INTRODUCTION
The presence of asymptomatic hypoxemia (AH) in patients with coronavirus disease (COVID-19) is well described.[1] AH is thought to be responsible for the phenomenon of rapid clinical deterioration and mortality in the hospital setting,[2] and is frequently associated with the delayed escalation of care.[3] In addition, at-home mortality is thought to be elevated among those with AH who are discharged from the emergency department following an apparently low-acuity ambulatory evaluation.[4,5] Such patients may have profound hypoxemia without significant dyspnea, with the initial sign of deterioration being confined to escalating oxygen requirement.[5]
CLINICAL RATIONALE
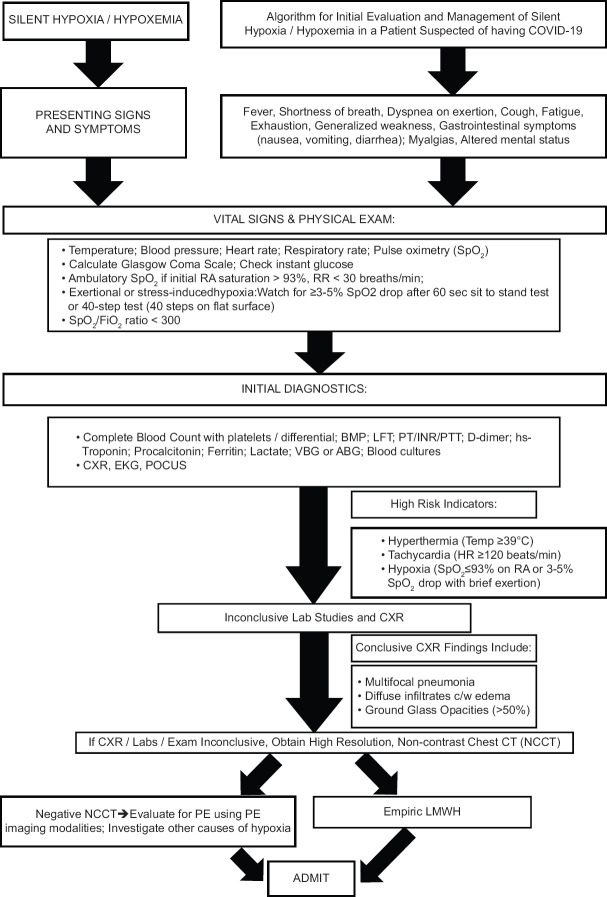
Following similar experiences across our institutions, spanning three continents and highly diverse patient populations, this working group of the combined American College of Academic International Medicine and World Academic Council of Emergency Medicine (ACAIM-WACEM) COVID-19 Taskforce arrived at an algorithm intended to establish a unified approach to this insidious and potentially lethal clinical problem [Figure 1]. Regardless of the algorithm utilized in the diagnosis and treatment of COVID-19, the evaluation of each patient should always begin with, and be based on, careful medical history and detailed clinical exam. Building on this foundation, the managing health-care provider (HCP) should obtain appropriate laboratory and radiographic tests to help confirm the diagnosis, to determine disease severity, and to accurately triage the patient.
Figure 1.
Management algorithm for subclinical hypoxemia in COVID-19 patients
PATIENT HISTORY AND BEDSIDE EVALUATION
The presence of COVID-19 should be suspected in patients who present with characteristic symptoms among which fever and cough are the most common.[6,7] Patients at higher risk of severe clinical course tend to be older, frail, immunocompromised, morbidly obese, carrying two or more chronic comorbid conditions, and male.[7,8,9,10] Additional correlates of severe illness may include tachycardia, hyperthermia of ≥39°C, encephalopathy, and hemodynamic instability. Although “typical” symptoms of COVID-19 are present in the vast majority of cases,[7] additional specific “red flags” must be kept in mind by the managing HCP. These warning signs may be subtle and include the appearance of ≥3%–5% drop in SpO2 after approximately 60 s of mild activity/ambulation, SpO2/FiO2 ratio <300, SpO2< 93% on room air, and the presence of hypoxemia without tachypnea or other signs of respiratory compromise [Figure 1].[4,11,12]
LABORATORY ASSESSMENT
Initial diagnostics include complete blood count with differential and platelets; comprehensive metabolic panel (inclusive of liver function tests); coagulation profile (e.g., prothrombin time, partial thromboplastin time [PTT], international normalized ratio [INR], see below); C-reactive protein; D-dimer; high sensitivity (hs) Troponin; procalcitonin; ferritin, lactate, venous or arterial blood gas analysis; blood cultures; and nasal and pharyngeal viral swabs.[7,13] Electrocardiogram may be considered based on the HCP's level of suspicion.[7,13] Laboratory findings of a neutrophil-to-lymphocyte ratio of >3.3; markedly elevated D-dimer; and early elevations in hs-Troponin, are significantly associated with severe disease and poorer prognosis.[7,14,15,16] Coagulation pathway abnormalities may also be seen among patients with more severe COVID-19 presentations.[17] More specifically, HCP's may see thrombocytopenia, increased INR, prolonged activated PTT, and abnormal levels of fibrin degradation products. Associated with the above findings is the elevated risk of venous thromboembolism, prompting recommendations for thromboprophylaxis.[18]
RADIOGRAPHY ASSESSMENT
Initial chest radiograph shows typical COVID-19 diagnostic changes in approximately two-thirds of patients; however, this may increase to >95% in those with severe disease.[15] Noncontrast computed tomography (NCCT) of the chest is characterized by good correlation with both the diagnosis and severity of COVID-19, providing an overall sensitivity of >90% at 2–5 days after the onset of symptoms and 97% sensitivity thereafter.[7,19,20] If the NCCT findings are highly suspicious for COVID-19,[21] the patient should be considered for thromboprophylaxis with low molecular weight heparin administration[18,22] and for the hospital admission. If the NCCT does not show findings characteristic of COVID-19, additional testing with contrast-enhanced computed tomography of the chest or ventilation/perfusion scanning may be considered to rule out other causes of hypoxia (e.g., pulmonary embolism) as per managing HCP's index of clinical suspicion. The decision regarding patient admission should be made on a case-by-case basis under such circumstances.
Important clinical considerations:
Coronavirus disease-2019 appears to have significant pro-thrombotic effects;[23,24] D-Dimer levels are elevated under these circumstances
Contrast computed tomographic angiography chest after a negative noncontrast computed tomography is not usually an option in a pandemic situation due to limited resources
Dehydration and acute kidney injury can exist hence cautious use of intravenous contrast is recommended[25,26]
Perform computed tomographic pulmonary angiography only if suspicion of pulmonary embolism (PE) is high. If contrast nephropathy risk is high, consider appropriate renal risk remediation or other imaging modalities (e.g. ventilation/perfusion scan when ruling out pulmonary embolism)
Surrogate findings on point-of-care ultrasound cardiac and thoracic/pulmonary ultrasound are important[27,28]
Post-admission empiric therapeutic doses of low molecular weight heparin appear to be both effective and preventive in the context of elevated PE risk.[29]
Figure 1 legend: ABG: Arterial blood gas, AKI: Acute kidney injury, BMP: Basic metabolic panel, BP: Blood pressure, CTA: Computed tomographic angiography, c/w: Consistent with, CXR: Chest radiograph, FiO2: Fraction of inspired oxygen, HR: Heart rate, INR: International normalized ratio, LFT: Liver function testing, LMWH: Low-molecular-weight heparin, NCCT: Noncontrast chest CT, PE: Pulmonary embolism, POCUS: Point-of-care ultrasound, PT: Prothrombin time, PTT: Partial thromboplastin time, RA: Room air, RR: Respiratory rate, SpO2: Peripheral capillary oxygen saturation, V/Q: Ventilation/Perfusion, VBG: Venous blood gas
SUMMARY AND CONCLUSIONS
In the early stages of COVID-19 clinical illness, the ability to oxygenate is impaired. However, the patient does not necessarily display the conventionally expected signs or symptoms of respiratory failure, including shortness of breath. Given the above, HCP's must remain vigilant and proactively look for 'red flags' described herein, such as the appearance of ≥3%–5% drop in SpO2 after approximately 60 s of mild activity/ambulation, SpO2/FiO2 ratio <300, SpO2< 93% on room air, and the presence of hypoxemia without tachypnea [Figure 1].[4,11,12] In summary, this expert group views AH as the proverbial “canary in the coalmine” and the first harbinger of future respiratory deterioration in COVID-19 patients.
REFERENCES
- 1.Gattinoni L, Chiumello D, Caironi P, Busana M, Romitti F, Brazzi L, et al. COVID-19 pneumonia: Different respiratory treatments for different phenotypes? Intensive Care Med. 2020;14:1–4. doi: 10.1007/s00134-020-06033-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.COVID-19 in the Emergency Department - County EM [Internet] Available from: http://blogclinicalmonstercom/2020/03/23/18788/ Last cited on 2020 May 13.
- 3.Yao W, Wang T, Jiang B, Gao F, Wang L, Zheng H, et al. Emergency tracheal intubation in 202 patients with COVID-19 in Wuhan, China: Lessons learnt and international expert recommendations. Br J Anaesth. 2020 doi: 10.1016/j.bja.2020.03.026. pii: S0007-0912 (20) 30203-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Levitan R. The Infection That's Silently Killing Coronavirus Patients. 2020. [Last accessed on 2020 Apr 20]. Available from: https://wwwnytimescom/2020/04/20/opinion/coronavirus-testing-pneumoniahtml .
- 5.Farkas J. COVID-19. 2020. [Last accessed on 2020 Apr 21]. Available from: https://emcritorg/ibcc/covid19/
- 6.CDC. Interim Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease (COVID-19) 2020. [Last accessed on 2020 Mar 24]. Available from: https://wwwcdcgov/coronavirus/2019-ncov/hcp/clinical-guida nce-management-patientshtml .
- 7.Stawicki SP, Jeanmonod R, Miller AC, Paladino L, Gaieski DF, Yaffee AQ, et al. The 2019-2020 Novel coronavirus (severe acute respiratory syndrome coronavirus 2) pandemic: A joint american college of academic international medicine-world academic council of emergency medicine multidisciplinary COVID-19 working group statement. J Global Infect Dis. 2020;12:47–93. doi: 10.4103/jgid.jgid_86_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Verity R, Okell LC, Dorigatti I, Winskill P, Whittaker C, Imai N, et al. Estimates of the severity of coronavirus disease 2019: A model-based analysis. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30243-7. pii: S1473-3099 (20) 30243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Julia CT, Jill CS, Riley H, Amanda M, Dan F, Peter D, et al. Comorbidity-Polypharmacy Score Predicts Readmissions and in-Hospital Mortality: A Six-Hospital Health Network Experience. J Basic Clin Pharma. 2017;8:98–103. [Google Scholar]
- 10.Stawicki SP, Kalra S, Jones C, Justiniano CF, Papadimos TJ, Galwankar SC, et al. Comorbidity polypharmacy score and its clinical utility: A pragmatic practitioner's perspective. J Emerg Trauma Shock. 2015;8:224–31. doi: 10.4103/0974-2700.161658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Webinar April 2, 2020 - Clinical Management of Critically Ill Adults with COVID-19 [Internet] 2020. Available from: https://emergency.cdc.gov/coca/calls/2020/callinfo_040220.asp . Last cited on 2020 May 13.
- 12.Liu Y, Yan LM, Wan L, Xiang TX, Le A, Liu JM, et al. Viral dynamics in mild and severe cases of COVID-19. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30232-2. pii: S1473-3099 (20) 30232-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R. StatPearls [Internet] Treasure Island (FL): StatPearls Publishing; 2020. Features, Evaluation and Treatment Coronavirus (COVID-19) Available from: http://www.ncbi.nlm.nih.gov/books/NBK554776/ Last cited on 2020 May 13. [PubMed] [Google Scholar]
- 14.Yang AP, Liu JP, Tao WQ, Li HM. The diagnostic and predictive role of NLR, d-NLR and PLR in COVID-19 patients. Int Immunopharmacol. 2020:84. doi: 10.1016/j.intimp.2020.106504. 106504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lippi G, Lavie CJ, Sanchis-Gomar F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): Evidence from a meta-analysis. Prog Cardiovasc Dis. 2020 doi: 10.1016/j.pcad.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020;395:1054–62. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Giannis D, Ziogas IA, Gianni P. Coagulation disorders in coronavirus infected patients: COVID-19, SARS-CoV-1, MERS-CoV and lessons from the past. J Clin Virol. 2020;127:104362. doi: 10.1016/j.jcv.2020.104362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, et al. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up. J Am Coll Cardiol. 2020 doi: 10.1016/j.jacc.2020.04.031. pii: S0735-1097 (20) 35008-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rodrigues JCL, Hare SS, Edey A, Devaraj A, Jacob J, Johnstone A, et al. An update on COVID-19 for the radiologist – A British society of Thoracic Imaging statement. Clin Radiol. 2020;75:323–5. doi: 10.1016/j.crad.2020.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wong HYF, Lam HYS, Fong AH, Leung ST, Chin TW, Lo CSY, et al. Frequency and distribution of chest radiographic findings in COVID-19 positive patients. Radiology. 2020:201160. doi: 10.1148/radiol.2020201160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: A report of 1014 cases. Radiology. 2020:200642. doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18:1094–9. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Klok FA, Kruip MJ, Van der Meer NJ, Arbous MS, Gommers DA, Kant KM, et al. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: An updated analysis. Thromb Res. 2020 doi: 10.1016/j.thromres.2020.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Middeldorp S, Coppens M, van Haaps TF, Foppen M, Vlaar AP, Müller MC, et al. Incidence of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost. 2020 doi: 10.1111/jth.14888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rouhezamin MR, Haseli S. Diagnosing Pulmonary Thromboembolism in COVID-19: A Stepwise Clinical and Imaging. Approach Acad Radiol. 2020 doi: 10.1016/j.acra.2020.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stawicki SP, Sims CA, Sharma R, Weger NS, Truitt M, Cipolla J, et al. Vena cava filters: a synopsis of complications and related topics. The Journal of Vascular Access. 2008;9:102–10. [PubMed] [Google Scholar]
- 27.Zhang L, Wang B, Zhou J, Kirkpatrick J, Xie M, Johri AM. Bedside Focused Cardiac Ultrasound in COVID-19 Infection From the Wuhan Epicenter: The Role of Cardiac Point of Care Ultrasound (POCUS), Limited Transthoracic Echocardiography and Critical Care Echocardiography. J Am Soc Echocardiogr. 2020 doi: 10.1016/j.echo.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kent A, Bahner DP, Boulger CT, Eiferman DS, Adkins EJ, Evans DC, et al. Sonographic evaluation of intravascular volume status in the surgical intensive care unit: a prospective comparison of subclavian vein and inferior vena cava collapsibility index. J Surg Res. 2013;184:561–6. doi: 10.1016/j.jss.2013.05.040. [DOI] [PubMed] [Google Scholar]
- 29.Connors JM, Levy JH. Thromboinflammation and the hypercoagulability of COVID-19. J Thromb Haemost. 2020 doi: 10.1111/jth.14849. [DOI] [PMC free article] [PubMed] [Google Scholar]