Abstract
Austrian syndrome is a rare triad of endocarditis, meningitis, and pneumonia caused by Streptococcus pneumonia described by Robert Austrian in 1956. The incidence has reduced since the introduction of beta-lactam therapy in the early 1940s. Additionally, the introduction of the pneumococcal vaccination in 1977 further decreased the incidence of infection. Streptococcal endocarditis could potentially be very aggressive and life threatening despite appropriate therapy. It has a high mortality rate nearing 30 % even after proper antibiotics and surgical intervention. Therefore, an early recognition is crucial for early intervention and mortality reduction. We present a patient with Austrian syndrome who had a poor outcome despite proper management that is attributed to late presentation and delayed treatment.
Keywords: Streptococcus, Austrian syndrome, Endocarditis, Pneumonia, Meningitis
Case presentation
A 43-year-old male with past medical history of alcohol abuse presented to the hospital due to 1-week history of pain of the left foot. Physical examination was significant for fever, tachycardia, and confusion without focal neurological deficits. There was a systolic murmur in the aortic area, clear lung auscultation, and edema of the left ankle. Laboratory results were significant for thrombocytopenia, hyponatremia, elevated creatinine, and transaminitis. His chest x-ray and x-ray of left ankle were negative. After blood cultures were obtained, ceftriaxone and vancomycin were empirically initiated due to sepsis of unknown organism.
The subsequent day, he became hypoxic requiring 6 L of supplemental oxygen and also hypotensive requiring intravenous crystalloids. Repeat chest x-ray showed bilateral infiltrates (Fig. 1).
Fig. 1.
Chest x-ray.
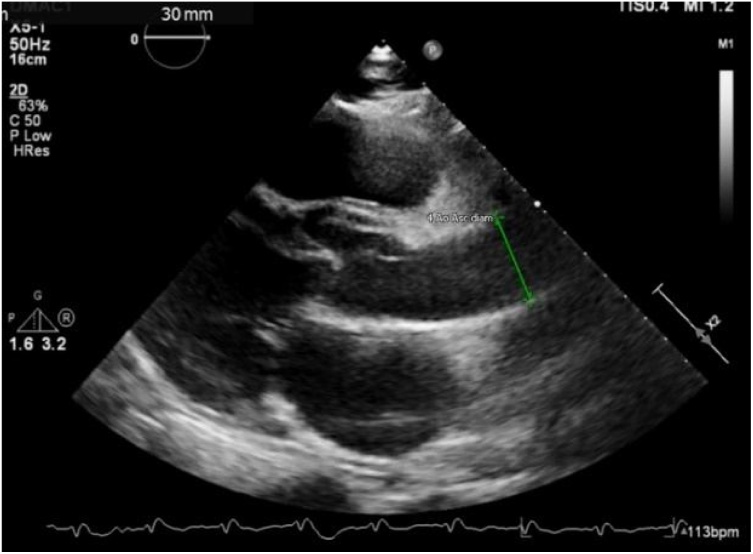
Blood cultures were positive for gram-positive cocci in pairs and chains. Transthoracic echocardiogram showed aortic valve vegetation, possible bicuspid morphology, severe aortic regurgitation and aortic root enlargement possibly from an abscess (Fig. 2).
Fig. 2.
Parasternal long-axis view on echocardiogram.
Lumbar puncture was performed due to worsening mental status. Cerebrospinal fluid analysis showed neutrophilic pleocytosis and hypoglycorrhachia. At that point, Ceftriaxone was increased to 2 g twice a day due to concern of acute bacterial meningitis. Blood cultures finalized with Streptococcus pneumoniae sensitive to cephalosporin. Vancomycin was discontinued.
Ultimately, the patient underwent surgery for aortic valve repair. He had a complicated surgery due to presence of extensive destruction of the aortic valve. The annulus near the interventricular septum and part of the aortic wall were destroyed by the infection. The aortic valve and ventricular wall were repaired.
After surgery, he developed shock and disseminated intravascular coagulation that was deemed multifactorial related to septic and hemorrhagic shock. He was persistently hypotensive despite maximum doses of vasopressors, Ceftriaxone, and massive transfusions. After discussion with the patient’s family, care was withdrawn.
Discussion
Our case highlights challenges in managing Austrian syndrome [1]. First, we emphasize the importance of having an elevated clinical suspicion for Austrian syndrome in patients with any predisposing risk factors (such as alcoholism, advanced age, male sex, or immunosuppression) in the setting of pneumococcal infection [2,4]. Streptococcal infections can progress rapidly with an aggressive clinical course, in which case it is associated with high morbidity and mortality [3,5]. Physicians should focus on cardiac evaluation if the patient has suspicion of pneumococcal pneumonia who has any of the above mentioned risk factors. Sometimes, this can present without any peripheral signs or symptoms of infective endocarditis. These patients may also develop acute encephalopathy that is usually secondary to sepsis. However, the possibility of streptococcal meningitis should always be considered. Lastly, the recommended antibiotic choice is a third generation cephalosporin. Vancomycin should be administered if there is any concern for concurrent bacterial meningitis or beta-lactam resistance until results of the antibiogram become available [6].
Funding
Nothing to declare.
CRediT authorship contribution statement
Yong Il Shin: Writing - original draft. Nana Papyan: Writing - review & editing. Harold Cedeño: Data curation. John Stratidis: Supervision.
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgement
None.
References
- 1.Austrian R Pneumococcal endocarditis, meningitis, and rupture of the aortic valve. Arch Intern Med. 1957;99:539. doi: 10.1001/archinte.1957.00260040039004. [DOI] [PubMed] [Google Scholar]
- 2.Battisha A., Madoukh B., Altibi A., Sheikh O. A rare presentation of Austrian syndrome with septic arthritis in an immunocompetent female. Egypt Heart J. 2019:71. doi: 10.1186/s43044-019-0010-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chirteș I.R., Florea D., Chiriac C., Mărginean O.M., Mănășturean C., Vitin A.A. Severe Austrian syndrome in an immunocompromised adult patient – a case report. J Crit Care Med (Targu Mures) 2018;4(1):17–22. doi: 10.1515/jccm-2017-0025. Published 2018 Feb 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rodríguez Nogué M., Gómez Arraiz I., Ara Martín G., Fraj Valle M.M., Gómez Peligros A. Síndrome de Austrian: Una rara manifestación de la enfermedad neumocócica invasiva. Presentación de un caso y revisión bibliográfica [Austrian syndrome: A rare manifestation of invasive pneumococcal disease. A case report and bibliographic review] Rev Esp Quimioter. 2019;32(2):98–113. [PMC free article] [PubMed] [Google Scholar]
- 5.Rakočević R., Shapouran S., Pergament K.M. Austrian syndrome – A devastating Osler’s triad: case report and literature review. Cureus. 2019;11(4):e4486. doi: 10.7759/cureus.4486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tunkel Allan R., Hartman Barry J., Kaplan Sheldon L., Kaufman Bruce A., Roos Karen L., Michael Scheld W. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis. 2004;39(November (9)):1267–1284. doi: 10.1086/425368. [DOI] [PubMed] [Google Scholar]