Abstract
Objective. To assess student pharmacists’ ability to impact the administration of complex prescription regimens using the universal medication schedule in a standardized laboratory exercise.
Methods. First and third professional year (P1 and P3) student pharmacists at three colleges of pharmacy completed a required activity to simplify and organize a complex medication regimen. Using a medication box, students planned how and when they would advise a patient to take seven fictitious medications over a 24-hour period. Picture documentation of each students’ activity was used for data analysis. Descriptive statistics were used to compare P1 and P3 students’ performance, and an independent t test was used to assess the frequency of daily dosing. A chi-square analysis was used to compare differences between P1 and P3 students, and analysis of variance was used to compare differences among individual institutions.
Results. Of 842 students invited, 459 P1 and 372 P3 students (98.7%) consented to participate. Student pharmacists recommended 5.1 (SD=1.0; Range=3-11) dosing intervals per 24 hours, with 27% of students successfully reducing the regimen to four total intervals. The P3 students were more effective than the P1 students in planning the number of dosing intervals (4.9 vs 5.4 per 24 hours).
Conclusion. Student pharmacists may become more effective at organizing complex medication regimens as they proceed through the pharmacy curriculum and gain experience. Student pharmacists can translate what they learned from this exercise to potentially improve patients’ self-organized medication regimens.
Keywords: polypharmacy, complex medication regimen, pharmacy, universal medication schedule
INTRODUCTION
Adverse drug events (ADEs) contribute to nearly 700,000 emergency department visits and 100,000 hospital admissions each year.1,2 Numerous factors including patient-, clinician-, or drug-specific reasons contribute to ADEs. Polypharmacy has been identified as a significant risk factor for ADEs in the elderly.3,4 Adverse drug events caused by medication nonadherence can occur when elderly patients are required to manage multiple medication regimens with complicated schedules and/or complex instructions. For example, when a patient is instructed to take a prescribed medication three or four times per day, they are less likely to take it correctly than they would a medication they are instructed to take only once a day.5 Additionally, instructions to take “two tablets by mouth twice daily” often leads to the common misinterpretation by the patient to “take a pill twice a day.”6 Both the clinician who prescribes the medication and the pharmacist who translates the prescription are culpable for labeling issues that may lead to unintended ADEs.
To address this problem, experts from policy, health literacy, and academia gathered at the National Academies (formerly the Institute of Medicine) to develop the universal medication schedule (UMS), a proposed prescribing and dispensing methodology that is intended to increase patient understanding of and adherence to their medication instructions.7,8 The UMS specifies four standard times (morning, noon, evening, and bedtime) to be used in the prescribing and labeling of medications. A study by Wolf and colleagues measured the ability of patients to adhere to and understand prescription labeling using the UMS.9 Within the study, 464 hospitalized patients aged 55 through 74 years were asked to organize a hypothetical, seven-drug medication regimen into a large pillbox with 24 slots representing each hour of the day. The investigators measured the accuracy and variability in the ways the subjects interpreted the medication regimen. On average, patients organized the medication to be taken six times per 24 hours, an increase of two dosing frequencies over the recommended maximum of four times per day. This increased frequency could result in an increased burden for patients who take multiple medications that could ultimately result in nonadherence, suboptimal dosing, and drug-food interactions.6
As medication experts, pharmacists have the capability and expertise to impact medication management to improve patient care, particularly in the elderly.10,11 Currently, pharmacy schools are mandated to address both medication management in special populations and medication safety within their curricula.12 Some pharmacy faculty members have created multiple pedagogical approaches to increase students’ empathy for geriatric patients and their awareness of polypharmacy in this population.13-16 However, research assessing student pharmacists’ ability to organize a complex medication regimen that adheres to the UMS is unavailable. This study assessed student pharmacists’ ability to organize and simplify a complex prescription regimen that adhered to the UMS within a standardized laboratory exercise.
METHODS
Professional year 1 (P1) and year 3 (P3) student pharmacists completed a required activity to organize and simplify a complex patient medication regimen during an ambulatory or community pharmacy-based laboratory sequence. This activity simulated the research on the Universal Medication Schedule (UMS), using an approach similar to that published by Wolf and colleagues.6 This activity occurred at three colleges of pharmacy located within research-intensive public universities (University of Kentucky, University of Illinois at Chicago, and Purdue University). This research protocol was approved by each university’s institutional review board and all students who were included in the analyses gave informed consent prior to participation.
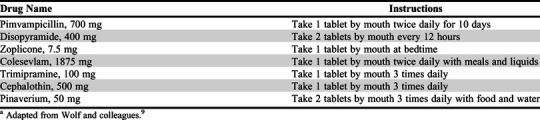
Each student was given seven fictitious or historical medication names and prescription instructions (Table 1). The medication regimens were complex, requiring patients to take medications multiple times per day including supplemental instructions such as at bedtime and/or with food. Students were asked to fill a 24-hour medication box (midnight to 11 pm) in the same way they would instruct a hypothetical patient to take these medications. The box also included the hypothetical patient’s daily schedule with wake, meal, and sleep times (eg, wakes at 5 am); eats breakfast at 8 am, lunch at 12 pm, and dinner at 6 pm; and goes to bed at 9 pm). Students were given the following instructions before beginning the exercise: “Imagine a physician has prescribed these medications for your patient. Please show me how you would suggest the patient take these medicines over the course of one day.” Administration frequency was defined as the total number of dosing intervals represented by the number of bins used within the medication box. This subsequently represented the amount of times the patient would need to take medication during the day to complete the complex medication regimen. Time between doses was measured for each medication and grouped based on alignment with the hypothetical patient’s daily schedule.
Table 1.
Fictitious Medications Used in an Activity to Determine Doctor of Pharmacy Students’ Skills in Scheduling an Optimal Patient Medication Regimena
After completion of the exercise, a deidentified picture of each 24-hour medication box was taken. Pictures were entered into an Excel spreadsheet by two individuals at each institution, and discrepancies were resolved by the lead investigator at each institution. Demographic information outside of year in pharmacy school was not obtained from students to ensure the anonymity of the results.
Next, errors were measured to capture discrepancies identified between the instructions on the label and the organization of the complex medication regimen. For reporting purposes, errors were divided into two categories: frequency and quantity. A frequency error was defined as a subtherapeutic discrepancy (eg, once daily when written for twice daily) or supratherapeutic discrepancy (eg, twice daily when written for once daily) based on total number of daily doses. A quantity error was defined as an inappropriate number of tablets or capsules at a given dosing interval (eg, two tablets were dosed when the prescription was written for one tablet).
The primary outcome of interest was the percent of students who adhered to the UMS recommendation that patients organize a medication regimen into four times per day. Secondary outcomes of interest included the mean (or median if not normally distributed) number of times per day students instructed a hypothetical patient to take medications, the percent of students who filled in less than or equal to four different slots in a 24-hour period, and the percent of students who filled in greater than or equal to seven or more slots in a 24-hour period. The analysis of medication regimens included percent of students who had frequency errors defined as either “no dose given” or “extra dose given” (eg, once daily when should have been twice daily) and the percent of students who had quantity errors defined as “incorrect number of tablets.” Additionally, the number of hours between doses of twice daily and three times daily medications were analyzed.
Descriptive statistics were reported as percentages for each outcome and stratified by year in school and by each institution. Differences in each outcome between P1 and P3 students and between the institutions were assessed. An independent t test was used to assess the number of times per day students instructed a hypothetical patient to take medications. A chi-square analysis was conducted to compare differences between P1 and P3 students. Analysis of variance (ANOVA) was used to compare differences between individual institutions. Odds ratios (OR) were calculated to compare adherence to the UMS among student pharmacists (P3 vs P1 students). All analyses were conducted using SPSS Statistics, version 23 (IBM, Armonk, NY).
RESULTS
A total of 831 student pharmacists across the three colleges of pharmacy consented to participate in the study (98.7% response rate; 831/842). This included 459 P3 students and 372 P1 students. Of the 831 students, 296 were from Purdue University College of Pharmacy (Purdue), 268 were from the University of Illinois at Chicago College of Pharmacy (UIC), and 267 were from the University of Kentucky College of Pharmacy (UK).
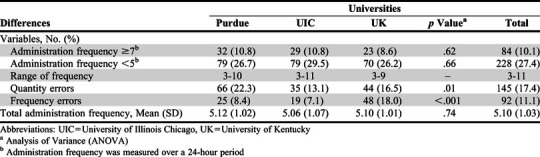
The mean frequency of dosing for the simulated medication regimen across all student pharmacists was 5.1 (SD=1.0) dosing intervals over the 24-hour period (range=3-11). There was no statistical difference in total number of bins used (p=.74) across students from the three colleges of pharmacy. Only 27% of student pharmacists organized the medication regimen according to the UMS of four or fewer standard intervals of dosing, while 10% of students recommended seven or more frequencies per day. Differences between the cohorts of students from each college of pharmacy are summarized in Table 2.
Table 2.
Student Pharmacist Performance on an Activity to Determine Their Skills in Scheduling an Optimal Patient Medication Regimen
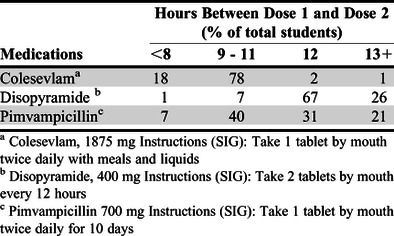
Time between doses was measured for each medication to determine potential causes of increased dosing frequency. Of the medications dosed twice daily (Table 1), 79% of student pharmacists separated the two doses of Colesevlam by 9 to 11 hours; 67% separated two doses of Disopyramide by 12 hours; and 40% separated two doses of Pimvampicillin by 9 to 11 hours, while 31% separated Pimvampicillin by 12 hours. Specific hours between dose 1 and dose 2 are summarized in Table 3.
Table 3.
Dosing Intervals for Twice Daily Medications in an Activity to Determine Their Skills in Scheduling an Optimal Patient Medication Regimen
The P3 student pharmacists were more effective at organizing complex medication regimens than the P1 students were. The average administration frequency that P3 students recommended was 4.9 (0.9) versus 5.3 (1.1) recommended by P1 students (p<.001). When stratified by year in pharmacy school, P3 students were significantly more likely than P1 students to organize the medication regimen according to the UMS (OR=2.81; 95% CI, 2.03-3.91). The P3 students were also significantly less likely to organize the regimen 7 or more times per day compared to P1 students (OR=0.46, 95% CI, 0.29-0.73). This difference was primarily driven by the significant difference in responses between P3 and P1 students at Purdue (4.9 [0.8] vs 5.3 [1.1], p<.001) and UK (4.6 [0.7] vs 5.6 [1.0]; p<.001) with no significant difference at UIC (5.1 [1.1] vs 5.0 [1.0], p=.75).
A total of 17% of student pharmacists’ regimens contained greater than or equal to one quantity error and 11% contained greater than or equal to one frequency error. Students’ progression in the pharmacy program was a significant effect as P3 students made fewer frequency errors compared to P1 students (7% vs 16%; p<.01). However, there was no significant difference in quantity errors when comparing P3 to P1 students (16% vs 19%; p=.84). Differences in quantity and frequency errors between each college of pharmacy student pharmacist cohort are also summarized in Table 2.
DISCUSSION
This study assessed student pharmacists’ ability to impact patients’ administration of complex prescription regimens using a dosing activity designed by Wolf and colleagues following the UMS construct. With neither group of students given any specific instructions or guidance to follow the UMS, P3 students were more likely than the P1 students to organize a medication regimen that adhered to the standard. In all three schools, this was the first-time students had been exposed to the activity, whether they were a P1 or P3 in any curriculum. These results demonstrate that students tend to gain effectiveness in managing complex prescription regimens just with curricular experience and increased time as a student pharmacist. These skills would not only increase the depth of pharmacy curricula but provide additional skills to help graduates in practice.
The primary driver for the increase in dosing frequency over that recommended by the UMS was the individual prescription instructions. A secondary analysis of the timing between medications describes the most likely cause of the increase in frequency. For example, of the three medications to be dosed twice daily, the instructions had a significant impact on the number of hours between dose 1 and dose 2 as described in Table 3. When the label instructions indicated that the medication Colesevlam was to be dosed with meals and liquid, the majority of student pharmacists separated the doses consistent with the patient’s schedule. When the label indicated that the medication Disopyramide was to be dosed every 12 hours, most separated it by 12 hours. Given that Pimvampicillin did not have a specific time or dietary requirement, and was simply to be taken “twice daily,” student pharmacists split the second dose between 9-11 hours or 12 hours, effectively splitting the third twice daily medication between the other two medications. Many students used these times to administer the medications; however, the instructions on one medication were “take 2 tablets by mouth every 12 hours.” Because the times given did not provide an exact 12-hour spread, many students administered the medication at a time that was exactly 12 hours after the first dose but not at a time the patient ate a meal or was going to bed. Realistically, a patient’s daily activities may not perfectly align with ideal medication administration times.
This study used a similar methodology to the research described by Wolf and colleagues.6 Compared to the general population of older adults represented in this previous research, student pharmacists reduced the medication regimen frequency by approximately one time per day compared to the previous patient population (5.1 vs 6.0 per 24 hours). While P1 and P3 students’ dosing regimens were an improvement over those followed by typical patient populations surveyed in previous studies, they still did not meet the standard proposed by the UMS. However, student pharmacists were 2.2 times more likely to organize the medication according to the UMS and were 73% less likely than older adult patients to dose the regimen seven or more times per day (10.1% vs 29.3%). Thus, our findings suggest that student pharmacists could potentially improve patients’ self-organized medication regimens, which could result in fewer administration errors and improved medication adherence.
While P1 and P3 student pharmacists reduced the dosing frequency of the medication regimen by approximately 1 time per day compared to the general population, the P3 student cohort decreased the frequency by approximately 1.5 times per day compared to the general population. A study examining how pharmacists with varying years of experience and/or training complete the same activity would further inform the profession if and how complex medication regimens are simplified in practice. Future research could focus on student pharmacists in experiential rotation and the role of extended-release formulations and the impact on medication regimens.
An additional consideration for future implementation and research is the medication regimen complexity index (MRCI).17 The MRCI is an observational tool that can categorically determine medication complexity. While the MRCI calculation requires evaluation by an observer, there is no clinical judgement involved, and higher MRCI scores have been associated with increased mortality, medication nonadherence, and hospitalizations.17 The regimen in this study had an MRCI score of 30.5, representing a complex regimen, especially for older adults. In previous population-based studies reviewing MRCI, this patient’s medication regimen would fall into the top quadrant (MRCI >20) of a sample of older adults.18 Further variation in the level of student and MRCI score could further validate student pharmacists’ ability to simply complex medication regimens on behalf of patients.
Limitations of this study include a lack of student accountability and variance in activity timing across universities. Students were not formally assessed on their individual performance on the activity and they knew they would not be prior to and while completing the activity. Additionally, the use of fictitious and historical drug names, while negating differences in clinical knowledge between P1 and P3 students, may have led to students not taking the activity seriously or failing to put forth their best effort. Any comparisons to the previous study by Wolf and colleagues, which involved older adults rather than pharmacy students, may be limited. Moreover, there were limited opportunities to conduct the activity within individual curricula, which led to the activity being implemented at different points (weeks) of the academic year, which may have also influenced the results. Finally, although students across institutions were in the same class (P1 or P3), they may have had different levels of training and personal and professional experience at the time they completed the activity.
CONCLUSION
Pharmacists are uniquely positioned to impact care of patients by simplifying medication regimens. The UMS is intended to assist patients in adhering to their medications by simplifying their dosing schedule; however, this tool is underutilized in both practice and education. Student pharmacists were more likely to organize a medication regimen according to the UMS than patients were, and the effectiveness with which student pharmacists organized the medication regimen improved in relation to their pharmacy training. Student pharmacists may be well-equipped to educate and simplify complicated regimens for patients and could impact patient care through effective interventions based on the UMS. Implementation of UMS instruction and/or practice exercises in skills-based courses could address polypharmacy issues, including what should be done in practice to optimize patient care. However, given the potential improvements in medication adherence with little to no foreseen consequences, the authors recommend that the profession adopt a formal position regarding use of the UMS, guiding its implementation in curricula and practice.
ACKNOWLEDGMENTS
The authors would like to thank Fei Wang, PharmD, and Jenny Beal, PharmD, for data collection and data entry and Jeff Cain, EdD, MS, for editorial review.
REFERENCES
- 1.Budnitz DS, Pollock DA, Weidenbach KN, Mendelsohn AB, Schroeder TJ. National Surveillance of Emergency Department visits for outpatient adverse drug events. JAMA. 2006;296:1858-1868. [DOI] [PubMed] [Google Scholar]
- 2.Budnitz DS, Lovegrove MC, Shehab N, Richards CL. Emergency hospitalizations for adverse drug events in older americans. N Engl J Med. 2011;365:2002-2012. [DOI] [PubMed] [Google Scholar]
- 3.Hajjar ER, Cafiero AC, Hanlon JT. Polypharmacy in elderly patients. Am J Geriatr Pharmacother. 2007;5(4):345-351. [DOI] [PubMed] [Google Scholar]
- 4.Maher RL, Hanlon J, Hajjar ER. Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf. 2014;13(1):57-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther. 2001;23(8):1296-1310. [DOI] [PubMed] [Google Scholar]
- 6.Wolf MS, Davis TC, Shrank W, et al. To err is human: patient misinterpretations of prescription drug label instructions. Patient Educ Couns. 2007;67(3):293-300. [DOI] [PubMed] [Google Scholar]
- 7. Literacy RO, Practice BO, Medicine IO. Standardizing Medication Labels: Confusing Patients Less, Workshop Summary. National Academies Press; 2008.
- 8.National Council for Prescription Drug Programs. Universal Medication Schedule White Paper. National Council for Prescription Drug Programs; 2013. https://www.ncpdp.org/NCPDP/media/pdf/WhitePaper/NCPDP-UMS-WhitePaper.pdf?ext=.pdf. Accessed July 30, 2020
- 9.Wolf MS, Curtis LM, Waite K, et al. Helping patients simplify and safely use complex prescription regimens. Arch Intern Med. 2011;171(4):300-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Viswanathan M, Kahwati LC, Golin CE, et al. Medication therapy management interventions in outpatient settings: a systematic review and meta-analysis. JAMA Intern Med. 2015;175(1):76-87. [DOI] [PubMed] [Google Scholar]
- 11.Nightingale G, Hajjar E, Swartz K, Andrel-sendecki J, Chapman A. Evaluation of a pharmacist-led medication assessment used to identify prevalence of and associations with polypharmacy and potentially inappropriate medication use among ambulatory senior adults with cancer. J Clin Oncol. 2015;33(13):1453-1459. [DOI] [PubMed] [Google Scholar]
- 12.Accreditation Council for Pharmacy Education. Accreditation Standards and Key Elements for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree ("Standards 2016"). Published February 2015. https://www.acpe-accredit.org/pdf/Standards2016FINAL.pdf. Accessed July 30, 2020.
- 13.Sauer BL. Student-directed learning in a community geriatrics advanced pharmacy practice experience. Am J Pharm Educ. 2006;70(3):Article 54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Estus EL, Hume AL, Owens NJ. An active-learning course model to teach pharmacotherapy in geriatrics. Am J Pharm Educ. 2010;74(3):Article 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Evans SL, Lombardo M, Belgeri MT, Fontane PE. The geriatric medication game in pharmacy education. Am J Pharm Educ. 2005;69(3):Article 46. [Google Scholar]
- 16.Taggart Blaszczyk A, Mahan RJ, McCarrell J, Sleeper RB. Using a polypharmacy simulation exercise to increase empathy in pharmacy students. Am J Pharm Educ. 2018;82(3):Article 6283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brysch EG, Cauthon KAB, Kalich BA, Sarbacker GB. Medication regimen complexity index in the elderly in an outpatient setting: a literature review. Consult Pharm. 2018;33(9):484-496. [DOI] [PubMed] [Google Scholar]
- 18.Wimmer BC, Johnell K, Fastbom J, Wiese MD, Bell JS. Factors associated with medication regimen complexity in older people: a cross-sectional population-based study. Eur J Clin Pharmacol. 2015;71(9):1099-1108. [DOI] [PubMed] [Google Scholar]


