the treatment of gastric cancer, including the inhibitors of epidermal growth factor receptor (EGFR), fibroblast growth factor receptor (FGFR), Met proto-oncogene receptor tyrosine kinase (MET), phosphatidylinositol-4,5-bisphosphate 3-kinase (PI3K) and vascular endothelial growth factor (VEGF) (7).
The application of next-generation sequencing (NGS) technologies exploiting whole genome sequencing to targeted sequencing has served an important role in the identification of genetic variations and anomalies in patients with gastric cancer, which has improved our understanding of the molecular profiles and heterogeneity of gastric cancers (1,2). Targeted NGS represents a resource- and cost-efficient approach, enabling the detection of somatic alterations of potential interest. The Oncomine Focus Assay (OFA) is a targeted NGS assay for the simultaneous and rapid identification of single nucleotide variants (SNVs), short insertions and deletions (indels; 35 genes), copy number variations (CNVs; 19 genes) and gene rearrangements (23 genes) in 52 cancer genes with therapeutic relevance, and can detect potential targets and current actionable genetic variants for personalized medicine (8). The OFA is designed for use with the Ion Torrent Personal Genome Machine (PGM™) that generates 10–100 Mb pairs (Mbp) of sequence data on various chips within several hours of instrument run time and leverages the uniquely minimal total of DNA or RNA input (10 ng), which is useful for frequent analysis of small amounts of clinical samples (9). Combined with Ion AmpliSeq technology, this approach enables highly accurate and reproducible sequence analysis of various types of tumor specimens (10).
The present study aimed to compare the clinicopathological characteristics with the mutation profiles of 50 Korean patients with advanced gastric cancer (AGC) by targeted NGS assay along with the OFA panel.
Materials and methods
DNA isolation and quantification
The study protocol was approved by the Institutional Review Board of The Catholic University of Korea (approval no. DC18SESI0113). All subjects provided written informed consent for clinical and molecular analyses and publication before the study. A total of 50 patients with AGC who received surgical resection between January 2015 and February 2019 at the Department of Surgery, Chungnam National University Hospital (Daejeon, Republic of Korea) were enrolled in the present study. The cohort comprised of 72% (36/50) male and 28% (14/50) female Korean patients with a mean age of 66 years (age range, 39–91 years). Genomic DNA was isolated from 50 frozen human AGC tissues using the RecoverAll Total Nucleic Acid Isolation kit (Thermo Fisher Scientific, Inc.) according to the manufacturer's instructions. Amplifiable genomic DNA was determined by fluorometric quantitation using Qubit 2.0 Fluorometer with Qubit dsDNA HS Assay kits and the TaqMan RNase P Detection Reagents kit (Thermo Fisher Scientific, Inc.) according to the manufacturer's protocols and was considered appropriate when the nucleic acid concentration was >30 ng/µl.
Library preparation
DNA libraries were constructed using the Ion AmpliSeq™ Library kit 2.0 (Thermo Fisher Scientific, Inc.) according to the manufacturer's instructions. The Oncomine Focus DNA Assay (Thermo Fisher Scientific, Inc.) was used to generate sequencing libraries from 10 ng input genomic DNA per specimen. The OFA panel can identify hotspot mutations, including SNVs, indels (35 genes) and CNVs (19 genes) that are commonly implicated in human cancers and relevant to targeted treatment of solid tumors (9). Unique Ion Xpress Barcode 1–16 and Ion P1 Adapter (Thermo Fisher Scientific, Inc.) were ligated to the amplicons and subsequently purified to ensure that each individual sample had a unique ID. The final amplicon libraries were amplified, purified and equalized to ~100 pM using an AMPure XP Reagent (Beckman Coulter, Inc.).
Semiconductor sequencing
A total of six uniquely barcoded library samples were pooled for sequencing per run on an Ion 318™ v2 chip (Thermo Fisher Scientific, Inc.). The Ion Chef™ System (Thermo Fisher Scientific, Inc.) was applied using the Ion PGM™ Hi-Q™ Chef Kit for fully automated template preparation and Ion 318™ v2 chip loading. Single-end sequence analysis was performed using the Ion PGM™ Hi-Q™ Sequencing Kit on the Ion Torrent PGM™ (Thermo Fisher Scientific, Inc.) for 200 base-read sequencing.
Variant calling and data analysis
Raw data from the DNA panel was generated for sequence reads, collected, processed and trimmed using the Ion Torrent platform-specific pipeline software as follows. Removal of polyclonal and poor signal profile reads as well as 3′ quality trimming of reads was performed using Torrent Suite Assay Development Mode v5.0 (Thermo Fisher Scientific, Inc.). Reads were aligned to the human genome hg19 (https://www.ncbi.nlm.nih.gov/assembly/GCF_000001405.13/) and Ion Reporter v5.1 software package (Thermo Fisher Scientific, Inc.) was used for data analysis of the DNA panel. A cut off of 500× coverage was applied to all analyses in the present study; the target regions with >500× demonstrated sufficient and uniform amplification and sequencing coverage, with mutant alleles detected at >5% allele frequency. Briefly, the ‘Oncomine Focus-520-w2.4-DNA-Single Sample’ automatic workflow in Ion Reporter was used to identify and annotate the SNVs, indels and CNVs from the OFA with the following Torrent Variant Caller parameter settings: Frequency cutoff for supporting a variant, SNV 0.04, indel 0.07, Hotspot 0.03; total coverage required of reads or no-call, SNV 15, indel 15, Hotspot 15; proportion of variant alleles coming overwhelmingly from one strand, SNV 0.96, indel 0.9, Hotspot 0.96 for SNV and indel calls; and median of the absolute values of all pairwise differences <0.4; 5% confidence interval CNV ploidy ≥ gain of 2 over normal for CNV calling.
Candidate variant prioritization
Pathogenic impact of missense mutations other than hotspot mutations on gene function was estimated using in silico prediction tools such as ‘Damaging’ (score 0) by SIFT (11) and ‘Probably damaging’ (score >0.8) by Polyphen-2 (12). Conservation change of an affected amino acid was compared by aligning protein sequences of various vertebrate species obtained from the Evolutionary Annotation Database (http://www.h-invitational.jp/evola/). In addition, the candidate mutation was investigated whether it has been reported as pathogenic for gastric cancer in the sequence databases including COSMIC (https://cancer.sanger.ac.uk/cosmic) (13) or ClinVar (https://www.ncbi.nlm.nih.gov/clinvar/).
Immunohistochemistry (IHC) for CDK4, EGFR, ERBB2, FGFR2, KRAS, MET, MYC and PIK3CA
A total of 10 tissue samples with the gene amplification identified by the OFA assay were fixed in buffered 10% formalin at 65°C for 10 min and embedded in paraffin. Formalin-fixed, paraffin-embedded (FFPE) samples were sectioned at a thickness of 4 µm. The BenchMark XT automated slide processing system (Ventana Medical Systems, Inc.) was used for deparaffinization pretreatment with Cell Conditioning 1 solution (Ventana) and ultraviolet irradiation to abrogate endogenous hydroperoxidase activity according to the manufacturer's instructions. These sections were incubated at 37°C for 24 min with primary antibodies (1:100; Abcam) against CDK4 (cat. no. ab108357), EGFR (cat. no. ab52894), ERBB2 (cat. no. ab16662), FGFR2 (cat. no. ab58201), KRAS (cat. no. ab180772), MET (cat. no. ab216574), MYC (cat. no. ab32072), PIK3CA (cat. no. ab40776). Sections, were then incubated with horseradish peroxidase-conjugated goat anti-rabbit IgG heavy & light chain secondary antibody (Abcam) at 37°C for 10 min. Sections were counterstained with hematoxylin II (Ventana) for 5 min and bluing reagent (Ventana) for 5 min at 37°C. Slides were imaged under a light microscope (BX51; Olympus Corporation). The intensity of immunostaining for protein expression was scored as follows: 0, negative; 1+, weak; 2+, moderate; and 3+, strong in >10% of tumor cells; only 2+ or 3+ were interpreted as being positive as previously described (14).
Statistical analysis
Data were presented as the means ± standard deviation. Statistical analysis was performed using MedCalc Statistical Software Version 17.6 (MedCalc Software, Ltd.). Normality was assessed using Kolmogorov-Smirnov and Shapiro-Wilk tests, and one-way analysis of variance followed by Tukey's post hoc test was used to compare the means of age between three groups categorized by Lauren's classification or mutation profiles by targeted NGS. The Fisher's exact test was used to compare the clinicopathological characteristics and mutation profiles between two or three groups. P<0.05 was considered to indicate a statistically significant difference.
Results
Mutation analysis
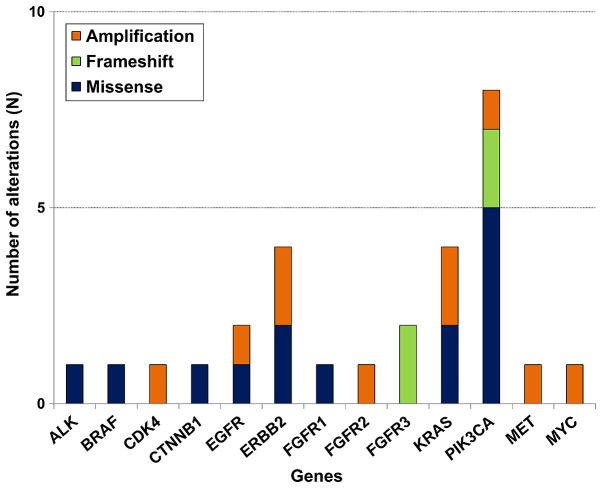
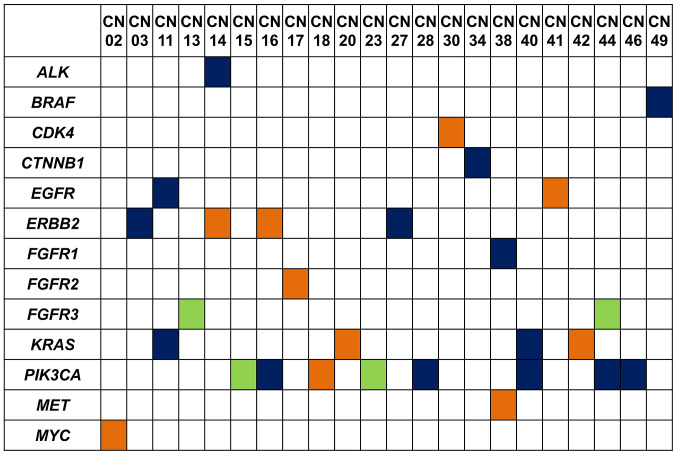
A median sequencing coverage depth of 1,845× (range, 129–2,000×) was achieved for the 50 gastric cancer tissues. Integrative analysis using the Ion Reporter identified somatic mutations with allele frequencies between 6 and 47% in tumor DNA samples without matched normal controls, in which a variant was classified as germline origin if its mutation frequency was near 50% (heterozygous) or 100% (homozygous), or otherwise classified as somatic. Null mutations (nonsense, frameshift or canonical ±1 or 2 splice sites) and missense variants with allele frequency <0.00001 predicted to be deleterious or damaging that were not registered in COSMIC database were also included. After applying stringent parameters for reliable variant calling (coverage depth >500×; allele frequency >5%) by filtering out unlikely pathogenic variants or potential raw base calling errors, at least one somatic alteration including SNVs, indels and amplification was detected in 22/50 (44%) patients. Details of the somatic alteration profiles identified by targeted NGS in these 22 cases of AGC are summarized in Tables I and II. Of the 35 hotspot genes and 19 genes for copy number variations (CNVs), 18 single nucleotide variants (SNVs) or small indels (14 missense and four frameshift mutations) and 10 amplifications were identified (Fig. 1). Amplification of the CDK4, EGFR, ERBB2, FGFR2, KRAS, MET, MYC and PIK3CA genes was confirmed to be graded as ≥2 by additional IHC (Fig. 2). Somatic alterations in the PIK3CA gene were the most frequently identified genetic alteration, occurring in 8/22 (36%) samples, followed by four ERBB2, four KRAS, two EGFR, two FGFR3 and one each for the other tested genes (Fig. 3).
Table I.
Results of somatic alteration profiles identified by the Oncomine focus assay in 22 patients with advanced gastric cancer.
| Sample | Gene | Transcript | Base change | Codon change | Effect | Freq % | COSMIC ID | dbSNP |
|---|---|---|---|---|---|---|---|---|
| CN03 | ERBB2 | NM_004448.3 | c.2524G>A | p.Val842Ile | Missense | 10 | COSM14065 | rs1057519738 |
| CN11 | EGFR | NM_005228.4 | c.2227G>A | p.Ala743Thr | Missense | 22 | – | rs759256622 |
| CN11 | KRAS | NM_033360.3 | c.38G>A | p.Gly13Asp | Missense | 47 | COSM532 | rs112445441 |
| CN13 | FGFR3 | NM_000142.4 | c.274delC | p.Gln92Serfs*6 | Frameshift | 28 | – | – |
| CN14 | ALK | NM_004304.4 | c.4061G>T | p.Cys1354Phe | Missense | 16 | – | rs963770969 |
| CN15 | PIK3CA | NM_006218.3 | c.328_330delGAA | p.Glu109del | Frameshift | 41 | COSM24710 | rs1060500031 |
| CN16 | PIK3CA | NM_006218.3 | c.323G>A | p.Arg108His | Missense | 27 | COSM27497 | rs886042002 |
| CN23 | PIK3CA | NM_006218.3 | c.328_330delGAA | p.Glu109del | Frameshift | 20 | COSM24710 | – |
| CN27 | ERBB2 | NM_004448.3 | c.2033G>A | p.Arg678Gln | Missense | 9 | COSM436498 | rs1057519862 |
| CN28 | PIK3CA | NM_006218.3 | c.1633G>A | p.Glu545Lys | Missense | 8 | COSM763 | rs104886003 |
| CN34 | CTNNB1 | NM_001904.3 | c.98C>T | p.Ser33Phe | Missense | 6 | COSM5669 | rs121913400 |
| CN38 | FGFR1 | NM_001174067.1 | c.2359C>T | p.Arg787Cys | Missense | 20 | – | – |
| CN40 | KRAS | NM_033360.3 | c.34G>A | p.Gly12Ser | Missense | 24 | COSM517 | rs121913530 |
| PIK3CA | NM_006218.3 | c.1633G>A | p.Glu545Lys | Missense | 7 | COSM763 | rs104886003 | |
| CN44 | FGFR3 | NM_000142.4 | c.274delC | p.Gln92Serfs*6 | Frameshift | 18 | – | – |
| PIK3CA | NM_006218.3 | c.1390T>G | p.Ser464Ala | Missense | 39 | – | – | |
| CN46 | PIK3CA | NM_006218.3 | c.1633G>A | p.Glu545Lys | Missense | 23 | COSM763 | rs104886003 |
| CN49 | BRAF | NM_004333.4 | c.1780G>A | p.Asp594Asn | Missense | 6 | COSM27639 | rs397516896 |
dbSNP, database for single nucleotide polymorphisms; freq, mutation frequency.
Table II.
Results of copy number variations identified by the Oncomine Focus DNA Assay in 22 patients with advanced gastric cancer.
| Sample | Gene | Length, kb | Variant class | CytoBand |
|---|---|---|---|---|
| CN02 | MYC | 4.4 | Amplification | 8q24.21(128,748,885-128,753,261)×13.51 |
| CN14 | ERBB2 | 15.1 | Amplification | 17q12(37,868,126-37,883,249)×24.58 |
| CN16 | ERBB2 | 15.1 | Amplification | 17q12(37,868,126-37,883,249)×14.25 |
| CN17 | FGFR2 | 107.0 | Amplification | 10q26.13(123,247,505-123,354,466)×13.78 |
| CN18 | PIK3CA | 35.4 | Amplification | 3q26.32(178,916,683-178,952,097)×13.23 |
| CN20 | KRAS | 35.5 | Amplification | 12p12.1(25,364,761-25,400,274)×19.43 |
| CN30 | CDK4 | 4.0 | Amplification | 12q14.1(58,142,052-58,146,026)×14.39 |
| CN38 | MET | 121.0 | Amplification | 7q31.2(116,313,480-116,434,565)×9.82 |
| CN41 | EGFR | 60.6 | Amplification | 7p11.2(55,198,956-55,259,538)×15.35 |
| CN42 | KRAS | 35.5 | Amplification | 12p12.1(25,364,761-25,400,274)×14.69 |
Figure 1.
Frequencies of somatic alteration types in various genes identified by the Oncomine Focus DNA assay in 50 patients with advanced gastric cancer. Genes are depicted on the x-axis, and the number of alterations is indicated on the y-axis.
Figure 2.
Representative images of immunohistochemistry staining on advanced gastric cancer tissues with gene amplification. (A) CDK4 in patient CN30. (B) EGFR in patient CN41. (C and D) ERBB2 in (C) patient CN14 and (D) patient CN16. (E) Fibroblast growth factor receptor 2 in patient CN17. (F and G) KRAS in (F) patient CN20 and (G) patient CN42. (H) Met proto-oncogene receptor tyrosine kinase in patient CN38. (I) MYC in patient CN02. (J) PI3K catalytic subunit α in patient CN18. CN, chungnam.
Figure 3.
Distribution of somatic alteration types among 50 patients with advanced gastric cancer identified by the Oncomine Focus DNA assay. Each patient is depicted on the x-axis, and the genes are indicated on the y-axis. Green, frameshift mutation; indigo, missense mutation; orange, amplification; white, no mutation.
Comparison of clinicopathological characteristics according to Lauren's classification
The 50 AGC cases were categorized into three subtypes according to Lauren's classification: Diffuse, intestinal and mixed type, and the clinicopathological characteristics and mutation profiles of patients in these three groups were compared. The mixed type was more frequently associated with a younger age compared with the diffuse or intestinal type (P=0.003; Table III). By contrast, the intestinal type more frequently exhibited moderate differentiation compared with the diffuse or mixed type (P<0.001). The frequency of mutations identified by targeted NGS with the OFA was not statistically different among the three groups (P=0.240).
Table III.
Comparison of clinicopathologic findings according to Lauren's classification subtypes in 50 patients with advanced gastric cancer.
| Characteristic | Diffuse (n=15) | Intestinal (n=30) | Mixed (n=5) | P-value |
|---|---|---|---|---|
| Male | 8 (53%) | 24 (80%) | 4 (80%) | 0.138 |
| Age, years (range) | 62 (39–91) | 71 (52–89) | 56 (53–59) | 0.003 |
| Differentiation | <0.001 | |||
| Moderate | 0 (0%) | 24 (80%) | 1 (20%) | |
| Poor | 15 (100%) | 6 (20%) | 4 (80%) | |
| TNM T stage | 0.830 | |||
| 2 | 1 (7%) | 3 (10%) | 0 (0%) | |
| 3 | 3 (20%) | 9 (30%) | 1 (20%) | |
| 4a | 11 (73%) | 18 (60%) | 4 (80%) | |
| TNM N stage | 0.378 | |||
| 0 | 3 (20%) | 7 (23%) | 0 (0%) | |
| 1 | 1 (7%) | 9 (30%) | 1 (20%) | |
| 2 | 4 (27%) | 7 (23%) | 1 (20%) | |
| 3a | 5 (33%) | 7 (23%) | 2 (40%) | |
| 3b | 2 (13%) | 0 (0%) | 1 (20%) | |
| TNM M stage | 0.088 | |||
| 0 | 14 (93%) | 30 (100%) | 4 (80%) | |
| 1 | 1 (7%) | 0 (0%) | 1 (20%) | |
| Any mutations (SNV + indel) | 0.240 | |||
| No | 13 (87%) | 19 (63%) | 3 (60%) | |
| Yes | 2 (13%) | 11 (37%) | 2 (40%) | |
| Any amplifications | 1.000 | |||
| No | 12 (80%) | 24 (80%) | 4 (80%) | |
| Yes | 3 (20%) | 6 (20%) | 1 (20%) | |
| Any mutations or amplifications | 0.522 | |||
| No | 10 (67%) | 16 (53%) | 2 (40%) | |
| Yes | 5 (33%) | 14 (47%) | 3 (60%) |
SNV, single nucleotide variant; indel, small insertion, duplication and deletion; TNM, Tumor-Node-Metastasis (4).
Comparison of clinicopathological characteristics according to mutation profiles
To examine the association between mutation profiles and clinicopathological characteristics, each element in the clinicopathological characteristics was categorized into three groups: No alteration, PIK3CA alterations and alterations other than PIK3CA. By Fisher's exact test, there were no statistical differences between clinicopathological findings except TNM staging (T) between the three groups (Table IV). AGCs with somatic alterations but no PIK3CA showed statistical difference in TNM staging (T), compared to AGCs without or with PIK3CA alterations (P=0.044). In addition, AGC with the PIK3CA alterations was categorized by Lauren's classification to the intestinal type only. The distribution of Lauren's classification in AGC with PIK3CA alterations was statistically different compared with AGC with alterations other than PIK3CA (P=0.028), but not with AGC with no alterations (P=0.076).
Table IV.
Comparison of clinicopathologic characteristics according to mutation profiles identified by Oncomine focus assay.
| Characteristics | No alterations (n=28) | Other alterationsa (n=14) | PIK3CA alterations (n=8) | P-value |
|---|---|---|---|---|
| Male | 19 (68%) | 9 (64%) | 8 (100%) | 0.152 |
| Age, years (range) | 62 (39–84) | 64 (53–91) | 77 (52–89) | 0.156 |
| Differentiation | 0.675 | |||
| Moderate | 14 (50%) | 6 (43%) | 5 (63%) | |
| Poor | 14 (50%) | 8 (57%) | 3 (37%) | |
| TNM T stage | 0.044 | |||
| 2 | 1 (4%) | 3 (21%) | 0 (0%) | |
| 3 | 11 (39%) | 1 (7%) | 1 (12%) | |
| 4a | 16 (57%) | 10 (72%) | 7 (88%) | |
| TNM N stage | 0.892 | |||
| 0 | 5 (18%) | 3 (21%) | 2 (25%) | |
| 1 | 6 (21%) | 3 (21%) | 2 (25%) | |
| 2 | 5 (18%) | 5 (37%) | 2 (25%) | |
| 3a/ | 10 (36%) | 2 (14%) | 2 (25%) | |
| 3b | 2 (7%) | 1 (7%) | 0 (0%) | |
| TNM M stage | 0.702 | |||
| 0 | 27 (96%) | 13 (93%) | 8 (100%) | |
| 1 | 1 (4%) | 1 (7%) | 0 (0%) | |
| Lauren's classification | 0.028b | |||
| 0.076c | ||||
| Diffuse | 10 (36%) | 5 (36%) | 0 (0%) | |
| Intestinal | 16 (57%) | 6 (43%) | 8 (100%) | |
| Mixed | 2 (7%) | 3 (21%) | 0 (0%) |
Alternations other than PIK3CA (single nucleotide variant, small insertion, duplication, deletion and amplification) identified by the Oncomine focus assay in the present study.
The distribution of Lauren's classification in AGC with PIK3CA alterations vs. AGC with alterations other than PIK3CA.
Discussion
Molecular characterization of gastric cancer may offer new tools for effective therapeutic strategies for well-defined sets of patients, as well as new clinical trial designs leading to an improvement of medical management of this disease (15). These novel classifications allow the identification of relevant gastric cancer genomic subsets by using techniques such as genomic screening, functional studies and molecular or epigenetic characterization (16). The large scale study of molecular profiling on gastric cancer in The Cancer Genome Atlas (TCGA), including a report from TCGA (5) and an independent study from the Asian Cancer Research Group (17), provide an outstanding opportunity to establish advanced molecular classifiers and predictors for the diagnosis and treatment of gastric cancer. In addition to these studies, several smaller studies have performed NGS to thoroughly establish the genomics of gastric cancer (18–21). Similar to these small-scale studies, the results of the present study demonstrated that AGC with PIK3CA alterations was associated with the intestinal type in Lauren's classification. The PIK3CA mutations activate the PI3K/Akt signaling pathway, have been reported in several types of carcinoma and are associated with negative outcome (22). PIK3CA amplification is associated with increased Akt phosphorylation levels, suggesting that this genetic alteration may serve a significant role in activating the PI3K/Akt signaling pathway that contributes to gastric carcinogenesis (23). Kim et al (24) have suggested that PIK3CA-mutated gastric cancer is a distinct disease entity that may require a different therapeutic approach. PIK3CA mutations were associated with Akt activation and high tumor aggressiveness in gastric cancer (24). In addition, high PIK3CA expression was significantly associated with tumor invasiveness, phenotype and poor patient survival (25). Unlike previous studies using quantitative PCR (24) or IHC (25) for the PIK3CA alterations only, the present study confirmed that PIK3CA mutation and amplification in gastric cancer were associated with adverse clinical manifestation using multi-gene analysis. The results of the present gene panel study demonstrated that AGC with mutated PIK3CA tended to be of an advanced TNM T stage (T4a, 88%), compared with AGC with wild-type PIK3CA (57%) or with mutations other than PIK3CA (72%), although Epstein-Barr virus (EBV) in situ hybridization was not investigated; a previous study demonstrated that PIK3CA mutations were more dispersed in EBV-positive cancer, but localized in the kinase domain (exon 20) in EBV-negative cancer (5).
The plethora of data obtained from recent NGS studies has resulted in the discovery of other candidate genes with similar functions to those of CDH1 and TP53 as classic driver genes of gastric cancer that may have valuable influence on therapeutic decisions and clinical outcomes (6). The novel main categories of driver mutations that have been ascertained by NGS include cell motility/cytoskeleton (26), chromatin remodeling (27), receptor tyrosine kinase pathway genes (28) and Wnt signaling (29). A recent study using NGS demonstrated notable mutation distributions in seven candidate genes (A-kinase anchoring protein 6, cyclic nucleotide binding domain containing 1, collagen type XIV alpha 1 chain, -box and WD repeat domain containing 7, integrin subunit alpha V, neurobeachin and xin actin binding repeat containing 2) that had not been previously report to be prominently mutated in gastric cancer (30). For medical genetic testing, which is crucial for precision medicine in cancer treatment, target NGS with a gene panel is advantageous due to cost savings, enhanced depth of coverage and precise target enhancement (31). Therefore, clinically helpful molecular classification based on targeted sequencing with a gene panel may enable the use of precise medicine in gastric cancer (21,30,32).
The identification of specific cancer subgroups is also enabling precise selection of patients who are likely to respond to immunotherapy (33). Through conventional methods for EBV and microsatellite instability, as well as the use of emerging genetics testing that focuses on a gene panel for mutations and amplifications, the proposed genetic group may be applied to new cases of AGC (5). Tumor heterogeneity and the incomplete understanding of the complex tumor biology represent an obstacle to the overcoming of the ‘one size fits all’ era of gastric cancer treatment (33). The most disturbed pathways in gastric cancer include adherens junction and focal adhesion (18). The clustered mutations in recurrent hotspots influence the functional domain and produce defective RHOA signaling, facilitating escape from anoikis in organoid cultures (18). In addition, gastric cancers with different Lauren's classifications exhibit diverse characteristics, and EGF containing fibulin extracellular matrix protein 1 (EFEMP1), frizzled related protein (FRZB) and keratin 23 (KRT23) have been identified as prognostic factors for gastric cancer subtypes (34). EFEMP1 and FRZB may be involved in diffuse gastric cancer-specific pathways, such as cell adhesion; KRT23 may serve a critical role in intestinal gastric cancer, considering that it has been demonstrated to be an oncogene that can influence DNA damage and proliferation response of colon cancer cells (35).
There were several limitations to the present study. The most notable limitation was the small sample size, as it was difficult to investigate significant relationships for the genetic landscape of gastric cancers from the present data. Thus, it is essential to further improve the molecular characterization of gastric cancer subtypes in order to provide researchers and medical oncologists with new tools for patient selection and stratification in future clinical development programs and subsequent trials (36). Comprehensive large-scale studies on the molecular classification in gastric cancer covering recent genomic, transcriptomic, proteomic and epigenomic features are required (37). Another limitation of the present study was that due to the inherent problems with the OFA, particularly important variants may have not been called; the OFA does not identify the mutations of previously known such as AT-rich interaction domain 1A (ARID1A), cadherin 1 (CDH1) and tumor protein p53 (TP53) as well as new, such as catenin alpha 2, GLI family zinc finger 3, mucin 6, and ring finger protein 43) significantly mutated driver genes. The OFA applied in the present study was a relatively small gene panel to be used for identification of complicated genetic alterations in AGC. Although PIK3CA gene alterations were the most frequently identified in the present study, frequencies of genetic alteration in ARID1A, LDL receptor related protein 1B and TP53 are higher compared with PIK3CA in public cancer genome databases such as cBioPortal for Cancer Genomics (www.cbioportal.org). Since PIK3CA alterations are significantly enriched in EBV-positive gastric cancer samples (28), EBV in situ hybridization should be required in a future study to confirm whether the previously published data may be extrapolated to the cohort of the present study. Similarly, although 15 diffuse type gastric cancer samples were included in the present study, no CDH1 mutations were reported, as the OFA did not cover coding region of the CDH1 gene. The identification of CDH1 gene mutations in diffuse type gastric cancer is important since most diffuse type gastric cancers are known to harbor pathogenic CDH1 mutations.
In conclusion, the present study demonstrated a molecular profiling approach that identified the potential molecular classifications for gastric cancer and suggested a framework for precision medicine in AGC. The improvements in this field may influence the discovery of novel driver mutations as well as sophisticated classification systems for gastric cancer that may be crucial for its pathogenesis if they can be effectively applied to improve the clinical outcome and therapeutic paradigm of AGC.
Acknowledgements
The authors would like to thank Mr. Taekyu Lee (Thermo Fisher Scientific, Inc.) for their contribution in providing technical support for Ion Torrent next generation sequencing.
Funding
This work was supported by The Catholic University of Korea Daejeon St. Mary's Hospital, Clinical Research Institute Grant (grant nos. CMCDJ-P-2018-010 and CMCDJ-P-2019-012) and the Chungnam National University Hospital Research Fund 2009. The bio-specimens and data used for this study were provided by the Biobank of Chungnam National University Hospital (Daejeon, Republic of Korea), which is a member of the Korea Biobank Network.
Availability of data and materials
The data generated and/or analyzed during the present study are available from the corresponding author on reasonable request.
Authors' contributions
JP and SL drafted the manuscript and revised it critically for important intellectual content. JP and SS performed the majority of the experiments and analyzed data. JH and HY performed the molecular experiments and interpreted data. SL and JK contributed to the conception and design of the work. JK gave the final approval of the version to be published. All authors agreed to be accountable for all aspects of the research in ensuring that the accuracy or integrity of any part of the work. All authors read and approved the final manuscript.
Ethics approval and consent to participate
The study protocol was approved by the Institutional Review Board of The Catholic University of Korea (DC18SESI0113). All subjects provided written informed consent for clinical and molecular analyses and publication before the study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Liang H, Kim YH. Identifying molecular drivers of gastric cancer through next-generation sequencing. Cancer Lett. 2013;340:241–246. doi: 10.1016/j.canlet.2012.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tan P, Yeoh KG. Genetics and molecular pathogenesis of gastric adenocarcinoma. Gastroenterology. 2015;149:1153–1162.e1153. doi: 10.1053/j.gastro.2015.05.059. [DOI] [PubMed] [Google Scholar]
- 4.Berlth F, Bollschweiler E, Drebber U, Hoelscher AH, Moenig S. Pathohistological classification systems in gastric cancer: Diagnostic relevance and prognostic value. World J Gastroenterol. 2014;20:5679–5684. doi: 10.3748/wjg.v20.i19.5679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cancer Genome Atlas Research Network, corp-author. Comprehensive molecular characterization of gastric adenocarcinoma. Nature. 2014;513:202–209. doi: 10.1038/nature13480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Katona BW, Rustgi AK. Gastric Cancer Genomics: Advances and future directions. Cell Mol Gastroenterol Hepatol. 2017;3:211–217. doi: 10.1016/j.jcmgh.2017.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arkenau HT. Gastric cancer in the era of molecularly targeted agents: Current drug development strategies. J Cancer Res Clin Oncol. 2009;135:855–866. doi: 10.1007/s00432-009-0583-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Paasinen-Sohns A, Koelzer VH, Frank A, Schafroth J, Gisler A, Sachs M, Graber A, Rothschild SI, Wicki A, Cathomas G, Mertz KD. Single-center experience with a targeted next generation sequencing assay for assessment of relevant somatic alterations in solid tumors. Neoplasia. 2017;19:196–206. doi: 10.1016/j.neo.2017.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Williams HL, Walsh K, Diamond A, Oniscu A, Deans ZC. Validation of the Oncomine™ focus panel for next-generation sequencing of clinical tumour samples. Virchows Arch. 2018;473:489–503. doi: 10.1007/s00428-018-2411-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee A, Lee SH, Jung CK, Park G, Lee KY, Choi HJ, Min KO, Kim TJ, Lee EJ, Lee YS. Use of the Ion AmpliSeq cancer hotspot panel in clinical molecular pathology laboratories for analysis of solid tumours: With emphasis on validation with relevant single molecular pathology tests and the Oncomine Focus Assay. Pathol Res Pract. 2018;214:713–719. doi: 10.1016/j.prp.2018.03.009. [DOI] [PubMed] [Google Scholar]
- 11.Sim NL, Kumar P, Hu J, Henikoff S, Schneider G, Ng PC. SIFT web server: Predicting effects of amino acid substitutions on proteins. Nucleic Acids Res. 2012;40:W452–W457. doi: 10.1093/nar/gks539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Adzhubei I, Jordan DM, Sunyaev SR. Predicting functional effect of human missense mutations using PolyPhen-2. Curr Protoc Hum Genet. 2013;7(Unit7.20) doi: 10.1002/0471142905.hg0720s76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Forbes SA, Beare D, Bindal N, Bamford S, Ward S, Cole CG, Jia M, Kok C, Boutselakis H, De T, et al. COSMIC: High-resolution cancer genetics using the catalogue of somatic mutations in cancer. Curr Protoc Hum Genet. 2016;91:10.11.1–10.11.37. doi: 10.1002/cphg.21. [DOI] [PubMed] [Google Scholar]
- 14.Matsusaka S, Kobunai T, Yamamoto N, Chin K, Ogura M, Tanaka G, Matsuoka K, Ishikawa Y, Mizunuma N, Yamaguchi T. Prognostic impact of KRAS mutant type and MET amplification in metastatic and recurrent gastric cancer patients treated with first-line S-1 plus cisplatin chemotherapy. Genes Cancer. 2016;7:27–35. doi: 10.18632/genesandcancer.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Serra O, Galán M, Ginesta MM, Calvo M, Sala N, Salazar R. Comparison and applicability of molecular classifications for gastric cancer. Cancer Treat Rev. 2019;77:29–34. doi: 10.1016/j.ctrv.2019.05.005. [DOI] [PubMed] [Google Scholar]
- 16.Alessandrini L, Manchi M, De Re V, Dolcetti R, Canzonieri V. Proposed molecular and miRNA classification of gastric cancer. Int J Mol Sci. 2018;19:1683. doi: 10.3390/ijms19061683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cristescu R, Lee J, Nebozhyn M, Kim KM, Ting JC, Wong SS, Liu J, Yue YG, Wang J, Yu K, et al. Molecular analysis of gastric cancer identifies subtypes associated with distinct clinical outcomes. Nat Med. 2015;21:449–456. doi: 10.1038/nm.3850. [DOI] [PubMed] [Google Scholar]
- 18.Wang K, Yuen ST, Xu J, Lee SP, Yan HH, Shi ST, Siu HC, Deng S, Chu KM, Law S, et al. Whole-genome sequencing and comprehensive molecular profiling identify new driver mutations in gastric cancer. Nat Genet. 2014;46:573–582. doi: 10.1038/ng.2983. [DOI] [PubMed] [Google Scholar]
- 19.Salomao M, Luna AM, Sepulveda JL, Sepulveda AR. Mutational analysis by next generation sequencing of gastric type dysplasia occurring in hyperplastic polyps of the stomach: Mutations in gastric hyperplastic polyps. Exp Mol Pathol. 2015;99:468–473. doi: 10.1016/j.yexmp.2015.08.014. [DOI] [PubMed] [Google Scholar]
- 20.Ge S, Li B, Li Y, Li Z, Liu Z, Chen Z, Wu J, Gao J, Shen L. Genomic alterations in advanced gastric cancer endoscopic biopsy samples using targeted next-generation sequencing. Am J Cancer Res. 2017;7:1540–1553. [PMC free article] [PubMed] [Google Scholar]
- 21.Ichikawa H, Nagahashi M, Shimada Y, Hanyu T, Ishikawa T, Kameyama H, Kobayashi T, Sakata J, Yabusaki H, Nakagawa S, et al. Actionable gene-based classification toward precision medicine in gastric cancer. Genome Med. 2017;9:93. doi: 10.1186/s13073-017-0484-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Engelman JA, Luo J, Cantley LC. The evolution of phosphatidylinositol 3-kinases as regulators of growth and metabolism. Nat Rev Genet. 2006;7:606–619. doi: 10.1038/nrg1879. [DOI] [PubMed] [Google Scholar]
- 23.Shi J, Yao D, Liu W, Wang N, Lv H, Zhang G, Ji M, Xu L, He N, Shi B, Hou P. Highly frequent PIK3CA amplification is associated with poor prognosis in gastric cancer. BMC Cancer. 2012;12:50. doi: 10.1186/1471-2407-12-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim JW, Lee HS, Nam KH, Ahn S, Kim JW, Ahn SH, Park DJ, Kim HH, Lee KW. PIK3CA mutations are associated with increased tumor aggressiveness and Akt activation in gastric cancer. Oncotarget. 2017;8:90948–90958. doi: 10.18632/oncotarget.18770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jang SH, Kim KJ, Oh MH, Lee JH, Lee HJ, Cho HD, Han SW, Son MW, Lee MS. Clinicopathological significance of elevated PIK3CA expression in gastric cancer. J Gastric Cancer. 2016;16:85–92. doi: 10.5230/jgc.2016.16.2.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thumkeo D, Watanabe S, Narumiya S. Physiological roles of Rho and Rho effectors in mammals. Eur J Cell Biol. 2013;92:303–315. doi: 10.1016/j.ejcb.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 27.Wang K, Kan J, Yuen ST, Shi ST, Chu KM, Law S, Chan TL, Kan Z, Chan AS, Tsui WY, et al. Exome sequencing identifies frequent mutation of ARID1A in molecular subtypes of gastric cancer. Nat Genet. 2011;43:1219–1223. doi: 10.1038/ng.982. [DOI] [PubMed] [Google Scholar]
- 28.Deng N, Goh LK, Wang H, Das K, Tao J, Tan IB, Zhang S, Lee M, Wu J, Lim KH, et al. A comprehensive survey of genomic alterations in gastric cancer reveals systematic patterns of molecular exclusivity and co-occurrence among distinct therapeutic targets. Gut. 2012;61:673–684. doi: 10.1136/gutjnl-2011-301839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pai P, Rachagani S, Dhawan P, Batra SK. Mucins and Wnt/β-catenin signaling in gastrointestinal cancers: An unholy nexus. Carcinogenesis. 2016;37:223–232. doi: 10.1093/carcin/bgw005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li X, Wu WK, Xing R, Wong SH, Liu Y, Fang X, Zhang Y, Wang M, Wang J, Li L, et al. Distinct subtypes of gastric cancer defined by molecular characterization include novel mutational signatures with prognostic capability. Cancer Res. 2016;76:1724–1732. doi: 10.1158/0008-5472.CAN-15-2443. [DOI] [PubMed] [Google Scholar]
- 31.Horak P, Frohling S, Glimm H. Integrating next-generation sequencing into clinical oncology: Strategies, promises and pitfalls. ESMO Open. 2016;1:e000094. doi: 10.1136/esmoopen-2016-000094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kuboki Y, Yamashita S, Niwa T, Ushijima T, Nagatsuma A, Kuwata T, Yoshino T, Doi T, Ochiai A, Ohtsu A. Comprehensive analyses using next-generation sequencing and immunohistochemistry enable precise treatment in advanced gastric cancer. Ann Oncol. 2016;27:127–133. doi: 10.1093/annonc/mdv508. [DOI] [PubMed] [Google Scholar]
- 33.Tirino G, Pompella L, Petrillo A, Laterza MM, Pappalardo A, Caterino M, Orditura M, Ciardiello F, Galizia G, De Vita F. What's new in gastric cancer: The therapeutic implications of molecular classifications and future perspectives. Int J Mol Sci. 2018;19:2659. doi: 10.3390/ijms19092659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Min L, Zhao Y, Zhu S, Qiu X, Cheng R, Xing J, Shao L, Guo S, Zhang S. Integrated analysis identifies molecular signatures and specific prognostic factors for different gastric cancer subtypes. Transl Oncol. 2017;10:99–107. doi: 10.1016/j.tranon.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Birkenkamp-Demtroder K, Hahn SA, Mansilla F, Thorsen K, Maghnouj A, Christensen R, Oster B, Orntoft TF. Keratin23 (KRT23) knockdown decreases proliferation and affects the DNA damage response of colon cancer cells. PLoS One. 2013;8:e73593. doi: 10.1371/journal.pone.0073593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pellino A, Riello E, Nappo F, Brignola S, Murgioni S, Djaballah SA, Lonardi S, Zagonel V, Rugge M, Loupakis F, Fassan M. Targeted therapies in metastatic gastric cancer: Current knowledge and future perspectives. World J Gastroenterol. 2019;25:5773–5788. doi: 10.3748/wjg.v25.i38.5773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ho SWT, Tan P. Dissection of gastric cancer heterogeneity for precision oncology. Cancer Sci. 2019;110:3405–3414. doi: 10.1111/cas.14191. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data generated and/or analyzed during the present study are available from the corresponding author on reasonable request.