Abstract
Background
We sought to understand the effects of coronavirus disease-2019 (COVID-19) on vascular surgery practices as related to the Vascular Activity Condition (VASCON) scale.
Methods
All members of the Vascular and Endovascular Surgery Society were surveyed on the effects of COVID-19 in their practices, educational programs, and self-reported grading of their surgical acuity level using the VASCON scale.
Results
Total response rate was 28% (206/731). Most respondents (99.5%) reported an effect of COVID-19 on their practice, and most were VASCON3 or lower level. Most reported a decrease in clinic referrals, inpatient/emergency room consults, and case volume (P < .00001). Twelve percent of respondents have been deployed to provide critical care and 11% medical care for COVID-19 patients. More than one-quarter (28%) face decreased compensation or salary. The majority of respondents feel vascular education is affected; however, most feel graduates will finish with the necessary experiences. There were significant differences in answers in lower VASCON levels respondents, with this group demonstrating a statistically significant decreased operative volume, vascular surgery referrals, and increased hospital and procedure limitations.
Conclusions
Nearly all vascular surgeons studied are affected by the COVID-19 pandemic with decreased clinical and operative volume, educational opportunities for trainees, and compensation issues. The VASCON level may be helpful in determining surgical readiness.
Keywords: Coronavirus, COVID, Vascular surgery, Practice, Compensation
The novel severe acute respiratory syndrome coronavirus-2 is a new human infecting pathogen that has spread rapidly around the globe since it was first identified.1 It is transmitted via respiratory droplets and most commonly results in fever, cough, dyspnea, and fatigue, although it may result also in pneumonias, acute respiratory distress syndrome, multiorgan system failure, thrombotic complications such as deep venous thrombosis and arterial occlusions, and death.2 As of April 22, 2020, there were more than 2.5 million cases globally with more than 175,000 deaths.3 The majority of U.S. states have imposed strict social distancing standards or formal stay-at-home orders. Although some hospitals have been inundated with coronavirus disease-19 (COVID-19) cases and pushed to their resource capacities, others who were not as affected by overwhelming COVID-19 cases have curtailed work other than emergency and urgent cases to flatten the curve of the pandemic. We sought to understand the effects of COVID-19 on vascular surgery practices by surveying all members of the Vascular and Endovascular Surgery Society (VESS) and correlate responses to the Vascular Activity Condition (VASCON) hospital surgical acuity scale.
Methods
All members of the VESS were sent an email invitation to take an anonymous and voluntary electronic survey with questions detailing general demographics, the effects of COVID-19 on their vascular surgery practice as well as vascular surgery educational programs they are involved with. This email was sent via the REDCap system on April 14, 2020, and a reminder email to complete the survey was sent out within 2 days of the initial request, and data collection was completed the morning of the fourth day. This expedited timeline was used to capture data at a distinct timepoint to prevent change in practice patterns over a prolonged period of data collection that may affect the results.
Statistical analysis
All data analysis was performed using Microsoft Excel (Redmond, Wash) and Graphpad (La Jolla, Calif). Descriptive statistics explored effects of COVID-19 on practice including the decision making process regarding common vascular surgery procedures, change in average caseload compared with before the COVID-19 pandemic, use of and availability of personal protective equipment (PPE), and changes to vascular surgery educational programs the respondent was involved with. Respondent data were categorized based on the VASCON scale into those with a low vs a high VASCON level. Respondents were also categorized based off the number of COVID-19 cases per 100,000 population in their state of primary practice. Categorical data between these groups was analyzed using a contingency table with Fisher exact test and two-tailed P values. A t-test with two-tailed P values was used for analyzing continuous data. A P value of less than .05 was considered statistically significant.
The Saint Louis University Institutional Review Board approved the protocol and questionnaire for this study before the collection of data.
VASCON Scale
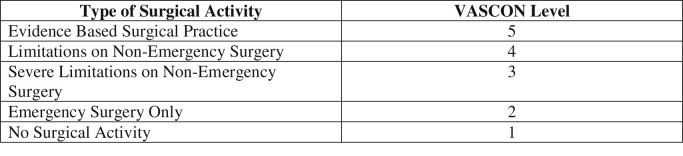
The VASCON was first suggested by Dr. Thomas Forbes during the COVID-19 pandemic as a way to describe the capability of hospitals/healthcare systems to provide surgical activity when resources become limited (Supplementary Fig 1, online only).4 It is based on the Defense Readiness Condition status used by the U.S. military to describe the levels of military readiness to world threats.5 Similar to this graduated scale of readiness, the VASCON is a scale demonstrating graduated levels of surgical activity from VASCON 5 (normal practice) to VASCON 1 (no surgical activity) and is self-reported, either by a practitioner or a health care system.
Supplementary Fig 1 (online only).
Vascular Activity Condition (VASCON) scale. Graduated scale that describes the capabilities of healthcare systems/hospital to provide surgical care when resources are limited.
COVID-19 pandemic information by state
On the day the initial survey was sent, COVID-19 case numbers (number of positive cases reported) from all U.S. states were collected via the Johns Hopkins Coronavirus resource website.6 These cases were normalized per 100,000 population within the states and the highest quintile of responses were considered high surge states (>150 cases/100,000 population). Participants were asked which state they predominantly practiced vascular surgery in, and these data were used to determine if the surgeon was in a high surge state or not.
Results
Demographics
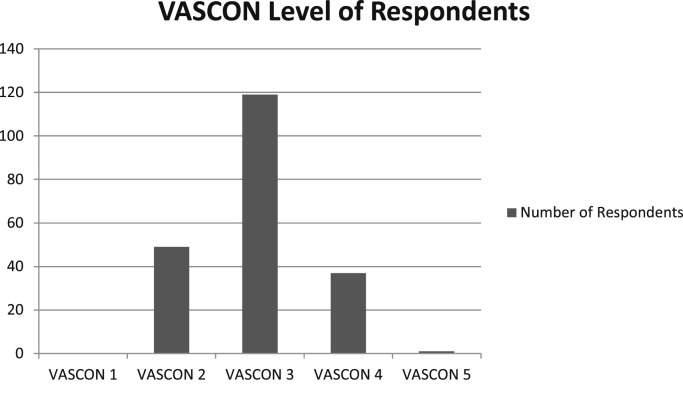
Of the 805 active and senior members of the VESS, accurate email addresses were available for 731, of which 206 completed our survey for an overall response rate of 28%. Most were under the age of 45 (69%), and practiced in a setting that had an academic affiliation (84%) (Supplementary Table, online only). Respondents were from 34 states and Puerto Rico, and nearly all (205/206 [99.5%]) reported their vascular surgery practices were being affected by the COVID-19 pandemic. When asked to determine what VASCON level their institution was currently in, most (168/206 [82%]) reported their facility in a VASCON 3 or lower level (168/206 [82%]), indicating increased limitations (Supplementary Fig 2, online only).
Supplementary Fig 2 (online only).
Vascular Activity Condition (VASCON) level of respondents. Bar chart showing number of respondents who report their center being in the above VASCON levels.
Effect of COVID-19 on overall clinical practice
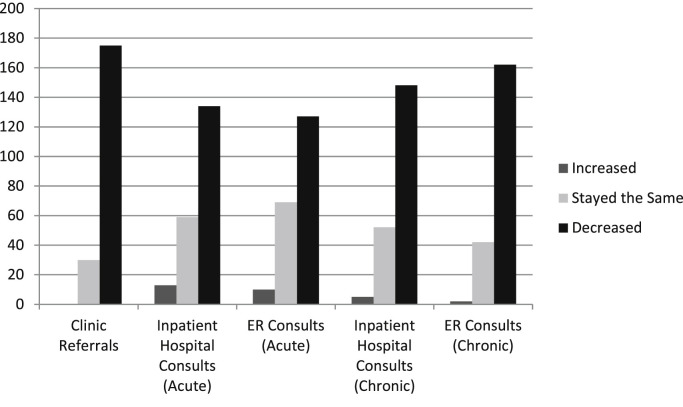
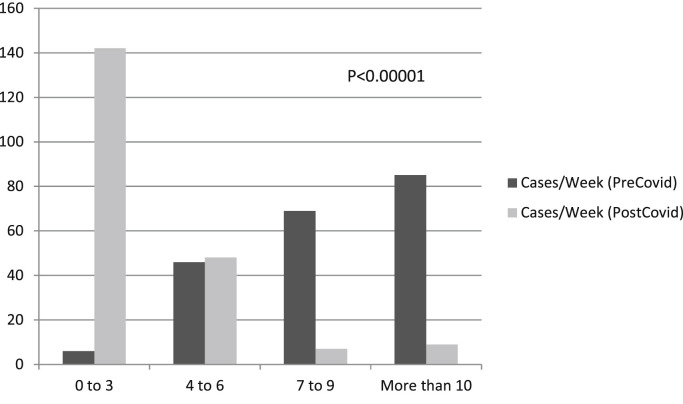
More respondents report having been affected fewer than 4 weeks, although those in lower VASCON levels reported a longer period of involvement and most have noticed a decrease in clinic referrals as well as inpatient and emergency room consults for acute and chronic vascular issues, with those in lower VASCON levels again more likely to report lower levels (Fig 1 ; Table I ). Those respondents located in high surge states were more likely to be in a lower VASCON level (38% vs 15%; P = .008). A significant number of other practice limitations were noted, including most commonly imposed limitations of elective cases, imposed limiting of in-person clinic visits, and increased time spent at home if no clinical duties. More than 10% of respondents have been redeployed to provide nonsurgical critical care for COVID-19 patients (25/206 [12%]) and a similar number have provided nonsurgical non-intensive care unit (ICU) care to COVID-19 patients on the floor (23/206 [11%]). More than one-quarter of respondents have faced decrease compensation or pay during this time period (57/206 [28%]). Overall, there has been a significant decrease in cases performed in the current time period as compared with before COVID-19 (P < .00001), with those in lower VASCON levels (higher acuity) performing significantly fewer cases compared with those in higher VASCON levels (P < .00001; Fig 2 ).
Fig 1.
Change in referrals and consults since the onset of the coronavirus disease-19 (COVID-19) pandemic. Bar chart showing respondents answers to questions on whether the above referrals/consults have increased, decreased, or stayed the same since the onset of COVID.
Table I.
Practice changes since the onset of the coronavirus disease-19 (COVID-19) pandemic
| Total respondents (N = 206) | VASCON level 1-3 (n = 168) | VASCON level 4-5 (n = 38) | P value | |
|---|---|---|---|---|
| Located in a high surge state | 70 (34) | 64 (38) | 6 (15) | .008 |
| Time affected, weeks | ||||
| 1-2 | 1 (0.5) | 93 (55) | 27 (71) | .0396 |
| 2-3 | 31 (15) | |||
| 3-4 | 88 (43) | |||
| >4 | 83 (40) | 74 (44) | 9 (24) | |
| Decrease in referrals | ||||
| Clinic referrals | 175 (85) | 148 (88) | 27 (71) | .0123 |
| Inpatient hospital consults (acute) | 134 (65) | 116 (69) | 18 (47) | .0144 |
| Emergency room consults (acute) | 127 (62) | 110 (65) | 17 (45) | .0258 |
| Inpatient hospital consults (chronic) | 148 (72) | 131 (78) | 17 (45) | .0001 |
| Emergency room consults (chronic) | 162 (79) | 140 (83) | 22 (58) | .0005 |
| Practice changes | ||||
| Limiting of elective cases | 201 (98) | 165 (98) | 36 (95) | .2299 |
| Limiting of urgent cases | 65 (32) | 60 (36) | 5 (13) | .0066 |
| Limiting of emergent cases | 10 (5) | 10 (6) | 0 (0) | .2136 |
| Limiting of in-person clinic visits | 192 (93) | 157 (93) | 35 (92) | .7258 |
| Limiting of vascular laboratory visits | 177 (86) | 150 (89) | 27 (71) | .0078 |
| ncreased telehealth visits | 186 (90) | 152 (90) | 34 (89) | .7687 |
| Lengthening call periods (increasing time off between call) | 90 (44) | 78 (46) | 12 (32) | .1060 |
| Staying at home if no clinical duty | 176 (85) | 143 (85) | 33 (87) | 1.0 |
| Providing surgical care you otherwise would not | 23 (11) | 21 (13) | 2 (5) | .2626 |
| Providing critical care for COVID-19 patients | 25 (12) | 24 (14) | 1 (3) | .0534 |
| Providing nonsurgical/non-ICU care for COVID-19 patients | 23 (11) | 24 (14) | 2 (5) | .2626 |
| Decreased compensation | 57 (28) | 45 (27) | 12 (32) | .5519 |
| Cases/week performed before COVID | ||||
| 0-3 | 6 (3) | 5 (3) | 1 (3) | .4933 |
| 4-6 | 46 (22) | 35 (20) | 11 (29) | |
| 7-9 | 69 (33) | 60 (36) | 9 (24) | |
| >10 | 85 (41) | 68 (41) | 17 (45) | |
| Cases/week performed after COVID | ||||
| 0-3 | 142 (69) | 127 (76) | 15 (40) | <.0001 |
| 4-6 | 48 (23) | 36 (21) | 12 (32) | |
| 7-9 | 7 (3) | 1 (6) | 6 (16) | |
| >10 | 9 (4) | 4 (2) | 5 (13) | |
| PPE use | ||||
| At work, I have easy access to PPE | 163 (79) | 126 (75) | 37 (97) | .0014 |
| At work, I have easy access to N95 mask | 130 (63) | 102 (61) | 28 (74) | .1919 |
| I feel pressure to generate RVU | 27 (13) | 20 (12) | 7 (18) | .2914 |
| I feel pressure to capture delayed cases | 65 (32) | 54 (32) | 11 (29) | .8471 |
| Vascular patients with emergent issues are not being handled in a safe/quick manner | 21 (10) | 21 (13) | 0 (0) | .0163 |
| My institution has handled the COVID-19 pandemic well | 148 (72) | 122 (73) | 26 (68) | .6899 |
| Once the COVID-19 pandemic is over, I will wear a mask for all patient care | 36 (18) | 31 (19) | 5 (13) | .6360 |
| Once the COVID-19 pandemic is over, I will wear a mask for patients with symptoms of cough or fever | 123 (60) | 104 (62) | 19 (50) | .2018 |
| Once the COVID-19 pandemic is over, I will stockpile PPE for my own personal use | 40 (19) | 36 (21) | 4 (11) | .1725 |
| I am spending more time with my family since the onset of COVID-19 | 172 (83) | 143 (85) | 29 (76) | .2251 |
ICU, Intensive care unit; PPE, personal protective equipment; RVU, relative value unit; VASCON, Vascular Activity Condition.
Self-reported changes in practice since onset of COVID-19. For PPE statements, respondents who answered agreed or strongly agreed with the statements above on a 5-point Likert scale (strongly disagree to strongly agree) were included.
Values are number (%). Boldface entries indicate statistical significance.
Fig 2.
Personal cases per week before and after the coronavirus disease-19 (COVID-19) pandemic. P < .00001. Self-reported cases per week before the onset of COVID-19 (PreCOVID) and after the onset of COVID-19 (PostCOVID).
Effect of COVID-19 on management of specific vascular disorders
Respondents were asked what type of vascular surgery cases they are currently delaying (Table II ). The vast majority report delaying peripheral arterial disease with claudication, asymptomatic carotid artery disease, smaller aneurysms (<6.5 cm abdominal and <7.0 cm thoracic aneurysms), and dialysis access for patients with end-stage renal disease in need of access more than 3 months from now. There was significant variation, however, in responses in regards to peripheral arterial disease with rest pain or tissue loss, and end-stage renal disease in need of access in less than 3 months. In both of these instances, however, those in lower VASCON (higher acuity) were more likely to be delaying these procedures.
Table II.
Procedures respondents would delay currently
| Total respondents (N = 206) | VASCON level 1-3 (n = 168) | VASCON level 4-5 (n = 38) | P value | |
|---|---|---|---|---|
| Peripheral arterial disease | ||||
| Claudication | 204 (99) | 167 (99) | 37 (97) | .3356 |
| Rest pain | 105 (51) | 94 (56) | 11 (29) | .0037 |
| Tissue loss | 26 (13) | 26 (16) | 0 (0) | .0055 |
| Carotid artery disease | ||||
| Severe stenosis (asymptomatic) | 199 (97) | 163 (97) | 36 (95) | .6152 |
| Severe stenosis with TIA/stroke | 10 (5) | 10 (6) | 0 (0) | .2136 |
| Aneurysmal disease | ||||
| Asymptomatic AAA 5.5-6.5 cm | 179 (87) | 148 (88) | 31 (82) | .2914 |
| Asymptomatic AAA >6.5 cm | 68 (33) | 62 (4) | 6 (16) | .0129 |
| Asymptomatic TAAA 6-7 cm | 141 (68) | 118 (70) | 23 (61) | .2519 |
| Asymptomatic TAAA >7 cm | 55 (27) | 50 (30) | 5 (13) | .0422 |
| Thoracic outlet syndrome with DVT | 88 (43) | 78 (46) | 10 (26) | .0290 |
| Chronic mesenteric ischemia | 139 (67) | 122 (73) | 17 (45) | .0018 |
| Dialysis access/ESRD | ||||
| In need of access (>3 months) | 187 (91) | 150 (89) | 37 (97) | .2098 |
| In need of access (<3 months) | 127 (62) | 107 (64) | 20 (53) | .2675 |
| In need of access with functioning catheter | 157 (76) | 133 (79) | 24 (63) | .0557 |
| In need of peritoneal dialysis catheter | 135 (66) | 111 (66) | 24 (63) | .8503 |
| With malfunctioning access | 27 (13) | 21 (13) | 6 (16) | .5972 |
AAA, Abdominal aortic aneurysm; DVT, deep vein thrombosis; ESRD, end-stage renal disease; TIA, transient ischemic attack; VASCON, Vascular Activity Condition.
Respondents who answered they would delay surgical or endovascular surgery procedures for these above patients.
Values are number (%). Boldface entries indicate statistical significance.
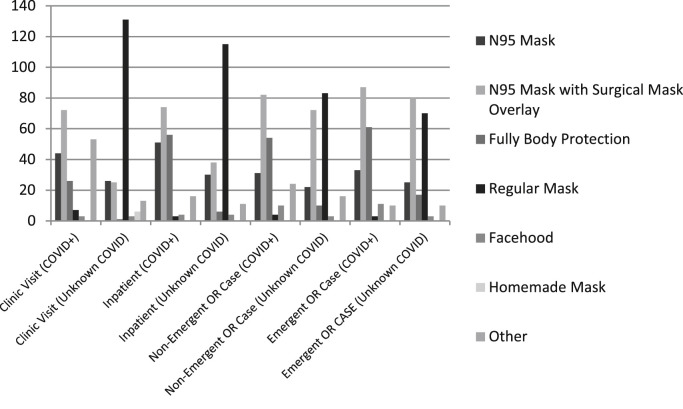
PPE considerations
The majority of respondents were using surgical masks (131/206 [64%]) for encounters with patients with unknown COVID-19 status in the clinic or on the wards; in the operating room for a nonemergent case, the majority were wearing N95 masks alone (22/206 [11%]) or in combination with surgical masks (72/206 [35%]) for patients with unknown COVID-19 status compared with 40% (83/206) who wore a surgical mask alone (Supplementary Fig 3, online only). There were similar numbers for emergent cases. Most respondents felt they had adequate access to PPE and N95 masks and the majority believed that their institutions were handling the COVID-19 pandemic well. More than 50% believe they will begin wearing masks when seeing patients with symptoms of cough or fever in the future, and a small percentage will begin wearing masks for all patient encounters (Table I).
Supplementary Fig 3 (online only).
Use of personal protective equipment (PPE) by respondents sorted by type of encounter and procedure type. COVID-19, Coronavirus disease-19.
Effects of COVID-19 on training programs and education
Of the 168 respondents in VASCON level 1 to 3, 143 had an academic affiliation (135 with vascular trainees) and 31 of the 38 respondents in VASCON 4 or 5 had such an affiliation (29 with vascular trainees). Those respondents with training programs report significant changes, with smaller resident in-house teams and increased periods of time off between call to limit exposure being the most common answers (Table III ). Programs with a lower VASCON level were more likely to reallocate both general and vascular surgery trainees to provide care for COVID-19 patients either in the ICU or medical floor setting. Although most participants believe the COVID-19 pandemic will negatively affect vascular surgery training, the majority believe that their learners will finish with enough cases to sit for the boards and that their trainees are using their time for adequate self-learning. Of the respondents, 41% (68/164 with vascular training programs) report their trainees are receiving less formal education during this time period.
Table III.
Changes in surgical trainee experiences since the coronavirus disease-19 (COVID-19) onset
| Total respondents | VASCON level 1-3 (n = 143) | VASCON level 4-5 (n = 31) | P value | |
|---|---|---|---|---|
| Surgical resident/fellow changes in workplace | ||||
| Smaller complement of residents in house | 152/174 (87) | 128 (90) | 24 (70) | .0775 |
| Increased home call | 92/174 (53) | 80 (56) | 12 (39) | .1117 |
| Increased time off between shifts | 97/174 (56) | 81 (57) | 16 (52) | .6921 |
| Reallocating vascular trainees to provide surgical care they would not otherwise | 36/174 (21) | 33 (23) | 3 (10) | .1404 |
| Reallocating vascular trainees to provide ICU care to COVID-19 patients | 31/174 (18) | 29 (20) | 2 (7) | .0745 |
| Reallocating general surgery residents to provide ICU care to COVID-19 patients | 46/174 (26) | 44 (31) | 2 (7) | .0059 |
| Reallocating vascular surgery residents to provide nonsurgical/non-ICU care to COVID-19 patients | 20/174 (12) | 20 (14) | 0 (0) | .0265 |
| Reallocating general surgery residents to provide nonsurgical/non-ICU care to COVID-19 patients | 26/174 (15) | 26 (18) | 0 (0) | .0051 |
| Vascular surgery trainee-specific statements | ||||
| The COVID-19 pandemic will negatively affect vascular surgery training | 99/164 (60) | 83 (61) | 16 (55) | .5374 |
| The COVID-19 pandemic will impact the ability of our learners to graduate with enough cases to sit for the boards | 39/164 (24) | 34 (25) | 5 (17) | .4736 |
| My vascular trainees have used the extra time they have been given to self study | 101/164 (62) | 88 (65) | 13 (45) | .0573 |
| My trainees are receiving less formal education during this time period | 68/164 (41) | 58 (43) | 10 (34) | .5337 |
| The training for vascular surgery trainees will need to be extended for them to get exposure to adequate vascular cases | 8/164 (5) | 7 (5) | 1 (3) | 1.0 |
ICU, Intensive care unit; VASCON, Vascular Activity Condition.
Self-reported changes in surgical training programs of respondents with academic affiliation. For the vascular surgery trainee-specific statements, respondents with vascular surgery trainees who answered agreed or strongly agreed to the statements above on a 5-point Likert scale (strongly disagree to strongly agree) were included.
Values are number (%). Boldface entries indicate statistical significance.
More than 10% of respondents (21/206) report that they or one of their partners have tested positive for COVID-19 and 14% of respondents (29/206) report that at least one of their trainees has tested positive.
Discussion
The COVID-19 pandemic has affected more than 800,000 Americans and has caused more than 50,000 deaths in the United States to date, a number that is exponentially increasing every day.6 It has overwhelmed hospital resources and healthcare supplies, such as PPE and ventilator use. One of the strategies to ensure adequate allocation of resources to deal with the COVID-19 outbreak has been to decrease the number of elective treatments, which can be safely delayed for weeks to months.7 , 8 By definition, any operation that allows a surgeon and the patient to elect the timing of the operation without having a negative impact on clinical outcome can be considered for inclusion in this category of treatments. This strategy has direct implications for surgeons, because the majority of surgical procedures performed across the United States are considered elective; however, there is not a uniform consensus as to what can be safely delayed in vascular surgery. Faced with differing guidelines from the federal government, state governments, and local hospitals, surgeons in the United States developed a graduated readiness level alert status, the Surgical Activity Condition, which was derived from the U.S. military system of Defense Readiness Condition. Forbes et al4 developed a similar model, the VASCON, to help prioritize operations for vascular surgeons in a uniform manner. Although this level was defined to describe the surgical readiness of vascular practices as a part of a larger healthcare system, it may perhaps be more useful in predicting and measuring the impact of a pandemic or other catastrophe on a vascular surgery practice as demonstrated in our article.
Although some hospitals are in the early phases of the pandemic, other health systems are completely overwhelmed by the significant number of patients with COVID-19 who need hospital admission and aggressive treatments. This survey was designed to determine the impact of the COVID-19 pandemic on practice patterns of vascular surgeons across the United States, including the effect on vascular surgery training programs, and to assess the validity of the tiered VASCON system as a means of identifying the differing levels of pandemic acuity. We chose this time to administer the survey as the United States is experiencing an unprecedented level of regional and national restrictions. At the time of writing, 41 of 51 states (including Washington, D.C.) were under some form of self-quarantine, with the remaining 10 encouraging social distancing. Our study confirms almost all (>99%) vascular surgery practices have been affected by this pandemic in some shape or form. At the time of the survey, most surgeons reported their facilities to be at VASCON level 3 or lower levels, and a majority of them reported a significant decrease in the number of elective operations, clinic visits, and consults for both acute and chronic vascular conditions. About 20% of vascular surgeons were deployed to provide nonvascular care to COVID-19 patients, and about 25% faced decreased compensation. Although vascular surgery activity in general was reported diminished by most of the respondents, those in the lower levels of VASCON (higher acuity) demonstrated statistically significant decreases in both referrals and consults for vascular disease, as well as limitations of urgent procedures and the number of vascular surgery procedures performed per week. Regardless of the VASCON levels, the majority of respondents report significant practice pattern changes, including increased length of time at home if not on clinical duty with nearly one-half experiencing changes to the call schedules to decrease overall exposure to the hospital.
The majority of elective vascular surgery operations serve to prevent catastrophic events such as death and limb loss. Postponing these operations, thus, involves complex decision-making processes, considering the risks, benefits, and alternatives. The long-term implication of delaying vascular surgery cases, which often fall in an urgent category, will not be realized until we emerge from the pandemic. There was wide agreement across the specialty in regard to some types of operations that should be deferred, such as asymptomatic carotid artery disease and moderate sized aneurysmal disease, however, in other categories of disease, such as peripheral arterial disease and dialysis access there was significant discrepancy in appropriate management strategies. Vascular surgeons in our survey were in broad agreement on delaying cases for claudication and not those with tissue loss, although there was significant equipoise when asked about patients with rest pain, with essentially one-half of the respondents reporting they would delay and one-half reporting they would not. When looking at responses based on VASCON level, however, those with lower VASCON levels (higher acuity) were significantly more likely to delay these cases. Similarly, there was significant equipoise when respondents were asked about dialysis access creation for a patient in need within 3 months, although there was no difference noted between VASCON levels.
During a global pandemic, the risk of viral transmission to health care providers cannot be underestimated. Owing to the invasive nature of care provided by surgeons, they are at an extremely high risk of getting exposed COVID-19; viral particles are found in virtually all body fluids, including sputum, blood, and stool.9 , 10 For healthcare providers treating the patients suffering from COVID-19, viral particles have been found on shoe covers and intubation for surgical procedures has been associated with aerosolization of viral particles into the air, which can persist for long periods of time.11 Different strategies for the protection of healthcare workers have been reported, but most focus on the availability of PPE, such as N95 masks.12 Although many media outlets have focused on the lack of availability of PPE for healthcare providers, our survey demonstrated that the majority of vascular surgeons reported that they had adequate PPE supplies, their institutions were handling the pandemic situation satisfactorily, and vascular surgery patients with acute issues were being handled appropriately. It should be noted, however, that those in the lower VASCON level (higher acuity) did have a statistically significant increase in respondents who believed their access to PPE was not adequate and that vascular surgery patients were not being handled expeditiously. The majority of respondents were universally wearing N95 masks alone or in combination with a surgical mask when managing patients in the operating room with an unknown COVID-19 status, and most were wearing a regular surgical mask when seeing patients with unknown COVID-19 status in the clinic or inpatient settings. Many centers have created protocols to preserve PPE, including recycling of masks or standardizing access and use.13 Looking to the future, the majority of the vascular surgeons believed that they would wear masks when they encounter patients with symptoms of upper respiratory tract illness, and a very small percentage felt that they would wear masks during all patient encounters, regardless of the symptomatic status of the patients.
Any significant interruption in patient-care comes with the unintended consequences on the quantity and quality of graduate medical education for vascular trainees. The majority of the vascular surgeons felt that altered surgical practices during the pandemic would negatively affect vascular surgery training; however, the majority agreed that the trainees would complete the training with enough operative cases to satisfy the American Board of Surgery requirements, and a majority felt that the trainees are using the free time in self-learning activities. Ultimately, ensuring the adequate education of future vascular surgeon falls on us. Providing vascular conferences via teleconferencing, and offering alternative educational opportunities remotely will be necessary if we have prolonged social distancing policies.
Looking at all survey responses, the self-reported VASCON level was a good indication of surgical acuity present at individual health centers. Those in lower self-reported VASCON levels (higher acuity) showed diminished clinical activity, increased effects on practice and academic endeavors, and access to PPE. In future pandemics, this scale may be used to accurately reflect levels of surgical readiness.
The end of this pandemic is not known, nor is it known with certainty where we lie on the curve of total cases. At this point in time, however, a not insignificant number of vascular surgeons have been directly affected, with 10% of respondents reporting their self or partners being infected and 14% reporting residents becoming infected. This finding has grave implications on staffing of vascular surgery practices as well as resident complement as we move through our new reality. The timing of the return to normal elective surgical practices is debated. A recent joint statement from the American College of Surgeons, American Society of Anesthesiologists, Association of Perioperative Registered Nurses, and the American Hospital Association recently suggested this return should occur when there were several conditions met.14 These include a sustained decrease in the rate of new COVID-19 cases in the geographic area for 14 days and the availability of PPE and COVID-19 testing. Additionally, they recommend case prioritization to ensure those patients with the highest needs will be taken care of first.
The limitations of this study are inherent to any self-reported research analysis. The results reflect the opinions of only those surgeons who participated in the survey (VESS members) and the majority of respondents were involved in academic practices, which may skew responses towards this group. Recall bias is often a limitation of any survey. We are also concerned about the number of multiple surveys being conducted by several vascular surgery societies, leading to survey fatigue, which may impact reporting of actual findings, especially if similar questions are being asked in all the surveys. As with any unsolicited emailed survey, the overall response rate (28%) was not high, although this does fall into the expected rates for this type of survey. VASCON levels are continually changing with time across the country, and these findings may change with different levels of severity of the pandemic. Additionally, we did not have the granular data (by city) to determine the exact COVID-19 surge amount the individual participants were experiencing and could only associate this to their state of practice. Data were not readily available for a more in-depth analysis of COVID-19 measures (such as ICU use or medical demands of the involved patients). A significant number of respondents were in VASCON 3 or lower levels, which limited in depth evaluation across the entire continuum of VASCON levels and resulted in analysis into just high and low acuity environments. Questions pertaining to surgical education were only delivered to survey participants who self-reported involvement with surgical training paradigms; however, we had no way to ascertain the educational authority or extent of involvement of these individuals with surgical education, thus relying on their role as faculty to provide opinions on the effects of COVID-19 on vascular surgery education. Owing to time constraints, and the desire to survey surgeons at the peak pandemic, the survey was not validated, but instead relies on descriptive statistics.
The strengths of this study are that it reflects vascular surgery practice patterns across the country at a distinct time in the midst of this severe pandemic. It includes surgeons from both academic and private practices and encompasses the views of vascular surgeons with different baseline practice patterns and hence provides a real-life picture of how this pandemic has affected surgeons at the front lines and those in communities not as affected.
In conclusion, the majority of U.S. vascular surgeons are affected by the COVID-19 global pandemic with decreased clinical and operative volume, educational opportunities for their trainees, and potential compensation issues. The VASCON level of surgical acuity scaling is a helpful way to determine surgical readiness in a healthcare system or hospital. Moving forward, vascular and institutional leadership need to think about PPE availability, reimbursement strategies, and plans for graduated return to normal activity as well as prepare for future pandemics by creating readiness response plans based off the VASCON scale.
Author contributions
Conception and design: FA, JB, MS
Analysis and interpretation: FA, JB, MS
Data collection: MS
Writing the article: FA, JB, MS
Critical revision of the article: FA, JB, MS
Final approval of the article: FA, JB, MS
Statistical analysis: MS
Obtained funding: Not applicable
Overall responsibility: MS
FA and JB contributed equally to this article and share co-first authorship.
Footnotes
Author conflict of interest: none.
Additional material for this article may be found online at www.jvascsurg.org.
The editors and reviewers of this article have no relevant financial relationships to disclose per the JVS policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
Additional material for this article may be found online at www.jvascsurg.org.
Appendix (online only).
Supplementary Table (online only).
Respondent demographics
| Variable | Respondents answering yes (N = 206) |
|---|---|
| Sex | |
| Male | 156 (76) |
| Female | 48 (23) |
| Preferred not answering | 2 (1) |
| Age, years | |
| <35 | 8 (4) |
| 35-40 | 56 (27) |
| 40-45 | 48 (23) |
| 45-50 | 29 (14) |
| 50-55 | 31 (15) |
| 55-60 | 18 (9) |
| >60 | 14 (7) |
| Type of practice | |
| Academic affiliation | 174 (84) |
| University practice | 114 (55) |
| Hospital-based with academic affiliation | 36 (17) |
| Private practice with academic affiliation | 20 (10) |
| Military with academic affiliation | 4 (2) |
| No academic affiliation | 32 (16) |
| Hospital-based with no academic affiliation | 13 (6) |
| Private practice with no academic affiliation | 16 (8) |
| Military practice with no academic affiliation | 1 (0.5) |
| Other | 2 (1) |
Values are number (%).
References
- 1.Hu Y., Sun J., Dai Z., Deng H., Li X., Huang Q., et al. Prevalence and severity of corona virus disease 2019 (COVID-19): a systematic review and meta-analysis. J Clin Virol. 2020;127:104371. doi: 10.1016/j.jcv.2020.104371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen T., Wu D., Chen H., Yan W., Yang D., Chen G., et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization Coronavirus Disease 2019 (COVID-19) Situation Report - 94. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200423-sitrep-94-covid-19.pdf?sfvrsn=b8304bf0_4 Available at:
- 4.Forbes T.L. Vascular surgery activity condition is a common language for uncommon times. J Vasc Surg. 2020;72:391–392. doi: 10.1016/j.jvs.2020.04.490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sagan S.D. Nuclear alerts and crisis management. Int Secur. 1985;9:99–139. [Google Scholar]
- 6.COVID-19 Dashboard by the Center for Systems Science and Engineering at the Johns Hopkins University. https://coronavirus.jhu.edu/map.html Available at: [DOI] [PMC free article] [PubMed]
- 7.Diaz A., Sarac B.A., Schoenbrunner A.R., Janis J.E., Pawlik T.M. Elective surgery in the time of COVID-19. Am J Surg. 2020;219:900–902. doi: 10.1016/j.amjsurg.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ng J.J., Ho P., Dharmaraj R.B., Wong J.C.L., Wong J.C.L., Choong A.M.T.L. The global impact of COVID-19 on vascular surgical services. J Vasc Surg. 2020;71:2182–2183.e1. doi: 10.1016/j.jvs.2020.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang W., Xu Y., Gao R., Lu R., Han K., Wu G., et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020;323:1843–1844. doi: 10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guan W.-J., Ni Z.-Y., Hu Y., Liang W.-H., Ou C.-Q., He J.-X., et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ong S.W.X., Tan Y.K., Chia P.Y., Lee T.H., Ng O.T., Wong M.S.Y., et al. Air, surface environmental, and personal protective equipment contamination by severe cute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020;323:1610–1612. doi: 10.1001/jama.2020.3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chang D., Xu H., Rebaza A., Sharma L., Dela Cruz C.S. Protecting healthcare workers from subclinical coronavirus infection. Lancet Respir Med. 2020;8:e13. doi: 10.1016/S2213-2600(20)30066-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Forrester J.D., Nassar A.K., Maggio P.M., Hawn M.T. Precautions for Operating room team members during the COVID-19 pandemic. J Am Coll Surg. 2020;230:1098–1101. doi: 10.1016/j.jamcollsurg.2020.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Joint Statement: Roadmap for resuming elective surgery after COVID-19 pandemic. https://www.facs.org/covid-19/clinical-guidance/roadmap-elective-surgery Available at: