ABSTRACT
Staff and employees “Zero infection” has been achieved during the whole medical activities in the COVID-19 Fangcang Shelter Hospital in Wuhan, China. This study analyses the personnel and environmental protection status of the East–West Lake Fangcang Shelter Hospital. The HCWs were mostly composed of national medical rescue teams, from different provinces in China. Before the COVID-19 outbreak, 82.64% of the HCWs had already known the proper procedure of wearing masks and other personal protective equipment (PPE). For the total of 634 participants entering the inpatient areas, 99.8% of them took occupational protection trainings via various methods. By carefully training and supervision, most of them were competent to work in the inpatient areas six hours/d, three-four times/week. Besides, 7.8% experienced different types of occupational exposure, which mainly caused by the damage of PPE. Once exposed, the HCWs would disinfect skin or mucous in time. No SARS-CoV-2 RNA was detected in 48 air and environmental samples after regular disinfection and cleaning. To conclude, the bundle including intensive training, strengthened personal protection, strict environmental disinfection and timely remedial measures for occupational exposure had ensured the safety of the East–West Lake Fangcang Shelter Hospital.
KEYWORDS: COVID-19, SARS-CoV-2, health-care workers, Fangcang Shelter Hospital, occupational protection
Introduction
In early February 2020, with the shortage of beds available for the treatment of viral infections in Wuhan, China, there were thousands of patients with mild to moderate COVID-19 sent home for isolation and observation. However, home isolation could put patients’ family members at risk. Therefore, a total of sixteen Fangcang shelter hospitals were built rapidly in different districts of Wuhan, to treat and isolate the patients with mild to moderate COVID-19, by converting exhibition centres and stadiums. Although there was some difference between these Fangcang shelter hospitals, all of the hospitals were supervised by infection control experts, and qualified health-care workers (HCWs) were employed there.
Compared to general hospitals or hospitals for infectious diseases, staff working in the Fangcang shelter hospitals was complexed. In addition to the activities directly participated by doctors and nurses, there were police officers, housekeeping, sanitation workers, and nucleic acid laboratory workers in the P3 laboratory. Therefore, the corresponding PPE requirements were established according to the biosafety risk level. For example, the nucleic acid and blood test personnel, sputum suction and respiratory tract sampling personnel, and the garbage removal/terminal disinfection personnel were protected in biosafety level 3 – PPE (GB19082-2009, EN14126), N95 masks, isolation gowns, goggles, face shields, long shoe covers or alternatives (e.g. thick plastic bags, rain boots), double medical gloves, waterproof apron/long gloves/long rain boots/splash screen (for garbage and excreta handlers); Doctors, CT testing personnel, non-sampling nurses, work/police maintenance support staff, and severe patient transfer staff were protected in level 2 – PPE (EN 14605 type3/type 4, ISO 13982-1&2 type5), goggles or face shield (difference compared with level 3); Catering/drinking water carrier, specimen transshipment staff, medicine dispensers who did not enter the Fangcang shelter hospitals were protected in enhanced level 1 – isolation or chemical protective clothing, N95 or medical surgical masks, goggles, and gloves; Outside management staff were protected in level 1 – isolation or work clothes, medical surgical masks, gloves and hats (Details of the criteria are shown in Supplementary file eTable 1).
The East–West Lake Fangcang shelter hospital was the first to be built, with 1760 confirmed patients admitted from February 7 to March 8, 2020. A total of 1169 HCWs were employed there, including 144 doctors, 839 nurses and 186 management and security personnel. “Zero infection” of HCWs was achieved. With the stabilization of the epidemic and the decrease of bed occupancy, all of the sixteen Fangcang shelter hospitals were closed by March 10, 2020. With the current lack of PPE globally and pressure on healthcare systems worldwide, the protection of HCWs is becoming an increasing concern. In this article, we focused on the occupational protection and environmental protection status of the East–West Lake Fangcang shelter hospital.
Materials and methods
Questionnaire
A cross-sectional study design was used. A questionnaire was sent to all 1169 HCWs by the management staff of the East–West Lake Fangcang shelter hospital via Web. They kept reminding the HCWs weekly to fill out the questionnaire from February 21 to March 8, 2020. In order to ensure the authenticity of the results, the HCWs were asked to fill out the questionnaire anonymously and voluntarily. The questionnaire was originally designed by the infection control team of the East–West Lake Fangcang shelter hospital based on the requirements of the infection control and personnel situation. It consisted of three sections: sociodemographic characteristics, occupational protection characteristics of HCWs at East–West Lake Fangcang shelter hospital, and occupational protection characteristics of HCWs entering inpatient areas. The original link of the questionnaire is available: https://www.wjx.cn/mobile/statnew.aspx?activity=58993199&reportid=#1 (Chinses version).
Environmental air and surface monitoring
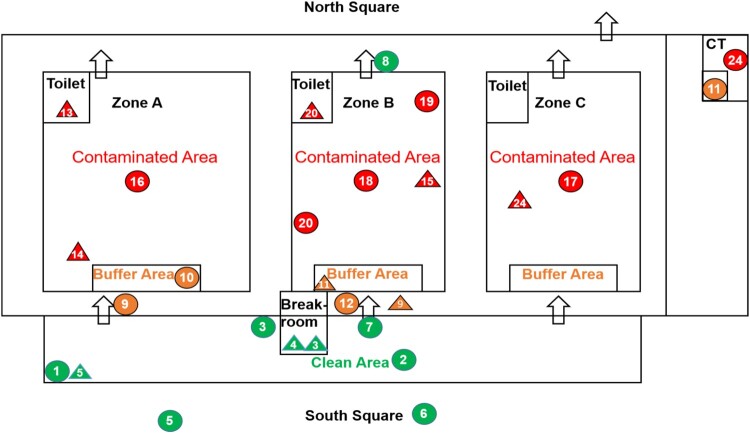
Air sampling was performed on four days using Air Virus collection equipment (NingBo iGene TecTM) with a 0.1 μm gelatin membrane filter for 10 min at 6 m3/h. The surface of the environmental object was sampled using a swab, and placed in a virus preservation solution for transportation. Samples were detected daily in a biosafety level 3 (BSL-3) laboratory (Peking Union Medical College Hospital, Chinese Academy of Medical Sciences) by polymerase chain reaction (PCR) testing (BGI Europe A/S kit, China) conducted within 24 h. The BGI kit was on the WHO emergency use listing for in vitro diagnostics detecting SARS-Cov-2 nucleic acid. The target gene to be amplified was ORF1ab. A total of 20 μL reaction buffer was set up containing 1.5 μL enzyme-mix and 18.5 μL reaction buffer in BGITM SARS-CoV-2 One-step Quantitative RT–PCR system. Thermal cycling was performed at 50°C for 20 min followed by an initial denaturation at 95°C for 10 min and 40 cycles of amplification at 95°C for 15 s and 60°C for 30 s. If the FAM channel amplification curve of the sample to be tested was an S-shaped curve (significant exponential growth period), and the Ct value was ≤38, then the nucleic acid result was supposed to be positive (The layout of the environment and air sampling locations is shown in Figure 1, Supplementary File eTable 2.).
Figure 1.
Layout Showing Environmental and Air Sampling Sites. Numbered labels correspond to environmental and air sampling sites listed in Supplementary File eTable 2. Green, yellow and red represent clean area, buffer area and contaminated area, respectively. Circles and triangle represent air and environmental sampling sites, respectively. Arrows show entrance and exit positions. Repeated measurement sites are not shown.
Evaluation of COVID-19 infection status in HCWs
According to the regulations of the Chinese Health and Safety Committee, all of the 1169 HCWs were quarantined for 14 days after the end of the work, during which time two whole blood and plasma SARS-CoV-2 antibody tests were performed, along with SARS-CoV-2 RNA detection of pharyngeal and nasopharyngeal swabs, and CT imaging of the lungs. A commercial reagent (Wondfo SARS-CoV-2 Antibody Test [Lateral Flow Method] Catalog No.: W195) approved by the CFDA and CE was used for SARS-CoV-2 antibody detection. According to the instruction, the sensitivity and specificity of the antibody kit were 86.43% and 99.57%. The positive predictive value and negative predictive value of it were 99.7% and 82.7%. The SARS-CoV-2 RNA detection method was the same as that described above.
Data analysis
The Statistical Package for the Social Sciences software (SPSS version 20.0; IBM Corporation, Armonk, NY, USA) was used for data analysis. Sociodemographic data and occupational characteristics data were summarized by the frequencies and percentages of occurrence. The chi-square test was used to compare the frequencies of respondents that did or did not experience occupational exposure associated with categorical variables. The variables included age, working years, education level, previous experience in medical rescue, type of masks used daily, the average duration of wearing one mask, residential hotels had proper infection control measures, satisfied with meals, major concerns regarding the current situation, felt discomfort during shifts, felt the polluted air or the unideal temperature, occupational exposure while working in inpatient areas, type of shoes wore in inpatient areas, extent the protective gears impacted on efficiency, and strictly followed the infection control procedure about putting on/taking off protection clothing every time entering/leaving inpatient areas. The validity of these variables was 0.698. For all statistical analyses, a P value of ≤0.05 was considered significant.
Results
Sociodemographic characteristics
A total of 1169 HCWs worked at the East–West Lake Fangcang shelter hospital, including 144 doctors, 839 nurses and 186 management and security personnel. There were 645 participants of them completed the questionnaire anonymously and voluntarily. Among the 645 HCWs, the majority (93.90%) were from provinces other than Hubei province. They comprised 140 (21.71%) males and 505 (78.29%) females, with ages ranging from 22 to 56 years (average 33.98 ± 6.701 years), and the number of working years ranging between 0.5 and 39 (average 11.82 ± 6.9511years). More than half (64.8%) were from tertiary hospitals, and almost all had achieved high-level education (66.67% undergraduate, 5.12% master’s degree or above). Nursing was the most common occupation (80.16%) (Table 1).
Table 1. Sociodemographic characteristics of HCWs at the East-West Fangcang shelter hospital.
| No. (%) | ||
|---|---|---|
| Gender | Male | 140 (21.71) |
| Female | 505 (78.29) | |
| Agea | ≤30 | 224 (34.78) |
| >30 | 420 (65.22) | |
| Working years | ≤15 | 447 (73.95) |
| >15 | 168 (26.05) | |
| Education level | Undergraduate | 430 (66.67) |
| Master's degree and above | 33 (5.12) | |
| Technical college | 164 (25.43) | |
| Technical secondary school | 18 (2.79) | |
| Regionb | Wuhan, Hubei | 39 (6.09) |
| Provinces bordering Hubei | 119 (18.59) | |
| Other provinces | 482 (75.31) | |
| Rank of the residential hospital | Tertiary | 418 (64.81) |
| Secondary | 225 (34.88) | |
| Primary | 2 (0.31) | |
| Job title | Physician | 48 (7.44) |
| Nursing | 517 (80.16) | |
| Technician | 14 (2.17) | |
| Administrative | 41 (6.36) | |
| Security guard | 2 (0.31) | |
| Others | 23 (3.57) | |
| Working department | Internal medicine | 244 (37.84) |
| Respiratory | 69 (10.70) | |
| Cardiology | 31 (4.81) | |
| Infectious Diseases | 25 (3.88) | |
| Surgery medicine | 100 (15.51) | |
| Department of Critical Medicine | 80 (12.40) | |
| Emergency Department | 53 (8.22) | |
| Pediatrics | 20 (3.10) | |
| Gynecology | 22 (3.41) | |
| Other clinical departments | 73 (11.32) | |
| Clinical assistant department | 15 (2.33) | |
| Administration | 3 (0.47) | |
| Infection control department | 4 (0.62) | |
| Operation support department | 31 (4.81) | |
| Ethnicity | Han | 611 (94.73) |
| Hui | 25 (3.88) | |
| Others | 9 (1.40) | |
| Number of days had been working in Hubei so fara | ≤3 weeks | 536 (83.23) |
| >3 weeks | 108 (16.77) |
aMissing one sample.
bMissing five samples.
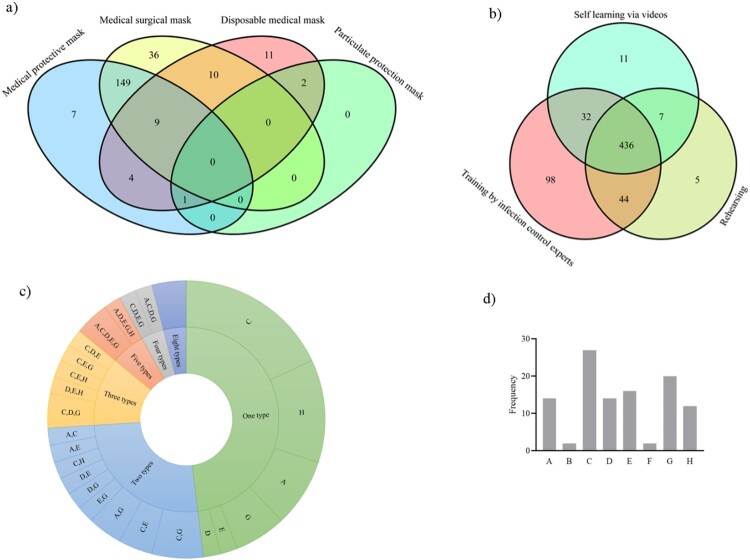
Occupational protection characteristics
Before the COVID-19 outbreak, 18.29% of the 645 HCWs had previous experience in medical rescue, and only 0.9% were inexperienced in the proper procedure for wearing masks. Medical surgical masks were the most common type of masks (61.09%) used by the HCWs during their daily work in the East–West Lake Fangcang shelter hospital, followed by disposable medical masks (27.60%) and medical protective masks (10.23%). Notably, particulate protection masks were also used (1.09%) (Table 2). Only approximately one-third of the HCWs (35.50%) wore multiple masks. Among them, 65.07% used medical protective masks together with medical surgical masks, and 15.72% used a double layer of medical surgical masks, while 1.31% used particulate protection masks together with disposable medical masks or medical protective masks (Figure 2). About half of the HCWs (54.26%) changed their masks every 4 h, 36.43% every 6–8 h and 9.31% of HCWs changed their masks every 12 h or even longer. Most HCWs (90.69%) entered inpatient areas no more than four times a week, while others entered 5–6 times (8.53%) or more than six times (0.78%).
Table 2. Occupational protection characteristics of HCWs at the East-West Fangcang shelter hospital (n = 645).
| No. (%) | ||
|---|---|---|
| Previous experience in medical rescue | Yes | 118 (18.29) |
| No | 527 (81.71) | |
| Occupation during previous medical rescue (n = 118) | Medical staff | 87 (73.73) |
| Medical technician | 5 (4.24) | |
| Administrator | 13 (11.02) | |
| Guard | 1 (0.85) | |
| Others | 12 (10.17) | |
| Knew about proper procedure of wearing masks | Yes | 533 (82.64) |
| Know some | 106 (16.43) | |
| No | 6 (0.93) | |
| Type of masks used dailya | Medical surgical mask | 394 (61.09) |
| Disposable medical mask | 178 (27.60) | |
| Medical protective mask | 66 (10.23) | |
| Particulate protection masks | 7 (1.09) | |
| Wore multiple masks | Yes | 229 (35.50) |
| No | 416 (64.50) | |
| Average duration of wearing one maskb | 4 h | 350 (54.26) |
| 6–8 h | 235 (36.43) | |
| 12 h | 17 (2.64) | |
| 24 h | 21 (3.26) | |
| >24 h | 22 (3.41) | |
| Frequency of entering the inpatient area (times/week) | 0 | 72 (11.16) |
| 1–2 | 312 (48.37) | |
| 3–4 | 201 (31.16) | |
| 5–6 | 55 (8.53) | |
| ≥7 | 5 (0.78) | |
| Living environment | Single room | 307 (47.60) |
| Twin room | 337 (52.25) | |
| Multi-person living room | 1 (0.16) | |
| Residential hotels had proper infection control measures | Yes | 608 (94.26) |
| No | 37 (5.74) | |
| Satisfied with meals | Yes | 572 (88.68) |
| No | 6 (0.93) | |
| Sometimes no | 67 (10.39) | |
| Major concerns regarding the current situation | Personal protection against the virus | 550 (85.27) |
| Safety of the residential environment | 34 (5.27) | |
| Mental health | 22 (3.41) | |
| Leisure | 31 (4.81) | |
| Dining | 8 (1.24) | |
| The most common infection source considered by the HCWs | In the Fangcang shelter hospital | 276 (68.66) |
| Exposure while taking off the PPE | 85 (21.14) | |
| Lack or damage of PPE | 66 (16.42) | |
| Contact patients closely | 20 (4.98) | |
| Others | 105 (26.12) | |
| Out of the Fangcang shelter hospital | 71 (17.66) | |
| Twin room | 40 (9.95) | |
| Crowded place | 18 (4.48) | |
| Others | 13 (2.23) | |
| Personal factors | 55 (13.68) | |
| Inappropriate self-protection | 36 (8.96) | |
| Fatigue | 11 (2.74) | |
| Decreased immunity | 7 (1.74) | |
| Mental health | 1 (0.25) |
aThe filtration efficiency for 0.3 micron particles of medical protective masks (N95/KN95 masks for medical usage)and particulate protection masks (N95/KN95 masks for industry usage) were ≥95%, The filtration efficiency for 0.3 micron particles and 3 micron particles (e.g. bacteria) of medical surgical masks was ≥30% and ≥95%. The filtration efficiency of disposable medical masks were unknown, but lower than the medical surgical masks.
bThe recommended time for each mask was 4 h.
Figure 2.
Occupational protection characteristics of HCWs according to the questionnaire. (a) Types of multiple masks worn by the HCWs (n = 229), (b) types of infection control training methods undertaken by the HCWs before entering the inpatient areas (n = 633), (c) types of occupational exposure experienced by the HCWs (n = 50), (d)the frequency with which each kind of occupational exposure occurred among the 50 HCWs (A-Dropped masks, B-Exposed to secretions without facial protection, C-Damaged protective suits, D-Damaged gloves, E-Damaged shoe covers and shoes, F-Needle stick injury, G-Exposure when taking off PPE, H-Others).
Of the 634 participants entering inpatient areas, only one, who worked as a driver, had not undergone any occupational protection training. When the driver delivered the supply of materials to the East–West Lake Fangcang shelter hospital for the first time, he handed over the materials to the nurse in the semi-contaminated area, which actually means that he did not enter the inpatient areas. After the situation was found, he was trained in time. Apart from that, the rest had undergone training via various methods (Figure 2, Table 3). Similarly, one of the HCWs, who worked as a nurse, did not follow the infection control procedure to put on/take off PPE on entering/leaving inpatient areas. Despite undergoing training through all three methods, this individual was confused by the lack of professional guidance from a dressing room instructor (data not shown). A minority of the HCWs (8.36%) wore their own shoes in inpatient areas. Notably, 50 of the HCWs (7.89%) experienced various types of occupational exposure while working in inpatient areas. Among them, more than one half experienced more than one type of occupational exposure. The percentage of HCWs who felt discomfort during shifts, were anxious about breathing polluted air or found the temperature difficult to tolerate, and who agreed that PPE had a large impact on their work, was higher among those that had undergone occupational exposure compared with those who had not (Table 4). The types of occupational exposure, ranked by cumulative frequency, were damaged protective suits (27), exposures when taking off PPE (20), damaged shoe covers and shoes (16), dropped masks (14) and damaged gloves (14).
Table 3. Occupational protection characteristics of HCWs in inpatient areas (n = 634).
| No. (%) | ||
|---|---|---|
| Training experience before entering | Yes | 633 (99.84) |
| No | 1 (0.16) | |
| Felt discomfort during shifts | Often | 78 (12.30) |
| occasionally | 412 (64.98) | |
| No | 144 (22.71) | |
| Felt the polluted air or the unideal temperature | Yes | 241 (38.01) |
| No | 393 (61.99) | |
| Occupational exposure while working in inpatient areas | Yes | 50 (7.89) |
| No | 584 (92.11) | |
| Type of shoes wore in inpatient areas | Nurse shoes | 294 (46.37) |
| Rubber shoes | 287 (45.27) | |
| Own shoes | 53 (8.36) | |
| Extent the protective gears impacted on efficiency | Largely | 199 (31.39) |
| Some | 325 (51.26) | |
| Basically able to adapt | 110 (17.35) | |
| Strictly followed the infection control procedure about putting on/taking off protection clothing every time entering/leaving inpatient areas | Yes | 633 (99.84) |
| No | 1 (0.16) | |
| Major concerns regarding the current situation | Quantity, quality, comfort of PPE | 133 (51.55) |
| Trainings on occupational exposure emergency treatment | 57 (22.09) | |
| Facilities | 21 (8.14) | |
| Cleaning, ventilation and air monitoring | 16 (6.20) | |
| Hand hygiene | 8 (3.10) | |
| Physical and mental health | 10 (3.88) | |
| Others | 13 (5.04) |
Table 4. Occupational characteristics compared between non-occupational exposure and occupational exposure of HCWs.
| No. (%) | P value | |||
|---|---|---|---|---|
| non-exposure (n = 584) | exposure (n = 50) | |||
| Felt discomfort during shifts | Often | 66(11.30) | 12(24.00) | 0.002 |
| Occasionally | 377(64.55) | 35(70.00) | ||
| No | 141(24.14) | 3(6.00) | ||
| Felt the polluted air or the unideal temperature | Yes | 210(35.96) | 31(62.00) | <0.001 |
| No | 374(64.04) | 19(38.00) | ||
| Major concerns regarding the current situation | Personal protection against the virus | 501(85.79) | 40(80.00) | 0.008 |
| Safety of the residential environment | 33(5.65) | 0(0) | ||
| Mental health | 18(3.08) | 4(8.00) | ||
| Leisure | 27(4.62) | 3(6.00) | ||
| Dining | 5(0.86) | 3(6.00) | ||
| Residential hotels had proper infection control measures | Yes | 555(95.03) | 43(86.00) | 0.002 |
| No | 29(4.97) | 7(14.00) | ||
| Extent the protective gears impacted on efficiency | Largely | 171(29.28) | 28(56.00) | <0.001 |
| Some | 305(52.23) | 20(40.00) | ||
| Basically able to adapt | 108(18.49) | 2(4.00) | ||
aOccupational exposure was supposed to occur when the following conditions happened: dropped masks, damaged protective suits, damaged shoe covers and shoes, damaged gloves, exposure when taking off PPE, needle stick injury, exposed to secretions without facial protection, etc.
Among the 645 participants, the major concern regarding their work was personal protection (85.3%). Additionally, the 50 HCWs who had experienced occupational exposure were concerned about mental health, dining and leisure (Table 4). The most common infection sources among the HCWs were supposed to include exposure while taking off PPE (21.14%), lack or damage of PPE (16.42%), close contact with patients (4.98%), as well as personal factors like inappropriate self-protection (8.96%), fatigue (2.74%), and decreased immunity (1.74%). Areas needing improvement included the quantity, quality, and comfort of PPE (51.55%); training on occupational exposure during emergency treatment (22.09%); facilities (8.14%); and cleaning, ventilation and air monitoring (6.20%). Furthermore, nearly half of the HCWs (52.41%) lived in twin or multi-person living rooms, and most of the residential hotels (94.26%) had proper infection control measures.
Environmental air and surface monitoring
A total of 48 air and environmental surface samples were collected over four days from February 26 to March 7. All PCR results were negative for SARS-CoV-2 RNA. That is, the 2019 SARS-COV2 nucleic acid values in the samples are lower than the detection limit of the BGITM SARS-CoV-2 RT–PCR system (100copies/mL).
Evaluation of the COVID-19 infection status among HCWs
All HCWs were quarantined for 14 days after finishing their work, during which time, two whole blood and plasma SARS-CoV-2 antibody tests, SARS-CoV-2 RNA detection of pharyngeal and nasopharyngeal swabs, and CT imaging of the lungs were performed. All of the results were negative.
Discussion
At present, the global COVID-19 epidemic is ongoing [1]. Traditional hospitals in many countries are unable to provide sufficient beds for the increasing number of infected patients. In the early stage of the COVID-19 epidemic in China, Fangcang shelter hospitals provided purpose-built places for the isolation and treatment of patients with mild and moderate symptoms, effectively promoting the control of the Chinese epidemic [2,3].
Although there were a large number of confirmed patients in the East–West Lake Fangcang shelter hospital, efficient infection control practices were undertaken by HCWs. Firstly, before entering the East–West Lake Fangcang shelter hospital, the HCWs received the latest information about symptom onset, transmission and standard procedure of daily practices, through various types of educational methods [7]. Similarly, other studies have reported the significant role of training on reducing the risk of infection [4–6,8]. We recommend that training and supervision for drivers, security personnel, cleaners, as well as instructors, need to be strengthened. Secondly, HCWs selected appropriate PPE, and applied and removed this PPE, following the standard guidelines. As previously stated, the improvements in PPE are required to increase comfort for HCWs [8–10], and experience in selecting the correct size of PPE, decreased the risk of damage [7]. Thirdly, effective emergency measures were developed. If PPE was damaged, and if there was no direct contact with the inner clothing and skin, the HCWs were asked to wash hand, change and replace with a new PPE immediately, as well as doff and exit ward according to the protocol after work. If the skin was exposed or damaged by sharp things, the HCWs were asked to clean the skin immediately with iodine and 75% alcohol. If mucous membranes (mostly the eyes) were exposed, the HCWs should rinse eyes with saline immediately. One shall report to the head nurse, and immediately doff and exit ward according to the protocol, as well as report the incident to leaders in charge, and arrange self-quarantine or isolation for observation. These measures ensured the safety of the HCWs who had experienced occupational exposure. Notably, our data raised concerns regarding the physical and mental health of exposed HCWs [11]. Finally, appropriate infection control measures were also conducted in the HCWs’ living accommodation, with the physical division being implemented in double rooms.
Additionally, strict cleaning procedures were applied to environmental surfaces and air disinfection measures were performed. Environmental contamination and airborne droplets have been proposed as common routes of transmission [12]. In the hospital, surfaces, such as floors and those in contact with patient belongings, were soaked, sprayed or scrubbed with 1000 mg/L chlorine-containing disinfectant, with an effect lasting > 30 min, at least 4 times/d. Similar to previous reports, after regular disinfection and cleaning, environmental samples tested negative following nucleic acid detection [1,13]. In addition, patients in the East–West Lake Fangcang shelter hospital were asked to wear masks at all times, and change their masks once daily. They were also educated to stop spitting around. Air purification and disinfection apparatus were operated. These measures help to decrease the risk of infection via airborne droplets [12]. It is worth nothing that although one study reported a positive result from an environmental sample from a patient toilet at a Fangcang shelter hospital, only negative results were obtained after rigorous sanitization [14].
This study has some limitations. Firstly, due to the fact that the public traffic in Wuhan was interrupted and communication was blocked at the time of our investigation, it was too challenge to conduct a multi-centre study with other Fangcang shelter hospitals. Secondly, in the design of the questionnaire survey, some characteristics such as suggestions for the infection control measures and feelings after occupational exposure can be more detailed. Thirdly, the guiding role of research results in subsequent infection control measures should be strengthened.
To conclude, the protection of HCWs during the COVID-19 epidemic is crucially important. There were approximately 3000 HCWs got infected in the early epidemic in China. Although the East–West Lake Fangcang shelter hospital admitted 1760 confirmed patients, none of the 1169 HCWs has infection symptoms so far. Overall, a variety of measures including intensive training, strengthened personal protection, thorough environmental disinfection and timely remedial measures following occupational exposure, all contributed to ensuring the safety of HCWs at the East–West Lake Fangcang shelter hospital.
Supplementary Material
Acknowledgments
We would like to thank the following staff for their support in conducting the questionnaire survey and for daily hospital infection management: Bo Liu, Department of Infection Management, the First Affiliated Hospital with Nanjing Medical University, Nanjing, China; Wenli Huang, Department of Neurology, Zhongnan Hospital of Wuhan University, Wuhan University, Wuhan, China; Yuan Wu, Operating Room, Jingxian Hospital, Jingxian, China; Chunxia Wang, Department of ICU, the First People's Hospital of Jinan, Medical College of Binzhou, Jinan, China; Lihua He, Department of Infection Management, Shanghai East Hospital, Tongji University School of Medicine, Shanghai, China; Li Wang, Department of Infection Management, Shaanxi Provincial People’s Hospital, Xi'an, China; Zhiyuan Zhang, Department of Infection Management, General Hospital of Ningxia Medical University, Ningxia, China; Xiao-Fang Wang, Disinfection Supply Center, Pingtan branch, Union Hospital of Fujian Medical University, Fujian, China. The environmental samples were detected in a biosafety level 3 (BSL-3) laboratory (Peking Union Medical College Hospital, Chinese Academy of Medical Sciences).
Funding Statement
This study was funded by the National Natural Science Foundation of China [grant number 81971990], the Municipal Human Resources Development Program for Outstanding Leaders in Medical Disciplines in Shanghai [grant number 2017BR032] and the Top-level Clinical Discipline Project of Shanghai Pudong [grant number PWYgf 2018-05].
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- 1.Cheng VCC, Wong SC, Chen JHK, et al. Escalating infection control response to the rapidly evolving epidemiology of the coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect Control Hosp Epidemiol. 2020 Mar 5: 1–6. doi: 10.1017/ice.2020.58. PubMed PMID: 32131908; PubMed Central PMCID: PMCPMC7137535. eng. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang X, Fang J, Zhu Y, et al. Clinical characteristics of non-critically ill patients with novel coronavirus infection (COVID-19) in a Fangcang Hospital. Clin Microbiol Infect. 2020 Apr 3;26:1063–1068. doi: 10.1016/j.cmi.2020.03.032. PubMed PMID: 32251842; eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen S, Zhang Z, Yang J, et al. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. Lancet. 2020 Apr 18;395(10232):1305–1314. doi: 10.1016/s0140-6736(20)30744-3. PubMed PMID: 32247320; eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhagavathula A, Aldhaleei WA, Rahmani JR, et al. Novel Coronavirus (COVID-19) knowledge and perceptions: A survey of healthcare workers. JMIR Public Health Surveillance. 2020 Apr 19;6:e19160. doi: 10.2196/19160. PubMed PMID: 32320381; eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khan S, Khan M, Maqsood K, et al. Is Pakistan prepared for the COVID-19 epidemic? A questionnaire-based survey. J Med Virol. 2020 Apr 1;92:824–832. doi: 10.1002/jmv.25814. PubMed PMID: 32237161; eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhou M, Tang F, Wang Y, et al. Knowledge, attitude and practice regarding COVID-19 among health care workers in Henan, China. J Hosp Infect. 2020 Apr 9;105:183–187. doi: 10.1016/j.jhin.2020.04.012. PubMed PMID: 32278701; eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu W, Lei H.. A practical handbook for infection control in Makeshift (Fangcang) hospitals: experience from coronavirus disease 2019 (COVID-19) pandemic. Yunfeng Wang, translator. China: Shanghai Science and Technology Press; 2020. [Google Scholar]
- 8.Verbeek JH, Rajamaki B, Ijaz S, et al. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database Syst Rev. 2020 Apr 15;4(4):Cd011621. doi: 10.1002/14651858. CD011621.pub4. PubMed PMID: 32293717; PubMed Central PMCID: PMCPMC7158881 Mischke: none known Jani Ruotsalainen: none known F Selcen Kilinc Balci: none known Riitta Sauni: none known Bronagh Blackwood: none known Elaine Toomley: none known. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lin P, Zhu S, Huang Y, et al. Adverse skin reactions among healthcare workers during the Coronavirus disease 2019 Outbreak: A survey in Wuhan and its surrounding regions. Br J Dermatol. 2020 Apr 7. doi: 10.1111/bjd.19089. PubMed PMID: 32255197; eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gheisari M, Araghi F, Moravvej H, et al. Skin reactions to non-glove personal protective equipment: An emerging issue in the COVID-19 pandemic. J Eur Acad Dermatol Venereol. 2020 Apr 17. doi: 10.1111/jdv.16492. PubMed PMID: 32302444; eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ran L, Chen X, Wang Y, et al. Risk factors of healthcare workers with Corona virus disease 2019: A retrospective cohort study in a designated hospital of Wuhan in China. Clin Infect Dis. 2020 Mar 17. doi: 10.1093/cid/ciaa287. PubMed PMID: 32179890; eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bahl P, Doolan C, de Silva C, et al. Airborne or droplet precautions for health workers treating COVID-19? J Infect Dis. 2020 Apr 16. doi: 10.1093/infdis/jiaa189. PubMed PMID: 32301491; eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ong SWX, Tan YK, Chia PY, et al. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020 Mar 4;323:1610. doi: 10.1001/jama.2020.3227. PubMed PMID: 32129805; PubMed Central PMCID: PMCPMC7057172. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu Y, Ning Z, Chen Y, et al. Aerodynamic characteristics and RNA concentration of SARS-CoV-2 aerosol in Wuhan hospitals during COVID-19 outbreak. bioRxiv. 2020:2020.03.08.982637. doi: 10.1101/2020.03.08.982637. [DOI]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.