Dear Editor
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the aetiological agent of coronavirus disease 2019 (COVID-19), has led to a global pandemic defying the geographical borders and putting the lives of billions at risk. The commonly evident symptoms include fever, altered sense of smell and/or taste, cough, sputum expectoration, sore throat, dyspnoea, fatigue and myalgia; whereas the uncommon symptoms include confusion, dizziness, headache, conjunctivitis, rhinorrhoea, nasal congestion, hemoptysis, chest pain, bronchial breath sounds, tachypnoea, crackles/rales on auscultation, cutaneous manifestations, cyanosis, and gastrointestinal symptoms. Throughout the world, mitigation strategies have lingered on the adoption of social distancing, face masks, hand hygiene and environmental disinfection. However, these precautionary measures are still not completely reliable until the modes of transmission of the SARS-CoV-2 remain unraveled.
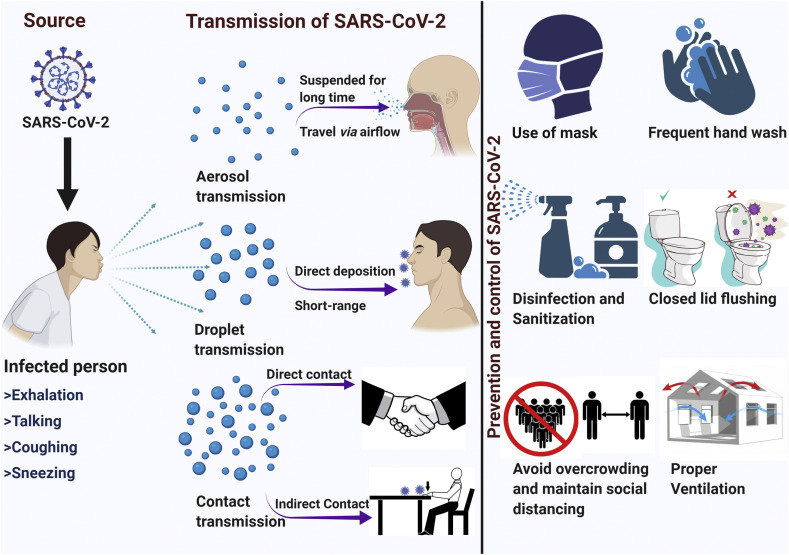
The transmission of respiratory pathogens have been associated with three primary modes known as “contact,” “droplet,” and “airborne” transmission. These modes are also being speculated in the context of SARS-CoV-2, but the existing research-based literature and the consequent guidance from the leading public health agencies are still paradoxical. The contact transmission can occur directly by physical touch or indirectly via fomites containing settled droplets. The droplet transmission involves large droplets more than 20 μm in diameter resulting from a violent expiratory event and deposited upon the conjunctiva or mucus membranes of a susceptible host directly [1] apart from being captured by inspiratory air flows and deposited along the respiratory tract.
The airborne or aerosol transmission occurs via small respiratory droplets or droplet nuclei, less than 10 μm in diameter, which remains airborne for sufficient time to transmit the pathogen and may get deposited deep into the respiratory tract, including alveolar region [1]. For the distinction of the transmission modes, droplet sizes need to be carefully interpreted; however, the propositions on the size-related terms are also paradoxical. An example of dichotomy is the postulation from the World Health Organization that respiratory droplets are more than 5–10 μm in diameter, whereas droplet nuclei are less than 5 μm in diameter. However, it is also being speculated that the particles of various sizes but indistinct behavior are produced in continuum during the respiratory activities of the infected person and particles as large as 50 μm can also remain airborne and travel the considerable distance as per the factors including force and volume of exhalation, airflow, temperature and humidity [2].
Although the contact and droplet routes are still being advocated as the main modes by leading public health agencies, including WHO, the airborne transmission had been recognized only for aerosol-generating procedures within the healthcare settings. But considering the emerging evidence of the presence of viable SARS-CoV-2 even in the absence of aerosol-generating procedures, the airborne transmission should also be recognized as an important mode of transmission of the SARS-CoV-2 [3]. Furthermore, it should not be neglected that the aerosols are generated even from activities such as exhalation, coughing, sneezing and talking by the infected individuals [2]. The indoor, as well as outdoor airborne transmission, have been elucidated by various empirical and laboratory studies conducted in countries including China, Italy, Singapore and USA [4].
The median estimates of the half-lives of the SARS-CoV-2 and SARS-CoV in aerosols are almost the same i.e. approximately 1.1–1.2 hours (3 hours viability), indicating that both viruses have similar stability characteristics for the plausible aerosol transmission and superspreading [5]. This time is enough for the exposure, inhalation and infection by the virus, which may occur near or far from the actual source, even beyond 1–2 m from an infected individual [6]. Recently, even the timeline of 16 hours has been reported for the virus to retain infectivity in laboratory-created aerosols [6].
Considering the airborne transmission, precautions such as hand washing and social distancing are appropriate but insufficient. As the viable SARS-CoV-2 has been isolated in air samples even 2–4.8 m away from the source, social distancing by currently recommended parameters of 6 feet would not be effective, especially in an indoor setting [3]. Additional mitigation measures should include the provision of effective ventilation, local exhausts, high-efficiency air filtration, germicidal ultraviolet light, avoidance of overcrowding in public places [6], toilet flushing with a closed lid, minimal use of central air conditioner, universal use of proper facial masks (N95 respirators or surgical or cloth masks as per the availability) fitting tightly to the face apart from proper personal protective equipment (PPE) including the N95 particle protective mask in the laboratory and healthcare settings [4] (Fig. 1 ). From the scientific community throughout the globe, there is an urgent and critical requirement of the research to unravel the paradox of SARS-CoV-2 transmission and infectivity so that effective mitigation measures can be outlined. Whereas, the policymakers and leading public health agencies need to upgrade the precautionary approach to interrupt all the plausible modes of transmission until this uncertainty is deciphered.
Fig. 1.
Primary control measures to mitigate the transmission of SARS-CoV-2 as per the consideration of aerosol transmission.
CRediT authorship contribution statement
Priyanka: Conceptualization, Data curation, Writing - original draft, Writing - review & editing. Om Prakash Choudhary: Conceptualization, Supervision, Visualization, Writing - original draft, Writing - review & editing. Indraj Singh: Writing - review & editing. Gautam Patra: Writing - review & editing.
Declaration of competing interest
We declare that we have no competing interests.
References
- 1.Drossinos Y., Stilianakis N.I. What aerosol physics tells us about airborne pathogen transmission. Aerosol Sci Tech. 2020;54(6):639–643. doi: 10.1080/02786826.2020.1751055. [DOI] [Google Scholar]
- 2.Wilson N., Corbett S., Tovey E. Airborne transmission of covid-19. BMJ. 2020;370 doi: 10.1136/bmj.m3206. m3206. [DOI] [PubMed] [Google Scholar]
- 3.Lednick J.A., Lauzardo M., Fan Z.H., Jutla A.S., Tilly T.B., Gangwar M. Viable SARS-CoV-2 in the air of a hospital room 1 with COVID-19 patients. medRxiv. 2020 doi: 10.1101/2020.08.03.20167395. 08.03.20167395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tang S., Mao Y., Jones R.M., Tan Q., Ji J.S., Li N., Shen J., Lv Y., Pan L., Ding P., Wang X., Wang Y., MacIntyre C.R., Shi X. Aerosol transmission of SARS-CoV-2? Evidence, prevention and control. Environ Int. 2020 doi: 10.1016/j.envint.2020.106039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., Tamin A., Harcourt J.L., Thornburg N.J., Gerber S.I., Smith J.O.L., Wit E., Munster V.J. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morawska L., Milton D.K. It is time to address airborne transmission of COVID-19. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa939. ciaa939. [DOI] [PMC free article] [PubMed] [Google Scholar]