ABSTRACT
Objective
Psychological interventions for post-traumatic stress disorder (PTSD) are not always effective and can leave some individuals with enduring symptoms. Little is known about factors that are associated with better or worse treatment outcome. Our objective was to address this gap.
Method
We undertook a systematic review following Cochrane Collaboration Guidelines. We included 126 randomized controlled trials (RCTs) of psychological interventions for PTSD and examined factors that were associated with treatment outcome, in terms of severity of PTSD symptoms post-treatment, and recovery or remission.
Results
Associations were neither consistent nor strong. Two factors were associated with smaller reductions in severity of PTSD symptoms post-treatment: comorbid diagnosis of depression, and higher PTSD symptom severity at baseline assessment. Higher education, adherence to homework and experience of a more recent trauma were associated with better treatment outcome.
Conclusion
Identifying and understanding why certain factors are associated with treatment outcome is vital to determine which individuals are most likely to benefit from particular treatments and to develop more effective treatments in the future. There is an urgent need for consistent and standardized reporting of factors associated with treatment outcome in all clinical trials.
KEYWORDS: Psychological intervention, randomized control trial, post-traumatic stress disorder, treatment outcome
HIGHLIGHTS: • This systematic review is the first to demonstrate factors associated with outcome of psychological treatment for PTSD.• This review provides potential treatment targets as well as informing future research assessing factors associated with psychological therapies for PTSD.
Objetivo: Las intervenciones psicológicas para el trastorno de estrés postraumático (TEPT) no son siempre efectivas y pueden dejar a algunos individuos con síntomas permanentes. Se sabe poco acerca de los factores que se han asociado con mejores o peores resultados del tratamiento. Nuestro objetivo fue abordar este vacío.
Método: Llevamos a cabo una revisión sistemática siguiendo las Pautas de Colaboración de Cochrane. Incluimos 126 ensayos controlados aleatorizados (RCTs por sus siglas en ingles) de intervenciones psicológicas para TEPT y examinamos los factores que estuvieron asociados con el resultado del tratamiento, en términos de severidad de síntomas de TEPT postratamiento, y recuperación o remisión.
Resultados: Las asociaciones no fueron ni consistentes ni fuertes. Dos factores se asociaron con reducciones más pequeñas en la severidad de síntomas de TEPT postratamiento: el diagnóstico comórbido de depresión y mayor severidad de los síntomas de TEPT en la evaluación inicial. Los niveles de educación más alta, la adherencia a las tareas y la experiencia de un trauma más reciente se asociaron con mejores resultados del tratamiento.
Conclusión: La identificación y comprensión de por qué ciertos factores se asociaron con los resultados del tratamiento es vital para determinar qué individuos se podrían beneficiar de determinados tratamientos y desarrollar en el futuro, tratamientos más efectivos. Existe una necesidad imperiosa de un reporte consistente y estandarizado de los factores asociados con los resultados de los tratamientos en todos los estudios clínicos.
Palabras clave: Intervención psicológica, Ensayo controlado aleatorizado, Trastorno de Estrés Postraumático, Resultado de tratamiento
目的:创伤后应激障碍(PTSD)的心理干预并不总是有效的,有时会给一些个体留下持久的症状。对于与治疗结果更好或更差的相关因素知之甚少。我们旨在解决此差距。
方法:我们根据Cochrane协作指南进行了系统综述。我们纳入了126项PTSD心理干预的随机对照试验(RCT),并就治疗后PTSD症状严重程度及恢复或缓解情况,考查了与治疗结果相关的因素。
结果:关联既不一致也不强健。两种因素与治疗后PTSD症状严重程度降低程度较小有关:与抑郁的共病诊断和基线评估的高PTSD症状严重程度。高教育水平、坚持家庭作业和最近的创伤经历与更好的治疗结果相关。
结论:识别和理解为什么某些因素与治疗结果相关,对于确定哪些人最有可能从特定治疗中受益以及未来开发更有效的治疗至关重要。亟需与全部临床试验治疗结果相关的一致且标准化因素的报告。
1. Introduction
Post-traumatic stress disorder (PTSD) is a debilitating psychiatric disorder with an estimated lifetime prevalence of 7.8% (Kessler et al., 2005). PTSD results from experiencing or witnessing traumatic events that involve actual or threatened death, serious injury, or sexual violence (American Psychiatric Association, 2000). A proportion of trauma-exposed individuals recover without treatment, while a third of those who initially develop PTSD and receive treatment remain symptomatic for 3 years or longer Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). Despite significant improvements in PTSD treatment, the complex psychopathology and frequency of co-morbid conditions such as depression can make PTSD difficult to treat (Coffey, Stasiewicz, Hughes, & Brimo, 2006) and suboptimal outcome or even treatment failure are not uncommon (Watts et al., 2013b). Understanding why people do better or worse in treatment is imperative and can inform us on the most effective treatments for individuals (Durham et al., 2005; Foa, 2011).
A number of psychological therapies have been evaluated in the treatment of PTSD. Trauma-focused therapies such as exposure-based interventions (Foa, 2011), cognitive-based treatment (Ehlers & Clark, 2008), and Eye Movement Desensitization and Reprocessing (Shapiro, 2014) have been investigated most extensively and shown to be the most effective (Bisson, Roberts, Andrew, Cooper, & Lewis, 2013). Whilst psychological therapies perform reasonably well for many patients, recent estimates suggest that up to 50% of people with PTSD who engage in treatment fail to respond adequately (Resick et al., 2017). Furthermore, 10%–20% of individuals from the general population and 20–40% of military veterans exposed to trauma, experience PTSD symptoms that persist and are associated with impairment despite treatment (Hall et al., 2019) (Rauch et al., 2018). It is not clear why treatments work more or less well for different people with PTSD and there is an urgent need to accurately identify factors that moderate treatment outcome in PTSD.
Enhancing understanding of factors associated with treatment outcome is important for several reasons. First, this knowledge can be helpful in determining treatment choice, especially because not all patients respond to first-line psychological interventions (Watts et al., 2013a). Second, increased knowledge may lead to insight into the fundamental processes underlying treatment and facilitate adaptations or the development of new approaches that improve outcomes. Third, clinicians will be enabled to adjust current treatment delivery and planning, in order to reduce poor response.
The aims of this review were to: (a) undertake the first comprehensive systematic review of factors associated with poor treatment outcome in randomized controlled trials (RCTs) of psychological treatments for individuals with PTSD, and (b) use a narrative synthesis to develop a description of common factors associated with outcome.
2. Methods
The protocol for this systematic review was published via PROSPERO (Barawi, Lewis, Hoskins, Simon, & Bisson, 2017).
This was a systematic review of RCTs. The standards for the conduct of Cochrane Intervention Reviews (MECIR) (Chandler, Churchill, Higgins, Lasserson, & Tovey, 2012) were implemented. A narrative synthesis was conducted in accordance with the ‘Guidance on the Conduct of Narrative Synthesis in Systematic Reviews’ (Popay, Sowden, Petticrew, Arai, & Rodgers et al., 2006).
2.1. Selection criteria
The review included RCTs of any defined psychological therapy aimed at the reduction of PTSD-symptoms in comparison with a control group (e.g. treatment as usual/waiting list), other psychological therapy, or psychosocial intervention (e.g. psychoeducation/relaxation training). To be included in the narrative synthesis, data needed to be available regarding factors associated with treatment outcome. There was no restriction on the type of analysis used to consider this association. Published studies in English of adults aged 18 or over were considered. At least 70% of study participants were required to be diagnosed with PTSD with a duration of 3 months or more, according to DSM or ICD criteria determined by clinician diagnosis or an established diagnostic interview. Co-morbidity was allowed as long as PTSD was the primary diagnosis; this led to the exclusion of studies that solely focused on populations with comorbid PTSD and SUD. There were no restrictions based on symptom severity or trauma-type.
2.2. Search strategy
2.2.1. Search method for identification of studies
This systematic review and narrative synthesis were undertaken alongside a review of the efficacy of psychological therapies for PTSD for an update of The International Society for Traumatic Stress Studies treatment guidelines (International Society of Traumatic Stress Studies (ISTSS) [Online], 2018). A search was conducted by the Cochrane Collaboration, which updated a previously published Cochrane review with the same inclusion criteria (Bisson et al., 2013). This search produced a group of RCTs related to the psychological treatment of PTSD in adults. Data on factors associated with treatment outcome were extracted from these papers.
2.2.2. Data extraction and management
Study characteristics and outcome data were extracted by one reviewer using a pre-designed data extraction spreadsheet. The outcome measures for the review were both diagnostic status and magnitude of change over time, measured by the reduction in the severity of PTSD symptoms at the end of treatment using a standardized measure. When available, clinician-ratedd measures were included in the narrative review (e.g. Clinician Administered Post Traumatic Stress Scale (CAPS)) (Blake et al., 1995). If no clinician rated measure was used or reported, self-report measures were included (e.g. PTSD Checklist for DSM-5 (PCL-5)) (Weathers et al., 2013). Study authors were contacted to obtain missing data and if any clarification was required.
We specifically looked for and extracted information on the following variables that had previously been identified within the literature to be associated with treatment outcome in PTSD, anxiety and depression: (1) age; (2) gender; (3) ethnicity; (4) marital status; (5) employment status; (6) university education; (7) history of psychological intervention; (8) current use of psychotropic medication; (9) type of trauma; (10) time since trauma; (11) time of onset of symptoms after trauma; (12) duration of trauma; and (13) number of traumatic events. This list was not intended to be exhaustive and information on other factors considered was extracted if present.
2.2.3. Data synthesis
The a priori intention was to undertake a meta-analysis. However, there was limited data reported in the studies identified by this review and, when collected, the data were inconsistent in terms of measures used and time points. Therefore, it was decided to undertake a narrative synthesis as opposed to a meta-analysis, in order to synthesis the data in as meaningful a way as possible. Information on factors associated with treatment outcome was tabulated. Factors were coded as either (a) not reported (the factor was not reported in the paper); (b) no association (the factor was reported to have no bearing on treatment outcome); (c) significant increase (the factor was associated with a significant increase in PTSD symptom severity or diagnostic change); or (d) significant decrease (the factor was associated with a significant reduction in PTSD symptom severity or diagnostic change). Due to variation in follow-up time points, the factors were studied as close to the end of treatment as possible.
3. Results
3.1. Systematic search results
The update search for the ISTSS treatment guideline in March 2018 included 114 RCTs. Twelve additional RCTs were identified in an updated search and included in this review, which resulted in 126 eligible RCTs. Fifteen of these RCTs reported on factors associated with treatment outcome; 111 authors were contacted for additional information, 87 responded, 19 supplementary analyses of RCTs were received and reviewed for eligibility. Nine did not meet inclusion criteria as they did not report any factors associated with treatment outcome. This resulted in a total of 126 eligible studies and 25 (20%%) RCTs reported on factors associated with treatment outcome. Figure 1 presents a flow diagram for study selection, and Table 1 presents a summary of the factors associated with treatment outcome.
Figure 1.
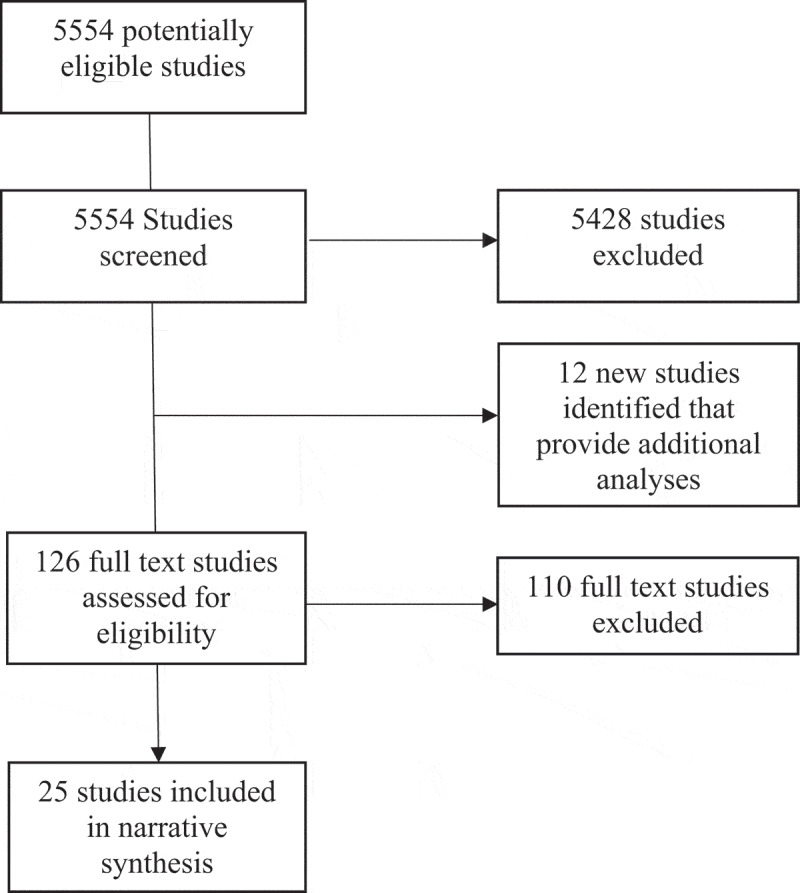
Study flow diagram.
Table 1.
A summary of the factors affecting PTSD treatment outcome.
| Factors associated with Treatment Outcome | Number of studies with a negative association with treatment outcome | Number of studies with a positive association with treatment outcome | Number of studies with no association with treatment outcome |
|---|---|---|---|
| Factors considered in two or more studies | |||
| Adherence to homework | 2 | 1 | |
| Age (younger) | 3 | ||
| Concurrent psychotropic medication | 2 | ||
| Diagnosis of anxiety | 1 | ||
| Diagnosis of depression | 2 | ||
| Gender of participant | 6 | ||
| Higher education | 1 | 5 | |
| Higher severity of PTSD at baseline | 1 | 7 | |
| Less time since trauma | 2 | 3 | |
| Low income | 2 | ||
| Lower severity of PTSD at baseline | 1 | ||
| Married | 1 | 3 | |
| Number of psychotherapy sessions/modules | 3 | ||
| Unemployment | 2 | ||
| Factors considered in one study only | |||
| Ability to describe internal experiences | 1 | ||
| Ethnicity (non-Hispanic white or other) | 1 | ||
| Greater dorsal lateral activation | 1 | ||
| Greater startle response during virtual reality | 1 | ||
| High emotional regulation (anger management and general emotion regulation capacity) | 1 | ||
| History of psychiatric illness | 1 | ||
| Improvement in negative regulation | 1 | ||
| Interpreter presence during therapy | 1 | ||
| Received higher no of psychotherapy treatment previously | 1 | ||
| Reduction in depression and anxiety over the course of therapy | 1 | ||
| Refugee status | 1 | ||
| Stressors outside of therapy (not specified) | 1 | ||
| Therapeutic alliance | 1 | ||
| Therapist gender | 1 | ||
| Therapy type (Eye Movement Desensitisation and Reprocessing (EMDR) versus Imaginal Exposure and Cognitive Restructuring (E+ CR) | 1 | ||
| Type of trauma | 1 | ||
3.2. Characteristics of included studies
The number of randomised participants ranged from 10 to 837. Studies were conducted in Australia (9), Canada (2), China (2), Denmark (1), Germany (5), Iran (2), Israel (1), Italy (2), Japan (1), the Netherlands (8), Norway (1), Portugal (1), Romania (1), Rwanda (1), Spain (1), Sweden (3), Syria (1), Thailand (1), Turkey (3), Uganda (2), UK (11), and USA (77). Participants were traumatised by military combat (28 studies), sexual assault or rape (9 studies), war/persecution (9 studies), road traffic accidents (6 studies), earthquakes (4 studies), childhood sexual abuse (9 studies), political detainment (1 study), physical assault (2 studies), domestic violence/Intimate partner violence (4 studies), trauma from a medical diagnosis/emergency (3 studies) and crime/organised violence (4 studies), and interpersonal violence (1 study). The remainder (56 studies) included individuals traumatised by a variety of different traumatic events. There were 27 studies of females only and 9 of only males; the percentage of females in the remaining studies ranged from 2% to 96%. Participant populations were mostly from the general public (89 studies), followed by military personal/veterans (37 studies), asylum seekers and refugees (8 studies), genocide survivors (1 study) and incarcerated women (1 study). Table 2 presents the characteristics of all the studies.
Table 2.
Characteristics of all the studies reviewed.
| Study | Intervention 1 | Intervention 2 | Intervention 3 | Intervention 4 | Population | % Unemployed | % University Educated |
|---|---|---|---|---|---|---|---|
| (Acarturk et al., 2016) | EMDR | WL | Refugees | Unknown | 4 | ||
| (Adenauer et al., 2011) | NET (CBT-T) | WL | Refugees | Unknown | Unknown | ||
| (Ahmadi, Hazrati, Ahmadizadeh, & Noohi, 2015) | EMDR | REM Desensitization | WL | Military Personnel/Veterans | Unknown | 33.3 | |
| (Akbarian et al., 2015) | Group CBT-T | MC/RA | General Population | Unknown | Unknown | ||
| (Asukai, Saito, Tsuruta, Kishimoto, & Nishikawa, 2010) | PE (CBT-T) | TAU | General Population | Unknown | Unknown | ||
| (Basoglu et al., 2005) | Single-session CBT-T | WL | General Population | Unknown | 5.1 | ||
| (Basoglu et al., 2007) | Single-session CBT-T | MC/RA | General Population | Unknown | 10 | ||
| (Beck, Coffey, Foy, Keane, & Blanchard, 2009) | Group CBT-T | MC/RA | General Population | 54 | Unknown | ||
| (Bichescu, Neuner, Schauer, & Elbert, 2007) | NET (CBT-T) | Psychoeducation | General Population | 0% | 72 | ||
| (Blanchard et al., 2003) | CBT-T | SC | WL | General Population | Unknown | Unknown | |
| (Bradshaw, McDonald, Grace, Detwiler, & Austin, 2014) | OEI | WL | General Population | 0 | Unknown | ||
| (Brom, Kleber, & Defares, 1989) | CBT-T | Psychodynamic Therapy | WL | General Population | 49 | Unknown | |
| (Bryant, Moulds, Guthrie, & Dang, 2003) | CBT-T | SC | General Population | Unknown | Unknown | ||
| (Bryant et al., 2011) | CBT-T | SC | General Population | 84% | Unknown | ||
| (Buhmann, Nordentoft, Ekstroem, Carlsson, & Mortensen, 2016) | CBT-T | WL | Refugees | Unknown | Unknown | ||
| (Butollo, Karl, König, & Rosner, 2016) | CPT (CBT-T) | DET | General Population | Unknown | Unknown | ||
| (Capezzani et al., 2013) | EMDR | CBT-T | General Population | Unknown | Unknown | ||
| (Carletto et al., 2016) | EMDR | RT | General Population | Unknown | Unknown | ||
| (Carlson, Chemtob, Rusnak, Hedlund, & Muraoka, 1998) | EMDR | RT | TAU | Military Personnel/Veterans | 62 | Unknown | |
| (Castillo et al., 2016) | Group PE/CT | WL | Military Personnel/Veterans | 44% | Unknown | ||
| (Chard, 2005) | Group + Individual CPT | WL | General Population | Unknown | Unknown | ||
| (Cloitre et al., 2002) | CBT-T | WL | General Population | 24% | 52 | ||
| (Cloitre et al., 2010) | STAIR (CBT-NTF) | CBT without a trauma focus | General Population | 31% | Unknown | ||
| (Cloitre et al., 2016) | STAIR/EXP | STAIR/SupC | SupC/EXP | General Population | |||
| Cooper & Clum, 1989) | Imaginal Flooding | Standard Group Treatment | Veterans | ||||
| (Cooper, Zoellner, Roy-Byrne, Mavissakalian, & Feeny, 2017) | PE | Sertraline | General Population | ||||
| (Devilly, Spence, & Rapee, 1998) | EMDR | TAU | Military Personnel/Veterans | Unknown | Unknown | ||
| (Devilly & Spence, 1999) | EMDR | CBT-T | General Population | Unknown | Unknown | ||
| (Dorrepaal et al., 2012) | Group Stabilising Treatment | TAU | General Population | 83% | Unknown | ||
| (Duffy, Gillespie, & Clark, 2007) | CT (CBT-T) | WL | General Population | Unknown | Unknown | ||
| (Dunne, Kenardy, & Sterling, 2012) | CBT-T | WL | General Population | 31% | 73 | ||
| (Echeburua, De Corral, Zubizarreta, & Sarasua, 1997) | CBT-T | RT | General Population | Unknown | 20 | ||
| (Ehlers, Clark, Hackman, McManus, & Fennell, 2005) | CT (CBT-T) | WL | General Population | 25% | 35 | ||
| (Ehlers et al., 2003) | CT (CBT-T) | MC/RA | General Population | Unknown | Unknown | ||
| (Ehlers et al., 2014) | CT (CBT-T) | SC | WL | General Population | 23 | 26 | |
| (Falsetti, Resnick, & Davis, 2008) | Group CBT-T | WL | General Population | Unknown | Unknown | ||
| (Fecteau & Nicki, 1999) | CBT-T | WL | General Population | Unknown | Unknown | ||
| (Feske, 2008) | PE (CBT-T) | TAU | General Population | 29% | 90% | ||
| (Foa, Rothbaum, Riggs, & Murdock, 1991) | PE (CBT-T) | CBT without a trauma focus | Supportive counselling | WL | General Population | Unknown | Unknown |
| (Foa et al., 1999) | PE (CBT-T) | CBT without a trauma focus | WL | General Population | 38% | 41% | |
| (Foa et al., 2005) | PE (CBT-T) | WL | General Population | 17% | 34% | ||
| (Foa et al., 2018) | Spaced PE (CBT-T) | PCT | MC/RA | Military Personnel/Veterans | 100% | 66% | |
| (Fonzo et al., 2017) | PE (CBT-T) | WL | General Population | Unknown | Unknown | ||
| (Forbes et al., 2012) | CPT (CBT-T) | TAU | Military Personnel/Veterans | 36% | Unknown | ||
| (Ford, Steinberg, & Zhang, 2011) | CBT without a trauma focus | PCT | WL | General Population | Unknown | 22% | |
| (Ford, Chang, Levine, & Zhang, 2013) | TARGET (CBT-T) Trauma Affect Regulation: Guide for Education and Therapy | Group Supportive Counselling | Incarcerated Women | Unknown | Unknown | ||
| (Galovski, Blain, Mott, Elwood, & Houle, 2012) | TARGET-Group (CBT-T) | MC/RA | General Population | Unknown | Unknown | ||
| (Gamito et al., 2010) | VRE (CBT-T) | Control Exposure | WL | Military Personnel/Veterans | Unknown | Unknown | |
| (Gersons, Lamberts, & Van der Kolk, 2000) | BEP (CBT-T) | WL | General Population | Unknown | Unknown | ||
| (Gray, Budden-Potts, & Bourke, 2019) | RTM (CBT-T) | WL | Military Personnel/Veterans | Unknown | Unknown | ||
| (Haagen et al., 2017) | EMDR + Stabilization | Stabilization | Refugees and Asylum Seekers | ||||
| (Hensel-Dittmann et al., 2011) | NET (CBT-T) | CBT without a trauma focus | Asylum Seekers | Unknown | Unknown | ||
| (Hien et al., 2017) | COPE + PE | Relapse Prevention Therapy | Active monitoring control group | General Population | |||
| Hinton et al., 2005 | CBT-T | WL | Refugees | Unknown | Unknown | ||
| (Hinton, Hofmann, Rivera, Otto, & Pollack, 2011) | Group CBT-T | WL | General Population | Unknown | Unknown | ||
| (Hogberg et al., 2007) | EMDR | WL | General Population | Unknown | Unknown | ||
| (Hollifield, Sinclair-Lian, Warner, & Hammerschlag, 2007) | Group trauma-focused CBT | WL | General Population | Unknown | 40% | ||
| (Ironson, Freund, Strauss, & Williams, 2002) | EMDR | PE (CBT-T) | General Population | Unknown | Unknown | ||
| (Ivarsson et al., 2014) | I-CBT | WL | General Population | 8% | 65% | ||
| (Jacob, Neuner, Maedl, Schaal, & Elbert, 2014) | NET (CBT-T) | WL | Genocide Survivors | Unknown | Unknown | ||
| (Jensen, 1994) | EMDR | WL | Military Personnel/Veterans | 68 | Unknown | ||
| (Johnson, Zlotnick, & Perez, 2011 | CBT without a trauma focus | TAU | General Population | 73 | 7% | ||
| (Johnson, Johnson, Perez, Palmieri, & Zlotnick, 2016 | CBT without a trauma focus | TAU | General Population | 77 | 5% | ||
| (Karatzias et al., 2007) | EMDR | E+ CR | General Population | ||||
| (Karatzias et al., 2011) | EMDR | EFT | General Population | 37 | 47% | ||
| (Keane, Fairbank, Caddell, & Zimering, 1989) | CBT-T | WL | Military Personnel/Veterans | Unknown | Unknown | ||
| (Krupnick et al., 2008) | Group IPT | WL | General Population | 80 | 13% | ||
| Kearney et al., 2013 | MBSR | TAU | Veterans | ||||
| (Krakow et al., 2000) | Imagery rehearsal | WL | |||||
| (Kubany, Hill, & Owens, 2003) | CBT-T | WL | General Population | Unknown | Unknown | ||
| (Kubany et al., 2004) | CBT-T | WL | General Population | Unknown | Unknown | ||
| (Laugharne et al., 2016) | EMDR | PE (CBT-T) | General Population | Unknown | Unknown | ||
| (Lee, Gavriel, Drummond, Richards, & Greenwald, 2002) | CBT-T | EMDR | General Population | Unknown | Unknown | ||
| (Lewis et al., 2017) | I-CBT | WL | General Population | 19 | 62% | ||
| (Littleton, Grills, Kline, Schoemann, & Dodd, 2016) | I-CBT | I-Psychoeducation | General Population | Unknown | Unknown | ||
| (Litz, Engel, Bryant, & Papa, 2007) | I-CBT | I-SC | Military Personnel/Veterans | Unknown | Unknown | ||
| (Lindauer et al., 2005) | BEP | WL | Police officers | ||||
| Marcus, Marquis, & Sakai, 1997 | EMDR | TAU | General Population | Unknown | Unknown | ||
| (Markowitz et al., 2015) | IPT | PE (CBT-T) | Relaxation Therapy | General Population | 21 | Unknown | |
| (Marks et al., 1998) | PE (CBT-T) | Cognitive Restructuring | PE (CBT-T) (CBT-T)(CBT-T)and Cognitive Restructuring | Relaxation without PE (CBT-T) (CBT-T)(CBT-T)or CR | General Population | 54 | Unknown |
| (McDonagh et al., 2005) | PE (CBT-T) | PCT | WL | General Population | 17 | Unknown | |
| (McLay et al., 2011) | VRE (CBT-T) | TAU | Military Personnel/Veterans | Unknown | Unknown | ||
| (McLay et al., 2017) | VRE (CBT-T) | CET | Military Personnel/Veterans | Unclear | Unclear | ||
| (Monson et al., 2012) | Couples CBT-T | CET | General Population | 40 | Unknown | ||
| Monson et al., 2006 | CPT (CBT-T) | WL | Military Personnel/Veterans | Unknown | Unknown | ||
| (Miyahira et al., 2012) | VR | Minimal attention | Active military | ||||
| (Morath et al., 2014) | NET (CBT-T) | WL | Refugees | Unknown | Unknown | ||
| (Mueser et al., 2008) | CBT-T | WL | General Population | Unknown | Unknown | ||
| (Nacasch et al., 2011) | PE (CBT-T) | TAU | Military Personnel/Veterans | 63 | Unknown | ||
| (Neuner et al., 2010) | NET (CBT-T) | TAU | Refugees | Unknown | Unknown | ||
| (Neuner et al., 2008) | NET (CBT-T) | TAU | Monitoring | Refugees | 49 | Unknown | |
| (Neuner, Schauer, Klaschik, Karunakara, & Elbert, 2004) | NET (CBT-T) | SC | Psychoeducation | Refugees | 28 | Unknown | |
| (Nijdam, Gersons, Reitsma, de Jongh, & Olff, 2012) | BEP (CBT-T) | SC | General Population | Unknown | 30 | ||
| (Pacella et al., 2012) | PE (CBT-T) (CBT-T) | EMDR | General Population | Unknown | Unknown | ||
| (Paunovic, 2011) | CBT-T | MC/RA | General Population | 74 | 11 | ||
| (Peniston & Kulkosky, 1991) | CBT-T | WL | Military Personnel/Veterans | Unknown | Unknown | ||
| (Polusny et al., 2015) | MBST | PC-GT | Veterans | ||||
| (Pigeon, Allen, Possemato, Bergen-Cico, & Treatman, 2015) | PCBMT | Primary Care | Veterans | ||||
| (Power et al., 2002) | EMDR | TAU | WL | General Population | Unknown | Unknown | |
| (SAM Rauch et al., 2015) | PE (CBT-T) (CBT-T) | CBT-T | Military Personnel/Veterans | Unknown | Unknown | ||
| (Ready, Gerardi, Backscheider, Mascaro, & Rothbaum, 2010) | VRE (CBT-T) | PCT | Military Personnel/Veterans | Unknown | Unknown | ||
| (Reger et al., 2016) | VRE (CBT-T) | PCT | WL | Military Personnel/Veterans | Active duty | 7 | |
| (Resick et al., 2015) | CPT-Group | PE (CBT-T) | Military Personnel/Veterans | 0 | 8 | ||
| (Resick, Nishith, Weaver, Astin, & Feuer, 2002) | CPT (CBT-T) (CBT-T) | Group PCT | Minimal Attention | General Population | Unknown | Unknown | |
| (Resick et al., 2017) | CPT (CBT-T) (CBT-T) | PE (CBT-T) | Military Personnel/Veterans | 100 | 19 | ||
| (Rothbaum, 1997) | EMDR | Group CBT-T | General Population | 19 | 43 | ||
| (Rothbaum, Astin, & Marsteller, 2005) | PE (CBT-T) | WL | WL | General Population | Unknown | Unknown | |
| (Sautter, Glynn, Cretu, Senturk, & Vaught, 2015 | Couples CBT without a trauma focus | EMDR | Military Personnel/Veterans | ||||
| Sautter et al., 2016 | SAT | PTSD family education intervention | Veterans | 12 | 75 | ||
| Scheck, Schaeffer, & Gillette, 1998 | EMDR | Couples Psychoeducation | General Population | Unknown | Unknown | ||
| Schnurr et al., 2003 | Group CBT-T | SC | Military Personnel/Veterans | 51 | Unknown | ||
| (Schnurr et al., 2007 | PE (CBT-T) (CBT-T) | Group PCT | Military Personnel/Veterans | 38 | Unknown | ||
| (Schnyder et al., 2011) | BEP (CBT-T) | Group PCT | General Population | Unknown | Unknown | ||
| (Schoorl, Putman, Van Der Werff, & Van Der Does, 2014) | ABM | AC | General Population | ||||
| (Shemesh et al., 2011) | IET | Control education condition | General Population | ||||
| (Sloan, Marx, Bovin, Feinstein, & Gallagher, 2012) | WET | MC/RA | General Population | 78 | 41 | ||
| (Sloan, Marx, Lee, & Resick, 2018) | WET | WL | General Population | Unknown | 13 | ||
| (Smyth, Hockemeyer, & Tulloch, 2008) | Expressive Writing; writing about their traumatic experience | Control Group (writing about time management) | Veterans | ||||
| (Spence et al., 2011) | I-CBT | CPT (CBT-T) | 41 | Not Clear | |||
| (Stenmark, Catani, Neuner, Elbert, & Holen, 2013) | NET (CBT-T) | WL | Refugees | Unknown | 25 | ||
| (Suris, Link-Malcolm, Chard, Ahn, & North, 2013) | CPT (CBT-T) | TAU | Military Personnel/Veterans | 43 | 16 | ||
| (Stirman et al., 2018) | Cognitive processing therapy with trauma account | Cognitive Processing Therapy without trauma account | General Population | ||||
| (Taylor et al., 2003 | PE (CBT-T) | PCT | EMDR | General Population | 13 | Unknown | |
| (Stapleton et al., 2006) | PE | EMDR | Relaxation Therapy | General Population | Unknown | Unknown | |
| (ter Heide, Mooren, Kleijn, de Jongh, & Kleber, 2011) | EMDR | Stabilization | Asylum Seekers and Refugees | ||||
| (Tylee, Gray, Glatt, & Bourke, 2017) | RTM (CBT-T) | Relaxation Therapy | General Population | ||||
| (Vaughan et al., 1994 | CBT-T | WL | EMDR | General Population | Unknown | Unknown | |
| (Wells, Walton, Lovell, & Proctor, 2015) | PE (CBT-T) | RT | WL | General Population | 6 | Unknown | |
| (Wells & Sembi, 2012) | CBT without a trauma focus | CBT without a trauma focus | General Population | Unknown | Unknown | ||
| (Wittmann et al., 2012) | BEP | Minimal attention Control Condition | General Population | ||||
| (Wilson et al., 1995) | EMDR | WL | General Population | ||||
| (Yehuda et al., 2014) | PE (CBT-T) | WL | Military Personnel/Veterans | Unknown | Unknown | ||
| (Zang, Hunt, & Cox, 2014) | NET (CBT-T) | MC/RA | General Population | Unknown | Unknown | ||
| (Zang, Hunt, & Cox, 2013) | NET (CBT-T) | WL | General Population | Unknown | Unknown | ||
| (Zlotnick et al., 1997) | Group CBT-T | WL | General Population | Unknown | 33 |
Acronyms
ATM = Attentional bias modification
BEP = Brief Eclectic Psychotherapy
CBT = Cognitive Behavioural Therapy
CBT-T = Cognitive Behavioural Therapy with a Trauma focus
CET = Control Exposure Therapy
COPE = Concurrent treatment of PTSD
CPT = Cognitive Processing Therapy
CR = Cognitive Restructuring
CT = Cognitive Therapy
RTM = Reconsolidation of Traumatic Memories
DET = Dialogical Exposure Therapy
E + CR = Imaginal Exposure + Cognitive Restructuring
EFT = Emotional Freedom Technique
EMDR = Eye Movement Desensitisation and Reprocessing
I-CBT = Internet-based Cognitive Behavioural Therapy
IET = Imaginal Exposure Therapy
I-Psychoeducation = Internet-based Psychoeducation
IPT = Interpersonal Psychotherapy
I-SC = Internet-basedd Supportive Counselling
MBSR = Mindfulness-Based Stress Reduction
MC/RA = Medical Checks/Repeated Assessments
NET = Narrative Exposure Therapy
NTF = Non-Trauma Focussed
OEI = Observed and Experimental Integration
PCBMT = Primary Care Brief Mindfulness Training
PCGT = Present Centred Group Therapy
PCT = Present Centred Therapy
PE = Prolonged Exposure
REM Desensitization = Rapid Eye Movement Desensitization
RT = Relaxation Therapy
SAT = Structured Approach Therapy
SC = Supportive Counselling
STAIR + SupC = Skills Training in Affective and Interpersonal Regulation + Supportive Counselling
STAIR = Skills Training in Affective and Interpersonal Regulation
TAU = Treatment as Usual
TARGET (CBT-T) Trauma Affect Regulation: Guide for Education and Therapy
VR = Virtual Reality
VRE = Virtual Reality Exposure
WET = Written Emotion Therapy
WL = Waiting List
3.3. Factors associated with treatment outcome
3.2. Clinical characteristics
Symptom Severity: Severity of PTSD symptoms at baseline was one of the most commonly reported factors examined in relation to treatment outcome. The majority of studies that examined this association (n = 7 studies) found that PTSD symptom severity scores at baseline had no association with treatment outcome (Basoglu, Salcioglu, & Livanou, 2007; Ehlers et al., 2003; Haagen, Ter Heide, Mooren, Knipscheer, & Kleber, 2017; Karatzias et al., 2007; Lewis et al., 2017; Schnyder, Müller, Maercker, & Wittmann, 2011; Wittmann, Schnyder, & Buchi, 2012). However, findings were not consistent: one study reported that the most severe PTSD symptoms at baseline were associated with benefiting less from treatment (Cloitre, Petkova, Su, & Weiss, 2016).
3.2.1.1. Comorbid symptomatology
Comorbid diagnosis of depression was associated with significant increase in PTSD symptom severity in two studies (Haagen et al., 2017; Cloitre et al., 2016) which found those with a diagnosis of depression did less well in treatment compared to those without the diagnosis.
3.2.1.2. Aspects of treatment
Three studies found that the number of sessions or modules completed was not associated with treatment outcome (Haagen et al., 2017; Karatzias et al., 2007; Lewis et al., 2017). Concurrent use of psychotropic medication was not associated with treatment outcome (Ivarsson et al., 2014; Karatzias et al., 2007).
3.2.1.3. Time since trauma
One study found that more recent trauma was associated with a slightly improved effect (Lewis et al., 2017). However, three papers found that time since trauma had no association with treatment outcome (Basoglu et al., 2007; Ehlers et al., 2003; Karatzias et al., 2007).
3.2.1.4.. Type of trauma
One study found no association between the type of trauma and treatment outcome (Karatzias et al., 2007).
3.3. Patient characteristics
Younger Age was found to have no association with treatment outcome in three studies (Basoglu et al., 2007; Karatzias et al., 2007; Lewis et al., 2017).
Education was considered in six studies; one found that those who had completed higher education had greater treatment effect (Lewis et al., 2017); and five studies found no association between years of education and treatment outcome (Basoglu et al., 2007; Basoglu, Salcioglu, Livanou, Kalender, & Acar, 2005; Ivarsson et al., 2014; Krakow et al., 2000; Wilson, Becker, & Tinker, 1995)
Employment status had no association with treatment outcome in two studies (Ivarsson et al., 2014; Karatzias et al., 2007).
Adherence to homework was found to be positively associated with treatment outcome in two studies (Marks, Lovell, Noshirvani, Livanou, & Thrasher, 1998) (Dorrepaal et al., 2012), but one study found no association with the amount of time spent on completing homework and treatment outcome (Spence et al., 2011). Completion of homework was associated with better outcomes for patients with fewer years of formal education compared to those who reported more years of education (Stirman et al., 2018).
Marital status was associated with greater gain from treatment in one study (Wilson et al., 1995) yet had no association with treatment outcome in three other studies (Ivarsson et al., 2014; Krakow et al., 2000; Karatzias et al., 2007).
Lower household income was reported to not have any association with treatment outcome in two studies (Krakow et al., 2000; Wilson et al., 1995).
Gender of participants was reported in seven studies to have no association with treatment outcome (Basoglu et al., 2007; Blanchard et al., 2003; Haagen et al., 2017; Ivarsson et al., 2014; Karatzias et al., 2007; Lewis et al., 2017; Wilson et al., 1995).
3.4. Other factors identified
Better emotional regulation was positively associated with treatment outcome in two studies, one found an association with better functioning (Cloitre et al., 2016) and one with greater reduction in PTSD (Hien, Lopez-Castro, Papini, Gorman, & Ruglass, 2017). Furthermore, low emotional dysregulation was associated with a reduction in substance abuse (Hien et al., 2017) and improvements in negative mood regulation (Cloitre, Koenen, Cohen, & Han, 2002). Three other studies found that the number of previous traumas had no association with treatment outcome (Basoglu et al., 2007, 2005; Haagen et al., 2017).
One study found that participants who were able to describe their internal experiences, thoughts, emotions and sensations in a non-judgemental manner were associated with a significant reduction in CAPS score (Possemato et al., 2016).
Ethnicity was not found to be associated with treatment outcome in one study (Krakow et al., 2000). Refugee status (Haagen et al., 2017) and the presence of stressors during the treatment (Stapleton, Taylor, & Asmundson, 2006) had no association with treatment outcome. Table 2 presents a summary of the factors associated with treatment outcome and Table 3 presents the characteristics of the papers that reported any factors associated with treatment outcome.
Table 3.
Characteristics of the studies: The following are studies that report any factors associated or not associated with treatment outcome of psychological therapies of PTSD.
| Study | Country | Intervention | Participants | Type of trauma | Factors associated (or not) with treatment outcome |
|---|---|---|---|---|---|
| (Basoglu et al., 2005) | Turkey | Single-session CBT | 59 | Earthquake | Greater PTSD severity, higher education and past trauma had no significant association with treatment outcome as measured by the CAPS-IV but it was associated with less improvement in the Patients Global Impression (a self-measure that reflect a patient’s belief about efficacy of treatment). |
| (Basoglu et al., 2007) | Turkey | Single-session CBT | 31 | Earthquake | Age, gender, education, past psychiatric illness, history of past trauma, time since the earthquake, and the pre-treatment clinical ratings were not significantly associated with treatment outcome. |
| (Blanchard et al., 2003) | USA | Trauma focused CBT | 98 | Road Traffic accidents | There was no main effect or interaction with therapist gender or no main effect of gender of patient to treatment outcome. |
| (Cloitre et al., 2002) | USA | CBT-T | 58 | Various | Predictors of improvement were therapeutic alliance and improvement in Negative mood regulation as measured by the NMR as measured by the CAPS. Significant reduction posttreatment in depression and anxiety were not associated with PTSD symptom severity reduction. |
| (Cloitre et al., 2016) | USA | Skills training in affective and interpersonal regulation (STAIR) followed by Prolonged Exposure (EXP) | 104 | Childhood sexual and physical trauma/abuse | Higher emotional regulation predicted better functioning. Those with high ‘Symptom burden’ (PTSD, depression, dissociation and interpersonal problems) was associated with worse treatment outcome, and did least well in exposure, moderately well in skills and best in the combination as measured by the PTSD symptom severity, assessed via the CAPS. |
| (Dorrepaal et al., 2012) | Netherlands | Stabilizing Group Treatment | 71 | Child Abuse | Diagnosis of Borderline Personality Disorder (BPD) was associated with greater compliance, defined by completed treatment, as opposed to those without the personality diagnosis. |
| (Ehlers et al., 2003 | UK | Cognitive Therapy (CT) | 85 | Road Traffic accident | Neither time since trauma nor the degree of change in PTSD severity (PDS) score with self-monitoring were associated with outcome. |
| (Fonzo et al., 2017) | USA | Prolonged Exposure (PE) | 66 | Not specified | Less Blood Oxygen Level Dependent activation (signal) in the brain at baseline was associated with greater reductions in symptom scores in the waiting list group in two right and two left dorsolateral prefrontal clusters. Finally, greater dorsal anterior cingulate activation at baseline was associated with greater reductions in symptom scores in the treatment group but not in the waiting list group |
| (Galovski et al., 2012) | USA | Modified Cognitive Processing Therapy (M-CPT) | 100 | Various | Treatment dropouts were younger, had fewer years of education and had lower annual household income and significantly higher pre-treatment CAPS severity at baseline assessment. Participant age, time since index trauma and pre-treatment CAPS and Beck Depression Inventory-II scores were identified as potential predictors of length of therapy. |
| (Haagen et al., 2017) | Netherlands | Eye Movement Desensitization and Reconsolidation and Stabilization (EMDR-S). | 72 | Various | Patients with severe levels of depression at baseline as measured by The Hopkins Symptom Checklist had progressively less PTSD symptom reduction over time. A diagnosis of major depressive disorder was predictive of poor treatment response, indicating that patients with a major depressive disorder improved less than patients without a major depressive disorder. None of the other predictors (pre-treatment PTSD severity, refugee status, interpreter presence during therapy, the number and nature of traumatic events, gender, number of psychotherapy sessions, and treatment dropout) were significantly associated with treatment outcome. |
| (Hien et al., 2017) | USA | Concurrent Treatment of PTSD and SUD using Prolonged Exposure (COPE). | 110 | Various | Baseline emotional dysregulation (ED) severity moderated treatment outcomes such that high ED was associated with greater reduction in PTSD severity among those who received COPE relative to RPT and AMCG. In contrast, low ED as association with greater reduction in substance use among those in RPT relative in COPE and AMCG. |
| (Ivarsson et al., 2014) | Sweden | Guided Internet Delivered Cognitive Behaviour Therapy for PTSD. | 62 | Various | Participant lost to follow-up were on average
younger compared to those who completed the study. Gender, age, marital status, highest educational level, unemployment status, psychopharmacological medication and history of psychotherapy were not associated with treatment outcome. |
| (Karatzias et al., 2007) | UK | Eye Movement Desensitisation and Repro- cessing (EMDR) vs Imaginal Exposure and Cognitive Restructuring (E+ CR) | 48 | Various | Higher pre- to post-treatment CAPS total change score was significantly associated with fewer sessions and a lower baseline CAPS total score. Age, gender, marital status, occupation, type of trauma, time since trauma, therapy type, number of sessions, psychotropic medication, CAPS total (baseline), HADS-A, HADS-Dwere not associated with treatment outcome, as measured by pre and post CAPS severity scores. |
| (Krakow et al., 2000) | USA | Imagery Rehearsal Therapy (IRT) | 169 | Sexual assault | Demographic covariates; ethnicity, marital status, annual income, or education were not significant in any of the analyses. |
| (Kubany et al., 2004) | USA | Cognitive Trauma Therapy for Battered Women (CTT-BW) | 125 | Domestic Abuse | Comorbidity with depression, low self-esteem, younger age, less educated, and more shame prone at the initial assessment were associated with non-completers of treatment. |
| (Lewis et al., 2017) | UK | Internet-based guided self-help | 42 | Various | There was no significant effect modification by age, gender, baseline CAPS score, number of modules completed, or number of therapist minutes. However, more recent trauma experienced a slightly improved effect. Higher education was associated with greatest treatment effect, and those with a higher degree experiencing greater improvement in CAPS scores. |
| (Marks et al., 1998) | UK | Prolonged Exposure (PE) Vs Cognitive restructuring | 87 | Various | Adherence to homework was associated with more improvement on the Global Improvement scale. |
| (McDonagh et al., 2005; Possemato et al., 2016) | USA | Primary Care Brief Mindfulness Training
(PCBMT) Cognitive Behavioural Therapy (CBT) |
6274 | Military Trauma Child Sexual Abuse | The ability to describe internal experiences, thoughts emotions and sensations, in non-judgemental way was associated with decrease in PTSD symptoms. Participants who dropped out of CBT endorsed more depression and greater anxiety, reported lower quality of life, and endorsed more distorted schemas on The Traumatic Stress Institute Beliefs Scale (TSI; Pearlman, 2001) than those who stayed in treatment. |
| (Possemato et al., 2016; Schnurr et al., 2003) | USA | Trauma-focused Group Psychotherapy Primary Care Brief Mindfulness Training (PCBMT) | 36,062 | Military Trauma | Individuals who were lost to follow-up had lower Global Assessment of Functioning scores, were more likely to be unemployed and have a lifetime history of substance abuse or dependence. The ability to describe internal experiences, thoughts emotions and sensations, in non-judgemental way was associated with decrease in PTSD symptoms. |
| (Schnurr et al., 2007; Schnurr et al., 2003) | USA | Prolonged Exposure (PE) vs Present-centred therapy (PCT). Trauma-focused Group Psychotherapy | 277,360 | Female Veterans Military Trauma | Participants in Present Centred Therapy received an increase or new medication during the study compared to those in the prolonged exposure group. Exploratory analyses to determine whether medication change during treatment modified the treatment effect for CAPS severity scores indicated that the interaction between medication change and treatment was not significant. Individuals who were lost to follow-up had lower Global Assessment of Functioning scores, were more likely to be unemployed and have a lifetime history of substance abuse or dependence. |
| (Schnurr et al., 2007; Spence et al., 2011) | USA | Internet delivered Cognitive Behavioural Therapy (I-CBT) for PTSD. Prolonged Exposure (PE) vs Present-centred therapy (PCT). | 125,277 | Various Female Veterans | There was no significant relationship between post-treatment outcome the amount of time spent on the homework or with the amount of time spent on thought challenging. Participants in Present Centred Therapy received an increase or new medication during the study compared to those in the prolonged exposure group. Exploratory analyses to determine whether medication change during treatment modified the treatment effect for CAPS severity scores indicated that the interaction between medication change and treatment was not significant. |
| (Spence et al., 2011; Stirman et al., 2018) | USA | Cognitive Processing Therapy
(CPT). Internet delivered Cognitive Behavioural Therapy (I-CBT) for PTSD. |
140,125 | Sexual or physical
violence Various |
Completing homework was associated with a greater decrease in PTSD symptom severity score, as measured by the PTSD symptom scale (PSS). There was no significant relationship between post-treatment outcome the amount of time spent on the homework or with the amount of time spent on thought challenging. |
| (Stapleton et al., 2006; Stirman et al., 2018) | USA | Prolonged Exposure (PE)Cognitive Processing Therapy (CPT). | 60,140 | Various Sexual or physical violence |
No evidence that treatment outcome varied as a function of the pre-treatment severity of anger or guilt. Additional presence of stressors had no associated with treatment outcome. Completing homework was associated with a greater decrease in PTSD symptom severity score, as measured by the PTSD symptom scale (PSS). |
| (Stapleton et al., 2006; Wilson et al., 1995) | USA | Eye Movement Desensitization and Reprocessing (EMDR) Prolonged Exposure (PE) | 8060 | Various | PTSD-I scale symptom severity at baseline, years of education, income, gender, gender of therapist were not associated with treatment outcome. Participants who were married were associated with greater gain. No evidence that treatment outcome varied as a function of the pre-treatment severity of anger or guilt. Additional presence of stressors had no associated with treatment outcome. |
| (Wilson et al., 1995) | USA | Eye Movement Desensitization and Reprocessing (EMDR) | 80 | Various | PTSD-I scale symptom severity at baseline, years of education, income, gender, gender of therapist were not associated with treatment outcome. Participants who were married were associated with greater gain. |
4. Discussion
This was the first systematic review to consider factors associated with treatment outcome of psychological treatments for PTSD. Whilst a number of factors have been found to be associated, the evidence is limited and inconsistent. A comorbid diagnosis of depression and higher levels of PTSD symptom severity at baseline were associated with poor treatment outcome (Hepgul et al., 2016). We also found some evidence that higher education, adherence to homework, and experience of more recent trauma were associated with better treatment outcome.
The association of comorbidity of depression with poor treatment outcome is recognised (National Institute for Health and Care Excellence [NICE], 2018) although the exact mechanism is unknown. One possible explanation (Angelakis & Nixon, 2015) considers emotional processing theory whereby successful treatment depends on the modification of traumatic memory structures that underlie emotions, via activation (engagement) of the fear structure through exposure and subsequent habituation (Jaycox, Foa, & Morral, 1998). Patients are required to emotionally engage during treatment and thus process traumatic memories. An inability to fully experience emotional affect (emotional numbing) in depressed patients may lead to under activation (under engagement) of the fear structure.
Alternatively, depressed patients may be more prone to use avoidance strategies such as overgeneralizing traumatic memories, which inhibit the full experience of negative emotions and successful habitation is prevented (Angelakis & Nixon, 2015). Rumination and overgeneralization may result in an over engagement for those who experience comorbid depression and risk them becoming overwhelmed by the emotional intensity of treatment and reduce its efficacy for PTSD (Rauch & Foa, 2006). It is important to recognize that psychiatric comorbidity might impact treatment planning and outcome.
PTSD symptom severity at baseline was associated with benefiting less from treatment but this was not a uniform finding and several studies found no association of baseline symptom severity and treatment outcome. It has been suggested that marked avoidance can interfere with the processing of the traumatic experiences due to the lack of engagement in therapy (Foa & Kozak, 1986; Resick & Schnicke, 1992) and the association of higher levels of avoidance of thoughts and feelings pre-treatment with higher rates of PTSD symptom severity post-treatment supports this (Gutner, Rizvi, Monson, & Resick, 2006; Krause, Kaltman, Goodman, & Dutton, 2008; Pineles et al., 2011). This suggests a possible need for interventions specifically focused on improving treatment engagement.
Higher education was associated with better treatment outcome. This could be due to the impact of educational background on understanding of psychological interventions and ability to fully engage in them. For example, trauma-focused CBT requires written homework, and more advanced literacy skills may facilitate better outcomes (Fairburn, 1995). Moreover, research has suggested that low educational status is a barrier to adherence to psychological intervention for PTSD because of greater difficulties in understanding the interventions’ content, which may result in a lack of motivation to engage in treatment (Waller & Gilbody, 2009).
Homework adherence was associated with better treatment outcome. People with PTSD vary greatly in their ability to complete homework assignments, due to various factors, including a mismatch between ability and difficulty of the homework assignment, or motivation/commitment on the part of the person with PTSD or the therapist. Strategies for improving participation in homework may increase the potential of completing homework assignments to enhance treatment outcome (NICE, 2018).
More recent trauma was associated with better treatment outcome. One explanation for these findings is that the secondary psychosocial consequences that trauma survivors may experience contribute to the emergence or continuation of other negative events (e.g. unemployment, partner separation and financial difficulties), which can increase PTSD or maintain already existing disorders (Freedy, Kilpatrick, & Resnick, 1993). These events themselves can lead to psychological distress, disruption of social relationships, and other psychosocial difficulties. For example, studies have observed an increase in alcohol and drug use after the experience of a traumatic event (Grieger, Fullerton, & Ursano, 2003), which can increase the likelihood of relapse and clinical worsening of symptoms. Some investigators contend that the post-trauma period can be characterized by an adverse social environment, defined as “a consistent pattern of chronic (negative) impacts to individuals and communities” (Picou, Marshall, & Gill, 2004). A meta-analysis has examined comparative outcomes and acceptability of different PTSD treatments (Merz, Schwarzer, & Gerger, 2019). However, the research was limited to 12 RCTs and, unlike our review, only included studies that directly compared one type of treatment with another. No treatment approach was found to be superior at the end of treatment, although psychotherapeutic treatment shown greater benefit than pharmacological treatment at last follow-up. The lack of long-term findings further limits the research and demonstrates the need for large-scaled comparative trials providing long-term follow-up data.
5. Strengths and limitations
Our work has a number of strengths including its adherence to rigorous systematic review methodological standards and the synthesis of data obtained from RCTs. However, limiting our review to RCTs may have excluded studies with other research designs that may also have reported on associations with treatment outcome. A meta-analysis was not considered appropriate due to the heterogeneity between studies and lack of consistent reporting. An alternative approach is meta-analysis of individual participant data (IPD), in which raw individual level data are obtained and used for synthesis (Simmonds et al., 2005). However, the resources and time required for such analysis is considerable and may limit their use. There are also some issues with the included studies that limit interpretation; for example, they adopted strict inclusion criteria which often excluded patients with active substance dependence, acute suicidal ideation, and major depressive disorder, all of which have been associated with greater severity of PTSD (Back, Brady, Jaanimagi, & Jackson, 2006; Clark, Masson, Delucchi, Hall, & Sees, 2001; Najavits et al., 2003). This may have resulted in the exclusion of participants from more vulnerable and, potentially, treatment-resistant populations, which limits the generalisability of the findings. That said, although the use of more pragmatic inclusion criteria (e.g. patients with substance misuse) may enhance generalizability, it may be difficult to then determine the true effects of the intervention and to whom the results apply. Finally, only the first author extracted and synthesised data from studies. However, data extraction followed the standardised criteria for narrative synthesis (Popay et al., 2006), thereby ensuring a standardised process across studies. Furthermore, frequent meetings with the review team were to discuss progress and interpretation of the results.
Overall, it is difficult to draw firm conclusions from this review due to the limited strength and consistency of evidence for the association of specific factors with treatment outcome. For example, a depression diagnosis and homework adherence were only found to be predictive in two studies, although the evidence was consistent. This contrasts with PTSD symptoms severity where only one of eight studies found an association with poorer outcome, the others finding this was not associated with outcome. Further research is required to determine the true nature of associations found in this review. As the systematic search is over 18 months old, an updated review may also provide additional information.
6. Clinical implications
The review has highlighted a current lack of knowledge in relation to factors associated with the treatment outcome of PTSD. This is further complicated by the inconsistency of reported factors and the variance in treatment outcome among patients with PTSD. It is unreasonable to expect that a simple explanation for variance in treatment outcome will be found for a mental health condition with such clinical and pathophysiological diversity as PTSD (Weathers & Keane, 2007). The results of this review do not suggest that anyone should be excluded from receipt of treatment due to the presence of the factors considered. The association between various factors and treatment outcome that should, however, be taken into account when recommending and delivering specific treatments to people with PTSD. This highlights the need to move to a more personalized treatment approach (Medicine, 2011). Considering the current inconsistency, it is essential to consider other factors that may facilitate personalization of treatments, for example, neuroimaging and cognitive testing in addition to routinely collected clinical characteristics may provide ‘a person with PTSD signature’ that predicts response or non-response to different treatments.
On the basis that co-morbid depression was found to be associated with poor treatment outcome, clinicians should pay particular attention to adapting treatments to individuals’ specific needs, including whether the initial targeting and treatment of PTSD symptoms will subsequently reduce depression symptoms, or whether initial targeting of depressive symptoms is necessary before commencing PTSD treatment. This could determine the best approach for the greatest improvement of both disorders. The findings that higher education was associated with better treatment outcome suggest that particular care should be taken to make treatments fully accessible to people with PTSD with different levels of education. However, this is likely confounded by socioeconomic deprivation and requires further research to better understand the association. It may be that where treatment is ineffective alternative strategies are required such as the provision of additional support or adoption of models that minimize cognitive demand, while maximizing active processing of new information. For example, the use of an adapted form of Eye Movement Desensitisation Reconsolidation (EMDR) to suit the individual’s level of cognitive and emotional functioning has been recommended (Tinker, 1999). This involved a short explanation of the treatment, visual cues instead of abstract language to represent feelings and physical gestures to help communication.
7. Research implications
A clear research implication from our work is the need for further work into the association of factors with PTSD treatment outcome and the reasons for these associations. The importance of exploring and reporting factors associated with treatment outcome cannot be overstated. Future treatment research should: (a) routinely examine and report factors that may be associated with or moderate outcome(s) to allow a better understanding of processes associated with treatment efficacy; (b) assess and report beyond the standard demographic and clinical variable(s) that are thought to influence outcome and consider a translational approach of combining neuroimaging, cognitive and genetic data to form a more detailed clinical phenotype. The direction of associations should also be considered with a view to identifying predictors of treatment outcome. This would provide empirical evidence that could inform the improvement of treatment efficacy, aid the development of new and better treatments and pave the way for a personalized medicine approach to the treatment of PTSD.
Complex PTSD (CPTSD), it is not known whether current established treatment provides the optimal outcome considering the usually prolonged and repeated nature of the trauma in CPTSD, as well as additional symptoms of disturbance of self-organisation. Whilst this review found a study that considered elements of disturbance of self-organisation (DSO) in the context of comorbid Borderline Personality Disorder (BPD), research is required to examine DSO in the context of individuals with a diagnosis of CPTSD to gain a better understanding of the effects of the additional symptoms on treatment outcome.
In order to improve the quality of data on factors associated with treatment outcome, a more universal reporting style must be adopted. The CONsolidated Standards of Reporting Trials (CONSORT) (Bennett, 2005) guidelines were specifically developed to eliminate inadequate reporting of RCTs. However, the guidelines do not address other facets of reporting that may require attention, namely factors associated with treatment outcome. As the CONSORT checklist provides guidelines to improve the completeness of the study, we suggest that the following additional factors are considered for inclusion: (a) characteristics of the participants (age, gender and ethnicity); (b) clinical characteristics (severity, chronicity, comorbidity, and prior treatment exposure), (c) social and economic variables (income, employability, living arrangements); (d) self-efficacy and social support (relationships, family and friends). These factors should be documented at baseline, during and after treatment in order to understand their association to treatment outcome at every stage. In cases of Complex PTSD, consideration of disturbances of self-organization and treatment outcome may also be important for treatment selection (Briere, Kaltman, & Green, 2008; Cloitre et al., 2009). This information will further our understanding of how these observed factors are associated with successful or unsuccessful outcome, and help clinicians and researchers design or adapt evidence-basedd interventions to reduce ineffectiveness.
There is also a need to develop more multidimensional-standardisedd measures of treatment outcome. Traditionally, and importantly, trials have focused on reduction of PTSD symptoms and rates of remission. In addition, measures of the acceptability of the treatment are also required, such as: (a) adherence (consisting of attendance to therapy and homework completion); (b) retention rates (the reasons people continued on with treatment, or withdrew); and (c) attitudes to treatment (to identify patient experiences and perspectives through semi-structured interviews). These additional measures will facilitate consistent reporting and a greater understanding of factors likely to be associated with treatment outcome.
A key research challenge is to develop an evidence base that facilitates a comprehensive understanding of the factors associated with treatment outcome. It is likely that these factors will vary across populations and people but some commonality is to be expected. The factors identified in this systematic review and narrative synthesis provide a useful starting point to meet this challenge and will, hopefully, stimulate the generation of a more rigorous and clinically relevant framework that can inform treatment selection in the future.
It is imperative that future studies explore factors associated with outcome. At this point, it is premature for firm conclusions to be made about the effect of the factors identified on treatment outcome. However, this study represents an important first step in discovering which treatments work best for whom and highlights the need for more research in this area to inform better treatment decisions, the development of better treatments and ultimately to achieve better outcomes.
Acknowledgments
We would like to thank Popay et al. for providing us with their unpublished guidance on narrative synthesis and to the many authors of included studies who responded to our requests for additional information.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Acarturk, C., Konuk, E., Cetinkaya, M., Senay, I., Sijbrandij, M., Gulen, B., & Cuijpers, P. (2016). The efficacy of eye movement desensitization and reprocessing for post-traumatic stress disorder and depression among Syrian refugees: Results of a randomized controlled trial. Psychological Medicine, 46(12), 2583–23. [DOI] [PubMed] [Google Scholar]
- Adenauer, H., Catani, C., Gola, H., Keil, J., Ruf, M., Schauer, M., & Neuner, F. (2011). Narrative exposure therapy for PTSD increases top-down processing of aversive stimuli - evidence from a randomized controlled treatment trial. BMC Neuroscience, 12(127), 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmadi, K., Hazrati, M., Ahmadizadeh, M., & Noohi, S. (2015). REM desensitization as a new therapeutic method for post-traumatic stress disorder: A randomized controlled trial. Acta medica Indonesiana, 47(2), 111–119. [PubMed] [Google Scholar]
- Akbarian, F., Bajoghli, H., Haghighi, M., Kalak, N., Holsboer-Trachsler, E., & Brand, S. (2015). The effectiveness of cognitive behavioral therapy with respect to psychological symptoms and recovering autobiographical memory in patients suffering from post-traumatic stress disorder. Neuropsychiatric Disease and Treatment, 11, 395–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association .(2000). Diagnostic criteria from dsM-iV-tr.. American Psychiatric Pub. [Google Scholar]
- Angelakis, S., & Nixon, R. D. V. (2015). The comorbidity of PTSD and MDD: Implications for clinical practice and future research. Behaviour Change, 32(1), 1–25. [Google Scholar]
- Asukai, N., Saito, A., Tsuruta, N., Kishimoto, J., & Nishikawa, T. (2010). Efficacy of exposure therapy for Japanese patients with posttraumatic stress disorder due to mixed traumatic events: A randomized controlled study. Journal of Traumatic Stress, 23(6), 744–750. Retrieved from http://onlinelibrary.wiley.com/store/10.1002/jts.20589/asset/20589_ftp.pdf?v=1&t=inu4f0rz&s=609604dd8f8c428dcf898427eb63c39666553d5a [DOI] [PubMed] [Google Scholar]
- Back, S. E., Brady, K. T., Jaanimagi, U., & Jackson, J. L. (2006). Cocaine dependence and PTSD: A pilot study of symptom interplay and treatment preferences. Addictive Behaviors, 31(2), 351–354. [DOI] [PubMed] [Google Scholar]
- Barawi K., Lewis C. E., Simon N., Bisson J. I., (2017). A systematic review on factors that are associated with poor treatment outcomes in randomised controlled trials (RCTs) of psychological and pharmacological treatments for individuals with Post Traumatic Stress Disorder (PTSD). Retrieved from https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42017072855
- Basoglu, M., Salcioglu, E., & Livanou, M. (2007). A randomized controlled study of single-session behavioural treatment of earthquake-related post-traumatic stress disorder using an earthquake simulator. Psychological Medicine, 37(2), 203–213. [DOI] [PubMed] [Google Scholar]
- Basoglu, M., Salcioglu, E., Livanou, M., Kalender, D., & Acar, G. (2005). Single-session behavioral treatment of earthquake-related posttraumatic stress disorder: A randomized waiting list controlled trial. Journal of Traumatic Stress, 18(1), 1–11. [DOI] [PubMed] [Google Scholar]
- Beck, J., Coffey, S., Foy, D., Keane, T., & Blanchard, E. (2009). Group cognitive behavior therapy for chronic posttraumatic stress disorder: An initial randomized pilot study. Behavior Therapy, 40(1), 82–92. Retrieved from http://ac.els-cdn.com/S0005789408000506/1-s2.0-S0005789408000506-main.pdf?_tid=ff3103b6-12a7-11e6-b659-00000aacb35e&acdnat=1462442523_d3eb4276230c9a8d7c40d7e76adfecda [DOI] [PubMed] [Google Scholar]
- Bennett, J. A. (2005). The consolidated standards of reporting trials (CONSORT): Guidelines for reporting randomized trials. Nursing Research, 54(2), 128–132. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/15778654 [DOI] [PubMed] [Google Scholar]
- Bichescu, D., Neuner, F., Schauer, M., & Elbert, T. (2007). Narrative exposure therapy for political imprisonment related chronic posttraumatic stress disorder and depression. Behaviour Research and Therapy, 45(9), 2212–2220. Retrieved from http://ac.els-cdn.com/S0005796706002932/1-s2.0-S0005796706002932-main.pdf?_tid=02c379dc-12a8-11e6-9257-00000aab0f02&acdnat=1462442529_bd5ed2eaf588ce2478797f5474138857 [DOI] [PubMed] [Google Scholar]
- Bisson, J. I., Roberts, N. P., Andrew, M., Cooper, R., & Lewis, C. (2013). Psychological therapies for chronic post‐traumatic stress disorder (PTSD) in adults. Cochrane Database of Systematic Reviews (12). doi: 10.1002/14651858.CD003388.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake, D. D., Weathers, F. W., Nagy, L. M., Kaloupek, D. G., Gusman, F. D., Charney, D. S., & Keane, T. M. (1995). The development of a clinician-administered PTSD scale. Journal of Traumatic Stress, 8(1), 75–90. [DOI] [PubMed] [Google Scholar]
- Blanchard, E., Hickling, E., Devineni, T., Veazey, C., Galovski, T., Mundy, E., & Buckley, T. C. (2003). A controlled evaluation of cognitive behaviorial therapy for posttraumatic stress in motor vehicle accident survivors. Behaviour Research and Therapy, 41(1), 79–96. Retrieved from http://ac.els-cdn.com/S0005796701001310/1-s2.0-S0005796701001310-main.pdf?_tid=05adb392-12a8-11e6-940d-00000aacb361&acdnat=1462442534_b3cf188cc83da80cfa3980e0e9f2a319 [DOI] [PubMed] [Google Scholar]
- Bradshaw, R. A., McDonald, M. J., Grace, R., Detwiler, L., & Austin, K. (2014). A randomized clinical trial of observed and experiential integration (OEI): A simple, innovative intervention for affect regulation in clients with PTSD. Traumatology Traumatology: An International Journal, 20(3), 161–171. [Google Scholar]
- Briere, J., Kaltman, S., & Green, B. L. (2008). Accumulated childhood trauma and symptom complexity. Journal of Traumatic Stress, 21(2), 223–226. [DOI] [PubMed] [Google Scholar]
- Brom, D., Kleber, R., & Defares, P. (1989). Brief psychotherapy for posttraumatic stress disorders. Journal of Consulting and Clinical Psychology, 57(5), 607–612. [DOI] [PubMed] [Google Scholar]
- Bryant, R., Moulds, M., Guthrie, R., & Dang, S. (2003). Imaginal exposure alone and imaginal exposure with cognitive restructuring in treatment of posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 71(4), 706–712. Retrieved from http://ovidsp.tx.ovid.com/ovftpdfs/FPDDNCLBAHADBG00/fs046/ovft/live/gv023/00004730/00004730-200308000-00009.pdf [DOI] [PubMed] [Google Scholar]
- Bryant, R. A., Ekasawin, S., Chakrabhand, S., Suwanmitri, S., Duangchun, O., & Chantaluckwong, T. (2011). A randomized controlled effectiveness trial of cognitive behavior therapy for post‐traumatic stress disorder in terrorist‐affected people in Thailand. World Psychiatry: Official Journal of the World Psychiatric Association (WPA), 10(3), 205–209. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3188775/pdf/wpa030205.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buhmann, C., Nordentoft, M., Ekstroem, M., Carlsson, J., & Mortensen, E. (2016). The effect of flexible cognitive-behavioural therapy and medical treatment, including antidepressants on post-traumatic stress disorder and depression in traumatised refugees: Pragmatic randomised controlled clinical trial. The British Journal of Psychiatry, 208(3), 252–259. [DOI] [PubMed] [Google Scholar]
- Butollo, W., Karl, R., König, J., & Rosner, R. (2016). A randomized controlled clinical trial of dialogical exposure therapy versus cognitive processing therapy for adult outpatients suffering from PTSD after type I trauma in adulthood. Psychotherapy and Psychosomatics, 85(1), 16–26. [DOI] [PubMed] [Google Scholar]
- Capezzani, L., Ostacoli, L., Cavallo, M., Carletto, S., Fernandez, I., Solomon, R., … Cantelmi, T. (2013). EMDR and CBT for cancer patients: Comparative study of effects on PTSD, anxiety, and depression. Journal of EMDR Practice and Research, 7(3), 134–143. [Google Scholar]
- Carletto, S., Borghi, M., Bertino, G., Oliva, F., Cavallo, M., Hofmann, A., & Ostacoli, L. (2016). Treating post-traumatic stress disorder in patients with multiple sclerosis: A randomized controlled trial comparing the efficacy of eye movement desensitization and reprocessing and relaxation therapy. Frontiers in Psychology, 7. doi: 10.3389/fpsyg.2016.00526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson, J., Chemtob, C., Rusnak, K., Hedlund, N., & Muraoka, M. (1998). Eye movement desensitization and reprocessing (EDMR) treatment for combat-related posttraumatic stress disorder. Journal of Traumatic Stress, 11(1), 3–32. Retrieved from http://onlinelibrary.wiley.com/store/10.1023/A:1024448814268/asset/2_ftp.pdf?v=1&t=inu4f8xg&s=1d73d505262fea18b649526c049e6ccc5f49b622 [DOI] [PubMed] [Google Scholar]
- Castillo, D. T., Chee, C. L., Nason, E., Keller, J., C’de Baca, J., Qualls, C., … Keane, T. M. (2016). Group-delivered cognitive/exposure therapy for PTSD in women veterans: A randomized controlled trial. Psychological Trauma: Theory, Research, Practice and Policy, (3). doi: 10.1037/tra0000111 [DOI] [PubMed] [Google Scholar]
- Chandler, J., Churchill, R., Higgins, J., Lasserson, T., & Tovey, D. (2012). Methodological standards for the conduct of new cochrane intervention reviews. 2.2. Retrieved from http://www.editorial-unit.cochrane.org/sites/editorial-unit.cochrane.org/files/uploads/MECIR_conduct_standards%202.2%2017122012.pdf
- Chard, K. M. (2005). An evaluation of cognitive processing therapy for the treatment of posttraumatic stress disorder related to childhood sexual abuse. Journal of Consulting and Clinical Psychology, 73(5), 965. Retrieved from http://ovidsp.tx.ovid.com/ovftpdfs/FPDDNCLBAHADBG00/fs047/ovft/live/gv024/00004730/00004730-200510000-00019.pdf [DOI] [PubMed] [Google Scholar]
- Clark, H. W., Masson, C. L., Delucchi, K. L., Hall, S. M., & Sees, K. L. (2001). Violent traumatic events and drug abuse severity. Journal of Substance Abuse Treatment, 20(2), 121–127. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/11306214 [DOI] [PubMed] [Google Scholar]
- Cloitre, M., Koenen, K. C., Cohen, L. R., & Han, H. (2002). Skills training in affective and interpersonal regulation followed by exposure: A phase-based treatment for PTSD related to childhood abuse. Journal of Consulting and Clinical Psychology, 70(5), 1067–1074. [DOI] [PubMed] [Google Scholar]
- Cloitre, M., Petkova, E., Su, Z., & Weiss, B. (2016). Patient characteristics as a moderator of post-traumatic stress disorder treatment outcome: Combining symptom burden and strengths. BJPsych Open, 2(2), 101–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloitre, M., Stolbach, B. C., Herman, J. L., van der Kolk, B., Pynoos, R., Wang, J., & Petkova, E. (2009). A developmental approach to complex PTSD: Childhood and adult cumulative trauma as predictors of symptom complexity. Journal of Traumatic Stress, 22(5), 399–408. [DOI] [PubMed] [Google Scholar]
- Cloitre, M., Stovall-McClough, K. C., Nooner, K., Zorbas, P., Cherry, S., Jackson, C. L., … Petkova, E. (2010). Treatment for PTSD related to childhood abuse: A randomized controlled trial. American Journal of Psychiatry, 167(8), 915–924. [DOI] [PubMed] [Google Scholar]
- Coffey, S. F., Stasiewicz, P. R., Hughes, P. M., & Brimo, M. L. (2006). Trauma-focused imaginal exposure for individuals with comorbid posttraumatic stress disorder and alcohol dependence: Revealing mechanisms of alcohol craving in a cue reactivity paradigm. Psychology of Addictive Behaviors, 20(4), 425–435. [DOI] [PubMed] [Google Scholar]
- Cooper, A. A., Zoellner, L. A., Roy-Byrne, P., Mavissakalian, M. R., & Feeny, N. C. (2017). Do changes in trauma-related beliefs predict PTSD symptom improvement in prolonged exposure and sertraline? Journal of Consulting and Clinical Psychology, 85(9), 873–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper, N. A., & Clum, G. A. (1989). Imaginal flooding as a supplementary treatment for PTSD in combat veterans: A controlled study. Behavior Therapy, 20(3), 381–391. [Google Scholar]
- Devilly, G., Spence, S., & Rapee, R. (1998). Statistical and reliable change with eye movement desensitization and reprocessing: Treating trauma within a veteran population. Behavior Therapy, 29(3), 435–455. [Google Scholar]
- Devilly, G. J., & Spence, S. H. (1999). The relative efficacy and treatment distress of EMDR and a cognitive-behavior trauma treatment protocol in the amelioration of posttraumatic stress disorder. Journal of Anxiety Disorders, 13(1–2), 131–157. [DOI] [PubMed] [Google Scholar]
- Dorrepaal, E., Thomaes, K., Smit, J., van Balkom, A., Veltman, D., Hoogendoorn, A., & Draijer, N. (2012). Stabilizing group treatment for complex posttraumatic stress disorder related to child abuse based on psychoeducation and cognitive behavioural therapy: A multisite randomized controlled trial. Psychotherapy and Psychosomatics, 81(4), 217–225. [DOI] [PubMed] [Google Scholar]
- Duffy, M., Gillespie, K., & Clark, D. (2007). Post-traumatic stress disorder in the context of terrorism and other civil conflict in Northern Ireland: Randomised controlled trial. British Medical Journal, 334(7604), 1147–1150. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1885307/pdf/bmj-334-7604-res-01147-el.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunne, R. L., Kenardy, J., & Sterling, M. (2012). A randomized controlled trial of cognitive-behavioral therapy for the treatment of PTSD in the context of chronic whiplash. The Clinical Journal of Pain, 28(9), 755–765. Retrieved from http://ovidsp.tx.ovid.com/ovftpdfs/FPDDNCLBAHADBG00/fs047/ovft/live/gv024/00002508/00002508-201211000-00002.pdf [DOI] [PubMed] [Google Scholar]
- Durham, R. C., Chambers, J. A., Power, K. G., Sharp, D. M., Macdonald, R. R., Major, K. A., … Gumley, A. I. (2005). Long-term outcome of cognitive behaviour therapy clinical trials in central Scotland. Health Technology Assessment, 9(42), 1–174. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/16266559 [DOI] [PubMed] [Google Scholar]
- Echeburua, E., De Corral, P., Zubizarreta, I., & Sarasua, B. (1997). Psychological treatment of chronic posttraumatic stress disorder in victims of sexual aggression. Behavior Modification, 21(4), 433–456. [DOI] [PubMed] [Google Scholar]
- Ehlers, A., Clark, D., Hackman, A., McManus, F., & Fennell, M. (2005). Cognitive therapy for post-traumatic stress disorder: Development and evaluation. Behaviour Research and Therapy, 43(4), 413–431. Retrieved from http://ac.els-cdn.com/S0005796704000889/1-s2.0-S0005796704000889-main.pdf?_tid=17a415c8-12a8-11e6-940d-00000aacb361&acdnat=1462442564_d80a820e16981bb647deacff10f75746 [DOI] [PubMed] [Google Scholar]
- Ehlers, A., & Clark, D. M. (2008). Post-traumatic stress disorder: The development of effective psychological treatments. Nordic Journal of Psychiatry, 62(Suppl sup47), 11–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers, A., Clark, D. M., Hackmann, A., McManus, F., Fennell, M., Herbert, C., & Mayou, R. (2003). A randomized controlled trial of cognitive therapy, a self-help booklet, and repeated assessments as early interventions for posttraumatic stress disorder. Archives of General Psychiatry, 60(10), 1024–1032. Retrieved from http://archpsyc.jamanetwork.com/data/Journals/PSYCH/5191/YOA20730.pdf [DOI] [PubMed] [Google Scholar]
- Ehlers, A., Hackmann, A., Grey, N., Wild, J., Liness, S., Albert, I., … Clark, D. M. (2014). A randomized controlled trial of 7-day intensive and standard weekly cognitive therapy for PTSD and emotion-focused supportive therapy. American Journal of Psychiatry, 171(3), 294–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn, C. G. 1995. Overcoming Binge Eating(pp. 44). New York: Guildford press. [Google Scholar]
- Falsetti, S., Resnick, H., & Davis, J. (2008). Multiple channel exposure therapy for women with PTSD and comorbid panic attacks. Cognitive Behaviour Therapy, 37(2), 117–130. [DOI] [PubMed] [Google Scholar]
- Fecteau, G., & Nicki, R. (1999). Cognitive behavioural treatment of post traumatic stress disorder after motor vehicle accident. Behavioural and Cognitive Psychotherapy, 27(3), 201–214. [Google Scholar]
- Feske, U. (2008). Treating low-income and minority women with posttraumatic stress disorder a pilot study comparing prolonged exposure and treatment as usual conducted by community therapists. Journal of Interpersonal Violence, 23(8), 1027–1040. Retrieved from http://jiv.sagepub.com/content/23/8/1027.full.pdf [DOI] [PubMed] [Google Scholar]
- Foa, E., Dancu, C., Hembree, E., Jaycox, L., Meadows, E., & Street, G. (1999). A comparison of exposure therapy, stress inoculation training, and their combination for reducing posttraumatic stress disorder in female assault victims. Journal of Consulting and Clinical Psychology, 67(2), 194–200. Retrieved from http://ovidsp.tx.ovid.com/ovftpdfs/FPDDNCLBAHADBG00/fs046/ovft/live/gv023/00004730/00004730-199904000-00004.pdf [DOI] [PubMed] [Google Scholar]
- Foa, E., McLean, C., Zang, Y., Rosenfield, D., Yadin, E., Yarvis, J., … Peterson, A. (2018). Effect of prolonged exposure therapy delivered over 2 weeks vs 8 weeks vs present-centered therapy on PTSD symptom severity in military personnel: A randomized clinical trial. Jama, 319(4), 354–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa, E., Rothbaum, B., Riggs, D., & Murdock, T. (1991). Treatment of posttraumatic stress disorder in rape victims: A comparison between cognitive-behavioral procedures and counseling. Journal of Consulting and Clinical Psychology, 59(5), 715–723. Retrieved from http://ovidsp.tx.ovid.com/ovftpdfs/FPDDNCLBAHADBG00/fs046/ovft/live/gv023/00004730/00004730-199110000-00010.pdf [DOI] [PubMed] [Google Scholar]
- Foa, E. B. (2011). Prolonged exposure therapy: Past, present, and future. Depression and Anxiety, 28(12), 1043–1047. [DOI] [PubMed] [Google Scholar]
- Foa, E. B., Hembree, E. A., Cahill, S. P., Rauch, S. A., Riggs, D. S., Feeny, N. C., & Yadin, E. (2005). Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: Outcome at academic and community clinics. Journal of Consulting and Clinical Psychology, 73(5), 953–964. [DOI] [PubMed] [Google Scholar]
- Foa, E. B., & Kozak, M. J. (1986). Emotional processing of fear: Exposure to corrective information. Psychological Bulletin, 99(1), 20–35. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/2871574 [PubMed] [Google Scholar]
- Fonzo, G., Goodkind, M., Oathes, D., Zaiko, Y., Harvey, M., Peng, K., … Etkin, A. (2017). PTSD psychotherapy outcome predicted by brain activation during emotional reactivity and regulation. American Journal of Psychiatry, 174(12), 1163–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes, D., Lloyd, D., Nixon, R., Elliott, P., Varker, T., Perry, D., … Creamer, M. (2012). A multisite randomized controlled effectiveness trial of cognitive processing therapy for military-related posttraumatic stress disorder. Journal of Anxiety Disorders, 26(3), 442–452. Retrieved from http://ac.els-cdn.com/S0887618512000114/1-s2.0-S0887618512000114-main.pdf?_tid=35fb9834-12a8-11e6-82af-00000aab0f6b&acdnat=1462442615_64a90ee18e2008a5a0220abc5baa4e2b [DOI] [PubMed] [Google Scholar]
- Ford, J. D., Chang, R., Levine, J., & Zhang, W. (2013). Randomized clinical trial comparing affect regulation and supportive group therapies for victimization-related PTSD with incarcerated women. Behavior Therapy, 44(2), 262–276. [DOI] [PubMed] [Google Scholar]
- Ford, J. D., Steinberg, K. L., & Zhang, W. (2011). A randomized clinical trial comparing affect regulation and social problem-solving psychotherapies for mothers with victimization-related PTSD. Behavior Therapy, 42(4), 560–578. [DOI] [PubMed] [Google Scholar]
- Freedy, J. R., Kilpatrick, D. G., & Resnick, H. S. (1993). Natural disasters and mental-health - theory, assessment, and intervention. Journal of Social Behavior and Personality, 8(5), 49–103. [Google Scholar]
- Galovski, T. E., Blain, L. M., Mott, J. M., Elwood, L., & Houle, T. (2012). Manualized therapy for PTSD: Flexing the structure of cognitive processing therapy. Journal of Consulting and Clinical Psychology, 80(6), 968–981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamito, P., Oliveira, J., Rosa, P., Morais, D., Duarte, N., Oliveira, S., & Saraiva, T. (2010). PTSD elderly war veterans: A clinical controlled pilot study. Cyberpsychology, Behavior and Social Networking, 13(1), 43–48. [DOI] [PubMed] [Google Scholar]
- Gersons, B. P., Lamberts, R. D., & Van der Kolk, B. A. (2000). Randomized clinical trial of brief eclectic psychotherapy for police officers with posttraumatic stress disorder. Journal of Traumatic Stress, 13(2), 333–347. Retrieved from http://onlinelibrary.wiley.com/store/10.1023/A:1007793803627/asset/208_ftp.pdf?v=1&t=inu4h938&s=fbefa6e2829ab98a6b355f6eb37f832920f717dd [DOI] [PubMed] [Google Scholar]
- Gray R., Budden-Potts D., Bourke F. (2019). Reconsolidation of Traumatic Memories for PTSD: A randomized controlled trial of 74 male veterans [published correction appears in Psychother Res. 2019. February;29(2):277]. Psychother Res. 29(5), 621–639. doi: 10.1080/10503307.2017.1408973 [DOI] [PubMed] [Google Scholar]
- Grieger, T. A., Fullerton, C. S., & Ursano, R. J. (2003). Posttraumatic stress disorder, alcohol use, and perceived safety after the terrorist attack on the Pentagon. Psychiatric Services, 54(10), 1380–1382. [DOI] [PubMed] [Google Scholar]
- Gutner, C. A., Rizvi, S. L., Monson, C. M., & Resick, P. A. (2006). Changes in coping strategies, relationship to the perpetrator, and posttraumatic distress in female crime victims. Journal of Traumatic Stress, 19(6), 813–823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haagen, J. F., Ter Heide, F. J., Mooren, T. M., Knipscheer, J. W., & Kleber, R. J. (2017). Predicting post-traumatic stress disorder treatment response in refugees: Multilevel analysis. British Journal of Clinical Psychology, 56(1), 69–83. [DOI] [PubMed] [Google Scholar]
- Hall, K. S., Morey, M. C., Bosworth, H. B., Beckham, J. C., Pebole, M. M., Sloane, R., & Pieper, C. F. (2019). Pilot randomized controlled trial of exercise training for older veterans with PTSD. Journal of Behavioral Medicine. doi: 10.1007/s10865-019-00073-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hensel-Dittmann, D., Schauer, M., Ruf, M., Catani, C., Odenwald, M., Elbert, T., & Neuner, F. (2011). Treatment of traumatized victims of war and torture: A randomized controlled comparison of narrative exposure therapy and stress inoculation training. Psychotherapy and Psychosomatics, 80(6), 345–352. [DOI] [PubMed] [Google Scholar]
- Hepgul, N., King, S., Amarasinghe, M., Breen, G., Grant, N., Grey, N., … Cleare, A. J. (2016). Clinical characteristics of patients assessed within an improving access to psychological therapies (IAPT) service: Results from a naturalistic cohort study (predicting outcome following psychological therapy; PROMPT). BMC Psychiatry, 16(1), 52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hien, D. A., Lopez-Castro, T., Papini, S., Gorman, B., & Ruglass, L. M. (2017). Emotion dysregulation moderates the effect of cognitive behavior therapy with prolonged exposure for co-occurring PTSD and substance use disorders. Journal of Anxiety Disorders, 52, 53–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinton, D., Chhean, D., Pich, V., Safren, S. A., Hofmann, S. G., & Pollack, M. H. (2005). A randomised controlled trial of cognitive behaviour therapy for Cambodian refugees with treatment resistant PTSD and panic attacks: A cross over design. Journal of Traumatic Stress, 18(6), 617–629. Retrieved from http://onlinelibrary.wiley.com/store/10.1002/jts.20070/asset/20070_ftp.pdf?v=1&t=inu4hma3&s=9995ebbb5a4e2c3c32cc58a5863884bbb9396542 [DOI] [PubMed] [Google Scholar]
- Hinton, D. E., Hofmann, S. G., Rivera, E., Otto, M. W., & Pollack, M. H. (2011). Culturally adapted CBT (CA-CBT) for Latino women with treatment-resistant PTSD: A pilot study comparing CA-CBT to applied muscle relaxation. Behaviour Research and Therapy, 49(4), 275–280. Retrieved from http://ac.els-cdn.com/S0005796711000222/1-s2.0-S0005796711000222-main.pdf?_tid=51084d52-12a8-11e6-af31-00000aacb360&acdnat=1462442660_27bb9e3ec361f8475b9c98d4a1f42a27 [DOI] [PubMed] [Google Scholar]
- Hogberg, G., Pagani, M., Sundin, O., Soares, J., Aberg-Wistedt, A., Tarnell, B., & Hallstrom, T. (2007). On treatment with eye movement desensitization and reprocessing of chronic post-traumatic stress disorder in public transportation workers - a randomized controlled trial. Nordic Journal of Psychiatry, 61(1), 54–60. [DOI] [PubMed] [Google Scholar]
- Hollifield, M., Sinclair-Lian, N., Warner, T. D., & Hammerschlag, R. (2007). Acupuncture for posttraumatic stress disorder. The Journal of Nervous and Mental Disease, 195(6), 504–513. [DOI] [PubMed] [Google Scholar]
- International Society of Traumatic Stress Studies (ISTSS) [Online] . (2018). New ISTSS prevention and treatment guidelines. Retrieved from http://www.istss.org/treating-trauma/new-istss-guidelines.aspx
- Ironson, G., Freund, B., Strauss, J. L., & Williams, J. (2002). Comparison of two treatments for traumatic stress: A community based study of EMDR and prolonged exposure. Journal of Clinical Psychology, 58(1), 113–128. Retrieved from http://onlinelibrary.wiley.com/store/10.1002/jclp.1132/asset/1132_ftp.pdf?v=1&t=inu4i1d3&s=31fab01489e1644b5acf8b8d0d9651c08c208ce1 [DOI] [PubMed] [Google Scholar]
- Ivarsson, D., Blom, M., Hesser, H., Carlbring, P., Enderby, P., Nordberg, R., & Andersson, G. (2014). Guided internet-delivered cognitive behavior therapy for post-traumatic stress disorder: A randomized controlled trial. Internet Interventions, 1(1), 33–40. [Google Scholar]
- Jacob, N., Neuner, F., Maedl, A., Schaal, S., & Elbert, T. (2014). Dissemination of psychotherapy for trauma spectrum disorders in postconflict settings: A randomized controlled trial in Rwanda. Psychotherapy and Psychosomatics, 83(6), 354–363. [DOI] [PubMed] [Google Scholar]
- Jaycox, L. H., Foa, E. B., & Morral, A. R. (1998). Influence of emotional engagement and habituation on exposure therapy for PTSD. Journal of Consulting and Clinical Psychology, 66(1), 185–192. [DOI] [PubMed] [Google Scholar]
- Jensen, J. (1994). An investigation of eye movement desensitisation and reprocessing as a treatment for posttraumatic stress disorder symptoms of vietnam combat veterans. Behavior Therapy, 25(2), 311–325. [Google Scholar]
- Johnson, D., Johnson, N., Perez, S., Palmieri, P., & Zlotnick, C. (2016). Comparison of adding treatment of PTSD during and after shelter stay to standard care in residents of battered women’s shelters: Results of a randomized clinical trial. Journal of Traumatic Stress, 29(4), 365–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson, D. M., Zlotnick, C., & Perez, S. (2011). Cognitive behavioral treatment of PTSD in residents of battered women’s shelters: Results of a randomized clinical trial. Journal of Consulting and Clinical Psychology, 79(4), 542–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karatzias, A., Power, K., McGoldrick, T., Brown, K., Buchanan, R., Sharp, D., & Swanson, V. (2007). Predicting treatment outcome on three measures for post-traumatic stress disorder. European Archives of Psychiatry and Clinical Neuroscience, 257(1), 40–46. [DOI] [PubMed] [Google Scholar]
- Karatzias, T., Power, K., Brown, K., McGoldrick, T., Begum, M., Young, J., … Adams, S. (2011). A controlled comparison of the effectiveness and efficiency of two psychological therapies for posttraumatic stress disorder: Eye movement desensitization and reprocessing vs. emotional freedom techniques. The Journal of Nervous and Mental Disease, 199(6), 372–378. [DOI] [PubMed] [Google Scholar]
- Keane, T., Fairbank, J. A., Caddell, J. M., & Zimering, R. T. (1989). Implosive (flooding) therapy reduces symptoms of PTSD in Vietnam combat veterans. Behavior Therapy, 20(2), 245–260. [Google Scholar]
- Kearney, D. J., Malte, C. A., McManus, C., Martinez, M. E., Felleman, B., Simpson, T. L. (2013). Loving-kindness meditation for posttraumatic stress disorder: a pilot study. J Trauma Stress. 26(4), 426–434. doi: 10.1002/jts.21832 [DOI] [PubMed] [Google Scholar]
- Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry, 62(6), 593–602. [DOI] [PubMed] [Google Scholar]
- Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M., & Nelson, C. B. (1995). Posttraumatic stress disorder in the national comorbidity survey. Archives of General Psychiatry, 52(12), 1048–1060. Retrieved from http://archpsyc.jamanetwork.com/article.aspx?articleid=497313 [DOI] [PubMed] [Google Scholar]
- Krakow, B., Hollifield, M., Schrader, R., Koss, M., Tandberg, D., Lauriello, J., … Kellner, R. (2000). A controlled study of imagery rehearsal for chronic nightmares in sexual assault survivors with PTSD: A preliminary report. Journal of Traumatic Stress, 13(4), 589–609. [DOI] [PubMed] [Google Scholar]
- Krause, E. D., Kaltman, S., Goodman, L. A., & Dutton, M. A. (2008). Avoidant coping and PTSD symptoms related to domestic violence exposure: A longitudinal study. Journal of Traumatic Stress, 21(1), 83–90. [DOI] [PubMed] [Google Scholar]
- Krupnick, J. L., Green, B. L., Stockton, P., Miranda, J., Krause, E., & Mete, M. (2008). Group interpersonal psychotherapy for low-income women with posttraumatic stress disorder. Psychotherapy Research, 18(5), 497–507. [DOI] [PubMed] [Google Scholar]
- Kubany, E., Hill, E., Owens, J., Iannce-Spencer, C., McCaig, M. A., Tremayne, K. J., & Williams, P. L. (2004). Cognitive trauma therapy for battered women with PTSD (CTT-BW). Journal of Consulting and Clinical Psychology, 72(1), 3–18. Retrieved from http://ovidsp.tx.ovid.com/ovftpdfs/FPDDNCLBAHADBG00/fs046/ovft/live/gv023/00004730/00004730-200402000-00001.pdf [DOI] [PubMed] [Google Scholar]
- Kubany, E., Hill, E. E., & Owens, J. A. (2003). Cognitive trauma therapy for battered women with PTSD: Preliminary findings. Journal of Traumatic Stress, 16(1), 81–91. Retrieved from http://onlinelibrary.wiley.com/store/10.1023/A:1022019629803/asset/311_ftp.pdf?v=1&t=inu4ibzk&s=7ac80529ebd3a9c7159b45637f6da593de46392e [DOI] [PubMed] [Google Scholar]
- Laugharne, J., Kullack, C., Lee, C., McGuire, T., Brockman, S., Drummond, P., & Starkstein, S. (2016). Amygdala volumetric change following psychotherapy for posttraumatic stress disorder, The Journal of Neuropsychiatry and Clinical Neurosciences, 28(4), 312–318. [DOI] [PubMed] [Google Scholar]
- Lee, C., Gavriel, H., Drummond, P., Richards, J., & Greenwald, R. (2002). Treatment of PTSD: Stress inoculation training with prolonged exposure compared to EMDR. Journal of Clinical Psychology, 58(9), 1071–1089. Retrieved from http://onlinelibrary.wiley.com/store/10.1002/jclp.10039/asset/10039_ftp.pdf?v=1&t=inu4ijzv&s=cb7d7061ee05d229988f0a1ebf73d3fc2b6d2cb5 [DOI] [PubMed] [Google Scholar]
- Lewis, C. E., Farewell, D., Groves, V., Kitchiner, N. J., Roberts, N. P., Vick, T., & Bisson, J. I. (2017). Internet-based guided self-help for posttraumatic stress disorder (PTSD): Randomized controlled trial. Depression and Anxiety, 34(6), 555–565. [DOI] [PubMed] [Google Scholar]
- Lindauer, R. J., Vlieger, E.-J., Jalink, M., Olff, M., Carlier, I. V., Majoie, C. B., … Gersons, B. P. (2005). Effects of psychotherapy on hippocampal volume in out-patients with post-traumatic stress disorder: A MRI investigation. Psychological Medicine, 35(10), 1421–1431. [DOI] [PubMed] [Google Scholar]
- Littleton, H., Grills, A. E., Kline, K. D., Schoemann, A. M., & Dodd, J. C. (2016). The from survivor to thriver program: RCT of an online therapist-facilitated program for rape-related PTSD. Journal of Anxiety Disorders, 43, 41–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litz, B. T., Engel, C. C., Bryant, R. A., & Papa, A. (2007). A randomized, controlled proof-of-concept trial of an internet-based, therapist-assisted self-management treatment for posttraumatic stress disorder. American Journal of Psychiatry, 164(11), 1676–1683. [DOI] [PubMed] [Google Scholar]
- Marcus, S., Marquis, P., & Sakai, C. (1997). Controlled study of treatment of PTSD using EMDR in an HMO setting. Psychotherapy Theory, Research and Practice, 34(3), 307–315. [Google Scholar]
- Markowitz, J., Petkov, A. E., Neria, Y., Van Meter, P., Zhao, Y., Hembree, E., … Marshall, R. (2015). Is exposure necessary? A randomized clinical trial of interpersonal psychotherapy for PTSD. American Journal of Psychiatry, 172(5), 430–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marks, I., Lovell, K., Noshirvani, H., Livanou, M., & Thrasher, S. (1998). Treatment of posttraumatic stress disorder by exposure and/or cognitive restructuring: A controlled study. Archives of General Psychiatry, 55(4), 317–325. Retrieved from http://archpsyc.jamanetwork.com/data/Journals/PSYCH/4686/yoa6362.pdf [DOI] [PubMed] [Google Scholar]
- McDonagh, A., Friedman, M., McHugo, G., Ford, J., Sengupta, A., Mueser, K., … Descamps, M. (2005). Randomized trial of cognitive-behavioral therapy for chronic posttraumatic stress disorder in adult female survivors of childhood sexual abuse. Journal of Consulting and Clinical Psychology, 73(3), 515–524. [DOI] [PubMed] [Google Scholar]
- McLay, R., Baird, A., Webb-Murphy, J., Deal, W., Tran, L., Anson, H., … Johnston, S. (2017). A randomized, head-to-head study of virtual reality exposure therapy for posttraumatic stress disorder. Cyberpsychology, Behavior and Social Networking, 20(4), 218–224. [DOI] [PubMed] [Google Scholar]
- McLay, R., Wood, D., Webb-Murphy, J., Spira, J., Wiederhold, M., Pyne, J., & Wiederhold, B. (2011). A randomized, controlled trial of virtual reality-graded exposure therapy for post-traumatic stress disorder in active duty service members with combat-related post-traumatic stress disorder. Cyberpsychology, Behavior, and Social Networking, 14(4), 223–229. [DOI] [PubMed] [Google Scholar]
- Merz, J., Schwarzer, G., & Gerger, H. (2019). Comparative efficacy and acceptability of pharmacological, psychotherapeutic, and combination treatments in adults with posttraumatic stress disorder: A network meta-analysis. JAMA Psychiatry (Chicago, Ill.), 76(9), 904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyahira, S. D., Folen, R. A., Hoffman, H. G., Garcia-Palacios, A., Spira, J. L., & Kawasaki, M. (2012). The effectiveness of VR exposure therapy for PTSD in returning warfighters.. Studies in Health technology and Informatics, 181, 128–132. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/22954842 [PubMed] [Google Scholar]
- Monson, C., Fredman, S., Macdonald, A., Pukay Martin, N., Resick, P., & Schnurr, P. (2012, August 15). Effect of cognitive-behavioral couple therapy for PTSD: A randomized controlled trial. JAMA, 308(7), 700–709. PMID: 22893170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monson, C., Schnurr, P. P., Resick, P. A., Friedman, M. J., Young-Xu, Y., & Stevens, S. P. (2006). Cognitive processing therapy for veterans with military related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 74(5), 898–907. Retrieved from http://ovidsp.tx.ovid.com/ovftpdfs/FPDDNCLBAHADBG00/fs047/ovft/live/gv024/00004730/00004730-200610000-00011.pdf [DOI] [PubMed] [Google Scholar]
- Morath, J., Moreno-Villanueva, M., Hamuni, G., Kolassa, S., Ruf-Leuschner, M., Schauer, M., … Kolassa, I. (2014). Effects of psychotherapy on DNA strand break accumulation originating from traumatic stress. Psychotherapy and Psychosomatics, 83(5), 289–297. [DOI] [PubMed] [Google Scholar]
- Mueser, K. T., Rosenberg, S. D., Xie, H., Jankowski, M. K., Bolton, E. E., Lu, W., … McHugo, G. J. (2008). A randomized controlled trial of cognitive-behavioral treatment for posttraumatic stress disorder in severe mental illness. Journal of Consulting and Clinical Psychology, 76(2), 259–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nacasch, N., Foa, E., Huppert, J., Tzur, D., Fostick, L., Dinstein, Y., … Zohar, J. (2011). Prolonged exposure therapy for combat- and terror-related posttraumatic stress disorder: A randomized control comparison with treatment as usual NCT00229372. The Journal of Clinical Psychiatry, 72(9), 1174–1180. [DOI] [PubMed] [Google Scholar]
- Najavits, L. M., Runkel, R., Neuner, C., Frank, A. F., Thase, M. E., Crits-Christoph, P., & Blaine, J. (2003). Rates and symptoms of PTSD among cocaine-dependent patients.. Journal of Studies on Alcohol, 64(5), 601–606. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/14572180 [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence (NICE) . (2018). Post-traumatic stress disorder (NICE guideline NG116). Retrieved from https://www.nice.org.uk/guidance/ng116. [PubMed]
- National Research Council . (2011). Toward precision medicine:Building a knowledge network for biomedical research and a new taxonomy of disease. National Academies Press. [PubMed] [Google Scholar]
- Neuner, F., Kurreck, S., Ruf, M., Odenwald, M., Elbert, T., & Schauer, M. (2010). Can asylum seekers with posttraumatic stress disorder be successfully treated? Cognitive Behaviour Therapy, 39(2), 81–91. [DOI] [PubMed] [Google Scholar]
- Neuner, F., Onyut, P. L., Ertl, V., Odenwald, M., Schauer, E., & Elbert, T. (2008). Treatment of posttraumatic stress disorder by trained lay counselors in an African refugee settlement: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 76(4), 686. Retrieved from http://ovidsp.tx.ovid.com/ovftpdfs/FPDDNCLBAHADBG00/fs046/ovft/live/gv023/00004730/00004730-200808000-00014.pdf [DOI] [PubMed] [Google Scholar]
- Neuner, F., Schauer, M., Klaschik, C., Karunakara, U., & Elbert, T. (2004). A comparison of narrative exposure therapy, supportive counselling, and psychoeducation for treating posttraumatic stress disorder in an African refugee settlement. Journal of Consulting and Clinical Psychology, 72(4), 579–587. Retrieved from http://ovidsp.tx.ovid.com/ovftpdfs/FPDDNCLBAHADBG00/fs046/ovft/live/gv023/00004730/00004730-200408000-00003.pdf [DOI] [PubMed] [Google Scholar]
- Nijdam, M. J., Gersons, B. P., Reitsma, J. B., de Jongh, A., & Olff, M. (2012). Brief eclectic psychotherapy v. eye movement desensitisation and reprocessing therapy for post-traumatic stress disorder: Randomised controlled trial. British Journal of Psychiatry, 200(3), 224–231. [DOI] [PubMed] [Google Scholar]
- Pacella, M. L., Armelie, A., Boarts, J., Wagner, G., Jones, T., Feeny, N., & Delahanty, D. L. (2012). The impact of prolonged exposure on PTSD symptoms and associated psychopathology in people living with HIV: A randomized test of concept. AIDS and Behavior, 16(5), 1327–1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paunovic, N. (2011). Exposure inhibition therapy as a treatment for chronic posttraumatic stress disorder: A controlled pilot study. Psychology, 2(6), 605. [Google Scholar]
- Peniston, E. G., & Kulkosky, P. J. (1991). Alpha-theta brainwave neurofeedback for Vietnam veterans with combat-related post-traumatic stress disorder. Medical Psychotherapy, 4(1), 47–60. [Google Scholar]
- Picou, J. S., Marshall, B. K., & Gill, D. A. (2004). Disaster, litigation, and the corrosive community. Social Forces, 82(4), 1493–1522. [Google Scholar]
- Pigeon, W., Allen, C., Possemato, K., Bergen-Cico, D., & Treatman, S. (2015). Feasibility and acceptability of a brief mindfulness program for veterans in primary care with posttraumatic stress disorder. Mindfulness, 6(5), 986–995. [Google Scholar]
- Pineles, S. L., Mostoufi, S. M., Ready, C. B., Street, A. E., Griffin, M. G., & Resick, P. A. (2011). Trauma reactivity, avoidant coping, and PTSD symptoms: A moderating relationship? Journal of Abnormal Psychology, 120(1), 240–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polusny, M. A., Erbes, C. R., Thuras, P., Moran, A., Lamberty, G. J., Collins, R. C., … Lim, K. O. (2015). Mindfulness-based stress reduction for posttraumatic stress disorder among veterans a randomized clinical trial. Jama-Journal of the American Medical Association, 314(5), 456–465. [DOI] [PubMed] [Google Scholar]
- Popay, J., Roberts, H., Sowden, A., Petticrew, M., Arai, L., Rodgers, M., ... & Duffy, S. (2006). Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC methods programme Version, 1, b92. [Google Scholar]
- Possemato, K., Bergen-Cico, D., Treatman, S., Allen, C., Wade, M., & Pigeon, W. (2016). A randomized clinical trial of primary care brief mindfulness training for veterans with PTSD. Journal of Clinical Psychology, 72(3), 179–193. [DOI] [PubMed] [Google Scholar]
- Power, K., McGoldrick, T., Brown, K., Buchanan, R., Sharp, D., Swanson, V., Karatzias, A. (2002). A controlled comparison of eye movement desensitisation and reprocessing versus exposure plus cognitive restructuring versus waiting list in the treatment of post-traumatic stress disorder. Clinical Psychology & Psychotherapy, 9(5), 229–318. [Google Scholar]
- Rauch, S., & Foa, E. (2006). Emotional processing theory (EPT) and exposure therapy for PTSD. Journal of Contemporary Psychotherapy, 36(2), 61–65. [Google Scholar]
- Rauch, S., King, A., Abelson, J., Tuerk, P., Smith, E., Rothbaum, B., … Liberzon, I. (2015). Biological and symptom changes in posttraumatic stress disorder treatment: A randomized clinical trial. Depression and Anxiety, 32(3), 204–212. [DOI] [PubMed] [Google Scholar]
- Rauch, S. A. M., Kim, H. M., Powell, C., Tuerk, P. W., Simon, N. M., Acierno, R., … Hoge, C. W. (2018). Efficacy of prolonged exposure therapy, sertraline hydrochloride, and their combination among combat veterans with posttraumatic stress disorder: A randomized clinical trial. JAMA Psychiatry (Chicago, Ill.). doi: 10.1001/jamapsychiatry.2018.3412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ready, D. J., Gerardi, R. J., Backscheider, A. G., Mascaro, N., & Rothbaum, B. O. (2010). Comparing virtual reality exposure therapy to present centred therapy with 11 US Vietnam veterans with PTSD. Cyberpsychology, Behavior and Social Networking, 13(1), 49–54. [DOI] [PubMed] [Google Scholar]
- Reger, G., Koenen-Woods, P., Zetocha, K., Smolenski, D., Holloway, K., Rothbaum, B., … Gahm, G. (2016). Randomized controlled trial of prolonged exposure using imaginal exposure vs. virtual reality exposure in active duty soldiers with deployment-related posttraumatic stress disorder (PTSD). Journal of Consulting and Clinical Psychology, 84(11), 946–959. [DOI] [PubMed] [Google Scholar]
- Resick, P., Nishith, P., Weaver, T., Astin, M., & Feuer, C. (2002). A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. Journal of Consulting and Clinical Psychology, 70(4), 867–879. Retrieved from http://ovidsp.tx.ovid.com/ovftpdfs/FPDDNCLBAHADBG00/fs046/ovft/live/gv023/00004730/00004730-200208000-00001.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick, P. A., & Schnicke, M. K. (1992). Cognitive processing therapy for sexual assault victims. Journal of Consulting and Clinical Psychology, 60(5), 748–756. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/1401390 [DOI] [PubMed] [Google Scholar]
- Resick, P. A., Wachen, J. S., Dondanville, K. A., Pruiksma, K. E., Yarvis, J. S., Peterson, A. L., … Hembree, E. A. (2017). Effect of group vs individual cognitive processing therapy in active-duty military seeking treatment for posttraumatic stress disorder: A randomized clinical trial. JAMA Psychiatry (Chicago, Ill.), 74(1), 28–36. [DOI] [PubMed] [Google Scholar]
- Resick, P. A., Wachen, J. S., Mintz, J., Young-McCaughan, S., Roache, J. D., Borah, A. M., … Peterson, A. L. (2015). A randomized clinical trial of group cognitive processing therapy compared with group present-centered therapy for PTSD among active duty military personnel. Journal of Consulting and Clinical Psychology Journal of Consulting Psychology, 83(6). 1058. doi: 10.1037/ccp0000016 [DOI] [PubMed] [Google Scholar]
- Rothbaum, B. (1997). A controlled study of eye movement desensitization and reprocessing in the treatment of posttraumatic stress disordered sexual assault victims. Bulletin of the Menninger Clinic, 61(61), 317–334. [PubMed] [Google Scholar]
- Rothbaum, B., Astin, M. C., & Marsteller, F. (2005). Prolonged exposure versus eye movement desensitisation and reprocessing (EMDR) for PTSD rape victims. Journal of Traumatic Stress, 18(6), 607–616. Retrieved from http://onlinelibrary.wiley.com/store/10.1002/jts.20069/asset/20069_ftp.pdf?v=1&t=inu4k2sk&s=2089585fa32ab246531de78671ffd54202c1c81f [DOI] [PubMed] [Google Scholar]
- Sautter, F. J., Glynn, S. M., Becker-Cretu, J. J., Senturk, D., Armelie, A. P., & Wielt, D. B. (2016). Structured approach therapy for combat-related PTSD in returning US veterans: Complementary mediation by changes in emotion functioning. Journal of Traumatic Stress, 29(4), 384–387. [DOI] [PubMed] [Google Scholar]
- Sautter, F. J., Glynn, S. M., Cretu, J. B., Senturk, D., & Vaught, A. S. (2015). Efficacy of structured approach therapy in reducing PTSD in returning veterans: A randomized clinical trial. Psychological Services, 12(3), 199–212. [DOI] [PubMed] [Google Scholar]
- Scheck, M., Schaeffer, J. A., & Gillette, C. (1998). Brief psychological intervention with traumatized young women: The efficacy of eye movement desensitisation and reprocessing. Journal of Traumatic Stress, 11(1), 25–44. Retrieved from http://onlinelibrary.wiley.com/store/10.1023/A:1024400931106/asset/3_ftp.pdf?v=1&t=inu4k8ar&s=c7c8505db644f5db54fe0ecceab19d99abb2e234 [DOI] [PubMed] [Google Scholar]
- Schnurr, P., Friedman, M. J., Engel, C. C., Foa, E. B., Shea, M. T., Chow, B. K., … Bernardy, N. (2007). Cognitive behavioural therapy for posttraumatic stress disorder in women. JAMA, 28(8), 820–830. [DOI] [PubMed] [Google Scholar]
- Schnurr, P. P., Friedman, M. J., Foy, D. W., Shea, M. T., Hsieh, F. Y., Lavori, P. W., ... & Bernardy, N. C. (2003). Randomized trial of trauma-focused group therapy for posttraumatic stress disorder: Results from a Department of Veterans Affairs cooperative study. Archives of General Psychiatry, 60(5), 481-489. [DOI] [PubMed] [Google Scholar]
- Schnyder, U., Müller, J., Maercker, A., & Wittmann, L. (2011). Brief eclectic psychotherapy for PTSD: A randomized controlled trial. The Journal of Clinical Psychiatry, 72(4), 564–566. [DOI] [PubMed] [Google Scholar]
- Schoorl, M., Putman, P., Van Der Werff, S., & Van Der Does, A. J. (2014). Attentional bias and attentional control in posttraumatic stress disorder. Journal of Anxiety Disorders, 28(2), 203–210. [DOI] [PubMed] [Google Scholar]
- Shapiro, F. (2014). The role of eye movement desensitization and reprocessing (EMDR) therapy in medicine: Addressing the psychological and physical symptoms stemming from adverse life experiences. The Permanente Journal, 18(1), 71–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shemesh, E., Annunziato, R. A., Weatherley, B. D., Cotter, G., Feaganes, J. R., Santra, M., … Rubinstein, D. (2011). A randomized controlled trial of the safety and promise of cognitive-behavioral therapy using imaginal exposure in patients with posttraumatic stress disorder resulting from cardiovascular illness. The Journal of Clinical Psychiatry, 72(2), 168–174. [DOI] [PubMed] [Google Scholar]
- Simmonds, M. C., Higgins, J. P., Stewart, L. A., Tierney, J. F., Clarke, M. J., & Thompson, S. G. (2005). Meta-analysis of individual patient data from randomized trials: A review of methods used in practice. Clinical Trials: Journal of the Society for Clinical Trials, 2(3), 209–217. [DOI] [PubMed] [Google Scholar]
- Sloan, D., Marx, B., Bovin, M., Feinstein, B., & Gallagher, M. (2012). Written exposure as an intervention for PTSD: A randomized clinical trial with motor vehicle accident survivors. Behaviour Research and Therapy, 50(10), 627–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sloan, D., Marx, B., Lee, D., & Resick, P. (2018). A brief exposure-based treatment vs cognitive processing therapy for posttraumatic stress disorder: A randomized noninferiority clinical trial. JAMA Psychiatry (Chicago, Ill.), 75(3), 233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smyth, J. M., Hockemeyer, J. R., & Tulloch, H. (2008). Expressive writing and post-traumatic stress disorder: Effects on trauma symptoms, mood states, and cortisol reactivity. British Journal of Health Psychology, 13(1), 85–93. [DOI] [PubMed] [Google Scholar]
- Spence, J., Titov, N., Dear, B. F., Johnston, L., Solley, K., Lorian, C., … Schwenke, G. (2011). Randomised controlled trial of internet delivered cognitive behavioural therapy for posttraumatic stress disorder. Depression and Anxiety, 28(7), 541–550. Retrieved from http://onlinelibrary.wiley.com/store/10.1002/da.20835/asset/20835_ftp.pdf?v=1&t=i2vvw2sv&s=d161fe6daeea338f2684077c6209c15152cb90a1 http://onlinelibrary.wiley.com/store/10.1002/da.20835/asset/20835_ftp.pdf?v=1&t=inuduqk3&s=7cef49e4a4c08c5bb86a0e210f9ef8f0ec04a006 [DOI] [PubMed] [Google Scholar]
- Stapleton, J. A., Taylor, S., & Asmundson, G. J. (2006). Effects of three PTSD treatments on anger and guilt: Exposure therapy, eye movement desensitization and reprocessing, and relaxation training. Journal of Traumatic Stress, 19(1), 19–28. [DOI] [PubMed] [Google Scholar]
- Stenmark, H., Catani, C., Neuner, F., Elbert, T., & Holen, A. (2013). Treating PTSD in refugees and asylum seekers within the general health care system. A randomized controlled multicenter study. Behaviour Research and Therapy, 51(10), 641–647. [DOI] [PubMed] [Google Scholar]
- Stirman, S. W., Gutner, C. A., Suvak, M. K., Adler, A., Calloway, A., & Resick, P. (2018). Homework completion, patient characteristics, and symptom change in cognitive processing therapy for PTSD. Behavior Therapy, 49(5), 741–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suris, A., Link-Malcolm, J., Chard, K., Ahn, C., & North, C. (2013). A randomized clinical trial of cognitive processing therapy for veterans with PTSD related to military sexual trauma. Journal of Traumatic Stress, 26(1), 28–37. [DOI] [PubMed] [Google Scholar]
- Taylor, S., Thordarson, D. S., Maxfield, L., Fedoroff, I. C., Lovell, K., & Ogrodniczuk, J. (2003). Comparative efficacy, speed, and adverse effects of three PTSD treatments: Exposure therapy, EMDR, and relaxation training. Journal of Consulting and Clinical Psychology, 71(2), 330–338. Retrieved from http://ovidsp.tx.ovid.com/ovftpdfs/FPDDNCLBAHADBG00/fs046/ovft/live/gv023/00004730/00004730-200304000-00012.pdf [DOI] [PubMed] [Google Scholar]
- ter Heide, F. J., Mooren, T. M., Kleijn, W., de Jongh, A., & Kleber, R. J. (2011). EMDR versus stabilisation in traumatised asylum seekers and refugees: Results of a pilot study. European Journal of Psychotraumatology, 2(1), 5881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinker, R. H. (1999). Through the eyes of a child. EMDR with children. New York: Norton. [Google Scholar]
- Tylee, D. S., Gray, R., Glatt, S. J., & Bourke, F. (2017). Evaluation of the reconsolidation of traumatic memories protocol for the treatment of PTSD: A randomized, wait-list-controlled trial. Journal of Military, Veteran and Family Health, 3(1), 21–33. [Google Scholar]
- Vaughan, K., Armstrong, M. S., Gold, R., O’Connor, N., Jenneke, W., & Tarrier, N. (1994). A trial of eye movement desensitization compared to image habituation training and applied muscle relaxation in post-traumatic stress disorder. Journal of Behavior Therapy and Experimental Psychiatry, 25(4), 283–291. [DOI] [PubMed] [Google Scholar]
- Waller, R., & Gilbody, S. (2009). Barriers to the uptake of computerized cognitive behavioural therapy: a systematic review of the quantitative and qualitative evidence. Psychological Medicine, 39(5), 705-712. [DOI] [PubMed] [Google Scholar]
- Watts, B. V., Schnurr, P. P., Mayo, L., Young-Xu, Y., Weeks, W. B., & Friedman, M. J. (2013a). Meta-analysis of the efficacy of treatments for posttraumatic stress disorder. The Journal of Clinical Psychiatry, 74(6), e541–550. [DOI] [PubMed] [Google Scholar]
- Watts, V., Schnurr, P., Mayo, L., Young-Xu, Y., Weeks, B., & Friedman, J. (2013b). Meta-analysis of the efficacy of treatments for posttraumatic stress disorder. The Journal of Clinical Psychiatry, 74(6), 541–550. [DOI] [PubMed] [Google Scholar]
- Weathers, F. W., & Keane, T. M. (2007). The crucial role of criterion a: A response to Maier’s commentary. Journal of Traumatic Stress, 20(5), 917–919. [Google Scholar]
- Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013). The ptsd checklist for dsm-5 (pcl-5). Scale available from the National Center for PTSD at www. ptsd. va. gov, 10. [Google Scholar]
- Wells, A., & Sembi, S. (2012). Metacognitive therapy for PTSD: A preliminary investigation of a new brief treatment. Journal of Behavior Therapy and Experimental Psychiatry, 35(4), 307–318. Retrieved from http://ac.els-cdn.com/S0005791604000667/1-s2.0-S0005791604000667-main.pdf?_tid=a671d812-12a8-11e6-abc2-00000aacb35e&acdnat=1462442803_096945b6e00c947d3393ed4b88041047 [DOI] [PubMed] [Google Scholar]
- Wells, A., Walton, D., Lovell, K., & Proctor, D. (2015). Metacognitive therapy versus prolonged exposure in adults with chronic post-traumatic stress disorder: A parallel randomized controlled trial. Cognitive Therapy and Research. doi: 10.1007/s10608-014-9636-6 [DOI] [Google Scholar]
- Wilson, S. A., Becker, L. A., & Tinker, R. H. (1995). Eye movement desensitization and reprocessing (EMDR) treatment for psychologically traumatized individuals. Journal of Consulting and Clinical Psychology, 63(6), 928–937. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/8543715 [DOI] [PubMed] [Google Scholar]
- Wittmann, L., Schnyder, U., & Buchi, S. (2012). PRISM (pictorial representation of illness and self measure): A new method for the assessment of suffering after trauma. Journal of Traumatic Stress, 25(1), 94–97. [DOI] [PubMed] [Google Scholar]
- Yehuda, R., Pratchett, L. C., Elmes, M. W., Lehrner, A., Daskalakis, N. P., Koch, E., … Bierer, L. M. (2014). Glucocorticoid-related predictors and correlates of post-traumatic stress disorder treatment response in combat veterans. Interface Focus, 4(5), 20140048. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4142020/pdf/rsfs20140048.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zang, Y., Hunt, N., & Cox, T. (2013). A randomised controlled pilot study: The effectiveness of narrative exposure therapy with adult survivors of the Sichuan earthquake. BMC Psychiatry, 13(1), 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zang, Y., Hunt, N., & Cox, T. (2014). Adapting narrative exposure therapy for Chinese earthquake survivors: A pilot randomised controlled feasibility study. BMC Psychiatry, 14(1). doi: 10.1186/s12888-014-0262-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zlotnick, C., Shea, T. M., Rosen, K., Simpson, E., Mulrenin, K., Begin, A., & Pearlstein, T. (1997). An affect‐management group for women with posttraumatic stress disorder and histories of childhood sexual abuse. Journal of Traumatic Stress, 10(3), 425–436. Retrieved from http://onlinelibrary.wiley.com/store/10.1002/jts.2490100308/asset/2490100308_ftp.pdf?v=1&t=inu4kx80&s=0c840332896ab7ee5185fa6a759bb5c19445ba3a [DOI] [PubMed] [Google Scholar]


