Abstract
This review examines the impact of cannabinoids on viral infections, as well as its effects on the mitochondria of the nervous and immune system. The paper conveys information about the beneficial and negative impacts of cannabinoids on viral infections, especially HIV-1. These include effects on the inflammatory response as well as neuroprotective effects. We also explore non-apoptotic mitochondrial pathways modulated by the activity of cannabinoids, resulting in modifications to cellular functions. As a large part of the literature derives from studies of the nervous system, we first compile the information related to mitochondrial functions in this system, particularly through the CB1 receptor. Finally, we reflect on how this knowledge could complement what has been demonstrated in the immune system, especially in the context of the CB2 receptor and Ca2+ uptake. The overall conclusion of the review is that cannabinoids have the potential to affect a broad range of cell types through mitochondrial modulation, be it through receptor-specific action or not, and that this pathway has a potential implication in cases of viral infection.
Keywords: cannabinoid, THC, mitochondria, immunity, metabolism, inflammation, viral infection, nervous system
1. Introduction: Importance of Mitochondria on Immunity and Viral Control
Cells can metabolize a variety of carbon substrates including glucose, fatty acids, ketone bodies and amino acids. The cell’s ability to use different carbon sources, which is done through proper mitochondrial function, is critical to their ability to adapt to stress conditions, such as changes in nutrient availability and metabolical needs [1,2,3]. This is especially true in the case of T-cells, where adaptive immunity is dictated by the mitochondria’s capacity to use all types of carbon sources available [4,5]. As an example, naïve T-cells preferentially use oxidative phosphorylation (OXPHOS) in their quiescent state [6], while they switch to glycolysis during their activation [7,8,9]. Although primarily relying on glucose, activated lymphocytes can use many amino acids, such as alanine, leucine, glutamine, serine and arginine, as carbon sources [10,11,12]. For instance, removing alanine and leucine as carbon sources reduces T-cells effector functions and growth [11,12]. Additionally, L-arginine contributes to T-cells’ long-term memory maintenance in the context of OVA immunization in mice [10]. Furthermore, increased mitochondrial fatty acid oxidation (FAO) characterizes memory and regulatory T-cells’ subsets [13,14,15]. Which pathway the mitochondria skews towards is not only important for cell differentiation, it is also critical for proper specific anti-viral response. For example, it is known that polyfunctional anti-human immunodeficiency viruses (HIV-1) CD8 T-cells are critical to control HIV-1 [16,17], and recent evidence shows that the capacity of CD8 T-cells to maintain polyfunctionality in glucose-deprived media might explain natural control of HIV-1 infection [18]. This was partially explained by an increase in lipid uptake. Similarly, CD8 T-cells from controller macaques can target simian immunodeficiency virus (SIV)-infected CD4 T-cells even in the absence of glucose [18]. Additionally, autophagy seems to be important for viral containment and for specific CD8 T-cells’ activity by delivering lipid substrates as an additional energy source [19,20]. HIV, as well as other chronic disease patients such as cancer and sclerosis, have been known to be treated by anti-palliative substances, including cannabis. This plant has a history of being used for therapeutic purposes, namely to alleviate nausea, help calm severe pain, and stimulate the appetite to counter weight loss [21,22,23]. Cannabinoids are a class of compounds that can be found in the cannabis plant. These include a variety of exogenous, endogenous, and synthetic components which exhibit similar psycho-active and immune properties. With their uses in the treatment of advanced stages of illnesses as well as other therapeutic approaches, e.g., as an antidepressant, along with its appetite-stimulating properties becoming more widespread, evidence emerged showing that cannabinoids could influence viral pathogenesis and the immune system [24,25,26,27,28]. Currently, with the increasing number of countries and states legalizing marijuana for recreational use, its impact on health in the context of disease susceptibility is an important aspect to evaluate. The biological activity of cannabinoids is mainly mediated by cannabinoid receptors CB1 and CB2, which are predominantly expressed in cells from the nervous system and immune-derived cells, respectively [29]. When it comes to the immune system, different aspects of it are known to be affected by cannabinoids such as the level of apoptosis, suppression of cell proliferation, inhibition of pro-inflammatory cytokine and chemokine production, and the induction of anti-inflammatory cytokines and regulatory T-cells. In terms of immunomodulation, increasing evidence points towards the cannabinoids-induced effect on metabolism as a crucial player, as it induces AMP-activated protein kinase (AMPK) activation [30,31,32]. Considering the importance of the mitochondria and cellular metabolism for cell function and antiviral response, as mentioned earlier [33], evaluating the role of cannabinoids on both phenomena is important. As such, we wish to place the potential impact of cannabinoids on viral infections, especially in the context of HIV-1, as well as its impact on mitochondria, in the context of the function of the immune system.
2. Cannabinoids and Viral Infections: Potential Role of Mitochondria
The effects of cannabinoids on infections, both viral and other types, have already been thoroughly explored in past reviews [24,34,35]. In general, the effect of cannabinoids can be beneficial or detrimental depending on the concentration used, the type of infection, and, of course, which receptor is targeted. Some examples of detrimental effects include: the suppression of inflammatory myeloid cell responses by THC during the response to influenza [36] and the promotion of hepatitis C virus (HCV) replication caused by glucose metabolism disorders of hepatocytes following CB1 activation [37]. In the context of antigen-specific responses, the effects of cannabinoids are still open to question. As an example, it was reported that treatments with THC led to an earlier disease onset in the context of smallpox vaccine virus exposition in mice [38], while in the context of HIV-1, THC enhances antigen-specific immune responses [39]. This study was based on a HIV gp120-derived peptide activation of the immune system. The assessment of the modulating effect of THC was done through the evaluation of antigen-specific responses in both lymphocyte populations as well as non-lymphocyte immune cells in WT and CB1 and CB2 knocked-out mice. For T-cells, peptide-specific activation was determined by the subsequent production of interleukin (IL)-2 and interferon (IFN)-γ, while B-cell activation was studied through the quantification of antibodies production and expression levels of activation markers. On the other hand, a slew of studies report beneficial effects for different treatment procedures such as the attenuation of CXCR4-tropic HIV infection following CB2 activation [40] as well as protection from HIV-1-Tat-mediated neuronal death [41,42] and HIV-1 gp120-mediated neural damage [43]. In this last study, Hu et al. used a human mesencephalic neuronal glial model with a composition similar to the human nervous system, then exposed it to gp120 and finally treated it with THC in a concentration and time of exposure optimized in their previous study. A CB1 and CB2 agonist, WIN55,212-2, significantly reduced the gp120-induced apoptosis in dopaminergic neurons by controlling its subsequent ROS production in microglia. Interestingly, the beneficial effects of cannabinoids on the nervous system are not only found in the case of HIV-1 infection, but also with Theiler’s virus, which is specifically used as a model of demyelination [44,45]. As mentioned earlier, cannabinoids can affect the inflammatory response, which is detrimental in the case of influenza [36]. However, considering that the inflammatory response can be detrimental in some infections [46], this effect of cannabinoids can potentially be beneficial. This is especially true in the context of HIV-1 infection, considering the lingering inflammation present in patients, even under highly active antiretroviral therapy (HAART) [47]. Reports by Henriquez et al. point toward THC as a way to control this inflammation and immune activation, as they demonstrate that treatment with THC reduces both the secretion of IFN-α by plasmacytoid dendritic cells (pDC) and its subsequent activation of T-cells [48,49]. This anti-inflammatory property of THC was also reported in a SIV model, where it reduced T-cell proliferation and activation in the intestine [50]. Similarly, Tahamtan et al. bring forth the important role of the endocannabinoid system in regulating the inflammatory response in the context of respiratory syncytial virus (RSV). In their studies, they demonstrate that activating either CB1 or CB2 decreased immune cell influx and cytokine production, resulting in alleviated lung pathology in a murine model [51,52]. This is particularly interesting considering that supressing inflammation in chronic infections such as HIV-1 is expected to be beneficial in controlling the disease progression since it is mediated through prolonged dysregulation of multiple signalling pathways caused by said inflammation. However, we see how dampening the immune response can also be beneficial in more acute infections, such as RSV (see Table 1 for an overview of the reported effects). The other side of the coin is how viral infections affect the mitochondria. T-cells specific to HIV-1 are subjected to constant immune activation which creates a high energetic demand for those cells [53,54]. Considering this, CD8 T-cells from HIV-1-infected patients not only display an increase in glycolysis but are dependent on glucose for their effector function, even following successful HAART [18]. Additionally, during HIV-1 infection, T-cells become progressively exhausted [55,56], displaying reduced mitochondrial mass and membrane potential. Those phenotypes could be mediated by programmed cell death protein 1 (PD-1) stimulation, resulting in reduced mitochondrial and glycolytic activities [57]. Moreover, another aspect to consider is the effect of treatment on mitochondria health. As an example, nucleoside reverse transcriptase inhibitor (NRTI) treatments for HIV-1 infection have been associated with mitochondrial DNA loss, altered membrane potential, inhibition of electron transport chain complexes, impairment of FAO and lower ATP production [58,59]. Similarly, many reports exist of different viruses modulating the mitochondria to enhance their replication [60,61,62]. Mitochondrial modulations by viruses are twofold. Firstly, considering that mitochondria play a crucial role in antiviral immunity, certain viruses interfere with functions conferring that role in order to proliferate. These include the disturbance of mitochondrial dynamics such as fission and fusion, the induction of mitophagy, and the regulation of apoptotic processes [61]. Secondly, some viruses will exploit the cell’s membrane transport pathways, generating organelles named viral factories. These organelles represent specialized compartments for viral replication, maturation, and export [62]. Given this fact and the role of cannabinoid signalling in modulating the mitochondria, the potential for those compounds to affect viral infections at that level are high, especially considering the reported impact of the endocannabinoid system on HCV replication through its effect on glucose metabolism [37]. However, we have to remain on the side of conjectures, as there are no direct reports on how the mitochondrial effect of cannabinoids might impact viral infections by using such mitochondrial changes. Nevertheless, in the following parts of this review, we will address the impact of cannabinoids on mitochondrial functions of cells from both the nervous and immune system. We explore this side of cannabinoids because, as we will see, they have a wide range of effects, making them strong candidates to control viral infections through mitochondrial modulation.
Table 1.
Effects of cannabinoids on viral infections. 2-AG: 2-Arachidonoylglycerol; AEA: N-arachidonoylethanolamine; CB1: Cannabinoid receptor type 1; CB2: Cannabinoid receptor type 2; CBD: Cannabidiol; HBV: hepatitis B virus; MAIDS: murine acquired immunodeficiency syndrome; THC: Δ⁹-tetrahydrocannabinol.
| Virus | Treatment/Context | Model | Observations | Reference |
|---|---|---|---|---|
| HIV-1 | ||||
| THC | Human | Suppression of IFN-α-mediated activation of T-cells | Henriquez et al., 2018 [48] | |
| Inhibition of AEA hydrolysis | Murine | Reduction in HIV-Tat-mediated neuronal death and dendritic degeneration | Hermes et al., 2018 [41] | |
| Cannabis use in HAART treated patients | Human | Reduction in systemic inflammation and immune activation | Manuzak et al., 2018 [63] | |
| AEA, 2-AG | Murine | Protection of neurons from HIV-Tat excitotoxicity | Xu et al., 2017 [42] | |
| THC | Human | Suppression of IFN-α secretion by pDC | Henriquez et al., 2017 [49] | |
| THC | Murine | Enhancement of pVRCgp120-induced IFN-γ production | Chen et al., 2015 | |
| by splenic lymphocyte populations and activation of T/B cells | [39] | |||
| AEA, 2-AG | Human | Suppression of pro-inflammatory and increase of anti-inflammatory cytokines, through the MAPK pathway | Krishnan and Chaterjee, 2014 [64] | |
| THC | Human | Reduction of cell surface HIV receptor (CD4, CCR5 and CXCR4) expression on macrophages | Williams et al., 2014 [65] | |
| THC, CP55940 (CB1/2 agonist) | Human | Inhibition of HIV-Tat-mediated adhesion of monocyte to extracellular matrix | Raborn et al., 2014 [66] | |
| JWH133, Gp1a, O-1966 (CB2 agonist) | Human | Inhibition of RT and LTR activity | Ramirez et al., 2013 [67] | |
| WIN55,212-2 (CB1/2 agonist) | Human | Protection of human dopaminergic neurons from gp120 | Hu et al., 2013 [43] | |
| THC, CBD | Murine | Enhancement of T-cell response after suboptimal stimulation | Chen et al., 2012 [68] | |
| Suppression of T-cell response after optimal stimulation | ||||
| JWH133, JWH150, 2-AG, AEA (CB2 agonists) | Human | Reduces cell-free and cell-to-cell transmission of CXCR4-tropic HIV | Constantino et al., 2012 [40] | |
| HIV-1 | THC, 2-AG | Murine | Reduction CCR3 expression resulting in less migration of BV-2 cells towards HIV-Tat | Fraga et al., 2011 [69] |
| WIN55,212-2 (CB1/2 agonist) | Murine | Inhibited gp120-induced IL-1β production and impairment of network functions | Kim et al., 2011 [70] | |
| THC, CP55940 (CB1/2 agonist) | Human | Inhibition of macrophage migration to HIV-Tat protein | Raborn and Cabral, 2010 [71] | |
| SIV | ||||
| THC | Rhesus | No upregulation of pro-inflammatory miR-21, miR-141 and miR-222 and alpha/beta defensins | Kumar et al., 2019 [50] | |
| Higher expression of tight junction proteins (occludin, claudin-3), anti-inflammatory MUC13, keratin-8 (stress protection), PROM1 (epithelial proliferation) | ||||
| THC | Rhesus | Upregulation of microRNA which targets proinflammatory molecules | Chandra et al., 2015 [72] | |
| THC | Rhesus | Chronic administration increased CXCR4 expression on T-cells | LeCapitaine et al., 2011 [73] | |
| THC | Rhesus | Chronic administration reduced early mortality, associated with attenuation of plasma viral load and body mass retention | Molina et al., 2011 [74] | |
| MAIDS | ||||
| JWH015, JWH133, Gp1a (CB2 agonists) | Murine | Acute antiallodynic effects on infection-induced neuropathic pain | Sheng et al., 2019 [75] | |
| HBV | ||||
| Rimonabant (CB1 inhibitor) | Human | Suppressed HBV propagation through the inhibition of hepatocyte nuclear factor 4α | Sato et al., 2020 [76] | |
| HCV | ||||
| AEA | Human | Decrease of AMPK phosphorylation, inhibition of cell surface expression of GLUT2, and suppression of cellular glucose uptake. Promotion of viral replication | Sun et al., 2014 [37] | |
| RSV | ||||
| JZL184 (CB1 agonist) | Murine | Decreased immune cell influx and cytokine/chemokine production, and alleviated lung pathology | Tahamtan et al., 2018 (a) [51] | |
| JWH133 (CB2 agonist) | Murine | Decreased immune cell influx and cytokine/chemokine production, and alleviated lung pathology | Tahamtan et al., 2018 (b) [52] | |
| Theiler’s | ||||
| CBD | Murine | Decreased frequency and severity of acute behavioral seizures | Patel et al., 2019 [45] | |
| Inhibition of 2-AG hydrolysis | Murine | Enhances remyelination | Feliu et al., 2017 [44] | |
| WIN55,212-2 (CB1/2 agonist) | Murine | Reduced CD4 + CD25 + Foxp3– T-cells activation in the CNS and increased regulatory CD4 + CD25 + Foxp3 + T-cell activation | Arevalo-Martin et al., 2012 [77] | |
| AEA | Murine | Inhibition of VCAM-1 potentially reducing neuroinflammation | Mestre et al., 2011 [78] | |
| Influenza | ||||
| THC | Murine | Suppressed DC, macrophages, monocytes, and inflammatory myeloid cell responses | Karmaus et al., 2013 [36] | |
| Vaccinia | ||||
| THC | Murine | Increased severity and duration of symptoms | Huemer et al., 2011 [38] | |
3. Cannabinoids, Mitochondria, and the Nervous System
As cannabinoids have been firstly identified as the neurotropic agents in cannabis, it comes as no surprise that a lot of early studies regarding its mechanism of action were focused on the nervous system. As such, it was discovered that the effects of cannabinoids in the brain are mainly due to the activation of the CB1 receptor. Of note, most of the information concerning the impact of cannabinoids on mitochondria comes from studies in this field of research. As such, even though the main point of this review is to consider the impact of cannabinoids on the immune system, it is necessary to place our knowledge in its initial context: the nervous system. The key element to placing CB1 and mitochondria together comes from the work of Hebert-Chatelain et al., who not only showed the presence of CB1 on the mitochondrial membrane of mouse neurons [79], but also reported its role in the regulation of cellular respiration and energy production [80]. To summarize, they demonstrated that cannabinoid signalling is necessary for PKA-dependent phosphorylation of the mitochondrial electron transport system. Thus, CB1 genetic exclusion leads to decreased cellular respiration. Although those findings came with their share of controversies [81,82], there is now a well-established link between cannabinoids, mitochondria and neuronal activity [83,84,85]. However, Jimenez-Blasco et al. describe in a recent study how the activation of mitochondrial CB1 actually reduces OXPHOS and hampers the metabolism of glucose in mouse astroglia [86]. In this study, they first confirmed that mitochondrial CB1 was responsible for reducing microglia oxygen consumption by comparing the effect of HU210, a CB1 agonist, with that of a cell-impermeable biotinylated version. Mitochondrial CB1 activation then leads to the destabilization of complex I. In addition to the effect on OXPHOS, mitochondrial CB1 activation also leads to a decrease in nuclear hypoxia-inducible factors 1 (HIF-1) resulting in the reduction in glycolytic activity [86]. To summarize, both complete exclusion of mitochondrial CB1 and a strong activation of this same receptor lead to reduced cellular respiration [80,86]. Interestingly, another recent study places CB1 as an important regulator of mitophagy in hippocampal neurons [87], showing that adult hippocampal CB1-KO mice displayed mitochondrial elongation and had reduced mitophagy activity compared to WT. The effect of CB1 knock-out on mitophagy was observed via the levels of Serine 65-phosphorylated ubiquitin serving as a biomarker for PTEN-induced kinase 1 (PINK1) activity. However, Kataoka et al. did not consider the localization of the CB1 to contextualize their observation. In addition to CB1-mediated mitochondrial modulation, Fisar et al. also demonstrated a non-receptor mechanism. They came to this conclusion after evaluating the effects of different cannabinoids with known receptor targets. Overall, they posit that cannabinoids can accumulate in the hydrophobic parts of the inner mitochondrial membrane, impairing the molecular interactions and assembly of the respiratory chain [88]. This comes in addition to previous reports of non-receptor specific effect of cannabinoids on mitochondria [89,90]. Interestingly, it has been shown that the CB1-mediated effect on mitochondrial dynamics is not restricted to cells of the nervous system [91]. In this study, it is shown that CB1 stimulation by the endocannabinoid, n-arachidonoylethanolamine (AEA), in renal proximal tubular cells leads to dynamin-related protein 1 (DRP1) activation, with its subsequent translocation to the mitochondria that results in mitochondrial fission. Inevitably, looking at the impact of cannabinoids on the nervous system leads to having a look at the microglia. These are specialized macrophages found in the central nervous system (CNS). They are important for maintaining the health of the CNS by dealing with infections and removing damaged neurons [92]. In this context, Ma et al. found that AM1241, a CB2 agonist, mediates anti-inflammatory responses in microglia. This was observed by the upregulation of markers associated with M2 phenotypes, such as arginase 1 and brain-derived neurotrophic factor with a downregulation of the M1 markers’ inducible nitric oxide synthase and tumor necrosis factor (TNF)-α. They suggest that this might be due to the peroxisome proliferator-activated receptor gamma coactivator 1-alpha (PGC-1α) and its association with the enhancement of mitochondria biogenesis. [93]. Both the idea that the effect of cannabinoids on mitochondria is not specific to neuronal cells as well as having a direct impact on microglia, which bridges the nervous and immune system, leads us to review the impact of cannabinoids on the mitochondria of immune cells.
4. Cannabinoids, Mitochondria, and the Immune System
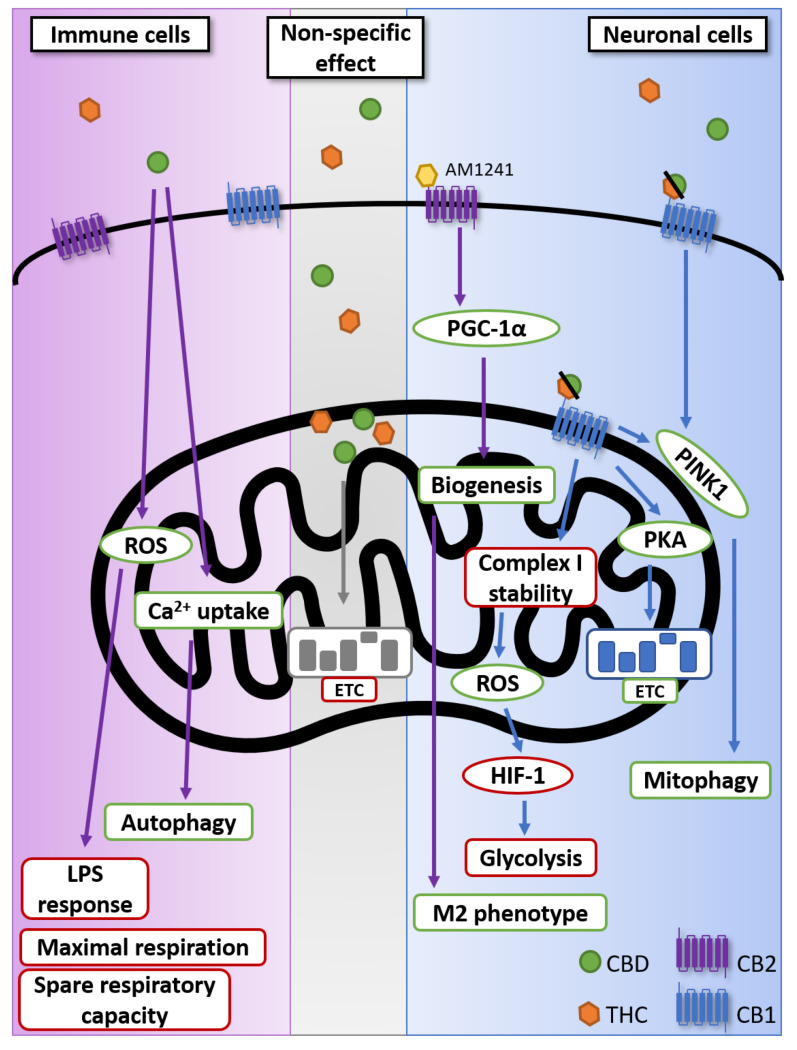
CB2, being abundantly present on immune cells, has made the study of cannabinoids in the context of infection a necessity. It is now well established that the activation of CB2 receptors, by endogenous or exogenous cannabinoids, is immunosuppressive [26,27]. A recent review is particularly thorough in describing the effects of cannabidiol (CBD) in regulating the immune responses [94] In the case of T-cells, this is notable through their suppression of IL-2, IFN-γ, and TNF-α [95]. Considering the crucial role that the mitochondria plays in apoptosis as well as in various intrinsic and extrinsic ways [96,97], it comes as no surprise that most studies of cannabinoids on mitochondria revolve around apoptosis [98]. One of the most recent examples of this is a study by Wu et al., who showed that CBD had a very important pro-apoptotic effect on monocytes because of its effect on mitochondrial membrane potential and cytochrome c release [99]. Although the studies indicating the non-apoptotic effect of cannabinoids on the mitochondria from immune cells remain few, some point towards a role in reactive oxygen species (ROS) production and an effect on mitochondrial respiration [95,100]. In their paper, Schultze et al. demonstrate that CBD reduces both maximal respiration and spare respiratory capacity in THP-1 monocytes [100]. Additionally, mitochondrial ROS could potentially have a role to play in LPS-induced inflammatory responses by macrophages. In this study, a 24 h treatment with CBD dramatically reduced IL-8 production by U937 monocytes [95]. Although in both studies they observed an increase in mitochondrial ROS, the effects observed were not directly linked to its production. Additional studies, with antioxidants, for example, are warranted to elucidate the role of ROS in the non-apoptotic effect of CBD on the mitochondria. As mentioned, the study of the impact of cannabinoids on the metabolism of mitochondria of immune cells is still at an early stage, especially in cells other than myeloid cells. Still, with the evidence currently at our disposition, we can see the potential importance of the cannabinoid pathway in the regulation of immune cell metabolism. Another potential non-apoptotic pathway to modulate mitochondria by cannabinoids is through calcium signalling. Indeed, ion channels, especially calcium, are known to be crucial for proper immune responses [101,102]. In this context, Olivas-Aguirre et al. found that CBD favors mitochondrial Ca2+ uptake on acute lymphoblastic leukemia of T lineage cells. This leads to a loss of mitochondrial membrane potential, disruption of the cristae, and ATP production, ultimately resulting in mitophagy. At sublethal concentration, they demonstrate that CBD induces a conversion of LC3-I to LC3-II, showing an activation of autophagy. [103]. This is of particular interest considering that Ca2+ intake is required for T-cell receptor stimulation [102,104]. Overall, the impact of cannabinoids on non-apoptotic mitochondrial pathways remains to be fully uncovered, but with the current knowledge at our disposition, we can expect it to have important ramifications for the immune system regulation, particularly in the inflammatory responses (see Figure 1 for an overview of non-apoptotic effect of cannabinoids on mitochondrial functions).
Figure 1.
Non-apoptotic impact of cannabinoids on mitochondria. Although CB1 and CB2 are found on immune cell, the reported activity of CBD on the mitochondria of immune cells was not confirmed to be dependent on either receptor [95,100,103]. Non-specific effect represents the effect of cannabinoids on mitochondrial membrane integrity demonstrated not to be dependent on CB1 or CB2 [88,89,90]. It is now well established that CB1 is found on mitochondrial membrane [80,86,87,93]. Green borders represent an upregulation or increased activity; red borders represent a downregulation or reduced activity. CB1: Cannabinoid receptor type 1; CB2: Cannabinoid receptor type 2; CBD: Cannabidiol; ETC: Electron transport chain; HIF-1; hypoxia-inducible factors 1; PGC-1α: peroxisome proliferator-activated receptor gamma coactivator 1-alpha; PINK1: PTEN-induced kinase 1; PKA: Protein kinase A; ROS: reactive oxygen species; THC: Δ⁹-tetrahydrocannabinol.
5. Conclusions
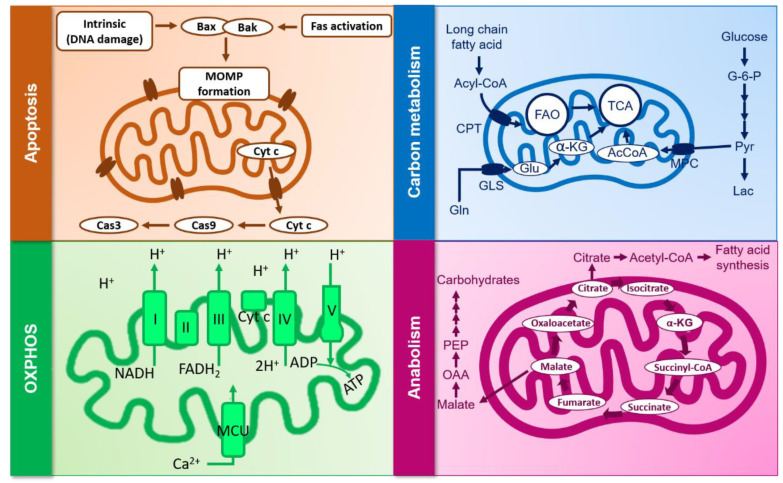
The recent legalization of marijuana in Canada, as well as in different European countries, made cannabinoids accessible as off-the-counter substances for patients in need of palliative treatment, as well as for recreational users. As such, the study of the effects of endogenous as well as exogenous cannabinoids on the immune system, be it in a resting state or in the case of viral infections, becomes crucial. Aside from their apoptotic and non-apoptotic effects, their impact on viral infections as well as inflammation and their effect on cellular metabolism and energy uptake, and sex- and age-dependent differences, in metabolizing such substances have been pointed out. In a study by Fattore et al., although no dissimilarities were pointed out when it comes to intoxication or plasmic THC levels, male smokers showed notably higher levels in circulating THC levels and larger cardiovascular effects than female smokers, who comparatively showed higher CB1 protein expressions and more explicit hemodynamic changes [105]. In line with this study, marijuana metabolizing is also impacted by body fat levels and sexual hormones, particularly testosterone and estrogen, which, respectively, lighten and intensify THC absorption and thus impact its conversion into inactive or active metabolites such as 11-hydroxy-THC [106]. In a similar context, a recent review by Gorey et al. summarized the impact of age on cannabis use and metabolization by focusing on its effect on attention, learning and memory in youths (under 18 years old) and adults (over 18 years old) almost daily on daily smokers as well as in young and adult rats [107]. The paper showed that multiple gaps and contradictions exist in studies done on both human and rats when it comes to THC effect on neuropsychological domains, but that young smokers showed more attention deficit as well as lower prose recall compared to adults, who showed higher memory impairments. Although the effects of cannabinoids on inflammation are well established, information about how the mitochondria are involved remains limited. Considering all of the facts above, cannabinoids’ metabolism, be it derived from cannabis or synthetic substances, needs to be further investigated, especially when it comes to its effect on mitochondrial plasticity in the context of viral infections and the resulting chronic inflammation. This is notable considering the growing interest in its usage during persistent infections which are associated with inflammation [34,108]. Another aspect to remember is the lipophilic nature of cannabinoids that allows them to enter cells passively. Given this property, they can potentially alter the integrity of any cellular membrane regardless of the presence of CB1/CB2 by accumulating in the hydrophobic parts, leading to impairment of molecular interactions [88]. An innovative strategy to investigate such an effect will be the use, development, and optimization of the Seahorse, which is a novel live-cell metabolic assay platform that allows the real time evaluation of cellular respiration and plasticity via the accurate measurements of mitochondrial respiration and plasticity (see Figure 2 and Table 2 for a summary of mitochondrial processes potentially affected by cannabinoids and in which cell type the effect was reported).
Figure 2.
Mitochondrial processes potentially affected by cannabinoids. α-KG: alpha-ketoglutarate; CPT: carnitine palmitoyltransferase; FAO: fatty acid oxidation; GLS: mitochondrial glutaminase; MOMP: mitochondrial outer membrane permeabilization; MCU: mitochondrial calcium uniporter; MPC: mitochondrial pyruvate carrier; OAA: oxaloacetate; TCA: tricarboxylic acid cycle.
Table 2.
Mitochondrial processes affected by cannabinoids in neuronal and immune cells. “+” indicates reported increase, “−” indicates reported reduction in the process. Although evidence suggests that carbon metabolism and anabolism might be affected by cannabinoids through AMPK activity, there are no direct reports of those effect [32,86,98,99,100,109,110,111,112].
| Neuronal | Immune | |
|---|---|---|
| Apoptosis | − | + |
| Carbon metabolism | − | ? |
| OXPHOS | +/− | − |
| Anabolism | ? | ? |
Author Contributions
Conceptualization, C.B., X.D.-L., and J.v.G.; investigation, C.B.; writing—original draft preparation, C.B. and X.D.-L.; writing—review and editing, H.L., R.T., and D.O.; visualization, C.B.; supervision: X.D.-L., and J.v.G.; project administration: J.v.G.; funding acquisition, J.v.G. All authors have read and agreed to the published version of the manuscript.
Funding
The present review was conducted with funds from the Natural Sciences and Engineering Research Council of Canada and the AIDS/Infectious Diseases Network (FRQ-S; Montreal).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Stanley I.A., Ribeiro S.M., Gimenez-Cassina A., Norberg E., Danial N.N. Changing appetites: The adaptive advantages of fuel choice. Trends Cell Biol. 2014;24:118–127. doi: 10.1016/j.tcb.2013.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goodpaster B.H., Sparks L.M. Metabolic Flexibility in Health and Disease. Cell Metab. 2017;25:1027–1036. doi: 10.1016/j.cmet.2017.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rambold A.S., Pearce E.L. Mitochondrial Dynamics at the Interface of Immune Cell Metabolism and Function. Trends Immunol. 2018;39:6–18. doi: 10.1016/j.it.2017.08.006. [DOI] [PubMed] [Google Scholar]
- 4.Desdin-Mico G., Soto-Heredero G., Mittelbrunn M. Mitochondrial activity in T cells. Mitochondrion. 2018;41:51–57. doi: 10.1016/j.mito.2017.10.006. [DOI] [PubMed] [Google Scholar]
- 5.Geltink R.I.K., Kyle R.L., Pearce E.L. Unraveling the Complex Interplay Between T Cell Metabolism and Function. Annu. Rev. Immunol. 2018;36:461–488. doi: 10.1146/annurev-immunol-042617-053019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jones N., Vincent E.E., Cronin J.G., Panetti S., Chambers M., Holm S.R., Owens S.E., Francis N.J., Finlay D.K., Thornton C.A. Akt and STAT5 mediate naive human CD4+ T-cell early metabolic response to TCR stimulation. Nat. Commun. 2019;10:2042. doi: 10.1038/s41467-019-10023-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chapman N.M., Boothby M.R., Chi H. Metabolic coordination of T cell quiescence and activation. Nat. Rev. Immunol. 2020;20:55–70. doi: 10.1038/s41577-019-0203-y. [DOI] [PubMed] [Google Scholar]
- 8.Jacobs S.R., Herman C.E., Maciver N.J., Wofford J.A., Wieman H.L., Hammen J.J., Rathmell J.C. Glucose uptake is limiting in T cell activation and requires CD28-mediated Akt-dependent and independent pathways. J. Immunol. 2008;180:4476–4486. doi: 10.4049/jimmunol.180.7.4476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Menk A.V., Scharping N.E., Moreci R.S., Zeng X., Guy C., Salvatore S., Bae H., Xie J., Young H.A., Wendell S.G., et al. Early TCR Signaling Induces Rapid Aerobic Glycolysis Enabling Distinct Acute T Cell Effector Functions. Cell Rep. 2018;22:1509–1521. doi: 10.1016/j.celrep.2018.01.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Geiger R., Rieckmann J.C., Wolf T., Basso C., Feng Y., Fuhrer T., Kogadeeva M., Picotti P., Meissner F., Mann M., et al. L-Arginine Modulates T Cell Metabolism and Enhances Survival and Anti-tumor Activity. Cell. 2016;167:829–842.e13. doi: 10.1016/j.cell.2016.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ron-Harel N., Ghergurovich J.M., Notarangelo G., LaFleur M.W., Tsubosaka Y., Sharpe A.H., Rabinowitz J.D., Haigis M.C. T Cell Activation Depends on Extracellular Alanine. Cell Rep. 2019;28:3011–3021.e4. doi: 10.1016/j.celrep.2019.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ma E.H., Bantug G., Griss T., Condotta S., Johnson R.M., Samborska B., Mainolfi N., Suri V., Guak H., Balmer M.L., et al. Serine Is an Essential Metabolite for Effector T Cell Expansion. Cell Metab. 2017;25:482. doi: 10.1016/j.cmet.2017.01.014. [DOI] [PubMed] [Google Scholar]
- 13.Bachem A., Makhlouf C., Binger K.J., de Souza D.P., Tull D., Hochheiser K., Whitney P.G., Fernandez-Ruiz D., Dahling S., Kastenmuller W., et al. Microbiota-Derived Short-Chain Fatty Acids Promote the Memory Potential of Antigen-Activated CD8(+) T Cells. Immunity. 2019;51:285–297. doi: 10.1016/j.immuni.2019.06.002. [DOI] [PubMed] [Google Scholar]
- 14.Berod L., Friedrich C., Nandan A., Freitag J., Hagemann S., Harmrolfs K., Sandouk A., Hesse C., Castro C.N., Bahre H., et al. De novo fatty acid synthesis controls the fate between regulatory T and T helper 17 cells. Nat. Med. 2014;20:1327–1333. doi: 10.1038/nm.3704. [DOI] [PubMed] [Google Scholar]
- 15.O’Sullivan D., van der Windt G.J., Huang S.C., Curtis J.D., Chang C.H., Buck M.D., Qiu J., Smith A.M., Lam W.Y., DiPlato L.M., et al. Memory CD8(+) T cells use cell-intrinsic lipolysis to support the metabolic programming necessary for development. Immunity. 2014;41:75–88. doi: 10.1016/j.immuni.2014.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ferrando-Martinez S., Casazza J.P., Leal M., Machmach K., Munoz-Fernandez M.A., Viciana P., Koup R.A., Ruiz-Mateos E. Differential Gag-specific polyfunctional T cell maturation patterns in HIV-1 elite controllers. J. Virol. 2012;86:3667–3674. doi: 10.1128/JVI.07034-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saez-Cirion A., Sinet M., Shin S.Y., Urrutia A., Versmisse P., Lacabaratz C., Boufassa F., Avettand-Fenoel V., Rouzioux C., Delfraissy J.F., et al. Heterogeneity in HIV suppression by CD8 T cells from HIV controllers: Association with Gag-specific CD8 T cell responses. J. Immunol. 2009;182:7828–7837. doi: 10.4049/jimmunol.0803928. [DOI] [PubMed] [Google Scholar]
- 18.Angin M., Volant S., Passaes C., Lecuroux C., Monceaux V., Dillies M.-A., Valle-Casuso J.C., Pancino G., Vaslin B., Le Grand R., et al. Metabolic plasticity of HIV-specific CD8+ T cells is associated with enhanced antiviral potential and natural control of HIV-1 infection. Nat. Metab. 2019;1:704–716. doi: 10.1038/s42255-019-0081-4. [DOI] [PubMed] [Google Scholar]
- 19.Nardacci R., Amendola A., Ciccosanti F., Corazzari M., Esposito V., Vlassi C., Taibi C., Fimia G.M., Del Nonno F., Ippolito G., et al. Autophagy plays an important role in the containment of HIV-1 in nonprogressor-infected patients. Autophagy. 2014;10:1167–1178. doi: 10.4161/auto.28678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xu X., Araki K., Li S., Han J.H., Ye L., Tan W.G., Konieczny B.T., Bruinsma M.W., Martinez J., Pearce E.L., et al. Autophagy is essential for effector CD8(+) T cell survival and memory formation. Nat. Immunol. 2014;15:1152–1161. doi: 10.1038/ni.3025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aviram J., Samuelly-Leichtag G. Efficacy of Cannabis-Based Medicines for Pain Management: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Pain Physician. 2017;20:E755–E796. [PubMed] [Google Scholar]
- 22.Mucke M., Phillips T., Radbruch L., Petzke F., Hauser W. Cannabis-based medicines for chronic neuropathic pain in adults. Cochrane Database Syst. Rev. 2018;3:CD012182. doi: 10.1002/14651858.CD012182.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bonini S.A., Premoli M., Tambaro S., Kumar A., Maccarinelli G., Memo M., Mastinu A. Cannabis sativa: A comprehensive ethnopharmacological review of a medicinal plant with a long history. J. Ethnopharmacol. 2018;227:300–315. doi: 10.1016/j.jep.2018.09.004. [DOI] [PubMed] [Google Scholar]
- 24.Tahamtan A., Tavakoli-Yaraki M., Rygiel T.P., Mokhtari-Azad T., Salimi V. Effects of cannabinoids and their receptors on viral infections. J. Med. Virol. 2016;88:1–12. doi: 10.1002/jmv.24292. [DOI] [PubMed] [Google Scholar]
- 25.Acharya N., Penukonda S., Shcheglova T., Hagymasi A.T., Basu S., Srivastava P.K. Endocannabinoid system acts as a regulator of immune homeostasis in the gut. Proc. Natl. Acad. Sci. USA. 2017;114:5005–5010. doi: 10.1073/pnas.1612177114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Roth M.D., Baldwin G.C., Tashkin D.P. Effects of delta-9-tetrahydrocannabinol on human immune function and host defense. Chem. Phys. Lipids. 2002;121:229–239. doi: 10.1016/S0009-3084(02)00159-7. [DOI] [PubMed] [Google Scholar]
- 27.Eisenstein T.K., Meissler J.J. Effects of Cannabinoids on T-cell Function and Resistance to Infection. J. Neuroimmune Pharmacol. Off. J. Soc. NeuroImmune Pharmacol. 2015;10:204–216. doi: 10.1007/s11481-015-9603-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tanasescu R., Constantinescu C.S. Cannabinoids and the immune system: An overview. Immunobiology. 2010;215:588–597. doi: 10.1016/j.imbio.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 29.Lu H.C., Mackie K. An Introduction to the Endogenous Cannabinoid System. Biol. Psychiatry. 2016;79:516–525. doi: 10.1016/j.biopsych.2015.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dando I., Donadelli M., Costanzo C., Dalla Pozza E., D’Alessandro A., Zolla L., Palmieri M. Cannabinoids inhibit energetic metabolism and induce AMPK-dependent autophagy in pancreatic cancer cells. Cell Death Dis. 2013;4:e664. doi: 10.1038/cddis.2013.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu J., Godlewski G., Jourdan T., Liu Z., Cinar R., Xiong K., Kunos G. Cannabinoid-1 Receptor Antagonism Improves Glycemic Control and Increases Energy Expenditure Through Sirtuin-1/Mechanistic Target of Rapamycin Complex 2 and 5′Adenosine Monophosphate-Activated Protein Kinase Signaling. Hepatology. 2019;69:1535–1548. doi: 10.1002/hep.30364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van Niekerk G., Mabin T., Engelbrecht A.M. Anti-inflammatory mechanisms of cannabinoids: An immunometabolic perspective. Inflammopharmacology. 2019;27:39–46. doi: 10.1007/s10787-018-00560-7. [DOI] [PubMed] [Google Scholar]
- 33.Loucif H., Dagenais-Lussier X., Beji C., Telittchenko R., Routy J.P., van Grevenynghe J. Plasticity in T-cell mitochondrial metabolism: A necessary peacekeeper during the troubled times of persistent HIV-1 infection. Cytokine Growth Factor Rev. 2020 doi: 10.1016/j.cytogfr.2020.02.004. [DOI] [PubMed] [Google Scholar]
- 34.Costiniuk C.T., Jenabian M.-A. Cannabinoids and inflammation. Aids. 2019 doi: 10.1097/QAD.0000000000002345. [DOI] [PubMed] [Google Scholar]
- 35.Hernandez-Cervantes R., Mendez-Diaz M., Prospero-Garcia O., Morales-Montor J. Immunoregulatory Role of Cannabinoids during Infectious Disease. Neuroimmunomodulation. 2017;24:183–199. doi: 10.1159/000481824. [DOI] [PubMed] [Google Scholar]
- 36.Karmaus P.W., Chen W., Crawford R., Kaplan B.L., Kaminski N.E. Delta9-tetrahydrocannabinol impairs the inflammatory response to influenza infection: Role of antigen-presenting cells and the cannabinoid receptors 1 and 2. Toxicol. Sci. Off. J. Soc. Toxicol. 2013;131:419–433. doi: 10.1093/toxsci/kfs315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sun L.J., Yu J.W., Wan L., Zhang X.Y., Shi Y.G., Chen M.Y. Endocannabinoid system activation contributes to glucose metabolism disorders of hepatocytes and promotes hepatitis C virus replication. Int. J. Infect. Dis. IJID Off. Publ. Int. Soc. Infect. Dis. 2014;23:75–81. doi: 10.1016/j.ijid.2013.12.017. [DOI] [PubMed] [Google Scholar]
- 38.Huemer H.P., Lassnig C., Bernhard D., Sturm S., Nowotny N., Kitchen M., Pavlic M. Cannabinoids lead to enhanced virulence of the smallpox vaccine (vaccinia) virus. Immunobiology. 2011;216:670–677. doi: 10.1016/j.imbio.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 39.Chen W., Crawford R.B., Kaplan B.L., Kaminski N.E. Modulation of HIVGP120 Antigen-Specific Immune Responses In Vivo by Delta9-Tetrahydrocannabinol. J. Neuroimmune Pharmacol. official J. Soc. Neuroimmune Pharmacol. 2015;10:344–355. doi: 10.1007/s11481-015-9597-x. [DOI] [PubMed] [Google Scholar]
- 40.Costantino C.M., Gupta A., Yewdall A.W., Dale B.M., Devi L.A., Chen B.K. Cannabinoid receptor 2-mediated attenuation of CXCR4-tropic HIV infection in primary CD4+ T cells. PLoS ONE. 2012;7:e33961. doi: 10.1371/journal.pone.0033961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hermes D.J., Xu C., Poklis J.L., Niphakis M.J., Cravatt B.F., Mackie K., Lichtman A.H., Ignatowska-Jankowska B.M., Fitting S. Neuroprotective effects of fatty acid amide hydrolase catabolic enzyme inhibition in a HIV-1 Tat model of neuroAIDS. Neuropharmacology. 2018;141:55–65. doi: 10.1016/j.neuropharm.2018.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Xu C., Hermes D.J., Nwanguma B., Jacobs I.R., Mackie K., Mukhopadhyay S., Lichtman A.H., Ignatowska-Jankowska B., Fitting S. Endocannabinoids exert CB1 receptor-mediated neuroprotective effects in models of neuronal damage induced by HIV-1 Tat protein. Mol. Cell Neurosci. 2017;83:92–102. doi: 10.1016/j.mcn.2017.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hu S., Sheng W.S., Rock R.B. CB2 receptor agonists protect human dopaminergic neurons against damage from HIV-1 gp120. PLoS ONE. 2013;8:e77577. doi: 10.1371/journal.pone.0077577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Feliu A., Bonilla Del Rio I., Carrillo-Salinas F.J., Hernandez-Torres G., Mestre L., Puente N., Ortega-Gutierrez S., Lopez-Rodriguez M.L., Grandes P., Mecha M., et al. 2-Arachidonoylglycerol Reduces Proteoglycans and Enhances Remyelination in a Progressive Model of Demyelination. J. Neurosci. 2017;37:8385–8398. doi: 10.1523/JNEUROSCI.2900-16.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Patel D.C., Wallis G., Fujinami R.S., Wilcox K.S., Smith M.D. Cannabidiol reduces seizures following CNS infection with Theiler’s murine encephalomyelitis virus. Epilepsia Open. 2019;4:431–442. doi: 10.1002/epi4.12351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dagenais-Lussier X., Loucif H., Murira A., Laulhe X., Stager S., Lamarre A., van Grevenynghe J. Sustained IFN-I Expression during Established Persistent Viral Infection: A “Bad Seed” for Protective Immunity. Viruses. 2017;10:12. doi: 10.3390/v10010012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Loucif H., Gouard S., Dagenais-Lussier X., Murira A., Stager S., Tremblay C., Van Grevenynghe J. Deciphering natural control of HIV-1: A valuable strategy to achieve antiretroviral therapy termination. Cytokine Growth Factor Rev. 2018;40:90–98. doi: 10.1016/j.cytogfr.2018.03.010. [DOI] [PubMed] [Google Scholar]
- 48.Henriquez J.E., Rizzo M.D., Crawford R.B., Gulick P., Kaminski N.E. Interferon-alpha-Mediated Activation of T Cells from Healthy and HIV-Infected Individuals Is Suppressed by Delta(9)-Tetrahydrocannabinol. J. Pharmacol. Exp. Ther. 2018;367:49–58. doi: 10.1124/jpet.118.250308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Henriquez J.E., Rizzo M.D., Schulz M.A., Crawford R.B., Gulick P., Kaminski N.E. Delta9-Tetrahydrocannabinol Suppresses Secretion of IFNalpha by Plasmacytoid Dendritic Cells From Healthy and HIV-Infected Individuals. J. Acquir. Immune. Defic. Syndr. 2017;75:588–596. doi: 10.1097/QAI.0000000000001449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kumar V., Torben W., Mansfield J., Alvarez X., Vande Stouwe C., Li J., Byrareddy S.N., Didier P.J., Pahar B., Molina P.E., et al. Cannabinoid Attenuation of Intestinal Inflammation in Chronic SIV-Infected Rhesus Macaques Involves T Cell Modulation and Differential Expression of Micro-RNAs and Pro-inflammatory Genes. Front. Immunol. 2019;10:914. doi: 10.3389/fimmu.2019.00914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tahamtan A., Tavakoli-Yaraki M., Shadab A., Rezaei F., Marashi S.M., Shokri F., Mokhatri-Azad T., Salimi V. The Role of Cannabinoid Receptor 1 in the Immunopathology of Respiratory Syncytial Virus. Viral Immunol. 2018;31:292–298. doi: 10.1089/vim.2017.0098. [DOI] [PubMed] [Google Scholar]
- 52.Tahamtan A., Samieipoor Y., Nayeri F.S., Rahbarimanesh A.A., Izadi A., Rashidi-Nezhad A., Tavakoli-Yaraki M., Farahmand M., Bont L., Shokri F., et al. Effects of cannabinoid receptor type 2 in respiratory syncytial virus infection in human subjects and mice. Virulence. 2018;9:217–230. doi: 10.1080/21505594.2017.1389369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cockerham L.R., Siliciano J.D., Sinclair E., O’Doherty U., Palmer S., Yukl S.A., Strain M.C., Chomont N., Hecht F.M., Siliciano R.F., et al. CD4+ and CD8+ T cell activation are associated with HIV DNA in resting CD4+ T cells. PLoS ONE. 2014;9:e110731. doi: 10.1371/journal.pone.0110731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Haas A., Zimmermann K., Oxenius A. Antigen-dependent and -independent mechanisms of T and B cell hyperactivation during chronic HIV-1 infection. J. Virol. 2011;85:12102–12113. doi: 10.1128/JVI.05607-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Day C.L., Kaufmann D.E., Kiepiela P., Brown J.A., Moodley E.S., Reddy S., Mackey E.W., Miller J.D., Leslie A.J., DePierres C., et al. PD-1 expression on HIV-specific T cells is associated with T-cell exhaustion and disease progression. Nature. 2006;443:350–354. doi: 10.1038/nature05115. [DOI] [PubMed] [Google Scholar]
- 56.Trautmann L., Janbazian L., Chomont N., Said E.A., Gimmig S., Bessette B., Boulassel M.R., Delwart E., Sepulveda H., Balderas R.S., et al. Upregulation of PD-1 expression on HIV-specific CD8+ T cells leads to reversible immune dysfunction. Nat. Med. 2006;12:1198–1202. doi: 10.1038/nm1482. [DOI] [PubMed] [Google Scholar]
- 57.Ogando J., Saez M.E., Santos J., Nuevo-Tapioles C., Gut M., Esteve-Codina A., Heath S., Gonzalez-Perez A., Cuezva J.M., Lacalle R.A., et al. PD-1 signaling affects cristae morphology and leads to mitochondrial dysfunction in human CD8(+) T lymphocytes. J. Immunother Cancer. 2019;7:151. doi: 10.1186/s40425-019-0628-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Maagaard A., Holberg-Petersen M., Lovgarden G., Holm M., Pettersen F.O., Kvale D. Distinct mechanisms for mitochondrial DNA loss in T and B lymphocytes from HIV-infected patients exposed to nucleoside reverse-transcriptase inhibitors and those naive to antiretroviral treatment. J. Infect Dis. 2008;198:1474–1481. doi: 10.1086/592713. [DOI] [PubMed] [Google Scholar]
- 59.Apostolova N., Blas-Garcia A., Esplugues J.V. Mitochondrial toxicity in HAART: An overview of in vitro evidence. Curr. Pharm. Des. 2011;17:2130–2144. doi: 10.2174/138161211796904731. [DOI] [PubMed] [Google Scholar]
- 60.Song S., Gong S., Singh P., Lyu J., Bai Y. The interaction between mitochondria and oncoviruses. Biochim. Biophys. Acta Mol. Basis Dis. 2018;1864:481–487. doi: 10.1016/j.bbadis.2017.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lai J.H., Luo S.F., Ho L.J. Operation of mitochondrial machinery in viral infection-induced immune responses. Biochem. Pharmacol. 2018;156:348–356. doi: 10.1016/j.bcp.2018.08.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.de Armas-Rillo L., Valera M.S., Marrero-Hernandez S., Valenzuela-Fernandez A. Membrane dynamics associated with viral infection. Rev. Med Virol. 2016;26:146–160. doi: 10.1002/rmv.1872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Manuzak J.A., Gott T.M., Kirkwood J.S., Coronado E., Hensley-McBain T., Miller C., Cheu R.K., Collier A.C., Funderburg N.T., Martin J.N., et al. Heavy Cannabis Use Associated With Reduction in Activated and Inflammatory Immune Cell Frequencies in Antiretroviral Therapy-Treated Human Immunodeficiency Virus-Infected Individuals. Clin. Infect Dis. 2018;66:1872–1882. doi: 10.1093/cid/cix1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Krishnan G., Chatterjee N. Endocannabinoids affect innate immunity of Muller glia during HIV-1 Tat cytotoxicity. Mol. Cell Neurosci. 2014;59:10–23. doi: 10.1016/j.mcn.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 65.Williams J.C., Appelberg S., Goldberger B.A., Klein T.W., Sleasman J.W., Goodenow M.M. Delta(9)-Tetrahydrocannabinol treatment during human monocyte differentiation reduces macrophage susceptibility to HIV-1 infection. J. Neuroimmune Pharmacol. Off. J. Soc. Neuroimmune Pharmacol. 2014;9:369–379. doi: 10.1007/s11481-014-9527-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Raborn E.S., Jamerson M., Marciano-Cabral F., Cabral G.A. Cannabinoid inhibits HIV-1 Tat-stimulated adhesion of human monocyte-like cells to extracellular matrix proteins. Life Sci. 2014;104:15–23. doi: 10.1016/j.lfs.2014.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ramirez S.H., Reichenbach N.L., Fan S., Rom S., Merkel S.F., Wang X., Ho W.Z., Persidsky Y. Attenuation of HIV-1 replication in macrophages by cannabinoid receptor 2 agonists. J. Leukoc. Biol. 2013;93:801–810. doi: 10.1189/jlb.1012523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chen W., Kaplan B.L., Pike S.T., Topper L.A., Lichorobiec N.R., Simmons S.O., Ramabhadran R., Kaminski N.E. Magnitude of stimulation dictates the cannabinoid-mediated differential T cell response to HIVgp120. J. Leukoc. Biol. 2012;92:1093–1102. doi: 10.1189/jlb.0212082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fraga D., Raborn E.S., Ferreira G.A., Cabral G.A. Cannabinoids inhibit migration of microglial-like cells to the HIV protein Tat. J. Neuroimmune Pharmacol. Off. J. Soc. Neuroimmune Pharmacol. 2011;6:566–577. doi: 10.1007/s11481-011-9291-6. [DOI] [PubMed] [Google Scholar]
- 70.Kim H.J., Shin A.H., Thayer S.A. Activation of cannabinoid type 2 receptors inhibits HIV-1 envelope glycoprotein gp120-induced synapse loss. Mol. Pharmacol. 2011;80:357–366. doi: 10.1124/mol.111.071647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Raborn E.S., Cabral G.A. Cannabinoid inhibition of macrophage migration to the trans-activating (Tat) protein of HIV-1 is linked to the CB(2) cannabinoid receptor. J. Pharmacol. Exp. Ther. 2010;333:319–327. doi: 10.1124/jpet.109.163055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chandra L.C., Kumar V., Torben W., Vande Stouwe C., Winsauer P., Amedee A., Molina P.E., Mohan M. Chronic administration of Delta9-tetrahydrocannabinol induces intestinal anti-inflammatory microRNA expression during acute simian immunodeficiency virus infection of rhesus macaques. J. Virol. 2015;89:1168–1181. doi: 10.1128/JVI.01754-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.LeCapitaine N.J., Zhang P., Winsauer P., Walker E., Vande Stouwe C., Porretta C., Molina P.E. Chronic Delta-9-tetrahydrocannabinol administration increases lymphocyte CXCR4 expression in rhesus macaques. J. Neuroimmune Pharmacol. Off. J. Soc. Neuroimmune Pharmacol. 2011;6:540–545. doi: 10.1007/s11481-011-9277-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Molina P.E., Winsauer P., Zhang P., Walker E., Birke L., Amedee A., Stouwe C.V., Troxclair D., McGoey R., Varner K., et al. Cannabinoid administration attenuates the progression of simian immunodeficiency virus. AIDS Res. Hum. Retrovir. 2011;27:585–592. doi: 10.1089/aid.2010.0218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sheng W.S., Chauhan P., Hu S., Prasad S., Lokensgard J.R. Antiallodynic Effects of Cannabinoid Receptor 2 (CB2R) Agonists on Retrovirus Infection-Induced Neuropathic Pain. Pain Res. Manag. 2019;2019:1260353. doi: 10.1155/2019/1260353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sato A., Ono C., Tamura T., Mori H., Izumi T., Torii S., Fauzyah Y., Yamamoto T., Morioka Y., Okuzaki D., et al. Rimonabant suppresses RNA transcription of hepatitis B virus by inhibiting hepatocyte nuclear factor 4alpha. Microbiol. Immunol. 2020;64:345–355. doi: 10.1111/1348-0421.12777. [DOI] [PubMed] [Google Scholar]
- 77.Arevalo-Martin A., Molina-Holgado E., Guaza C. A CB(1)/CB(2) receptor agonist, WIN 55,212-2, exerts its therapeutic effect in a viral autoimmune model of multiple sclerosis by restoring self-tolerance to myelin. Neuropharmacology. 2012;63:385–393. doi: 10.1016/j.neuropharm.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 78.Mestre L., Inigo P.M., Mecha M., Correa F.G., Hernangomez-Herrero M., Loria F., Docagne F., Borrell J., Guaza C. Anandamide inhibits Theiler’s virus induced VCAM-1 in brain endothelial cells and reduces leukocyte transmigration in a model of blood brain barrier by activation of CB(1) receptors. J. Neuroinflammation. 2011;8:102. doi: 10.1186/1742-2094-8-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hebert-Chatelain E., Reguero L., Puente N., Lutz B., Chaouloff F., Rossignol R., Piazza P.V., Benard G., Grandes P., Marsicano G. Cannabinoid control of brain bioenergetics: Exploring the subcellular localization of the CB1 receptor. Mol. Metab. 2014;3:495–504. doi: 10.1016/j.molmet.2014.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hebert-Chatelain E., Desprez T., Serrat R., Bellocchio L., Soria-Gomez E., Busquets-Garcia A., Pagano Zottola A.C., Delamarre A., Cannich A., Vincent P., et al. A cannabinoid link between mitochondria and memory. Nature. 2016;539:555–559. doi: 10.1038/nature20127. [DOI] [PubMed] [Google Scholar]
- 81.Piomelli D. A mighty (ochondrial) fight? Mol. Metab. 2014;3:345–346. doi: 10.1016/j.molmet.2014.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Morozov Y.M., Dominguez M.H., Varela L., Shanabrough M., Koch M., Horvath T.L., Rakic P. Antibodies to cannabinoid type 1 receptor co-react with stomatin-like protein 2 in mouse brain mitochondria. Eur. J. Neurosci. 2013;38:2341–2348. doi: 10.1111/ejn.12237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Djeungoue-Petga M.A., Hebert-Chatelain E. Linking Mitochondria and Synaptic Transmission: The CB1 Receptor. BioEssays News Rev. Mol. Cell. Dev. Biol. 2017;39:1700126. doi: 10.1002/bies.201700126. [DOI] [PubMed] [Google Scholar]
- 84.Mancini G., Horvath T.L. Mitochondria Bioenergetic and Cognitive Functions: The Cannabinoid Link. Trends Cell Biol. 2017;27:391–392. doi: 10.1016/j.tcb.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 85.Harkany T., Horvath T.L. (S)Pot on Mitochondria: Cannabinoids Disrupt Cellular Respiration to Limit Neuronal Activity. Cell Metab. 2017;25:8–10. doi: 10.1016/j.cmet.2016.12.020. [DOI] [PubMed] [Google Scholar]
- 86.Jimenez-Blasco D., Busquets-Garcia A., Hebert-Chatelain E., Serrat R., Vicente-Gutierrez C., Ioannidou C., Gomez-Sotres P., Lopez-Fabuel I., Resch-Beusher M., Resel E., et al. Glucose metabolism links astroglial mitochondria to cannabinoid effects. Nature. 2020;583:603–608. doi: 10.1038/s41586-020-2470-y. [DOI] [PubMed] [Google Scholar]
- 87.Kataoka K., Bilkei-Gorzo A., Nozaki C., Togo A., Nakamura K., Ohta K., Zimmer A., Asahi T. Age-dependent Alteration in Mitochondrial Dynamics and Autophagy in Hippocampal Neuron of Cannabinoid CB1 Receptor-deficient Mice. Brain Res. Bull. 2020;160:40–49. doi: 10.1016/j.brainresbull.2020.03.014. [DOI] [PubMed] [Google Scholar]
- 88.Fisar Z., Singh N., Hroudova J. Cannabinoid-induced changes in respiration of brain mitochondria. Toxicol. Lett. 2014;231:62–71. doi: 10.1016/j.toxlet.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 89.Bino T., Chari-Bitron A., Shahar A. Biochemical effects and morphological changes in rat liver mitochondria exposed to 1 -tetrahydrocannabinol. Biochim. Biophys. Acta. 1972;288:195–202. doi: 10.1016/0005-2736(72)90238-6. [DOI] [PubMed] [Google Scholar]
- 90.Mahoney J.M., Harris R.A. Effect of 9 -tetrahydrocannabinol on mitochondrial processes. Biochem. Pharmacol. 1972;21:1217–1226. doi: 10.1016/0006-2952(72)90283-3. [DOI] [PubMed] [Google Scholar]
- 91.Drori A., Permyakova A., Hadar R., Udi S., Nemirovski A., Tam J. Cannabinoid-1 receptor regulates mitochondrial dynamics and function in renal proximal tubular cells. Diabetes Obes. Metab. 2019;21:146–159. doi: 10.1111/dom.13497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Augusto-Oliveira M., Arrifano G.P., Lopes-Araujo A., Santos-Sacramento L., Takeda P.Y., Anthony D.C., Malva J.O., Crespo-Lopez M.E. What Do Microglia Really Do in Healthy Adult Brain? Cells. 2019;8:1293. doi: 10.3390/cells8101293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ma L., Niu W., Lv J., Jia J., Zhu M., Yang S. PGC-1alpha-Mediated Mitochondrial Biogenesis is Involved in Cannabinoid Receptor 2 Agonist AM1241-Induced Microglial Phenotype Amelioration. Cell. Mol. Neurobiol. 2018;38:1529–1537. doi: 10.1007/s10571-018-0628-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Nichols J.M., Kaplan B.L.F. Immune Responses Regulated by Cannabidiol. Cannabis Cannabinoid Res. 2020;5:12–31. doi: 10.1089/can.2018.0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Muthumalage T., Rahman I. Cannabidiol differentially regulates basal and LPS-induced inflammatory responses in macrophages, lung epithelial cells, and fibroblasts. Toxicol. Appl. Pharmacol. 2019;382:114713. doi: 10.1016/j.taap.2019.114713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bock F.J., Tait S.W.G. Mitochondria as multifaceted regulators of cell death. Nat. Rev. Mol. Cell Biol. 2020;21:85–100. doi: 10.1038/s41580-019-0173-8. [DOI] [PubMed] [Google Scholar]
- 97.Estaquier J., Vallette F., Vayssiere J.L., Mignotte B. The mitochondrial pathways of apoptosis. Adv. Exp. Med. Biol. 2012;942:157–183. doi: 10.1007/978-94-007-2869-1_7. [DOI] [PubMed] [Google Scholar]
- 98.Rieder S.A., Chauhan A., Singh U., Nagarkatti M., Nagarkatti P. Cannabinoid-induced apoptosis in immune cells as a pathway to immunosuppression. Immunobiology. 2010;215:598–605. doi: 10.1016/j.imbio.2009.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Wu H.Y., Huang C.H., Lin Y.H., Wang C.C., Jan T.R. Cannabidiol induced apoptosis in human monocytes through mitochondrial permeability transition pore-mediated ROS production. Free Radic. Biol. Med. 2018;124:311–318. doi: 10.1016/j.freeradbiomed.2018.06.023. [DOI] [PubMed] [Google Scholar]
- 100.Schultze N., Wanka H., Zwicker P., Lindequist U., Haertel B. Mitochondrial functions of THP-1 monocytes following the exposure to selected natural compounds. Toxicology. 2017;377:57–63. doi: 10.1016/j.tox.2016.12.006. [DOI] [PubMed] [Google Scholar]
- 101.Vaeth M., Feske S. Ion channelopathies of the immune system. Curr. Opin. Immunol. 2018;52:39–50. doi: 10.1016/j.coi.2018.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Trebak M., Kinet J.P. Calcium signalling in T cells. Nat. Rev. Immunol. 2019;19:154–169. doi: 10.1038/s41577-018-0110-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Olivas-Aguirre M., Torres-Lopez L., Valle-Reyes J.S., Hernandez-Cruz A., Pottosin I., Dobrovinskaya O. Cannabidiol directly targets mitochondria and disturbs calcium homeostasis in acute lymphoblastic leukemia. Cell Death Dis. 2019;10:779. doi: 10.1038/s41419-019-2024-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hoth M., Fanger C.M., Lewis R.S. Mitochondrial regulation of store-operated calcium signaling in T lymphocytes. J. Cell Biol. 1997;137:633–648. doi: 10.1083/jcb.137.3.633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Fattore L., Spano M.S., Altea S., Fadda P., Fratta W. Drug- and cue-induced reinstatement of cannabinoid-seeking behaviour in male and female rats: Influence of ovarian hormones. Br. J. Pharmacol. 2010;160:724–735. doi: 10.1111/j.1476-5381.2010.00734.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Narimatsu S., Watanabe K., Yamamoto I., Yoshimura H. Sex difference in the oxidative metabolism of delta 9-tetrahydrocannabinol in the rat. Biochem. Pharmacol. 1991;41:1187–1194. doi: 10.1016/0006-2952(91)90657-Q. [DOI] [PubMed] [Google Scholar]
- 107.Gorey C., Kuhns L., Smaragdi E., Kroon E., Cousijn J. Age-related differences in the impact of cannabis use on the brain and cognition: A systematic review. Eur. Arch. Psychiatry Clin. Neurosci. 2019;269:37–58. doi: 10.1007/s00406-019-00981-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Costiniuk C.T., Saneei Z., Routy J.P., Margolese S., Mandarino E., Singer J., Lebouche B., Cox J., Szabo J., Brouillette M.J., et al. Oral cannabinoids in people living with HIV on effective antiretroviral therapy: CTN PT028-study protocol for a pilot randomised trial to assess safety, tolerability and effect on immune activation. BMJ Open. 2019;9:e024793. doi: 10.1136/bmjopen-2018-024793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Fujii M., Sherchan P., Soejima Y., Hasegawa Y., Flores J., Doycheva D., Zhang J.H. Cannabinoid receptor type 2 agonist attenuates apoptosis by activation of phosphorylated CREB-Bcl-2 pathway after subarachnoid hemorrhage in rats. Exp. Neurol. 2014;261:396–403. doi: 10.1016/j.expneurol.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Nguyen C.H., Krewenka C., Radad K., Kranner B., Huber A., Duvigneau J.C., Miller I., Moldzio R. THC (Delta9-Tetrahydrocannabinol) Exerts Neuroprotective Effect in Glutamate-affected Murine Primary Mesencephalic Cultures Through Restoring Mitochondrial Membrane Potential and Anti-apoptosis Involving CB1 Receptor-dependent Mechanism. Phytother Res. 2016;30:2044–2052. doi: 10.1002/ptr.5712. [DOI] [PubMed] [Google Scholar]
- 111.Viscomi M.T., Oddi S., Latini L., Bisicchia E., Maccarrone M., Molinari M. The endocannabinoid system: A new entry in remote cell death mechanisms. Exp. Neurol. 2010;224:56–65. doi: 10.1016/j.expneurol.2010.03.023. [DOI] [PubMed] [Google Scholar]
- 112.Xu Z., Lv X.A., Dai Q., Ge Y.Q., Xu J. Acute upregulation of neuronal mitochondrial type-1 cannabinoid receptor and it’s role in metabolic defects and neuronal apoptosis after TBI. Mol. Brain. 2016;9:75. doi: 10.1186/s13041-016-0257-8. [DOI] [PMC free article] [PubMed] [Google Scholar]