Editor—Patients with coronavirus disease 2019 (COVID-19) who require invasive mechanical ventilation frequently meet the acute respiratory distress syndrome (ARDS) diagnostic criteria. Both guidelines and expert opinion recommend 12–16 h per day of prone positioning for patients with moderate-to-severe ARDS from COVID-19.1 , 2 Many of the most severely affected survivors from COVID-19 are now being discharged to inpatient rehabilitation hospitals.3 This provides an important opportunity to assess the long-term sequelae of prone positioning in this patient population. Here, we describe 11 patients who were diagnosed with acquired peripheral nerve injury in association with the use of prone positioning for COVID-19-related ARDS.
Study approval was granted by the Northwestern University Institutional Review Board. Patients were identified during their admission to a single rehabilitation hospital (Shirley Ryan AbilityLab, Chicago, IL, USA). Patients admitted to our hospital post-COVID-19 were received from 19 separate hospitals. Use of prone positioning while patients were mechanically ventilated was confirmed either through review of medical records or, when records were not available, interview with family. For the subset from our academic affiliate, Northwestern Memorial Hospital, prone positioning was performed by a team of respiratory therapists and nurses trained in accordance with guidelines set forth by the Intensive Care Society and Society of Critical Care Medicine. Whenever possible, the diagnosis of peripheral nerve injury was made by electromyography and nerve conduction studies (EMG-NCS). In three cases, localisation of the peripheral nerve injury was informed by magnetic resonance neurography (Fig 1 a), B-mode ultrasonography, or both.
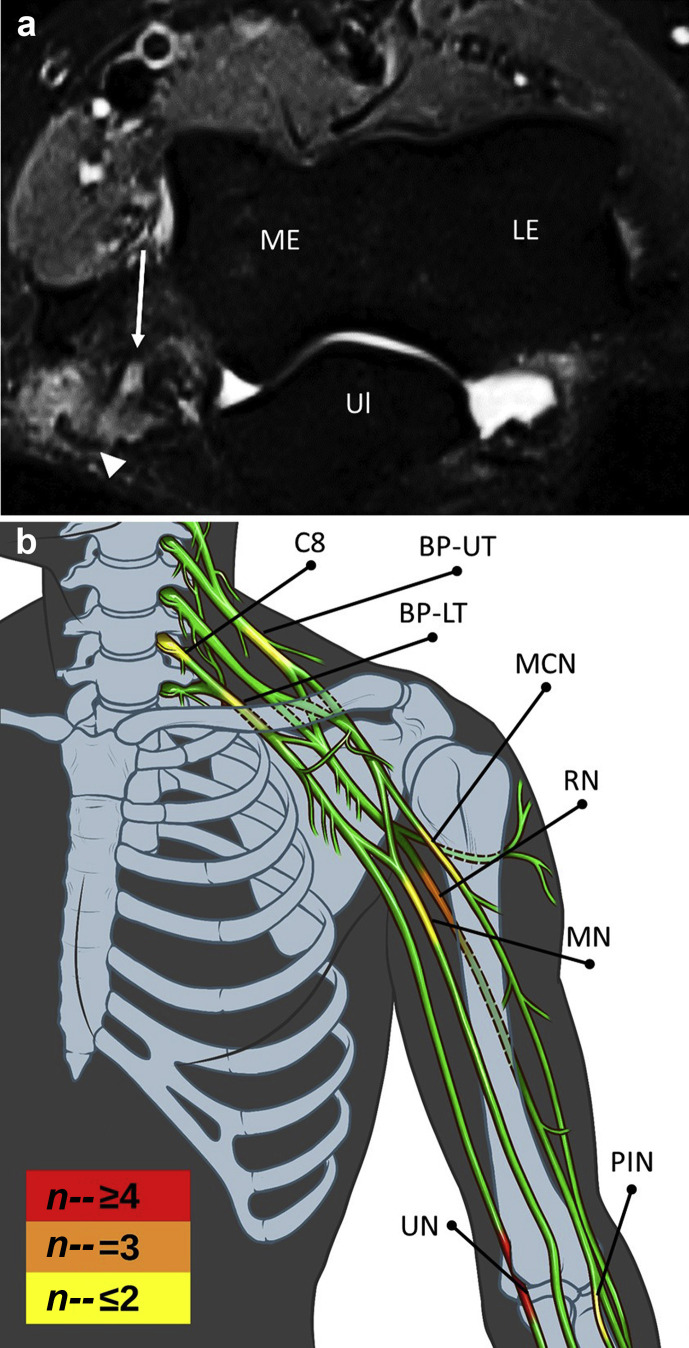
Fig. 1.
Locations of upper limb peripheral nerve injuries associated with prone positioning of patients with coronavirus disease 2019 (COVID-19)-related acute respiratory distress syndrome (ARDS). (a) Axial STIR image from magnetic resonance neurography of the left humerus (Patient 5) demonstrates focal signal hyperintensity of the ulnar nerve (arrow) with focal adjacent soft tissue oedema (arrowhead). (b) Graphical summary of all upper limb PNI sites in this report. Heat map represents the frequency of PNI at defined anatomical sites. BP-LT, lower trunk of brachial plexus; BP-UT, upper trunk of brachial plexus; C8, C8 nerve root; LE, lateral epicondyle; MCN, musculocutaneous nerve; ME, medial epicondyle; MN, median nerve; RN, radial nerve; PIN, posterior interosseous nerve; PNI, peripheral nerve injury; STIR, short tau inversion recovery; Ul, ulna; UN, ulnar nerve.
Between April 24, 2020 and June 30, 2020, 83 patients were admitted to our facility after hospitalisation for COVID-19-related ARDS. Of these, 12 patients (14.5%) were then diagnosed with peripheral nerve injury, and all but one patient had a confirmed history of prone positioning in acute care (91.7%). Patient characteristics, clinical characteristics, and electrophysiology findings are provided (Supplementary Table S1). In total, there were 21 focal peripheral nerve injury sites across these 12 patients and one newly acquired distal symmetric polyneuropathy. The majority of these peripheral nerve injuries occurred in the upper limb (76.2%; Fig 1). The most frequent sites of injury included the ulnar nerve (six cases, 28.6%), radial nerve (three cases, 14.3%), sciatic nerve (three cases, 14.3%), brachial plexus (two cases, 9.5%), and median nerve (two cases, 9.5%). For the 19 peripheral nerve injury sites confirmed by EMG-NCS, 94.7% had Seddon classification of axonotmesis. Complete acute care records were available from a subset of patients from our academic affiliate, Northwestern Memorial Hospital (21 patients) representing a plurality (25.3%) of our total post-COVID-19 admissions. At least one prone positioning session was performed in the management of 61.9% (13 patients), of which there were five patients with peripheral nerve injury. Notably, no focal peripheral nerve injury was identified in the other eight patients from this subset. This aligns with our finding that 11 of the 12 post-COVID-19 patients with peripheral nerve injury in this report had a history of acute management in the prone position.
This report represents the largest description of acquired peripheral nerve injury associated with prone positioning for management of ARDS, and to our knowledge, the first description specific to COVID-19. Peripheral nerve injuries are a well-known, albeit uncommon, positioning-related complication in perioperative medicine reported to occur in 0.14% of surgical cases.4 However, this has been rarely reported with prone positioning in the setting of ARDS. For example, the landmark PROne positioning in SEvere Acute respiratory distress syndrome (PROSEVA) trial does not even mention peripheral nerve injury as a complication.5 Hospitals based in the USA have been incorporating prone positioning into COVID-19-related ARDS treatment plans at a higher rate than normal. The alarmingly high prevalence of peripheral nerve injury in this cohort of rehabilitation patients (14.5%) not only contributes to the burden of disability, but raises the question as to why patients with COVID-19 ARDS are so vulnerable to peripheral nerve injury?
The reason for the high rate of peripheral nerve injury in this cohort is likely multifactorial. There were high rates of diabetes mellitus, obesity, and older age seen in our cohort which are characteristics of severe COVID-19-related ARDS patients,6 and established risk factors for peripheral nerve injury.7 COVID-19 has been associated with muscle injury, acute inflammatory demyelinating polyneuropathy, and a virus-induced state of hyperinflammation and hypercoagulability which increase the vulnerability of peripheral nerves.8 The overlap in COVID-19 mechanisms with type 2 diabetes mellitus, which itself is associated with peripheral nerve injury by a combination of inflammatory and vascular involvement, may also contribute.9
As the subjects described in this study presented from six different tertiary care facilities, hospital-specific approaches to prone positioning cannot alone account for these peripheral nerve injuries. Since only two patients are believed to have received more than four sessions (Supplementary Table S1), it is unlikely that extreme duration of prone positioning was the main cause of the peripheral nerve injury. To put this in perspective, the average number of sessions in the PROSEVA trial was four.5 To mitigate the peripheral nerve injury risk associated with prone positioning for COVID-19-related ARDS, careful consideration must be given to protection of the elbow, upper arm, and shoulder given the distribution of injuries reported here (Fig 1b). Reduction in the mechanical loads on peripheral nerves, specifically avoiding positions of prolonged focal compression, stretching of nerves, or both should be an immediate focus. There are undoubtedly lessons to be learned from perioperative medicine10 to optimise positioning, frequency of repositioning, unloading, and cushioning of susceptible nerve compression sites. Ultrasound elastography may prove to be a useful quantitative measurement tool for assessment of nerve tension and stiffness.11 Limitations of this study include missing clinical data for some patients, lack of a control group, and the retrospective design, which precludes establishment of a causal relationship between prone positioning and peripheral nerve injury. Additionally, many of these patients spent significant time in the supine position on neuromuscular blocking agents which could also increase susceptibility to tissue injury.
In conclusion, peripheral nerve injury after prone positioning for management of severe COVID-19-related ARDS patients is surprisingly common. Physicians must be aware of an increased susceptibility to peripheral nerve injury in severe COVID-19 and refine standard protocols in order to reduce the risk.
Authors' contributions
Conception and design: GRM, ARW, RS, LR, LFW, SD, JHK, JMW, PJ, CKF
Acquisition of data: GRM, ARW, RS, LR, SD, RPN, SDD, CKF
Analysis and interpretation of data: GRM, ARW, JMW, CKF
Manuscript proof reading and editing: all authors
Declarations of interest
The authors declare that they have no conflicts of interest.
Funding
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bja.2020.08.045.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
Multimedia component 1
References
- 1.Alhazzani W., Møller M.H., Arabi Y.M. Surviving sepsis campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19) Intensive Care Med. 2020;46:854–887. doi: 10.1007/s00134-020-06022-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McNicholas B., Cosgrave D., Giacomini C., Brennan A., Laffey J.G. Prone positioning in COVID-19 acute respiratory failure: just do it? Br J Anaesth Adv. 2020 doi: 10.1016/j.bja.2020.06.003. Accessed published on June 08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iannaccone S., Castellazzi P., Tettamanti A. Role of rehabilitation department for adult individuals with COVID-19: the experience of the San Raffaele Hospital of Milan. Arch Phys Med Rehabil. 2020;101:1656–1661. doi: 10.1016/j.apmr.2020.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Parks B.J. Postoperative peripheral neuropathies. Surgery. 1973;74:348–357. [PubMed] [Google Scholar]
- 5.Guérin C., Reignier J., Richard J.C. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 6.Goyal P., Choi J.J., Pinheiro L.C. Clinical characteristics of covid-19 in New York city. N Engl J Med. 2020;382:2372–2374. doi: 10.1056/NEJMc2010419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cohen S.L., Mason K.P., Saxen M.A. Literature review for office-based anesthesia. Anesth Prog. 2018;65:66–68. doi: 10.2344/anpr-65-01-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koralnik I.J., Tyler K.L. COVID-19: a global threat to the nervous system. Ann Neurol. 2020;88:1–11. doi: 10.1002/ana.25807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sasaki H., Kawamura N., Dyck P.J., Dyck P.J.B., Kihara M., Low P.A. Spectrum of diabetic neuropathies. Diabetol Int. 2020;11:87–96. doi: 10.1007/s13340-019-00424-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Practice advisory for the prevention of perioperative peripheral neuropathies 2018: an updated report by the American Society of Anesthesiologists Task Force on prevention of perioperative peripheral neuropathies. Anesthesiology. 2018;128:11–26. doi: 10.1097/ALN.0000000000001937. [DOI] [PubMed] [Google Scholar]
- 11.Rugel C.L., Franz C.K., Lee S.S.M. Influence of limb position on assessment of nerve mechanical properties by using shear wave ultrasound elastography. Muscle Nerve. 2020;61:616–622. doi: 10.1002/mus.26842. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Multimedia component 1