Abstract
Background
Airway management in patients with hereditary heart disease is an important therapeutic intervention.
Objectives
The purpose of this study was to compare direct laryngoscopy (DL) with video laryngoscopy (VL) in pediatric airways management for congenital heart surgery.
Methods
This study was designed as a prospective randomized clinical trial. Two consecutive groups of 30 patients undergoing elective noncyanotic congenital heart surgery. The patients were divided into direct laryngoscopy versus video laryngoscopy for intubation of the trachea. The main outcomes were the number of success rate in the first attempt, and the secondary outcomes were the duration of successful intubation and complications, such as desaturation and bradycardia.
Results
Intubation procedure time was measured as 51.13 ± 17.88 seconds for the group with direct laryngoscopy and 59.66 ± 45.91 seconds for group with VL that was significant (P = 0.006). In DL group, 22 patients were intubated on the first attempt, 8 patients on the second attempt, and 6 patients on the third attempt, compared to 24, 6, and 2 respectively, in VL group. The differences were significant only in the third attempt between groups (P = 0.033). The important difference established in heart rate (HR) and SpaO2 amounts between the two groups at any time (P < 0.05).
Conclusions
VL can produce better visualization for intubation of trachea in congenital heart disease, but this is time-consuming. Indeed, training in the use of the VL should be increased to reduce the time required for performance. Moreover, further studies are recommended to approve these helpful findings.
Keywords: Airway Management, Children Congenital Heart Disease, Direct Laryngoscopy, Video Laryngoscopy
1. Background
Endotracheal intubation is a life‐saving procedure performed in pediatrics for the protection of the airway, improving oxygenation, and accomplish acceptable ventilation. Visibility of the airway and the related structures as imperative factors required for successful intubation. In infants and children, the low cardiopulmonary reserve and high oxygen consumption can reduce the time required for teaching and correction during direct laryngoscopy (DL) considered as the most common method for airway management and orotracheal intubation. In this technique as indirect laryngoscopy, occasionally, the larynx visibility unexpected weakness as well as vocal cords by a non-direct vision can observe (1). The orotracheal intubation is an essential approach for airway protection in emergency care, but in these situations, it can be challenging due to the patient often life-threatening conditions (2). On the other hand, mouth opening limitations, instability of neck spine, blood or fluid secretion in airway passage, and facial injuries, as well as the experience of present physicians, were the factors that cause the challenge for airway establishing (2). In the first attempt for emergency patients, the success rate of intubation is relatively low, and long or failed intubation can cause major complications (3). Airway related complications are the most common critical adverse events in pediatric anesthesia, which are four times more common in infants and newborns than older children. For airway management in pediatric, both awareness and preparation are required (4). Although the problems of airway management are minor, but often severe. Many improvements in airway management, as well as advances in devices and technologies, have increased the ability of physicians to manage difficult airways in children. In this line, a video laryngoscope (VL), developed in the 21st century, is a device containing a small blubber tip that helps indirectly to look at the glottis. Many studies have shown that the VL glottis view has several advantages compared to DL. Over the last few years, VLs have received much attention as new devices for airway management in children (2, 3, 5). In this regard, a recent meta-analysis that focused on patients in intensive care units showed that VL reduced the difficulty of intubation and increased success rate in the first try compared to DL (1) However, it cannot reduce the intubation time and the number of tries for intubation (5). On the other hand, in several recent clinical trials, DL was compared to the laryngoscopy via video in emergency cases, and some of them did not have many advantages in terms of the success rate or intubation time, which can be due to requirements for more experience and training with this device (2, 3, 6, 7). Airway management in patients with congenital heart disease (CHD) is an important therapeutic intervention to provide these patients with the critical disease, surgery, and other procedures. In addition, airway management in these patients is strategic by the lesser reserve of the cardiopulmonary system due to cardiac pathophysiology, and the significant occurrence of the anomaly of craniofacial and airway in these people (8). Extrinsic airway compression frequently complicates the sequence of CHD repair evaluated by computed tomography (CT) in CHD patients (9). No sufficient data is showing that VL agreements a benefit over direct laryngoscopy in the managing of difficult airways in pediatric patients with CHD.
2. Objectives
This study aimed to compare DL with VL in pediatric airways management in terms of congenital heart surgery.
3. Methods
3.1. Study Design and Sample Size
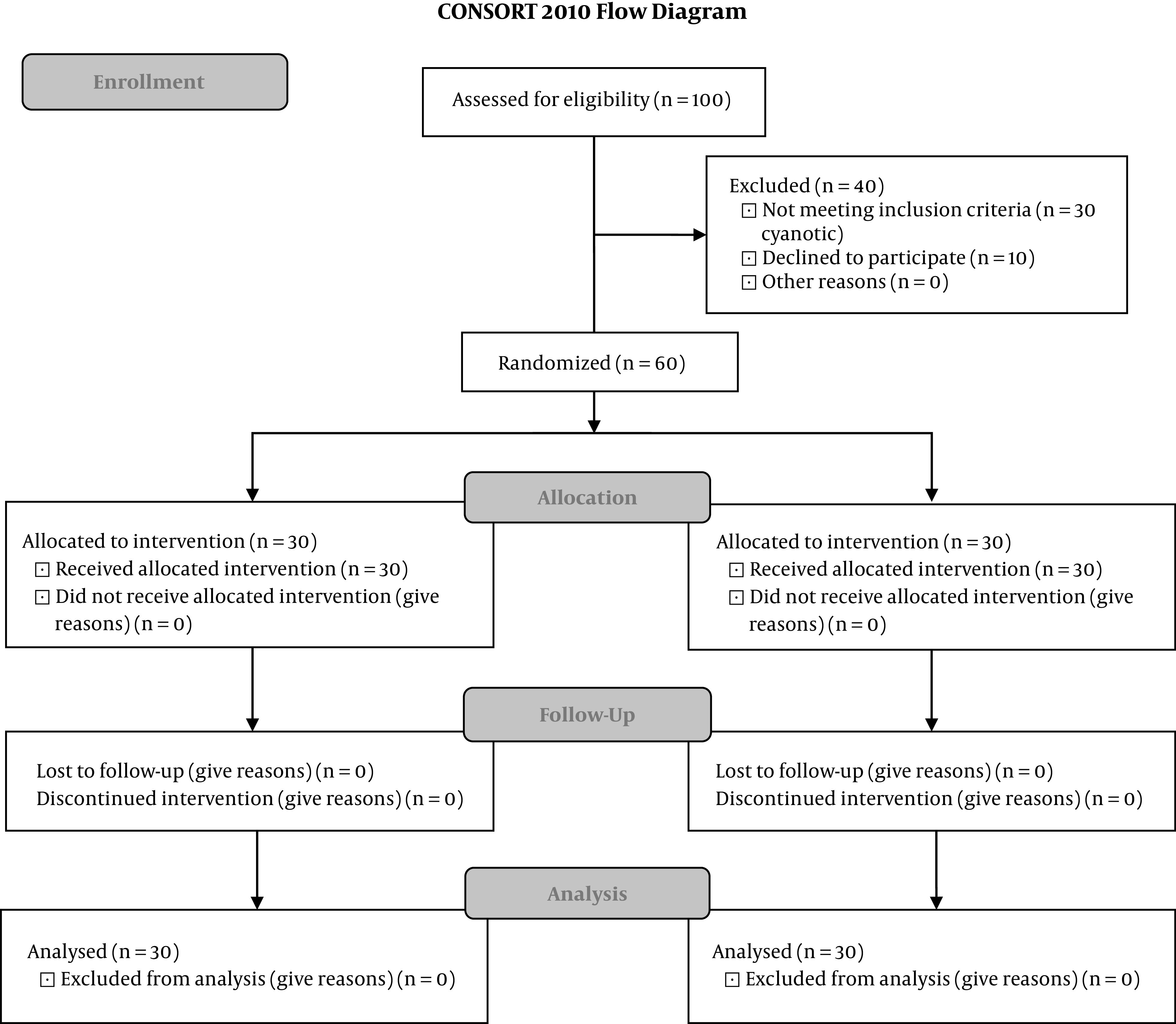
This prospective randomized clinical trial was conducted from September 2018 to March 2019 in Golestan Hospital, Ahvaz, Iran. During the study period, 100 children undergoing elective congenital cardiac surgery were eligible for contributing to the study. 90 Parents of patients decided to contribute and providing consent from parents. Amongst them, 30 patients did not have inclusion criteria (were cyanotic). Finally, 60 cases remained involved in two groups, including DL and VL (30 patients in each group, Figure 1). Inclusion criteria were 1 - 5 years old children, weighting between 3 - 15 kg, scheduled for elective non-cyanotic congenital heart surgery with anesthesiologists classification (ASA) class of 1 - 3; The exclusion criteria included the difficulty of the airway (such as anomaly of craniofacial), risk of pulmonary aspiration and reactive airway disease. The preoperative visit was done one day before surgery by an anesthesiologist that was blind from research. Informed written consent was obtained from the parents of children. All of the patients were kept fasting, according to standard fasting guidelines. In the operating room (OR), randomization of children to VL and direct DL was performed based on a computer-generated random number table. Closed opaque covers were unlocked in the OR, and the intubation method rendering to the specific randomized group was decided. The routine monitors (electrocardiogram, noninvasive blood pressure, and pulse oximetry) were attached to the child. The anesthesia was induced by 100% O2 and sevoflurane with the mapelson system. Following ventilation, 10 µg/kg fentanyl, and 0.5 mg/kg atracurium were injected intravenously. Upon the muscle relaxation, intubations were performed by one anesthetic assistants who has experience with about 40 months of anesthesia education period and intubated a certain number of patients in two ways and have the necessary experience under the supervision of attending of anesthesia. Patient selection for DL or VL was based on a simple random table with a miller blade 0 to 2 (depending on the child’s age). At first, the view of glottis determined by DL, and then intubation was performed by VL (Infant view control unit, Germany). In the patients who were suitable for intubation with the DL, the video laryngoscopic view was first recorded, and then intubation was performed by a direct laryngoscope. Intubation time (IT) was also recorded in each group. In addition, IT was defined as the time from the end of preoxygenation to intubate, and intubation procedures time (IPT) was defined as the time from the end of preoxygenation to the first detection of end-tidal CO2. Moreover, IPT involved the time between efforts and the time to fixation ETT. Effort numbers were also noted, and more than one effort was mandatory. Between efforts, the patient also established mask ventilation. After successful intubation of the trachea, and the connection of ETT to a closed circuit, patients were ventilated with 100% oxygen. Confirmation of intubation was checked. During the process, if SpaO2 reduced fewer than 90%, ventilation with hand with 100% oxygen was sustained. If intubation remained ineffective after 2 efforts, it was regarded as a failure at intubation. Mask ventilation is established to achieve SpaO2 of 97% - 100%. More than 3 tries were not acceptable and were considered as the disappointment of intubation and excluded from the study. Before insert of the tube into the trachea, the Cormack-Lehane grade was documented in the two groups. At the end of the surgery, the patients were admitted to the CVICU, assisted by the portable mechanical ventilator, and they were extubated whenever they found the weaning conditions. The primary outcome includes the number of success rate in the first attempt to tracheal intubation, and the secondary outcomes were the duration of intubation time, the duration of intubation procedure, Cormack–Lehane score, and complications, such as desaturation (SpaO2 < 90%) and bradycardia (heart rate less than 20% of baseline).
Figure 1. flow diagram of the study.
3.2. Ethical Considerations
This study was approved by the ethics committee of Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran, (no.: IR.AJUMS.REC.1397.907). The trial registration number was IRCT20180909040979N2. A consent form for involvement in the study was obtained from the parents of patients.
3.3. Statistical Analysis
To explain the data, the mean ± standard deviation (SD) for quantitative variables were used. For qualitative variables, frequency and percentage were used. Independent t-test and chi-square tests were used for comparing the results. The analyses were performed using the statistical software of SPSS ver.22. and P ≤ 0.05 was considered significant.
4. Results
The final 60 patients participated in the study. Regarding the demographic characteristics, there are no significant differences between the two groups (Table 1). In group DL, 22 (73.3%) patients were intubated on the first attempt, 8 patients (26.7%) on the second attempt and 6 patients (20%) on the third attempt, compared to 24 (80%), 6 (20%), and 2 (6%) respectively, in group VL. The data showed that the differences were significant only in the third attempt between groups (P = 0.033). Intubation time was also measured, and 29.33 ± 13.75 seconds for group DL and 33.33 ± 15.72 seconds for group VL were recorded without significant differences (P = 0.2; Table 2). Intubation procedure time was recorded 51.13 ± 17.88 seconds for Group DL and 59.66 ± 45.91 seconds for group VL, which was statistically significant (P=0.006). Laryngoscopic grade) Cormack-Lehane score) was 1 for 22 patients in group VL in comparison with 12 patients in group DL, individually (P = 0.036). The laryngoscopic grade was 2 for 8 patients in group VL in comparison with 12 patients in group DL (P = 0.032). Cormack-Lehane score was 3 in 0 patients in group VL and 6 patients in DL (P = 0.034). We did not detect any desaturation or bradycardia while important differences were established in HR and SpaO2 amounts between the two groups at any time (P < 0.05; Table 3). It should be noted that we did not have any dental trauma, too.
Table 1. Preoperative Characteristics of Direct Laryngoscopy Group and Video Laryngoscopy Groupa.
| Variable | Direct Laryngoscopy Group (N = 30) | Video Laryngoscopy Group (N = 30) | P Value | 95% CI |
|---|---|---|---|---|
| Age, y | 25.80 ± 3.34 | 27 ± 3.06 | 0.665 | (-13.12, 10.72) |
| Gender | 0.731 | |||
| Male | 20 (66.66) | 14 (46.66) | ||
| Female | 10 (33.33) | 16 (53.33) |
Abbreviation: CI, confidence interval of the difference.
aValues are expressed as mean ± SD or N0. (%).
Table 2. Intubation Characteristic of Direct Laryngoscopy Group and Video Laryngoscopy Groupa.
| Parameter | Direct Laryngoscopy Group (N = 30) | Video Laryngoscopy Group (N = 30) | P Valueb | 95% CI |
|---|---|---|---|---|
| Intubation time, s | 29.33 ± 13.75 | 33.33 ± 15.72 | 0.2 | (-12.12, 4.12) |
| Intubation procedure time, s | 51.13 ± 17.88 | 59.66 ± 45.91 | 0.006c | (-28.49, 11.42) |
| Intubation attempts | ||||
| 1 | 22 (73.3) | 24 (80) | 0.514 | |
| 2 | 8 (26.7) | 6 (20) | 0.063 | |
| 3 | 6 (20) | 2 (6) | 0.033c | |
| 4 | 0 | 0 | - | |
| Cormac Lyhan grade | ||||
| 1 | 12 (40) | 22 (73.33) | 0.036c | |
| 2 | 12 (40) | 8 (26.66) | 0.032c | |
| 3 | 6 (20) | 0 (0) | 0.034c | |
| 4 | 0 (0) | 0 (0) | - |
Abbreviation: CI, confidence interval of the difference.
aValues are expressed as mean ± SD.
bIndependent t-test and chi-square test were used.
cSignificant at the level of 0.05.
Table 3. SpaO2 and HR Changes During Laryngoscopy and Its Comparison in Two Direct Laryngoscopy Group and Video Laryngoscopy Groupa.
| Parameter | Direct Laryngoscopy Group (N = 30) | Video Laryngoscopy Group (N = 30) | P Valueb | 95% CI |
|---|---|---|---|---|
| SpO 2 | 96.26 ± 1.85 | 93.76 ± 2.59 | 0.001c | 1.40, 3.59 |
| HR | 127.60 ± 25.18 | 140.33 ± 21.41 | 0.04c | -25.49, 0.027 |
Abbreviation: CI, confidence interval of the difference.
aValues are expressed as mean ± SD.
bIndependent t-test and chi-square test were used.
cSignificant at the level of 0.05.
5. Discussion
The anatomy of the airway and the physiologic differences between adults and children are major concern that increase morbidity and mortality rates during the intubation of the trachea (9). Airway management in congenital cardiac patients is complex by slighter cardiopulmonary reserve owing to heart pathophysiology, and the significant frequency of craniofacial problems and anatomic airway irregularities in these patients. Thus, intubation in these patients must be performed more carefully (9). Due to the anatomical airway differences and lack of data is requisite to allow assessment of difficulties in airways in the preoperative period, difficult laryngoscopic view and intubation can be significant explanations for preoperative morbidity and mortality. Regardless of the new advances in equipment and evidence correlated to the management of the airway in pediatric, intubation of endotracheal with straight laryngoscopy persists an excellent regular in the airway protection (10). Recently, the application of VL for pediatric patients with difficulty in the airway has augmented (11). However, no sufficient data is showing that VL confers a benefit over direct laryngoscopy in the managing of difficult airways in pediatric patients with CHD. Multiple studies have examined the DL with all types of VL techniques. Some of these training has been performed to develop cardiopulmonary resuscitation state in the mannequin that industrialized for difficult airway reproduction; nevertheless, neither of these techniques is superior to the other. In our study, the VL delivered a good view of the glottis; however, a longer intubation procedure time in the normal airway. The alternation in SpaO2 and heart rate (HR) varied significantly between the two groups but did not present a serious problem. In a study by Riveros et al. (12), DL with the Macintosh blade, GVL, and True View PCD as well as VL in 134 children from newborn to 10 years were analyzed and they established that the DL providing the greatest descriptions, whereas true view PCD had the extended IT. They suggested the limitation of VL usage methods in individuals likely to have a difficult airway (12). These findings were similar to our results. Kim et al., evaluated VL with the Macintosh blade in 203 children. They found VL view that was similar to or better than direct laryngoscopy. In the VL group, 62% of the patients had a laryngoscopic grade > 1. Moreover, the participants of repeated trials were greater in the VL group (13). However, in our study, 26.6 % of patients in the VL group had Cormack Lehane greater than 2. Another study also presented that VL improved visualization of glottis but extended the time of intubation (1). We established the Cormack-Lehane scores to be 1, 2, and 3 consequently in groups VL (73.33, 26.66 and 0%, respectively) and DL (40, 40, and 20%, respectively). We also reported an improved glottic view with the VL, though acceptable glottis views were gained in both groups. The comparison between DL with the Miller blade to VL was studied by Fiadjoe et al. (14), in 60 neonates and infants who had typical normal airway anatomy. They declared a comparable time for intubation (ITs) and presentations better and quicker glottis in the VL group, while there is an extended alignment time associated with the DL group. The intubation time was 22.6 seconds in the VL group than 21.4 seconds in the direct laryngoscopy group. The alignment time was 14.3 and 8.5 seconds, individually (14). In our study, a longer Intubation procedure time was found with the VL group, which was consistent with other studies on pediatric. The intubation procedure time in our study was 51.13 ± 17.88 and 59.66 ± 45.91 seconds in the direct laryngoscopy and VL, individually. The visualization of the glottis and insert of an endotracheal tube is required for successful laryngoscopy and intubation. In the VL intubation, imaging has acceptable quality while the time of endotracheal tube insertion is prolonged than that of the DL. In this study, our result showed that the success rate for intubation in the first attempt was increased in the VL group (80% vs. 73.3%), but there is not significant differences between groups. This finding was in consistent with the study conducted by Moussa et al. (15) To better words; they founded VL increased the success of intubation at first attempt (typical RR: 1.44; 95% CI: 1.20 to 1.73; typical RD: 0.19; 95% CI: 0.10 to 0.28; NNTB: 5; 95% CI: 4 to 10; 3 studies; 467 intubations). Our results showed that VL could not reduce the number of attempts for intubation (Table 2). In fact, they reported that VL did not decrease the number of intubation attempts (MD: -0.05; 95%: CI ‐0.18 to 0.07; 2 studies; 427 intubations (15). Increased HR develops due to the catecholamine release caused following intubation and laryngoscopy (16). In Maassen et al. (17) study in adult subjects, they found that the increase in HR and systolic blood pressure were less in the video group than in the direct laryngoscopy. In this line, we detected the important differences between HR and SpaO2 between the two groups during intubation (P < 0.05). This can be due to the low cardiac reserve of congenital cardiac patients.
5.1. Conclusions
In conclusion, we found that VL is associated with improved intubation success rates; however, it was not significant in the first and second attempt, but increase time to intubate in a pediatric with CHD, therefore training by using the VL should be increased. Moreover, VL intubation may be safer with decreased dental trauma. Together, further studies are recommended to approve these helpful findings.
5.2. Limitations
This study was a single-centered study with 60 patients; Therefore, future educations with more patients is recommended.
Acknowledgments
This paper was a part of the research with the ethics code (no.: IR.AJUMS.REC.1397.907). This study was designed as a placebo-controlled double-blind clinical trial: IRCT20180909040979N2. We sincerely thank the patients who cooperated with us in this project and supported the research team, and a special thanks to the EDO Unit of Golestan Hospital of Ahvaz, Iran.
Footnotes
Authors' Contribution: FJ and LG collected data and drafted the manuscript. FJ provided study materials and patients’ information. FJ and LG conceived of the study and participated in its design. All authors read and approved the final manuscript.
Clinical Trial Registration Code: The clinical trial registration code was IRCT20180909040979N2
Conflict of Interests: The authors report no conflict of interest.
Ethical Approval: The local Ethics Committee of Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran, approved all of the procedures of this study (ethic code: IR.AJUMS.REC.1397.907). The RCT code of this study was IRCT20180909040979N2.s
Funding/Support: Ahvaz Jundishapur University of Medical Sciences funded this research.
Informed Consent: Written informed consent signed by the study patients.
Contributor Information
Fatemeh Javaherforooshzadeh, Email: f_javaherforoosh@yahoo.com.
Laleh Gharacheh, Email: lalehgharacheh@yahoo.com.
References
- 1.Sun Y, Lu Y, Huang Y, Jiang H. Pediatric video laryngoscope versus direct laryngoscope: a meta‐analysis of randomized controlled trials. Pediatric Anesthesia. 2014;24(10):1056–65. doi: 10.1111/pan.12458. [DOI] [PubMed] [Google Scholar]
- 2.Donoghue AJ, Ades AM, Nishisaki A, Deutsch ES. Videolaryngoscopy versus direct laryngoscopy in simulated pediatric intubation. Annals of emergency medicine. 2013;61(3):271–7. doi: 10.1016/j.annemergmed.2012.09.008. [DOI] [PubMed] [Google Scholar]
- 3.Sakles JC, Patanwala AE, Mosier JM, Dicken JM. Comparison of video laryngoscopy to direct laryngoscopy for intubation of patients with difficult airway characteristics in the emergency department. Internal and Emergency Medicine. 2014;9(1):93–8. doi: 10.1007/s11739-013-0995-x. [DOI] [PubMed] [Google Scholar]
- 4.Huang AS, Rutland L, Hajduk K, Jagannathan N. Difficult airway management of children in ambulatory anesthesia: challenges and solutions. Ambulatory Anesthesia. 2016;3:37–45. [Google Scholar]
- 5.Lingappan K, Arnold JL, Fernandes CJ, Pammi M. Videolaryngoscopy versus direct laryngoscopy for tracheal intubation in neonates. The Cochrane database of systematic reviews. 2018;6(6):CD009975. doi: 10.1002/14651858.CD009975.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Foy KE, Mew E, Cook TM, Bower J, Knight P, Dean S, et al. Paediatric intensive care and neonatal intensive care airway management in the United Kingdom: the PIC‐NIC survey. Anaesthesia. 2018;73(11):1337–44. doi: 10.1111/anae.14359. [DOI] [PubMed] [Google Scholar]
- 7.Sinha R, Sharma A, Ray BR, Kumar Pandey R, Darlong V, Punj J, et al. Comparison of the success of two techniques for the endotracheal intubation with C-MAC video laryngoscope Miller blade in children: A prospective randomized study. Anesthesiology research and practice. 2016;2016 doi: 10.1155/2016/4196813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Andropoulos DB. Airway Management in Congenital Heart Disease. In: Da Cruz EM, Ivy D, Jaggers J, editors. Pediatric and Congenital Cardiology, Cardiac Surgery and Intensive Care. London: Springer London; 2014. pp. 955–69. [DOI] [Google Scholar]
- 9.An HS, Choi EY, Kwon BS, Kim GB, Bae EJ, Noh CI, et al. Airway compression in children with congenital heart disease evaluated using computed tomography. The Annals of thoracic surgery. 2013;96(6):2192–7. doi: 10.1016/j.athoracsur.2013.07.016. [DOI] [PubMed] [Google Scholar]
- 10.Holm‐Knudsen RJ, Rasmussen LS. Paediatric airway management: basic aspects. Acta Anaesthesiologica Scandinavica. 2009;53(1):1–9. doi: 10.1111/j.1399-6576.2008.01794.x. [DOI] [PubMed] [Google Scholar]
- 11.Wald SH, Keyes M, Brown A. Pediatric video laryngoscope rescue for a difficult neonatal intubation. Pediatric Anesthesia. 2008;18(8):790–1. doi: 10.1111/j.1460-9592.2008.02542.x. [DOI] [PubMed] [Google Scholar]
- 12.Riveros R, Sung W, Sessler DI, Sanchez IP, Mendoza ML, Mascha EJ, et al. Comparison of the Truview PCD™ and the GlideScope® video laryngoscopes with direct laryngoscopy in pediatric patients: a randomized trial. Canadian Journal of Anesthesia/Journal canadien d'anesthésie. 2013;60(5):450–7. doi: 10.1007/s12630-013-9906-x. [DOI] [PubMed] [Google Scholar]
- 13.Kim J-T, Na H-S, Bae J-Y, Kim D-W, Kim H-S, Kim CS, et al. GlideScope® video laryngoscope: a randomized clinical trial in 203 paediatric patients. British journal of anaesthesia. 2008;101(4):531–4. doi: 10.1093/bja/aen234. [DOI] [PubMed] [Google Scholar]
- 14.Fiadjoe JE, Gurnaney H, Dalesio N, Sussman E, Zhao H, Zhang X, et al. A prospective randomized equivalence trial of the GlideScope Cobalt® video laryngoscope to traditional direct laryngoscopy in neonates and infants. Anesthesiology: The Journal of the American Society of Anesthesiologists. 2012;116(3):622–8. doi: 10.1097/ALN.0b013e318246ea4d. [DOI] [PubMed] [Google Scholar]
- 15.Moussa A, Luangxay Y, Tremblay S, Lavoie J, Aube G, Savoie E, et al. Videolaryngoscope for teaching neonatal endotracheal intubation: a randomized controlled trial. Pediatrics. 2016;137(3):e20152156. doi: 10.1542/peds.2015-2156. [DOI] [PubMed] [Google Scholar]
- 16.Abdelgawad AF, Shi Q, Halawa MA, Wu Z, Wu Z, Chen X, et al. Comparison of cardiac output and hemodynamic responses of intubation among different videolaryngoscopies in normotensive and hypertensive patients. Journal of Huazhong University of Science and Technology [Medical Sciences]. 2015;35(3):432–8. doi: 10.1007/s11596-015-1449-7. [DOI] [PubMed] [Google Scholar]
- 17.Maassen RL, Pieters BM, Maathuis B, Serroyen J, Marcus MA, Wouters P, et al. Endotracheal intubation using videolaryngoscopy causes less cardiovascular response compared to classic direct laryngoscopy, in cardiac patients according a standard hospital protocol. Acta Anaesthesiol Belg. 2012;63(4):181–6. [PubMed] [Google Scholar]


