Abstract
Background
Food fortification and biofortification are well-established strategies to address micronutrient deficiencies in vulnerable populations. However, the effectiveness of fortification programs is not only determined by the biological efficacy of the fortified foods but also by effective and sustainable implementation, which requires continual monitoring, quality assurance and control, and corrective measures to ensure high compliance.
Objective
To provide an overview of efficacy, effectiveness, economics of food fortification and biofortification, and status of and challenges faced by large-scale food fortification programs in low- and middle-income countries (LMIC).
Methods
A literature review of PubMed publications in English from 2000 to 2017, as well as gray literature, targeting nongovernmental organizations whose work focuses on this topic, complemented by national reports and a “snowball” process of citation searching. The article describes remaining technical challenges, barriers, and evidence gap and prioritizes recommendations and next steps to further accelerate progress and potential of impact.
Results
The review identifies and highlights essential components of successful programs. It also points out issues that determine poor program performance, including lack of adequate monitoring and enforcement and poor compliance with standards by industry.
Conclusions
In the last 17 years, large-scale food fortification initiatives have been reaching increasingly larger segments of populations in LMIC. Large-scale food fortification and biofortification should be part of other nutrition-specific and nutrition-sensitive efforts to prevent and control micronutrient deficiencies. There are remaining technical and food system challenges, especially in relation to improving coverage and quality of delivery and measuring progress of national programs.
Keywords: large-scale food fortification, biofortification, low- and middle-income countries, economics, compliance
Introduction
Deficiencies of micronutrients (vitamins and minerals/trace elements), and the resulting negative health consequences of such deficiencies, affect over an estimated 2 billion people globally.1 The most common forms of micronutrient deficiencies include iron, iodine, vitamin A, zinc, and folate.1 The most vulnerable populations include reproductive-aged women, young children, and female adolescents, particularly in LMIC.2,3
Micronutrient malnutrition or “hidden hunger” has significant health and economic consequences.4-7 Just in LMIC, micronutrient deficiencies alone have been estimated to cost an annual gross domestic product loss of 2% to 5%8-11 with direct costs estimated between US$20 and US$30 billion every year.10 Anemia, for example, has been estimated to lead to 17% reduced lower productivity in heavy manual labor and an estimated 2.5% loss of earnings due to lower cognitive skills.9
The World Health Organization (WHO) and the United Nations Food and Agriculture Organization (FAO) have identified 4 main strategies for addressing micronutrient malnutrition: nutrition education leading to increased diversity and quality of diets, food fortification and biofortification, supplementation, and disease control measures.12 Each of these strategies has a place in reducing micronutrient malnutrition. For maximum impact, the appropriate mix of these strategies should be in place simultaneously to promote equity in access to interventions and social mechanisms that allow consumption and utilization of an adequate diet for all people in the world.12
Food fortification is a sound public health strategy because it can reach large segments of at-risk populations through existing food delivery systems, without requiring major changes in existing consumption patterns.13 Compared to other interventions, food fortification is likely to be more cost-effective, and if fortified foods are regularly consumed, there is an advantage of maintaining consistent physiological body stores of certain micronutrients used in the fortification.12
Large-scale food fortification programs have been in place in industrialized countries since the early 20th century and have helped to eliminate deficiency diseases in high-income countries, mainly in North America and Europe.4,14 More recently, food fortification has gained traction in LMIC as well, and its health impact in these countries is growing.15 However, the effectiveness of fortification programs is not only determined by the biological efficacy of the fortified food but also by its effective implementation, which includes among others monitoring, quality assurance (QA)/quality control (QC) followed by correction of identified issues, as well as compliance by industry with the fortifications standards.
In 2006, the WHO published guidelines for effective fortification, including the appropriate selection of food vehicles and fortificants, determining fortification concentrations, and implementing effective and sustainable food fortification programs.12 In September 2015, the #Future Fortified Global Summit on Food Fortification was held in Arusha, Tanzania, to discuss the state of the art on achievements and challenges in large-scale food fortification in LMIC. The Arusha Summit aimed to develop a consensus among key global stakeholders around a vision and strategy for scaling up fortification that would, in turn, contribute to the Sustainable Development Goals and beyond.15 The resulting “Arusha Statement on Food Fortification” (http://www.gainhealth.org/wp-content/uploads/2015/05/Arusha-Statement.pdf) summarized commitments to address remaining challenges around monitoring, compliance, and equity. It also outlined 5 critical areas needing to be addressed for immediate progress: (1) modest but new investments by governments and donors to ensure technical support and capacity, compliance, and leveraging coinvestment by the private sector; (2) improving the oversight and enforcement of food fortification standards and legislation; (3) generating more evidence to demonstrate impact and further guide fortification policy and program design; (4) more transparent accountability and global reporting; and (5) continuing advocacy for greater attention to fortification by governments.15
As part of the global response to the Arusha Statement, this article will provide an overview of efficacy, effectiveness, and economics of food fortification and biofortification, as well as an analysis of the overall status of large-scale food fortification programs in LMIC. The article is based on 2 detailed review reports published in the aftermath of the Arusha meeting.16,17 It reviews and identifies essential components of successful programs, points out issues around the frequent lack of adequate compliance, and describes remaining technical challenges, barriers, and evidence gaps. It then uses this information to prioritize recommendations and next steps, with a focus on mass fortification of staples, edible fats and oils, sugar, and condiments (including salt). In addition, it reviews the current evidence base and promise of biofortification efforts in LMIC.
Methods
A literature review of both formal and gray literature was conducted, targeting nongovernmental organizations whose work focuses on this topic, including the Food Fortification Initiative (FFI), the Global Alliance for Improved Nutrition (GAIN), Nutrition International (NI), and the Iodine Global Network (IGN), complemented by national reports. This work was underpinned by a formal literature search, focusing on articles and reports from 2000 to 2017, in English only. Keywords used were “Fortified food*,” “Enriched food*,” “Supplemented food*,” and for Medical Subject Headings (MeSH)-Medline (via OvidSP) “Food, fortified//adverse effects.” Complementary keywords were “Government program*,” “Government sponsored program*,” “Nutritional policy,” “Government health promotion,” “Food fortification program*,” “Policymaker*,” “Health policy*,” “Mandatory program*,” and under MeSH were “Health promotion/og,” “Nutrition policy/,” “Health policy/,” “Mandatory programs/,” “Policy making,” and “Legislation, Food/.” In addition, references were added by a process of forwarding citation searching: for example, identifying relevant references of key articles such as the WHO/FAO 2006 guidelines,12 following them up, and then repeating the process with each article used.
Results
Efficacy of Food Fortification
The efficacy of food fortification has been demonstrated consistently for different micronutrients and different food vehicles.6,12 As a result, it is now well accepted that micronutrient fortification of foods has the potential to significantly increase serum micronutrient concentrations and reduce clinical and physiological manifestations of deficiencies.18,19 A systematic review of randomized and pseudorandomized controlled trials included 60 acceptable trials on iron fortification and iron biofortification and found that iron fortification of foods resulted in a significant increase in hemoglobin (0.42 g/dL, 95% confidence interval [CI]: 0.28-0.56) and serum ferritin (1.36 μg/L; 95% CI: 1.23-1.52), a reduced risk of anemia (risk ratio [RR]: 0.59; 95% CI: 0.48-0.71), and iron deficiency (RR: 0.48; 95% CI: 0.38-0.62); no effect was found on rate of infections, physical growth, or mental and motor development.20 The efficacy of rice fortification with iron has been demonstrated in different settings.21-23 In Mexico, daily consumption of iron-fortified rice 5 d/wk over a 6-month period significantly increased body iron stores and mean plasma ferritin concentration in working women between 18 and 49 years of age and improved hemoglobin concentration of women with anemia, resulting in an overall reduction of the prevalence of anemia of 80%.21 Fortification of wheat flour with folic acid has been widely shown to significantly improve folate status in the population, and its significant effect in reducing the risk of neural tube defects (NTDs) has been repeatedly documented and is now widely accepted.24,25 Efficacy of vitamin A fortification has been documented in the Philippines, where monosodium glutamate,26 margarine,27 and wheat buns are fortified with this vitamin.28 The efficacy of multiple micronutrient fortification has been demonstrated in studies with iron, β-carotene, and iodine-fortified biscuits in South Africa and multiple micronutrient-fortified beverages in Botswana and Tanzania.12
Condiments, spices, and seasonings are increasingly being used as vehicles to increase the intake of vitamins and minerals.29 Mandatory or market-driven condiment fortification with iron has been used with various vehicles such as soy sauce, fish sauce, salt, and bouillon cubes.12 Until now, most of the experience with fortification of condiments and seasonings has been with NaFe-EDTA added to soy and fish sauces in Southeast Asian countries. Other condiments, such as bouillon cubes or curry powders, are now also being fortified with iron and other vitamins and minerals.29 A recent systematic review has demonstrated that iron fortification of condiments is associated with increased hemoglobin, improved iron status, and reduced anemia across targeted populations.30
Efficacy of Biofortification
Evidence for the efficacy of biofortified crops in improving micronutrient status has been documented in different studies, particularly for vitamin A–biofortified crops, as summarized in a review of evidence from Harvest Plus by Bouis and Saltzman.31 The first efficacy data on biofortification came from studies demonstrating that consumption of vitamin A–biofortified orange-fleshed sweet potato increased circulating β-carotene and had a moderate effect on vitamin A status.31 Biofortified provitamin A maize improved total body stores of vitamin A in 5- to 7-year-old children in Zambia and significantly improved visual function in deficient children.32 In Kenya, provitamin A cassava was efficacious in improving vitamin A status of schoolchildren.33 Iron-biofortified beans and pearl millet improved hemoglobin and total body iron stores in Rwanda and Maharashtra, India.31 Biofortification with other micronutrients, such as zinc-biofortified wheat or rice, has shown to be feasible and to offer bioavailable zinc, but as yet there are no efficacy trials.31
Effectiveness of Food Fortification
In high-income countries, food fortification has been largely responsible for the control or elimination of several micronutrient deficiency diseases of public health significance. For instance, marked declines in the prevalence of pellagra from niacin deficiency and beriberi from thiamine deficiency were observed in the Southern United States and Canada, respectively, after voluntary and mandatory fortification of flours and bread with high-vitamin yeast.4,14 In the United States, mandatory large-scale fortification of enriched cereal grain products with folic acid was authorized in 1996 and fully implemented in 1998. Within 5 years, the prevalence of NTDs was dramatically reduced to around 0.66 in 1000 pregnancies or less.34 Fortification of cereal grain products with folic acid became mandatory in several countries soon after and has been consistently effective in reducing the prevalence of NTDs to around 0.5 × 1000 total births in countries where it has been implemented.12,35-37 Mandatory addition of vitamin D to milk, which started in 1965 in Canada, eliminated the widespread problem of childhood rickets.14 Salt iodization, in place since the 1920s in Switzerland and the United States and rapidly expanding in LMIC, has reduced goiter prevalence globally, and universal salt iodization (USI) has prevented an estimated 750 million cases of goiter in the past 25 years.38 After the introduction of vitamin A–fortified margarine in Denmark in 1917, the number of cases of xerophthalmia reported at Copenhagen Hospital fell by more than 90% and had been eliminated by 1918.39,40
Pachon et al41 recently published the first systematic review of evidence of the effect of flour fortification on iron status and anemia in women and children ≤15 years in LMIC. They identified only 13 large-scale flour fortification programs that collected national-level data before fortification and ≥12 months after fortification. Their analysis found that flour fortification was associated with consistent reductions in low ferritin prevalence in one-third of women but not in children. Also, there was statistically significant reduction of anemia in 4 of 12 subgroups of women and 4 of 13 subgroups of children.41 This study recognized several caveats, including lack of use of an adequate program design to evaluate effectiveness, a large heterogeneity in implementation, and lack of adequate use of biological markers to evaluate impact.41,42 The authors also mention the fact that anemia may be due to many other causes different from iron deficiency. As a way to address this last point, Barkley et al43 evaluated if anemia prevalence was reduced in LMIC that fortified wheat flour, alone or in combination with maize flour, with at least iron, folic acid, vitamin A, or vitamin B12, comparing nationally representative data before/after fortification started. In the 12 countries that had fortified, there was a 2.4% reduction in the odds of anemia prevalence, in comparison with no reduction in the odds of anemia prevalence in 20 countries that never fortified flour.43
In several Latin American countries, vitamin A–fortified sugar has been effective in reducing vitamin A deficiencies.44 In Guatemala, where the technology for fortifying sugar with vitamin A was developed, an evaluation of the fortification program carried out showed that after 12 months of implementation, low retinol levels had decreased to 5% and prevalence of human milk samples with less than 20-μg retinol/dL was reduced by 50%.45,46 A recent systematic evaluation of 76 studies and 41 contextual reports15 concluded that there is strong evidence of important and measurable improvements after food fortification in micronutrient status and health outcomes in women and children in wide geographic settings in LMIC.15 Fortifying with vitamin A was estimated to reduce the prevalence of deficiency in children less than 5 years from 33.3% to 25.7% globally; effectively fortifying with iron would reduce anemia by 14%; salt iodization has reduced goiter by 40% in countries such as Pakistan; and fortifying flour with folic acid has reduced NTDs by 40% to 50%.15
In spite of the efficacy of rice as a suitable food to be fortified, there is still only limited evidence for its effectiveness.23 Japan has fortified grains to add to rice before being cooked since decades ago (on the market since 1981).47 In Costa Rica, mandatory rice fortification with folic acid, vitamin B1 (thiamine), vitamin B3 (niacin), vitamin B12 (cobalamin), vitamin E, selenium, and zinc has been in place since 2001. Rice differs from other fortified food staples, such as maize or wheat, in that the grain needs to be fortified directly rather than the subproducts (eg, flour or porridge).48,49 The reduction of NTDs in Costa Rica is attributed to its experiences with food fortification in general, its centralized rice industry, government leadership, and private sector support.50 Detailed rice fortification guidelines are in development,51,52 and currently, a Cochrane systematic review of the fortification of rice with vitamins and minerals for addressing micronutrient malnutrition is underway.53
Effectiveness of Biofortification
The primary evidence for the effectiveness of biofortification comes from provitamin A–rich orange-fleshed sweet potato in large randomized controlled trials, reaching 24 000 households in Uganda and Mozambique from 2006 to 2009.54-56 Introduction of orange-fleshed sweet potato in rural Uganda resulted in increased vitamin A intakes among children and women and improved vitamin A status among children. Women who got more vitamin A from the crop also had a lower likelihood of having marginal vitamin A deficiency.55 In addition, recent research on the health benefits of biofortified orange-fleshed sweet potato in Mozambique showed that biofortification can improve child health; consumption of biofortified orange sweet potato reduced the prevalence and duration of diarrhea in children younger than 5 years.57
Economics of Food Fortification
Assessing monetary benefits across a range of countries is challenging mainly because these benefits are driven by savings in access to health care and costs of providing health care. Other costs related to the intervention may include factors such as transport. In spite of these caveats, food fortification has been recognized as one of the most cost-effective (note 1) interventions to address nutrient deficiencies in public health; for instance, top economists gathered at the Copenhagen Consensus consistenly ranked food fortification as one of the top 4 priority development interventions.58 Depending on the setting and micronutrient, cost-effectiveness of fortification has been estimated between $22 per disability-adjusted life year (DALY) saved for iron fortification in East Africa to $140 per DALY saved for iron fortification in Latin America,9 while the cost-effectiveness of fortifying staple foods with vitamin A may be as high as US$81 per DALY.
The cost–benefit (note 2) ratio of fortification depends on various other factors, such as deficiency trends, resources, food vehicle, and fortificants used. Because these costs are higher in high–middle income and high-income countries, the cost–benefit ratio of fortification tends to be higher in these countries. Therefore, the cost– benefit and cost-effectiveness will vary depending on the food vehicle and micronutrient being reviewed. Nevertheless, after a thorough review of costs and benefits, the Copenhagen Consensus proposed micronutrient fortification, particularly iron fortification of staples and salt iodization, as one of the “best-buys” among the 30 interventions they considered for addressing the 10 great challenges facing global development.6
Keeping in mind the previously mentioned caveat related to different health benefits due to differences in the severity and spread of a given micronutrient deficiency, in a review presented at the #Future Fortified summit, Horton et al estimated that the median benefit–cost ratio (note 3) of iron fortification in 10 countries with high levels of anemia is 8.7:1.15 Iodization of salt had a benefit–cost ratio of around 30:1, while for folic acid, the range extended from 11.8:1 in Chile to 30:1 in South Africa.15 For an annual cost of $286 million, the Copenhagen Consensus estimated the corresponding benefits would be $2.7bn (a benefit–cost ratio of 9.5:1).5
Economics of Biofortification
For biofortification, the cost-effectiveness will be dependent on the crop, micronutrient, and delivery country.31 Cost-effectiveness data are currently available for orange-fleshed sweet potato in Uganda, where biofortification was demonstrated to cost US$15 to US$20 per DALY saved, which the World Bank considers highly cost-effective.31,59
Results of cost-effectiveness studies have shown that for each of the country–crop–micronutrient combinations considered, biofortification is a cost-effective intervention based on cost per DALY saved, using World Bank standards.60 The Copenhagen Consensus concluded that for every dollar invested in biofortification, as much as US$17 of benefits may be gained.5
Overview of Large-Scale Food Fortification Programs
Large-scale food fortification refers to the production capacity (more than 50 metric tons/d), often a prerequisite for mass fortification, which refers to the reach of a fortified product. The process involves the addition at central level or point of production of 1 or more micronutrients to foods commonly consumed by the general population, such as grains, salt and condiments, sugar, or edible oil, and is usually mandated and regulated by the government sector, in response to evidence of micronutrient deficiencies or where a population, or subpopulation, may benefit. These efforts are concentrated on the organized food processing sector among large- and medium-sized industries.
Many food vehicles have been mandated for fortification with programs that have gone to scale. For example, by the end of 2017, over 140 countries implemented national USI programs, more than 90 nations had mandatory fortification programs for at least 1 kind of cereal grain (wheat, maize, or rice), and over 50 mandated the fortification of edible oils, margarine, or ghee. Sugar is fortified in a smaller number of countries. Progress on a range of indicators for large-scale food fortification programs of salt, staples, and edible oils is regularly monitored and updated by a recently launched online tool (http://fortificationdata.org/#data).61
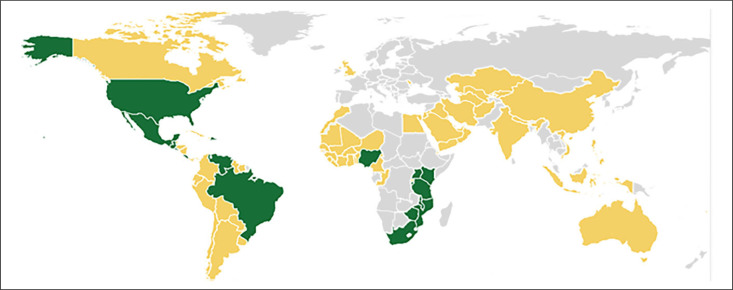
In 2017, there were 75 countries (plus the Indian Punjab province) with mandatory legislation to fortify wheat flour, 16 countries to fortify both wheat and maize flour, and 1 country (Rwanda) to fortify only maize flour, specifically with iron and folic acid (see Figure 1). In addition, 5 countries (Democratic Republic of Congo, Gambia, Namibia, Qatar, and United Arab Emirates) fortify at least half their industrially milled wheat flour with iron and/or folic acid through voluntary efforts.61 Although it is estimated that 48% of industrially milled maize flour is currently fortified,61 one of the main challenges to reach large segments of the population with a fortified product is that many consumers, particularly in Africa, largely consume locally produced, unprocessed (and hence unfortified) maize meal or wheat flour milled at the village level or in small-scale hammer mills.62 Consequently, the number of small mills without fortification technology in a country will affect whether the fortification of maize or wheat flour is a feasible option for that particular country.62
Figure 1. Countries with mandatory or voluntary cereal grain fortification in 2017.61 Yellow countries have mandatory legislation for wheat flour; green countries have mandatory or voluntary fortification of wheat and maize flour.
Of the 222 million metric tons of rice that are industrially milled each year, less than 1% are fortified with essential vitamins and minerals. Currently, 8 countries (Costa Rica, Nicaragua, Panama, Venezuela, India, Papua New Guinea, the Philippines, and the United States) have mandatory rice fortification,61 and Brazil, Colombia, and the Dominican Republic have large-scale nonmandatory rice fortification programs.23
The USI is the preferred strategy for the control of iodine deficiency disorders in most countries.63 Salt has been the vehicle of choice for fortification as it is consumed by nearly everyone at roughly equal amounts throughout the year and is relatively cheap/inexpensive (less than US$0.02-US$0.10 per person per year). For salt iodization, there is global information on legislation, coverage, and status (at least in children), in contrast to other food fortification programs, for which most of the information is limited to the legislation and coverage from a few countries. Salt production is often limited to a few centers, which facilitates QC, and the addition of potassium iodate or potassium iodide does not affect the taste or smell of the salt.64 Iodine deficiency has been considerably reduced due to iodization of salt and is now recognized as one of the great public health nutrition achievements.64,65
The world has moved from 110 countries iodine deficient in 1993 to now only 19 deficient countries.38 Nevertheless, although there is recognition of the importance of iodization of salt, some 30% of LMIC households are still not consuming iodized salt in households, with especially low coverage in some European and Central European countries, in South Asia, and some Sub-Sahara African countries.65
Following national-level documentation of widespread vitamin A deficiency in large sectors of the population, carried out in 1965 to 1966, sugar was legislated for fortification with vitamin A in Guatemala, Honduras, and El Salvador early in the 1970s. Sugar was chosen as the most appropriate food vehicle because of its high and stable daily consumption by the population at large, including vulnerable target groups, and its industrialized, centralized processing that facilitated adding the vitamin at minimal cost and under close supervision. Public–private partnerships were established to work toward the establishment of national programs, supported by a careful advocacy and promotion campaign. Mandatory fortification legislation was decreed in each of the countries for both domestic and industrial use. Evaluations from each of the countries showed that these programs had great success in improving vitamin A intake.66
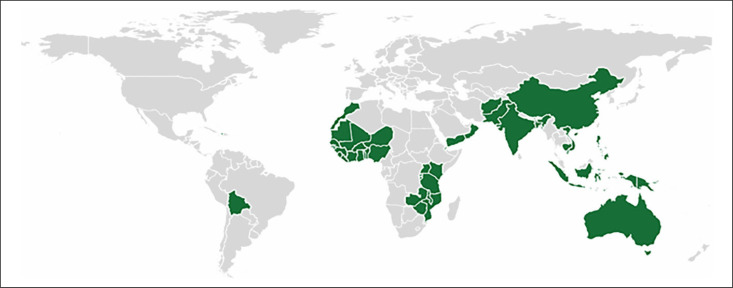
Edible oils are consumed by almost everyone, usually, at uniform rates in particular regions (10-20 g/d in African countries and up to 70-90 g/capita/d in Asia),40 which makes them an attractive vehicle for fortification. Fortification programs for vitamin A in edible oils are currently in place in 50 countries worldwide (see Figure 2).61 Of these 50, well over half have mandatory fortification of margarine and/or oils, whereas 8 programs are described as “industry led” (or voluntary), 1 in which it is permitted and 7 where it was not specified.40 Importantly, around half of those with mandatory fortification are in LMIC.
Figure 2. Low–middle–high income countries with mandatory or voluntary oil fortification in 2017.61 Green countries have mandatory or voluntary oil fortification.
Components of Successful Food Fortification Programs
A recent review on the coverage and utilization of food fortification programs in 8 countries (Bangladesh, Cote d’Ivoire, India [Rajasthan], Nigeria, Senegal, South-Africa, Tanzania, and Uganda) identified some successful fortification programs, whereby the majority of the food vehicle used was fortifiable and fortified, and coverage was equitable in reaching the entire population.67 Programs in some other countries were identified with potential for effective fortification, largely based on very high use of a fortifiable food vehicle (note 4) by the entire population, but that potential was not currently being reached because of low compliance with fortification requirements.68 Four key lessons for successful programs were learned: (1) the potential for impact will depend on the appropriate choice of food fortification vehicle and on the proportion of the food vehicle consumed that is fortifiable; (2) the design of fortification programs should be informed by the magnitude and distribution of inadequate intake and deficiency and consumption of fortifiable foods, in addition, food fortification programs should be part of national micronutrient deficiency control strategies to ensure coordination with other programs; (3) effective QC of fortification levels in foods needs strengthening of capacity and resources, as well as governance and policy commitment; and (4) to ensure safe and impactful programs, periodic reviews of the assumptions related to dietary patterns that underpin food fortification are needed.67
In a similar review on successful staple food fortification programs in Latin America, institutional research capacity and champions of fortification, as well as private/public partnerships, were considered key features of successful and sustainable programs.66,69
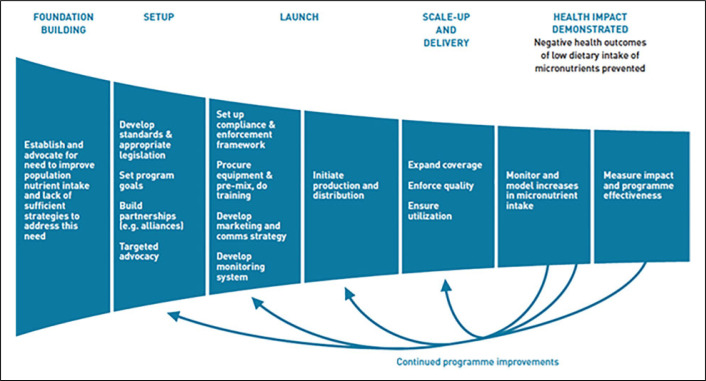
Successful programs are built on multisectoral foundations that include government, private sector, international organizations, civil society, and academia and which have worked together to generate evidence identifying the need, setting standards, ensuring legislation and alignment with national nutrition policies, ensuring QA and control throughout the manufacturing processes, and establishing strong monitoring and evaluation to ensure compliance and impact (see Figure 3).17,66,70
Figure 3. Impact model for staple food fortification.17.
Fortification can be either mandatory or voluntary, and in both cases, appropriate standards—as set by WHO—are required to ensure impact and safety.12 For mandatory fortification to work, consistent and effective monitoring to ensure both QA and QC during product manufacturing and distribution, as well as consumption by the target population, are necessary.70 Procedures on good manufacturing practice are available through ISO and are described in the WHO/FAO guidelines.12 In addition, monitoring and evaluation to assess the degree to which the fortified food is actually reaching households and individuals need to be in place in order to address issues of potential for impact and utilization across different population subgroups. It is also critical for providing program planners and policymakers with the necessary information to make decisions about course correction, scaling up, or even ending of a program.70
Poor Program Performance and Monitoring of Fortification Programs
A review of external QA activities in GAIN-supported staple food fortification programs in 25 countries found that the percentage of foods meeting national standards ranged from 18% to 97%, with an average around 45% to 50%.71 Many nonfortified foods were found to be labeled as fortified, further misleading consumers on vitamin and mineral content and contributing to a reduced health impact of fortification programs as a result of foods not appropriately fortified.72 It must be noted that classifying single samples as in or out of range may overestimate the level of noncompliance of fortification programs because the minimum content is highly variable depending on a range of factors. Nonetheless, 5 underlying issues were described that are leading to poor program performance and possibly poor compliance in these 25 country programs.73
Food laws and regulations related to monitoring, inspection, and enforcement of food fortification are often fragmented and not appropriately embedded within legal frameworks, leading to a lack of—or weak—enforcement.
Food fortification is not prioritized in food safety and QC practice and culture, especially where resources are limited. Over 80% of government respondents noted that their current funding was not sustainable over the next 5 years.
There is a perceived or real political risk in enforcing compliance with regulations. Even where resources and capacity exist, over 60% of respondents thought that regulatory agencies are often unwilling to enforce regulations due to perceived or actual resistance from interest groups.
The additional costs to industry to fortify may lead to some industries lacking appropriate internal budget and expertise to fortify appropriately while others purposely underfortify.
Regulatory monitoring agencies and consumer protection groups often do not actively protect consumers from underfortified or nonfortified foods, or fraudulent labeling, thereby misleading consumers who should be able to trust what is stated on packages in relation to vitamin and mineral content.
Given the possibility of over consumption of nutrients in groups outside the target population, identifying additional intakes and nutritional status associated with the consumption of fortified foods should be actively and consistently monitored as an integral part of any fortification program.44,71 In China, careful monitoring has identified counties where much of the population is likely getting too much iodine from the local water source as judged by urinary iodine levels, and in these areas, iodine is being reduced in the iodized salt distributed.74 Similarly, in Ireland, mandatory folic acid fortification of bread was reconsidered in 2008 because of concerns of excessive intakes due to the high intakes of voluntarily fortified foods.75 Using modeling techniques for fortificants, 1 study concluded that the adoption of fortification content for staple foods near the safe limit also brings into consideration the need for restricting the voluntary addition of the specific nutrient to other foods and to dietary supplements,76 especially where the risk of deficiency is not universal.77
Many national programs are currently not achieving national targets, especially in iodine “because of weak regulatory/monitoring systems” (Yusafali, MSc, personal communication, 2015). Setting up effective monitoring systems and tools for assessing QC and compliance, as well as setting up rigorous impact evaluations, requires a thorough understanding of the different pathways leading to effective coverage and impact. Insufficient budgets are often identified as constraining adequate QC and compliance.72
Challenges of Large-Scale Food Fortification
Although long experience and numerous studies and reports attest to fortification’s effectiveness and feasibility,12,78,79 the following challenges do remain.
Evidence gaps. Evidence gaps remain in assessing the potential for impact on public health outcomes and how to effectively measure these. Program impact evaluations should be guided by impact pathways, prioritizing impact assessment in programs with an appropriate design and implementation to substantially increase the quality of evidence.80 Although the effectiveness of food fortification on nutrient intakes and nutrient status is largely established, there is still insufficient evidence of effectiveness on functional outcomes, including growth, cognitive development, morbidity, and mortality, especially in LMIC.18,81 This is especially an issue, as much emphasis is currently being placed on the prevention of stunting. The translation of evidence into realistic target settings for policies and programs is often lacking. In addition, changes in dietary habits over time may results in challenges, as in the case of decreasing consumption of iodized table salt in Europe,82 as well as opportunities, such as in the case of fortified breakfast cereals now being the dominant source of iron in UK schoolchildren.19
In a recent WHO/FAO Technical Consultation on scaling up rice fortification in Asia,83 the following research gaps on technical issues were identified: (1) assessing the stability of different micronutrients in different context-specific environments; (2) studying the nutrient–nutrient interactions, in particular related to relative bioavailability and phytate effect on iron absorption; and (3) evaluating the optimal delivery platforms for reaching the (hard to reach) target populations.
Finally, although mandated programs usually cover only registered producers, small-scale mills remain the predominant source of (iron-fortified) wheat and maize flours in many rural subsistence farming areas, while small-holding salt production units require small batch iodization. In 2015, United Nations Children’s Fund, GAIN, IGN, and NI completed a review of country experiences in small-scale salt fortification, with a smaller focus on wheat and maize fortification. The study identified number of evidence gaps and challenges for this type of food fortification, including clarity on small-scale contribution to supply; possibility of industry consolidation or quasi-consolidation in the form of cooperatives; understanding social impact; identifying incentives, models of cooperation, business plan development, and appropriate inputs for external support; establishing minimum criteria for quality; and understanding market forces and competition.17
Ensuring effective coverage. Effective coverage is defined as the proportion of the population who utilize an intervention as per intended to achieve a biological/health impact.84 For food fortification, this could be interpreted as the proportion of the population consuming adequately fortified food.85 Effective coverage is a precondition for impactful programs, along with other factors as described in this article. Challenges in reaching impact have been described from the very early days of large-scale fortification programs in the United States, and such challenges, including the choice of appropriate fortification vehicles, the use of a bioavailable fortificant, not reaching populations most likely to benefit, avoiding over consumption in nontargeted groups, and adequate monitoring of nutritional status, currently still exist in all countries.44 To support assessments of effective coverage in both population-based and targeted fortification programs, GAIN developed a Fortification Assessment Coverage Toolkit (FACT). An 8-country series of FACT coverage surveys were completed between 2013 and 2015 and assessed coverage (including equity aspects) of 18 identified large-scale fortification programs. Coverage varied widely by food vehicle and country, and the 2 main program bottlenecks were a poor choice of vehicle and failure to properly fortify a fortifiable vehicle (ie, the absence of adequate fortification).68
Accessibility and equity. One of the criticisms of mass fortification is that it may not be accessible to those most in need. Commercially fortified products may not be affordable for the poorest segments of societies, partly because in some countries import duties and taxes on premixes or fortification equipment drive prices up. Inequity in access to fortified foods needs to be locally researched and contextually understood, as reasons for lack of accessibility will differ within countries and within households. Programs often lack such particular understanding and do not assess intra-household food distribution practices, which are often disadvantaging women and young children within households.86,87 To effectively reach populations most in need, opportunities to link with, for example, social protection programs, need to be explored and better utilized.
Conclusions and Recommendations
Food fortification is one of several evidence-based interventions that improve the overall quality of the diet, working through existing delivery systems. In addition, in recent years, biofortification has been shown as a promising, feasible, and cost-effective means of delivering micronutrients to populations who may have limited access to diverse diets and other micronutrient interventions, and efforts are underway to scale up its use to further improve global nutrition.31 It is important to acknowledge that, although food fortification programs are highly efficient and cost-effective, to ensure sustained impact they require continued interest and investment by governments for monitoring of delivery. In addition, investments by donors for both existing and new programs can further improve fortification’s footprint and impact. Large-scale food fortification and biofortification should be integrated into nutrition-specific and nutrition-sensitive efforts to prevent and control micronutrient deficiencies. In the past 2 decades, large-scale food fortification programs have been reaching increasingly large segments of populations in LMIC, paired with an acceleration of knowledge and guidance on large-scale fortification. Yet, a number of technical and food system challenges remain, especially in relation to improving coverage and quality of delivery and to measuring the progress of national programs. Tackling these issues in a concerted manner, as articulated in the 2015 Arusha Statement on Food Fortification,15 can help to further accelerate progress and potential of impact.
Authors’ Note
SJMO conceptualized the manuscript with IDH, LMN, HM, and GG and wrote the first draft of the manuscript. IDH performed the literature review, and IDH, LMN, MV, SJMO, and HM authored the review report entitled “Large-scale food fortification: an overview of trends and challenges in Low and Middle-Income Countries in 2017” which was the basis for this manuscript. All authors provided substantial technical and editorial input in the draft versions, and reviewed and approved the final manuscript.
Acknowledgments
The authors would like to acknowledge the contribution of Rafael Flores-Ayala to help scope this paper as well as his comments to an earlier version.
Notes
The denominator in this ratio is gain in health (expressed, for example, as years of life saved, disability-adjusted life years [DALYs], or micronutrient status and its links to morbidity/mortality outcomes) and the numerator is the cost associated with the health gain.
An indicator that summarizes the value for money of a proposal; both costs and benefits are expressed in monetary terms.
The inverse of cost–benefit.
According to World Health Organization and the United Nations Food and Agriculture Organization guidelines (2006), a food vehicle suitable for fortification refers to a food that is widely consumed in relatively constant quantities by the target population, available all year round, of relatively low cost, centrally processed, and with no interactions between the fortificant and the carrier food.12
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Homero Martinez http://orcid.org/0000-0002-1435-0306
References
- 1.Muthayya S, Rah JH, Sugimoto JD, Roos FF, Kraemer K, Black RE.. The global hidden hunger indices and maps: an advocacy tool for action. PLoS One. 2013;8(6):e67860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang Z, Huffman SL.. Review of fortified food and beverage products for pregnant and lactating women and their impact on nutritional status. Matern Child Nutr. 2011(7 suppl 3):19-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thurnham DI. Nutrition of adolescent girls in low-and middle-income countries. Sight Life Mag. 2013;27(3):26-37. [Google Scholar]
- 4.Fletcher RJ, Bell IP, Lambert JP.. Public health aspects of food fortification: a question of balance. Proc Nutr Soc. 2004;63(4):605-614. [DOI] [PubMed] [Google Scholar]
- 5.Horton S, Alderman H, Rivera J.. Copenhagen Consensus 2008 Challenge Paper: Hunger and Malnutrition, Draft. Denmark: Copenhagen Consensus Center; 2008. [Google Scholar]
- 6.Bhutta ZA, Das JK, Rizvi A, et al. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? Lancet. 2013;382(9890):452-477. [DOI] [PubMed] [Google Scholar]
- 7.Black RE, Victora CG, Walker SP, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382(9890):427-451. [DOI] [PubMed] [Google Scholar]
- 8.Stein AJ, Qaim M.. The human and economic cost of hidden hunger. Food Nutr Bull. 2007;28(2): 125-134. [DOI] [PubMed] [Google Scholar]
- 9.Horton S. The economics of food fortification. J Nutr. 2006;136(4):1068-1071. [DOI] [PubMed] [Google Scholar]
- 10.Horton S. Options for investment in nutrition in low-income Asia. Asian Dev Rev. 1999;17(1-2): 246-273. [Google Scholar]
- 11.The World Bank Enriching Lives: Overcoming Vitamin and Mineral Malnutrition in Developing Countries. Development in Practice Series Washington, DC: World Bank; 1994. [Google Scholar]
- 12.WHO/FAO Guidelines on Food Fortification with Micronutrients. Geneva, Switzerland: World Health Organization/Food and Agriculture Organization of the United Nations; 2006. [Google Scholar]
- 13.Spohrer R, Larson M, Maurin C, Laillou A, Capanzana M, Garrett GS.. The growing importance of staple foods and condiments used as ingredients in the food industry and implications for large-scale food fortification programs in Southeast Asia. Food Nutr Bull. 2013;34(suppl 2):S50-S61. [DOI] [PubMed] [Google Scholar]
- 14.Canadian Public Health Association (CPHA) Food fortification with vitamins and minerals. 2015. https://www.cpha.ca/food-fortification-vitamins-and-minerals. Accessed April 30, 2018.
- 15.Sight and Life The #Future fortified global summit on food fortification-events proceedings and recommendations for food fortification programs. 2016. http://www.gainhealth.org/wp-content/uploads/2016/07/FutureFortifiedSupplement-6July-2016.pdf. Accessed April 30, 2018.
- 16.Darnton-Hill A, Neufeld LM, Vossenaar M, Osendarp S, Martinez H.. Large-scale food fortification: an overview of trends and challenges in low- and middle-income countries in 2017. Micronutrient Forum. 2017. [DOI] [PMC free article] [PubMed]
- 17.Hoogendoorn A, Luthringer C, Parvanta I, Garrett G. Food Fortification Global Mapping Study 2016 . Technical Assistance for Strengthening Capacities in Food Fortification. European Commission; 2017. https://ec.europa.eu/europeaid/sites/devco/files/global-mapping-_study-2016.pdf. Accessed April 30, 2018. [Google Scholar]
- 18.Das JK, Salam RA, Kumar R, Bhutta ZA.. Micronutrient fortification of food and its impact on woman and child health: a systematic review. Syst Rev. 2013;2:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hennessy A, Walton J, Flynn A.. The impact of voluntary food fortification on micronutrient intakes and status in European countries: a review. Proc Nutr Soc. 2013;72(4):433-440. [DOI] [PubMed] [Google Scholar]
- 20.Gera T, Sachdev HS, Boy E.. Effect of iron-fortified foods on hematologic and biological outcomes: systematic review of randomized controlled trials. Am J Clin Nutr. 2012;96(2):309-324. [DOI] [PubMed] [Google Scholar]
- 21.Hotz C, Porcayo M, Onofre G, et al. Efficacy of iron-fortified ultra rice in improving the iron status of women in Mexico. Food Nutr Bull. 2008;29(2): 140-149. [DOI] [PubMed] [Google Scholar]
- 22.Angeles-Agdeppa I, Capanzana MV, Barba CV, Florentino RF, Takanashi K.. Efficacy of iron-fortified rice in reducing anemia among schoolchildren in the Philippines. Int J Vitam Nutr Res. 2008;78(2):74-86. [DOI] [PubMed] [Google Scholar]
- 23.Muthayya S, Hall J, Bagriansky J, et al. Rice fortification: an emerging opportunity to contribute to the elimination of vitamin and mineral deficiency worldwide. Food Nutr Bull. 2012;33(4):296-307. [DOI] [PubMed] [Google Scholar]
- 24.Abdollahi A, Elmadfa I, Djazayery A, Golalipour MH, Sadighi J, Sadeghian Sharif S.. Efficacy of flour fortification with folic acid in women of childbearing age in Iran. Ann Nutr Metab. 2011; 58(3):188-196. [DOI] [PubMed] [Google Scholar]
- 25.MRC Vitamin Study Research Group Prevention of neural tube defects: results of the medical research council vitamin study. Lancet. 1991; 338(8760):131-137. [PubMed] [Google Scholar]
- 26.Muhilal A, Murdiana A, Azis I, Saidin S, Jahari AB, Karyadi D.. Vitamin A-fortified monosodium glutamate and vitamin A status: a controlled field trial. Am J Clin Nutr. 1988;48(5):1265-1270. [DOI] [PubMed] [Google Scholar]
- 27.Solon FS, Solon MS, Mehansho H, et al. Evaluation of the effect of vitamin A-fortified margarine on the vitamin A status of preschool Filipino children. Eur J Clin Nutr. 1996;50(11):720-723. [PubMed] [Google Scholar]
- 28.Solon FS, Klemm RD, Sanchez L, et al. Efficacy of a vitamin A-fortified wheat–flour bun on the vitamin A status of Filipino school children. Am J Clin Nutr. 2000;72(3):738-744. [DOI] [PubMed] [Google Scholar]
- 29.Garcia-Casal MN, Pena-Rosas JP, McLean M, De-Regil LM, Zamora G; Consultation Working Groups. Fortification of condiments with micronutrients in public health: from proof of concept to scaling up. Ann N Y Acad Sci. 2016;1379(1):38-47. [DOI] [PubMed] [Google Scholar]
- 30.Self JL, Serdula M, Dowswel lT, De-Regil LM.. Fortification of condiments and seasonings with iron for preventing anaemia and improving health. Cochrane Database Syst Rev. 2012;(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bouis HE, Saltzman A.. Improving nutrition through biofortification: a review of evidence from harvest plus, 2003 through 2016. Glob Food Sec. 2017;12:49-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gannon B, Kaliwile C, Arscott SA, et al. Biofortified orange maize is as efficacious as a vitamin A supplement in zambian children even in the presence of high liver reserves of vitamin A: a community-based, randomized placebo-controlled trial. Am J Clin Nutr. 2014;100(6): 1541-1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Talsma EF, Brouwer ID, Verhoef H, et al. Biofortified yellow cassava and vitamin A status of Kenyan children: a randomized controlled trial. Am J Clin Nutr. 2016;103(1):258-267. [DOI] [PubMed] [Google Scholar]
- 34.Honein MA, Paulozzi LJ, Mathews TJ, Erickson JD, Wong LY.. Impact of folic acid fortification of the US food supply on the occurrence of neural tube defects. JAMA. 2001;285(23):2981-2986. [DOI] [PubMed] [Google Scholar]
- 35.Berry RJ, Bailey L, Mulinare J, Bower C.. Fortification of flour with folic acid. Food Nutr Bull. 2010;31(suppl 1):S22-S35. [DOI] [PubMed] [Google Scholar]
- 36.Caudill MA, Cruz AC, Gregory JF 3rd, Hutson AD, Bailey LB.. Folate status response to controlled folate intake in pregnant women. J Nutr. 1997;127(12):2363-2370. [DOI] [PubMed] [Google Scholar]
- 37.Crider KS, Devine O, Hao L, et al. Population red blood cell folate concentrations for prevention of neural tube defects: Bayesian model. BMJ. 2014; 349:g4554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Iodine Global Network (IGN) Global scorecard of iodine nutrition in 2017. 2017. http://www.ign.org/cm_data/IGN_Global_Scorecard_AllPop_and_PW_May2017.pdf. Accessed April 30, 2018.
- 39.Bloch CE. Klinische untersuchungen über dystrophie und xerophthalmie bei jungen Kindern. Jahrb kinderheilk phys erziehung [In German]. 1919;89: 405-441. [Google Scholar]
- 40.Diosady LL, Mannar MGV.. Vitamin A fortification of cooking oils In: Preedy VR, Srirajaskanthan R, Patel VB, eds. Handbook of Food Fortification and Health from Concepts to Public Health Applications Vol 2 New York, NY: Springer and Humana Press; 2013:275-290. [Google Scholar]
- 41.Pachon H, Spohrer R, Mei Z, Serdula MK.. Evidence of the effectiveness of flour fortification programs on iron status and anemia: a systematic review. Nutr Rev. 2015;73(11):780-795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dewey KG. The challenge of meeting nutrient needs of infants and young children during the period of complementary feeding: an evolutionary perspective. J Nutr. 2013;143(12):2050-2054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Barkley JS, Wheeler KS, Pachon H.. Anaemia prevalence may be reduced among countries that fortify flour. Br J Nutr. 2015;114(2):1-9. [DOI] [PubMed] [Google Scholar]
- 44.Dwyer JT, Wiemer KL, Dary O, et al. Fortification and health: challenges and opportunities. Adv Nutr. 2015;6(1):124-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pineda O. Fortification of sugar with vitamin A. Food Nutr Bull. 1988;19(2):131-136. [Google Scholar]
- 46.Arroyave G, Aguilar JR, Flores M, Guzman MA.. Evaluation of Sugar Fortification with Vitamin A at the National Level. Washington, DC: Pan American Health Organization; 1979. [Google Scholar]
- 47.Zimmermann MB, Muthayya S, Moretti D, Kur-pad A, Hurrell RF.. Iron fortification reduces blood lead levels in children in Bangalore, India. Pediatrics. 2006;117(6):2014-2021. [DOI] [PubMed] [Google Scholar]
- 48.De-Regil LM, Pena-Rosas JP, Laillou A, Moench-Pfanner R.. Considerations for rice fortification in public health: conclusions of a technical consultation. Ann N Y Acad Sci. 2014;1324:1-6. [DOI] [PubMed] [Google Scholar]
- 49.Steiger G, Muller-Fischer N, Cori H, Conde-Petit B.. Fortification of rice: technologies and nutrients. Ann N Y Acad Sci. 2014;1324:29-39. [DOI] [PubMed] [Google Scholar]
- 50.Tacsan L, Fabrizio C, Smit J.. Rice fortification in Costa Rica In: Codling K, Fabrizio C, Ghoos K, Rosenzweig J, Smit J, Yusufali R, eds. Scaling Up Rice Fortification in Asia. Basel, Switzerland: Sight & Life/WFP; 2015:73-78. [Google Scholar]
- 51.de Pee S. Proposing nutrients and nutrient levels for rice fortification. Ann N Y Acad Sci. 2014; 1324:55-66. [DOI] [PubMed] [Google Scholar]
- 52.Sight and Life, WFP Scaling Up Rice Fortification in Asia. 2015. https://sightandlife.org/wp-content/uploads/2017/02/SAL_WFP_Suppl.pdf. Accessed April 30, 2018.
- 53.Ashong J, Muthayya S, De-Regil LM, et al. Fortification of rice with vitamins and minerals for improved maternal and child nutrition and health outcomes (Protocol). Cochrane Database Syst Rev. 2012;(6): CD009902. [Google Scholar]
- 54.Hotz C, Loechl C, Lubowa A, et al. Introduction of beta-carotene-rich orange sweet potato in rural Uganda resulted in increased vitamin A intakes among children and women and improved vitamin A status among children. J Nutr. 2012;142(10): 1871-1880. [DOI] [PubMed] [Google Scholar]
- 55.Hotz C, Loechl C, de Brauw A, et al. A large-scale intervention to introduce orange sweet potato in rural Mozambique increases vitamin A intakes among children and women. Br J Nutr. 2012; 108(1):163-176. [DOI] [PubMed] [Google Scholar]
- 56.Low JW. Biofortifed crops with a visible trait: the example of orange-fleshed sweet potato in Sub-Saharan Africa In: Preedy VR, Srirajaskanthan R, Patel VB, eds. Handbook of Food Fortification and Health from Concepts to Public Health Applications Vol 2 New York, NY: Springer and Humana Press; 2013:371-384. [Google Scholar]
- 57.Jones KM, deBrauw A.. Using agriculture to improve child health: promoting orange sweet potatoes reduces diarrhea. World Development. 2015;74:15-24. [Google Scholar]
- 58.Horton S, Alderman H, Rivera J.. Copenhagen Consensus 2008. Tewksbury, MA: Copenhagen Consensus Center; 2008. [Google Scholar]
- 59.The World Bank World Development Indicators: Nutrition intake and supplements. 2015. [cited August 11, 2015]. http://wdi.worldbank.org/table/2.16. Accessed April 30, 2018.
- 60.Meenakshi JV, Johnson NL, Manyong VM, et al. How cost-effective is biofortification in combating micronutrient malnutrition? An ex ante assessment. World Development. 2010;38(1):64-75. [Google Scholar]
- 61.Global Fortification Data Exchange Count of food vehicles with standards. 2017. http://fortificationdata.org/map-number-of-food-vehicles/. Accessed April 30, 2018.
- 62.Pena-Rosas JP, Garcia-Casal MN, Pachon H, McLean MS, Arabi M.. Technical considerations for maize flour and corn meal fortification in public health: consultation rationale and summary. Ann N Y Acad Sci. 2014;1312:1-7. [DOI] [PubMed] [Google Scholar]
- 63.WHO/UNICEF/ICCIDD Recommended Iodine Levels in Salt and Guidelines for Monitoring their Adequacy and Effectiveness. (WHO/NUT/96.13). Geneva, Switzerland: World Health Organization; 1996. [cited July 2015]. http://apps.who.int/iris/bitstream/10665/63322/1/WHO_NUT_96.13.pdf [Google Scholar]
- 64.Zimmermann MB, Jooste PL, Pandav CS.. Iodine-deficiency disorders. Lancet. 2008;372(9645): 1251-1262. [DOI] [PubMed] [Google Scholar]
- 65.Pearce EN, Andersson M, Zimmermann MB.. Global iodine nutrition: where do we stand in 2013? Thyroid. 2013;23(5):523-528. [DOI] [PubMed] [Google Scholar]
- 66.Mora JO, Dary O, Chinchilla D, Arroyave G.. Vitamin A Sugar Fortification in Central America Experience and Lessons Learned. MOST Project. Washington, DC: USAID ; 2000. [Google Scholar]
- 67.Neufeld LM, Baker S, Garrett GS, Haddad L.. Coverage and utilization in food fortification programs: critical and neglected areas of evaluation. J Nutr. 2017;147(5):1015S-1019S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Aaron GJ, Friesen VM, Jungjohann S, Garrett GS, Neufeld LM, Myatt M.. Coverage of large-scale food fortification of edible oil, wheat flour, and maize flour varies greatly by vehicle and country but is consistently lower among the most vulnerable: results from coverage surveys in 8 countries. J Nutr. 2017;147(5):984S-994S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Martorell R, de Romana DL.. Components of successful staple food fortification programs: lessons from Latin America. Food Nutr Bull. 2017;38(3): 384-404. [DOI] [PubMed] [Google Scholar]
- 70.Harvey PW, Dary O.. Governments and academic institutions play vital roles in food fortification: iron as an example. Public Health Nutr. 2012; 15(10):1791-1795. [DOI] [PubMed] [Google Scholar]
- 71.Garrett GS, Luthringer CL.. The Urgent Need to Improve Compliance of National Fortification Programmes. Geneva, Switzerland; 2015. [cited August 2015]. http://globalnutritionreport.org/2015/06/23/the-urgent-need-to-improve-compliance-of-national-fortification-programmes/ [Google Scholar]
- 72.van den Wijngaart A, Begin F, Codling K, Randall P, Johnson QW.. Regulatory monitoring systems of fortified salt and wheat flour in selected ASEAN countries. Food Nutr Bull. 2013;34(suppl 2): S102-S111. [DOI] [PubMed] [Google Scholar]
- 73.Luthringer CL, Rowe LA, Vossenaar M, Garrett GS.. Regulatory monitoring of fortified foods: identifying barriers and good practices. Glob Health Sci Prac. 2015;3(3):446-461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ming Q, Codling K, Yuqin Y, Zupei C.. China: improving USI to ensure optimal iodine nutrition for all. IDD Newsletter. 2015;43:13-15. [Google Scholar]
- 75.Crider KS, Bailey LB, Berry RJ.. Folic acid food fortification – its history, effect, concerns and future directions. Nutrients. 2011;3(3):370-384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dary O. Establishing safe and potentially efficacious fortification contents for folic acid and vitamin B12. Food Nutr Bull. 2008;29(suppl 2): S214-S224. [DOI] [PubMed] [Google Scholar]
- 77.Taylor CL, Bailey RL, Carriquiry AL.. Use of folate-based and other fortification scenarios illustrates different shifts for tails of the distribution of serum 25-hydroxyvitamin D concentrations. J Nutr. 2015;145(7):1623-1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mannar MG, Sankar R.. Micronutrient fortification of foods – rationale, application and impact. Indian J Pediatr. 2004;71(11):997-1002. [DOI] [PubMed] [Google Scholar]
- 79.Haas JH, Miller DD.. Overview of experimental biology 2005 symposium: food fortification in developing countries. J Nutr. 2006;136(4): 1053-1054. [Google Scholar]
- 80.Neufeld LM, Friesen VM.. Impact evaluation of food fortification programs: review of methodological approaches used and opportunities to strengthen them In: Hurrel R, Mannar V, eds. Food Fortification in a Globalized World. Cambridge, England: Academic Press; Forthcoming. [Google Scholar]
- 81.Best C, Neufingerl N, Del Rosso JM, Transler C, van den Briel T, Osendarp S.. Can multimicronutrient food fortification improve the micronutrient status, growth, health, and cognition of schoolchildren? A systematic review. Nutr Rev. 2011;69(4):186-204. [DOI] [PubMed] [Google Scholar]
- 82.Zimmermann MB, Andersson M.. Assessment of iodine nutrition in populations: past, present, and future. Nutr Rev. 2012;70(10):553-570. [DOI] [PubMed] [Google Scholar]
- 83.Moench-Pfanner R, Ghoos K.. Highlights from WHO/GAIN technical consultation meeting In: Codling K, Fabrizio C, Ghoos K, Rosenzweig J, Smit J, Yusufali R, eds. Scaling Up Rice Fortification in Asia. Geneva, Switzerland: Sight & Life/WFP; 2015:18-19. [Google Scholar]
- 84.Tanahashi T. Health service coverage and its evaluation. Bull WHO. 1978;56(2):295-303. [PMC free article] [PubMed] [Google Scholar]
- 85.Colston J. The use of effective coverage in the evaluation of maternal and child health programs. A technical note for the IDB’s social protection and health division; Inter-American Development Bank; Technical Notes IDB_TN_280, 2011. http://services.iadb.org/wmsfiles/products/Publications/36279205.pdf. Accessed April 30, 2018. [Google Scholar]
- 86.Webb P, Nishida C, Darnton-Hill I.. Age and gender as factors in the distribution of global micronutrient deficiencies. Nutr Rev. 2007;65(5): 233-245. [DOI] [PubMed] [Google Scholar]
- 87.Darnton-Hill I, Webb P, Harvey PW, et al. Micronutrient deficiencies and gender: social and economic costs. Am J Clin Nutr. 2005;81(5): 1198S-1205S. [DOI] [PubMed] [Google Scholar]