ABSTRACT
Background
PTSD in pregnant women is associated with adverse outcomes for mothers and their children. It is unknown whether pregnant women with PTSD, or symptoms of PTSD, can receive targeted treatment that is safe and effective.
Objective
The purpose of the present paper was to assess the effectiveness and safety of treatment for (symptoms of) PTSD in pregnant women.
Method
A systematic review was conducted in accordance with the PRISMA guidelines in Pubmed, Embase, PsychINFO, and Cochrane. In addition, a case is presented of a pregnant woman with PTSD who received eye-movement desensitization and reprocessing (EMDR) therapy aimed at processing the memories of a previous distressing childbirth.
Results
In total, 13 studies were included, involving eight types of interventions (i.e. trauma-focused cognitive behavioural therapy, exposure therapy, EMDR therapy, interpersonal psychotherapy, explorative therapy, self-hypnosis and relaxation, Survivor Moms Companion, and Seeking Safety Intervention). In three studies, the traumatic event pertained to a previous childbirth. Five studies reported obstetrical outcomes. After requesting additional information, authors of five studies indicated an absence of serious adverse events. PTSD symptoms improved in 10 studies. However, most studies carried a high risk of bias. In our case study, a pregnant woman with a PTSD diagnosis based on DSM-5 no longer fulfilled the criteria of PTSD after three sessions of EMDR therapy. She had an uncomplicated pregnancy and delivery.
Conclusion
Despite the fact that case studies as the one presented here report no adverse events, and treatment is likely safe, due to the poor methodological quality of most studies it is impossible to allow inferences on the effects of any particular treatment of PTSD (symptoms) during pregnancy. Yet, given the elevated maternal stress and cortisol levels in pregnant women with PTSD, and the fact that so far no adverse effects on the unborn child have been reported associated with the application of trauma-focused therapy, treatment of PTSD during pregnancy is most likely safe.
KEYWORDS: Posttraumatic stress disorder, eye movement desensitization and reprocessing therapy, pregnancy, childbirth, trauma, treatment
HIGHLIGHTS: • This is the first systematic review about the treatment of PTSD during pregnancy.• There is a large heterogeneity in study designs, and a lack of obstetrical outcome and safety measurements.• The findings suggest treatment of PTSD during pregnancy is safe.
Antecedentes: El TEPT en mujeres embarazadas se asocia con consecuencias adversas para las madres y sus hijos. Se desconoce si las mujeres que están embarazadas y sufren de TEPT, o síntomas de TEPT, pueden recibir un tratamiento dirigido que sea seguro y efectivo.
Objetivo: El objetivo del presente trabajo fue evaluar la efectividad y la seguridad del tratamiento para (síntomas de) TEPT en mujeres embarazadas.
Método: Se realizó una revisión sistemática de acuerdo con las directrices PRISMA en Pubmed, Embase, PsychINFO y Cochrane. Además, se presenta un caso de una mujer embarazada con TEPT que recibió terapia de desensibilización y reprocesamiento por movimientos oculares (EMDR) destinada a procesar los recuerdos de un parto traumático anterior.
Resultados: En total, se incluyeron 13 estudios, que incluyeron ocho tipos de intervenciones (es decir, terapia cognitivo conductual centrada en el trauma, terapia de exposición, terapia EMDR, psicoterapia interpersonal, terapia exploratoria, autohipnosis y relajación, Compañera de madres sobrevivientes e intervención de Búsqueda de Seguridad). En tres estudios, el evento traumático pertenecía a un parto previo. Cinco estudios informaron consecuencias obstétricas. Después de solicitar información adicional, los autores de cinco estudios indicaron la ausencia de eventos adversos graves. Los síntomas de TEPT mejoraron en diez estudios. Sin embargo, la mayoría de los estudios conllevaban un alto riesgo de sesgo. En nuestro estudio de caso, una mujer embarazada con diagnóstico de TEPT basado en DSM-5 ya no cumplía los criterios de TEPT después de tres sesiones de terapia EMDR. Ella tuvo un embarazo y parto sin complicaciones.
Conclusión: Debido a la mala calidad metodológica de la mayoría de los estudios, es imposible permitir inferencias sobre los efectos de cualquier tratamiento particular de TEPT (síntomas) durante el embarazo. Sin embargo, dado el elevado nivel de estrés materno y los niveles de cortisol en mujeres embarazadas con TEPT, y el hecho de que hasta ahora no se han reportado efectos adversos en el feto asociados con la aplicación de terapia centrada en el trauma, el tratamiento del TEPT durante el embarazo es muy seguro.
PALABRAS CLAVE: Trastorno de estrés postraumático, terapia de desensibilización y reprocesamiento por movimiento ocular, embarazo, parto, trauma, tratamiento
背景: 孕妇的PTSD与母亲及其子女的负面后果有关。尚不清楚患有PTSD或具有PTSD症状的孕妇是否可以接受安全有效的靶向治疗。
目标: 本文旨在评估孕妇PTSD (症状) 治疗的有效性和安全性。
方法: 按照PRISMA指南, 在Pubmed, Embase, PsychINFO和Cochrane中进行了系统综述。此外, 还介绍了一个患有PTSD的孕妇的案例, 该女子接受了旨在处理先前痛苦的分娩记忆的眼动脱敏与再加工 (EMDR) 疗法。
结果: 总共纳入13项研究, 涉及八种类型的干预措施 (即聚焦创伤认知行为疗法, 暴露疗法, EMDR疗法, 人际心理疗法, 探索性疗法, 自我催眠和放松, 幸存妈妈陪伴以及寻求安全干预) 。三项研究中创伤事件与先前的分娩有关。五项研究报告了分娩结局。在请求提供更多信息后, 五项研究的作者指出没有严重的不良事件。十项研究PTSD症状有所改善。然而, 大多数研究带有很高风险的偏差。在我们的案例研究中, 基于DSM-5诊断为PTSD的孕妇在三疗程EMDR治疗后不再符合PTSD的标准, 怀孕和分娩过程都很简单。
结论: 由于大多数研究的方法学质量较差, 因此无法推断妊娠期间对PTSD (症状) 的任何特殊治疗的效果。然而, 考虑到PTSD孕妇的母体应激水平和皮质醇水平升高, 以及目前尚无报告对未出生婴儿的不良影响与聚焦创伤疗法相关, 因此妊娠期PTSD的治疗很有可能是安全的。
关键词: 创伤后应激障碍, 眼动脱敏与再加工疗法, 妊娠, 分娩, 创伤, 治疗
Although pregnancy and childbirth are generally considered to be positive life events, 10–20% of women experience birth as a traumatic event (Alcorn, O’Donovan, Patrick, Creedy, & Devilly, 2010; Haagen, Moerbeek, Olde, Van Der Hart, & Kleber, 2015; Olde et al., 2005; Soet, Brack, & DiIorio, 2003; Stramrood et al., 2011). It is estimated that 3% of women develop posttraumatic stress disorder (PTSD) following childbirth (Ayers, Bond, Bertullies, & Wijma, 2016; Grekin & O’Hara, 2014), albeit in at-risk groups the proportion of individuals who develop PTSD is much higher (15.7%; Grekin & O’Hara, 2014). However, women may also be exposed to other, unrelated, traumatic events prior to pregnancy. For example, there is evidence to suggest that in community samples the prevalence of PTSD during pregnancy is about 3%, and that in high-risk groups almost 20% of pregnant women suffer from PTSD (Yildiz, Ayers, & Phillips, 2016). PTSD symptoms may continue into subsequent pregnancies if they are not diagnosed and treated adequately (Söderquist, Wijma, & Wijma, 2006), and may even increase in severity (Beck & Watson, 2010). This is important, because experiencing posttraumatic stress during pregnancy has been associated with negative maternal and foetal outcomes, such as low birth-weight (Cook, Ayers, & Horsch, 2018).
There are several diagnostic challenges regarding PTSD after childbirth that make it difficult to timely initiate adequate treatment. The core features of PTSD are re-experiencing, avoidance and numbing, negative cognitions and mood, and hyperarousal (American Psychiatric Association, 2013). In the postpartum period, for both patient, partner, and medical professional it may be difficult to differentiate posttraumatic stress symptoms from physiological characteristics of the maternity period, including recurrent thoughts of the delivery, sleeping problems, concentration difficulties, emotional dysregulation, irritability, and hypervigilance (Ayers, Wright, & Ford, 2015). Symptoms of PTSD could also easily be mistaken for postpartum depression, since both PTSD and depression may include negative mood and cognitions. The prevalence of childbirth-related PTSD is higher when pregnancy or childbirth are complicated (Ayers et al., 2016). However, it is important to emphasize that symptoms of PTSD may also occur after uneventful deliveries, which makes it even more difficult to be recognized and detected. Lastly, the core PTSD feature avoidance may result in avoiding conversations about the childbirth, or cancellation of appointments with professionals, thereby complicating adequate assessment of PTSD symptoms. Conceivably, avoidance symptoms may lead to terminating the pregnancy, or demanding a planned caesarean, whereas it also has been observed that in a subsequent pregnancy, pregnant women avoid prenatal care (Fuglenes, Aas, Botten, Øian, & Kristiansen, 2011).
While there are a number of first choice trauma-focused psychotherapeutic interventions for treating symptoms of PTSD available (National Institute for Health and Clinical Excellence (NICE), 2018), unfortunately, pregnant women are often excluded or severely underrepresented in clinical research (Shields & Lyerly, 2013). Consequently, there is a lack of evidence about the effectiveness and potential risks of treating PTSD (symptoms) during pregnancy. Clearly, in PTSD, trauma memories are related to psychological and physiological distress, and trauma-focused therapies include processing the trauma memories. Because it can’t be ruled out that this short-term arousal is harmful for the unborn child, patients and professionals are reluctant to start therapy for symptoms of PTSD (e.g. Forgash, Leeds, Stramrood, & Robbins, 2013) which is likely to lead to postponing psychological treatment until after childbirth. Conversely, untreated PTSD equals a continuous amount of psychological distress, and an elevated level of stress hormones (e.g. cortisol), which may lead to complications later in life (Graham et al., 2019; LeWinn et al., 2009). To this end, it is unknown whether we might do more harm by treating a pregnant woman while she suffers from PTSD than withholding pregnant women an evidence-based treatment (e.g. PE, CBT, EMDR therapy) for symptoms of PTSD.
The purpose of the present paper was to conduct a systematic review to assess the effects of applying both trauma-focused and non-trauma-focused therapies for PTSD symptoms in pregnant women. Therapies were considered trauma-focused in case they are psychotherapies for PTSD involving direct discussion of the traumatic event. Examples are EMDR therapy, prolonged exposure, cognitive restructuring aimed at trauma-related beliefs, and other therapeutic procedures such as written autobiographical narratives, and hypnosis. Because it is difficult to evaluate the effects of different trauma histories we were interested in the effects of these therapies on women with PTSD in general; that is, women with childbirth-related PTSD and/or PTSD from any trauma. More specifically, we aimed to determine the effectiveness and safety (both psychological as obstetric outcomes) of therapy for these PTSD symptoms during pregnancy. In addition, given the lack of studies on the effects of trauma-focused treatment of pregnant women that have formally been classified as having PTSD, the absence of cases diagnosed using the Clinician Administered PTSD Scale (CAPS-5), and to further enrich the literature on this subject, we report the results of a first-line trauma-focused therapy (i.e. EMDR therapy) in a pregnant woman with PTSD aimed at processing the memories of a previous distressing childbirth.
1. Methods of literature review
1.1. Literature search
A systematic search of the literature was carried out in accordance with the PRISMA guidelines (Moher, Liberati, Tetzlaff, & Altman, 2009). The current study was registered prospectively in the PROSPERO database. Relevant articles that were published from 1980 to June 2019 were identified in four databases (PubMed, Embase, PsychINFO, and Cochrane Library). Search terms consisted of a combination of several synonyms for post-traumatic stress disorder/trauma, pregnancy/childbirth/postpartum, and treatment, in combination with relevant database-specific MeSH terms (Appendix A). The language was restricted to English and Dutch. After removing all duplicates, author MB reviewed all title and abstracts. The remaining articles were assessed for eligibility by full-text reviewing by both MB and LB. Inclusion criteria consisted of (1) pregnant women in research population, (2) intervention study, (3) outcome including PTSD diagnosis or PTSD symptoms. Inclusion was not restricted to trauma-focused or evidence-based interventions. In addition, references were searched for relevant articles that fulfilled the inclusion criteria. After discussion, consensus was reached among the reviewers in all cases. Independently, data were extracted by both reviewers using a standardized data abstraction form, and a quality assessment was performed using the Cochrane Risk of Bias Tool (Higgins & Altman, 2008). Minor disagreements were discussed and consented. Interventions were referred to as trauma-focused if they consisted of evidence-based psychotherapy for PTSD, involving direct discussion of the traumatic event (e.g. imagery exposure, cognitive restructuring of trauma-related beliefs, EMDR therapy). Safety was defined as the absence of any adverse events, such as increased suicidal ideation, suicidal attempts, serious self-injurious behaviour (injuries that needed hospitalization) and crisis contacts (contacts with healthcare providers in case of mental health crisis, where a person thinks about suicide of self-harm) for any of the aforementioned reasons (FDA, 2016). Regarding obstetrical safety, we evaluated serious adverse events in terms of preterm birth earlier than 32 weeks gestational age, foetal growth restriction, or (maternal, foetal, or neonatal) death.
2. Methods of case study
A pregnant woman was randomized for EMDR therapy within the OptiMUM-study, a multicentre Randomized Controlled Trial that evaluates the safety and efficacy of EMDR therapy for pregnant women with PTSD or Fear of Childbirth after previous childbirth (Baas, Stramrood, Dijksman, de Jongh, & van Pampus, 2017).
EMDR therapy included all eight phases of the EMDR standard (three-pronged) protocol. To address patients’ anticipatory fear and avoidance behaviour (i.e. giving birth to another child), the flashforward protocol (Logie & de Jongh, 2014) was applied to target patients’ most scary fantasies (i.e. the baby dying intrapartum, or the need for an emergency caesarean section). This was followed with a mental video check: the patient imagines a movie of a future confrontation with the situation or object, seeing themselves coping with the challenges. If the patient feels any tension, she opens her eyes and a set of eye movements will be conducted before continuing the mental video. This is repeated until the movie can be played without any significant disturbance (Logie & de Jongh, 2014; Shapiro, 2018). EMDR therapy was carried out with the use of rapid deployment of sets of eye movements. To maximize taxation of patients’ working memory (de Jongh, Ernst, Marques, & Hornsveld, 2013), the therapist was allowed to switch to the use of a light bar in combination with earphones with a clicking sound, alternating to either the left or the right ear, and two hand-holdable pulsers providing alternating bilateral, tactile stimulation.
2.1. Measures
The WDEQ (Wijma Delivery Expectations/experiences Questionnaire A/B; Wijma, Wijma, & Zar, 1998) assesses Fear of Childbirth (FoC) during pregnancy (version A), or after delivery (version B) in terms of the woman’s cognitive appraisal of childbirth. It is possible to dichotomize the total sum score to conclude if there is FoC or not (cut-off ≥85) (Wijma et al., 1998).
The PSS-SR (PTSD symptom scale) (Foa, Cashman, Jaycox, & Perry, 1997) is a 17-item self-report questionnaire that was used to assess the course of PTSD-symptoms.
The Dutch CAPS-5 (Clinician-administered PTSD scale) was used (Boeschoten et al., 2014). The CAPS is the gold standard for diagnosing PTSD according to DSM-5.
The MINI-plus (Mini international neuropsychiatric interview-plus) (Sheehan et al., 1998) is a structured interview for axis I DSM-IV conditions, and was used to evaluate comorbidity.
3. Results of the systematic review
Figure 1 presents the stage-wise results of the article selection process. The literature search resulted in 10.927 eligible articles. After eliminating duplicates, a total of 7808 articles remained. Next, 7780 articles were excluded after reviewing title and abstract because these did not meet inclusion criteria. Subsequently, full-text review took place of the pre-selected 28 articles by both reviewers. In addition, three articles were included from reference lists of the selected articles. Finally, 13 articles were included for the analysis (Tables 1 and 2). Due to large heterogeneity between the studies in design, study population and measurement of symptoms, pooling of data for a meta-analysis proved not to be feasible.
Figure 1.
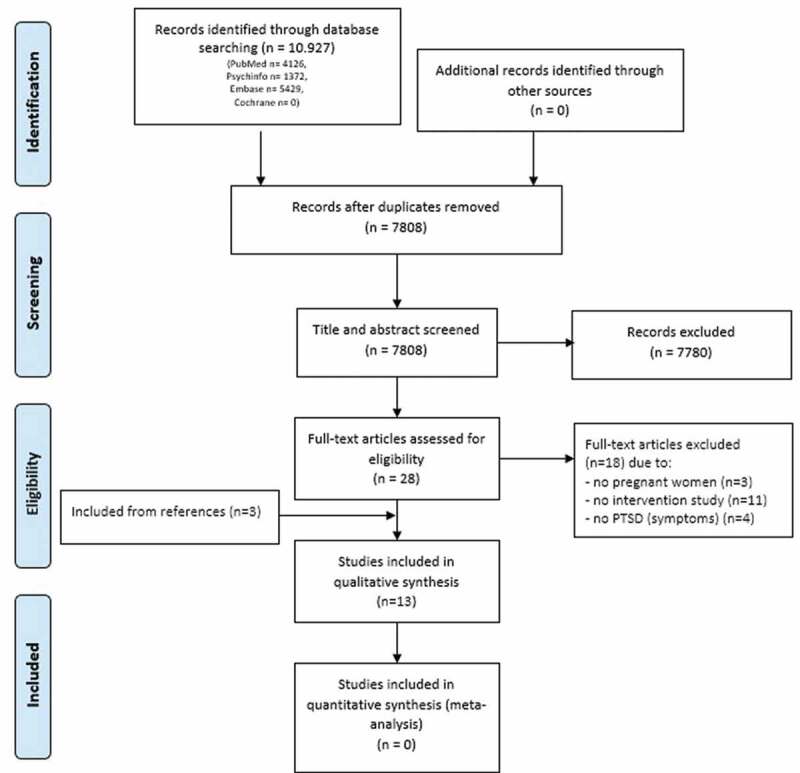
Article selection process.
Table 1.
Characteristics of included studies.
| Author | Type of study | N | Inclusion criteria | Exclusion criteria | Type of intervention | Number of sessions |
Traumatic event | Assessment of (symptoms of) PTSD |
|---|---|---|---|---|---|---|---|---|
| Beck and Barnes (2006) | Case series | 1 of 2 | Not reported | Not reported | Psycho-education | Not reported | Foetal reduction | No instruments |
| Kavakci et al. (2014) | Case series | 1 of 5 | Inpatient pregnant women with therapy-resistant hyperemesis | Not reported | EMDR therapy (tapping) | 2 | Domestic violence | No instruments |
| Madigan et al. (2015) | RCT | 10 intervention versus 11 controls | Adolescents between 12–23 weeks pregnant, planning to keep their baby, fluent in English, meeting criteria for an unresolved classification on the AAI or DSM-IV criteria for PTSD | Current suicidal ideation, ongoing substance use and/or evidence of psychosis | Trauma-focused CBT | 12 | Not reported | C-PTSD-I |
| Rowe et al. (2014) | Quasi-experimental study | 17 intervention versus 43 matched controls | Pregnant women with a history of childhood maltreatment | Active psychotic disorders, untreated substance abuse, past year suicide attempts, intimate partner or parents abuse, high-risk pregnancy conditions, psychotropic medication, current long-term psychotherapy | Psycho-education (“Survivor Moms Companion”) | 10 | Childhood maltreatment | NWS-PTSD |
| Sandstrom et al. (2008) | Case series | 1 of 4 | Severe fear of childbirth after a previous traumatic childbirth, DSM-IV PTSD | Not reported | EMDR therapy | 2 | Childbirth | TES |
| Seng et al. (2011) | Quasi-experimental study | 32 | English speaking, currently at less than 28 weeks gestational age, a history of childhood maltreatment or sexual trauma, experiencing at least some posttraumatic stress sequelae, willingness to complete the modules and measures | Active psychotic disorders, untreated substance abuse, past year suicide attempts, intimate partner or parents abuse, high-risk pregnancy conditions, psychotropic medication, current long-term individual psychotherapy | Psycho-education (“Survivor Moms Companion”) | 10 | Childhood maltreatment or sexual abuse | NWS-PTSD |
| Slater (2015) | Case series | 2 | Pregnant women with posttraumatic stress disorder | Not reported | Self-hypnosis, relaxation, rewind technique. Spiegel induction method. | 4/not reported | Childbirth | No instruments |
| Sperlich et al. (2011) | Quasi-experimental study | 32 | (see Seng et al., 2011) | (see Seng et al., 2011) | Psycho-education (“Survivor Moms Companion”) | 10 | Childhood maltreatment or sexual trauma | NWS-PTSD |
| Stevens et al. (2019) | Cohort study | 21 | Less than 30 weeks pregnant, history of physical or sexual abuse, reported at least three or more PTS symptoms, fluent in English. Completing at least three sessions of CBT. | History of bipolar disorder or psychosis, significant suicidal ideation or risk, or suffered from medical conditions that would impact participation | CBT (non-trauma-focused), trauma-sensitive care, | 6 | Physical or sexual abuse | PCL-C |
| Stramrood et al. (2012) | Case series | 3 | Pregnant women with posttraumatic stress symptoms following previous birth | Not reported | EMDR therapy | 2-4 | Childbirth | No instruments |
| Twohig and Donohue (2007) | Case series | 1 | Not reported | Not reported | Exposure therapy (trauma-focused) |
14 | A series of traumatic events, including abuse | SCID, PCL-C |
| Weinreb et al. (2018) | RCT | 89 intervention versus 60 controls | Screenings at threshold level (3–4 symptoms) or sub-threshold level (2 symptoms) on PC-PTSD, ≥18 years old, < 27 weeks gestation, spoke one of the languages of the prenatal care advocates. | Not reported | Psycho-education (“Seeking Safety intervention”) | 8 | Multiple types of trauma, the majority physical or sexual abuse | PC-PTSD, PSS |
| Zlotnick (2011) | RCT | 28 versus 26 controls | Pregnant women between 18–40 years old, with intimate partner violence in the past year | Current affective disorders, PTSD or substance use as determined by SCID-NP | Interpersonal psychotherapy | 5 | Intimate partner violence | DTS |
AAI = Adolescent/Adult Attachment Interview, CBT = Cognitive Behavioural therapy, C-PTSD-I = Children’s PTSD Inventory, DSM = Diagnostic and Statistical Manual of Mental Disorders, DTS = Davidson Trauma Scale, EMDR = Eye-Movement Desensitization and Reprocessing therapy, PCL-C = PTSD Symptom Checklist for Civilians, PC-PTSD = Primary Care-PTSD screen, PSS = Posttraumatic Stress Scale, PTSD = Posttraumatic Stress Disorder, SCID = Structured Clinical Interview for the DSM, NWS-PTSD = National Women’s Study PTSD Module, Traumatic Event Scale.
Table 2.
Effects and safety of interventions of included studies.
| Author | Retention (% completers) |
Effects (symptom measurement, or if absent, indirect measurements) | Safety | Follow-up |
|---|---|---|---|---|
| Beck and Barnes (2006) | 1/1 (100%) | Undergoing caesarean delivery without any significant anxiety or fear. | Healthy infant | Not reported |
| Kavakci and Yenicesu (2014) | 1/1 (100%) | Complete remission of PTSD symptoms | No serious adverse events | Timing not specified |
| Madigan et al. (2015) | 12/21 (57%) at leat five sessions | No differences on PTSD classification between groups | Not reported | 6 and 12 months postpartum |
| Rowe et al. (2014) | 69% | The intervention group had significantly less dissociation in labour (d = 0.46) compared to the control group. No significant results in PTSD symptoms. | (see Sperlich et al., 2011) | Not reported |
| Sandström et al. (2008) | 0/1 (did not show at final appointment) | At the end of the last session SUD related to the emotionality of the traumatic memory decreased. However, other disturbing memories started to appear during therapy. After treatment: missing data at one year postpartum. Three years postpartum PTSD cluster and sum score decreased. | Not reported | 1-3 years |
| Seng et al. (2011) | 18/32 (56%) all ten modules | Intention-to-treat analysis showed no significant change in PTSD symptoms. In completers, there was a significant decrease in level of PTSD symptoms (η2 = 0.5). | (see Sperlich et al., 2011) | Not reported |
| Slater (2015) | 2/2 (100%) | Patient 1: Still anxious, but persistent neutral feelings about previous childbirth. | Uneventful caesarean, healthy baby | A few weeks |
| Patient 2: relaxation during hypnosis. Remained anxious after delivery, but suffered no adverse psychological disturbances. | Healthy infant | Not reported | ||
| Sperlich et al. (2011) | 18/32 (56%) all ten modules | PTSD scores as indexed with MPSS decreased significantly (large effect size). | No serious adverse events | Not reported |
| Stevens et al. (2019) | 21/45 (46%) at least three sessions | Four participants (19%), and one participant (4,8%) demonstrated significant improvements in PTSD symptoms direct posttreatment and 6 weeks postpartum compared to pretreatment. | No serious adverse events | 6 weeks postpartum |
| Stramrood et al. (2012) | 3/3 | Patient 1: No physical symptoms when passing the hospital, more relaxed, less emotional, no guilt. Attempted vaginal childbirth. | No serious adverse events. Caesarean, healthy infant. Positive birth experience | Not reported |
| Patient 2: Calmer, less alone, more confident about upcoming birth. Attempting vaginal childbirth instead of elective caesarean at first | No serious adverse events. Uncomplicated vaginal childbirth, positive birth experience | Not reported | ||
| Patient 3: No posttraumatic stress symptoms, no debilitating anxiety, calmer, better emotional coping. | No serious adverse events. Postpartum haemorrhage (1100 ml) and hypertension. Positive birth experience | Not reported | ||
| Twohig and Donohue (2007) | 1/1 | PTSD symptoms decreased throughout treatment, and this decrease continued at follow-up two months after treatment. | No serious adverse events Vaginal delivery, healthy mother and infant |
Two months after treatment |
| Weinreb et al. (2018) | 51/89 (57%) all sessions | PTSD symptoms decreased over time in both groups, but the intervention group showed significantly greater improvements(d = 0.34). | No significant differences in birth outcome | One month postpartum |
| Zlotnick et al. (2011) | Not reported | No significant reduction of symptoms of PTSD during pregnancy or postpartum. During pregnancy moderate effect for reducing PTSD symptoms (d = 0.78) and from pregnancy up to three months postpartum (d = 0.35). | Not reported | Three months postpartum |
Note. HG = hyperemesis gravidarum, OO = Obstetrical Outcome, MPSS = Modified Posttraumatic Stress Disorder (PTSD) Symptom Scale, NR = not-reported, PCL-C = PTSD Checklist Civilian Version, PTSD = Posttraumatic Stress Disorder.
3.1. Setting and design
All studies were published in English. All but one (Kavakci & Yenicesu, 2014) studies were conducted in high-income countries. Recruitment methods varied widely. Some studies included only patients that were self-referred (e.g. Beck & Barnes, 2006; Twohig & Donohue, 2007) or referred by their maternity care provider (Slater, 2015; Stramrood et al., 2012) based on reporting PTSD (symptoms), while in two studies recruitment consisted of screening all pregnant women of a certain cohort for PTSD (symptoms) (e.g. Stevens et al., 2019; Weinreb, Wenz-gross, & Upshur, 2018). One study (Kavakci & Yenicesu, 2014) included pregnant women during their hospital admission for hyperemesis gravidarum, whereas in all other studies recruitment took place in outpatient settings. Gestational age at the start of therapy was reported in eight out of 13 included studies. In four studies therapy started before the third trimester without any further specification (Seng, Sperlich, Rowe, & Cameron, 2011; Sperlich, Seng, Rowe, & Cameron, 2011; Stevens et al., 2019; Weinreb et al., 2018), in two studies the intervention started in the second trimester (Madigan et al., 2015; Twohig & Donohue, 2007), and in two studies in the third trimester (Beck & Barnes, 2006; Slater, 2015).
Four out of 13 studies contained a control group (Madigan et al., 2015; Rowe, Sperlich, Cameron, & Seng, 2014; Weinreb et al., 2018; Zlotnick, Capezza, & Parker, 2011). In three of these studies the effectiveness of the intervention was compared with standard prenatal care, whereas in the fourth study (Rowe et al., 2014) participants in the control group were offered educational material and a listing of resources for victims of domestic violence in addition to standard prenatal care.
3.2. Participants
Correcting for two studies describing the same sample of 32 participants (Seng et al., 2011; Sperlich et al., 2011), treatments aimed at symptoms of PTSD were evaluated in a total of 206 pregnant women. In three out of the 13 included studies the traumatic event was patients’ first childbirth (Sandström, Wiberg, Wikman, Willman, & Högberg, 2008; Slater, 2015; Stramrood et al., 2012) and in one study an obstetric procedure (Beck & Barnes, 2006). In the other studies, the traumatic events included childhood maltreatment, physical or sexual abuse and in two studies (Twohig & Donohue, 2007; Weinreb et al., 2018) a series of such events.
3.3. Assessment
Validated instruments to assess symptoms of PTSD were used in nine of the 13 studies. In only five of these a DSM-IV PTSD-diagnosis was established using a standardized clinician-administered interview for PTSD (Madigan et al., 2015; Rowe et al., 2014; Seng et al., 2011; Sperlich et al., 2011; Twohig & Donohue, 2007; see Table 1). In four of the 13 studies, no formal instruments (i.e. established clinical interviews or self-report questionnaires) were used. The gold standard for diagnosing PTSD, the Clinician Administered PTSD Scale (CAPS-5; Boeschoten et al., 2014), was not used in any of the included studies. Whether or not psychiatric comorbidity was present was reported in two studies (Madigan et al., 2015; Stramrood et al., 2012).
3.4. Interventions
The 13 included studies contained the use of eight types of interventions. These interventions can be categorized into six different therapeutic frameworks or approaches, of which four were aimed at targeting memories of traumatic events (Kavakci & Yenicesu, 2014; Madigan et al., 2015; Sandström et al., 2008; Slater, 2015; Stramrood et al., 2012; Twohig & Donohue, 2007) and two include other ways to cope with the symptoms related to PTSD (Beck & Barnes, 2006; Rowe et al., 2014; Seng et al., 2001; Sperlich et al., 2011; Stevens et al., 2019; Zlotnick et al., 2011, see Table 1). Five studies evaluated evidence-based treatments for PTSD (Kavakci & Yenicesu, 2014; Madigan et al., 2015; Sandström et al., 2008; Stramrood et al., 2012; Twohig & Donohue, 2007). In two case studies, each on one patient, the number of sessions was not described (Beck & Barnes, 2006; Slater, 2015). In all other studies, the interventions varied largely in duration, ranging from two sessions of an unknown amount of minutes (Kavakci & Yenicesu, 2014) to a total of 14 sessions with 30–45 minutes of in-session exposure in session 5 to session 14 (Twohig & Donohue, 2007).
3.4.1. Trauma-focused therapy
Trauma-focused treatments were evaluated in six studies. One study used 12 sessions trauma-focused cognitive behavioural therapy (TF-CBT; Madigan et al., 2015). Twohig et al. (2007) applied 14 sessions of exposure therapy only. Three studies examined two to four sessions of standard EMDR therapy (Kavakci & Yenicesu, 2014; Sandström et al., 2008; Stramrood et al., 2012). Slater (2015) investigated self-hypnosis and relaxation and ‘rewind techniques’ aimed at the traumatic event.
3.4.2. Non-trauma-focused interventions
A non-trauma-focused treatment approach was evaluated in seven studies. Zlotnick et al. (2011) examined the effect of four-session interpersonal psychotherapy which included helping patients improving their social network, and other forms of empowerment to prepare them for their transition into motherhood. All other studies evaluating a non-trauma-focused treatment offered interventions in a psychoeducational framework. Beck et al. (2006) studied a psychoeducational intervention focused on normalizing the future birth experience by making realistic expectations. Stevens et al. (2019) evaluated a method named TO-CARE (Trauma-sensitive Obstetrics to promote Control, Anxiety-Reduction, and Empowerment), in which six weekly sessions of cognitive behavioural therapy (CBT) were conducted including trauma education, relaxation techniques, assertive communication skills, and enhancing coping. In addition, patients were supported to use adequate coping mechanisms by their obstetric physicians, who were coached to recognize and support patients with symptoms of PTSD. Three studies from one research group examined the use of the ‘Survivor Moms Companion’ self-study intervention (Rowe et al., 2014; Seng et al., 2011; Sperlich et al., 2011), which includes 10 self-study modules aimed at psycho-education, skills training, and addressing the woman’s needs in terms of emotional support. One study examined the effects of the ‘Seeking Safety Intervention’, an eight-session intervention also focusing on developing adequate mechanisms to cope with symptoms of PTSD (Weinreb et al., 2018).
3.5. Treatment effectiveness
Improvement of PTSD symptoms was reported in 10 of the 13 studies, yielding significant results in four studies (Seng et al., 2011; Sperlich et al., 2011; Stevens et al., 2019; Weinreb et al., 2018). All three studies that evaluated EMDR therapy showed a decrease in PTSD symptoms in short term as well as in follow-up (Kavakci & Yenicesu, 2014; Sandström et al., 2008; Stramrood et al., 2012), effects that lasted up to 36 months (Sandström et al., 2008). However, due to the nature of the EMDR studies being case series, the significance could not be tested. Application of CBT (Twohig & Donohue, 2007) resulted in a decrease in PTSD, and TF-CBT (Stevens et al., 2019) reached a significant decrease in PTSD symptoms on self-report measurements. Finally, two interventions aimed at psycho-education (i.e. ‘Seeking Safety Intervention’ and ‘Survivor Moms Companion’) showed a significant decrease in PTSD symptoms in three studies (Seng et al., 2011; Sperlich et al., 2011; Weinreb et al., 2018).
3.6. Outcome measures of safety
Only one study explicitly reported a strategy for collecting or analysing safety information (Sperlich et al., 2011). The authors reported no adverse events. Obstetrical outcome was not reported in eight of the 13 included studies, and quantified in only one (Weinreb et al., 2018). Stramrood et al. (2012) reported a postpartum haemorrhage in one patient with pre-existent risk factors for postpartum haemorrhage. Because this incident does not fit our safety definition we did not consider it as a serious adverse event.
Due to this lack of safety data, corresponding authors were contacted for any additional information. Of the 11 authors that were contacted, six authors responded. They reported no additional safety information (Madigan et al., 2015; Seng et al., 2001) or indicated an absence of occurrence of adverse events (Kavakci & Yenicesu, 2014; Stevens et al., 2019; Stramrood et al., 2012; Twohig & Donohue, 2007).
4. Risk of bias in included studies
Three of the included studies were conducted as randomized controlled trials, all other studies, therefore, have a considerable risk of bias. The risk of bias is summarized for each study in Figure 2. Nine of the 13 studies evaluated one type of intervention, resulting in a lack of applicability of several aspects of risk of bias analysis. Although blinding of participants and personnel when conducting psychological interventions is impossible, blinding of outcome measurements is possible. Only Madigan et al. (2015) reported blinded outcome assessment while all other studies did not report on blinding.
Figure 2.

Risk of bias summary of included studies.
5. Results of the case study
Patient A was a 36 year old multipara pregnant woman, who delivered three times before. Her first delivery was complicated by a postpartum haemorrhage due to a retained placenta. In her second pregnancy, she received one EMDR session aimed at the loss of control during her first delivery. Her PTSD symptoms decreased after this therapy session and the delivery was uncomplicated. In her third pregnancy, an intra-uterine foetal death occurred unexpectedly at a gestational age of 39 weeks. Postpartum, she received about 10 monthly sessions of grief therapy.
During the screening for the OptiMUM-study in her fourth pregnancy, she scored above the cut-off for both PTSD and FoC (WDEQ-A total score: 98). During the first clinical interview, she was diagnosed with an obsessive compulsive disorder with intrusive thoughts preoccupied with guilt about several aspects of her life. When administering the CAPS-5, at first she identified her first childbirth as the ‘worst’ in terms of emotional difficulties in the aftermath. After continuing the interview, she quickly corrected herself: the intrauterine foetal death in her third pregnancy was the most traumatic (CAPS-5 sum score: 26).
In the first session, the treatment plan was the EMDR target, second the flash forward followed by a mental videotape. The session commenced with the EMDR target of the image of herself, sitting with her baby, and her partner hugging her and her baby. The SUD (Subjective Units of Disturbance Scale; while looking at the image, the client rates the felt disturbance on a scale 0–10, where 0 is no disturbance or neutral, 10 is the highest disturbance one can imagine) was 8, and tension was mostly felt in her abdomen. During the course of the session the SUDs went from 8 to 1. The second therapy session started with flashforward EMDR aimed at the image of herself in a hospital bed with her partner next to her, and the same doctor who diagnosed the intra-uterine foetal death saying to her ‘I have something terrible to tell you …’. Looking at this image, she felt extreme sadness, SUD 10. Besides eye movements, ‘buzzers’ were added. During the course of this session the SUDs decreased from 10 to 0 (VoC 7). She felt no tension in her body anymore.
At the start of the third session, she indicated that she was doing very well, experiencing less tension. A mental video check was conducted in which she constructed her future childbirth.
After finishing therapy, at 36 weeks gestational age, she scored under the cut-off value for FoC (WDEQ-A score 84), and the diagnoses of obsessive-compulsive disorder and PTSD (CAPS sum score 9) were in complete remission. She had an uncomplicated childbirth at term. Postpartum she rated the satisfaction around pregnancy and delivery both 8 out of 10. At follow-up, her PTSD and FoC-symptoms showed a further decrease (CAPS-5 sum score: 3; WDEQ-B: 54). For the treatment response of patient A, see Figure 3.
Figure 3.

Treatment response patient A.
6. Discussion
This is the first systematic review evaluating the effectiveness and safety of treatment for PTSD symptoms during pregnancy. The results show that the literature on this topic is scarce, and that there is large heterogeneity in study designs. The 13 included studies that have been carried out until now examined eight types of interventions of which most lacked a proper research design, six studies were small-number case series with a maximum of three cases, and only three studies used a RCT design. Although improvement in PTSD symptoms was demonstrated in 10 studies, due to the poor methodological quality of the included studies it is impossible to draw conclusions about the effectiveness or superiority of any particular treatment for PTSD or its symptoms during pregnancy. Also, many of the interventions were not evidence-based. In addition, because few studies used control groups, we cannot determine whether the interventions are better than a control group or not. Conversely, no indications were found supporting the notion that therapy aimed to reduce PTSD symptoms would be harmful.
The latter finding was supported by our single case study, including a pregnant woman with a formal DSM-5 PTSD diagnosis using the gold standard clinical interview. It was found that after three sessions of EMDR therapy, she no longer fulfilled the diagnostic criteria of PTSD, scored below the threshold for Fear of Childbirth, and experienced an uncomplicated delivery.
In this review, as far as safety data were available, we found no support for a course of action in which the continued presence of PTSD is preferable to the low chance of short-term physiological arousal during treatment for symptoms of PTSD. There is mounting evidence that PTSD is associated with elevated levels of the stress hormone cortisol. For example, Seng et al. (2018) found that pregnant women with PTSD related to childhood abuse showed cortisol levels up to 10 times higher than their non-traumatized counterparts. The effect of exposure to such high levels of maternal stress hormones on the foetal HPA-axis and related brain areas during pregnancy has been found to exert lasting negative effects on the foetus and on child development, including verbal skills, attention deficits, and learning (Graham et al., 2019; LeWinn et al., 2009; Owen, Andrews, & Matthews, 2005). Therefore, in these cases, it seems much more important to intervene, and first of all to bring down the chronic stress and related cortisol levels, so that the foetus can grow in a more optimal and safe environment, rather than fear the possible stress of the treatment of PTSD, a negative effect that has never been demonstrated.
This study has several limitations, most notably the small number of studies that are eligible to be included in systematic reviews and meta-analyses. Study populations were mostly very heterogeneous, inclusion criteria varied across studies from probable posttraumatic symptoms during intake to a formally established PTSD diagnosis, with designs not allowing pooled analyses. Measurements of symptoms of PTSD varied largely, was sometimes indirect (‘undergoing a caesarean “without significant anxiety or fear”’, Beck et al., 2006), and only five studies used a standardized clinical interview for diagnosing PTSD (Madigan et al., 2015; Rowe et al., 2014; Seng et al., 2011; Sperlich et al., 2011; Twohig & Donohue, 2007). In addition, the lack of protocolled safety measures and obstetrical outcome data of the studies that have been carried out so far is a severe limitation that makes it difficult to draw reliable conclusions. Despite these limitations, several recommendations can be made. Foremost, in future research to use validated PTSD-measures including a clinical interview. Furthermore, future studies should focus on established evidence-based treatments according to international treatment guidelines for PTSD (e.g. PE, CBT, EMDR therapy). In addition, they should have adequate designs: RCT’s with sufficient power and low risk of bias, actively monitoring safety and reporting on any adverse events, comorbid psychopathology and obstetrical outcomes.
In conclusion, due to the poor methodological quality of most studies, it is impossible to allow inferences on the effects of any particular treatment of PTSD (symptoms) during pregnancy. Yet, given the elevated maternal stress and cortisol levels in pregnant women with PTSD, and the fact that so far no adverse effects on the unborn child have been reported associated with the application of trauma-focused therapy, treatment of PTSD during pregnancy is most likely safe. Further research is necessary to rule out the possibility of harm when applying (trauma-focused or non-trauma focused) therapy, and to give the early life of the baby the chance to start its life with the love of a mother who is not tormented and haunted by intrusions from the past.
Supplementary Material
Acknowledgments
We thank our participants, clinical interviewers, therapists, local researchers, independent physician, and all midwives and obstetrician-gynecologists who aided in making this the OptiMUM-study possible. We also thank librarian/information specialist Bert Berenschot for helping with the literature search.
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary material
The supplemental data for this article can be accessed here.
References
- Alcorn, K. L., O’Donovan, A., Patrick, J. C., Creedy, D., & Devilly, G. J. (2010). A prospective longitudinal study of the prevalence of post-traumatic stress disorder resulting from childbirth events. Psychological Medicine, 40(11), 1849–13. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC. [Google Scholar]
- Ayers, S., Bond, R., Bertullies, S., & Wijma, K. (2016). The aetiology of post-traumatic stress following childbirth: A meta-analysis and theoretical framework. Psychological Medicine, 46(6), 1121–1134. [DOI] [PubMed] [Google Scholar]
- Ayers, S., Wright, D. B., & Ford, E. (2015). Traumatic birth and hyperarousal symptoms: Are they normal or pathological? Journal of Reproductive and Infant Psychology, Issue 33(3), 282–293. [Google Scholar]
- Baas, M. A. M., Stramrood, C. A. I., Dijksman, L. M., de Jongh, A., & van Pampus, M. G. (2017). The optimum-study: EMDR therapy in pregnant women with posttraumatic stress disorder after previous childbirth and pregnant women with fear of childbirth: Design of a multicentre randomized controlled trial. European Journal of Psychotraumatology, 8(1). Advance online publication. doi: 10.1080/20008198.2017.1293315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck, C. T., & Barnes, D. L. (2006). Post-traumatic stress disorder in pregnancy. Annals of the American Psychotherapy Association, 4–9. [Google Scholar]
- Beck, C. T., & Watson, S. (2010). Subsequent childbirth after a previous traumatic birth. Nursing Research, 59(4), 241–249. [DOI] [PubMed] [Google Scholar]
- Boeschoten, M. A., Bakker, A., Jongedijk, R. A., van Minnen, A., Elzinga, B. M., Rademaker, A. R., & Olff, M. (2014). Clinician administered PTSD scale for DSM-5 – Dutch version. (Arq Psychotrauma Expert Groep, Ed.). Diemen. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook, N., Ayers, S., & Horsch, A. (2018). Maternal posttraumatic stress disorder during the perinatal period and child outcomes: A systematic review. Journal of Affective Disorders, 225(225), 18–31. [DOI] [PubMed] [Google Scholar]
- De Jongh, A., Ernst, R., Marques, L., & Hornsveld, H. (2013). The impact of eye movements and tones on disturbing memories involving PTSD and other mental disorders. Journal of Behavior Therapy and Experimental Psychiatry, 44(4), 477–483. [DOI] [PubMed] [Google Scholar]
- Foa, E. B., Cashman, L., Jaycox, L., & Perry, K. (1997). The validation of a self-report measure of posttraumatic stress disorder: The posttraumatic diagnostic scale.. Psychological Assessment, 9(4), 445–451. [Google Scholar]
- Food and Drug Administration (FDA) . (2016). Retrieved March 2, 2020, from http://www.fda.gov/safety/reporting-serious-problems-fda/what-serious-adverse-event.
- Forgash, C., Leeds, A., Stramrood, C. A. I., & Robbins, A. (2013). Case consultation: Traumatized pregnant woman. Journal of EMDR Practice and Research, 7(1), 45–49. [Google Scholar]
- Fuglenes, D., Aas, E., Botten, G., Øian, P., & Kristiansen, I. S. (2011). Why do some pregnant women prefer cesarean? The influence of parity, delivery experiences, and fear. American Journal of Obstetrics and Gynecology, 205(1), 45–49. [DOI] [PubMed] [Google Scholar]
- Graham, A. M., Rasmussen, J. M., Entringer, S., Ben Ward, E., Rudolph, M. D., Gilmore, J. H., … Buss, C. (2019). Maternal cortisol concentrations during pregnancy and sex-specific associations with neonatal amygdala connectivity and emerging internalizing behaviors. Biological Psychiatry, 85(2), 172–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grekin, R., & O’Hara, M. (2014). Prevalence and risk factors of postpartum posttraumatic stress disorder: A meta-analysis. Clinical Psychology Review, 34(4), 389–401. 10.1016/j.cpr.2014.05.003 [DOI] [PubMed] [Google Scholar]
- Haagen, J. F. G., Moerbeek, M., Olde, E., Van Der Hart, O., & Kleber, R. J. (2015). PTSD after childbirth: A predictive ethological model for symptom development. Journal of Affective Disorders, 185, 135–143. [DOI] [PubMed] [Google Scholar]
- Higgins, J. P. T., & Altman, D. G. Eds.. (2008). Chapter 8: Assessing risk of bias in included studies. In Cochrane handbook for systematic reviews of interventions version 5.0.1 (updated September 2008), The Cochrane Collaboration. Retrieved fromwww.cochrane-handbook.org [Google Scholar]
- Kavakci, O., & Yenicesu, G. I. (2014). Eye movement desensitization and reprocessing (EMDR) for hyperemesis gravidarum. The Journal of Psychiatry and Neurological Sciences, 27(4), 335–341. [Google Scholar]
- LeWinn, K. Z., Stroud, L. R., Molnar, B. E., Ware, J. H., Koenen, K. C., & Buka, S. L. (2009). Elevated maternal cortisol levels during pregnancy are associated with reduced childhood IQ. International Journal of Epidemiology, 38(6), 1700–1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logie, R., & de Jongh, A. (2014). The “Flashforward procedure”: Confronting the Catastrophe. Journal of EMDR Practice and Research, 8(1), 25–32. [Google Scholar]
- Madigan, S., Vaillancourt, K., Mckibbon, A., Benoit, D., Madigan, S., Vaillancourt, K., … Benoit, D. (2015). Trauma and traumatic loss in pregnant adolescents: The impact of trauma-focused cognitive behavior therapy on maternal unresolved states of mind and posttraumatic stress disorder. Attachment & Human Development, 17(2), 175–198. [DOI] [PubMed] [Google Scholar]
- Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med, 6(7). doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- NICE . (2018). Post-traumatic stress disorder. Evidence reviews on care pathways for adults, children and young people with PTSD. [PubMed] [Google Scholar]
- Olde, E., van der Hart, O., Kleber, R. J., Van Son, M. J., Wijnen, H. A. A., & Pop, V. J. M. (2005). Peritraumatic dissociation and emotions as predictors of PTSD symptoms following childbirth. Journal of Trauma & Dissociation, 6, 6(3), 125–142. [DOI] [PubMed] [Google Scholar]
- Owen, D., Andrews, M. H., & Matthews, S. G. (2005). Maternal adversity, glucocorticoids and programming of neuroendocrine function and behaviour. Neuroscience and Biobehavioral Reviews, 29(2), 209–226. [DOI] [PubMed] [Google Scholar]
- Rowe, H., Sperlich, M., Cameron, H., & Seng, J. (2014). A quasi-experimental outcomes analysis of a psychoeducation intervention for pregnant women with abuse-related posttraumatic stress. Journal of Obstetric, Gynecologic & Neonatal Nursing, 43(3), 282–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandström, M., Wiberg, B., Wikman, M., Willman, A. K., & Högberg, U. (2008). A pilot study of eye movement desensitisation and reprocessing treatment (EMDR) for post-traumatic stress after childbirth. Midwifery, 24(1), 62–73. [DOI] [PubMed] [Google Scholar]
- Seng, J. S., Li, Y., Yang, J. J., King, A., Kane Low, L. M., Sperlich, M., … Liberzon, I. (2018). Gestational and postnatal cortisol profiles of women with posttraumatic stress disorder and the dissociative subtype. Journal of Obstetric, Gynecologic & Neonatal Nursing, 47(1), 12–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seng, J. S., Oakley, D. J., Sampselle, C., Killion, C., Graham-Bermann, S., & Liberzon, I. (2001). Posttraumatic stress disorder and pregnancy complications. Obstetrics and Gynecology, 97(1), 17–22. [DOI] [PubMed] [Google Scholar]
- Seng, J. S., Sperlich, M., Rowe, H., & Cameron, H. (2011). The survivor moms’ companion: Open pilot of a posttraumatic stress specific psychoeducation program for pregnant survivors of childhood maltreatment and sexual trauma. International Journal of Childbirth, 1(2), 111–121. [Google Scholar]
- Shapiro, F. (2018). Eye movement desensitization and reprocessing (EMDR) therapy: Basic principles, protocols, and procedures (3rd ed.). New York, NY, US: Guilford Press. [Google Scholar]
- Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., … Dunbar, G. (1998). The mini-international neuropsychiatric interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. The Journal of Clinical Psychiatry, 59, 34–57. [PubMed] [Google Scholar]
- Shields, K. E., & Lyerly, A. D. (2013). Exclusion of pregnant women from industry-sponsored clinical trials. Obstetrics and Gynecology, 122(5), 1077–1081. [DOI] [PubMed] [Google Scholar]
- Slater, P. (2015). Post-traumatic stress disorder managed successfully with hypnosis and the rewind technique : Two cases in obstetric patients. International Journal of Obstetric Anesthesia, 24(3), 272–275. [DOI] [PubMed] [Google Scholar]
- Söderquist, J., Wijma, B., & Wijma, K. (2006). The longitudinal course of post-traumatic stress after childbirth. Journal of Psychosomatic Obstetrics and Gynaecology, 27(2), 113–119. [DOI] [PubMed] [Google Scholar]
- Soet, J. E., Brack, G., & DiIorio, C. (2003). Prevalence and predictors of women’s experience of psychological trauma during childbirth. Birth, 30(1), 36–46. [DOI] [PubMed] [Google Scholar]
- Sperlich, M., Seng, J. S., Rowe, H., Cameron, H., Harris, A., McCracken, A., & Bell, S. A. (2011). The survivor moms’ companion; feasibility, safety, and acceptability of a posttraumatic stress specific psychoeducation program for pregnant survivors of childhood maltreatment and sexual trauma. International Journal of Childbirth, 1(2), 122‐135. [Google Scholar]
- Stevens, N. R., Lillis, T. A., Wagner, L., Tirone, V., Hobfoll, S. E., Lillis, T. A., … Hobfoll, S. E. (2019). A feasibility study of trauma-sensitive obstetric care for low-income, ethno-racial minority pregnant abuse survivors. Journal of Psychosomatic Obstetrics & Gynecology, 40(1), 66–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stramrood, C. A. I., Paarlberg, K. M., Huis In’t Veld, E. M. J., Berger, L. W. A. R., Vingerhoets, A. J. J. M., Weijmar Schultz, W. C., & Van Pampus, M. G. (2011). Posttraumatic stress following childbirth in homelike- and hospital settings. Journal of Psychosomatic Obstetrics and Gynaecology, 32(2), 88–97. [DOI] [PubMed] [Google Scholar]
- Stramrood, C. A. I., Van der Velde, J., Doornbos, B., Paarlberg, K. M., Weijmar Schultz, W. C., & Van Pampus, M. G. (2012). The patient observer: Eye-movement desensitization and reprocessing for the treatment of posttraumatic stress following childbirth. Birth, 39(1), 70–76. [DOI] [PubMed] [Google Scholar]
- Twohig, M. P., & Donohue, W. T. O. (2007). Treatment of posttraumatic stress disorder with exposure therapy during late term pregnancy. Clinical Case Studies, 6(6), 525–535. [Google Scholar]
- Weinreb, L., Wenz-gross, M., & Upshur, C. (2018). Postpartum outcomes of a pilot prenatal care-based psychosocial intervention for PTSD during pregnancy. Archives of Women’s Mental Health, 21(3), 299–312. [DOI] [PubMed] [Google Scholar]
- Wijma, K., Wijma, B., & Zar, M. (1998). Psychometric aspects of the W-DEQ; a new questionnaire for the measurement of fear of childbirth. Journal of Psychosomatic Obstetrics & Gynecology, 19(2), 84–97. [DOI] [PubMed] [Google Scholar]
- Yildiz, P. D., Ayers, S., & Phillips, L. (2016). The prevalence of posttraumatic stress disorder in pregnancy and after birth: A systematic review and meta-analysis. Journal of Affective Disorders, 18(2). doi: 10.1016/j.jad.2016.10.009 [DOI] [PubMed] [Google Scholar]
- Zlotnick, C., Capezza, N., & Parker, D. (2011). An interpersonally based intervention for low-income pregnant women with intimate partner violence: A pilot study. Archives of Women’s Mental Health, 14(1), 55–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


