Abstract
In this cross-sectional study of 60 American Indian mother-child dyads from southeastern North Carolina, we examined whether child asthma control was related to household-level factors, such as environmental tobacco smoke and family management. We also examined the relationship between family management and maternal depressive symptoms. We used logistic regression to assess the relationships between child asthma control and presence of environmental tobacco smoke and family management, specifically condition management ability and condition management effort. We used linear regression to evaluate the relationships between both condition management ability and condition management effort and maternal depressive symptoms. Better asthma control in children was associated with the absence of environmental tobacco smoke in the home and the maternal perception of asthma as a manageable condition. Mothers perceived an increase in effort to manage their child’s asthma as their depressive symptoms increased. These findings emphasize the importance of environmental triggers, perceptions of condition management, and maternal mental health in controlling child asthma in American Indian children. Interventions to reduce environmental triggers, treat maternal depressive symptoms, and support mothers in their ability to manage child asthma may yield better asthma control and help to reduce existing racial disparities in this population.
Keywords: American Indians, asthma control, environmental tobacco smoke, family management, maternal depressive symptoms
Introduction
Although child asthma prevalence is declining overall, racial and ethnic minority children, compared to White children, continue to have double the asthma prevalence, with significantly higher morbidity and mortality – four times more hospitalizations and seven times the number of deaths (Akinbami, Moorman, Simon, & Schoendorf, 2014; Aakinbami, Simon, & Rossen, 2016). Among small racial/ethnic minority groups, American Indian and Alaska Native (AIAN) children were found to have the highest current asthma prevalence of any racial group (14.6%), 1.6 times that of non-Hispanic White children (9.2%), according to data from the 2006 – 2015 National Health Interview Survey (Wen, Liu, Li, Sheffield, & Liu, 2019). The increased asthma prevalence among AIAN children is especially alarming because of their 11.15 higher odds of inpatient mortality from asthma hospitalizations compared to White children (Glick, Tomopoulos, Fierman, & Trasande, 2016). In North Carolina (NC), racial disparities in asthma morbidity reflect national trends: for example, among children ages 0–14, the number of asthma-related hospital discharges in American Indian children is greater than 3.4 times the number in White children (245 vs 71.8 per 100,000 respectively; Bell, Foglia, & Ries, 2017). Concentrated largely in the least resourced counties in rural southeastern NC, American Indian children are at particular risk based on geographic disparities in asthma and asthma morbidities burdening rural and impoverished counties disproportionately (Dieu, Kearney, Bian, Jones, & Mohan, 2018; Estrada & Ownby, 2017). Achieving better asthma control in high-risk groups such as American Indians is a practical step toward narrowing the racial disparities gap in child asthma, although ideal solutions for asthma disparities must target contributing factors within the social, economic, and physical environments (Arthur, Knusten, Spencer-Hwang, Shavlik, & Montgomery, 2019; Kelley & Kearney, 2018).
Adequately controlled asthma in children is an important indicator of how well families manage the condition. Relatively little is known, however, about how American Indian parents incorporate the recommended treatment regimen into their child’s and family’s everyday life or how family management processes and beliefs are related to condition control. As conceptualized in the Family Management Style Framework, family management is a multidimensional construct that includes parents’ beliefs about the condition and its consequences for their child and family, their condition management goals, and behavioral efforts to incorporate needed treatments into the child’s and family’s daily routine (Knafl & Deatrick, 2003; Knafl et al., 2013). Effective management requires adoption and daily practice of condition-specific management behaviors: administration of medications, avoidance of environmental triggers, coordination of healthcare visits, and monitoring of daily symptoms (Beacham & Deatrick, 2015; Gautier & Charpin, 2017; Searle, Jago, Henderson, & Turner, 2017).
Social, economic, and physical environmental factors unique to rural minority communities can create additional challenges in the mangagement of asthma in rural minority children. Beyond disproportionate exposures to poor quality housing, tobacco smoke, and agriculture, rural families experience additional barriers that include lack of insurance, less access to healthcare services, and adverse socioeconomic conditions (Estrada & Ownby, 2017). Focusing on common, yet avoidable, asthma triggers in the child’s physical environment within parents’ control (e.g., environmental tobacco smoke) may improve asthma control in children (Abreo, Gebradik, Stone, & Hartert, 2018). Widening the scope to include other relevant, but less obvious social environmental factors that can compromise family management, such as maternal depressive symptoms, however, might be more fruitful. Mothers of children with asthma often have depressive symptoms (Behmanesh, Moharreri, Soltanifar, Hamzeh, & Heidari, 2017; Ghaempanah et al., 2013; Kub et al., 2018). Consequently, depressive symptoms may impair mothers’ ability to manage their child’s asthma, resulting in poor asthma control (Medsker et al., 2016; Pak & Allen, 2012; Wood et al., 2018). Consideration of multiple environmental influences and complex contexts in which they occur is essential to achieve asthma control in groups with the highest health risks, such as American Indian children. Using the Family Management Style Framework (Knafl & Deatrick, 2003; Knafl, Deatrick, & Havill, 2012) to guide our study, we aimed to examine child asthma control and its relationships to environmental tobacco smoke and family management in a subgroup of American Indian (Lumbee Indian) mothers and children in southeastern NC. Given the evidence suggesting that depressive symptoms are likely related to how mothers perceive their child’s symptoms and treatment regimen (Pak & Allen, 2012), we also assessed the relationship between family management of child asthma and maternal depressive symptoms.
Child Asthma and Environmental Tobacco Smoke
Differences in metabolic processes and oxygen consumption rates make children more vulnerable than adults to environmental tobacco smoke (Landrigan & Goldman, 2011). More than half of all children with asthma in the US are exposed to smoke from commercial tobacco, which contains thousands of potentially dangerous chemicals and heavy metals (Quinto, Kit, Lukacs, & Akinbami, 2013). Serious health threats posed by environmental tobacco smoke exposure include decreased pulmonary function, increased airway reactivity, and acute asthma exacerbations, any or all of which can increase symptom severity and frequency of asthma episodes in children, leading to otherwise avoidable urgent care and emergency department visits or hospitalizations (Dick, Doust, Cowie, Ayres, & Turner, 2014; Wang et al., 2015). The wide variation in environmental tobacco smoke exposure across racial groups likely worsens the racial disparities in child asthma (Akinbami, Kit, & Simon, 2013; Fedele et al., 2016; Merianos, Jandarov, Choi, & Mahabee-Gittens, 2019). As a population, AIANs have the highest smoking prevalence (34.0%) of all racial groups, a behavior that unequally predisposes American Indian children to environmental tobacco smoke exposure (Agaku, Odani, Okuyemi, & Armour, 2019; Odani, Armour, Graffunder, Garrett, & Agaku, 2017). The 2007 National Survey of Children’s Health reported that American Indian children had 2.0 times higher odds of being exposed to environmental tobacco smoke than the reference group (Hispanic children; Singh, Siahpush, & Kogan, 2010). Given the increased odds of environmental tobacco smoke exposure in this population, inadequately controlled asthma and thus worse asthma outcomes are likely.
Child Asthma and the Family Management Style Framework
Used to study family management of childhood chronic conditions, including asthma (Gibson-Young, Turner-Henson, Gerald, Vance, & Lorenzo, 2014; Zhang, Wei, Shen, & Zhang, 2015), the Family Management Style Framework has three major components: definition of the situation, management behaviors, and perceived consequences (Knafl & Deatrick, 1990; 2003; Knafl, Deatrick, & Havill, 2012). Investigators who ground their research in the Family Management Style Framework look beyond condition-specific management activities to examine parents’ underlying management goals, perceptions of the ease or difficulty of carrying out the treatment regimen, and the extent to which parents have developed a daily management routine.
In this paper, we focus on the management of child asthma from the perspective of mothers, because they are typically children’s primary caregivers (Gibson-Young et al., 2014; Long & Marsland, 2011). Using the Family Management Measure (FaMM), developed by Knafl and Deatrick (2006) to assess various aspects of family management, Gibson-Young and colleagues (2014) examined the relationship between mothers’ perceptions of their ability and their effort to manage the treatment regimen, and asthma morbidity, measured by emergency department visits, hospitalizations, and school days missed. Mothers’ perception of their management ability was significantly related to hospitalization frequency, with greater perceived ability related to fewer hospitalizations. Similarly, mothers’ perception of their management effort was significantly associated with school days missed, with lower perceived effort related to fewer school days missed. Interestingly, child racial status and family income also affected maternal perceptions of management ability and effort.
Maternal caregivers of non-minority children with asthma reported less perceived effort and greater perceived ability to manage the child’s asthma condition. Maternal caregivers of non-minority children also reported fewer emergency department visits and child hospitalizations. Higher family income was associated with less perceived effort and greater perceived ability by the mother to manage the child’s asthma condition and fewer child hospitalizations and school days missed. Furthermore, maternal perceptions of ability, family income, and child minority status independently predicted child hospitalizations, whereas maternal perceptions of effort predicted school days missed (Gibson-Young et al., 2014). These results point to the importance of addressing these key aspects of mothers’ asthma management experiences to improve asthma-related outcomes in children.
Family management of child asthma and maternal depressive symptoms
Mothers’ ability to manage child asthma effectively may be compromised by maternal depressive symptoms (Pak & Allen, 2012; Wood et al., 2018). More prevalent among mothers of children with asthma than those without asthma, depressive symptoms have been linked to child asthma symptoms and more asthma-related hospitalizations and unscheduled health care visits (Behmanesh et al., 2017; Ghaempanah et al., 2013; Kub et al., 2018; Pak & Allen, 2012). Maternal depressive symptoms were associated with healthcare expenditures for publicly insured children with chronic health conditions. Specifically, emergency department and predicted healthcare expenditures were higher for children of mothers with depressive symptoms compared to children of mothers without depressive symptoms (Brooks, Beil, & Beeber, 2015). Among those caring for a child with asthma, mothers with more depressive symptoms have reported lower self-efficacy and sense of empowerment in their caring ability than those with fewer depressive symptoms (Pak & Allen, 2012).
The presence of depressive symptoms also appears to influence maternal perceptions and beliefs about the child’s condition (Dow-Fleisner & Hawkins, 2018). Bartlett et al. (2004) found that mothers with high levels of depressive symptoms had more negative beliefs regarding their child’s asthma, and that their beliefs did not necessarily align with health care providers’ recommendations. Mothers perceived that health care providers were uninterested in addressing their child’s emotional needs and that providers often overlooked important medical information. In their integrative literature review, Pak and Allen (2012) found that maternal depressive symptoms were related to more disruption in life and normal daily activities, more child problems related to asthma medication doses and use of asthma inhalers, more frequent use of quick-relief asthma medications, less maternal understanding about the function and use of their child’s medications, and lower perceived ability by the mother to control child’s asthma symptoms. Despite the accumulating evidence linking family management of child asthma and maternal depressive symptoms, little is known about this relationship within American Indian families. The importance of maternal mental health, especially maternal depressive symptoms in relation to family management of child asthma, and the strong potential for less adequate control of asthma among American Indian children, necessitates further examination in this racial minority subgroup.
Methods
In this cross-sectional study, we examined the relationships between child asthma control and presence of environmental tobacco smoke and family management in American Indian children. We also explored the relationship between family management and maternal depressive symptoms.
Sample
We enrolled 60 Lumbee Indian mothers and their children with asthma from three pediatric clinics located in southeast NC. Families were approached for participation by the principal investigator of the study, who has an established relationship with the clinics and is a member of the Lumbee Tribe. Children between 4 and 12 years of age with a current medical diagnosis of asthma were eligible for the study. We included mothers who self-identified as Lumbee Indian, were between the ages of 18 and 60 years, were the biological or adoptive mother of the child, and were the primary caregiver. We excluded children who had not experienced asthma symptoms (e.g., wheezing, coughing, nighttime awakenings) in the past 12 months or who had co-morbid conditions (e.g., diabetes, cystic fibrosis, heart disease). A power analysis in which we computed power values using the ‘logistic’ sub-routine in the POWER procedure in SAS, version 9.4 (SAS Institute Inc., Cary, NC) showed that with 60 families we would be able to detect odds ratios of 1.22 and 14.8 (>80% power α = 0.05, two-tailed) for condition management ability and presence of environmental tobacco smoke, respectively, in relation to asthma control.
Measures
Childhood Asthma Control Test
Children and their mothers completed the Childhood Asthma Control Test (C-ACT), a tool designed to assess the level of asthma control in children between 4 and 17 years of age. We asked children to complete the measure most appropriate for their age. The version for children ages 4–11 years consists of seven questions: three parent-reported and four child-reported. Parents were able to assist younger children in answering the child-reported questions. Scores are summed and range from 0 to 27. The 5-item version for children ages 12 years and older is completed independently by the child. Scores range from 5 to 25. In both versions, higher ratings indicate better asthma control; a score of 19 or less suggests that the child’s asthma is inadequately controlled (Liu et al., 2010). The C-ACT has acceptable internal reliability (α =0.76) and test-retest reliability (α =0.72) and is correlated significantly with other asthma control measures (Bime et al., 2016; Ortiz-Lizcano, Niederbacher-Velasquez, Diaz-Martinez, 2016).
Family Management Measure
To assess family management of childhood asthma, mothers completed the FaMM. The FaMM is a 53-item measure comprised of six scales addressing distinct aspects of family life: child’s daily life; condition management ability; condition management effort; family life difficulty; view of condition impact; and parental mutuality. Scales are scored separately (Knafl et al., 2011).
We are reporting results from the Condition Management Ability (CMA) and Condition Management Effort (CME) scales. Briefly, CMA assesses parents’ perceptions of their competence to take care of the child’s condition and CME assesses perceptions of the time and work needed to manage the condition (Knafl et al., 2011). Items are scored from 1 to 5 (strongly disagree to strongly agree). Higher values on the CMA scale, which has a hypothetical range of 12 to 60, indicate more efficient management of the child’s illness, whereas higher scores on the CME scale, (hypothetical range 4 to 20) indicate greater effort in management of the illness. Although CMA and CME were significantly correlated (r= −.34, p = .008), the strength of the correlation is considered weak, indicating that these two scales measure different aspects of family management. FaMM scales have demonstrated construct validity and acceptable internal consistency reliability (.71-.94) and test-retest reliability (.71-.94; Knafl et al., 2011).
Center for Epidemiologic Studies Depression Scale (CES-D)
Mothers completed the CES-D, a 20-item scale designed by Radloff (1977) to measure the current level of depressive symptomatology. We asked mothers to indicate how often over the past week they experienced symptoms such as crying spells, feeling lonely, and poor appetite. Item responses are on a 4-point Likert scale (0=rarely or none of the time to 3=all of the time). Four of the items are reverse scored. Scores, calculated as the sum of all items, range from 0 to 60, with higher scores indicating more depressive symptoms. A meta-analysis of 22 studies showed that the cutoff score of ≥16, often used to identify individuals at risk for clinical depression, has high sensitivity (0.87) and moderate specificity (0.70; Vilagut, Forero, Barbaglia, & Alonso, 2016). The CES-D is correlated with other depression measures and has high internal consistency (α = 0.85–0.91; Carleton et al., 2013).
Child Health Questionnaire and Demographic Characteristics
Mothers provided information on child age at diagnosis, presence of upper respiratory infections, unscheduled medical visits, ER visits and/or hospitalizations related to asthma, school days missed, daytime and nighttime asthma symptoms, current prescribed asthma medications, use of home remedies or herbs, the degree to which asthma interfered with physical activity, peak flow meter use, whether an asthma action plan is followed, type of health insurance, and child exposure to household environmental tobacco smoke. We collected mothers’ demographic information by maternal report: age, level of education, employment, marital status, household income, others living in the home, their ages and relationships to the child, and receipt of supplemental security income disability payments.
Procedures
We obtained study approval from the tribal health and human services committee and Institutional Review Board (IRB) of the primary author’s university. Mothers provided informed consent for themselves and gave permission for their children to participate in the study. We obtained assent for children ages of 7–12 years based on IRB guidelines. Following parental consent and child assent, mothers and their children completed a series of questionnaires during a pediatric office visit or in the home setting at a time determined by the mother. We gave mothers and their children a small incentive (gift cards of $20 and $5, respectively) for their participation.
Data Analysis
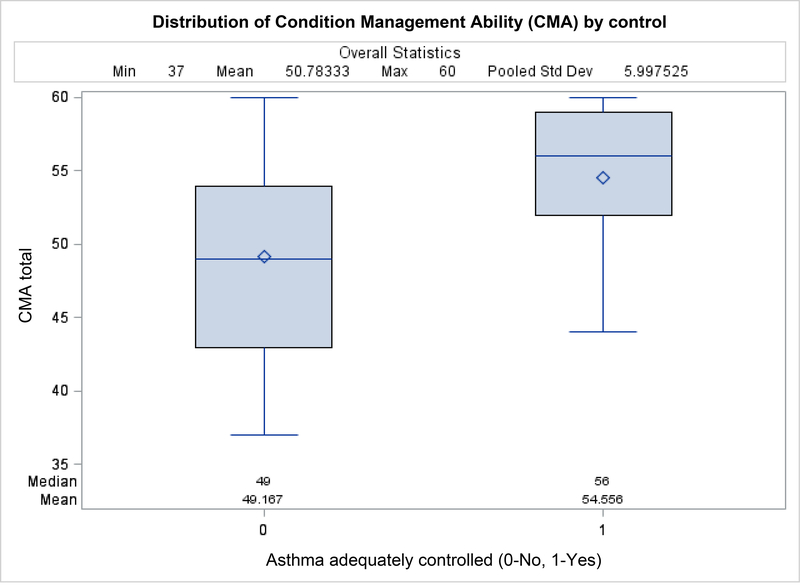
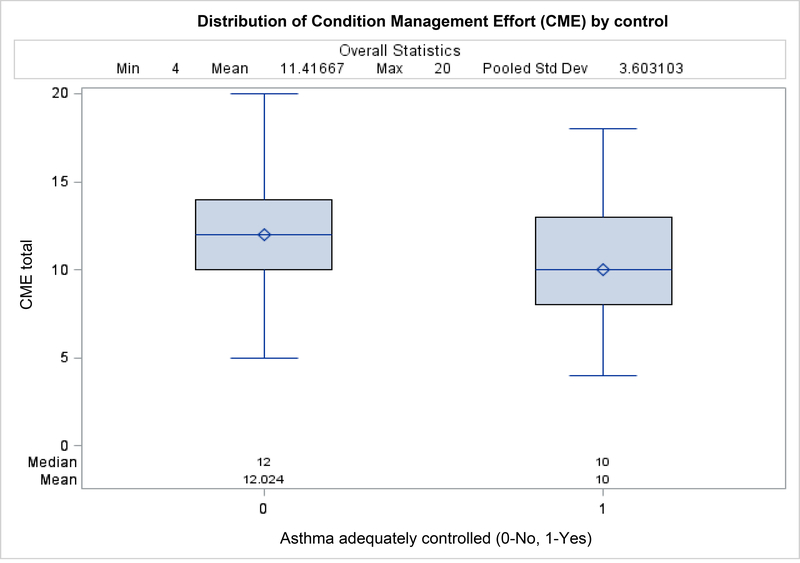
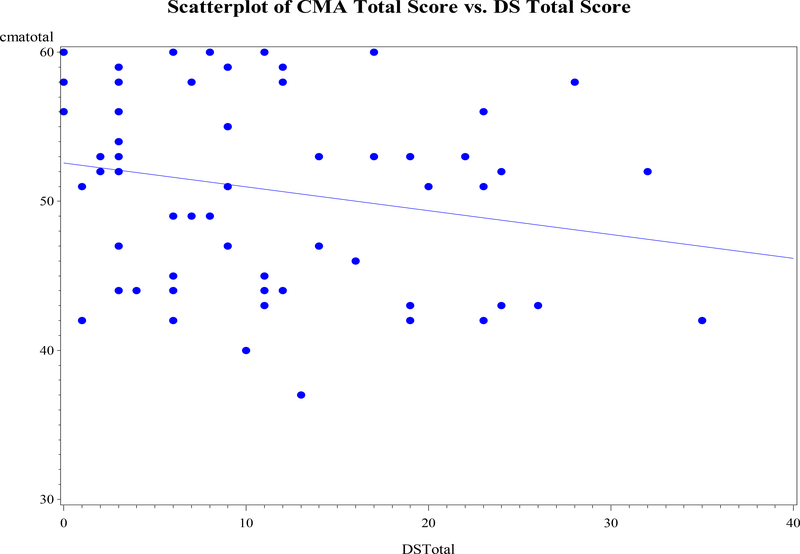
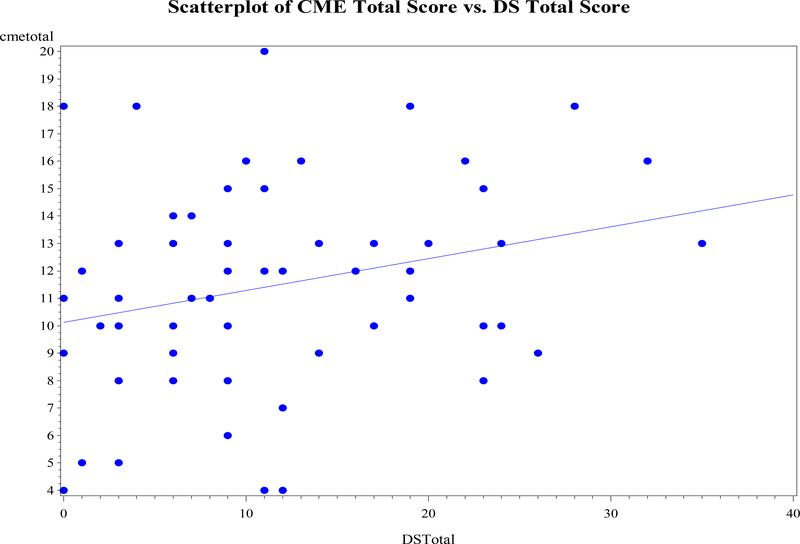
We computed descriptive statistics for all demographic characteristics (means and standard deviations for continuous variables; frequencies and percentages for categorical variables). We constructed boxplots to examine the relationships between CMA and asthma control, and between CME and asthma control. We used scatterplots to examine the relationship between CMA and maternal depressive symptom score, and between CME and maternal depressive symptom score.
Using multiple logistic regression, we assessed the relationship between adequately controlled asthma (>19) and the following: CMA, CME, presence of environmental tobacco smoke, a dummy variable indicating the child had more than two upper respiratory infections, the child’s gender, age, and age at diagnosis. Using multiple linear regression, we evaluated the relationship between CMA and maternal depressive symptoms while controlling for covariate effects of marital status and maternal age. Marital status was specified as single to include separated, divorced, and living apart and married to include living with partner. We used this modeling approach to assess the relationship between CME and maternal depressive symptom score while controlling for the covariate effect of maternal age. We did not include marital status as a covariate in this model, given its lack of significance with CME and maternal depressive symptom score.
Using PROC LOGISTIC (SAS Version 9.4), we fit the logistic models and used PROC GLM to fit each linear regression model, and set the significance level at 0.05 for each model. For significant effects with more than two levels, we used post hoc tests based on the Holm-Bonferroni correction method (Holm, 1979).
Results
Demographics and Descriptive Statistics
Demographic characteristics of the sample are presented in Table 1. Sixty-six percent of the children (N = 60) were male and had a mean age of 7.2 years (range 4 −12 years). The mean age at asthma diagnosis was 1.73 years. Forty percent of children were exposed to environmental tobacco smoke. Mean maternal age was 32.4 years (range 18 – 44 years); 63% of sample mothers were employed and 45% were married. Other marital statuses included single (23.3%), partnered (8.3%), and separated, divorced, or living apart (23.3%). Approximately 71% of mothers reported an annual household income of < $50K.
Table 1.
Demographic Characteristics of the 60 American Indian Mothers and their Children
| Characteristic | Frequency | Percent | Mean | SD |
|---|---|---|---|---|
| Maternal age (years) | 32.38 | 5.87 | ||
| Child age (years) | 7.17 | 2.29 | ||
| Child age at diagnosis (years) | 1.73 | 1.48 | ||
| Child gender | ||||
| Male | 40 | 66.67 | ||
| Female | 20 | 33.33 | ||
| Marital status | ||||
| Single | 14 | 23.33 | ||
| Married | 27 | 45 | ||
| Living with partner | 5 | 8.33 | ||
| Separated | 5 | 8.33 | ||
| Divorced | 7 | 11.67 | ||
| Living apart | 2 | 3.33 | ||
| Employment status | ||||
| Yes | 38 | 63.33 | ||
| No | 22 | 36.67 | ||
| SSI Disability | ||||
| Yes | 4 | 6.67 | ||
| No | 53 | 88.33 | ||
| Household income | ||||
| ≥ $75K/year | 9 | 15 | ||
| $50–74.999K/year | 4 | 6.67 | ||
| $25–49.999K/year | 14 | 23.33 | ||
| $10–24.999K/year | 18 | 30 | ||
| < $10K/year | 11 | 18.33 | ||
| No income | 2 | 3.33 | ||
| Don’t know | 2 | 3.33 | ||
| Child ETS exposurea | ||||
| Yes | 24 | 40 | ||
| No | 36 | 60 | ||
| Child asthma control | ||||
| Adequately controlled | 18 | 30 | ||
| Inadequately controlled | 42 | 70 | ||
ETS = Environmental Tobacco Smoke; Yes = at least one smoker in the home
Descriptive statistics for maternal depressive symptoms and family management of child asthma are presented in Table 2. Maternal depressive symptoms among mothers ranged from 0 to 35. The means for CMA and CME were 50.78 (SD = 6.45) and 11.42 (SD = 3.69), respectively.
Table 2.
Descriptive Statistics for Maternal Depressive Symptoms and Family Management of Child Asthma
| Characteristic | Mean | SD | Min | Max | Cronbach’s α |
|---|---|---|---|---|---|
| Condition Management Ability (CMA) | 50.78 | 6.45 | 37.0 | 60.0 | 0.72 |
| Condition Management Effort (CME) | 11.42 | 3.69 | 4.0 | 20.0 | 0.68 |
| Maternal Depressive Symptoms | 11.10 | 8.66 | 0 | 35.0 | 0.85 |
Adequately Controlled Asthma and Its Relationships with Environmental Tobacco Smoke and Family Management of Child Asthma
The adjusted odds of asthma being adequately controlled was 14.43 times greater in families in which no one smoked in the home (p = .006, 95% CI = 2.186, 95.182) compared to families in which at least one member smoked (Table 3). Distributions of CMA and CME scores (Figures 1 and 2) for each level of asthma control (adequately controlled, inadequately controlled) showed that CMA scores were higher among children whose asthma was adequately controlled. A one unit higher CMA score (i.e., about one-quarter of an SD [1/3.69 = .27]) was significantly associated with higher odds of having adequately controlled asthma (adjusted odds ratio (OR) = 1.159, p = .029, 95% CI = 1.015, 1.324) (Table 3).
Table 3.
Well-Controlled Asthma and Its Composite Relationship With Family Management, Environmental Tobacco Smoke, and Child Health Problems
| Variables | Adjusted OR Estimate | 95% Confidence Limits | p-value |
|---|---|---|---|
| Condition management ability | 1.159* | 1.015, 1.324 | 0.029 |
| Condition management effort | 0.798 | 0.622, 1.024 | 0.076 |
| Environmental tobacco smoke (no vs. yes) | 14.426* | 2.186, 95.182 | 0.006 |
| >2 upper respiratory infections (no vs. yes) | 1.958 | 0.386, 9.930 | 0.417 |
| Child age | 1.224 | 0.891, 1.682 | 0.213 |
| Child age at diagnosis | 1.495 | 0.896, 2.495 | 0.124 |
| Child gender (female vs. male) | 1.373 | 0.252, 7.483 | 0.714 |
indicates that p-values are significant at the0.05 level
Figure 1.
Box plots of condition management ability according to whether asthma was adequately controlled (upper line represents the 75th percentile; middle line represents the 50th percentile; diamond represents the mean; lower line represents the 25th percentile).
Figure 2.
Box plots of CME according to whether child asthma was adequately controlled.
Relationship Between Family Management of Child Asthma and Maternal Depressive Symptoms
Figures 3 and 4 show the relationships between CMA scores and maternal depressive symptom scores, and between CME scores and maternal depressive symptom scores. Although CMA score and maternal depressive symptom score were not significantly correlated (r = −.21, p = .100), CME score and maternal depressive symptom score were significantly positively correlated (r = .27, p = .035). Tables 4 and 5 display the results of the linear regression models for the outcomes of CME and CMA score. On average, CME score increased by 0.116 units with each unit increase in maternal depression score (p = .036, 95% CI = 0.008, 0.225), which is equivalent to a .03 SD higher CME being associated with a one tenth SD higher depression score (1 unit /8.66 [SD of depressive symptoms]= .115 SD; a 0.116 unit change in CME is equivalent to 0.116/3.69 [SD of CME] = .03 SD). CMA score significantly decreased by 7.537 units for single parents relative to married parents (p = .007, 95% CI = −13.764, −1.310), which is equivalent to a 1.17 SD higher CMA being associated with being married.
Figure 3.
Scatterplot of condition management ability versus maternal depressive symptoms score.
Figure 4.
Scatterplot of condition management effort versus maternal depressive symptoms score.
Table 4.
Relationship between Condition Management Effort and Maternal Depressive Symptoms Controlling for Maternal Age
| Variables | Slope Estimate | 95% Confidence Limits | p-value |
|---|---|---|---|
| Maternal depression score | 0.116* | 0.008, 0.225 | 0.036 |
| Maternal age | −0.049 | −0.209, 0.111 | 0.541 |
indicates that p-values are significant at the 0.05 level
Table 5.
The Relationship Between Condition Management Ability and Maternal Depressive Symptoms Controlling for Marital Status and Maternal Age
| Variables | Slope Estimate | 95% Confidence Limits | p-value |
|---|---|---|---|
| Maternal depression score | −0.065 | −0.253,0.123 | 0.490 |
| Marital status (single vs. married) | −7.537* | −13.764, −1.310 | 0.007 |
| Maternal age | −0.013 | −0.282, 0.255 | 0.921 |
indicates that p-values are significant at the 0.05 level
Discussion
In this cross-sectional study, we examined environmental tobacco smoke, family management, and maternal depressive symptoms as modifiable factors contributing to asthma control in a sample of American Indian children from rural southeast NC. Despite the high burden of asthma and disproportionately high rates of poor asthma outcomes among American Indian children in NC, to our knowledge this is the only study that has focused exclusively on the relationships between asthma control and broader environmental factors in this population. In a recent integrative literature review, Lowe et al. (2018) assessed the effect of environmental factors on asthma prevalence and severity among reservation-based Navajo children but considered only environmental pollutants, such as diesel exhaust, indoor allergens, and tobacco smoke. Further, our use of the Family Management Style Framework, an established conceptual model, enhanced our ability to study two aspects of management, CMA and CME, which we showed to be compromised by maternal depressive symptoms.
Our results showed that physical environmental factors known to be more prevalent in American Indian families, such as environmental tobacco smoke, made asthma management more challenging for Lumbee Indian mothers. In this study, 40% of Lumbee Indian children were exposed to environmental tobacco smoke, which is higher than the national smoking prevalence (34.0%) among American Indians (Agaku et al., 2019). The presence of environmental tobacco smoke in our sample was substantially higher than the rate of tobacco smoking in the general U.S. population (16.8%), which is particularly concerning because American Indian children are exposed disproportionately to harmful toxins that elevate their risk for asthma and its ensuing complications (Jamal et al., 2016; Martell, Garrett, & Caraballo, 2016). Clearly an important physical environmental concern in this population, elevated exposure to environmental tobacco smoke among Lumbee Indian children appears to contribute to inadequate asthma control. Seventy percent of Lumbee Indian children in our sample had asthma that was inadequately controlled. Further supporting the environmental tobacco smoke-asthma control relationship (Dick et al., 2014; Wang et al., 2015), our data showed that exposure to environmental tobacco smoke was associated with a lower odds of asthma being adequately controlled in Lumbee Indian children. Future interventions targeted at improving asthma control in American Indian children should address environmental tobacco smoke as a known risk factor within the physical environment that can threaten child health.
We found that asthma control in Lumbee Indian children was associated with family management of asthma, as determined by CMA and CME. Greater condition management ability (CMA) was significantly associated with higher odds of having adequately controlled asthma. Greater condition management effort (CME) was also associated with adequately controlled asthma. In their study, Gibson-Young et al. (2014) found that maternal caregivers of non-minority children with asthma reported greater perceived ability and less perceived effort to manage their child’s asthma condition. Our finding that more perceived effort by Lumbee Indian mothers was associated with better control of child asthma justifies the need for additional research examining factors that contribute to racial differences in perceived management effort. The requirement of greater effort to manage child asthma effectively in minority children could reflect additional challenges or barriers, possibly leading to worse child asthma-related outcomes (Gibson-Young et al., 2014).
We found that factors in the social environment, such as maternal depressive symptoms, were a crucial factor in the management of asthma in Lumbee Indian children. Not surprisingly, as maternal depressive symptoms increased, mothers perceived a decrease in their management ability and an increase in the effort needed to manage their child’s asthma. Our results are consistent with those of other investigators that indicate lower self-efficacy and less sense of empowerment in the caring ability of mothers with more depressive symptoms who care for a child with asthma compared to mothers with fewer symptoms (Pak & Allen, 2012). The presence of depressive symptoms, often accompanied by a disruption in daily life activities, could lead to difficulty in following routines and consequently, inadequately controlled asthma (Ghaempanah et al., 2013). This particular finding could be problematic for children of American Indian mothers in NC, given the disproportionately high rates of mental health problems reported within the American Indian population (North Carolina American Indian Health Board and the Office of Minority Health and Health Disparities, 2017). With potential for increased risk in this population, culturally-relevant interventions designed to improve the family management of child asthma should also address disparities in maternal mental health.
Additional socioeconomic factors emerged in our study as important in the management of child asthma. Over 23% of households were headed by Lumbee Indian females; this number approached 47% when we considered families where parents were separated, divorced, or living apart. Estimates from our study are consistent with those reported by the U.S. Census Bureau (2017), which indicated that a female heads 22.1% of Lumbee Indian households. Our findings showed that mothers raising children as single parents was associated with less effective management (CMA score significantly decreased by 7.537 points for single parents relative to married parents) suggesting that this factor can place Lumbee Indian children at higher risk for poor asthma management.
One possible explanation for the lower management ability reported by single parents is the strong link between marital status and socioeconomic status, in which single mothers tend to live in more impoverished conditions compared to married mothers (Brooks, Beil, & Beeber, 2015). According to the U.S. Census Bureau (2017), female-headed households account for 44.5% of the Lumbee Indian families living in poverty, defined as family annual income below a particular poverty threshold. Almost half (48%) of our sample earned a household income of less than $25K per year, well below the median annual income of $32,407 for households in Robeson County, NC (Data USA, 2017). Enduring some of the greatest socioeconomic burden in NC, 25.5% of American Indian families were living below the federal poverty threshold in 2018, which was more than double that for White families at 12.0% (N.C. Department of Health and Human Services and Office of Minority Health and Health Disparities, 2018). The combination of female heads of households and socioeconomic hardship may create a situation in the child’s care environment that leads to more difficulty in the management of child asthma and increased child asthma morbidity (Beeber, Perreira, & Schwartz, 2008; Moncrief, Beck, Simmons, Huang, & Kahn, 2014).
One of the limitations of our study is sample size. With 60 families, the study was sufficiently powered to detect relationships between asthma control and presence of environmental tobacco smoke and family management, specifically CMA. Although there was only 20% power to detect a slope of 0.02 (based on pilot data) for maternal depressive symptoms when modeling its relationship with CME, the slope using the full data proved to be much larger (0.116) and was significantly different from zero. Results from this study should be interpreted with caution given insufficient power to detect relationships between asthma control and CME, and maternal depressive symptoms and family management. Nonetheless, our findings remain valuable and contribute to the literature on factors influencing asthma control in an understudied population. Another limitation of our study was that some of the measurement tools had not been previously assessed for reliability and validity in the American Indian population. In our assessment, we found the internal consistency reliability of one scale – the CME – to be slightly less than acceptable at .68. However, we believe our results are informative in spite of this limitation. When possible, researchers should assess the psychometric properties of measurement tools with diverse populations to determine the reliability and cultural validity of such instruments.
Conclusion
In this study, we found that absence of environmental tobacco smoke in the home and maternal perceptions of asthma as a manageable condition were associated with better asthma control in American Indian children. These findings suggest the importance of environmental factors and perceptions of condition management in controlling asthma in American Indian children. Further, maternal depressive symptoms may affect certain aspects of asthma management in American Indian children. Due to the increased prevalence of asthma and the intersection of social, economic, and physical environmental factors (i.e., environmental tobacco smoke, family management, maternal depressive symptoms, marital status) that lead to increased risk for poorly controlled asthma in this population, standard interventions are unlikely to be effective. Modifications to and cultural tailoring of interventions that improve the quality of the home environment for American Indian children would likely lead to better asthma control and reduce the asthma disparities gap in this population.
Acknowledgments
This project was supported by a postdoctoral fellowship to the first author as part of an Institutional National Service Award to the University of North Carolina at Chapel Hill School of Nursing (T32 NR007091), from the National Institute for Nursing Research, National Institutes of Health. We want to acknowledge Kathleen A. Knafl, author of the Family Management Style Framework and Family Management Measure, for her valuable contribution to this manuscript.
Acknowledgement of Funding Source
This research was supported by a postdoctoral fellowship to the first author as part of an institutional National Service Award to the University of North Carolina at Chapel Hill School of Nursing (T32 NR007091), from the National Institute for Nursing Research (NINR), National Institute of Health.
Footnotes
Declaration of Conflicting Interests
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Agaku IT, Odani S, Okuyemi KS, & Armour B (2019). Disparities in current cigarette smoking among US adults, 2002–2016. Tobacco Control, 0, 1–8. doi: 10.1136/tobaccocontrol-2019-054948. [DOI] [PubMed] [Google Scholar]
- Abreo A, Gebretsadik T, Stone CA, & Hartert TV (2018). The impact of modifiable risk factor reduction on childhood asthma development. Clinical and Translational Medicine, 7(1), 15. doi: 10.1186/s40169-018-0195-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akinbami LJ, Kit BK, & Simon AE (2013). Impact of environmental tobacco smoke on children with asthma, United States, 2003–2010. Academic Pediatrics, 13(6), 508–516. doi: 10.1016/j.acap.2013.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akinbami LJ, Moorman JE, Simon AE, & Schoendorf KC (2014). Trends in racial disparities for asthma outcomes among children 0 to 17 years, 2001–2010. The Journal of Allergy and Clinical Immunology, 134(3), 547–553 e545. doi: 10.1016/j.jaci.2014.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akinbami LJ, Simon AE, & Rossen LM (2016). Changing trends in asthma prevalence among children. Pediatrics, 137(1), e20152354. doi: 10.1542/peds.2015-2354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arthur KN, Knusten SF, Spencer-Hwang DS, Shavlik D, & Montgomery S (2019). Health-predictive social-environmental stressors and social buffers are place based: A multilevel example from San Bernardino communities. Journal of Primary Care & Community Health, 10, 2150132719835627. doi: 10.11177/2150132719835627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartlett SJ, Krishnan JA, Riekert KA, Butz AM, Malveaux FJ, & Rand CS (2004). Maternal depressive symptoms and adherence to therapy in inner-city children with asthma. Pediatrics, 113(2), 229–237. [DOI] [PubMed] [Google Scholar]
- Beacham BL & Deatrick JA (2015). Children with chronic conditions: Perspectives on condition management. Journal of Pediatric Nursing, 30(1), 25–35. doi: 10.1016/j.pedn.2014.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beeber LS, Perreira KM, & Schwartz T (2008). Supporting the mental health of mothers raising children in poverty: How do we target them for intervention studies? Annals of the New York Academy of Sciences, 1136, 86–100. doi: 10.1196/annals.1425.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behmanesh F, Moharreri F, Soltanifar A, Hamzeh M, & Heidari E (2017). Evaluation of anxiety and depression in mothers of children with asthma. Electronic Physician, 9(12), 6058–6062. doi: 10.19082/6058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell LA, Foglia A, & Ries M (2017). NC Child Health Report Card, 2017. Retrieved from http://nciom.org/wp-content/uploads/2017/07/2017-FINAL-3.17@235.pdf
- Bime C, Gerald JK, Wei CY, Holbrook JT, Teague WG, Wise RA, & Gerald LB (2016). Measurement characteristics of the Childhood Asthma- Control Test and a shortened, child-only version. NPJ Primary Care Respiratory Medicine, 26, 16075. doi: 10.1038/npjpcrm.2016.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks JL, Beil H & Beeber LS (2015). Maternal depressive symptoms and healthcare expenditures for publicly insured children with chronic health conditions. Maternal and Child Health Journal, 19(4), 790–797. doi: 10.1007/s10995-014-1570-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carleton RN, Thibodeau MA, Teale MJ, Welch PG, Abrams MP, Robinson T, & Asmundson GJ (2013). The Center for Epidemiologic Studies Depression Scale: A review with a theoretical and empirical examination of item content and factor structure. PLoS One, 8(3), e58067. doi: 10.1371/journal.pone.0058067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Data USA. (2017). Robeson County, NC: Retrieved from https://datausa.io/profile/geo/robeson-county-nc [Google Scholar]
- Dick S, Doust E, Cowie H, Ayres JG, & Turner S (2014). Associations between environmental exposures and asthma control and exacerbations in young children: A systematic review. BMJ Open, 4(2), e003827. doi: 10.1136/bmjopen-2013-003827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dieu H, Kearney GD, Bian H, Jones K, & Mohan A (2018). Asthma-related emergency department visits in North Carolina, 2010–2014. NC Medical Journal, 79(2), 81–87. doi: 10.18043/ncm.79.2.81. [DOI] [PubMed] [Google Scholar]
- Dow-Fleisner S & Hawkins SS (2018). Child physical well-being in the context of maternal depression. Social Work Research, 42(2), 95–105. doi: 10.1093/swr/svy006. [DOI] [Google Scholar]
- Estrada RD, & Ownby DR (2017). Rural asthma: Current understanding of prevalence, patterns, and internventions for children and adolescents. Current Allergy and Asthma Reports, 17(6), 37. doi: 10.1007/s11882-017-0704-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagnano M, Berkman E, Wiesenthal E, Butz A, & Halterman JS (2012). Depression among caregivers of children with asthma and its impact on communication with health care providers. Public Health, 162(12), 1051–1057. doi: 10.1016/j.puhe.2012.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fedele DA, Tooley E, Busch A, McQuaid EL, Hammond SK, & Borrelli B (2016). Comparison of secondhand smoke exposure in minority and nonminority children with asthma. Health Psychology, 35(2), 115–122. doi: 10.1037/hea0000220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gautier C & Charpin D (2017). Environmental triggers and avoidance in the management of asthma. Journal of Asthma and Allergy, 10, 47–56. doi: 10.2147/JAA.S121276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghaempanah Z, Fazlollahi RM, Noorbala AA, Movahedi M, Kazemnejad A, Pourpak Z, & Moin M (2013). Impact of maternal mental health on pediatric asthma control. Tanaffos Journal of Respiratory Diseases, Thoracic Surgery, Intensive Care and Tuberculosis, 12(4): 23–27. [PMC free article] [PubMed] [Google Scholar]
- Gibson-Young L, Turner-Henson A, Gerald L, Vance D, & Lorenzo D (2014). The relationship among family management behaviors and asthma morbidity in maternal caregivers of children with asthma. Journal of Family Nursing, 20, 442–461. doi: 10.1177/1074840714552845. [DOI] [PubMed] [Google Scholar]
- Glick AF, Tomopoulos S, Fierman AH, & Trasande L (2016). Disparities in mortality and morbidity in pediatric asthma hospitalizations, 2007 to 2011. Academic Pediatrics, 16(5), 430–437. doi: 10.1016/j.acap.2015.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holm S (1979). A simple sequentially rejective multiple test procedure. Scandanavian Journal of Statistics, 6, 65–70. [Google Scholar]
- Jamal A, Homa DM, O’ Connor E, Babb SD, Caraballo RS, Singh T, Hu SS & King BA (2016). Current cigarette smoking among adults -- United States, 2005–2014. Morbidity and Mortality Weekly Report (MMWR), 64(44): 1233–1240. [DOI] [PubMed] [Google Scholar]
- Kelley T & Kearney GD (2018). Insights into the environmental health burden of childhood asthma. Environmental Health Insights, 12, 1–3. doi: 10.1177/1178630218757445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knafl K, & Deatrick J (2006). Family management style and the challenge of moving from conceptualization to measurement. Journal of the Association of Pediatric Oncology Nurses, 23, 12–18. doi: 10.1177/1043454205283585. [DOI] [PubMed] [Google Scholar]
- Knafl K, & Deatrick J (2003). Further refinement of the Family Management Style Framework. Journal of Family Nursing, 9, 232–256. doi: 10.1177/1074840703255435. [DOI] [Google Scholar]
- Knafl KA, & Deatrick JA (1990). Family management style: Concept analysis and development. Journal of Pediatric Nursing, 5(1), 4–14. [PubMed] [Google Scholar]
- Knafl K, Deatrick JA, Gallo A, Dixon J, Grey M, Knafl G, & O’Malley J (2011). Assessment of the psychometric properties of the Family Management Measure. Journal of Pediatric Psychology, 36(5), 494–505. doi: 10.1093/jpepsy/jsp034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knafl KA, Deatrick JA, & Havill NL (2012). Continued development of the Family Management Style Framework. Journal of Family Nursing, 18(1), 11–34. doi: 10.1177/1074840711427294. [DOI] [PubMed] [Google Scholar]
- Knafl KA, Deatrick JA, Knafl GJ, Gallo AM, Grey M, & Dixon J (2013). Patterns of family management of chronic childhood conditions and their relationship to child and family functioning. Journal of Pediatric Nursing, 28(6), 523–535. doi: 10.1016/j.pedn.2013.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kub J, Bellin MH, Butz AM, Bollinger ME, Lewis-Land C, & Osteen P (2018). The chronicity of depressive symptoms in mothers of children with asthma. Western Journal of Nursing Research, 40(11), 1581–1597. doi: 10.1177/0193945917705858. [DOI] [PubMed] [Google Scholar]
- Landrigan PJ & Goldman LR (2011). Children’s vulnerability to toxic chemicals: A challenge and opportunity to strengthen health and environmental policy. Health Affairs, 30(5), 842–850. doi: 10.1377/hlthaff.2011.0151. [DOI] [PubMed] [Google Scholar]
- Liu AH, Zeiger RS, Sorkness CA, Ostrom NK, Chipps BE, Rosa K, … McDonald J (2010). The Childhood Asthma Control Test: Retrospective determination and clinical validation of a cut point to identify children with very poorly controlled asthma. Journal of Allergy and Clinical Immunology, 126(2), 267–273. doi: 10.1016/j.jaci.2010.05.031. [DOI] [PubMed] [Google Scholar]
- Long KA, & Marsland AL (2011). Family adjustment to childhood cancer: A systematic review. Clinical Child and Family Psychology Review, 14(1), 57–88. doi: 10.1007/s10567-010-0082-z. [DOI] [PubMed] [Google Scholar]
- Lowe AA, Bender B, Liu AH, Solomon T, Kobernick A, Morgan W, & Gerald LB (2018). Environmental concerns for children with asthma on the Navajo Nation. Annals of the American Thoracic Society, 15(6), 745–753. doi: 10.1513/AnnalsATS.201708-674PS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martell BN, Garrett BE, Caraballo RS (2016). Disparities in adult cigarette smoking -- United States, 2002–2005 and 2010–2013. Morbidity and Mortality Weekly Report (MMWR), 65(30), 753–758. [DOI] [PubMed] [Google Scholar]
- Medsker BH, Brew BK, Forno E, Olsson H, Lundholm C, Han Y, … Acosta-Perez E (2017). Maternal depressive symptoms, maternal asthma, and asthma in school-aged children. Annals of Allergy, Asthma &Immunology, 118(1), 55–60. doi: 10.1016/j.anai.2016.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merianos AL, Jandarov RA, Choi K, & Mahabee-Gittens M (2019). Tobacco smoke exposure disparities persist in U.S. children: NHANES 1999–2014. Preventive Medicine, 123, 138–142. doi: 10.1016/j.ypmed.2019.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moncrief T, Beck AF, Simmons JM, Huang B, & Kahn RS (2014). Single parent households and increased child asthma morbidity. The Journal of Asthma: Official Journal of the Association for the Care of Asthma, 51(3), 260–266. doi: 10.3109/02770903.2013.873806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- North Carolina American Indian Health Board and the Office of Minority Health and Health Disparities (2017). North Carolina American Indian Health Disparities Infographics (2017). Retrieved from https://files.nc.gov/ncdoa/NCAIHB-Infographics-Presentation.pdf?3qBUo1bkNJsqCEu5Wvffvaub8zPJ3w4i
- North Carolina Department of Health and Human Services and the Office of Minority Health and Health Disparities (2018). North Carolina health equity report 2018: Racial and ethnic health disparities in North Carolina. Raleigh, NC: State Center for Health Statistics. [Google Scholar]
- Odani S, Armour BS, Graffunder CM, Garrett BE, & Agaku IT (2017). Prevalence and disparities in tobacco product use among American Indians/Alaska Natives -- United States, 2010–2015. Morbidity and Mortality Weekly Report (MMWR), 66(50), 1374–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortiz-Lizcano CJ, Niederbacher-Velasquez J, & Diaz-Martinez LA (2016). Correlation between the Childhood-Asthma Control Test and the criterion for clinical asthma control. Health, 8, 623–629. doi: 10.4236/health.2016.87065. [DOI] [Google Scholar]
- Pak L, & Allen PJ (2012). The impact of maternal depression on children with asthma. Pediatric Nursing, 38(1), 11–19, 30. [PubMed] [Google Scholar]
- Quinto KB, Kit BK, Lukacs SL, & Akinbami LJ (2013). Environmental tobacco smoke exposure in children aged 3–19 years with and without asthma in the United States, 1999–2010. NCHS Data Brief, 126, 1–8. [PubMed] [Google Scholar]
- Radloff L (1977). The CES-D scale: A self report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. [Google Scholar]
- Searle A, Jago R, Henderson J, & Turner KM (2017). Children’s parents’, and health professionals’ views on the management of childhood asthma: A qualitative study. NPJ Primary Care and Respiratory Medicine, 27(1), 53. doi: 10.1038/s41533-017-0053-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh GK, Siahpush M, & Kogan MD (2010). Disparities in children’s exposure to environmental tobacco smoke in the United States, 2007. Pediatrics, 126(1), 4–13. doi: 10.1542/peds.2009-2744. [DOI] [PubMed] [Google Scholar]
- Sly PD, & Flack F (2008). Susceptibility of children to environmental pollutants. Annals of the NY Academy of Sciences, 1140, 163–183. doi: 10.1196/annals.1454.017. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau (2017). 2017 American Community Survey 1-Year Estimates: Table S0201. Generated by Gail Currin using American FactFinder. Retrieved from http://factfinder.census.gov. [Google Scholar]
- Vilagut G, Forero CG, Barbaglia G, Alonso J (2016). Screening for depression in the general population with the Center for Epidemiologic Studies Depression (CES-D): A systematic review with meta-analysis. PLoS One, 11(5), e0155431. doi: 10.1371/journal.pone.0155431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z, May SM, Charoenlap S, Pyle R, Ott NL, Mohammed K, & Joshi AY (2015). Effects of secondhand smoke exposure on asthma morbidity and health care utilization in children: A systematic review and meta-analysis. Annals of Allergy, Asthma, and Immunology, 115(5), 396–401. doi: 10.1016/j.anai.2015.08.005. [DOI] [PubMed] [Google Scholar]
- Wen C, Liu SH, Li Y, Sheffield P, & Liu B (2019). Pediatric asthma Among small racial/ethnic minority groups: An analysis of the 2006–2015 National Health Interview Survey. Public Health Reports, 134(4), 338–343. doi: 10.1177/0033354919849943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood BL, Brown ES, Lehman HK, Lehman HK, Khan DA, Lee MJ, & Miller BD (2018). The effects of caregiver depression on childhood asthma: Pathways and mechanisms. Annals of Allergy, Asthma, and Immunology, 121(4), 421–427. doi: 10.1016/j.anai.2018.06.031. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Wei M, & Shen N, & Zhang Y (2015). Identifying factors related to family management during the coping process of families with chronic childhood conditions: A multi-site study. Journal of Pediatric Nursing, 30, 160–173. doi: 10.1016/j.pedn.2014.10.002. [DOI] [PubMed] [Google Scholar]