The name of the COVID-19 pandemic is derived from the coronavirus disease that started in 2019. It is caused by coronavirus 2 virus of severe acute respiratory syndrome. It was first identified in December 2019 in Wuhan City, the capital of Hubei Province in the People’s Republic of China. A group of sick people with an unknown type of pneumonia were reported. Most affected individuals were linked to workers at the Wuhan South China Wholesale Seafood Market. The World Health Organization recognized it as a pandemic on March 11, 2020.1
When the disease was studied in more detail, one of the transmission routes was found to be aerosols and drops or secretions. Upper digestive endoscopy was determined as a probable transmission route for the virus. For this reason, by recommendation of the different scientific associations around the world and the WHO, in the initial phases of the pandemic, only emergency endoscopy procedures were performed. As Knowledge has grown regarding the safety of medical staff and patients, priority patients have begun being treated in most countries.2
We believe, medically, that the pandemic will not end quickly; only with a vaccine and the social conscience of the people can the contagion be reduced. In these circumstances, even if the contagion rate decreases, aerosol-generating procedures should continue to be carried out with all precautions, including programs to create community awareness, use of personal protection elements, social distancing, and hand washing. Some publications have shown devices that are being used by endoscopists to decrease aerosol loading, such as the Aponte et al3 face mask and the Sabbagh barrier.4
There are some masks that anesthesiologists use for ventilation. These have 4 pins (Fig. 1). We have adapted them using bands with holes that are anchored to the pins (Fig. 2), thus creating an almost perfect seal with the patient’s face. If there is a gap, we reinforce the closure with micropore tapes; however, this occurs in few cases. The mask has a hole in the center that is used for ventilation maneuvers with the AMBU (airway mask bag unit); we put a glove finger on this site, which fits perfectly and does not move. We make a small cut with scissors in this glove finger; endoscopes, including duodenoscopes, enteroscopes, and endosonographs, pass perfectly through this, and the glove finger makes an adequate filter.
Figure 1.

Mask that anesthesiologists use for ventilation. These have 4 pins.
Figure 2.

We adapt the mask using bands with holes, which are anchored to the pins.
This procedure includes the following steps:
-
1.
We place the endoscopy nozzle and the nasal cannula (Fig. 3); both are fixed with adhesive tape (Fig. 4).
-
2.
We place the mask on the patient’s face, making an almost complete seal in which the bands perfectly fit the pins (Fig. 5).
-
3.
We put the mask on the patient. Between the mask and the patient's face, we put an aspiration probe, connected to an aspiration instrument. This instrument vacuums drops and aerosols, reducing the contamination risk further (Fig. 6).
-
4.
In the central hole of the ventilation mask, we place the glove finger (Fig. 7) and make a small cut with scissors (Fig. 8).
-
5.
At the end of the procedure, the mask is removed by the endoscopist and placed directly in a red bag. It is then taken to disinfection management, where it is washed with enzymatic soap for 20 minutes and glutaraldehyde for another 20 minutes and then rinsed with water and dried. These masks can thus be reused.
Figure 3.

We place the endoscopy nozzle and the nasal cannula.
Figure 4.
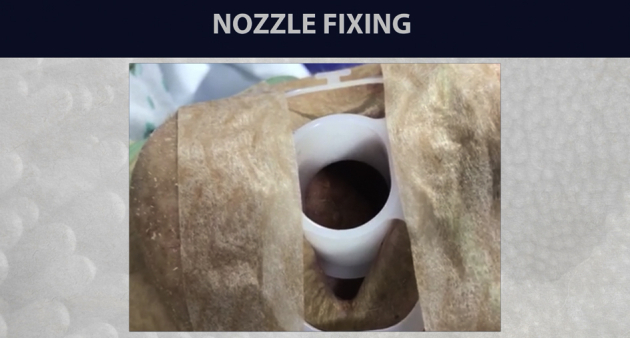
The endoscopic nozzle and the nasal cannula are fixed.
Figure 5.

Mask completely sealed to the patient’s face.
Figure 6.
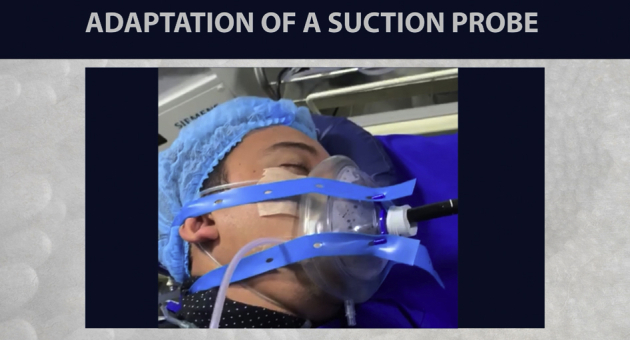
Suction probe between mask and the patient’s face.
Figure 7.

We place a glove finger in the mask hole.
Figure 8.

We make a small cut in the glove finger with scissors.
As shown in Figure 9, the mask is a handmade accessory that protects against secretions and aerosols, preventing contamination of health personnel working in the unit (Video 1, available online at www.VideoGIE.org).
Figure 9.
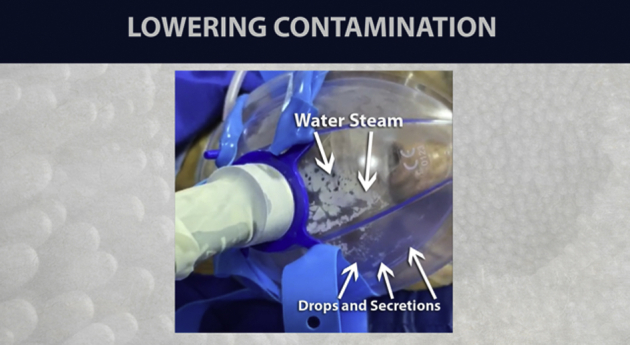
The mask protects against secretions and aerosols, preventing contamination.
Disclosure
All authors disclosed no financial relationships.
Footnotes
If you would like to chat with an author of this article, you may contact Dr Arango at lazaro.arango.m@gmail.com.
Supplementary data
Video 1. Operation of the mask with the glove finger as a filter during the endoscopic procedure.
References
- 1.Soetikno R., Teoh A.Y.B., Kaltenbach T. Considerations in performing endoscopy during the COVID-19 pandemic. Gastrointest Endosc. 2020;92:176–183. doi: 10.1016/j.gie.2020.03.3758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Repici A., Maselli R., Colombo M. Coronavirus (COVID-19) outbreak: What the department of endoscopy should know. Gastrointest Endosc. 2020;92:192–197. doi: 10.1016/j.gie.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aponte D, Corso C, Fuentes C, et al. Use of a new face shield for patients of the endoscopy unit to avoid aerosol exchange in the COVID-19 era. VideoGIE. Epub 2020 Jul 4. [DOI] [PMC free article] [PubMed]
- 4.Sabbagh L, Huertas M, Preciado J. New protection barrier for endoscopic procedures in the era of pandemic COVID-19. VideoGIE. Epub 2020 May 13. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video 1. Operation of the mask with the glove finger as a filter during the endoscopic procedure.


