Abstract
The coronavirus disease 2019 pandemic caused by severe acute respiratory syndrome coronavirus 2 presents with a spectrum of clinical manifestations from asymptomatic or mild, self-limited constitutional symptoms to a hyperinflammatory state (“cytokine storm”) followed by acute respiratory distress syndrome and death. The objective of this study was to provide an evidence-based review of the associated pathways and potential treatment of the hyperinflammatory state associated with severe acute respiratory syndrome coronavirus 2 infection. Dysregulated immune responses have been reported to occur in a smaller subset of those infected with severe acute respiratory syndrome coronavirus 2, leading to clinical deterioration 7 to 10 days after initial presentation. A hyperinflammatory state referred to as cytokine storm in its severest form has been marked by elevation of IL-6, IL-10, TNF-α, and other cytokines and severe CD4+ and CD8+ T-cell lymphopenia and coagulopathy. Recognition of at-risk patients could permit early institution of aggressive intensive care and antiviral and immune treatment to reduce the complications related to this proinflammatory state. Several reports and ongoing clinical trials provide hope that available immunomodulatory therapies could have therapeutic potential in these severe cases. This review highlights our current state of knowledge of immune mechanisms and targeted immunomodulatory treatment options for the current coronavirus disease 2019 pandemic.
Key words: IL-6, sepsis, cytokine storm, cytokines, COVID-19, SARS-CoV-2, TNF-α, JAK, STING, proinflammatory, hyperinflammatory, hemophagocytic lymphohistiocytosis
Abbreviations used: ACE2, Angiotensin-converting enzyme 2; ARDS, Acute respiratory distress syndrome; BTK, Bruton’s tyrosine kinase; CAR, Chimeric antigen receptor; CP, Convalescent plasma; COVID-19, Coronavirus disease 2019; CRP, C-reactive protein; CRS, Cytokine release syndrome; CS, Cytokine storm; FDA, Food and Drug Administration; HLH, Hemophagocytic lymphohistiocytosis; JAK, Janus-associated kinase; MAS, Macrophage activation syndrome; MERS, Middle East respiratory syndrome; MERS-CoV, MERS coronavirus; SARS-CoV, SARS coronavirus; SARS-CoV-2, Severe acute respiratory syndrome coronavirus 2; STING, Stimulator of IFN genes
Information for Category 1 CME Credit
Credit can now be obtained, free for a limited time, by reading the review articles in this issue. Please note the following instructions.
Method of Physician Participation in Learning Process: The core material for these activities can be read in this issue of the Journal or online at the JACI Web site: www.jacionline.org. The accompanying tests may only be submitted online at www.jacionline.org. Fax or other copies will not be accepted.
Date of Original Release: September 2020. Credit may be obtained for these courses until August 31, 2021.
Copyright Statement: Copyright © 2020-2021. All rights reserved.
Overall Purpose/Goal: To provide excellent reviews on key aspects of allergic disease to those who research, treat, or manage allergic disease.
Target Audience: Physicians and researchers within the field of allergic disease.
Accreditation/Provider Statements and Credit Designation: The American Academy of Allergy, Asthma & Immunology (AAAAI) is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians. The AAAAI designates this journal-based CME activity for a maximum of 1.00 AMA PRA Category 1 Credit™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
List of Design Committee Members: Ana Copaescu, MD, FRCPC, Olivia Smibert, MBBS, FRACP, Andrew Gibson, PhD, Elizabeth Phillips, MD, and Jason Trubiano, MBBS, BBiomedSci, PhD, FRACP (authors); Zuhair K. Ballas, MD (editor)
Disclosure of Significant Relationships with Relevant Commercial Companies/Organizations: The authors declare that they have no relevant conflicts of interest. Z. K. Ballas (editor) disclosed no relevant financial relationships.
Activity Objectives:
-
1.
To define the immunopathogenesis of the cytokine storm associated with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
-
2.
To explore the role of the IL-6 in the SARS-CoV-2 inflammatory and viral responses.
-
3.
To describe the role of biological immunotherapies targeting the hyperinflammatory immune response in SARS-CoV-2.
-
4.
To outline the therapeutic strategy targeting upstream and downstream immunologic pathways in SARS-CoV-2.
Recognition of Commercial Support: This CME activity has not received external commercial support.
List of CME Exam Authors: Ana Copaescu, MD, FRCPC, and Elizabeth Jane Phillips, MD.
Disclosure of Significant Relationships with Relevant Commercial
Companies/Organizations: The examination authors declare no relevant conflicts of interest.
The coronavirus disease 2019 (COVID-19) pandemic caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) presents an enormous challenge for public health and clinicians globally. Increased understanding of the immunopathogenesis of SARS-CoV-2 infection as well as ongoing clinical trials of host target drugs such as hydroxychloroquine, direct antivirals, convalescent plasma (CP), and other immunomodulatory agents hold promise for future evidence-based and targeted therapies to reduce the morbidity and mortality of the most vulnerable populations.
Although infection is often asymptomatic or associated with mild to moderate self-limiting symptoms such as fever, dry cough, myalgia, and fatigue,1, 2, 3, 4, 5, 6 a subset of patients with severe SARS-CoV-2 infection develop a clinically severe hyperinflammatory state or cytokine storm (CS) for which pulmonary involvement such as acute respiratory distress syndrome (ARDS) is a cardinal feature.1 , 7 Furthermore, a subgroup of previously healthy children has been diagnosed with a multisystem inflammatory syndrome associated with acute SARS-CoV-2 infection that appears distinct from the adult CS.8
Although the individual components of CS are varied, IL-6 has emerged of particular interest in the context of SARS-CoV-2 infection after being identified as the most significant predictor of mortality in recent retrospective studies of patient survival in COVID-19.1 Herein, we review the current understanding of the origin and mechanisms of CS associated with SARS-CoV-2 infection, with focus on the identification and implication of IL-6 and other proinflammatory cytokines and pathways in CS-driven ARDS, and discuss the potential utility of anti–IL-6 and other cytokine-targeting immunomodulatory biologics for the treatment of this critically ill population.
Search strategy and selection criteria
We searched PubMed for peer-reviewed articles published between January 1, 2000, and April 18, 2020 (date of last search), with the terms (“IL-6” OR “interleukin-6” OR “cytokine”) AND (“sepsis” OR “SIRS” OR “systemic inflammatory response syndrome” OR “non-infectious systemic inflammatory response syndrome” OR “ARDS” OR “acute respiratory distress syndrome” OR “cytokine storm” OR “inflammatory response” OR “septic shock” OR “critically ill” OR “organ dysfunction” OR “infection”) AND (“ICU” OR “intensive care unit” OR “ED” OR “emergency department”). A second search was oriented on treatment, with the terms (“IL-6” OR “interleukin-6” OR “IL-1” OR “interleukin-1” OR “TNF” OR “tumor necrosis factor” OR “interferon gamma” OR “STING” OR “interferon pathway”) AND (“sepsis” OR “SIRS” OR “systemic inflammatory response syndrome” OR “ARDS” OR “acute respiratory distress syndrome” OR “cytokine storm” OR “inflammatory response” OR “septic shock” OR “critically ill” OR “organ dysfunction” OR “infection”) AND (“IL-6 inhibitor” OR “interleukin-6 inhibitor” OR “JAK-STAT” OR “tocilizumab” OR “humanized IL-6R antibody” OR “anakinra” OR “IL-1 inhibitor”). Please refer to Fig E1 in this article’s Online Repository at www.jacionline.org for details concerning the number of articles entered in PubMed with the “cytokine storm” keywords.
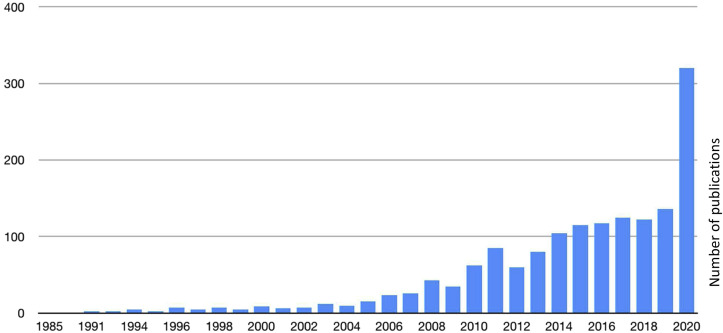
Fig E1.
“Cytokine Storm” in PubMed Search (1985-May 2020). The figure represents the number of articles entered in PubMed from 1985 to May 2020. This marks several events that have led to CS including the 1985 original description in graft-versus-host disease, a small increase during the 2003-2005 SARS-CoV, a more significant number for the 2009-2010 H1N109, and the ongoing rise in publications associated with SARS-CoV-2.
All recent articles on COVID-19/SARS-CoV-2 were reviewed including preprints from bioRxiv and medRxiv as a more real-time resource, but realizing the lack of peer review limitation. To carefully include the proposed trials for COVID-19, we researched the ClinicalTrials.gov/trials website.
Articles published in English were selected and reviewed. There was a focus on clinical trials, meta-analysis, randomized controlled trials, and systematic reviews as well as novel and significant studies. Finally, we also identified several new references from those listed in the reviewed articles. Please note that although there is increasing information about SARS-CoV-2 and its immune consequences, most of the literature available on COVID-19 and SARS-CoV-2 infection originates from the onset of the pandemic, in China, with various publications from disease phenotype to immunopathogenesis and follow-up.
Overview of sepsis and immune dysregulation
The release of large quantities of proinflammatory cytokines is termed CS and is associated with various infective precipitants and other hyperinflammatory states.9 , 10 Virally associated causes of particular relevance are the 2003 SARS coronavirus (SARS-CoV) infection that infected more than 8000 globally, primarily in Asia and Canada (Toronto) with an 11% mortality rate,11, 12, 13, 14 and the 2012 Middle East respiratory syndrome (MERS) coronavirus (MERS-CoV) with a reported case-fatality rate of 35%.15, 16, 17 Although SARS-CoV-2 belongs to the same Betacoronavirus genus as SARS-CoV and MERS-CoV, the case fatality associated with both SARS-CoV and MERS-CoV significantly exceeds that of SARS-CoV-2 but the number of cases worldwide associated with SARS-CoV and MERS-CoV is much lower.18 Genomic evidence suggests that SARS-CoV and SARS-CoV-2 share the same human cell receptor for host entry, the angiotensin-converting enzyme 2 (ACE2).19 SARS-CoV-2 binds with increased affinity to the ACE2 receptor compared with SARS-CoV, a possible explanation for the widely spread community transmission from asymptomatic hosts.18
The clinical correlates of increased inflammation or CS are persistent hypotension, hypothermia or hyperthermia, and end-organ dysfunction, while the laboratory features include hematological anomalies (leukocytosis or leukopenia, thrombocytopenia, and disseminated intravascular coagulation with high fibrinogen, triglycerides, and ferritin), elevated IL-2R (CD25), elevated IL-6, and general markers of end-organ dysfunction (such as elevated creatinine and deranged liver function tests).10 The CS clinical phenotype is variable and regroups systemic signs of inflammation, multiorgan failure, and mortality.20
The hyperinflammatory state associated with severe viral infection shares significant features with CS, and genetic factors associated with hemophagocytic lymphohistiocytosis (HLH) have been identified, suggesting that these conditions may in fact be part of the same spectrum.21 HLH is caused by an abnormal regulation of activated macrophages and lymphocytes, leading to a hyperinflammatory state.21 IFN-γ is an important cytokine responsible for the organ damage leading to mortality in HLH.20 Other cytokines such as IL-6, TNF-α, IL-1, and IL-18 are also increased during HLH.22 Several genes that play a role in the pathway of natural killer cells and CD8+ T cells have been described as causal for the development of the familial form of HLH. Some examples include the lysosomal trafficking regulator mutation described in the Chediak-Higashi syndrome, the RAB27A mutation in the Griscelli syndrome as well as other mutations in perforin (PRF1). The main clinical and laboratory manifestations of HLH are fever, cytopenia, coagulopathy, liver dysfunction, hyperferritinemia, decreased or absent natural killer–cell function, increased soluble CD25 (IL-2R), and presence of hemophagocytosis on bone marrow biopsy or other organs.21 The secondary form of HLH has been described in influenza during the 2009 H1N1 pandemic, the largest cohort describing 9 cases with a mortality rate of 89% (8 of 9 cases).23 The macrophage activation syndrome (MAS) has similar clinical features to HLH and is considered a related disorder that occurs primarily in patients with rheumatologic diseases.24 The excessive inflammatory response described in MAS is characterized by an increased IL-1β, with successful reports on the use of anakinra, an IL-1 receptor antagonist.25 , 26 In a cohort of 19 adult patients with secondary HLH/MAS, 63.1% (12 of 19) had systemic infections as precipitating causes.27 This group used anakinra in 12 of 19 patients and reported 4 deaths among those patients treated with anakinra.27
The concept of shared immunologic features between HLH, MAS, and CS has been entertained with extensive discussion that these diseases could be part of an overlapping immunopathology with shared but also distinctive triggers and genetic features.20 To assess the possible genetic predisposition of individuals with no past medical history to develop HLH secondary to severe H1N1 influenza, Schulert et al27 performed whole-exome sequencing in 14 patients, 13 of whom had evidence of hemophagocytosis at autopsy, and detected 5 heterozygous variants in lysosomal trafficking regulator (2 of whom also had a heterozygous PRF1 mutation).27
Pediatric multisystem inflammatory syndrome
Children appear protected from SARS-CoV-2 infection and are more likely to be asymptomatic or have less severe infection compared with their adult counterparts.28 , 29 However, more recently, a pediatric multisystem inflammatory syndrome has been described that appears distinct from the adult CS associated with acute SARS-CoV-2 infection and may follow mild or asymptomatic SARS-CoV-2 infection in previously healthy children. This illness has been reported in children aged from early childhood to adolescence, has Kawasaki-like features, and has been reported in areas with a high SARS-CoV-2 prevalence in children exposed to positive COVID-19 family members. In multiple cases, the child had positive SARS-CoV-2 serology but negative SARS-CoV-2 PCR result. Deaths of at least 3 children associated with this syndrome have been reported in the United States and the United Kingdom.8 Children with this syndrome have presented with similar features to Kawasaki disease,29 , 30 with high fever, rash, conjunctivitis, and diarrhea, and shown evidence of myocardial involvement, with elevated troponins, arrhythmia, shock, abnormal echocardiographic vascular findings, and coronary artery aneurysms. They have shown evidence of a hyperinflammatory state with elevated ferritin, triglycerides, and D-dimers. Treatments have included high-dose intravenous immunoglobulin and aspirin, as suggested for Kawasaki disease.30 Currently, the specific immunopathogenic link to SARS-CoV-2 infection and the role of adjunctive immunomodulatory and anticytokine therapy in this syndrome is unknown.
The immunopathogenesis of CS in the setting of a viral respiratory tract infection
The airway epithelium is part of the first line of defense in presence of an airborne viral pathogen recognized as a pathogen-associated molecular pattern and/or damage-associated molecular pattern that bind to pattern recognition receptors such as Toll-like receptors on the surface of macrophages.9 The resident-activated alveolar macrophages, after several intracellular signaling cascades, generate TNF, IL-1β, and IL-6 and trigger a systemic inflammatory response (Fig 1 ).31 This simultaneously prompts a well-coordinated local innate response composed of specific enzymes (defensins, mucins, lysozymes), nitric oxide, reactive oxygen species, platelet-activating factor, and other cytokines.32 Other key components of the innate immunity against viral infection are the type I IFNs. In contrast with findings on the influenza virus, patients with severe COVID-19 patients have minimal peripheral quantities of type I IFNs but increased IFNs and IFN genes in the bronchoalveolar environment, a discovery associated with CS development in a mouse model of SARS-CoV infection.33 Furthermore, in vitro, SARS-CoV-2 failed to produce IFN expression in infected cells,34 indicating a dampened early innate immune response.35
Fig 1.
COVID-19 immunologic mechanisms for CS and the possible role of biologics. When SARS-CoV-2 PAMPs and/or DAMPs bind to TLRs on the surface of resident alveolar macrophages, they become activated and secrete TNF, IL-1β, and IL-6. In increased levels, these cytokines will be the hallmark of the CS responsible for the ARDS and CS in COVID-19. The different targets of biologics are illustrated in the figure. Specifically, the downstream effect of IL-6 can be blocked with tocilizumab, sarilumab, or siltuximab and the effects of IL-1β with anakinra or canakinumab. CD8+ T cells produce IFN-γ, causing direct tissue damage, whereas activated CD4+ T cells, in the presence of transforming growth factor β and IL-6, will differentiate into the TH17-cell subset, responsible for secreting IL-17A and IL-17F, which, among numerous roles, target macrophages, dendritic cells, endothelial cells, and fibroblasts to increase the production of IL-1, IL-6, and TNF. DAMP, Damage-associated molecular pattern; PAMP, pathogen-associated molecular pattern; TLR, Toll-like receptor; TMPRSS2, transmembrane protease, serine 2.
Monocytes and macrophages play a central role and a disruption in the mononuclear phagocyte compartment is considered to increase the COVID-19–related hyperinflammation.36 , 37 Also, an increase in the CD14+CD16+ monocytes producing IL-6 has been noted in the peripheral blood of critically ill patients with COVID-19.38 , 39 Bruton’s tyrosine kinase (BTK), an intracellular kinase, also appears to have a role in monocytes and macrophage activation and specifically in infection clearance by macrophages.40
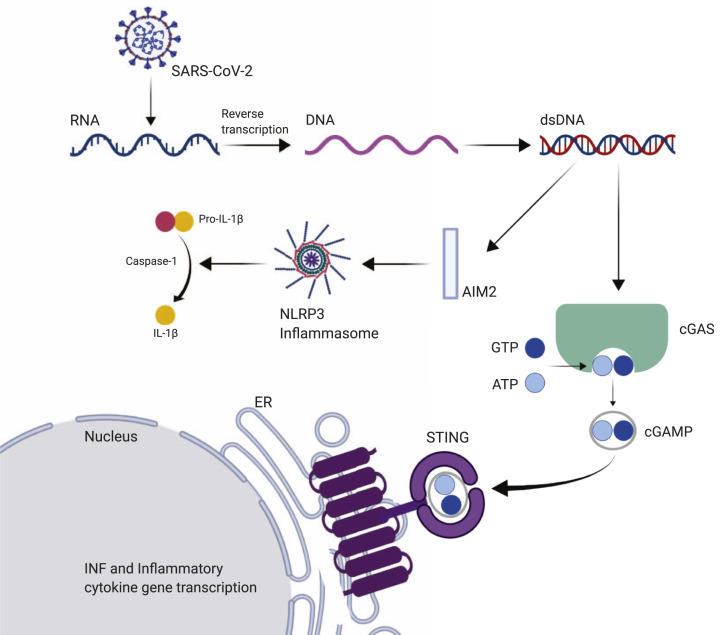
IL-1β is produced after the inflammasome (especially nucleotide-binding and oligomerization domain–, leucine-rich repeats–, and pyrin domain–containing protein 3), activated by absent in melanoma 2–sensing foreign DNA, induces the formation of caspase-1, which cleaves pro–IL-1β into IL-1β (Fig 2 ). In a study using single-cell RNA sequencing in the PBMCs of 10 patients with COVID-19 compared with 5 healthy controls, the authors reported an increased quantity of CD14++ monocytes with inflammatory gene expression and CD14++ IL-1β+ monocytes in the early recovery stages of SARS-CoV-2.41 IL-1β is also implicated in the activity of nuclear factor kappa-light-chain-enhancer of activated B cells, inducing the synthesis of various inflammatory genes of mediators such as IL-6.9 Thus, a reduction in IL-1β activity would reduce IL-6 production.42
Fig 2.
The implications of the STING pathway in coronavirus. The cGAS-STING pathway is activated by sensing foreign cytosolic DNA (obtained after reverse transcription from SARS-CoV-2). cGAS catalyzes the generation of cyclic GMP-AMP (cGAMP), which binds and activates STING in the ER, leading to the expression of IFNs and other cytokines. IL-1β is produced after the NLRP3 inflammasome, activated by AIM2-sensing foreign DNA, induces the formation of caspase-1, which will cleave pro–IL-1β into IL-1β. AIM2, Absent in melanoma 2; AMP, adenosine monophosphate; cGAMP, cyclic GMP-AMP; cGAS, cyclic GMP-AMP synthetase; dsDNA, double-stranded DNA; GMP, guanosine monophosphate; GTP, guanosine triphosphate; ER, endoplasmic reticulum; NLRP3, nucleotide-binding and oligomerization domain–, leucine-rich repeats–, and pyrin domain–containing protein 3.
Following initial escape of the innate response, recognition of virus promotes the migration of pulmonary dendritic cells to the lymph nodes for presentation of antigen to passing T cells for the development of more robust antigen-specific T- and B-cell adaptive response. During this response, soluble mediators play a role in cellular function and signal transduction by binding to specific receptors on the surface of target cells. For example, CD8+ T cells produce excessive amounts of TNF-α and IFN-γ, causing direct tissue damage, whereas activated CD4+ T cells, in the presence of transforming growth factor β and IL-6, will differentiate into TH17-cell subset, important for extracellular pathogen elimination and autoimmunity (Fig 1).43 The defining cytokines secreted by TH17 cells are IL-17A and IL-17F, which primarily target macrophages, dendritic cells, endothelial cells, and fibroblasts to increase the production of IL-1, IL-6, and TNF-α.43 In this particular setting, IL-6 will also inhibit the transforming growth factor β–dependent development of CD4+ regulatory T cells, a critical mediator of immune tolerance with a major role in regulating the effector T-cell response.44
In the setting of CS syndromes, overactivation of effector CD4+ and CD8+ T cells and production of cytokines and chemokines generate an uncontrolled hyperinflammatory injury at the tissue level, resulting in local and distant injury.13 Increased inflammation is associated with peripheral blood lymphopenia, a significant drop in the lymphocyte to neutrophil ratio, and CD4+ T-cell dysfunction in observational studies but the mechanisms for these changes are unclear.38 , 45 , 46 In one of the first studies describing the postmortem pathological findings in 1 patient with COVID-19, peripheral flow cytometry indicated a reduced CD4+ and CD8+ cell count but an increased proportion of activation markers such as HLA-DR and CD38 as well as an increased concentration of TH17 cells.47
Summary statement
Inflammatory cytokines and chemokines, including IL-6, IL-1β, and TNF-α, are significantly elevated in patients with severe SARS-CoV-2 infection, suggesting that CS may play a role in the SARS-CoV-2 severity, morbidity, and mortality.
The pleiotropic role of IL-6 in inflammatory and viral responses
IL-6 is secreted by a plethora of immune and stromal cells including monocytes, macrophages, endothelial cells, B and T cells, hepatocytes, keratinocytes, adipocytes, dendritic cells, and fibroblasts. IL-6 exerts effects on a similarly broad array of cellular targets expressing the functional IL-6 receptor (IL-6R) such as T cells, B cells, vascular endothelial cells, monocytes, and hepatocytes.44 , 48 As may be expected, such diversity of targets translates into functional pleiotropy including the synthesis of acute-phase proteins in the liver, such as C-reactive protein (CRP), which is a surrogate for IL-6; the decreased production of proteins such as albumin; the differentiation of B cells into plasma cells; and hematopoiesis and other metabolic and neurologic processes.44 , 48 CRP is an acute-phase reactant that binds the phospholipid component of microorganisms and damaged cells that is frequently used as a screening marker of infection and/or inflammation.31
IL-6 affects cellular immunity with both proinflammatory and anti-inflammatory functions. IL-6 genetic knockout mice present with varied impairments of inflammatory response including a well-documented increased susceptibility to microbial infection, whereas humans expressing defective IL-6 receptors experience a hyper-IgE syndrome–like disorder that clinically manifests as dermatitis and recurrent (staphylococcal and mycotic) infections, highlighting the important role that IL-6 likely plays in the diverse pathways of IgE-mediated allergy and microbial defense.49
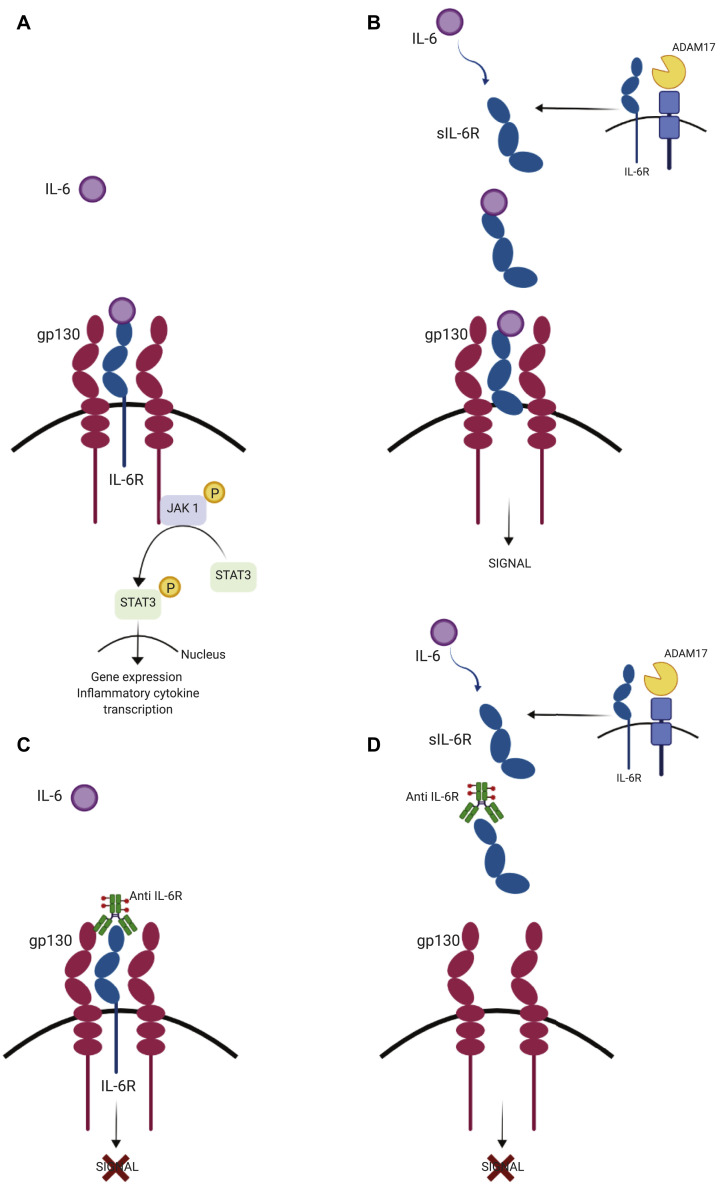
Contrasting inflammatory functions of IL-6 are mediated through its modality of receptor binding. Classical binding of IL-6 to the membrane-bound IL-6 receptor (IL-6R) leads to glycoprotein 130 dimerization, Janus-associated kinase (JAK) 1 signaling, and activation, among others, of the classical RAS/RAF/mitogen-activated protein kinase pathways, leading to anti-inflammatory responses (Fig 3 ).50 Although all human cells display preformed, inactive glycoprotein 130 receptors on their cell surface, this receptor remains inactive without the presence of IL-6R, which is expressed only on certain cell types.51 However, proinflammatory functions have been found to be mediated through binding of soluble IL-6R, termed trans-signaling, with important ramifications for potential therapeutic targeting.52 It has been shown that an important source of soluble IL-6R is shredded from cells undergoing ADAM17-mediated apoptosis, which controls mononuclear phagocyte recruitment, leading to amplified inflammatory response.53 The proinflammatory responses of IL-6 are mediated by trans-signaling, whereas the anti-inflammatory functions are probably realized by classic signaling (Fig 3).50 Selective blockage of this trans-signaling pathway is likely to have the beneficial effect of blocking inflammation without the undesirable off-target effects of broad immune suppression.
Fig 3.
Classic and trans-signaling IL-6R. A and B, Different signaling pathways stimulated by IL-6. Binding of IL-6 to the membrane-bound or soluble IL-6 receptor (IL-6R) leads to gp130 dimerization and JAK 1–STAT 3 signaling and activation, leading to gene expression of inflammatory cytokines. This pathway is represented only in Fig 3, A, and replaced by the word “SIGNAL” in Fig 3, B. A, Classic signaling, which is restricted to several cell types, is initiated through binding of IL-6 to the membrane IL-6R and forms a complex with gp130. B, Trans-signaling is driven by IL-6 in all gp130-expressing cells. Proinflammatory functions have been found to be mediated through binding of soluble IL-6R shredded from cells undergoing ADAM17-mediated apoptosis. C and D, IL-6 blockade therapy using a humanized anti–IL-6R mAb. A humanized anti–IL-6R antibody blocks IL-6–mediated signaling pathway by inhibiting IL-6 binding to the membrane (Fig 3, C) and soluble (Fig 3, D) receptors. ADAM17, A disintegrin and metalloprotease family protein; gp130, glycoprotein 130; IL-6R, IL-6 receptor; sIL-6R, soluble IL-6R; STAT, signal transducer and activator of transcription.
Summary statement
IL-6 has major effects on cellular immunity with both proinflammatory and anti-inflammatory functions.
The role of IL-6 and other mediators in the response to SARS-CoV-2 infection
A multitude of markers for COVID-19 severity have been proposed such as CD4+ and CD8+ T-cell lymphopenia3 , 5 , 54 as well as global lymphopenia. Homing of lymphocytes to the lungs is significantly increased in nonsurvivors compared with survivors.1 A number of publications now highlight that an increase in IL-6 correlates with severe response to SARS-CoV-2, defined as the development of sepsis, ARDS, requirement for mechanical ventilation, and death.1 , 3 , 5 , 7 , 46 , 54, 55, 56 The clinical and immunologic parameters associated with in-hospital mortality in patients with COVID-19 are reported in Table I .57 , 58 The structural N protein of coronaviruses performs an essential role during host cell entry as well as virus particle assembly and release.11 The N protein from SARS-CoV activates the transcription factor nuclear factor kappa-light-chain-enhancer of activated B cells and, subsequently, the expression of IL-6 in human airway epithelial cells, providing a biologically plausible explanation for the role of IL-6 in SARS-CoV-2 infection immune pathogenesis.11
Table I.
Clinical and immunologic parameters associated with in-hospital mortality in COVID-19
| Parameter | Studies |
||||
|---|---|---|---|---|---|
| Zhou et al,1 2020 | Ruan et al,7 2020 | Wu et al,3 2020 | Wang et al,6 2020 | Li et al,57 2020 | |
| Country | China | China | China | China | China |
| Type of study | Retrospective cohort | Retrospective cohort | Retrospective cohort | Retrospective cohort | Retrospective cohort |
| Patients | 191 | 150 | 201 | 33 | 548 |
| Comorbidities∗ | Age > 69 y HTN CAD Diabetes |
Age > 68 y HTN CAD |
Age > 65 y HTN |
NA | Age > 65 y HTN Male |
| Clinical∗ | ↑ SOFA score† > 4.5 | Dyspnea Respiratory failure ARDS AKI Other infection |
Dyspnea | NA | NA |
| Laboratory∗ | Lymphopenia < 0.6 × 109/L Leucopenia < 4 × 109/L ↑ Procalcitonin < 0.1 ng/mL ↑ Creatinine > 133 μmol/L ↑ D-dimer > 1 μg/mL ↑ ALT > 40 U/L ↑ LDH > 245 U/L ↑ Troponin I > 28 pg/mL ↑ CK > 185 U/L ↑ Ferritin > 300 μg/L |
Lymphopenia < 0.6 × 109/L Leucocytosis > 10.6 × 109/L ↑ CRP > 126.6 mg/L ↑ Creatinine > 91.2 μmol/L ↑ Urea > 8.6 μmol/L ↑ Troponin I > 30 pg/mL ↑ Myoglobin > 258.9 ng/mL |
Lymphopenia < 0.6 × 109/L ↑ Urea > 7.4 μmol/L ↑ D-dimer > 3.95 μg/mL ↑ LDH > 484 U/L |
Lymphopenia < 1.1 × 109/L Neutrophilia > 6 × 109/L ↑ Creatinine > 100 μmol/L ↑ Urea > 7.5 μmol/L ↑ D-dimer > 500 μg/L |
Leucocytosis ↑ LDH > 445 U/L |
| IL-6 | Nonsurvivors (N = 54) 11 (7.5-14.4) pg/mL Survivors (N = 137) 6.3 (5.0-7.9) pg/mL |
Nonsurvivors‡ (N = 68) 11.4 ± 8.5 ng/mL Survivors‡ (N = 82) 6.8 ± 3.6 ng/mL (N = 82) |
Nonsurvivors‡ (N = 44) 10.1 (7.4-14.8) pg/L Survivors‡ (N = 117) 6.3 (5.4-7.8) pg/L |
NA | NA |
AKI, Acute kidney injury; ALT, alanine transaminase; CAD, coronary artery disease; CK, creatine kinase; HTN, hypertension; LDH, lactate dehydrogenase; NA, not available; SOFA, Sequential Organ Failure Assessment.
Values are expressed as mean ± SD or mean (interquartile range).
Only statistically significant variables are presented (P < .05).
SOFA score: This score includes multiples parameters such as assessment of respiratory status (partial pressure of oxygen, fraction of inspired oxygen and oxygen saturation), coagulation parameters (platelets), liver function (bilirubin), hypotension, central nervous assessment with Glasgow coma score, and renal function (creatinine).58
The IL-6 units reported in these studies do not compare with the units generally presented. Unfortunately, the method used for measuring IL-6 was not provided.
In a cohort of 60 patients hospitalized with SARS-CoV-2 infection, IL-6 concentrations were 163 ± 153 pg/mL for the group with mild symptoms and 517 ± 796 pg/mL for the patients with severe presentation (intensive care unit admitted).59 A summary of the observations from studies of IL-6 in patients hospitalized with COVID-19 is presented in Table II .1 , 3 , 4 , 7 , 54, 55, 56 , 60 IL-6 may be both a biomarker and a potential therapeutic target for patients hospitalized with COVID-19, which is an attractive concept in the absence of alternative direct-acting antiviral strategies.
Table II.
Review of hospital admission IL-6 values in patients with COVID-19
| Reference | Setting Country |
N | Control∗ (pg/mL) | Cutoff (pg/mL) | Critically ill patients† (pg/mL) | Predictor of complications‡ (pg/mL) | Predictor of mortality‡ (pg/mL) | Method for IL-6 monitoring |
|---|---|---|---|---|---|---|---|---|
| 4 | Hospital Germany |
40 | 19.6 (0-76.5), N = 27 | 80 | NA | 121.0 (19.2-430.0), N = 13 | NA | NA |
| 3§ | Hospital China |
201 | 6.3 (5.4-7.8) pg/L, N = 117 | NA | 6.1 (5.1-6.7) pg/L, N = 40 | 7.4 (5.6-10.9) pg/L, N = 84 | 10.1 (7.4-14.8) pg/L, N = 44 | NA |
| 7§ | Hospital China |
150 | 6.8 ± 3.6 ng/mL, N = 82 | NA | NA | NA | 11.4 ± 8.5 ng/mL, N = 68 | NA |
| 1 | Hospital China |
191 | 6.3 (5.0-7.9), N = 137 | NA | NA | NA | 11.0 (7.5-14.4), N = 54 | NA |
| 55 | Hospital China |
48 | 10.4 (3.8-31.0), N = 21 | 100 | 64 (25.6-111.9), N = 17 | NA | NA | ECLIA (Roche Ltd) |
| 56 | Hospital China |
43 | 10.6 (5.1-24.2), N = 28 | 24.3 | NA | 36.1 (23.0-59.2), N = 17 | NA | ECLIA (Rochecobase601) |
| 60 | Hospital China |
43 | 6.7 (4.4-12.4), N = 36 | NA | NA | 51.7 (34.3-161.7), N = 7 | NA | NA |
| 54 | Hospital China |
53 | 13.4 ± 1.8, N = 45 | NA | 37.8 ± 7.8, N = 18 | NA | NA | FMBA (Qingdao Raisecare Biotechnology Co) |
ECLIA, Electrochemiluminescence method; FMBA, flow cytometer microsphere-based assay; NA, not available.
Values are expressed as mean ± SD or mean (interquartile range). N is the number of patients included in each study.
The “control” IL-6 value represents the patients diagnosed with mild symptoms of COVID-19 included in the studies (no healthy controls included).
Some studies included IL-6 levels dosed after hospital admission and during disease progression.
This value was recorded upon hospital admission and predicted either sepsis or mortality.
The IL-6 units reported in these studies do not match the units generally presented. Unfortunately, the method used for measuring IL-6 was not provided.
Importantly, proposed clinical cutoff values for IL-6 in this setting have started to emerge, with greater than 80 pg/mL determined to predict respiratory failure in a study with 40 patients with COVID-19 in which 13 required medical ventilation4 and greater than 100 pg/mL in patients with detectable serum SARS-CoV-2 nucleic acid was found to correlate with mortality (N = 17 of 48).55 However, other authors have reported specificity at much lower concentrations, with a retrospective study of 43 patients with COVID-19 from China indicating that severe cases could be predicted using an IL-6 value greater than 24.3 pg/mL (sensitivity of 73.3% and specificity of 89.3%).56 Although studies with larger sample sizes are urgently required to determine the true IL-6 cutoff associated with severe disease, intensive care unit admission, and mortality, these initial results are promising. The presented data are limited by their retrospective nature and uncertainty whether IL-6 levels can be ascertained by clinical laboratories in an expedited fashion to guide therapy in real time.
Summary statement
Several recent publications have shown that an increase in the proinflammatory cytokine IL-6 correlates with disease severity, defined as sepsis, ARDS, or mechanical ventilation, and mortality in SARS-CoV-2.
Lessons from IL-6 and other proinflammatory states including sepsis
IL-6 levels are considered to be undetectable, or below 10 pg/mL (with some intertest variability), in healthy controls.12 , 61 , 62 Conversely, mean IL-6 levels at presentation appear highest in severe sepsis (51.4 pg/mL) compared with patients who do not develop severe sepsis (36.5 pg/mL; P < .03) in a study of community-acquired pneumonia.63 This response is highly specific for severe disease, and some studies indicate a role in disease progression, demonstrating up to a 4-fold decrease in IL-6 3 days after initial diagnosis. Moreover, IL-6 values appear to drop abruptly in survivors while remaining higher in nonsurvivor groups.62, 63, 64 Nonetheless, IL-6 currently represents one of the best characterized markers of disease severity and an early rise in IL-6 is associated with sepsis, organ failure, and death.65, 66, 67
Assigning discrete cutoff values for IL-6 to enable its use as a clinical diagnostic tool has remained ill-defined because of variations in the literature. Song et al68 demonstrated in 142 patients that an IL-6 cutoff value of 52.60 pg/mL and 348.9 pg/mL was associated with a diagnostic and prognostic value, respectively, in patients with systemic inflammatory response syndrome.68 In contrast, in another systemic inflammatory response syndrome cohort (N = 177), a cutoff of 75 pg/mL for sepsis and 145 pg/mL for septic shock was defined.64 Thus, even if further clarification is required, the literature demonstrates that elevated IL-6 values are associated with sepsis or septic shock development.62 , 69, 70, 71 This is also supported by a 2016 meta-analysis of 2680 critically ill patients from 22 studies—the use of IL-6 was of moderate diagnostic capacity and relatively high specificity in defining sepsis from other systemic inflammatory response syndrome,72 and, thus, IL-6 may be of utility to confirm infectious causation in patients with complex presentation while considering the limitation in terms of availability of IL-6 levels. The specific IL-6 values from critically ill patients are represented in Table III .12 , 59 , 61, 62, 63, 64, 65 , 68, 69, 70, 71 , 73, 74, 75
Table III.
Literature review of hospital admission IL-6 values in critically ill patients
| Reference | Population/IL-6 dosage technique | Setting Country |
Study design | N | Control∗ (pg/mL) | Cutoff† (pg/mL) | Sepsis ‡ (pg/mL) | Predictor of sepsis§ (pg/mL) | Predictor of mortality (pg/mL) |
|---|---|---|---|---|---|---|---|---|---|
| 12 | Patients with SARS-CoV Detection level NA (CBA) |
Hospital Taiwan |
MCRC | 88 | 7.5 ± 30.4 | NA | 245.7 ± 770.2 | NA | 387.2 ± 911.82 |
| 59 | Patients with SARS-CoV Detection >10 pg/mL (ELISA) |
Hospital China |
SCPC | 228 | 61.0 ± 10.1 | NA | NA | 163 ± 153 517 ± 796 (severe) |
NA |
| 68 | Patients with SIRS, sepsis (S), and septic shock (C) Detection level NA (ELISA) |
ED Korea |
SCPC | 142 | 23.6 (11.2-43.5) | 52.60 (S) 348.9 (C) |
NA | 89.9 (45.2-272.6) (S) 1,378.6 (256.4-11,062.1) (C) |
≥348.92 7,609.5 (4,526.0-12,208.4) (28 d) |
| 70 | Critically ill patients with organ dysfunction Detection level NA (RT) |
ICU Japan |
SCPC | 100 | 104 (46-152) | 152 | NA | 720 (183-7,656) | NA |
| 62 | Patients with severe sepsis Detection level NA (ELISA) |
ED Taiwan |
SCPC | 76 | 32.9 (0-663.5) | NA | NA | 223.4 (3.1-979.1) septic shock | 196.3 (0.5-979.1) |
| 73 | Patients with sepsis Detection level NA (ELISA) |
ICU Finland |
MCPC | 61 | 426 (234-1,000) | NA | NA | NA | 1,000 (269-2,000) |
| 74 | Patients with SIRS Detection level > 9.7 pg/mL (ELISA) |
ICU Malaysia |
SCPC | 239 | 183 (61-358) | 238 (86-3,159) | 1,127 (218-8,643) (30 d) | ||
| 64 | Patients with SIRS Detection level NA (ECLIA) |
ED Korea |
SCPC | 177 | 55.3 ± 100.9 | 75 (sepsis) 145 (shock) |
NA | 900.1 ± 1,643.4 | 1,018.8 |
| 69 | Patients with infection suspicion Detection level NA (ECLIA) |
ED Finland |
SCPC | 539 | 15.3 (1.5-653) | NA | NA | 93.5 (1.5-43 790) | NA |
| 71 | Patients with infection and SIRS Detection level NA (ECLIA) |
ICU Switzerland |
SCPC | 78 | 44.2 | 200 | NA | NA | 1,000 |
| 75 | Patients with major trauma (female vs male) Detection level NA (ELISA) |
ED Germany |
SCPC | 343 | 163.7 ± 25.98 | NA | NA | 363.9 ± 72.58 | NA |
| 61 | Patients with major trauma Detection level > 7.8 pg/mL (ELISA) |
ICU France |
SCPC | 100 | 55.7 (45.9-83.8) | NA | NA | 95.1 (71.3-210.3) | NA |
| 65 | Patients with major trauma Detection level NA (ELISA) |
Trauma unit Switzerland |
SCRC | 1,032 | 282.1 ± 39.8 | NA | NA | 551.6 ± 124.1 | NA |
| 63 | Patients with CAP Detection level > 5.9 pg/mL (ECLIA) |
ED The United States |
MCPC | 1,426 | 38.7 | NA | 98.7 | 51.4 | 109.4 (90 d) |
CBA, Human TH1/TH2 cytokine or chemokine bead array kit; CAP, community-acquired pneumonia; ED, emergency department; ECLIA, electrochemiluminescence method; ICU, intensive care unit; NA, not available; RT, routine testing; SIRS, systemic inflammatory response syndrome.
Types of study design: SCRC, single-center retrospective cohort; SCPC, single-center prospective cohort; MCRC, multicenter retrospective cohort; MCPC, multicenter prospective cohort.
Values are expressed as mean ± SD or mean (interquartile range). N is the number of patients included in each study.
The control group does not include any healthy controls.
The authors calculated a cutoff value that could predict sepsis.
Some studies included IL-6 levels dosed after sepsis diagnostic.
This initial value was recorded on admission to the hospital (ED) or ICU depending on the study and predicted either sepsis or mortality.
Summary statement
As with the development of any novel diagnosis and because increased levels of IL-6 are associated with sepsis and septic shock, clinical cutoffs must be defined.
Lessons from IL-6 response in chimeric antigen receptor T-cell–associated cytokine release syndrome
There are similarities between the immunopathology of sepsis-associated CS and the cytokine release syndrome (CRS), a well-described complication of chimeric antigen receptor T-cell (CAR T-cell) therapy or hematopoietic cell transplantation. Although these terms should not be used interchangeably, CRS was described as part of the CS syndromes.14 The CRS is a cytokine-mediated systemic inflammatory disease that groups signs and symptoms of multiple organ damage ranging from mild constitutional symptoms (grade 1) to end-organ damage (grade 4).23 , 24 Multiple grading systems for CRS have been provided in the literature, and a commonly used one is presented in Table IV . In the case of CRS, the cytokines are released directly by the infused CAR T cells or by other immune cells such as macrophages in response to the cytokines produced by the CAR T cells.25 In some series of CRS, serum IL-6 levels correlated with the activation of potent T lymphocytes and CAR T-cell expansion, predicting subsequent therapeutic response and tumor control.78 , 79 Humanized IL-6R inhibitors such as tocilizumab have been integrated into CAR T-cell treatment protocols to preemptively manage CRS.
Table IV.
Cytokine release storm—Grades and treatment76
| Cytokine release storm: A multiorgan clinical diagnostic involving constitutional, cardiovascular, hematological, gastrointestinal, cutaneous, and neurological manifestations | ||
|---|---|---|
| Grade | Clinical manifestations | Recommended treatment |
| 1: Mild | Patients require symptomatic treatment only Fever ± other constitutional symptoms (no organ dysfunction) |
Supportive care (fluids, antipyretics, analgesics as needed) |
| 2: Moderate | Symptoms respond to moderate intervention Hypoxia (oxygen requirement < 40% FiO2) or hypotension (responsive to IV fluids or low-dose vasopressors) Grade 2 organ toxicity∗ |
Supportive care Cardiac and other organ function monitoring If comorbidities or older age, consider treatment as per grade 3 |
| 3: Severe | Symptoms respond to aggressive intervention Hypoxia (oxygen requirement ≥ 40% FiO2) or hypotension requiring high-dose or multiple vasopressors Grade 3 organ toxicity† or grade 4 transaminitis‡ |
Tocilizumab§ Adults: 4 mg/kg Children: 8 mg/kg Repeat the dose if clinical improvement does not occur within 24-48 h ± low-dose corticosteroids‖ |
| 4: Life-threatening | Requirement for mechanical ventilation or grade 4 organ toxicity‡ (excluding transaminitis) | Tocilizumab ± low-dose corticosteroids‖ |
CTCAE, Common Terminology Criteria for Adverse Events; FiO2, fraction of inspired oxygen; IV, intravenous.
CTCAE grade 2: Moderate; minimal, local, or noninvasive intervention indicated; limiting age-appropriate instrumental activities of daily living.
CTCAE grade 3: Severe or medically significant but not immediately life-threatening; hospitalization or prolongation of hospitalization indicated; disabling; limiting self-care.
CTCAE grade 4: Life-threatening consequences; urgent intervention indicated.
Dose of tocilizumab approved for adults and children with rheumatoid arthritis.
Data concerning the use of steroids in COVID-19 are limited. Please refer to the National Institutes of Health treatment guidelines.77
Role of biological immunotherapies in SARS-CoV-2
Targeting IL-6
The use of biomarkers such as IL-6 and downstream CRP to recognize early the hyperinflammatory state of SARS-CoV-2 infection has been proposed as a trigger point for using immunologic therapies. Importantly, many such immunotherapies are already available for different treatment indications including those that target the IL-6 and IL-6R. Tocilizumab is a humanized anti–IL-6R antibody engineered by grafting the complementarily determining regions of a mouse antihuman IL-6R antibody into a human IgG1κ to create a human antibody with a human IL-6R binding site. Critically for the opposing proinflammatory and anti-inflammatory functions previously discussed, tocilizumab binds to both membrane-bound and soluble IL-6R for total inhibition of IL-6 signal transduction (Fig 3). The main side effects of completely blocking IL-6 signaling are neutropenia, thrombocytopenia, and liver enzyme abnormalities.80 Serious infections have been reported in patients treated long-term with tocilizumab so caution should be used.81 Nonetheless, tocilizumab is Food and Drug Administration (FDA) approved for not only rheumatoid arthritis for which it was originally developed and provides beneficial relief from this largely TH17-driven disease, but, more recently, for severe or life-threatening (grade 3 or 4) CRS associated with CAR T-cell therapy (Table IV) with a dramatic reversal of the clinical manifestations.20 For CRS, initial studies dosed patients at 8 mg/kg and 12 mg/kg infused intravenously over 60 minutes, with up to 3 additional doses if needed (minimum 8 hours between consecutive doses).82 Responders were defined as patients with symptom resolution within 14 days.
Because of the proposed benefits of using tocilizumab in patients with CAR T-cell–induced CRS and the described similarities between CRS and CS following infection, randomized trials are recruiting in COVID-19. In certain centers, tocilizumab has been used in a compassionate access fashion in critically severe patients with COVID-19. A retrospective study from China (N = 21) that used tocilizumab 400 mg intravenous drip (single dose) with or without lopinavir/ritonavir and methylprednisolone demonstrated improvement in fever, hypoxemia, CRP levels, and pulmonary computed tomography imaging, without adverse events.83 The mean CRP levels before the drug were 75.06 ± 66.80 mg/L and decreased to 38.13 ± 54.21 mg/L at day 1, 10.61 ± 13.79 mg/L at day 3, and 2.72 ± 3.60 mg/L at day 5.83 The mean IL-6 level before the first dose of tocilizumab was 132.38 ± 278.54 pg/mL.83 Although follow-up IL-6 levels were not subsequently ascertained in this study, the pretreatment IL-6 concentration aligns with severe disease cutoffs in those studies mentioned earlier. Of immense importance for monitoring, increased serum IL-6 may be expected after initial treatment with tocilizumab.84 Indeed, it is considered that the usual IL-6R–mediated consumption of IL-6 is altered by the bound between tocilizumab and IL-6R and that the IL-6 level during tocilizumab treatment probably reflects disease activity.84 Furthermore, in this study, IL-6 was also significantly increased in 20 healthy volunteers 7 days after a single dose of tocilizumab (3.0 ± 0.6 pg/mL at baseline and 9.3 ± 1.0 pg/mL at day 7).84 Therefore, it is proposed that posttocilizumab use, monitoring of CRP may be a more appropriate assay for monitoring inflammation.44 , 84 A French center has also shared its experience with tocilizumab 8 mg/kg (up to 2 doses) in 30 severe patients with SARS-CoV-2, defined as requiring more than 6 L/min oxygen therapy with rapid changes in oxygen needs (increase of more than 3 L/min in 12 hours) and having a more than 5-day disease diagnosis.85 The authors found that, when compared with a matched control group, the drug decreased the need for mechanical ventilation and intensive care unit admission (23 of 30).85 Finally, in an observational study from the United States, 153 patients with severe COVID-19 (defined as patients requiring supplemental oxygen and critical disease) were treated with an 8 mg/kg intravenous tocilizumab dose (maximum 800 mg). When compared with the nonsevere group, survival rates were similar (P = .11).86
In light of these promising results, the FDA has approved a randomized, double-blind, placebo-controlled phase III clinical trial A Study to Evaluate the Safety and Efficacy of Tocilizumab in Patients With Severe COVID-19 Pneumonia (COVACTA) with 55 locations in North America and Europe. This trial aims to test the efficacy and safety of intravenous tocilizumab in patients with severe SARS-CoV-2 infection (NCT04320615). Similarly, a multicenter, randomized controlled trial was started in China to test the efficacy and safety of tocilizumab in the treatment of patients with COVID-19 pneumonia and elevated IL-6 levels (ChiCTR2000029765). The Italian Regulatory Drug Agency (Agenzia italiana del farmaco; AIFA) has approved a multicenter, single-arm, open-label, phase 2 study (TOCIVID-19) where all the patients will be treated with tocilizumab 8 mg/kg intravenously (up to a maximum of 800 mg per dose), the primary goal being to assess the mortality rate after the first month (EudraCT: 2020-001110-38). There are currently more than 20 registered COVID-19–associated tocilizumab trials (Table V ). A study registered in Greece proposes to individualize immunomodulatory treatment including tocilizumab or anakinra in COVID-19 depending on their cytokine profile (NCT04339712).
Table V.
Potential therapies for COVID-19 ARDS and CS
| Name | Commercial name | Target | Role | FDA indications | Trials Country |
Planned clinical trials |
|---|---|---|---|---|---|---|
| Tocilizumab | Actemra RoActemra |
Membrane or soluble IL-6R | Inhibits IL-6 signal transduction | CRS Rheumatoid arthritis Giant cell arteritis Juvenile idiopathic arthritis |
COVACTA-the United States Italy Spain France Belgium Greece Switzerland Denmark Malaysia China |
NCT04320615 NCT04356937 NCT04331795 NCT04346355 NCT04332913 NCT04317092 NCT04315480 NCT04335305 NCT04332094 NCT04331808 NCT04330638 NCT04339712 NCT04335071 NCT04322773 NCT04345445 NCT04310228 NCT04306705 |
| Sarilumab | Kevzara | Membrane or soluble IL-6R | Inhibits IL-6 signal transduction | Rheumatoid arthritis | International The United States Canada France Spain Denmark |
NCT04327388 NCT04315298 NCT04321993 NCT04324073 NCT04357808 NCT04357860 NCT04322773 NCT04345289 |
| Siltuximab | Sylvant | IL-6 | Inhibits IL-6 signal transduction | Multicentric Castleman disease | Italy Spain Belgium |
NCT04322188 NCT04329650 NCT04330638 |
| Anakinra | Kineret | Type 1 IL-1 receptor | Inhibits IL-1α and IL-1β signal transduction | Rheumatoid arthritis NOMID |
The United States Italy Greece France |
NCT04362111 NCT04324021 NCT04339712 NCT04357366 NCT04341584 |
| Canakinumab | Ilaris | IL-1β | Blocking IL-1β interaction with IL-1 receptors | Periodic fever syndromes Juvenile idiopathic arthritis |
Italy | NCT04348448 |
| Ruxolitinib | Jakafi Jakavi |
JAK1, JAK2 inhibitor | Inhibits cytokine-induced STAT phosphorylation | Myelofibrosis Polycythemia Vera Acute graft-versus-host disease |
The United States Canada Mexico Germany Spain |
NCT04354714 NCT04348071 NCT04331665 NCT04334044 NCT04359290 NCT04348695 |
| Tofacitinib | Xeljanz | JAK1, JAK2, JAK3, TYK2 inhibitor | Inhibits cytokine-induced STAT phosphorylation | Rheumatoid arthritis Psoriatic arthritis Ulcerative colitis |
Italy | NCT04332042 |
| Baricitinib | Olumiant | JAK2 (JAK 1/3, TYK2), AAK1 inhibitor | Inhibits cytokine-induced STAT phosphorylation | Rheumatoid arthritis | The United States Canada Italy |
NCT04340232 NCT04321993 NCT04320277 |
| Fedratinib | Inrebic | JAK2, FLT3, and BRD4 inhibitor | Inhibits cytokine-induced STAT phosphorylation | Myelofibrosis | None | None |
| Acalabrutinib | Calquence | BTK | Inhibits BTK signaling/B-cell activation | Mantle cell lymphoma Chronic lymphocytic leukemia Small lymphocytic lymphoma |
The United States Europe |
NCT04380688 NCT04346199 |
| Eculizumab | Soliris | Complement protein C5 | Inhibits C5 cleavage to C5a and C5b (prevents formation of C5b-9) | Paroxysmal nocturnal hemoglobinuria (PNH) | The United States France |
NCT04288713 NCT04346797 NCT04355494 |
| Ravulizumab | Ultomiris | Complement protein C5 | Inhibits C5 cleavage to C5a and C5b (prevents formation of C5b-9) | Paroxysmal nocturnal hemoglobinuria (PNH) | The United States |
NCT04369469 NCT04390464 |
| Emapalumab | Gamifant | IFN-γ | Binds to and neutralizes IFN-γ | Primary HLH | Italy | NCT04324021 |
| Adalimumab | Humira | TNF-α | Inhibits TNF-α signal transduction | Rheumatoid arthritis Psoriatic arthritis Ankylosing spondylitis Crohn disease Ulcerative colitis Plaque psoriasis Hidradenitis suppurativa |
China | ChiCTR2000030089 |
| Secukinumab | Cosentyx | IL-17A | Inhibits IL-17A signal transduction (via IL-17 receptor) | Psoriatic arthritis Ankylosing spondylitis Plaque psoriasis |
None | None |
AAK1, AP2-associated protein kinase 1; BRD4, bromodomain-containing protein 4; FLT3, fms-like tyrosine kinase 3; NOMID, neonatal-onset multisystem inflammatory; STAT, signal transducer and activator of transcription; TYK2, tyrosine kinase 2.
Sarilumab, an mAb to IL-6 receptor, is also being investigated in COVID-19 trials. A French multicenter randomized controlled trial (Cohort Multiple Randomized Controlled Trials Open-label of Immune Modulatory Drugs and Other Treatments in COVID-19 Patients - Sarilumab Trial; CORIMUNO-SARI) aiming to assess the efficacity and safety of sarilumab versus standard of care is ongoing (NCT04324073). Two additional industry-driven clinical trials (NCT04315298 and NCT04327388) aiming to assess the efficacy and safety of sarilumab in patients hospitalized with COVID-19 are recruiting. Although the clinical outcome data for sarilumab are lacking, the comparative response with tocilizumab will be of interest given the longer half-life of sarilumab and greater affinity for the IL-6R.80
Siltuximab, a chimeric mAb targeting IL-6 directly and preventing binding to both soluble and membrane-bound IL-6 receptors, is FDA approved for the multicentric Castleman disease.87 There are currently 3 European trials recruiting patients diagnosed with COVID-19 (NCT04322188, NCT04329650, and NCT04330638).
Targeting IL-1β
IL-1β leads to an increase in body temperature, lung inflammation, and fibrosis.36 Increased levels of IL-1β were noted in patients diagnosed with SARS-CoV88 and similar to IL-6, were associated with increased mortality in sepsis.9 Anakinra is a nonglycosylated human decoy IL-1 receptor antagonist (IL-1Ra) that binds to the type 1 IL-1 receptor and inhibits IL-1α and IL-1β signal transduction.89 This drug is FDA approved for rheumatoid arthritis and neonatal-onset multisystem inflammatory disease90 and suggested in the treatment algorithm for secondary HLH/MAS.91
A recent study found that the serum IL-1β levels were undetectable in 100% (N = 17) of the patients with severe or moderate SARS-CoV-2 infection,5 an expected result considering the mechanism of action of this exocrine cytokine. Anakinra was used in a cohort from Italy to treat 29 adult patients diagnosed with COVID-19–related moderate to severe ARDS and hyperinflammation (defined as serum CRP ≥100 mg/L, ferritin ≥900 ng/mL, or both).92 Survival was 90% compared with 56% in a standard treatment group (N = 16) (P = .009).92 Other improvements included a reduction in CRP and a decrease in mechanical ventilation use. Posttreatment inflammatory relapse was not reported and the treatment was well tolerated.92
Furthermore, the post hoc analysis of a phase III randomized controlled trial studying the use of anakinra in severe sepsis indicated a significant improvement in survival of patients with sepsis with features of MAS in the absence of any severe adverse reactions.26 CORIMUNO-ANA is a trial that aims to determine the efficacy of anakinra in SARS-CoV-2–infected patients (NCT04341584). Anakinra will be administered twice daily as decreasing doses of intravenous infusions (400 mg on day 1, 2, and 3; 200 mg on day 4; and 100 mg on day 5). Canakinumab is a human anti–IL-1β mAb that blocks IL-1β interaction with the IL-1 receptor for which there is currently 1 registered observational study (NCT04348448).
Targeting TNF-α and IFN-γ
Similar to IL-1β, TNF-α has a direct role in acute systemic inflammation and is increased in patients with severe SARS-CoV-2 infection.2 , 5 , 57 However, this finding is not consistent among the different studies.54 Besides the observational reports that indicate an increase in the levels of this cytokine, a direct pathogenic mechanism of cellular viral entry involving the shedding of the coronavirus’ functional receptor, the ACE2, was studied. This process of binding and shedding of the ACE2 is coupled with TNF-α production and the production of a TNF-α–converting enzyme.93 Thus, it has been suggested that an anti-TNF drug could not only inhibit TNF-α directly but also downregulate the expression and shedding of ACE2. Also, some studies showed a decrease in sepsis-related mortality with anti-TNF treatment.9
There are multiple commercialized anti-TNF biologics. Adalimumab is a recombinant human IgG1 mAb that specifically binds to human TNF-α and blocks its interaction with the p55 and p75 cell-surface TNF receptors. This drug could be potentially useful in managing severe COVID-19 manifestations. To analyze the benefits of an anti–TNF-α treatment in COVID-19, a randomized controlled trial of adalimumab injection in severe patients with COVID-19 has been registered (ChiCTR2000030089).
Similar to TNF, the major proinflammatory cytokine IFN-γ is also increased in the CS associated with COVID-19. IFN-γ was particularly well described in patients with SARS-CoV12 and may be targeted by emapalumab for which a comparative multicenter randomized clinical trial is also underway in combination with anakinra (NCT04324021).
Targeting IL-17
Another cytokine that could have a role in the CS caused by COVID-19 is IL-17. This was not a cytokine of interest in the recent SARS-CoV-2 studies, and the only study that characterized IL-17 in COVID-19 found normal levels using a flow cytometry method.54
As described in this review, IL-17 stimulates the production of proinflammatory cytokines such as IL-1β, IL-6, and TNF-α. Secukinumab is a human IgG1κ mAb that binds to IL-17A (inhibits the interaction with the IL-17 receptor) and is currently used for plaque psoriasis and several rheumatological conditions.94 The further rational for inhibiting IL-17 is that it is a proximal target to IL-1 and IL-6 and, hence, could reduce neutrophil recruitment to the lungs and prevent organ dysfunction in ARDS. To our knowledge, there are no ongoing trials involving this drug.
Targeting JAK
Targeting the TH17 pathway, research on murine models showed promising results with the use of fedratinib, a JAK2 inhibitor. In this study, the drug decreased the expression of IL-17. Because IL-6 and IL-23 are signals for TH17 cell initial differentiation and effector function through the JAK2-signal transducer and activator of transcription 3 pathway, the use of this inhibitor could decrease the proinflammatory function of TH17.95 This drug is currently FDA approved for myelofibrosis.96 To our knowledge, there are no current registered trials involving this drug.
As mentioned, the cell-surface ACE2 receptor is needed for coronavirus endocytosis, and one of the regulators of this process is the AP2-associated protein kinase 1, part of the numb-associated kinase family.97 AP2-associated protein kinase 1 inhibitors have been shown to prevent virus infections by disrupting viral cell invasion. Baricitinib is an oral JAK inhibitor (JAK1/JAK2, JAK1/JAK3, JAK1/tyrosine kinase 2, and JAK2/tyrosine kinase 2) but also an AP2-associated protein kinase 1 inhibitor, having direct antiviral activity, that is currently FDA approved for rheumatoid arthritis resistant to anti-TNF drugs.98 Several trials are ongoing to confirm its safety and efficacy, and it is also being investigated in combination therapy with remdesivir (NCT04340232, NCT04321993, and NCT04320277). Remdesivir, an adenosine analogue with demonstrated antiviral activity against a broad range of RNA virus families, has been used in a randomized placebo-controlled trial showing a decrease in time to recovery (15 vs 11 days) and a trend toward decrease in mortality.99 This drug gained an FDA approval for use in children and adults with severe COVID-19.
Ruxolitinib is a JAK1 and JAK2 inhibitor that mediates the signaling of numerous cytokines such as IL-6, IFN-γ, and growth factors with essential roles in immune function and hematopoiesis. This drug is FDA approved for myelofibrosis, hydroxyurea-resistant polycythemia vera, and steroid-refractory acute graft-versus-host disease.100 A multicenter, single-blinded, randomized trial (1:1) of 44 patients with COVID-19 showed a tendency (not statistically significant) toward improvement in clinical outcomes in the ruxolitinib group.101 Several larger clinical trials from North American and Europe are ongoing (Table V).
Another attractive drug is tofacitinib, which has been shown to inhibit the in vitro activity of JAK1/JAK2, JAK1/JAK3, and JAK2/JAK2 and thus decrease the related cytokines. According to the FDA, it can be used for rheumatoid arthritis, psoriatic arthritis, and ulcerative colitis.81 There is a planned Italian trial that aims to assess the advantage of early administration of tofacitinib in SARS-CoV-2–related interstitial pneumonia (NCT04332042).
Serious bacterial, mycobacterial, fungal, and viral infections have been reported with the use of JAK inhibitors. This potential off-target effect of these drugs combined with the decreased IFN innate response can lead to severe complications, and caution should be used in the SARS-CoV-2 context with theoretical benefit for the anti-JAK molecules that have more specific targets.
Other targeted immunomodulatory therapies and combination therapies
As described, the production of cytokines and chemokines by macrophages is regulated by the BTK. Thus, inhibition of this protein could be a promising strategy for reducing COVID-19–related complications, with therapeutic inhibition of BTK in patients with lymphoid malignancies resulting in decreased proinflammatory cytokines.
Company-sponsored trials with acalabrutinib, a small-molecule inhibitor of BTK enzymatic activity, that aim to study its efficacy and safety compared with best supportive care in hospitalized patients with COVID-19 are currently listed and will begin recruitment shorty in the United States and Europe (Table V).
By sensing self or pathogenic cytosolic double-stranded DNA, the cyclic guanosine monophosphate-adenosine monophosphate synthetase stimulator of IFN genes (STING) plays an important role in innate immunity and tumor development.102 STING is expressed in T cells, monocytes, natural killer cells, and dermal fibroblasts, and cyclic guanosine monophosphate-adenosine monophosphate synthetase-STING signaling promotes the production of IL-6 and the downstream activation of signal transducer and activator of transcription 3.102 The STING–IFN-β pathway is triggered by the binding of cyclic guanosine monophosphate-adenosine monophosphate synthetase to STING, which leads to IFN regulatory factor 3 phosphorylation and subsequent transcription of the gene encoding IFN-β.103 The JAK receptors and their specific pathways are activated by the IFN-β binding to its receptor. The regulation of STING and other proinflammatory cytokine genes is also achieved with the synthesis and release of IFNs. Thus, this proinflammatory loop can be obstructed by JAK inhibition.103
Combination therapy with lopinavir-ritonavir, ribavirin, and IFN-β-1b compared with lopinavir-ritonavir monotherapy was evaluated in an intention-to-treat multicenter, randomized phase 2 clinical trial from China. The primary end point was the time before a negative nasopharyngeal swab (RT-PCR) in patients with SARS-CoV-2, with the median time reported for the combination group (N = 86) being 7 days and the time in the control group (N = 41) being 12 days (P = .0010).104 Anti-Coronavirus Therapies COVID-19 is a clinical trial that aims to evaluate the combination of chloroquine and azithromycin with subcutaneous injection of IFN-β1b for SARS-CoV-2 prevention by assessing admission to intensive care, mechanical ventilation, and/or death (NCT04324463).
The complement system is also a potential therapeutic target in SARS-CoV-2 infection. Complement is key to the innate immune response to all viruses, and complement inhibition is a potential treatment for severe SARS-CoV-2 infection by reducing the severity and end-organ consequences of the innate immune response.105 , 106 A recent mouse model suggested that complement activation through C3 exacerbates SARS-CoV–associated ARDS and that C3-deficient mice infected with SARS-CoV showed less respiratory decline.107 Lung biopsy samples from patients with SARS-CoV-2–associated ARDS showed evidence of complement activation with C3 fragment deposition and associated increased serum 5a levels.105 However, there is little clinical data on the potential role of complement activation and its role in ARDS associated with SARS-CoV-2. There are now several proposed and ongoing studies examining the role of C5 inhibitors such as eculizumab and ravulizumab (Table V).
Convalescent plasma
Given the lack of evidence-based treatment and the novelty of this disease, CP has re-emerged as an emergency intervention passive immunization strategy aiming to decrease morbidity and mortality in critically ill patients with COVID-19.108 , 109 This treatment has been shown to be favorable during the SARS-CoV infection with a decrease in hospital stays and mortality compared with controls.110 , 111 Also, a recent systematic review, while acknowledging the limited data, indicated that CP is safe and clinically effective and can play a role in reducing mortality.112 The described mechanisms of action are direct neutralization of the virus aimed at the spike viral protein113 , 114 as well as other immunomodulatory and anti-inflammatory functions such as neutralization of cytokines, complement, and autoantibodies.108 A clinical report on the use of CP in critically ill patients with SARS-CoV-2 showed a hypothetical benefit with decrease in body temperature, increase in respiratory function, and ARDS resolution in 4 of the 5 patients included.114 In an open-label, multicenter, randomized clinical trial from China, adding convalescent plasma to the treatment plan did not result in increased clinical recovery.115 Several questions remain unanswered regarding CP, and there is a need for larger randomized controlled trials to answer these questions, but emerging successful reports related with its use in severe COVID-19 highlight the intense inflammatory response that accompanies this infection.
Summary statement
Clinical trials are urgently warranted to evaluate a therapeutic strategy targeting upstream and downstream pathways in SARS-CoV-2. The effective dose and the ideal administration timing of the immunomodulatory drugs remain under investigation.
Conclusions
Severe SARS-CoV-2 infection is associated with CS producing a hyperinflammatory state and a clinical and laboratory picture similar to hemophagocytic lymphohistiocytosis that typically occurs 7 to 10 days after the onset of acute illness. In this setting, IL-6 levels correlate with respiratory failure, poor outcomes, and mortality. Blocking this and other appealing cytokines and signaling pathways at an early stage shows promise to target specific and undesirable immune responses in the setting of acute SARS-CoV-2 infection. Currently, studies examining the combination of direct antiviral agents with immunomodulatory therapy are ongoing and will be important in the quest to prevent acute respiratory deterioration, ventilation use, morbidity, and mortality from SARS-CoV-2 infection.
Acknowledgments
We thank Al Chorfi for graphic design work and Austin Health Sciences Library for access to the medical literature.
Footnotes
E.J.P. receives support from National Institutes of Health grants 1P50GM115305, R21AI139021, 1 R01 HG010863, and 1R01AI152183.
Appendix
References
- 1.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu C., Chen X., Cai Y., Xia J., Zhou X., Xu S., et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180:1–11. doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Herold T, Jurinovic V, Arnreich C, Hellmuth J, von Bergwelt-Baildon M, Klein M, et al. Level of IL-6 predicts respiratory failure in hospitalized symptomatic COVID-19 patients [published online ahead of print April 10, 2020]. medRxiv. 10.1101/2020.04.01.20047381. [DOI]
- 5.Chen G., Wu D., Guo W.Z., Cao Y., Huang D., Wang H., et al. Clinical and immunologic features in severe and moderate coronavirus disease 2019. J Clin Investig. 2020;130:2620–2629. doi: 10.1172/JCI137244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ruan Q., Yang K., Wang W., Jiang L., Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46:846–848. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Riphagen S., Gomez X., Gonzalez-Martinez C., Wilkinson N., Theocharis P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet. 2020;395:1607–1608. doi: 10.1016/S0140-6736(20)31094-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chousterman B.G., Swirski F.K., Weber G.F. Cytokine storm and sepsis disease pathogenesis. Semin Immunopathol. 2017;39:517–528. doi: 10.1007/s00281-017-0639-8. [DOI] [PubMed] [Google Scholar]
- 10.Tisoncik J.R., Korth M.J., Simmons C.P., Farrar J., Martin T.R., Katze M.G. Into the eye of the cytokine storm. Microbiol Mol Biol Rev. 2012;76:16–32. doi: 10.1128/MMBR.05015-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang X., Wu K., Wang D., Yue X., Song D., Zhu Y., et al. Nucleocapsid protein of SARS-CoV activates interleukin-6 expression through cellular transcription factor NF-kappaB. Virology. 2007;365:324–335. doi: 10.1016/j.virol.2007.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huang K.J., Su I.J., Theron M., Wu Y.C., Lai S.K., Liu C.C., et al. An interferon-gamma-related cytokine storm in SARS patients. J Med Virol. 2005;75:185–194. doi: 10.1002/jmv.20255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Channappanavar R., Perlman S. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Semin Immunopathol. 2017;39:529–539. doi: 10.1007/s00281-017-0629-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Jong M.D., Simmons C.P., Thanh T.T., Hien V.M., Smith G.J., Chau T.N., et al. Fatal outcome of human influenza A (H5N1) is associated with high viral load and hypercytokinemia. Nat Med. 2006;12:1203–1207. doi: 10.1038/nm1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Choi W.S., Kang C.I., Kim Y., Choi J.P., Joh J.S., Shin H.S., et al. Clinical presentation and outcomes of Middle East respiratory syndrome in the Republic of Korea. Infect Chemother. 2016;48:118–126. doi: 10.3947/ic.2016.48.2.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saad M., Omrani A.S., Baig K., Bahloul A., Elzein F., Matin M.A., et al. Clinical aspects and outcomes of 70 patients with Middle East respiratory syndrome coronavirus infection: a single-center experience in Saudi Arabia. Int J Infect Dis. 2014;29:301–306. doi: 10.1016/j.ijid.2014.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Azhar E.I., Hui D.S.C., Memish Z.A., Drosten C., Zumla A. The Middle East respiratory syndrome (MERS) Infect Dis Clin North Am. 2019;33:891–905. doi: 10.1016/j.idc.2019.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Petrosillo N., Viceconte G., Ergonul O., Ippolito G., Petersen E. COVID-19, SARS and MERS: are they closely related? Clin Microbiol Infect. 2020;26:729–734. doi: 10.1016/j.cmi.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wan Y., Shang J., Graham R., Baric R.S., Li F. Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS coronavirus. J Virol. 2020;94 doi: 10.1128/JVI.00127-20. e00127-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Behrens E.M., Koretzky G.A. Review: cytokine storm syndrome: looking toward the precision medicine era. Arthritis Rheumatol. 2017;69:1135–1143. doi: 10.1002/art.40071. [DOI] [PubMed] [Google Scholar]
- 21.Filipovich A., McClain K., Grom A. Histiocytic disorders: recent insights into pathophysiology and practical guidelines. Biol Blood Marrow Transplant. 2010;16:S82–S89. doi: 10.1016/j.bbmt.2009.11.014. [DOI] [PubMed] [Google Scholar]
- 22.Schulert G.S., Grom A.A. Macrophage activation syndrome and cytokine-directed therapies. Best Pract Res Clin Rheumatol. 2014;28:277–292. doi: 10.1016/j.berh.2014.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beutel G., Wiesner O., Eder M., Hafer C., Schneider A.S., Kielstein J.T., et al. Virus-associated hemophagocytic syndrome as a major contributor to death in patients with 2009 influenza A (H1N1) infection. Crit Care. 2011;15:R80. doi: 10.1186/cc10073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schulert G.S., Grom A.A. Pathogenesis of macrophage activation syndrome and potential for cytokine- directed therapies. Annu Rev Med. 2015;66:145–159. doi: 10.1146/annurev-med-061813-012806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miettunen P.M., Narendran A., Jayanthan A., Behrens E.M., Cron R.Q. Successful treatment of severe paediatric rheumatic disease-associated macrophage activation syndrome with interleukin-1 inhibition following conventional immunosuppressive therapy: case series with 12 patients. Rheumatology (Oxford) 2011;50:417–419. doi: 10.1093/rheumatology/keq218. [DOI] [PubMed] [Google Scholar]
- 26.Shakoory B., Carcillo J.A., Chatham W.W., Amdur R.L., Zhao H., Dinarello C.A., et al. Interleukin-1 receptor blockade is associated with reduced mortality in sepsis patients with features of macrophage activation syndrome: reanalysis of a prior phase III trial. Crit Care Med. 2016;44:275–281. doi: 10.1097/CCM.0000000000001402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schulert G.S., Zhang M., Fall N., Husami A., Kissell D., Hanosh A., et al. Whole-exome sequencing reveals mutations in genes linked to hemophagocytic lymphohistiocytosis and macrophage activation syndrome in fatal cases of H1N1 influenza. J Infect Dis. 2016;213:1180–1188. doi: 10.1093/infdis/jiv550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gudbjartsson D.F., Helgason A., Jonsson H., Magnusson O.T., Melsted P., Norddahl G.L., et al. Spread of SARS-CoV-2 in the Icelandic population. N Engl J Med. 2020;382:2302–2315. doi: 10.1056/NEJMoa2006100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Deza Leon M.P., Redzepi A., McGrath E., Abdel-Haq N., Shawaqfeh A., Sethuraman U., et al. COVID-19 associated pediatric multi-system inflammatory syndrome. J Pediatric Infect Dis Soc. 2020;9:407–408. doi: 10.1093/jpids/piaa061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jones V.G., Mills M., Suarez D., Hogan C.A., Yeh D., Segal J.B., et al. COVID-19 and Kawasaki disease: novel virus and novel case. Hosp Pediatr. 2020;10:537–540. doi: 10.1542/hpeds.2020-0123. [DOI] [PubMed] [Google Scholar]
- 31.Faix J.D. Biomarkers of sepsis. Crit Rev Clin Lab Sci. 2013;50:23–36. doi: 10.3109/10408363.2013.764490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chalmers S., Khawaja A., Wieruszewski P.M., Gajic O., Odeyemi Y. Diagnosis and treatment of acute pulmonary inflammation in critically ill patients: the role of inflammatory biomarkers. World J Crit Care Med. 2019;8:59–71. doi: 10.5492/wjccm.v8.i5.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Acharya D., Liu G., Gack M.U. Dysregulation of type I interferon responses in COVID-19. Nat Rev Immunol. 2020;20:397–399. doi: 10.1038/s41577-020-0346-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chu H, Chan JF, Wang Y, Yuen TT, Chai Y, Hou Y, et al. Comparative replication and immune activation profiles of SARS-CoV-2 and SARS-CoV in human lungs: an ex vivo study with implications for the pathogenesis of COVID-19 [published online ahead of print April 9, 2020]. Clin Infect Dis. https://doi.org/10.1093/cid/ciaa410. [DOI] [PMC free article] [PubMed]
- 35.O’Brien TR, Thomas DL, Jackson SS, Prokunina-Olsson L, Donnelly RP, Hartmann R. Weak Induction of interferon expression by SARS-CoV-2 supports clinical trials of interferon lambda to treat early COVID-19 [published online ahead of print April 17, 2020]. Clin Infect Dis. https://doi.org/10.1093/cid/ciaa453. [DOI] [PMC free article] [PubMed]
- 36.Mehta P., McAuley D.F., Brown M., Sanchez E., Tattersall R.S., Manson J.J., et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Merad M, Martin JC. Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages [published online ahead of print May 6, 2020]. Nat Rev Immunol. https://doi.org/10.1038/s41577-020-0331-4. [DOI] [PMC free article] [PubMed]
- 38.Zhou Y, Fu B, Zheng X, Wang D, Zhao C, Qi Y, et al. Pathogenic T cells and inflammatory monocytes incite inflammatory storm in severe COVID 19 patients [published online ahead of print March 13, 2020]. Natl Sci Rev. https://doi.org/10.1093/nsr/nwaa041. [DOI] [PMC free article] [PubMed]
- 39.Zhang D, Guo R, Lei L, Liu H, Wang Y, Wang Y, et al. COVID-19 infection induces readily detectable morphological and inflammation-related phenotypic changes in peripheral blood monocytes, the severity of which correlate with patient outcome [published online ahead of print March 26, 2020]. medRxiv. 10.1101/2020.03.24.20042655. [DOI]
- 40.Weber A.N.R., Bittner Z., Liu X., Dang T.M., Radsak M.P., Brunner C. Bruton’s tyrosine kinase: an emerging key player in innate immunity. Front Immunol. 2017;8:1454. doi: 10.3389/fimmu.2017.01454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wen W., Su W., Tang H., Le W., Zhang X., Zheng Y., et al. Immune cell profiling of COVID-19 patients in the recovery stage by single-cell sequencing. Cell Discov. 2020;6:31. doi: 10.1038/s41421-020-0168-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dinarello C.A. Interleukin-1 in the pathogenesis and treatment of inflammatory diseases. Blood. 2011;117:3720–3732. doi: 10.1182/blood-2010-07-273417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Miossec P., Korn T., Kuchroo V.K. Interleukin-17 and type 17 helper T cells. N Engl J Med. 2009;361:888–898. doi: 10.1056/NEJMra0707449. [DOI] [PubMed] [Google Scholar]
- 44.Tanaka T., Kishimoto T. The biology and medical implications of interleukin-6. Cancer Immunol Res. 2014;2:288–294. doi: 10.1158/2326-6066.CIR-14-0022. [DOI] [PubMed] [Google Scholar]
- 45.Pedersen S.F., Ho Y.C. SARS-CoV-2: a storm is raging. J Clin Invest. 2020;130:2202–2205. doi: 10.1172/JCI137647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Diao B, Wang C, Tan Y, Chen X, Liu Y, Ning L, et al. Reduction and functional exhaustion of T cells in patients with coronavirus disease 2019 (COVID-19) [published online ahead of print May 1, 2020]. medRxiv. https://doi.org/10.3389/fimmu.2020.00827. [DOI] [PMC free article] [PubMed]
- 47.Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C., et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Uciechowski P., Dempke W.C.M. Interleukin-6: a masterplayer in the cytokine network. Oncology. 2020;98:131–137. doi: 10.1159/000505099. [DOI] [PubMed] [Google Scholar]
- 49.Spencer S., Kostel Bal S., Egner W., Lango Allen H., Raza S.I., Ma C.A., et al. Loss of the interleukin-6 receptor causes immunodeficiency, atopy, and abnormal inflammatory responses. J Exp Med. 2019;216:1986–1998. doi: 10.1084/jem.20190344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Scheller J., Chalaris A., Schmidt-Arras D., Rose-John S. The pro- and anti-inflammatory properties of the cytokine interleukin-6. Biochim Biophys Acta. 2011;1813:878–888. doi: 10.1016/j.bbamcr.2011.01.034. [DOI] [PubMed] [Google Scholar]
- 51.Adam N., Rabe B., Suthaus J., Grotzinger J., Rose-John S., Scheller J. Unraveling viral interleukin-6 binding to gp130 and activation of STAT-signaling pathways independently of the interleukin-6 receptor. J Virol. 2009;83:5117–5126. doi: 10.1128/JVI.01601-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Scheller J., Ohnesorge N., Rose-John S. Interleukin-6 trans-signalling in chronic inflammation and cancer. Scand J Immunol. 2006;63:321–329. doi: 10.1111/j.1365-3083.2006.01750.x. [DOI] [PubMed] [Google Scholar]
- 53.Schumacher N., Rose-John S. ADAM17 activity and IL-6 trans-signaling in inflammation and cancer. Cancers (Basel) 2019;11 doi: 10.3390/cancers11111736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wan S, Yi Q, Fan S, Lv J, Zhang X, Guo L, et al. Characteristics of lymphocyte subsets and cytokines in peripheral blood of 123 hospitalized patients with 2019 novel coronavirus pneumonia (NCP) [published online ahead of print February 12, 2020]. medRxiv. 10.1101/2020.02.10.20021832. [DOI]
- 55.Chen X, Zhao B, Qu Y, Chen Y, Xiong J, Feng Y, et al. Detectable serum SARS-CoV-2 viral load (RNAaemia) is closely associated with drastically elevated interleukin 6 (IL-6) level in critically ill COVID-19 patients [published online ahead of print March 3, 2020]. medRxiv. 10.1101/2020.02.29.2002952. [DOI]
- 56.Gao Y., Li T., Han M., Li X., Wu D., Xu Y., et al. Diagnostic utility of clinical laboratory data determinations for patients with the severe COVID-19. J Med Virol. 2020;92:791–796. doi: 10.1002/jmv.25770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Li X., Xu S., Yu M., Wang K., Tao Y., Zhou Y., et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol. 2020;146:110–118. doi: 10.1016/j.jaci.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jones A.E., Trzeciak S., Kline J.A. The sequential organ failure assessment score for predicting outcome in patients with severe sepsis and evidence of hypoperfusion at the time of emergency department presentation. Crit Care Med. 2009;37:1649–1654. doi: 10.1097/CCM.0b013e31819def97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhang Y., Li J., Zhan Y., Wu L., Yu X., Zhang W., et al. Analysis of serum cytokines in patients with severe acute respiratory syndrome. Infect Immun. 2004;72:4410–4415. doi: 10.1128/IAI.72.8.4410-4415.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wang Z, Yang B, Li Q, Wen L, Zhang R. Clinical features of 69 cases with coronavirus disease 2019 in Wuhan, China [published online ahead of print March 16, 2020]. Clin Infect Dis. https://doi.org/10.1093/cid/ciaa272. [DOI] [PMC free article] [PubMed]
- 61.Gouel-Cheron A., Allaouchiche B., Guignant C., Davin F., Floccard B., Monneret G., et al. Early interleukin-6 and slope of monocyte human leukocyte antigen-DR: a powerful association to predict the development of sepsis after major trauma. PLoS One. 2012;7 doi: 10.1371/journal.pone.0033095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wu H.P., Chen C.K., Chung K., Tseng J.C., Hua C.C., Liu Y.C., et al. Serial cytokine levels in patients with severe sepsis. Inflamm Res. 2009;58:385–393. doi: 10.1007/s00011-009-0003-0. [DOI] [PubMed] [Google Scholar]
- 63.Kellum J.A., Kong L., Fink M.P., Weissfeld L.A., Yealy D.M., Pinsky M.R., et al. Understanding the inflammatory cytokine response in pneumonia and sepsis: results of the Genetic and Inflammatory Markers of Sepsis (GenIMS) study. Arch Intern Med. 2007;167:1655–1663. doi: 10.1001/archinte.167.15.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Jekarl D.W., Lee S.Y., Lee J., Park Y.J., Kim Y., Park J.H., et al. Procalcitonin as a diagnostic marker and IL-6 as a prognostic marker for sepsis. Diagn Microbiol Infect Dis. 2013;75:342–347. doi: 10.1016/j.diagmicrobio.2012.12.011. [DOI] [PubMed] [Google Scholar]
- 65.Billeter A., Turina M., Seifert B., Mica L., Stocker R., Keel M. Early serum procalcitonin, interleukin-6, and 24-hour lactate clearance: useful indicators of septic infections in severely traumatized patients. World J Surg. 2009;33:558–566. doi: 10.1007/s00268-008-9896-y. [DOI] [PubMed] [Google Scholar]
- 66.Stensballe J., Christiansen M., Tonnesen E., Espersen K., Lippert F.K., Rasmussen L.S. The early IL-6 and IL-10 response in trauma is correlated with injury severity and mortality. Acta Anaesthesiol Scand. 2009;53:515–521. doi: 10.1111/j.1399-6576.2008.01801.x. [DOI] [PubMed] [Google Scholar]
- 67.Maier B., Lefering R., Lehnert M., Laurer H.L., Steudel W.I., Neugebauer E.A., et al. Early versus late onset of multiple organ failure is associated with differing patterns of plasma cytokine biomarker expression and outcome after severe trauma. Shock. 2007;28:668–674. [PubMed] [Google Scholar]
- 68.Song J., Park D.W., Moon S., Cho H.J., Park J.H., Seok H., et al. Diagnostic and prognostic value of interleukin-6, pentraxin 3, and procalcitonin levels among sepsis and septic shock patients: a prospective controlled study according to the Sepsis-3 definitions. BMC Infect Dis. 2019;19:968. doi: 10.1186/s12879-019-4618-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Uusitalo-Seppala R., Koskinen P., Leino A., Peuravuori H., Vahlberg T., Rintala E.M. Early detection of severe sepsis in the emergency room: diagnostic value of plasma C-reactive protein, procalcitonin, and interleukin-6. Scand J Infect Dis. 2011;43:883–890. doi: 10.3109/00365548.2011.600325. [DOI] [PubMed] [Google Scholar]
- 70.Takahashi W., Nakada T.A., Yazaki M., Oda S. Interleukin-6 levels act as a diagnostic marker for infection and a prognostic marker in patients with organ dysfunction in intensive care units. Shock. 2016;46:254–260. doi: 10.1097/SHK.0000000000000616. [DOI] [PubMed] [Google Scholar]
- 71.Harbarth S., Holeckova K., Froidevaux C., Pittet D., Ricou B., Grau G.E., et al. Diagnostic value of procalcitonin, interleukin-6, and interleukin-8 in critically ill patients admitted with suspected sepsis. Am J Respir Crit Care Med. 2001;164:396–402. doi: 10.1164/ajrccm.164.3.2009052. [DOI] [PubMed] [Google Scholar]
- 72.Ma L., Zhang H., Yin Y.L., Guo W.Z., Ma Y.Q., Wang Y.B., et al. Role of interleukin-6 to differentiate sepsis from non-infectious systemic inflammatory response syndrome. Cytokine. 2016;88:126–135. doi: 10.1016/j.cyto.2016.08.033. [DOI] [PubMed] [Google Scholar]
- 73.Pettila V., Hynninen M., Takkunen O., Kuusela P., Valtonen M. Predictive value of procalcitonin and interleukin 6 in critically ill patients with suspected sepsis. Intensive Care Med. 2002;28:1220–1225. doi: 10.1007/s00134-002-1416-1. [DOI] [PubMed] [Google Scholar]
- 74.Mat-Nor M.B., Md Ralib A., Abdulah N.Z., Pickering J.W. The diagnostic ability of procalcitonin and interleukin-6 to differentiate infectious from noninfectious systemic inflammatory response syndrome and to predict mortality. J Crit Care. 2016;33:245–251. doi: 10.1016/j.jcrc.2016.01.002. [DOI] [PubMed] [Google Scholar]
- 75.Mors K., Braun O., Wagner N., Auner B., Voth M., Stormann P., et al. Influence of gender on systemic IL-6 levels, complication rates and outcome after major trauma. Immunobiology. 2016;221:904–910. doi: 10.1016/j.imbio.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 76.Lee D.W., Gardner R., Porter D.L., Louis C.U., Ahmed N., Jensen M., et al. Current concepts in the diagnosis and management of cytokine release syndrome. Blood. 2014;124:188–195. doi: 10.1182/blood-2014-05-552729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.National Institutes of Health The National Institutes of Health COVID-19 Treatment Guidelines Panel provides recommendations for dexamethasone in patients with COVID-19. 2020.. https://www.covid19treatmentguidelines.nih.gov/dexamethasone/ Available from:
- 78.Klaver Y., van Steenbergen S.C.L., Sleijfer S., Debets R., Lamers C.H.J. Plasma IFN-gamma and IL-6 levels correlate with peripheral T-cell numbers but not toxicity in RCC patients treated with CAR T-cells. Clin Immunol. 2016;169:107–113. doi: 10.1016/j.clim.2016.06.014. [DOI] [PubMed] [Google Scholar]
- 79.Fraietta J.A., Lacey S.F., Orlando E.J., Pruteanu-Malinici I., Gohil M., Lundh S., et al. Determinants of response and resistance to CD19 chimeric antigen receptor (CAR) T cell therapy of chronic lymphocytic leukemia. Nat Med. 2018;24:563–571. doi: 10.1038/s41591-018-0010-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ogata A., Kato Y., Higa S., Yoshizaki K. IL-6 inhibitor for the treatment of rheumatoid arthritis: a comprehensive review. Mod Rheumatol. 2019;29:258–267. doi: 10.1080/14397595.2018.1546357. [DOI] [PubMed] [Google Scholar]
- 81.Food and Drug Administration XELJANZ® (tofacitinib) 2018.. https://www.fda.gov/Drugs Available from:
- 82.Le R.Q., Li L., Yuan W., Shord S.S., Nie L., Habtemariam B.A., et al. FDA approval summary: tocilizumab for treatment of chimeric antigen receptor T cell-induced severe or life-threatening cytokine release syndrome. Oncologist. 2018;23:943–947. doi: 10.1634/theoncologist.2018-0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Xu X., Han M., Li T., Sun W., Wang D., Fu B., et al. Effective treatment of severe COVID-19 patients with tocilizumab. Proc Natl Acad Sci U S A. 2020;117:10970–10975. doi: 10.1073/pnas.2005615117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Nishimoto N., Terao K., Mima T., Nakahara H., Takagi N., Kakehi T. Mechanisms and pathologic significances in increase in serum interleukin-6 (IL-6) and soluble IL-6 receptor after administration of an anti-IL-6 receptor antibody, tocilizumab, in patients with rheumatoid arthritis and Castleman disease. Blood. 2008;112:3959–3964. doi: 10.1182/blood-2008-05-155846. [DOI] [PubMed] [Google Scholar]
- 85.Roumier M, Paule R, Groh M, Vallée A, Ackermann F. Interleukin-6 blockade for severe COVID-19 [published online ahead of print April 22, 2020]. medRxiv.
- 86.Price CC, Altice FL, Shyr Y, Koff A, Pischel L, Goshua G, et al. Tocilizumab treatment for cytokine release syndrome in hospitalized COVID-19 patients: survival and clinical outcomes [published online ahead of print June 15, 2020]. Chest. https://doi.org/10.1016/j.chest.2020.06.006. [DOI] [PMC free article] [PubMed]
- 87.Food and Drug Administration SYLVANT® (siltuximab) 2014.. https://www.accessdata.fda.gov/drugsatfda_docs/label/2014/125496s000lbl.pdf Available from:
- 88.Wong C.K., Lam C.W., Wu A.K., Ip W.K., Lee N.L., Chan I.H., et al. Plasma inflammatory cytokines and chemokines in severe acute respiratory syndrome. Clin Exp Immunol. 2004;136:95–103. doi: 10.1111/j.1365-2249.2004.02415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Cohen S.B. The use of anakinra, an interleukin-1 receptor antagonist, in the treatment of rheumatoid arthritis. Rheum Dis Clin North Am. 2004;30:365–380. doi: 10.1016/j.rdc.2004.01.005. vii. [DOI] [PubMed] [Google Scholar]
- 90.Food and Drug Administration Kineret® (anakinra) 2012.. https://www.fda.gov/Drugs Available from:
- 91.Kumar B., Aleem S., Saleh H., Petts J., Ballas Z.K. A personalized diagnostic and treatment approach for macrophage activation syndrome and secondary hemophagocytic lymphohistiocytosis in adults. J Clin Immunol. 2017;37:638–643. doi: 10.1007/s10875-017-0439-x. [DOI] [PubMed] [Google Scholar]
- 92.Cavalli G., De Luca G., Campochiaro C., Della-Torre E., Ripa M., Canetti D., et al. Interleukin-1 blockade with high-dose anakinra in patients with COVID-19, acute respiratory distress syndrome, and hyperinflammation: a retrospective cohort study. Lancet Rheumatol. 2020;2:e325–e331. doi: 10.1016/S2665-9913(20)30127-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Haga S., Yamamoto N., Nakai-Murakami C., Osawa Y., Tokunaga K., Sata T., et al. Modulation of TNF-alpha-converting enzyme by the spike protein of SARS-CoV and ACE2 induces TNF-alpha production and facilitates viral entry. Proc Natl Acad Sci U S A. 2008;105:7809–7814. doi: 10.1073/pnas.0711241105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Fala L. Cosentyx (Secukinumab): first IL-17A antagonist receives FDA approval for moderate-to-severe plaque psoriasis. Am Health Drug Benefits. 2016;9:60–63. [PMC free article] [PubMed] [Google Scholar]
- 95.Wu D., Yang X.O. TH17 responses in cytokine storm of COVID-19: an emerging target of JAK2 inhibitor Fedratinib. J Microbiol Immunol Infect. 2020;53:368–370. doi: 10.1016/j.jmii.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Food and Drug Administration INREBIC® (fedratinib) 2019.. https://www.fda.gov/Drugs Available from.
- 97.Zhang W., Zhao Y., Zhang F., Wang Q., Li T., Liu Z., et al. The use of anti-inflammatory drugs in the treatment of people with severe coronavirus disease 2019 (COVID-19): the perspectives of clinical immunologists from China. Clin Immunol. 2020;214:108393. doi: 10.1016/j.clim.2020.108393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Food and Drug Administration OLUMIANT (baricitinib) 2018.. https://www.fda.gov/Drugs Available from:
- 99.Beigel JH, Tomashek KM, Dodd LE, Mehta AK, Zingman BS, Kalil AC, et al. Remdesivir for the treatment of Covid-19—preliminary report [published online ahead of print May 22, 2020]. N Engl J Med. https://doi.org/10.1056/NEJMoa2007764. [DOI] [PubMed]
- 100.Food and Drug Administration JAKAFI® (ruxolitinib) 2019.. https://www.fda.gov/Drugs Available from:
- 101.Cao Y., Wei J., Zou L., Jiang T., Wang G., Chen L., et al. Ruxolitinib in treatment of severe coronavirus disease 2019 (COVID-19): a multicenter, single-blind, randomized controlled trial. J Allergy Clin Immunol. 2020;146:137–146.e3. doi: 10.1016/j.jaci.2020.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Pei J., Zhang Y., Luo Q., Zheng W., Li W., Zeng X., et al. STAT3 inhibition enhances CDN-induced STING signaling and antitumor immunity. Cancer Lett. 2019;450:110–122. doi: 10.1016/j.canlet.2019.02.029. [DOI] [PubMed] [Google Scholar]
- 103.Liu Y., Jesus A.A., Marrero B., Yang D., Ramsey S.E., Sanchez G.A.M., et al. Activated STING in a vascular and pulmonary syndrome. N Engl J Med. 2014;371:507–518. doi: 10.1056/NEJMoa1312625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hung I.F., Lung K.C., Tso E.Y., Liu R., Chung T.W., Chu M.Y., et al. Triple combination of interferon beta-1b, lopinavir-ritonavir, and ribavirin in the treatment of patients admitted to hospital with COVID-19: an open-label, randomised, phase 2 trial. Lancet. 2020;395:1695–1704. doi: 10.1016/S0140-6736(20)31042-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Risitano A.M., Mastellos D.C., Huber-Lang M., Yancopoulou D., Garlanda C., Ciceri F., et al. Complement as a target in COVID-19? Nat Rev Immunol. 2020;20:343–344. doi: 10.1038/s41577-020-0320-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Campbell C.M., Kahwash R. Will complement inhibition be the new target in treating COVID-19 related systemic thrombosis? Circulation. 2020;141:1739–1741. doi: 10.1161/CIRCULATIONAHA.120.047419. [DOI] [PubMed] [Google Scholar]
- 107.Gralinski L.E., Sheahan T.P., Morrison T.E., Menachery V.D., Jensen K., Leist S.R., et al. Complement activation contributes to severe acute respiratory syndrome coronavirus pathogenesis. mBio. 2018;9 doi: 10.1128/mBio.01753-18. e01753-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Rojas M., Rodriguez Y., Monsalve D.M., Acosta-Ampudia Y., Camacho B., Gallo J.E., et al. Convalescent plasma in Covid-19: possible mechanisms of action. Autoimmun Rev. 2020;19 doi: 10.1016/j.autrev.2020.102554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Bloch E.M., Shoham S., Casadevall A., Sachais B.S., Shaz B., Winters J.L., et al. Deployment of convalescent plasma for the prevention and treatment of COVID-19. J Clin Invest. 2020;130:2757–2765. doi: 10.1172/JCI138745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Soo Y.O., Cheng Y., Wong R., Hui D.S., Lee C.K., Tsang K.K., et al. Retrospective comparison of convalescent plasma with continuing high-dose methylprednisolone treatment in SARS patients. Clin Microbiol Infect. 2004;10:676–678. doi: 10.1111/j.1469-0691.2004.00956.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Cheng Y., Wong R., Soo Y.O., Wong W.S., Lee C.K., Ng M.H., et al. Use of convalescent plasma therapy in SARS patients in Hong Kong. Eur J Clin Microbiol Infect Dis. 2005;24:44–46. doi: 10.1007/s10096-004-1271-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Rajendran K, Krishnasamy N, Rangarajan J, Rathinam J, Natarajan M, Ramachandran A. Convalescent plasma transfusion for the treatment of COVID-19: systematic review [published online ahead of print May 1, 2020]. J Med Virol. https://doi.org/10.1002/jmv.25961. [DOI] [PMC free article] [PubMed]
- 113.Chen L., Xiong J., Bao L., Shi Y. Convalescent plasma as a potential therapy for COVID-19. Lancet Infect Dis. 2020;20:398–400. doi: 10.1016/S1473-3099(20)30141-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Shen C., Wang Z., Zhao F., Yang Y., Li J., Yuan J., et al. Treatment of 5 critically ill patients with COVID-19 with convalescent plasma. JAMA. 2020;323:1582–1589. doi: 10.1001/jama.2020.4783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Li L, Zhang W, Hu Y, Tong X, Zheng S, Yang J, et al. Effect of convalescent plasma therapy on time to clinical improvement in patients with severe and life-threatening COVID-19: a randomized clinical trial [published online ahead of print June 3, 2020]. JAMA. https://doi.org/10.1001/jama.2020.10044. [DOI] [PMC free article] [PubMed]