Abstract
Background
In the Corona Virus Disease 2019 (COVID-19) pandemic, the primary problem is respiratory-related, but there also is increasing evidence of central nervous system (CNS) involvement. This study aims to summarize the literature on neurological manifestations of COVID-19, underlying mechanisms of CNS involvement and cognitive consequences.
Methods
A scoping review was conducted with multiple searches in PubMed, PsycInfo, and CINAHL databases. Full text articles in English were included if they involved humans with COVID-19. The search was updated twice, the latest on 19 May 2020.
Results
After screening 266 records and cross referencing, 85 articles were included. The articles were case studies, opinion papers, letters to editors, and a few observational studies. No articles were found regarding cognitive consequences in COVID-19 patients. All reported on neurological manifestations and/or underlying mechanisms of CNS involvement in COVID-19.
Conclusion
Neurological manifestations of COVID-19 vary from mild (e.g. loss of taste and smell, dizziness, headache) to severe (e.g. ischemic stroke, encephalitis). Underlying pathways are suggested to be both indirect (as a result of thrombotic complication, inflammatory consequences, hypoxia, blood pressure dysregulation), and direct (neurotropic properties of the virus). Since most articles were opinion papers and no studies have been conducted on cognitive consequences, further research is warranted.
Keywords: Corona Virus Disease 2019, neurological, neurotropic, cognitive, scoping review
Introduction
The recent outbreak of Corona Virus Disease 2019 (COVID-19) caused by the Severe Acute Respiratory Syndrome Corona Virus 2 (SARS-CoV-2) led to the current pandemic, which is characterized by ominously high infection rates. By the end of May, over 4.8 million people have been infected and over 323,000 deceased worldwide due to COVID-19 (1). To stop the devastating impact of COVID-19, scientists are in a race to find a cure or vaccine for the virus.
SARS-CoV-2 is primarily transmitted between people through respiratory droplets. It can bind to the angiotensin-converting enzyme 2 (ACE2) receptor in the lungs. After which most people develop mild symptoms, such as coughing or fever. However, the disease can lead to more severe problems such as pneumonia (2). In the Netherlands, a quarter of all identified patients were admitted to the hospital due to COVID-19. The leading cause of hospital admittance was respiratory failure due to acute respiratory distress syndrome (ARDS) (3, 4).
Although the most prominent symptoms of COVID-19 are respiratory-related, there is also emerging literature on neurological manifestations of the virus. First opinion papers, letters to the editors, and case studies have been published. The primary aim of the current study was to summarize the literature on neurological manifestations due to COVID-19 and its underlying mechanisms. Furthermore, if COVID-19 might lead to neurological tissue damage, then it could lead to impaired cognitive functioning (e.g. memory impairment or attention problems). Therefore, the secondary aim was to summarize the literature on cognitive consequences of COVID-19.
Methods
Design
A scoping review was used to provide an overview of the relevant literature on neurological and cognitive manifestations in COVID-19 patients (5). Possible mechanisms underlying these manifestations will be presented based on the available evidence. A scoping review was chosen over a systematic review to provide a broader overview of the literature using multiple sources (e.g., opinion papers, letters to the editors, case studies). We used the extended PRISMA checklist for scoping reviews and the following methodological framework: identifying the research question, study selection, charting the data, and reporting the results (5–7).
Data Sources, Search Strategy, and Inclusion and Exclusion Criteria
The databases PubMed, PsycInfo, and CINAHL were searched using a search strategy based on free text terms in Title/Abstract and descriptor terms. Some basic searches were carried out by two authors to identify key terms. The search strategy is provided in the Supplementary Material. We included all relevant publications on the neurological manifestations in COVID-19, underlying mechanisms, and cognitive consequences. A limit was placed on year of publication (2019–2020). Animal studies, studies in neonates, and articles without a full text in English were excluded. The search was carried out on 29 April 2020 and updated on 12 May and 19 May 2020.
Study Selection and Charting of the Data
One author independently screened all titles and abstracts. Two authors discussed the included full texts and found a perfect agreement on the included papers. Cross referencing was applied to determine if relevant articles were missing. Two authors reviewed, extracted, and summarized the full text articles. The main topics were analyzed using a qualitative content approach and narratively described. The following themes were determined: neurological manifestations in COVID-19 and its underlying mechanisms. Descriptives were reported from the observational studies.
Results
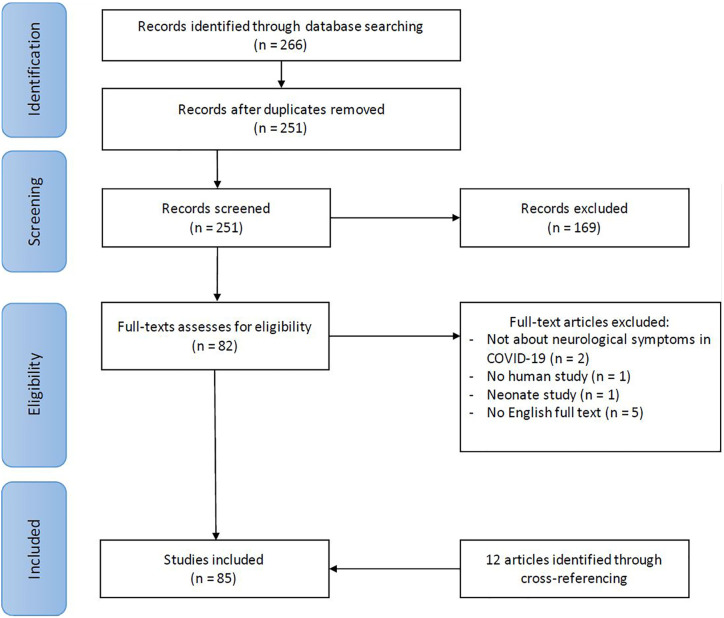
The first search (29 April) yielded 160 records, the second update (12 May) 206 records, and the final update (19 May) 266 records. A total of 82 full texts were evaluated for inclusion, of which 73 were included. Through cross referencing another twelve articles were identified, which led to the inclusion of 85 papers. Figure 1 shows the flowchart of this selection process. In this scoping review, all included papers were summarized using a narrative report. An overview of the findings of all articles are described in Table 1 in the Supplementary Material. The 85 articles were 25 opinion papers, 22 case studies, 16 letters to the editor, 13 reviews (11 literature reviews, 1 systematic review, 1 scoping review), 6 observational studies, and 3 comments on other publications.
Figure 1.
Flowchart article selection procedure.
Neurological Manifestations and Neuropsychological Consequences
Unfortunately, no papers have been reported yet on cognitive consequences of COVID-19, such as memory impairment or attention deficits in COVID-19 patients. However, the literature on neurological manifestations of SARS-CoV-2 is emerging. A few observational studies on neurological symptoms have been conducted in COVID-19 patients. Mao, Wang (8) demonstrate that 36.4% of 214 hospitalized COVID-19 patients had neurological symptoms, varying from dizziness and headache, to cerebrovascular disease. In the COVID-19 intensive care (IC) population neurological symptoms were found in 84 percent of 58 patients included in the study of Helms et al. (9), and 21 percent of 235 patients included in the study of Kandemirli, Dogan (10).
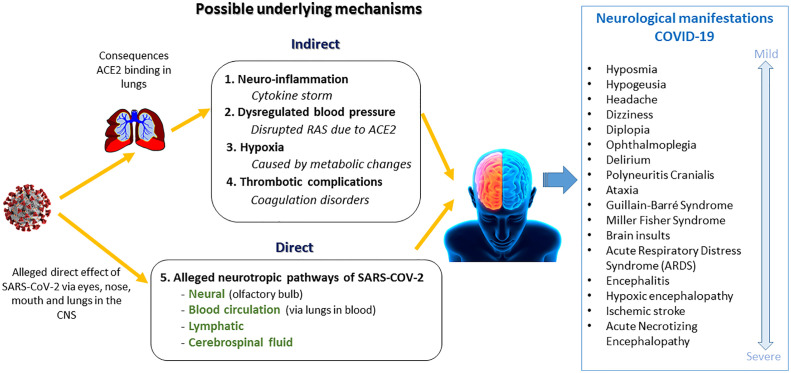
There is a great variety in the type and severity of the neurological manifestations of COVID-19. The first evidence of mild neurological symptoms emerged quickly after the outbreak, such as hyposmia, hypogeusia, headache, dizziness, diplopia, and ophthalmoplegia (11–18). Case studies have been published since February on neurological symptoms as an atypical presentation of COVID-19 (19). To illustrate, a delirium could be a first atypical symptom of COVID-19, especially in the elderly (20–22). Neurological movement disorders have also been reported in COVID-19 cases, such as Guillain-Barré syndrome, Miller Fisher syndrome, polyneuritis cranialis, and ataxia (8, 23, 24). Furthermore, Lu, Xiong (25) found acute symptomatic seizures in 27% of 304 COVID-19 patients with no prior history of seizures. More severe types of brain disease (encephalopathy) have been described as well, such as hypoxic encephalopathy, encephalitis, and stroke (11–13, 26). A retrospective study from Chen, Wu (27) showed that 20% of 113 COVID-19 ICU patients had hypoxic encephalopathy. In another study 31% of 184 ICU patients with COVID-19 had thrombotic complications with ischemic strokes (28). Furthermore, acute necrotizing encephalopathy (ANE) is also described in a case report of a COVID-19 patient (29). ANE is a rare disease, which can lead to severe brain damage including hemorrhage. In conclusion, neurological manifestations vary from mild to severe, all summarized in Figure 2.
Figure 2.
Neurological manifestations of COVID-19 and possible underlying mechanisms.
COVID-19 Mechanisms Underlying the Neurological Manifestations
The literature about possible pathways in which COVID-19 can cause neurological manifestations is emerging. Both direct and indirect suggested pathways are summarized in Figure 2.
The suggested indirect effects of SARS-CoV-2 on the brain are:
Neuro-inflammation: a cytokine storm, induced by the immune system in reaction to the virus, can spread through the body, pass the blood brain barrier, and can cause brain infections or damage nearby neurons and glial cells (20, 30–38).
Blood pressure imbalance: since ACE2 regulates blood pressure in the renin angiotensin aldosterone system (RAS), damage of the ACE2 receptor can lead to hypertension or hypotension (30, 38–41).
Hypoxia: metabolic disruption, caused by lung damage, can lead to an oxygen deficiency in the brain (30, 32, 37, 38).
Thrombosis: thrombotic complications can lead to ischemic strokes (32, 38).
First opinion papers are published in which scientists assume that SARS-CoV-2 can enter the central nervous system CNS (12, 14, 16, 17, 27, 42, 43). It is stated that other coronaviruses have been found to be neurotropic (16, 27, 42, 44). Hereby ACE2, to which the virus is binding to, is assumed also to be present in the brain (42–44). In a case study in two patients, SARS-CoV-2 was not found in the cerebrospinal fluid (CSF) (45). However, two other case studies mentioned presence of the virus in the frontal lobe and CSF (39, 40). Various direct pathways are proposed to which the virus could possibly have a direct effect on the brain. After the virus enters the body via the eyes, nose, or mouth, it can bind to ACE2 receptors. The possibility of binding to the ACE2 receptors in the nose and taste buds could explain the possible loss of taste and smell in COVID-19 (16). A neural pathway is suggested, in which the virus enters the CNS along the olfactory pathway penetrating the olfactory bulb in the forebrain (15, 30–32, 34, 35, 46–48). Also, the virus could be transported to the brain via the lymphatic system through lymphoid tissue (32, 43, 49). The blood circulation is another supposed pathway. When the virus enters the blood circulation it can be transported to the brain. The virus could possibly pass the blood brain barrier by infecting the endothelial cells (49). Once in the CNS, the virus could possibly enter the cerebrospinal fluid, through which it can spread through the brain (15, 30, 35). The medulla oblongata is the primary respiratory control center, located in the lowest portion of the brain stem. It is suggested that damage to the medulla oblongata, caused by direct effects of SARS-CoV-2, can possibly explain respiratory failure in COVID-19 (20, 32, 37, 43, 46, 48, 50–53). Scientists propose that this neurotropic potential of SARS-CoV-2 may account for the difference in respiratory distress in patients (51). However, some researchers believe this is not the case, since recovery of respiratory distress symptoms takes place (32).
Discussion
The aim of the current study was to summarize the literature on neurological manifestations in COVID-19, underlying mechanisms, and cognitive consequences. This scoping review included 85 articles. Neurological manifestations were prominently described with suggestions for underlying mechanisms. The CNS is involved in COVID-19, as neurological manifestations (e.g., consequences of hypoxia and thrombosis) were shown in several case reports and observational studies (7, 8, 25, 53, 54). Suggested pathways of CNS involvement are both direct (neurotropic) and indirect. Since no literature on cognitive consequences of COVID-19 was found yet, previous research on other coronaviruses should be taken into account. A systematic review and meta-analysis on recovered patients of other coronaviruses found that a significant proportion of patients developed a delirium during the acute stage, and almost halve (44%) had a memory impairment post-illness (54). Elderly, people with already existing neurodegenerative diseases, or people with psychiatric comorbidities might be even more at risk for cognitive impairment following COVID-19, due to their cognitive vulnerability. Hereby, since people living with dementia might have difficulties in understanding and remembering the public health information, they are more vulnerable to be infected with COVID-19 (55, 56). In case of co-occurrence of COVID-19 and dementia, delirium could complicate the presentation of dementia (55, 56). Furthermore, as a result of neuro-inflammation that causes or progresses neurodegenerative processes in the brain, it is suggested that COVID-19 could result in a higher incidence of neurodegenerative diseases (30).
A strength of the current study is the use of scoping review methodology to gain insight into the current available evidence on neurological manifestations and underlying mechanisms while using a systematic process with a replicable and transparent approach. To our knowledge, this is the first scoping review on both neurological manifestations, its underlying mechanisms, and cognitive consequences in COVID-19 patients. Some limitations have to be considered as well. No quality appraisal of the studies was taken into account, which is often the case in scoping reviews. Due to the quick rise of literature on COVID-19 new publications might have emerged. The body of literature is fast-growing, which is illustrated by the inclusion of 27 articles after our first search on the 29 April 2020, and the latest update on 19 May 2020 resulting in a total of 85 articles.
Therapeutic Implications
Clinicians should be vigilant for CNS involvement and possible neurological manifestations of COVID-19.
Clinicians should be aware of possible neurological and cognitive complaints post-COVID-19, especially in older patients, patients with cognitive impairment and/or psychiatric comorbidity.
In case of cognitive complaints post-COVID-19 cognitive screening or neuropsychological assessment is recommended.
In case of complex cognitive of emotional complaints post-COVID-19 it is recommended to involve a psychiatrist or psychologist.
Conclusion and Recommendations
In conclusion, neurological manifestations of COVID-19 vary from mild, such as headache and dizziness, to severe, such as ischemic stroke and encephalitis. Underlying mechanisms of CNS involvement are suggested to be both direct (neurotropic) and indirect (as a result of thrombotic complication, inflammatory consequences, hypoxia, blood pressure dysregulation). Since most articles were opinion papers, further research is warranted.
No literature was found on the cognitive consequences of COVID-19. Therefore, cross sectional and longitudinal studies are needed. Neuropsychological assessment could be used to monitor the course of cognitive functioning after recovering from COVID-19. This should not only be conducted in hospitalized COVID-19 patients, but should also contain community-based studies in adults and children that recovered from COVID-19.
Author Contributions
AW and AG carried out abstract screening and full text extraction of the scoping review. The first draft of the manuscript was written by both AW and AG. All other authors contributed to revisions of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2020.00860/full#supplementary-material
References
- 1. World Health Organization. Coronavirus disease 2019 (COVID-19): situation report - 122 (2020). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/.
- 2. Zhou Y, Li W, Wang D, Mao L, Jin H, Li Y, et al. Clinical time course of COVID-19, its neurological manifestation and some thoughts on its management. Stroke Vasc Neurol (2020) 5:177–9. 10.1136/svn-2020-000398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. RIVM Richtlijn COVID-19. (2020) RIVM; Available from: https://lci.rivm.nl/richtlijnen/covid-19 [Google Scholar]
- 4. World Health Organization Coronavirus disease (COVID-19) Pandemic. (2020) WHO; Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 [Google Scholar]
- 5. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol (2005) 8(1):19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 6. Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci (2010) 5(1):69. 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med (2018) 169(7):467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 8. Mao L, Wang M, Chen S, He Q, Chang J, Hong C, et al. Neurological manifestations of hospitalized patients with COVID-19 in Wuhan, China: a retrospective case series study. JAMA Neurol (2020) 77:1–9. 10.1001/jamaneurol.2020.1127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Helms J, Kremer S, Merdji H, Clere-Jehl R, Schenck M, Kummerlen C, et al. Neurologic features in severe SARS-CoV-2 infection. N Engl J Med (2020) 382:2268–70. 10.1056/NEJMc2008597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kandemirli SG, Dogan L, Sarikaya ZT, Kara S, Akinci C, Kaya D, et al. Brain MRI findings in patients in the intensive care unit with COVID-19 infection. Radiology (2020), 201697. 10.1148/radiol.2020201697 [DOI] [PMC free article] [PubMed]
- 11. Gautier J-F, Ravussin Y. A new symptom of COVID-19: Loss of taste and smell. Obesity (2020) 28(5):848. 10.1002/oby.22809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Das G, Mukherjee N, Ghosh S. Neurological insights of COVID-19 pandemic. ACS Chem Neurosci (2020) 11:1206–9. 10.1021/acschemneuro.0c00201 [DOI] [PubMed] [Google Scholar]
- 13. Asadi-Pooya AA, Simani L. Central nervous system manifestations of COVID-19: A systematic review. J Neurol Sci (2020) 413:116832. 10.1016/j.jns.2020.116832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Liu K, Pan M, Xiao Z, Xu X. Neurological manifestations of the coronavirus (SARS-CoV-2) pandemic 2019-2020. J Neurol Neurosurg Psychiatry (2020) 91:669–70. 10.3389/fneur.2020.00498 [DOI] [PubMed] [Google Scholar]
- 15. Baig AM. Neurological manifestations in COVID-19 caused by SARS-CoV-2. CNS Neurosci Ther (2020) 26(5):499–501. 10.1111/cns.13372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Finsterer J, Stollberger C. Causes of hypogeusia/hyposmia in SARS-CoV2 infected patients. J Med Virol (2020). 10.1002/jmv.25903 [DOI] [PMC free article] [PubMed]
- 17. Carod-Artal FJ. Neurological complications of coronavirus and COVID-19. Rev Neurologia (2020) 70(9):311–22. 10.33588/rn.7009.2020179 [DOI] [PubMed] [Google Scholar]
- 18. Baig AM. Updates on what ACS Reported: Emerging evidences of COVID-19 with nervous system involvement. ACS Chem Neurosci (2020) 11(9):1204–5. 10.1021/acschemneuro.0c00181 [DOI] [PubMed] [Google Scholar]
- 19. Li Z, Huang Y, Guo X. The brain, another potential target organ, needs early protection from SARS-CoV-2 neuroinvasion. Sci China Life Sci (2020) 63(5):771–3. 10.1007/s11427-020-1690-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Steardo L, Steardo L, Jr., Zorec R, Verkhratsky A. Neuroinfection may contribute to pathophysiology and clinical manifestations of COVID-19. Acta Physiol (Oxf) (2020) 229(30):e13473. 10.1111/apha.13473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. British Geriatrics Society Coronavirus: Managing delirium in confirmed and suspected cases. (2020) British Geriatrics Society; Available from: https://www.bgs.org.uk/resources/coronavirus-managing-delirium-in-confirmed-and-suspected-cases [Google Scholar]
- 22. Nederlandse Internisten Vereniging Delier bij patiënten met COVID-19. (2020). Nederlandse Internisten Vereniging. Available from https://internisten.nl/sites/internisten.nl/files/berichten/Delier%20bij%20COVID-19_26%20maart%202020_4.pdf
- 23. Gutiérrez-Ortiz C, Méndez A, Rodrigo-Rey S, San Pedro-Murillo E, Bermejo-Guerrero L, Gordo-Mañas R, et al. Miller Fisher syndrome and polyneuritis cranialis in COVID-19. Neurology (2020) 95:211 Nederlandse Internisten Vereniging. 10.1212/WNL.0000000000009619 [DOI] [PubMed] [Google Scholar]
- 24. Scheidl E, Canseco DD, Hadji-Naumov A, Bereznai B. Guillain-Barre syndrome during SARS-CoV-2 pandemic: a case report and review of recent literature. J Peripher Nerv Syst (2020) 25(2):204–7. 10.1111/jns.12382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lu L, Xiong W, Liu D, Liu J, Yang D, Li N, et al. New onset acute symptomatic seizure and risk factors in coronavirus disease 2019: A retrospective multicenter study. Epilepsia (2020) 61(6):e49–53. 10.1111/epi.16524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bernard-Valnet R, Pizzarotti B, Anichini A, Demars Y, Russo E, Schmidhauser M, et al. Two patients with acute meningo-encephalitis concomitant to SARS-CoV-2 infection. Eur J Neurol (2020). 10.1111/ene.14298 [DOI] [PMC free article] [PubMed]
- 27. Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ (2020) 368:m1091. 10.1136/bmj.m1091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res (2020) 191:145–7. 10.1016/j.thromres.2020.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Poyiadji N, Shahin G, Noujaim D, Stone M, Patel S, Griffith B, et al. COVID-19–associated acute hemorrhagic necrotizing encephalopathy: CT and MRI Features. Radiology (2020) 296(2):e119–20. 10.1148/radiol.2020201187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wu Y, Xu X, Chen Z, Duan J, Hashimoto K, Yang L, et al. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun (2020) 87:18–22. 10.1016/j.bbi.2020.03.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bertran Recasens B, Martinez-Llorens JM, Rodriguez-Sevilla JJ, Rubio MA. Lack of dyspnea in COVID-19 patients; another neurological conundrum? Eur J Neurol (2020). 10.1111/ene.14265 [DOI] [PMC free article] [PubMed]
- 32. Bostanciklioğlu M. SARS-CoV2 entry and spread in the lymphatic drainage system of the brain. Brain Behav Immun (2020) 87:122–3. 10.1016/j.bbi.2020.04.080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. De Felice FG, Tovar-Moll F, Moll J, Munoz DP, Ferreira ST. Severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2) and the central nervous system. Trends Neurosci (2020) 43(6):355–7. 10.1016/j.tins.2020.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. De Santis G. SARS-CoV-2: A new virus but a familiar inflammation brain pattern. Brain Behav Immun (2020). 10.1016/j.bbi.2020.04.066 [DOI] [PMC free article] [PubMed]
- 35. Mankad K, Perry MD, Mirsky DM, Rossi A. COVID-19: A primer for nuroradiologists. Neuroradiology (2020) 62(6):647–78. 10.1007/s00234-020-02437-5 [DOI] [Google Scholar]
- 36. Toljan K. Letter to the Editor Regarding the Viewpoint “Evidence of the COVID-19 virus targeting the CNS: tissue distribution, host-virus Interaction, and proposed neurotropic mechanism”. ACS Chem Neurosci (2020) 11(8):1192–4. 10.1021/acschemneuro.0c00174 [DOI] [PubMed] [Google Scholar]
- 37. Li Z, Liu T, Yang N, Han D, Mi X, Li Y, et al. Neurological manifestations of patients with COVID-19: potential routes of SARS-CoV-2 neuroinvasion from the periphery to the brain. Front Med (2020). 10.1007/s11684-020-0786-5 [DOI] [PMC free article] [PubMed]
- 38. Needham EJ, Chou SH, Coles AJ, Menon DK. Neurological implications of COVID-19 infections. Neurocrit Care (2020) 32(3):667–71. 10.1007/s12028-020-00978-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hess DC, Eldahshan W, Rutkowski E. COVID-19-related stroke. Transl Stroke Res (2020) 11:322–5. 10.1007/s12975-020-00818-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Wang H, Li X-L, Yan Z-R, Sun X-P, Han J, Zhang B-W. Potential neurological symptoms of COVID-19. Ther Adv Neurol Disord (2020) 13:1756286420917830. 10.1177/1756286420917830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Oudkerk M, Büller HR, Kuijpers D, van Es N, Oudkerk SF, McLoud TC, et al. Diagnosis, prevention, and treatment of thromboembolic complications in COVID-19: Report of the national institute for public health of the Netherlands. Radiology (2020) 201629. 10.1148/radiol.2020201629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Baig AM, Khaleeq A, Ali U, Syeda H. Evidence of the COVID-19 virus targeting the CNS: Tissue distribution, host-virus interaction, and proposed neurotropic mechanisms. ACS Chem Neurosci (2020) 11(7):995–8. 10.1021/acschemneuro.0c00122 [DOI] [PubMed] [Google Scholar]
- 43. Chigr F, Merzouki M, Najimi M. Comment on “The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients”. J Med Virol (2020) 9(1):45. 10.1002/jmv.25960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Li MY, Li L, Zhang Y, Wang XS. Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infect Dis Poverty (2020) 9(1):45. 10.1186/s40249-020-00662-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Al Saiegh F, Ghosh R, Leibold A, Avery MB, Schmidt RF, Theofanis T, et al. Status of SARS-CoV-2 in cerebrospinal fluid of patients with COVID-19 and stroke. J Neurol Neurosurg Psychiatry (2020) 91(8):846–8. 10.1136/jnnp-2020-323522 [DOI] [PubMed] [Google Scholar]
- 46. Butowt R, Bilinska K. SARS-CoV-2: Olfaction, brain Infection, and the urgent need for clinical samples allowing earlier virus detection. ACS Chem Neurosci (2020) 11(9):1200–3. 10.1021/acschemneuro.0c0017 [DOI] [PubMed] [Google Scholar]
- 47. Pereira A. Long-term neurological threats of COVID-19: A call to update the thinking about the outcomes of the coronavirus pandemic. Front Neurol (2020) 11:308. 10.3389/fneur.2020.00308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Gandhi S, Srivastava AK, Ray U, Tripathi PP. Is the collapse of the respiratory center in the brain responsible for respiratory breakdown in COVID-19 patients? ACS Chem Neurosci (2020). 10.1021/acschemneuro.0c00217 [DOI] [PubMed]
- 49. Li Z, Liu T, Yang N, Han D, Mi X, Li Y, et al. Neurological manifestations of patients with COVID-19: potential routes of SARS-CoV-2 neuroinvasion from the periphery to the brain. Front Med (2020) 1–9. 10.1007/s11684-020-0786-5 [DOI] [PMC free article] [PubMed]
- 50. Tassorelli C, Mojoli F, Baldanti F, Bruno R, Benazzo M. COVID-19: what if the brain had a role in causing the deaths? Eur J Neurol (2020). 10.1111/ene.14275 [DOI] [PMC free article] [PubMed]
- 51. Li YC, Bai WZ, Hashikawa T. The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients. J Med Virol (2020) 92(6):552–5. 10.1002/jmv.25728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Sellner J, Taba P, Öztürk S, Helbok R. The need for neurologists in the care of COVID-19 patients. Eur J Neurol (2020). 10.1111/ene.14257 [DOI] [PMC free article] [PubMed]
- 53. Shaikh AG, Mitoma H, Manto M. Cerebellar scholars’ challenging time in COVID-19 pandemia. Cerebellum (2020) 19(3):343–4. 10.1007/s12311-020-01131-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Rogers JP, Chesney E, Oliver D, Pollak TA, McGuire P, Fusar-Poli P, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiat (2020) 7(7):611–27. 10.1016/S2215-0366(20)30203-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Wang H, Li T, Barbarino P, Gauthier S, Brodaty H, Molinuevo JL, et al. Dementia care during COVID-19. Lancet (2020) 395(10231):1190–1. 10.1016/S0140-6736(20)30755-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Brown EE, Kumar S, Rajji TK, Pollock BG, Mulsant BH. Anticipating and mitigating the impact of the COVID-19 pandemic on Alzheimer’s disease and related dementias. Am J Geriatr Psychiatry (2020) 28(7):712–21. 10.1016/j.jagp.2020.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.