ABSTRACT
The importance of apolipoprotein E (APOE) in late-onset Alzheimer's disease (LOAD) has been firmly established, but the mechanisms through which it exerts its pathogenic effects remain elusive. In addition, the sex-dependent effects of APOE on LOAD risk and endophenotypes have yet to be explained. In this Review, we revisit the different aspects of APOE involvement in neurodegeneration and neurological diseases, with particular attention to sex differences in the contribution of APOE to LOAD susceptibility. We discuss the role of APOE in a broader range of age-related neurodegenerative diseases, and summarize the biological factors linking APOE to sex hormones, drawing on supportive findings from rodent models to identify major mechanistic themes underlying the exacerbation of LOAD-associated neurodegeneration and pathology in the female brain. Additionally, we list sex-by-genotype interactions identified across neurodegenerative diseases, proposing APOE variants as a shared etiology for sex differences in the manifestation of these diseases. Finally, we present recent advancements in ‘omics’ technologies, which provide a new platform for more in-depth investigations of how dysregulation of this gene affects the development and progression of neurodegenerative diseases. Collectively, the evidence summarized in this Review highlights the interplay between APOE and sex as a key factor in the etiology of LOAD and other age-related neurodegenerative diseases. We emphasize the importance of careful examination of sex as a contributing factor in studying the underpinning genetics of neurodegenerative diseases in general, but particularly for LOAD.
KEY WORDS: APOE, Late-onset, Alzheimer's disease, Sex effect, Neurodegenerative diseases, Gene-by-sex interaction
Summary: The APOE ε4 allele and female sex are among the strongest risk factors for late-onset Alzheimer's disease. We explore how the interplay between these factors affects risk for this and other age-related neurodegenerative diseases.
Introduction
Apolipoprotein E (APOE) was the first discovered and is by far the strongest genetic risk factor for late-onset Alzheimer's disease (LOAD). Since the discovery of the association between the ε4 allele of APOE and LOAD risk (Roses, 1996; Strittmatter et al., 1993), the role of APOE and the protein it encodes, APOE, in disease pathogenesis has been rigorously investigated. Researchers discovered that APOE ε4 exerts a stronger effect on disease risk in females than in males (Payami et al., 1994), and, over the years, the sex-specific effect of APOE ε4 on LOAD has become extensively characterized. However, the molecular mechanisms underlying the role of APOE ε4 in disease pathogenesis overall and at a sex-specific level remain unknown.
Recently, several key reports have put the spotlight on APOE. Foremost, recent studies described the protective effects of the Christchurch mutation (R136S) in the APOE ε3 allele (Arboleda-Velasquez et al., 2019) and of APOE ε2 homozygosity (Reiman et al., 2020). In addition, recent single-cell genomics studies identified LOAD-associated differential expression of APOE in specific subpopulations of glial cells (Grubman et al., 2019; Mathys et al., 2019; Nott et al., 2019). These findings not only reaffirm the importance of the APOE gene in LOAD, but also pinpoint its role in microglia as the potential culprit in disease pathogenesis. However, whether these effects are sex specific remains unexplored.
Here, we review the literature on APOE, with a focus on its understudied neurobiological functions and the sex-specificity of its pathogenic effect in LOAD and other neurodegenerative diseases. Although many of the articles we cite use the term ‘gender’ (see Glossary, Box 1), we will use the term ‘sex’ (Box 1) to emphasize the biological differences. We discuss various mechanisms based on accumulating evidence to explain the sex-dependent role of APOE in neurodegeneration.
Box 1. Glossary.
3xTgAD mice: triple-transgenic mice harboring three human transgenes, each with mutations linked to familial Alzheimer's disease (AD) or frontotemporal dementia (APP KM670/671NL, MAPT P301L and PSEN1 M146V).
Amyloid-β (Aβ): the oligomeric peptide formed by proteolytic cleavage of amyloid precursor protein (APP); Aβ aggregates form one of the pathological hallmarks of (LO)AD, amyloid plaques.
APOE-targeted replacement (APOE-TR) mice: a humanized mouse model in which the murine Apoe gene is replaced with human APOE ε2, ε3 or ε4; human APOE expression is controlled by murine regulatory sequences.
APP/PS1 double-transgenic mice: a mouse model harboring two human transgenes, each with mutations linked to familial AD (APP KM670/671NL and PSEN1 L166P) and under the control of the neuron-specific Thy1 minigene promoter.
Blood-brain barrier: a semi-permeable barrier between peripheral tissues and the central nervous system formed by a border of endothelial cells connected by tight junctions.
Bulbar-onset ALS: a form of amyotrophic lateral sclerosis (ALS) beginning with symptoms such as slurred speech and difficulty swallowing; involves upper motor neurons in the brain stem.
Gender: a broad description of sex that encompasses social and cultural differences; not discussed in this Review.
J20 mice: transgenic mice that overexpress human APP with two mutations linked to familial AD (APP KM670/671NL and APP V717F), driven by the PDGFB promoter.
Hypothalamic-pituitary adrenal axis: a stress response system linking the central nervous system with the endocrine system; composed of the hypothalamus, the pituitary gland and the adrenal gland.
Incidence: number of individuals developing a disease within a given time period, divided by total individuals at risk; represents new cases developing in a given time period.
Life-long risk: probability that an individual of a given age will develop a disease during their remaining life span.
Limb-onset ALS: a form of ALS in which symptoms such as muscle weakness and twitching begin in the legs and arms; involves lower motor neurons in the spinal cord; also called spinal-onset ALS.
Long-term potentiation: electrophysiological and structural strengthening of synapses due to patterns of activity; widely thought to underlie learning and memory.
Neurotrophins: a class of secreted growth factor proteins involved in cell survival, growth and differentiation; promote neuronal function.
N-methyl-D-aspartate (NMDA) receptor (NMDAR): an excitatory ionotropic receptor activated upon binding of either glutamate or glycine ligands.
Polygenic risk score: a calculation to predict disease risk based on known common genetic risk variants.
PPAR-γ/PGC-1α pathway: the signaling mechanism between PPAR-γ, a nuclear receptor, and PGC-1α, a transcriptional coactivator, that supports neuronal function by activating genes involved in energy metabolism.
Prevalence: number of individuals with a disease divided by total individuals in the population; represents the number of existing cases.
Renin-angiotensin system: a circulating hormone system that promotes blood pressure regulation and hydroelectrolytic balance; dysfunction is implicated in hypertension and cardiovascular risk.
Sex: either of two biological categories based on sex chromosome composition: male (XY) or female (XX).
Tau: the main axonal microtubule-associated protein in the mammalian central nervous system that forms one of the pathological hallmarks of (LO)AD, neurofibrillary tangles.
Vascular dementia: a broad term for cognitive dysfunction caused by impaired blood flow to the brain, usually due to multiple strokes.
Sex differences in the epidemiology and manifestation of neurodegenerative diseases
Sex differences are established in the developing central nervous system during a period termed sexual differentiation, in which the brain is influenced by exposure to hormones and by changes in gene expression. These differences persist in the adult and aging brain, reflected in the neurological differences between healthy men and women. For example, synapse density is lower, whereas levels of tau (encoded by MAPT) and amyloid-β (Aβ; Box 1) are higher, in females than in males (Alonso-Nanclares et al., 2008; Buckley et al., 2019). Although women can be prone to developing neuropathology with aging, men are more likely to exhibit signs of neurodegeneration, especially in the hippocampus (Jack et al., 2017). However, once neurodegeneration begins in women, the rate of atrophy is faster than in men (Holland et al., 2013). These sex differences in how the healthy brain responds to the aging process may modulate susceptibility to developing neurodegenerative diseases.
LOAD
Women are at higher risk of developing LOAD (Hebert et al., 2001), and the prevalence (Box 1) of LOAD is higher in females than in males (Prince et al., 2016). Out of 5.6 million people in the USA with LOAD aged 65 and older, 3.5 million were women and 2.1 million were men in 2019 (Alzheimer's Association, 2019). This sex bias has been attributed to increased longevity of females, as age is the biggest risk factor for LOAD. However, the incidence and life-long risk (Box 1) of LOAD remains higher in females even after adjusting for age and lifespan (Alzheimer's Association, 2016, 2019; Ruitenberg et al., 2001), suggesting that there are other biological causes for this discrepancy. Furthermore, women with LOAD exhibit worse cognitive decline and neuropathology than men with LOAD (Irvine et al., 2012). In fact, the rate of cognitive decline and brain atrophy is faster in women with mild cognitive impairment (MCI) and LOAD (Holland et al., 2013; Hua et al., 2010; Koran et al., 2017), and the impact of the neuropathology on this decline is greater in women (Barnes et al., 2005).
However, some studies have failed to detect sex differences in LOAD progression (Edland et al., 2002), perhaps due to aspects of study design, geographic region, statistical power and method of confirming LOAD diagnosis, such as with autopsy. Alarmingly, one meta-study found dramatic inconsistencies between clinical diagnoses and autopsy results, with less than 42% of participants across two studies showing alignment between LOAD pathology and diagnosis (Schneider et al., 2009). These inconsistencies, combined with a dearth of studies reporting findings stratified by sex (Fiest et al., 2016), present challenges for understanding whether women are truly more vulnerable to the development of LOAD. Nevertheless, there are compelling biological factors that generate hypotheses explaining why the female brain is more susceptible to this disease.
Other neurodegenerative diseases
Sex differences have also been reported in the development and progression of multiple sclerosis (MS), Parkinson's disease (PD), dementia with Lewy bodies (DLB) and amyotrophic lateral sclerosis (ALS). MS is an autoimmune demyelinating disease with sex differences in prevalence, symptoms and severity. MS is more prevalent in women (Ramagopalan et al., 2010), who experience more frequent relapses and more inflammatory lesions (Kalincik et al., 2013; Pozzilli et al., 2003). Conversely, men with MS exhibit faster progression, exacerbated neurodegeneration and cognitive impairment, and greater cerebellar involvement (Antulov et al., 2009; Confavreux et al., 2003; Schoonheim et al., 2012).
Lewy body-spectrum diseases, including PD and DLB, also exhibit sex biases. PD is more prevalent in men than in women by a sex ratio of roughly 2:1 (Baldereschi et al., 2000). Similarly, DLB is more common in men (Savica et al., 2013). However, women with PD tend to exhibit increased mortality, dyskinesia, tremor and non-motor symptoms such as mood and sleep disturbances (Chandran et al., 2014; Dahodwala et al., 2016; Haaxma et al., 2007; Solla et al., 2012). Other aspects of PD, such as motor dysfunction and cognitive impairment, are more severe in men (Chandran et al., 2014; Lubomski et al., 2014; Szewczyk-Krolikowski et al., 2014).
Finally, ALS is a motor neuron disease that is more common and has an earlier age of onset in men than in women (Georgoulopoulou et al., 2011; McGuire et al., 1996). The clinical features of ALS are sex dependent, as women are more likely to develop bulbar-onset ALS (Box 1), whereas men are more likely to develop limb-onset ALS (Box 1) (Manjaly et al., 2010). Interestingly, a rare flail-arm presentation is much more common in men (Wijesekera et al., 2009), and men are also more likely to become cognitively impaired due to ALS (Portet et al., 2001). Biomarker studies suggest that ALS is more severe in men, but the disease-associated inflammatory response is exaggerated in women (Boylan et al., 2009; Nygren et al., 2002). In this Review, we propose the involvement of APOE polymorphisms in the manifestation of sex differences across these neurodegenerative diseases (Box 2).
Box 2. APOE in shared sex-specific etiology across neurodegenerative diseases.
Multiple sclerosis (MS)
• The APOE ε4 allele worsens MS severity in men (Table 1).
• ε4-associated APOE dysfunction is detrimental to myelin maintenance and repair (Bartzokis et al., 2006; Dean et al., 2014) and anti-inflammatory processes (Mailleux et al., 2017).
• Estrogen likely mediates a neuroprotective response in male brains, as local upregulation of aromatase and ERβ occurs near MS lesions in the male central nervous system (Luchetti et al., 2014), and genetic variance that reduces estrogen levels increases MS severity in men (Qureshi et al., 2017).
• Because APOE is required for some of the protective effects of estrogen, the ε4 allele likely exacerbates disease severity in males via impaired function of APOE.
• Therefore, a combination of myelin impairment, neuroinflammation and loss of estrogen-mediated neuroprotection might contribute to ε4-associated MS severity in men.
Lewy body spectrum diseases
• APOE polymorphisms contribute to sex-specific risk for Parkinson's disease (PD) and dementia with Lewy bodies (DLB) (Table 1).
• The APOE ε4 allele worsens α-synuclein pathology (Davis et al., 2020; Dickson et al., 2018; Zhao et al., 2020a) and cognitive function in PD (Mata et al., 2014).
• Dopamine transporter activity in the nigrostriatal dopaminergic system may underlie sex-specific vulnerability for developing PD (Gillies and McArthur, 2010), as males exhibit less efficient uptake and vesicular packaging of dopamine than females (Bhatt and Dluzen, 2005), possibly due to male-specific gene expression (Cantuti-Castelvetri et al., 2007) or renin-angiotensin system activity in the substantia nigra (Rodriguez-Perez et al., 2010).
• Estrogen attenuates the neurotoxic effects of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP), commonly used to induce PD in in animal models, on striatal dopamine release in female, but not male, rats (Disshon and Dluzen, 2000).
• Therefore, male dopaminergic neurons may be less responsive to the protective effects of estrogen, an effect exacerbated by lower plasma estradiol levels observed in male PD patients (Nitkowska et al., 2015).
• Collectively, these findings suggest that male dopaminergic neurons are more vulnerable to the pathogenic effects of the APOE ε4 isoform, making PD more prevalent and severe in men than in women.
Amyotrophic lateral sclerosis (ALS)
• The APOE ε4 allele increases the risk for bulbar-, but not limb-onset, ALS in males (Table 1).
• Androgens have toxic effects on motor neurons (Katsuno et al., 2002); however, motor neuron atrophy can also arise from androgen insensitivity due to reduced androgen receptor (AR) expression (Grunseich et al., 2014).
• Because androgens can reverse some of the toxic effects of the ε4 isoform (Raber et al., 2002), ε4-positive males may be protected against limb-onset ALS due to the increased abundance of ARs in spinal motor neurons compared to other populations of motor neurons (Lumbroso et al., 1996; Sar and Stumpf, 1977).
• More sex-specific genetic polymorphisms associated with ALS continue to be discovered (Dunckley et al., 2007), warranting further research in this area.
• Of note, there is considerable clinical and genetic overlap between ALS and a related group of neurodegenerative diseases known as frontotemporal dementia, particularly in the development of TDP-43 (TARDBP) pathology (Boeve et al., 2012). Although APOE ε4 was observed to be a risk factor for TDP-43 pathology in LOAD (Wennberg et al., 2018), whether or not this applies to ALS and frontotemporal dementia or has a sex-specific role remains to be determined.
Non-genetic sex-dependent determinants in LOAD
Vascular and metabolic factors
Cardiovascular and metabolic conditions that develop in mid-life are risk factors for neurodegenerative diseases and increase the likelihood of cognitive dysfunction in late life (Kritz-Silverstein et al., 2017). The interactions of these conditions with risk for neurodegenerative disease is different between men and women. Men tend to have more coronary artery disease and cardiac arrhythmias, which correlate with LOAD biomarkers (Vemuri et al., 2017). This could explain the increased risk for vascular dementia (Box 1) in males (Ruitenberg et al., 2001), hypothesized to be attributed to a reduced activity of enzymes in the renin-angiotensin system (Box 1) specifically in males (Fernandez-Atucha et al., 2017). Interestingly, although hypertension is more common in middle-aged men, it is only a risk factor for dementia in women (Gilsanz et al., 2017) and is only associated with reduced cortical thickness in women (Kim et al., 2019). Women with poor metabolic phenotypes and high blood pressure have impaired cognitive performance compared to healthy post-menopausal women (Rettberg et al., 2016). In addition, men who survive to advanced age tend to have healthier cardiometabolic profiles overall, a survival bias that may contribute to the finding that women are at increased risk for neurodegenerative disease (Chêne et al., 2015).
Inflammation
Generally, high levels of inflammation caused by vascular and metabolic disorders can increase one's risk for neurodegenerative diseases. Females are known to have a more robust peripheral immune response than males, which might relate to increased susceptibility to autoimmune disease. Studies showing sex differences in microglia, the immune cells of the brain, during neurodevelopment suggest that perturbation of immune pathways during early life stages may increase inflammation levels later in life and therefore increase the risk for neurodegenerative diseases. The proliferation and morphology of microglia in the developing mammalian brain is sex dependent, with males exhibiting greater densities of microglia, especially those of amoeboid morphology (Lenz et al., 2013; Schwarz et al., 2012). Acute immune activation with lipopolysaccharide accelerates the development of hippocampal microglia derived from male, but not female, wild-type mice (Hanamsagar et al., 2017), suggesting that higher sensitivity of the male brain to inflammation may accelerate microglial aging, affecting vulnerability to neurodegenerative disease. Indeed, sex differences found in developing microglia persist into adulthood, suggesting that sex-dependent microglial traits are determined at birth. In adult mice, male microglia display a pro-inflammatory bias, whereas female microglia express more genes involved in protection and repair mechanisms (Guneykaya et al., 2018; Villa et al., 2018). In support of the latter, female microglia respond more efficiently than male microglia to brain injury (Villa et al., 2018). In contrast, males display increased variability of microglial-specific gene expression with aging (Mangold et al., 2017), which might contribute to the development of neurological diseases. There is undoubtedly a relationship between the immune system and the development of LOAD, as most risk genes for this disease, including CLU, TREM2, MS4A6A, CD33, PICALM and ABCA7 (Jansen et al., 2019; Kunkle et al., 2019), encode proteins related to immune functions. Whether or not the functional impact of these genetic variants differs between men and women, at the genomic or cellular level, remains to be studied.
Sex hormones
Changes in hormone levels with aging can increase susceptibility to neurodegenerative diseases, as the human brain responds to estrogen, androgen and progesterone throughout life. Estrogen receptors are widely expressed in the brain, including in regions involved in learning and memory (Hutson et al., 2019), leading to the activation of both genomic and non-genomic pathways to regulate a range of neurobiological processes. Genomic pathways are mediated by the translocation of estrogen receptors (ERα and ERβ) to the nucleus upon estrogen binding (Kocanova et al., 2010). These estrogen-bound receptors can bind to estrogen response element motifs in chromatin (Palaniappan et al., 2019), transcription factors (Teyssier et al., 2001) or other coactivators (Shang et al., 2000) to modulate gene expression. The genes affected by estrogen treatment are involved in glucose transport and metabolism, mitochondrial function, inflammation, cholesterol homeostasis and myelination (Sárvári et al., 2011; Voskuhl et al., 2019; Zhao et al., 2012).
Aside from regulating gene expression, estrogen signaling directly affects the electrophysiological properties of neurons (Zhang et al., 2010), regulates long-term potentiation (Box 1) (Mukai et al., 2010) and promotes the activation of proteins with known roles in synaptic plasticity such as PSD-95 (DLG4) (Spencer-Segal et al., 2012). As estrogen receptors are located on axons, they are ideally positioned to regulate plasticity, and this axonal localization is more pronounced in female compared to male mice (Waters et al., 2015). The effects of estrogen on neuronal plasticity extend to structural factors, affecting the density and morphology of dendritic spines of hippocampal neurons (Mukai et al., 2010). Estrogen mitigates cellular stress by counteracting the production of reactive oxygen species and oxidative damage (Kemper et al., 2014; Numakawa et al., 2011), and has established anti-inflammatory properties, including reduction of microglial pro-inflammatory cytokine secretion (Habib et al., 2013). Finally, estrogen has been labeled as a master regulator of brain bioenergetics, helping to meet the high energy demands of neurons by increasing mitochondrial biogenesis and energy production via key elements in the tricarboxylic acid cycle, oxidative phosphorylation, respiratory efficiency and ATP synthesis (Kemper et al., 2014; Nilsen et al., 2007).
The irregular fluctuations in estrogen during the perimenopausal transition, as well as the dramatic loss of estrogen post-menopause, may make the female brain vulnerable to pathology and neurodegeneration via an ovarian-neural estrogen axis. In support of this, early surgical menopause doubles dementia risk, LOAD pathology and cognitive decline (Bove et al., 2014). In addition, loss of estradiol leads to hippocampal dysfunction (Jacobs et al., 2016; Rentz et al., 2017), and a reduced lifelong exposure to estrogen caused by delayed menarche and early menopause is associated with increased dementia risk (Gilsanz et al., 2019). Post-menopausal women with LOAD exhibit dysregulated alternative splicing of estrogen receptors, lower brain levels of estrogen and reduced estrogen sensitivity (Ishunina and Swaab, 2012; Rosario et al., 2011; Weiss et al., 2004), exacerbating the effect. In one study, post-menopausal women receiving hormone replacement therapy had reduced mortality due to LOAD and dementia (Manson et al., 2017). However, other reports suggest that hormone replacement therapy actually worsens cognitive decline, as discussed in a recent review (Marongiu, 2019).
Perimenopause coincides with the prodromal phase of LOAD, about 20 years before clinical diagnosis, a phase during which the pathological hallmarks of the disease, such as gliosis, begin to manifest (Jack et al., 2013). Increased indicators of LOAD endophenotypes, including hypometabolism, Aβ deposition and reductions in brain volume also begin at perimenopause (Mosconi et al., 2017a,b). Conditions like sleep disturbances and depression, which can arise during perimenopause, are associated with LOAD-like cognitive dysfunction and LOAD risk (Freeman et al., 2009; Hahn et al., 2014; Norton et al., 2014). During perimenopause, the female brain enters a hypometabolic state (Brinton et al., 2015), triggering a switch in energy source from glucose to ketone bodies (Yao et al., 2010), which are primarily derived from white matter (Klosinski et al., 2015). Perhaps due to this ketogenic switch, females, but not males, with LOAD and cerebrovascular disease exhibit dysregulation of myelin basic protein, a regulator of myelination (Gallart-Palau et al., 2016). Taken together, these findings suggest that menopause and the associated glucose hypometabolism are key players in determining female-specific susceptibility to LOAD. Because of the highly variable trajectory of hormone decline in women (Tepper et al., 2012), well-controlled research that includes reliably diagnosed perimenopause is needed to establish whether estrogen irregularities versus declines underlie the female-specific LOAD risk.
Similar to estrogen, testosterone has neuroprotective effects in brain; for example, against oxidative stress, neuronal injury and apoptosis through androgen receptors (Ahlbom et al., 2001; Hammond et al., 2001; Pike, 2001). Testosterone promotes neuronal growth (Brannvall et al., 2005), neurite outgrowth (Marron et al., 2005) and hippocampal long-term potentiation (Schulz and Korz, 2010). Consistent with these findings, reductions in androgens compromise brain function. Similar to menopause in women, men undergo a process known as andropause or androgen deficiency in aging males. This is more gradual than menopause and is not necessarily coupled to loss of reproductive function, but rather to dysfunction of androgen-responsive tissues (Feldman et al., 2002; Muller et al., 2003). Andropause is associated with cognitive dysfunction in men (Cherrier et al., 2015) and with risk for neurodegenerative diseases (Rosario et al., 2011). Men with LOAD have even lower levels of testosterone than age-matched, cognitively healthy men, further emphasizing the effects of testosterone loss in old age (Rosario et al., 2011). Some conflicting findings show that androgens can actually be harmful by reducing neuron survival (Johnson et al., 2010), but this may depend on the specific cell population and type of cellular stress being studied (Cunningham et al., 2009).
Growing evidence indicates that the neuroprotection conferred by sex hormones can counteract some aspects of neurodegenerative disease. At a genomic level, estrogen globally upregulates genes found to be downregulated in LOAD, especially those related to synaptic and mitochondrial function (Ratnakumar et al., 2019). In addition, testosterone supplementation in older men modestly improves cognition (Wahjoepramono et al., 2016). Sex hormones have also been shown to be neuroprotective against Aβ and tau toxicity (Park et al., 2007; Pike, 2001; Wang et al., 2016), as well as the mitochondrial deficits associated with these pathologies (Grimm et al., 2016).
APOE: a sex-dependent genetic determinant in LOAD
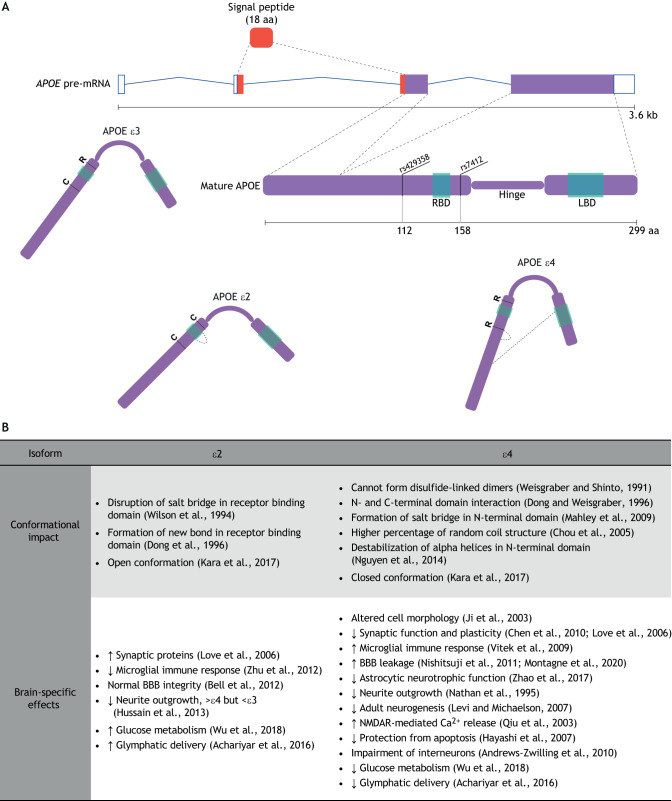
APOE encodes three protein isoforms designated ε2, ε3 and ε4 based on two single-nucleotide variants that alter the amino acid sequence at positions 112 (rs429358, C/T) and 158 (rs7412, C/T) (Weisgraber, 1994) (Fig. 1A). The frequencies of the alleles in the global population are 7% for ε2, 79% for ε3 and 14% for ε4, with the ε3/3 (62%), ε3/4 (22%) and ε2/3 (11%) genotypes being the most common (Bertram et al., 2007). The amino acid differences at positions 112 and 158 affect protein conformation relative to the more common ε3 allele (Fig. 1A), and studies show that these consequently affect APOE biology and its brain-specific functions (Fig. 1B). As outlined in Fig. 1B, unique domain interactions in the ε2 (Dong et al., 1996; Wilson et al., 1994) and ε4 (Dong and Weisgraber, 1996; Mahley et al., 2009) isoforms result in a more open or closed conformation, respectively, compared to ε3 (Kara et al., 2017). In addition, hydrophobic residue exposure is exaggerated in the ε4 isoform compared to ε3 (Chou et al., 2005), leading to structural instability, increased lipid-binding efficacy (Nguyen et al., 2014) and inability to dimerize (Weisgraber and Shinto, 1991). These contrasting conformational properties between APOE isoforms have consequences for synaptic function (Chen et al., 2010; Love et al., 2006; Qiu et al., 2003), glial cell function (Vitek et al., 2009; Zhu et al., 2012), blood-brain barrier (Box 1) integrity (Bell et al., 2012; Montagne et al., 2020; Nishitsuji et al., 2011), generation and differentiation of newborn neurons (Levi and Michaelson, 2007; Nathan et al., 1995), and distribution of APOE in the brain (Achariyar et al., 2016). The following section explores the multifunctional nature of APOE in the brain, explaining why differential effects of APOE isoforms extend to cell survival (Andrews-Zwilling et al., 2010; Hayashi et al., 2007; Zhao et al., 2017), glucose delivery to cells (Wu et al., 2018), formation of toxic fragments (Huang et al., 2001; Love et al., 2017) and gene expression patterns (Lin et al., 2018) (Fig. 1B).
Fig. 1.
APOE variants differentially affect its conformational properties and biological effects in the brain. (A) Diagram of APOE pre-mRNA, which consists of four exons to encode a 317-residue pre-APOE protein. An 18-residue signal peptide is co-translationally removed from pre-APOE (Lin-Lee et al., 1981; Zannis et al., 1984) to produce the mature 299-aa APOE, which consists of N-terminal and C-terminal arms connected by a hinge region (Wetterau et al., 1988). A receptor-binding domain (RBD) is located in the N-terminal arm (Wilson et al., 1991), while a lipid-binding domain (LBD) is located in the C-terminal arm (Weisgraber, 1990). Two single-nucleotide variants affect the aa sequence around the RBD – rs42958 (aa 112, C→R, ε4, 14% allele frequency) and rs7412 (aa 158, R→C, ε2, 7% allele frequency) (Bertram et al., 2007). These aa changes result in different APOE isoforms with altered functions. The schematic drawings of the three isoforms illustrate the shapes as described in B. (B) Table listing the effects of aa changes in the ε2 and ε4 isoforms of APOE relative to ε3, except where otherwise specified. aa, amino acids; BBB, blood-brain barrier; kb, kilobases; NMDAR, N-methyl-D-aspartate receptor.
Brain-specific functions of APOE
A number of recent reviews discuss the structure and function of APOE (e.g. Abondio et al., 2019; Marais, 2019). However, as APOE biology in the brain is distinct from that in the periphery, a summary of its brain-relevant functions here provides helpful context for understanding subsequent discussions of its sex-specific role in LOAD. The glycoprotein APOE is coded from four exons on chromosome 19 (Fig. 1A). APOE is composed of an N-terminal arm that contains a receptor-binding domain, and a C-terminal arm, which contains a lipid-binding domain (Fig. 1A). To resolve the three-dimensional structure of monomeric APOE, a recent study combined cross-linking and mass spectrometry at high resolution to show that APOE is highly dynamic, adapting its conformation to dimerize and bind receptors and lipids (Henry et al., 2018). APOE is a lipid-transport protein expressed most highly in the liver and kidney, but also at relatively high levels in most areas of the brain (Fagerberg et al., 2014). In the brain, APOE is predominantly expressed in astrocytes and, to a lesser extent, in microglia and neurons (Xu et al., 2006), and the major APOE pathway in the brain is astrocyte derived. Naïve APOE secreted from astrocytes undergoes lipidation to form high-density lipoprotein (HDL) particles (Fagan et al., 1999). Although APOE has many interacting partners, it is mainly lipidated by the ATP-binding cassette transporter ABCA1 (Kim et al., 2007). Lipid-rich APOE then interacts predominantly with low-density lipoprotein (LDL) receptors (LDLRs) on microglia and neurons, facilitating the endocytosis of cholesterol and phospholipids. Single-cell genomics studies align with growing evidence indicating cell type-specific functions of APOE (Box 3).
Box 3. APOE and single-cell genomics studies of LOAD.
The brain is a highly heterogeneous tissue composed of many different cell types. The notion of cell type-specific responses to LOAD progression is not novel – it has been firmly established that neurons are lost, whereas glial cells proliferate. Multiple lines of evidence suggest that the function of APOE is cell type specific. For instance, while most astrocytes express APOE, a subset do not, and a subset of microglia do not increase APOE production in response to injury (Xu et al., 2006). In addition, APOE from specific cell types has stronger affinities for specific receptors; for instance, astrocyte-derived APOE has a strong affinity for LDLR (Fryer et al., 2005). LRP1 is mainly found on neurons, whereas LDLR is more prominently expressed in glia (Rapp et al., 2006), possibly inducing cell type-specific downstream effects of APOE. Advanced single-cell technologies now allow researchers to interrogate cell subtype-specific genomic profiles with unprecedented cellular resolution and are becoming more widespread. Two recent single-cell studies of human brain tissue derived from LOAD and healthy control subjects characterized the cell type-specific pathogenic mechanisms of LOAD and revealed that APOE is upregulated in a disease-associated subpopulation of microglia, whereas it is downregulated in oligodendrocyte and astrocyte subpopulations (Grubman et al., 2019; Mathys et al., 2019). These findings are highly significant for our understanding of APOE function and dysfunction in the brain, and may open the door for novel therapeutic strategies such as genome editing systems that target specific cell subpopulations.
APOE redistributes lipids between cells, modulating lipid homeostasis in the brain. Lipids are central to the structure and function of all cells, as they are the principal components of cell membranes, contributing to membrane fluidity and remodeling. There is a particularly high demand for lipids such as cholesterol in the brain, which contains up to 25% of the body's total cholesterol (Bjorkhem and Meaney, 2004). Although there are other cholesterol transporters throughout the body, APOE is by far the most abundant in the brain. As a regulator of brain cholesterol homeostasis, APOE plays a role in many of the same functions that require cholesterol, including neurite outgrowth in cultured olfactory epithelia (Hussain et al., 2013), synapse formation in cultured retinal ganglion cells (Mauch et al., 2001), maintenance of myelin as shown by diffusion tensor imaging of healthy human adults (Westlye et al., 2012), synaptic integrity and plasticity as demonstrated by Apoe knockout mice (Lane-Donovan et al., 2016), and dendritic complexity of neurons in both APOE-targeted replacement (APOE-TR) mice (Box 1) and human LOAD patients (Ji et al., 2003). APOE also helps maintain the structural integrity of the blood-brain barrier in immune-challenged wild-type compared to Apoe knockout mice (Zheng et al., 2014), regulates the development of newborn neurons during adult neurogenesis, as shown by comparing wild-type, Apoe knockout and APOE-TR mice (Tensaouti et al., 2018), and helps remove debris from degenerating cells in wild-type mice with induced demyelinating lesions in the brain (Cantuti-Castelvetri et al., 2018). The involvement of APOE in such a diverse array of functions adds layers of complexity to understanding its biological function in the brain and in neurodegenerative diseases.
APOE and sex hormones
APOE is regulated by estrogen, progesterone and testosterone, raising the possibility that hormone-APOE interactions underlie the sex differences in susceptibility to neurodegenerative disease and, furthermore, that the role of APOE in LOAD pathogenesis is sex specific. Estrogen increases the synthesis and expression of APOE in the brain (Ratnakumar et al., 2019; Zhao et al., 2012). Downstream effects of estrogen administration on APOE expression depend on whether ERα or ERβ is predominantly activated. Wang and colleagues used cultured rat hippocampal neurons and an in vivo rat model to show that Apoe mRNA and protein expression increase in response to ERα activation and decrease by ERβ activation (Wang et al., 2006); however, ERα can outcompete and displace ERβ from chromatin (Charn et al., 2010).
APOE facilitates the neuroprotective effects of estrogens and androgens. Estradiol-mediated increases in APOE result in neurite outgrowth in cultured mouse cortical neurons (Nathan et al., 2004), and in neuronal maturation and synaptogenesis in the murine olfactory bulb (Nathan et al., 2010). APOE is also required for estrogen-mediated neuroprotection in a mouse model of global ischemia (Horsburgh et al., 2002). In addition, studies suggest a link between estrogen-APOE neuroprotection and the hypothalamic-pituitary adrenal axis (Box 1). Cortisol/corticosterone exacerbates neurotoxicity (Goodman et al., 1996), and estrogen counteracts this via an ERα-corticotropin-releasing hormone-binding protein (CRH-BP) pathway (van de Stolpe et al., 2004). APOE may be involved in tonic inhibition of the hypothalamic-pituitary adrenal axis through estrogen signaling via reduction of cortisol levels (Raber et al., 2000). Testosterone has similar APOE-mediated anti-inflammatory effects to estrogen (Brown et al., 2007).
The literature on cholesterol metabolism and menopause provides further evidence for a mechanistic link between estrogen and APOE. Estrogen regulates elements of cholesterol synthesis and uptake, including LDLR-related protein 1 (LRP1), LDLR (Cheng et al., 2007) and hydroxymethylglutaryl-CoA reductase (HMG-CR) (De Marinis et al., 2008). HMG-CR transcription is activated by SREBP2, which is co-activated with APOE by cholesterol metabolism in astrocytes (Abildayeva et al., 2006). These studies suggest a potential convergence of estrogen and APOE signaling on the SREBP2/HMG-CR pathway to regulate cholesterol transport and homeostasis in the brain. This pathway may affect Aβ and tau pathology through LRP1 and cholesterol-ester mechanisms (van der Kant et al., 2019). In fact, APOE ε4-mediated Aβ pathology likely depends on LRP1, as LRP1 deficiency in neurons blocks the APOE ε4-mediated exacerbation of amyloid plaque burden in APP/PS1 (PSEN1) double-transgenic mice (Box 1) (Tachibana et al., 2019). Estrogen also reduces LDL cholesterol levels (Ghosh et al., 2015; Hussain et al., 2015); however, it remains unknown whether this affects APOE and/or lipid homeostasis in the brain. Finally, APOE genotype modulates estradiol levels and age at menopause – the ε3/ε3 genotype is associated with later menopause and lower estradiol serum concentrations than the other five genotypes (Ryl et al., 2016), while another study found that the presence of at least one ε2 allele is associated with later menopause than ε3/ε3 (Tempfer et al., 2005). Early menopause is thought to be linked to increased LOAD risk due to reduced life-long exposure to estrogen (Gilsanz et al., 2019).
In conclusion, owing to the interactions of APOE and sex hormones through various pathways, fluctuations and/or loss of estrogens at perimenopause and post-menopause may contribute to the increased susceptibility to and severe manifestation of LOAD in females through APOE. The presence of the high-risk APOE ε4 allele might further exacerbate this sex-specific effect.
APOE ε4
It has been firmly established that the APOE ε4 allele increases the risk for developing non-Mendelian AD (Roses, 1996; Strittmatter et al., 1993). APOE ε4 is associated with earlier disease onset (Corder et al., 1993), heavier amyloid pathology (Jack et al., 2015; Schmechel et al., 1993), increased brain atrophy (Agosta et al., 2009; Tosun et al., 2010) and faster rate of disease progression (Stone et al., 2010). A multi-center meta-analysis genome-wide association study (GWAS) showed that of all genetic loci contributing to LOAD risk, the APOE linkage disequilibrium region is by far the strongest (Kunkle et al., 2019). This association was attributed, at least in part, to APOE ε4.
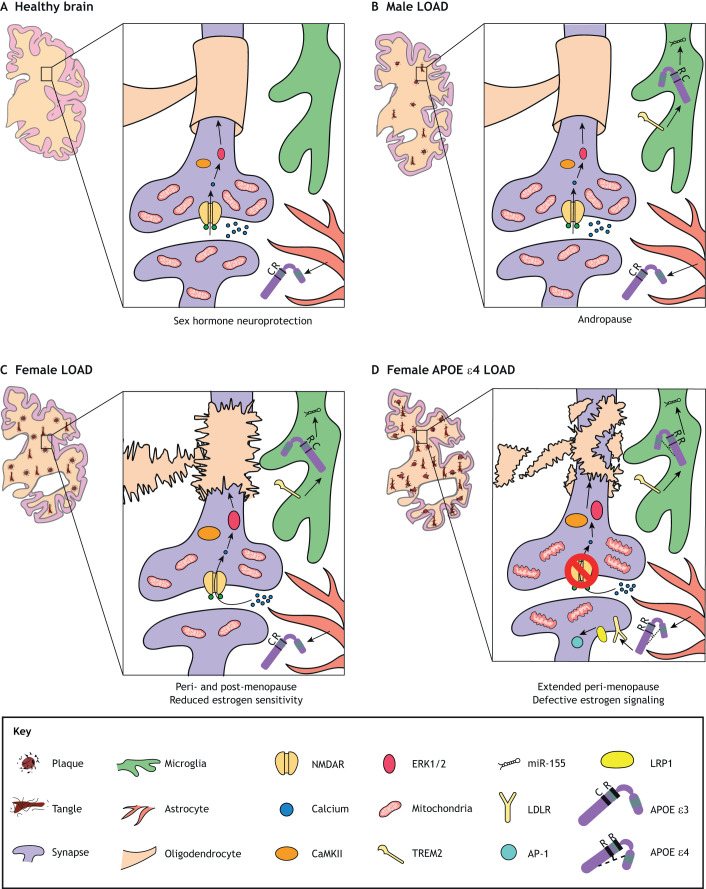
Studies have demonstrated a greater risk and earlier development of LOAD (Bretsky et al., 1999; Fisher et al., 2018; Poirier et al., 1993) and a higher MCI-LOAD conversion risk (Altmann et al., 2014) in ε4-carrier females than ε4-carrier males. Strikingly, one study found that heterozygote ε4/– women have the same level of risk as homozygote ε4/ε4 men (Payami et al., 1994). In addition to increased risk for LOAD, female carriers of APOE ε4 exhibit more severe presentation of endophenotypes including more severe Aβ and tau pathology (Corder et al., 2004), worse cognitive decline (Beydoun et al., 2012; Lin et al., 2015) and worse atrophy (Fleisher et al., 2005; Sampedro et al., 2015) (Fig. 2). Although the vast majority of studies on the relationship between APOE ε4 and LOAD risk showed increased vulnerability in women compared to men, some reported conflicting findings (Fisher et al., 2018). However, these age-matched studies do not account for sex differences in age of diagnosis and disease trajectories, which are accelerated in females (Corder et al., 2004; Cosentino et al., 2008; Holland et al., 2013). The confounding effects of increased cardiovascular disease risk in men can also influence the results due to survival bias (Beydoun et al., 2013).
Fig. 2.
Exacerbation of LOAD neurodegeneration and pathology by female sex and APOE ε4, and hypothesized mechanisms. (A) The healthy APOE ε3/ε3 brain benefits from neuroprotection conferred by sex hormones, with abundant mitochondria at synapses, intact myelin, intact NMDAR-mediated neuroplasticity and homeostatic microglia. (B) The male LOAD brain exhibits degeneration, neuropathology, reduced mitochondria and pro-inflammatory signature in microglia, in part due to the gradual loss of sex hormones during andropause. (C) With fluctuations and declines in sex hormones at peri- and post-menopause, in addition to reduced estrogen sensitivity, the female LOAD brain exhibits more severe atrophy and neuropathology, loss of mitochondria and myelin abnormalities. (D) APOE ε4 is associated with defective estrogen signaling and a delay in menopause, which may lengthen the perimenopausal transition period of intense estrogen level fluctuations. Therefore, the female APOE ε4-positive LOAD brain exhibits the most severe atrophy and neuropathology, disruption of the myelin sheath, mitochondrial deficits, impairments in neuroplasticity and increased activation of AP-1, which drives APP expression and, consequently, Aβ deposition. LDLR, low-density lipoprotein receptor; LRP1, LDLR-related protein 1; NMDAR, N-methyl-D-aspartate receptor.
The mechanisms underlying this female-specific effect of the APOE ε4 allele on LOAD risk are largely unknown, but studies suggest that the APOE ε4 allele exacerbates the effects of fluctuations/loss of sex hormones during peri-/post-menopause. APOE ε4 negates the beneficial effects of estrogen on neurite extension (Nathan et al., 2004) and on anti-inflammatory responses in microglia (Brown et al., 2008). The APOE ε4 allele can also have an additive effect on LOAD-associated brain glucose hypometabolism (Ossenkoppele et al., 2013; Reiman et al., 2005), as this allele contributes to glucose hypometabolism even in the absence of neurodegeneration and cognitive decline (Knopman et al., 2014; Sundermann et al., 2018). As the ε4 allele is associated with delayed menopause (Meng et al., 2012), it perhaps lengthens the perimenopausal transition and worsens glucose hypometabolism. A proposed mechanism underlying ε4-associated hypometabolism is the inhibition of the PPAR-γ/PGC-1α (PPARGC1A) pathway (Box 1), which supports neuronal function by promoting mitochondrial energy production (Wu et al., 2018). APOE ε4 is thought to reduce PGC-1α activity via downregulation of the deacetylase sirtuin 1 (SIRT1) (Theendakara et al., 2016). Because estrogen counteracts this mechanism by upregulating SIRT1 (Theendakara et al., 2016), age-related estrogen loss in women may exacerbate ε4-induced brain hypometabolism. In line with the ketogenic switch that co-occurs with menopause and the fact that ketone bodies are primarily derived from white matter, LOAD and its associated endophenotypes are linked to reductions in white matter and dysregulation of myelination (Gallart-Palau et al., 2016; Mosconi et al., 2017b), and ε4 homozygotes exhibit increased white matter diffusivity, most likely due to myelin sheath disruption (Operto et al., 2018). Overall, these findings support the idea that estrogen loss underlies the increased vulnerability to neurodegeneration in the APOE ε4-positive female brain via energy imbalance (Fig. 2).
The sex-specific effects of APOE ε4 can also occur at a genomic level. APOE ε4 acts as a transcription factor in the brain, binding the promoter regions of genes associated with programmed cell death, microtubule disassembly, synaptic function and aging (Theendakara et al., 2016). APOE ε4-mediated transcriptional activity was found to be sex specific, with genes involved in regulation of the immune system response, inflammation, oxidative stress, aging and estrogen signaling showing different patterns of activation between female and male ε4-positive brains (Hsu et al., 2019). One comparative study found that the ε4 isoform activates transcription factors like AP-1 more strongly than ε3 does in induced human-derived neurons and glia (Lin et al., 2018). ε4-associated AP-1 activation promotes APP transcription, leading to a rise in Aβ levels (Huang et al., 2017).
The presence of an ε4 allele may also exacerbate disease pathogenesis and progression due to the absence of ε2- or ε3-associated neuroprotection. APOE ε2 is more neuroprotective in women than in men, promoting survival and longevity (Rosvall et al., 2009; Schachter et al., 1994). Another study found that APOE ε2 reduces LOAD risk in women more than in men (Neu et al., 2017); however, a more recent study did not confirm this (Reiman et al., 2020). APOE ε3 may also be more protective against neurodegeneration in women, as this allele reduces total cerebrospinal fluid tau levels in women more than in men (Damoiseaux et al., 2012). In men, APOE ε4 exacerbates the contribution of andropause to increased LOAD risk (Panizzon et al., 2010). However, as andropause is more gradual than menopause, females could be more susceptible to the detrimental effects of ε4 earlier than men (Feldman et al., 2002; Harlow et al., 2012; Muller et al., 2003). In addition, accumulating evidence suggests that APOE variants drive sex-specific vulnerability to neurodegenerative diseases other than LOAD (reviewed in Box 2).
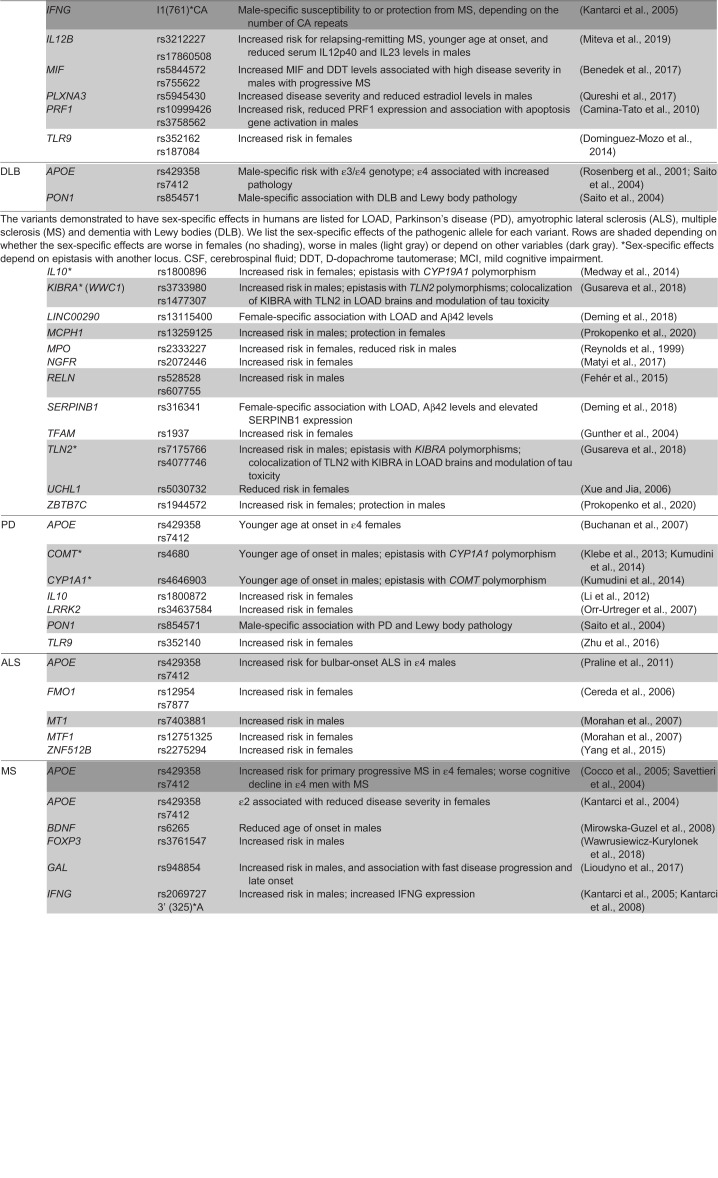
Sex-by-gene interactions in LOAD
Genetic factors can differentially affect males and females; thus, when testing for genetic associations, it is crucial not only to include sex as a confounding factor but also to stratify association analyses by sex. The importance of sex and the sex stratification approach has been exemplified numerous times, and has enabled the identification of novel genetic risk loci for neurological diseases including not only LOAD, but also PD, ALS, MS and DLB (Table 1). As the use of polygenic risk scores (Box 1) is proving beneficial for predicting disease risk (Box 4), the same approach may be applied to sex-specific risk. Furthermore, family-based analytical designs, which robustly recapitulate population structure, can be employed to test for sex-specific disease risk loci (Prokopenko et al., 2020). In addition to the sex-dependent effect described for APOE, other genetic and genomic factors contribute to LOAD in a sex-specific manner, as we review here.
Table 1.
Sex-by-genotype interactions across neurodegenerative disorders
Box 4. Polygenic risk scores for LOAD.
• A polygenic risk score (PRS) is a method of calculating disease risk by combining multiple disease-associated genetic variants in a single algorithm. While single subthreshold variants contribute little to disease risk, the performance of a combined risk score constructed from the weighted genome-wide association study (GWAS) single-nucleotide polymorphism (SNP) is much greater (area under the curve, 84%) (Escott-Price et al., 2017).
• PRS calculations were proposed based on thousands of LOAD-associated SNPs that do not reach genome-wide significance (Kunkle et al., 2019; Marioni et al., 2018).
• The potential advantages of PRS include:
(1) Enhanced predictability for LOAD diagnosis early in life
(2) Identification of convergent molecular pathways for the development of new therapeutic strategies and/or models in which to test therapies
(3) Selection of individuals with high PRS for clinical trials and precision medicine
(4) Enhanced understanding of early disease pathogenesis for biomarker development
• The PRS method is a powerful tool to predict the conversion from mild cognitive impairment to LOAD (Chaudhury et al., 2019), and PRS can be correlated to clinical outcomes, molecular signatures, neuropathology and brain function (Tasaki et al., 2018; Xiao et al., 2017).
• Although the majority of the predictability in these models comes from the contribution of APOE-associated risk, PRSs have predictive utility even for ε4 and ε2-negative individuals (Escott-Price et al., 2019).
• As sex-specific genetic associations with LOAD become more evident (Table 1), sex-stratified approaches are now more commonly applied, leading to the discovery of sex-dependent polygenic effects on LOAD risk. For example, these approaches revealed that the previously identified GWAS loci BIN1 and MS4A6A contribute more to LOAD progression in women than in men (Fan et al., 2020).
LOAD genetic loci
Genetic loci other than APOE exhibit sex-specific effects on LOAD risk, some of which directly relate to sex hormone activity and maintenance. For example, CYP19A1 encodes aromatase, which is involved in the conversion of androgens to estrogens. Aromatase may be neuroprotective by increasing local estrogen levels in injured neurons (Azcoitia et al., 2001). Therefore, loss-of-function mutations can have detrimental effects in the brain. Indeed, several polymorphisms in CYP19A1 increase LOAD risk in females (Table 1). Aromatase levels are increased in post-menopausal women but are decreased in the LOAD brain (Ishunina et al., 2007), which, when combined with loss of estrogen, can exacerbate disease progression. The sex-specific effect of CYP19A1 variation depends on epistasis with a polymorphism in the gene encoding the anti-inflammatory cytokine interleukin-10 (IL10), which further suggests an interaction between hormonal balance and neuroinflammation (Table 1). In addition, the male-specific effect of androgen receptor (AR) gene variants on LOAD risk (Table 1) suggests that compromising AR-mediated neuroprotective effects of hormones increases vulnerability to neurodegeneration (Hammond et al., 2001).
Another example is ESR1, which encodes the estrogen receptor ERα. In addition to its sex-specific effects on LOAD risk (Table 1), polymorphisms in this gene affect cognitive impairment (Kravitz et al., 2006; Yaffe et al., 2009), metabolic syndrome (Goulart et al., 2009), ovarian (Yang et al., 2010) and cardiovascular function (Lawlor et al., 2006), and cholesterol levels (Sowers et al., 2006) in a sex-specific manner, suggesting that estrogen signaling dysregulation leads to widespread detrimental effects throughout the body. Many novel LOAD-associated single-nucleotide polymorphisms (SNPs) were found to be female specific in a recent GWAS; however, these have yet to be replicated (Nazarian et al., 2019). Other genes with known sex-specific effects in LOAD are related to blood pressure regulation, neurotrophin (Box 1) signaling, DNA replication, cognition, and mitochondrial and neuronal function (Table 1).
Transcriptomic and epigenomic profiles
Non-coding variants, epigenomic signatures and transcriptomic changes associated with LOAD provide clues for the role of gene dysregulation in LOAD etiology. Sex differences in LOAD were reported at the genome sequence level (non-coding SNPs) and also observed for other ‘omics’ attributes, in particular transcriptomic and epigenomic profiles. Collectively, these studies suggest that gene dysregulation may, at least in part, be the underpinning mechanism for sex-dependent vulnerability to LOAD. Most recently, Mathys et al. characterized sex-specific cell subtype responses to LOAD pathology in human brain tissue and found that oligodendrocyte transcriptional activity becomes upregulated only in males, while excitatory and inhibitory neuron genes become downregulated only in females (Mathys et al., 2019). As aging is the biggest risk factor for LOAD, a microarray study revealed a striking 90% overlap between the prefrontal cortex gene expression patterns of healthy middle-aged females and male LOAD patients (Sanfilippo et al., 2019), suggesting that the female brain's transcriptional response to aging predisposes it to the development of LOAD. Other transcriptomics studies reinforce the idea that sex hormones are centrally involved in female-specific susceptibility to LOAD. For example, estrogen upregulates many of the genes found to be downregulated in female LOAD (Ratnakumar et al., 2019), consistent with previous studies demonstrating estrogen-mediated neuroprotection via genomic pathways. In addition, a meta-analysis of transcriptomic studies of LOAD generated protein-protein interaction networks, which centered on estrogen and androgen receptors (Winkler and Fox, 2013). As APOE ε4 is known to act as a transcription factor, one study found a strong correlation between APOE expression in ε4-carrying females and expression of genes involved in hormone pathways (Hsu et al., 2019).
As LOAD is likely to be caused by a complex interplay between genetic and environmental factors, it is no surprise that there are well-established epigenomic signatures of LOAD. Growing evidence suggests that sex-specific epigenomic signatures may be upstream of the transcriptomic profiles discussed above. Sex influences epigenetic factors like DNA methylation (Boks et al., 2009; El-Maarri et al., 2007). While some studies have failed to detect a significant effect of sex on LOAD-associated DNA methylation (Di Francesco et al., 2015; Kobayashi et al., 2016), others have identified a handful of specific loci that exhibit different methylation levels in females versus males with LOAD. For example, a methylome analysis of human neurons revealed that a CpG island in the promoter region of the mitotic gene aurora kinase C (AURKC) is hypomethylated in LOAD, leading to upregulation of AURKC (Mano et al., 2017). This same CpG island is hypermethylated in females compared to males with LOAD, and it also becomes hypomethylated as the number of APOE ε4 alleles increases (Mano et al., 2017). This suggests that the presence of the ε4 allele in females increases susceptibility to LOAD in part due to AURKC upregulation. Another study found a weak influence of sex on TREM2 methylation in the peripheral leukocytes of LOAD patients (Ozaki et al., 2017). In addition, the promoter of GPR50, a candidate risk gene for LOAD, is hypermethylated in LOAD females and hypomethylated in LOAD males compared to healthy controls (Chen et al., 2019). The App promoter is hypermethylated, and thus transcriptionally silenced, in female wild-type mice (Mani and Thakur, 2006). However, the same study showed that App expression increased with ovariectomy and decreased with estradiol treatment (Mani and Thakur, 2006), suggesting that estrogen acts through genomic pathways to silence App.
Histone acetylation represents another layer of epigenomic regulation, and is hypothesized to play a role in LOAD pathogenesis (Graff et al., 2012). One study examined histone deacetylase activity in human brain tissue, specifically in cholinergic neurons containing pathological tau, and found that the abundance of histone deacetylase 2 (HDAC2) was reduced in females regardless of clinical diagnosis (normal, MCI or LOAD) (Mahady et al., 2019). As HDAC2 is involved in synaptic plasticity (Akhtar et al., 2009), neuroinflammation (Hsing et al., 2015) and cellular stress (Peng et al., 2015), gene dysregulation due to its reduction may be a contributing factor to neurodegeneration in the female brain. In addition, long non-coding (lnc)RNA regulation has been linked to the development of LOAD (Magistri et al., 2015; Zhou et al., 2019; Zhou and Xu, 2015); however, the role of sex in this relationship remained unclear until recently. A bioinformatics analysis of human LOAD brain microarray datasets revealed a total of 42 lncRNAs that were differentially expressed in LOAD versus normal tissue, 13 of which were sex specific, such as SLC25A25-AS1, PWRN1 and LY86-AS1 (Cao et al., 2019). FOXO signaling and glioma pathways were over-represented within the sex-specific lncRNAs (Cao et al., 2019). This work demonstrates that LOAD affects the expression of lncRNAs in a sex-dependent manner. Other types of non-coding RNAs may play a sex-specific role in LOAD pathogenesis; however, this was not confirmed in a recent study on microRNAs (Nelson et al., 2018). These findings highlight that integrative multi-omics studies will be essential to understanding whether epigenomic changes directly affect gene expression patterns in LOAD. This knowledge will be instrumental to further elucidating the molecular pathways underlying sex differences in LOAD susceptibility, as well as uncovering new therapeutic strategies.
Findings from animal models
Several transgenic animal models harboring LOAD-related genetic modifications exhibit more severe disease-like phenotypes in females than males (Schmid et al., 2019; Wang et al., 2003; Yue et al., 2011). Although female rodents do not undergo menopause, they do experience a period of altered estrous cycling (Guimarães et al., 2015) followed by persistently low estrogen levels at old ages (Felicio et al., 1984), similar to peri- and post-menopause in women. Findings from these models are in agreement with two possibilities in humans: (1) reduced estrogen exposure in adult females exacerbates disease progression, as in J20 mice (Box 1) (Broestl et al., 2018); and/or (2) the organizational effects of sex hormones during neurodevelopment have lasting effects that increase susceptibility to neurodegenerative disease later in life, as in 3xTgAD mice (Box 1) (Carroll et al., 2010). For more information, we direct the reader to a review summarizing findings from LOAD animal models consistent and inconsistent with the sex differences observed in humans (Fisher et al., 2018). However, a more detailed examination of the interplay between APOE and hormones in rodent models can provide mechanistic insights for how these processes underlie sex differences in disease pathogenesis.
The detrimental effects of the ε4 allele on APOE-estrogen interactions, centering on synaptic dysfunction and cellular stress, have been demonstrated in several rodent models. APOE-TR mice, in which the murine Apoe gene is replaced with human APOE ε2, ε3 or ε4, have been used extensively in the study of molecular mechanisms of LOAD (Knouff et al., 1999). Following previous studies demonstrating that APOE-TR female mice with the APOE ε4 genotype are more susceptible to cognitive dysfunction than males, one group demonstrated that N-methyl-D-aspartate (NMDA) receptor (NMDAR; Box 1) activation, linked to downstream effectors such as CaMKII (CAMK2A), ERK1/2 (MAPK3/MAPK1) and CREB proteins, is reduced in aged female APOE-TR ε4 but not ε3 mice (Yong et al., 2014). Deficiency in these NMDAR-related pathways may underlie the susceptibility of ε4-positive women to cognitive dysfunction via loss of neuroprotection and synaptic function. Similar to deficits in synaptic density found in human females, synaptic proteins are downregulated in APOE-TR ε4 female mice, owing to dysregulation of factors involved in mitochondrial function and oxidative stress such as prohibitin 2, VDAC2, NADH dehydrogenase and GSTM1 (Shi et al., 2014). Also, like in humans, carrying the ε4 genotype reduces APOE levels in APOE-TR mice (Yong et al., 2014), which may be mediated by decreases in 17β-hydroxysteroid dehydrogenase 10 (HSD17B10), a key enzyme in sex hormone synthesis, coupled with increases in aromatase (Shi et al., 2014). A recent study used APOE-TR mice to examine the interactive effects of sex, APOE and age on brain transcriptomic profiles, and found that these variables interactively influenced the expression of genes in the unfolded protein response pathway (Zhao et al., 2020b), a response to endoplasmic reticulum stress implicated in the etiology of neurodegenerative diseases (Scheper and Hoozemans, 2015). Together, these findings suggest that estrogen signaling is defective in APOE ε4 carriers, and that loss of estrogen results in energy deficiencies and elevated cellular stress, particularly within synapses (Fig. 2). Reduced levels of and sensitivity to estrogen, exacerbated by both the APOE ε4 allele and menopause, likely makes older women particularly vulnerable to neurodegenerative disease.
Animal models of AD also support hypotheses related to glucose hypometabolism and female susceptibility to LOAD. Compared to non-transgenic mice, aging female 3xTgAD mice show an exaggerated decline in expression and activity of transporters and enzymes needed for glucose metabolism, switching to ketone bodies as an alternative fuel in response (Ding et al., 2013a). Ovariectomy can induce this ketogenic switch in 3xTgAD mice, which is associated with increased expression of enzymes required for conversion of ketone bodies to acetyl-CoA (Ding et al., 2013b). In a rat model of perimenopause, a similar ketogenic switch was found to be regulated by insulin-like growth factor 1 (IGF1) and AMPK (PRKAA2)/PGC-1α signaling, as well as by ERβ expression (Yin et al., 2015). As ketone bodies are primarily derived from white matter, white matter volume, myelinated fiber volume and myelin sheath volume were all reduced in aged female APP/PS1 double-transgenic mice compared to males (Zhou et al., 2018). A recent metabolomic and transcriptomic study in APOE-TR mice confirmed that metabolic shifts in the female ε4 brain are accompanied by loss of myelin integrity (Shang et al., 2020).
The ongoing progress in rodent modeling is expanding on what we have learned from ovariectomy models, which more closely recapitulate surgical rather than natural menopause. The recently developed accelerated ovarian failure model mimics natural menopause, as reviewed separately (Marongiu, 2019). Parallel studies of multiple models of different neurodegenerative diseases will also prove useful in identifying shared disease etiologies. For instance, a recent study highlighted a potential APOE-centered unifying mechanism in microglia underlying LOAD, ALS and MS across three animal models (Krasemann et al., 2017). As TREM2 is a putative receptor for APOE (Yeh et al., 2016), Krasemann and colleagues report that a TREM2-APOE pathway triggers a phenotypic switch in microglia from homeostatic to inflammatory through the microRNA miR-155 (Krasemann et al., 2017) (Fig. 2). Whether or not this pathway is influenced by sex hormones or different APOE isoforms remains to be studied.
Conclusions
Here, we review evidence supporting three non-mutually exclusive hypotheses explaining sex-specific vulnerability to neurodegenerative diseases: (1) organizational effects of sex hormones during development; (2) synergistic effects of coexisting vascular, metabolic and inflammatory conditions that are risk factors for neurodegenerative diseases; and (3) irregularity and/or decline of sex hormone levels with aging. APOE is a multifunctional protein and therefore its role in LOAD pathogenesis is complex. However, it is becoming increasingly clear that estrogen is a key player in APOE ε4-mediated female-specific vulnerability to LOAD. The major mechanisms underlying this ε4-estrogen relationship seem to be negation of estrogen-associated neuroprotection and menopause-associated brain hypometabolism. Both human and animal studies support the overarching hypothesis that a ketogenic switch occurs as a response to the hypometabolic state triggered during perimenopause. Because ε4 can lengthen this transition period by delaying post-menopause, energy imbalance might represent the first step in ε4-associated toxicity in the female brain. Other important considerations in understanding the sex-specific effects of APOE ε4 include gene dysregulation via transcriptional effects and loss of female-specific protection conferred by the ε2 or ε3 alleles. Finally, animal models have largely aligned with studies in humans and have extended those findings to uncover potential causal mechanisms. Importantly, rodent models have revealed that estrogen signaling is defective in APOE ε4-positive individuals, leading to energy imbalance, cellular stress and synaptic dysfunction. All of this evidence highlights the need to carefully examine the role of sex in LOAD risk and, specifically, to test the hypotheses outlined herein. LOAD studies stratified by sex, such as integrative multi-omics profiling of disease-relevant human brain tissues, will enable the discovery of new genetic factors that remained masked in a sex-mixed sample and reveal known loci with greater effects in females or males. To achieve sufficient statistical power in studies stratified by sex, researchers now have access to more widespread and affordable whole-genome sequencing technologies than in previous analyses (Bansal and Boucher, 2019; Lightbody et al., 2019). This type of work will be essential for implementation in precision medicine based on sex, including the development of sex-specific diagnostic tools for clinical testing and identification of sex-specific targets for drug discovery in LOAD and other neurodegenerative diseases. In conclusion, this Review advocates for the importance of gene-by-sex interactions in studying the underpinning genetics of neurodegeneration, as many aspects of central nervous system function differ between males and females.
Footnotes
Competing interests
The authors declare no competing or financial interests.
Funding
This work was funded in part by the National Institutes of Health/National Institute on Aging [R01-AG057522-01 and R01-AG040370-01A1 to O.C-F.].
References
- Abildayeva K., Jansen P. J., Hirsch-Reinshagen V., Bloks V. W., Bakker A. H., Ramaekers F. C., de Vente J., Groen A. K., Wellington C. L., Kuipers F. et al. (2006). 24(S)-hydroxycholesterol participates in a liver X receptor-controlled pathway in astrocytes that regulates apolipoprotein E-mediated cholesterol efflux. J. Biol. Chem. 281, 12799-12808. 10.1074/jbc.M601019200 [DOI] [PubMed] [Google Scholar]
- Achariyar T. M., Li B., Peng W., Verghese P. B., Shi Y., McConnell E., Benraiss A., Kasper T., Song W., Takano T. et al. (2016). Glymphatic distribution of CSF-derived apoE into brain is isoform specific and suppressed during sleep deprivation. Mol. Neurodegener 11, 74 10.1186/s13024-016-0138-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abondio P., Sazzini M., Garagnani P., Boattini A., Monti D., Franceschi C., Luiselli D. and Giuliani C. (2019). The genetic variability of APOE in different human populations and its implications for longevity. Genes (Basel) 10, 222 10.3390/genes10030222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agosta F., Vossel K. A., Miller B. L., Migliaccio R., Bonasera S. J., Filippi M., Boxer A. L., Karydas A., Possin K. L. and Gorno-Tempini M. L. (2009). Apolipoprotein E ε4 is associated with disease-specific effects on brain atrophy in Alzheimer's disease and frontotemporal dementia. Proc. Natl. Acad. Sci. USA 106, 2018-2022. 10.1073/pnas.0812697106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahlbom E., Prins G. S. and Ceccatelli S. (2001). Testosterone protects cerebellar granule cells from oxidative stress-induced cell death through a receptor mediated mechanism. Brain Res. 892, 255-262. 10.1016/S0006-8993(00)03155-3 [DOI] [PubMed] [Google Scholar]
- Akhtar M. W., Raingo J., Nelson E. D., Montgomery R. L., Olson E. N., Kavalali E. T. and Monteggia L. M. (2009). Histone deacetylases 1 and 2 form a developmental switch that controls excitatory synapse maturation and function. J. Neurosci. 29, 8288-8297. 10.1523/JNEUROSCI.0097-09.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alonso-Nanclares L., Gonzalez-Soriano J., Rodriguez J. R. and DeFelipe J. (2008). Gender differences in human cortical synaptic density. Proc. Natl. Acad. Sci. USA 105, 14615-14619. 10.1073/pnas.0803652105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altmann A., Tian L., Henderson V. W., Greicius, M. D. and Alzheimer's Disease Neuroimaging Initiative Investigators (2014). Sex modifies the APOE-related risk of developing Alzheimer disease. Ann. Neurol. 75, 563-573. 10.1002/ana.24135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alzheimer's Association (2016). 2016 Alzheimer's disease facts and figures. Alzheimer's & Dementia 12, 459-509. 10.1016/j.jalz.2016.03.001 [DOI] [PubMed] [Google Scholar]
- Alzheimer's Association (2019). 2019 Alzheimer's disease facts and figures. Alzheimer's & Dementia 15, 321-387. 10.1016/j.jalz.2019.01.010 [DOI] [Google Scholar]
- Andrews-Zwilling Y., Bien-Ly N., Xu Q., Li G., Bernardo A., Yoon S. Y., Zwilling D., Yan T. X., Chen L. and Huang Y. (2010). Apolipoprotein E4 causes age- and Tau-dependent impairment of GABAergic interneurons, leading to learning and memory deficits in mice. J. Neurosci. 30, 13707-13717. 10.1523/JNEUROSCI.4040-10.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antulov R., Weinstock-Guttman B., Cox J. L., Hussein S., Durfee J., Caiola C., Dwyer M. G., Bergsland N., Abdelrahman N., Stosic M. et al. (2009). Gender-related differences in MS: a study of conventional and nonconventional MRI measures. Mult. Scler. 15, 345-354. 10.1177/1352458508099479 [DOI] [PubMed] [Google Scholar]
- Arboleda-Velasquez J. F., Lopera F., O'Hare M., Delgado-Tirado S., Marino C., Chmielewska N., Saez-Torres K. L., Amarnani D., Schultz A. P., Sperling R. A. et al. (2019). Resistance to autosomal dominant Alzheimer's disease in an APOE3 Christchurch homozygote: a case report. Nat. Med. 25, 1680-1683. 10.1038/s41591-019-0611-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azcoitia I., Sierra A., Veiga S., Honda S., Harada N. and Garcia-Segura L. M. (2001). Brain aromatase is neuroprotective. J. Neurobiol. 47, 318-329. 10.1002/neu.1038 [DOI] [PubMed] [Google Scholar]
- Baldereschi M., Di Carlo A., Rocca W. A., Vanni P., Maggi S., Perissinotto E., Grigoletto F., Amaducci L. and Inzitari D. (2000). Parkinson's disease and parkinsonism in a longitudinal study: two-fold higher incidence in men. ILSA working group. Italian longitudinal study on aging. Neurology 55, 1358-1363. 10.1212/WNL.55.9.1358 [DOI] [PubMed] [Google Scholar]
- Bansal V. and Boucher C. (2019). Sequencing technologies and analyses: where have we been and where are we going? iScience 18, 37-41. 10.1016/j.isci.2019.06.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes L. L., Wilson R. S., Bienias J. L., Schneider J. A., Evans D. A. and Bennett D. A. (2005). Sex differences in the clinical manifestations of Alzheimer disease pathology. Arch. Gen. Psychiatry 62, 685-691. 10.1001/archpsyc.62.6.685 [DOI] [PubMed] [Google Scholar]
- Bartzokis G., Lu P. H., Geschwind D. H., Edwards N., Mintz J. and Cummings J. L. (2006). Apolipoprotein E genotype and age-related myelin breakdown in healthy individuals: implications for cognitive decline and dementia. Arch. Gen. Psychiatry 63, 63-72. 10.1001/archpsyc.63.1.63 [DOI] [PubMed] [Google Scholar]
- Bell R. D., Winkler E. A., Singh I., Sagare A. P., Deane R., Wu Z., Holtzman D. M., Betsholtz C., Armulik A., Sallstrom J. et al. (2012). Apolipoprotein E controls cerebrovascular integrity via cyclophilin A. Nature 485, 512-516. 10.1038/nature11087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benedek G., Meza-Romero R., Jordan K., Zhang Y., Nguyen H., Kent G., Li J., Siu E., Frazer J., Piecychna M. et al. (2017). MIF and D-DT are potential disease severity modifiers in male MS subjects. Proc. Natl. Acad. Sci. USA 114, E8421-E8429. 10.1073/pnas.1712288114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertram L., McQueen M. B., Mullin K., Blacker D. and Tanzi R. E. (2007). Systematic meta-analyses of Alzheimer disease genetic association studies: the AlzGene database. Nat. Genet. 39, 17-23. 10.1038/ng1934 [DOI] [PubMed] [Google Scholar]
- Beydoun M. A., Boueiz A., Abougergi M. S., Kitner-Triolo M. H., Beydoun H. A., Resnick S. M., O'Brien R. and Zonderman A. B. (2012). Sex differences in the association of the apolipoprotein E epsilon 4 allele with incidence of dementia, cognitive impairment, and decline. Neurobiol. Aging 33, 720-731.e724. 10.1016/j.neurobiolaging.2010.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beydoun M. A., Beydoun H. A., Kaufman J. S., An Y., Resnick S. M., O'Brien R., Ferrucci L. and Zonderman A. B. (2013). Apolipoprotein E epsilon4 allele interacts with sex and cognitive status to influence all-cause and cause-specific mortality in U.S. older adults. J. Am. Geriatr. Soc. 61, 525-534. 10.1111/jgs.12156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatt S. D. and Dluzen D. E. (2005). Dopamine transporter function differences between male and female CD-1 mice. Brain Res. 1035, 188-195. 10.1016/j.brainres.2004.12.013 [DOI] [PubMed] [Google Scholar]
- Bjorkhem I. and Meaney S. (2004). Brain cholesterol: long secret life behind a barrier. Arterioscler. Thromb. Vasc. Biol. 24, 806-815. 10.1161/01.ATV.0000120374.59826.1b [DOI] [PubMed] [Google Scholar]
- Boeve B. F., Boylan K. B., Graff-Radford N. R., DeJesus-Hernandez M., Knopman D. S., Pedraza O., Vemuri P., Jones D., Lowe V., Murray M. E. et al. (2012). Characterization of frontotemporal dementia and/or amyotrophic lateral sclerosis associated with the GGGGCC repeat expansion in C9ORF72. Brain 135, 765-783. 10.1093/brain/aws004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boks M. P., Derks E. M., Weisenberger D. J., Strengman E., Janson E., Sommer I. E., Kahn R. S. and Ophoff R. A. (2009). The relationship of DNA methylation with age, gender and genotype in twins and healthy controls. PLoS ONE 4, e6767 10.1371/journal.pone.0006767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bove R., Secor E., Chibnik L. B., Barnes L. L., Schneider J. A., Bennett D. A. and De Jager P. L. (2014). Age at surgical menopause influences cognitive decline and Alzheimer pathology in older women. Neurology 82, 222-229. 10.1212/WNL.0000000000000033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boylan K., Yang C., Crook J., Overstreet K., Heckman M., Wang Y., Borchelt D. and Shaw G. (2009). Immunoreactivity of the phosphorylated axonal neurofilament H subunit (pNF-H) in blood of ALS model rodents and ALS patients: evaluation of blood pNF-H as a potential ALS biomarker. J. Neurochem. 111, 1182-1191. 10.1111/j.1471-4159.2009.06386.x [DOI] [PubMed] [Google Scholar]
- Brannvall K., Bogdanovic N., Korhonen L. and Lindholm D. (2005). 19-Nortestosterone influences neural stem cell proliferation and neurogenesis in the rat brain. Eur. J. Neurosci. 21, 871-878. 10.1111/j.1460-9568.2005.03942.x [DOI] [PubMed] [Google Scholar]
- Bretsky P. M., Buckwalter J. G., Seeman T. E., Miller C. A., Poirier J., Schellenberg G. D., Finch C. E. and Henderson V. W. (1999). Evidence for an interaction between apolipoprotein E genotype, gender, and Alzheimer disease. Alzheimer Dis. Assoc. Disord. 13, 216-221. 10.1097/00002093-199910000-00007 [DOI] [PubMed] [Google Scholar]
- Brinton R. D., Yao J., Yin F., Mack W. J. and Cadenas E. (2015). Perimenopause as a neurological transition state. Nat. Rev. Endocrinol. 11, 393-405. 10.1038/nrendo.2015.82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broestl L., Worden K., Moreno A. J., Davis E. J., Wang D., Garay B., Singh T., Verret L., Palop J. J. and Dubal D. B. (2018). Ovarian cycle stages modulate alzheimer-related cognitive and brain network alterations in female mice. eNeuro 5, ENEURO.0132-17.2018 10.1523/ENEURO.0132-17.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown C. M., Xu Q., Okhubo N., Vitek M. P. and Colton C. A. (2007). Androgen-mediated immune function is altered by the apolipoprotein E gene. Endocrinology 148, 3383-3390. 10.1210/en.2006-1200 [DOI] [PubMed] [Google Scholar]
- Brown C. M., Choi E., Xu Q., Vitek M. P. and Colton C. A. (2008). The APOE4 genotype alters the response of microglia and macrophages to 17beta-estradiol. Neurobiol. Aging 29, 1783-1794. 10.1016/j.neurobiolaging.2007.04.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchanan D. D., Silburn P. A., Prince J. A. and Mellick G. D. (2007). Association of APOE with Parkinson disease age-at-onset in women. Neurosci. Lett. 411, 185-188. 10.1016/j.neulet.2006.07.080 [DOI] [PubMed] [Google Scholar]
- Buckley R. F., Mormino E. C., Rabin J. S., Hohman T. J., Landau S., Hanseeuw B. J., Jacobs H. I. L., Papp K. V., Amariglio R. E., Properzi M. J. et al. (2019). Sex differences in the association of global amyloid and regional tau deposition measured by positron emission tomography in clinically normal older adults. JAMA Neurol. 76, 542-551. 10.1001/jamaneurol.2018.4693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camina-Tato M., Morcillo-Suarez C., Bustamante M. F., Ortega I., Navarro A., Muntasell A., Lopez-Botet M., Sanchez A., Carmona P., Julia E. et al. (2010). Gender-associated differences of perforin polymorphisms in the susceptibility to multiple sclerosis. J. Immunol. 185, 5392-5404. 10.4049/jimmunol.1000102 [DOI] [PubMed] [Google Scholar]
- Cantuti-Castelvetri I., Keller-McGandy C., Bouzou B., Asteris G., Clark T. W., Frosch M. P. and Standaert D. G. (2007). Effects of gender on nigral gene expression and parkinson disease. Neurobiol. Dis. 26, 606-614. 10.1016/j.nbd.2007.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantuti-Castelvetri L., Fitzner D., Bosch-Queralt M., Weil M. T., Su M., Sen P., Ruhwedel T., Mitkovski M., Trendelenburg G., Lütjohann D. et al. (2018). Defective cholesterol clearance limits remyelination in the aged central nervous system. Science 359, 684-688. 10.1126/science.aan4183 [DOI] [PubMed] [Google Scholar]
- Cao M., Li H., Zhao J., Cui J. and Hu G. (2019). Identification of age- and gender-associated long noncoding RNAs in the human brain with Alzheimer's disease. Neurobiol. Aging 81, 116-126. 10.1016/j.neurobiolaging.2019.05.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll J. C., Rosario E. R., Kreimer S., Villamagna A., Gentzschein E., Stanczyk F. Z. and Pike C. J. (2010). Sex differences in beta-amyloid accumulation in 3xTg-AD mice: role of neonatal sex steroid hormone exposure. Brain Res. 1366, 233-245. 10.1016/j.brainres.2010.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cereda C., Gabanti E., Corato M., de Silvestri A., Alimonti D., Cova E., Malaspina A. and Ceroni M. (2006). Increased incidence of FMO1 gene single nucleotide polymorphisms in sporadic amyotrophic lateral sclerosis. Amyotroph Lateral Scler. 7, 227-234. 10.1080/17482960600864413 [DOI] [PubMed] [Google Scholar]
- Chandran S., Krishnan S., Rao R. M., Sarma S. G., Sarma P. S. and Kishore A. (2014). Gender influence on selection and outcome of deep brain stimulation for Parkinson's disease. Ann. Indian Acad. Neurol. 17, 66-70. 10.4103/0972-2327.128557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charn T. H., Liu E. T., Chang E. C., Lee Y. K., Katzenellenbogen J. A. and Katzenellenbogen B. S. (2010). Genome-wide dynamics of chromatin binding of estrogen receptors alpha and beta: mutual restriction and competitive site selection. Mol. Endocrinol. 24, 47-59. 10.1210/me.2009-0252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudhury S., Brookes K. J., Patel T., Fallows A., Guetta-Baranes T., Turton J. C., Guerreiro R., Bras J., Hardy J., Francis P. T. et al. (2019). Alzheimer's disease polygenic risk score as a predictor of conversion from mild-cognitive impairment. Transl. Psychiatry 9, 154 10.1038/s41398-019-0485-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Durakoglugil M. S., Xian X. and Herz J. (2010). ApoE4 reduces glutamate receptor function and synaptic plasticity by selectively impairing ApoE receptor recycling. Proc. Natl. Acad. Sci. USA 107, 12011-12016. 10.1073/pnas.0914984107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen W., Ji H., Li L., Xu C., Zou T., Cui W., Xu S., Zhou X., Duan S. and Wang Q. (2019). Significant association between GPR50 hypomethylation and AD in males. Mol. Med. Rep. 20, 1085-1092. 10.3892/mmr.2019.10366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chêne G., Beiser A., Au R., Preis S. R., Wolf P. A., Dufouil C. and Seshadri S. (2015). Gender and incidence of dementia in the Framingham Heart Study from mid-adult life. Alzheimers Dement 11, 310-320. 10.1016/j.jalz.2013.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng X., McAsey M. E., Li M., Randall S., Cady C., Nathan B. P. and Struble R. G. (2007). Estradiol replacement increases the low-density lipoprotein receptor related protein (LRP) in the mouse brain. Neurosci. Lett. 417, 50-54. 10.1016/j.neulet.2007.02.030 [DOI] [PubMed] [Google Scholar]
- Cherrier M. M., Anderson K., Shofer J., Millard S. and Matsumoto A. M. (2015). Testosterone treatment of men with mild cognitive impairment and low testosterone levels. Am. J. Alzheimers Dis. Other Demen. 30, 421-430. 10.1177/1533317514556874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou C.-Y., Lin Y.-L., Huang Y.-C., Sheu S.-Y., Lin T.-H., Tsay H.-J., Chang G.-G. and Shiao M.-S. (2005). Structural variation in human apolipoprotein E3 and E4: secondary structure, tertiary structure, and size distribution. Biophys. J. 88, 455-466. 10.1529/biophysj.104.046813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou P.-S., Wu S.-J., Kao Y.-H., Chou M.-C., Tai S.-Y. and Yang Y.-H. (2017). Angiotensin-converting enzyme insertion/deletion polymorphism is associated with cerebral white matter changes in Alzheimer's disease. Geriatr. Gerontol. Int. 17, 945-950. 10.1111/ggi.12815 [DOI] [PubMed] [Google Scholar]
- Cocco E., Sotgiu A., Costa G., Murru M. R., Mancosu C., Murru R., Lai M., Contu P. and Marrosu M. G. (2005). HLA-DR,DQ and APOE genotypes and gender influence in Sardinian primary progressive MS. Neurology 64, 564-566. 10.1212/01.WNL.0000150579.54878.00 [DOI] [PubMed] [Google Scholar]
- Confavreux C., Vukusic S. and Adeleine P. (2003). Early clinical predictors and progression of irreversible disability in multiple sclerosis: an amnesic process. Brain 126, 770-782. 10.1093/brain/awg081 [DOI] [PubMed] [Google Scholar]
- Corder E. H., Saunders A. M., Strittmatter W. J., Schmechel D. E., Gaskell P. C., Small G. W., Roses A. D., Haines J. L. and Pericak-Vance M. A. (1993). Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer's disease in late onset families. Science 261, 921-923. 10.1126/science.8346443 [DOI] [PubMed] [Google Scholar]
- Corder E. H., Ghebremedhin E., Taylor M. G., Thal D. R., Ohm T. G. and Braak H. (2004). The biphasic relationship between regional brain senile plaque and neurofibrillary tangle distributions: modification by age, sex, and APOE polymorphism. Ann. N. Y. Acad. Sci. 1019, 24-28. 10.1196/annals.1297.005 [DOI] [PubMed] [Google Scholar]
- Cosentino S., Scarmeas N., Helzner E., Glymour M. M., Brandt J., Albert M., Blacker D. and Stern Y. (2008). APOE epsilon 4 allele predicts faster cognitive decline in mild Alzheimer disease. Neurology 70, 1842-1849. 10.1212/01.wnl.0000304038.37421.cc [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford F., Abdullah L., Schinka J., Suo Z., Gold M., Duara R. and Mullan M. (2000). Gender-specific association of the angiotensin converting enzyme gene with Alzheimer's disease. Neurosci. Lett. 280, 215-219. 10.1016/S0304-3940(00)00791-6 [DOI] [PubMed] [Google Scholar]
- Cunningham R. L., Giuffrida A. and Roberts J. L. (2009). Androgens induce dopaminergic neurotoxicity via caspase-3-dependent activation of protein kinase Cdelta. Endocrinology 150, 5539-5548. 10.1210/en.2009-0640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahodwala N., Pei Q. and Schmidt P. (2016). Sex differences in the clinical progression of Parkinson's disease. J. Obstet. Gynecol. Neonatal. Nurs. 45, 749-756. 10.1016/j.jogn.2016.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damoiseaux J. S., Seeley W. W., Zhou J., Shirer W. R., Coppola G., Karydas A., Rosen H. J., Miller B. L., Kramer J. H., Greicius M. D. and Alzheimer's Disease Neuroimaging Investigators (2012). Gender modulates the APOE epsilon4 effect in healthy older adults: convergent evidence from functional brain connectivity and spinal fluid tau levels. J. Neurosci. 32, 8254-8262. 10.1523/JNEUROSCI.0305-12.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis A. A., Inman C. E., Wargel Z. M., Dube U., Freeberg B. M., Galluppi A., Haines J. N., Dhavale D. D., Miller R., Choudhury F. A. et al. (2020). APOE genotype regulates pathology and disease progression in synucleinopathy. Sci. Transl. Med. 12, eaay3069 10.1126/scitranslmed.aay3069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Marinis E., Martini C., Trentalance A. and Pallottini V. (2008). Sex differences in hepatic regulation of cholesterol homeostasis. J. Endocrinol. 198, 635-643. 10.1677/JOE-08-0242 [DOI] [PubMed] [Google Scholar]
- Dean D. C. III, Jerskey B. A., Chen K., Protas H., Thiyyagura P., Roontiva A., O'Muircheartaigh J., Dirks H., Waskiewicz N., Lehman K. et al. (2014). Brain differences in infants at differential genetic risk for late-onset Alzheimer disease: a cross-sectional imaging study. JAMA Neurol. 71, 11-22. 10.1001/jamaneurol.2013.4544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deming Y., Dumitrescu L., Barnes L. L., Thambisetty M., Kunkle B., Gifford K. A., Bush W. S., Chibnik L. B., Mukherjee S., De Jager P. L. et al. (2018). Sex-specific genetic predictors of Alzheimer's disease biomarkers. Acta Neuropathol. 136, 857-872. 10.1007/s00401-018-1881-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Francesco A., Arosio B., Falconi A., Micioni Di Bonaventura M. V., Karimi M., Mari D., Casati M., Maccarrone M. and D'Addario C. (2015). Global changes in DNA methylation in Alzheimer's disease peripheral blood mononuclear cells. Brain Behav. Immun. 45, 139-144. 10.1016/j.bbi.2014.11.002 [DOI] [PubMed] [Google Scholar]
- Dickson D. W., Heckman M. G., Murray M. E., Soto A. I., Walton R. L., Diehl N. N., van Gerpen J. A., Uitti R. J., Wszolek Z. K., Ertekin-Taner N. et al. (2018). APOE ε4 is associated with severity of Lewy body pathology independent of Alzheimer pathology. Neurology 91, e1182-e1195. 10.1212/WNL.0000000000006212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding F., Yao J., Rettberg J. R., Chen S. and Brinton R. D. (2013a). Early decline in glucose transport and metabolism precedes shift to ketogenic system in female aging and Alzheimer's mouse brain: implication for bioenergetic intervention. PLoS ONE 8, e79977 10.1371/journal.pone.0079977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding F., Yao J., Zhao L., Mao Z., Chen S. and Brinton R. D. (2013b). Ovariectomy induces a shift in fuel availability and metabolism in the hippocampus of the female transgenic model of familial Alzheimer's. PLoS ONE 8, e59825 10.1371/journal.pone.0059825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Disshon K. A. and Dluzen D. E. (2000). Estrogen reduces acute striatal dopamine responses in vivo to the neurotoxin MPP+ in female, but not male rats. Brain Res. 868, 95-104. 10.1016/S0006-8993(00)02329-5 [DOI] [PubMed] [Google Scholar]
- Dominguez-Mozo M. I., Garcia-Montojo M., López-Cavanillas M., De Las Heras V., Garcia-Martinez A., Arias-Leal A. M., Casanova I., Urcelay E., Arroyo R. and Alvarez-Lafuente R. (2014). Toll-like receptor-9 in Spanish multiple sclerosis patients: an association with the gender. Eur. J. Neurol. 21, 537-540. 10.1111/ene.12209 [DOI] [PubMed] [Google Scholar]
- Dong L.-M., Parkin S., Trakhanov S. D., Rupp B., Simmons T., Arnold K. S., Newhouse Y. M., Innerarity T. L. and Weisgraber K. H. (1996). Novel mechanism for defective receptor binding of apolipoprotein E2 in type III hyperlipoproteinemia. Nat. Struct. Biol. 3, 718-722. 10.1038/nsb0896-718 [DOI] [PubMed] [Google Scholar]
- Dong L.-M. and Weisgraber K. H. (1996). Human apolipoprotein E4 domain interaction: arginine 61 and glutamic acid 255 interact to direct the preference for very low density lipoproteins. J. Biol. Chem. 271, 19053-19057. 10.1074/jbc.271.32.19053 [DOI] [PubMed] [Google Scholar]
- Dumitrescu L., Barnes L. L., Thambisetty M., Beecham G., Kunkle B., Bush W. S., Gifford K. A., Chibnik L. B., Mukherjee S., De Jager P. L. et al. (2019). Sex differences in the genetic predictors of Alzheimer's pathology. Brain 142, 2581-2589. 10.1093/brain/awz206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunckley T., Huentelman M. J., Craig D. W., Pearson J. V., Szelinger S., Joshipura K., Halperin R. F., Stamper C., Jensen K. R., Letizia D. et al. (2007). Whole-genome analysis of sporadic amyotrophic lateral sclerosis. N. Engl. J. Med. 357, 775-788. 10.1056/NEJMoa070174 [DOI] [PubMed] [Google Scholar]
- Edland S. D., Rocca W. A., Petersen R. C., Cha R. H. and Kokmen E. (2002). Dementia and Alzheimer disease incidence rates do not vary by sex in Rochester, Minn. Arch. Neurol. 59, 1589-1593. 10.1001/archneur.59.10.1589 [DOI] [PubMed] [Google Scholar]
- El-Maarri O., Becker T., Junen J., Manzoor S. S., Diaz-Lacava A., Schwaab R., Wienker T. and Oldenburg J. (2007). Gender specific differences in levels of DNA methylation at selected loci from human total blood: a tendency toward higher methylation levels in males. Hum. Genet. 122, 505-514. 10.1007/s00439-007-0430-3 [DOI] [PubMed] [Google Scholar]
- Escott-Price V., Myers A. J., Huentelman M. and Hardy J. (2017). Polygenic risk score analysis of pathologically confirmed Alzheimer disease. Ann. Neurol. 82, 311-314. 10.1002/ana.24999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Escott-Price V., Myers A., Huentelman M., Shoai M. and Hardy J. (2019). Polygenic risk score analysis of Alzheimer's disease in cases without APOE4 or APOE2 alleles. J. Prev. Alzheimers Dis. 6, 16-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagan A. M., Holtzman D. M., Munson G., Mathur T., Schneider D., Chang L. K., Getz G. S., Reardon C. A., Lukens J., Shah J. A. et al. (1999). Unique lipoproteins secreted by primary astrocytes from wild type, apoE (−/−), and human apoE transgenic mice. J. Biol. Chem. 274, 30001-30007. 10.1074/jbc.274.42.30001 [DOI] [PubMed] [Google Scholar]
- Fagerberg L., Hallström B. M., Oksvold P., Kampf C., Djureinovic D., Odeberg J., Habuka M., Tahmasebpoor S., Danielsson A., Edlund K. et al. (2014). Analysis of the human tissue-specific expression by genome-wide integration of transcriptomics and antibody-based proteomics. Mol. Cell. Proteomics 13, 397-406. 10.1074/mcp.M113.035600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan C. C., Banks S. J., Thompson W. K., Chen C. H., McEvoy L. K., Tan C. H., Kukull W., Bennett D. A., Farrer L. A., Mayeux R. et al. (2020). Sex-dependent autosomal effects on clinical progression of Alzheimer's disease. Brain143, 2272-2280. 10.1093/brain/awaa164 [DOI] [PMC free article] [PubMed]
- Fehér A., Juhász A., Pákáski M., Kálmán J. and Janka Z. (2015). Genetic analysis of the RELN gene: Gender specific association with Alzheimer's disease. Psychiatry Res. 230, 716-718. 10.1016/j.psychres.2015.09.021 [DOI] [PubMed] [Google Scholar]
- Feldman H. A., Longcope C., Derby C. A., Johannes C. B., Araujo A. B., Coviello A. D., Bremner W. J. and McKinlay J. B. (2002). Age trends in the level of serum testosterone and other hormones in middle-aged men: longitudinal results from the Massachusetts male aging study. J. Clin. Endocrinol. Metab. 87, 589-598. 10.1210/jcem.87.2.8201 [DOI] [PubMed] [Google Scholar]
- Felicio L. S., Nelson J. F. and Finch C. E. (1984). Longitudinal studies of estrous cyclicity in aging C57BL/6J mice: II. Cessation of cyclicity and the duration of persistent vaginal cornification. Biol. Reprod. 31, 446-453. 10.1095/biolreprod31.3.446 [DOI] [PubMed] [Google Scholar]
- Fernandez-Atucha A., Izagirre A., Fraile-Bermudez A. B., Kortajarena M., Larrinaga G., Martinez-Lage P., Echevarria E. and Gil J. (2017). Sex differences in the aging pattern of renin-angiotensin system serum peptidases. Biol. Sex Differ. 8, 5 10.1186/s13293-017-0128-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiest K. M., Roberts J. I., Maxwell C. J., Hogan D. B., Smith E. E., Frolkis A., Cohen A., Kirk A., Pearson D., Pringsheim T. et al. (2016). The prevalence and incidence of dementia due to Alzheimer's disease: a systematic review and meta-analysis. Can. J. Neurol. Sci. 43, Suppl. 1, S51-S82. 10.1017/cjn.2016.36 [DOI] [PubMed] [Google Scholar]
- Fisher D. W., Bennett D. A. and Dong H. (2018). Sexual dimorphism in predisposition to Alzheimer's disease. Neurobiol. Aging 70, 308-324. 10.1016/j.neurobiolaging.2018.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleisher A., Grundman M., Jack C. R. Jr, Petersen R. C., Taylor C., Kim H. T., Schiller D. H., Bagwell V., Sencakova D., Weiner M. F. et al. (2005). Sex, apolipoprotein E epsilon 4 status, and hippocampal volume in mild cognitive impairment. Arch. Neurol. 62, 953-957. 10.1001/archneur.62.6.953 [DOI] [PubMed] [Google Scholar]
- Freeman E. W., Sammel M. D. and Lin H. (2009). Temporal associations of hot flashes and depression in the transition to menopause. Menopause 16, 728-734. 10.1097/gme.0b013e3181967e16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fryer J. D., Demattos R. B., McCormick L. M., O'Dell M. A., Spinner M. L., Bales K. R., Paul S. M., Sullivan P. M., Parsadanian M., Bu G. et al. (2005). The low density lipoprotein receptor regulates the level of central nervous system human and murine apolipoprotein E but does not modify amyloid plaque pathology in PDAPP mice. J. Biol. Chem. 280, 25754-25759. 10.1074/jbc.M502143200 [DOI] [PubMed] [Google Scholar]
- Gallart-Palau X., Lee B. S., Adav S. S., Qian J., Serra A., Park J. E., Lai M. K., Chen C. P., Kalaria R. N. and Sze S. K. (2016). Gender differences in white matter pathology and mitochondrial dysfunction in Alzheimer's disease with cerebrovascular disease. Mol. Brain 9, 27 10.1186/s13041-016-0205-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Georgoulopoulou E., Vinceti M., Bonvicini F., Sola P., Goldoni C. A., De Girolamo G., Ferraro D., Nichelli P. and Mandrioli J. (2011). Changing incidence and subtypes of ALS in modena, Italy: a 10–years prospective study. Amyotroph Lateral Scler. 12, 451-457. 10.3109/17482968.2011.593037 [DOI] [PubMed] [Google Scholar]
- Ghosh M., Gälman C., Rudling M. and Angelin B. (2015). Influence of physiological changes in endogenous estrogen on circulating PCSK9 and LDL cholesterol. J. Lipid Res. 56, 463-469. 10.1194/jlr.M055780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillies G. E. and McArthur S. (2010). Independent influences of sex steroids of systemic and central origin in a rat model of Parkinson's disease: a contribution to sex-specific neuroprotection by estrogens. Horm. Behav. 57, 23-34. 10.1016/j.yhbeh.2009.06.002 [DOI] [PubMed] [Google Scholar]
- Gilsanz P., Mayeda E. R., Glymour M. M., Quesenberry C. P., Mungas D. M., DeCarli C., Dean A. and Whitmer R. A. (2017). Female sex, early-onset hypertension, and risk of dementia. Neurology 89, 1886-1893. 10.1212/WNL.0000000000004602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilsanz P., Lee C., Corrada M. M., Kawas C. H., Quesenberry C. P. Jr and Whitmer R. A. (2019). Reproductive period and risk of dementia in a diverse cohort of health care members. Neurology 92, e2005-e2014. 10.1212/WNL.0000000000007326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman Y., Bruce A. J., Cheng B. and Mattson M. P. (1996). Estrogens attenuate and corticosterone exacerbates excitotoxicity, oxidative injury, and amyloid beta-peptide toxicity in hippocampal neurons. J. Neurochem. 66, 1836-1844. 10.1046/j.1471-4159.1996.66051836.x [DOI] [PubMed] [Google Scholar]
- Goulart A. C., Zee R. Y., Pradhan A. and Rexrode K. M. (2009). Associations of the estrogen receptors 1 and 2 gene polymorphisms with the metabolic syndrome in women. Metab. Syndr. Relat. Disord. 7, 111-117. 10.1089/met.2008.0030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graff J., Rei D., Guan J. S., Wang W. Y., Seo J., Hennig K. M., Nieland T. J., Fass D. M., Kao P. F., Kahn M. et al. (2012). An epigenetic blockade of cognitive functions in the neurodegenerating brain. Nature 483, 222-226. 10.1038/nature10849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimm A., Biliouris E. E., Lang U. E., Götz J., Mensah-Nyagan A. G. and Eckert A. (2016). Sex hormone-related neurosteroids differentially rescue bioenergetic deficits induced by amyloid-beta or hyperphosphorylated tau protein. Cell. Mol. Life Sci. 73, 201-215. 10.1007/s00018-015-1988-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grubman A., Chew G., Ouyang J. F., Sun G., Choo X. Y., McLean C., Simmons R. K., Buckberry S., Vargas-Landin D. B., Poppe D. et al. (2019). A single-cell atlas of entorhinal cortex from individuals with Alzheimer's disease reveals cell-type-specific gene expression regulation. Nat. Neurosci. 22, 2087-2097. 10.1038/s41593-019-0539-4 [DOI] [PubMed] [Google Scholar]
- Grunseich C., Zukosky K., Kats I. R., Ghosh L., Harmison G. G., Bott L. C., Rinaldi C., Chen K.-L., Chen G., Boehm M. et al. (2014). Stem cell-derived motor neurons from spinal and bulbar muscular atrophy patients. Neurobiol. Dis. 70, 12-20. 10.1016/j.nbd.2014.05.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guimarães R. A., Asth L., Engelberth R. C., Cavalcante Jde S., Soares-Rachetti Vde P. and Gavioli E. C. (2015). Spontaneous failure of the estrous cycle induces anxiogenic-related behaviors in middle-aged female mice. Physiol. Behav. 147, 319-323. 10.1016/j.physbeh.2015.05.009 [DOI] [PubMed] [Google Scholar]
- Guneykaya D., Ivanov A., Hernandez D. P., Haage V., Wojtas B., Meyer N., Maricos M., Jordan P., Buonfiglioli A., Gielniewski B. et al. (2018). Transcriptional and translational differences of microglia from male and female brains. Cell Rep. 24, 2773-2783.e2776. 10.1016/j.celrep.2018.08.001 [DOI] [PubMed] [Google Scholar]
- Gunther C., von Hadeln K., Muller-Thomsen T., Alberici A., Binetti G., Hock C., Nitsch R. M., Stoppe G., Reiss J., Gal A. et al. (2004). Possible association of mitochondrial transcription factor A (TFAM) genotype with sporadic Alzheimer disease. Neurosci. Lett. 369, 219-223. 10.1016/j.neulet.2004.07.070 [DOI] [PubMed] [Google Scholar]
- Gusareva E. S., Twizere J. C., Sleegers K., Dourlen P., Abisambra J. F., Meier S., Cloyd R., Weiss B., Dermaut B., Bessonov K. et al. (2018). Male-specific epistasis between WWC1 and TLN2 genes is associated with Alzheimer's disease. Neurobiol. Aging 72, 188.e183-188.e112. 10.1016/j.neurobiolaging.2018.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haaxma C. A., Bloem B. R., Borm G. F., Oyen W. J., Leenders K. L., Eshuis S., Booij J., Dluzen D. E. and Horstink M. W. (2007). Gender differences in Parkinson's disease. J. Neurol. Neurosurg. Psychiatry 78, 819-824. 10.1136/jnnp.2006.103788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habib P., Dreymueller D., Ludwig A., Beyer C. and Dang J. (2013). Sex steroid hormone-mediated functional regulation of microglia-like BV-2 cells during hypoxia. J. Steroid Biochem. Mol. Biol. 138, 195-205. 10.1016/j.jsbmb.2013.06.003 [DOI] [PubMed] [Google Scholar]
- Hahn E. A., Wang H. X., Andel R. and Fratiglioni L. (2014). A change in sleep pattern may predict Alzheimer disease. Am. J. Geriatr. Psychiatry 22, 1262-1271. 10.1016/j.jagp.2013.04.015 [DOI] [PubMed] [Google Scholar]
- Hammond J., Le Q., Goodyer C., Gelfand M., Trifiro M. and LeBlanc A. (2001). Testosterone-mediated neuroprotection through the androgen receptor in human primary neurons. J. Neurochem. 77, 1319-1326. 10.1046/j.1471-4159.2001.00345.x [DOI] [PubMed] [Google Scholar]
- Hanamsagar R., Alter M. D., Block C. S., Sullivan H., Bolton J. L. and Bilbo S. D. (2017). Generation of a microglial developmental index in mice and in humans reveals a sex difference in maturation and immune reactivity. Glia 65, 1504-1520. 10.1002/glia.23176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harlow S. D., Gass M., Hall J. E., Lobo R., Maki P., Rebar R. W., Sherman S., Sluss P. M., de Villiers T. J. and Group S. C. (2012). Executive summary of the Stages of Reproductive Aging Workshop+10: addressing the unfinished agenda of staging reproductive aging. Menopause 19, 387-395. 10.1097/gme.0b013e31824d8f40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayashi H., Campenot R. B., Vance D. E. and Vance J. E. (2007). Apolipoprotein E-containing lipoproteins protect neurons from apoptosis via a signaling pathway involving low-density lipoprotein receptor-related protein-1. J. Neurosci. 27, 1933-1941. 10.1523/JNEUROSCI.5471-06.2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hebert L. E., Scherr P. A., McCann J. J., Beckett L. A. and Evans D. A. (2001). Is the risk of developing Alzheimer's disease greater for women than for men? Am. J. Epidemiol. 153, 132-136. 10.1093/aje/153.2.132 [DOI] [PubMed] [Google Scholar]
- Henry N., Krammer E. M., Stengel F., Adams Q., Van Liefferinge F., Hubin E., Chaves R., Efremov R., Aebersold R., Vandenbussche G. et al. (2018). Lipidated apolipoprotein E4 structure and its receptor binding mechanism determined by a combined cross-linking coupled to mass spectrometry and molecular dynamics approach. PLoS Comput. Biol. 14, e1006165 10.1371/journal.pcbi.1006165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holland D., Desikan R. S., Dale A. M. and McEvoy L. K. and Alzheimer's Disease Neuroimaging Investigators. (2013). Higher rates of decline for women and apolipoprotein E ε4 carriers. AJNR Am. J. Neuroradiol. 34, 2287-2293. 10.3174/ajnr.A3601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horsburgh K., Macrae I. M. and Carswell H. (2002). Estrogen is neuroprotective via an apolipoprotein E-dependent mechanism in a mouse model of global ischemia. J. Cereb. Blood Flow Metab. 22, 1189-1195. 10.1097/01.wcb.0000037991.07114.4e [DOI] [PubMed] [Google Scholar]
- Hsing C. H., Hung S. K., Chen Y. C., Wei T. S., Sun D. P., Wang J. J. and Yeh C. H. (2015). Histone deacetylase inhibitor trichostatin a ameliorated endotoxin-induced neuroinflammation and cognitive dysfunction. Mediators Inflamm. 2015, 163140 10.1155/2015/163140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu M., Dedhia M., Crusio W. E. and Delprato A. (2019). Sex differences in gene expression patterns associated with the APOE4 allele. F1000Res 8, 387 10.12688/f1000research.18671.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hua X., Hibar D. P., Lee S., Toga A. W., Jack C. R. Jr, Weiner M. W. and Thompson P. M. and Alzheimer's Disease Neuroimaging Investigators. (2010). Sex and age differences in atrophic rates: an ADNI study with n=1368 MRI scans. Neurobiol. Aging 31, 1463-1480. 10.1016/j.neurobiolaging.2010.04.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Liu X. Q., Wyss-Coray T., Brecht W. J., Sanan D. A. and Mahley R. W. (2001). Apolipoprotein E fragments present in Alzheimer's disease brains induce neurofibrillary tangle-like intracellular inclusions in neurons. Proc. Natl. Acad. Sci. USA 98, 8838-8843. 10.1073/pnas.151254698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y. A., Zhou B., Wernig M. and Sudhof T. C. (2017). ApoE2, ApoE3, and ApoE4 Differentially Stimulate APP Transcription and Abeta Secretion. Cell 168, 427-441.e421. 10.1016/j.cell.2016.12.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussain A., Luong M., Pooley A. and Nathan B. P. (2013). Isoform-specific effects of apoE on neurite outgrowth in olfactory epithelium culture. J. Biomed. Sci. 20, 49 10.1186/1423-0127-20-49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussain Y., Ding Q., Connelly P. W., Brunt J. H., Ban M. R., McIntyre A. D., Huff M. W., Gros R., Hegele R. A. and Feldman R. D. (2015). G-protein estrogen receptor as a regulator of low-density lipoprotein cholesterol metabolism: cellular and population genetic studies. Arterioscler. Thromb. Vasc. Biol. 35, 213-221. 10.1161/ATVBAHA.114.304326 [DOI] [PubMed] [Google Scholar]
- Hutson D. D., Gurrala R., Ogola B. O., Zimmerman M. A., Mostany R., Satou R. and Lindsey S. H. (2019). Estrogen receptor profiles across tissues from male and female Rattus norvegicus. Biol. Sex Differ. 10, 4 10.1186/s13293-019-0219-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irvine K., Laws K. R., Gale T. M. and Kondel T. K. (2012). Greater cognitive deterioration in women than men with Alzheimer's disease: a meta analysis. J. Clin. Exp. Neuropsychol. 34, 989-998. 10.1080/13803395.2012.712676 [DOI] [PubMed] [Google Scholar]
- Ishunina T. A. and Swaab D. F. (2012). Decreased alternative splicing of estrogen receptor-α mRNA in the Alzheimer's disease brain. Neurobiol. Aging 33, 286-296.e283. 10.1016/j.neurobiolaging.2010.03.010 [DOI] [PubMed] [Google Scholar]
- Ishunina T. A., Fischer D. F. and Swaab D. F. (2007). Estrogen receptor alpha and its splice variants in the hippocampus in aging and Alzheimer's disease. Neurobiol. Aging 28, 1670-1681. 10.1016/j.neurobiolaging.2006.07.024 [DOI] [PubMed] [Google Scholar]
- Jack C. R. Jr, Knopman D. S., Jagust W. J., Petersen R. C., Weiner M. W., Aisen P. S., Shaw L. M., Vemuri P., Wiste H. J., Weigand S. D. et al. (2013). Tracking pathophysiological processes in Alzheimer's disease: an updated hypothetical model of dynamic biomarkers. Lancet Neurol. 12, 207-216. 10.1016/S1474-4422(12)70291-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jack C. R. Jr, Wiste H. J., Weigand S. D., Knopman D. S., Vemuri P., Mielke M. M., Lowe V., Senjem M. L., Gunter J. L., Machulda M. M. et al. (2015). Age, sex, and APOE epsilon4 effects on memory, brain structure, and beta-amyloid across the adult life span. JAMA Neurol. 72, 511-519. 10.1001/jamaneurol.2014.4821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jack C. R. Jr, Wiste H. J., Weigand S. D., Therneau T. M., Knopman D. S., Lowe V., Vemuri P., Mielke M. M., Roberts R. O., Machulda M. M. et al. (2017). Age-specific and sex-specific prevalence of cerebral beta-amyloidosis, tauopathy, and neurodegeneration in cognitively unimpaired individuals aged 50-95 years: a cross-sectional study. Lancet Neurol. 16, 435-444. 10.1016/S1474-4422(17)30077-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs E. G., Weiss B. K., Makris N., Whitfield-Gabrieli S., Buka S. L., Klibanski A. and Goldstein J. M. (2016). Impact of sex and menopausal status on episodic memory circuitry in early midlife. J. Neurosci. 36, 10163-10173. 10.1523/JNEUROSCI.0951-16.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansen I. E., Savage J. E., Watanabe K., Bryois J., Williams D. M., Steinberg S., Sealock J., Karlsson I. K., Hagg S., Athanasiu L. et al. (2019). Genome-wide meta-analysis identifies new loci and functional pathways influencing Alzheimer's disease risk. Nat. Genet. 51, 404-413. 10.1038/s41588-018-0311-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji Y., Gong Y., Gan W., Beach T., Holtzman D. M. and Wisniewski T. (2003). Apolipoprotein E isoform-specific regulation of dendritic spine morphology in apolipoprotein E transgenic mice and Alzheimer's disease patients. Neuroscience 122, 305-315. 10.1016/j.neuroscience.2003.08.007 [DOI] [PubMed] [Google Scholar]
- Johnson M. L., Day A. E., Ho C. C., Walker Q. D., Francis R. and Kuhn C. M. (2010). Androgen decreases dopamine neurone survival in rat midbrain. J. Neuroendocrinol. 22, 238-247. 10.1111/j.1365-2826.2010.01965.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalincik T., Vivek V., Jokubaitis V., Lechner-Scott J., Trojano M., Izquierdo G., Lugaresi A., Grand'maison F., Hupperts R., Oreja-Guevara C. et al. (2013). Sex as a determinant of relapse incidence and progressive course of multiple sclerosis. Brain 136, 3609-3617. 10.1093/brain/awt281 [DOI] [PubMed] [Google Scholar]
- Kantarci O. H., Hebrink D. D., Schaefer-Klein J., Sun Y., Achenbach S., Atkinson E. J., Heggarty S., Cotleur A. C., de Andrade M., Vandenbroeck K. et al. (2008). Interferon gamma allelic variants: sex-biased multiple sclerosis susceptibility and gene expression. Arch. Neurol. 65, 349-357. [DOI] [PubMed] [Google Scholar]
- Kantarci O. H., Hebrink D. D., Achenbach S. J., Pittock S. J., Altintas A., Schaefer-Klein J. L., Atkinson E. J., De Andrade M., McMurray C. T., Rodriguez M. et al. (2004). Association of APOE polymorphisms with disease severity in MS is limited to women. Neurology 62, 811-814. 10.1212/01.WNL.0000113721.83287.83 [DOI] [PubMed] [Google Scholar]
- Kantarci O. H., Goris A., Hebrink D. D., Heggarty S., Cunningham S., Alloza I., Atkinson E. J., de Andrade M., McMurray C. T., Graham C. A. et al. (2005). IFNG polymorphisms are associated with gender differences in susceptibility to multiple sclerosis. Genes Immun. 6, 153-161. 10.1038/sj.gene.6364164 [DOI] [PubMed] [Google Scholar]
- Kara E., Marks J. D., Fan Z., Klickstein J. A., Roe A. D., Krogh K. A., Wegmann S., Maesako M., Luo C. C., Mylvaganam R. et al. (2017). Isoform- and cell type-specific structure of apolipoprotein E lipoparticles as revealed by a novel Forster resonance energy transfer assay. J. Biol. Chem. 292, 14720-14729. 10.1074/jbc.M117.784264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katsuno M., Adachi H., Kume A., Li M., Nakagomi Y., Niwa H., Sang C., Kobayashi Y., Doyu M. and Sobue G. (2002). Testosterone reduction prevents phenotypic expression in a transgenic mouse model of spinal and bulbar muscular atrophy. Neuron 35, 843-854. 10.1016/S0896-6273(02)00834-6 [DOI] [PubMed] [Google Scholar]
- Kemper M. F., Stirone C., Krause D. N., Duckles S. P. and Procaccio V. (2014). Genomic and non-genomic regulation of PGC1 isoforms by estrogen to increase cerebral vascular mitochondrial biogenesis and reactive oxygen species protection. Eur. J. Pharmacol. 723, 322-329. 10.1016/j.ejphar.2013.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim W. S., Rahmanto A. S., Kamili A., Rye K. A., Guillemin G. J., Gelissen I. C., Jessup W., Hill A. F. and Garner B. (2007). Role of ABCG1 and ABCA1 in regulation of neuronal cholesterol efflux to apolipoprotein E discs and suppression of amyloid-β peptide generation. J. Biol. Chem. 282, 2851-2861. 10.1074/jbc.M607831200 [DOI] [PubMed] [Google Scholar]
- Kim S. E., Lee J. S., Woo S., Kim S., Kim H. J., Park S., Lee B. I., Park J., Kim Y., Jang H. et al. (2019). Sex-specific relationship of cardiometabolic syndrome with lower cortical thickness. Neurology 93, e1045-e1057. 10.1212/WNL.0000000000008084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klebe S., Golmard J. L., Nalls M. A., Saad M., Singleton A. B., Bras J. M., Hardy J., Simon-Sanchez J., Heutink P., Kuhlenbaumer G. et al. (2013). The Val158Met COMT polymorphism is a modifier of the age at onset in Parkinson's disease with a sexual dimorphism. J. Neurol. Neurosurg. Psychiatry. 84, 666-673. 10.1136/jnnp-2012-304475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klosinski L. P., Yao J., Yin F., Fonteh A. N., Harrington M. G., Christensen T. A., Trushina E. and Brinton R. D. (2015). White Matter Lipids as a Ketogenic Fuel Supply in Aging Female Brain: Implications for Alzheimer's Disease. EBioMedicine 2, 1888-1904. 10.1016/j.ebiom.2015.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knopman D. S., Jack C. R. Jr, Wiste H. J., Lundt E. S., Weigand S. D., Vemuri P., Lowe V. J., Kantarci K., Gunter J. L., Senjem M. L. et al. (2014). 18F-fluorodeoxyglucose positron emission tomography, aging, and apolipoprotein E genotype in cognitively normal persons. Neurobiol. Aging 35, 2096-2106. 10.1016/j.neurobiolaging.2014.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knouff C., Hinsdale M. E., Mezdour H., Altenburg M. K., Watanabe M., Quarfordt S. H., Sullivan P. M. and Maeda N. (1999). Apo E structure determines VLDL clearance and atherosclerosis risk in mice. J. Clin. Invest. 103, 1579-1586. 10.1172/JCI6172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi N., Shinagawa S., Nagata T., Shimada K., Shibata N., Ohnuma T., Kasanuki K., Arai H., Yamada H., Nakayama K. et al. (2016). Usefulness of DNA methylation levels in COASY and SPINT1 gene promoter regions as biomarkers in diagnosis of Alzheimer's disease and amnestic mild cognitive impairment. PLoS ONE 11, e0168816 10.1371/journal.pone.0168816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kocanova S., Mazaheri M., Caze-Subra S. and Bystricky K. (2010). Ligands specify estrogen receptor alpha nuclear localization and degradation. BMC Cell Biol. 11, 98 10.1186/1471-2121-11-98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koran M. E. I., Wagener M., Hohman T. J. and Alzheimer's Neuroimaging I. (2017). Sex differences in the association between AD biomarkers and cognitive decline. Brain Imaging Behav. 11, 205-213. 10.1007/s11682-016-9523-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krasemann S., Madore C., Cialic R., Baufeld C., Calcagno N., El Fatimy R., Beckers L., O'Loughlin E., Xu Y., Fanek Z. et al. (2017). The TREM2-APOE pathway drives the transcriptional phenotype of dysfunctional microglia in neurodegenerative diseases. Immunity 47, 566-581.e569. 10.1016/j.immuni.2017.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kravitz H. M., Meyer P. M., Seeman T. E., Greendale G. A. and Sowers M. R. (2006). Cognitive functioning and sex steroid hormone gene polymorphisms in women at midlife. Am. J. Med. 119, S94-S102. 10.1016/j.amjmed.2006.07.030 [DOI] [PubMed] [Google Scholar]
- Kritz-Silverstein D., Laughlin G. A., McEvoy L. K. and Barrett-Connor E. (2017). Sex and age differences in the association of blood pressure and hypertension with cognitive function in the elderly: the rancho bernardo study. J. Prev. Alzheimers Dis. 4, 165-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumudini N., Uma A., Naushad S. M., Mridula R., Borgohain R. and Kutala V. K. (2014). Sexual dimorphism in xenobiotic genetic variants-mediated risk for Parkinson's disease. Neurol. Sci. 35, 897-903. 10.1007/s10072-013-1622-3 [DOI] [PubMed] [Google Scholar]
- Kunkle B. W., Grenier-Boley B., Sims R., Bis J. C., Damotte V., Naj A. C., Boland A., Vronskaya M., van der Lee S. J., Amlie-Wolf A., et al. (2019). Genetic meta-analysis of diagnosed Alzheimer's disease identifies new risk loci and implicates Abeta, tau, immunity and lipid processing. Nat. Genet. 51, 414-430. 10.1038/s41588-019-0358-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane-Donovan C., Wong W. M., Durakoglugil M. S., Wasser C. R., Jiang S., Xian X. and Herz J. (2016). Genetic Restoration of Plasma ApoE Improves Cognition and Partially Restores Synaptic Defects in ApoE-Deficient Mice. J. Neurosci. 36, 10141-10150. 10.1523/JNEUROSCI.1054-16.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawlor D. A., Timpson N., Ebrahim S., Day I. N. and Smith G. D. (2006). The association of oestrogen receptor alpha-haplotypes with cardiovascular risk factors in the British Women's Heart and Health Study. Eur. Heart J. 27, 1597-1604. 10.1093/eurheartj/ehi833 [DOI] [PubMed] [Google Scholar]
- Lehmann D. J., Butler H. T., Warden D. R., Combrinck M., King E., Nicoll J. A., Budge M. M., de Jager C. A., Hogervorst E., Esiri M. M. et al. (2003). Association of the androgen receptor CAG repeat polymorphism with Alzheimer's disease in men. Neurosci. Lett. 340, 87-90. 10.1016/S0304-3940(03)00069-7 [DOI] [PubMed] [Google Scholar]
- Lenz K. M., Nugent B. M., Haliyur R. and McCarthy M. M. (2013). Microglia are essential to masculinization of brain and behavior. J. Neurosci. 33, 2761-2772. 10.1523/JNEUROSCI.1268-12.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levi O. and Michaelson D. M. (2007). Environmental enrichment stimulates neurogenesis in apolipoprotein E3 and neuronal apoptosis in apolipoprotein E4 transgenic mice. J. Neurochem. 100, 202-210. 10.1111/j.1471-4159.2006.04189.x [DOI] [PubMed] [Google Scholar]
- Li D., He Q., Li R., Xu X., Chen B. and Xie A. (2012). Interleukin-10 promoter polymorphisms in Chinese patients with Parkinson's disease. Neurosci. Lett. 513, 183-186. 10.1016/j.neulet.2012.02.033 [DOI] [PubMed] [Google Scholar]
- Li G. D., Bi R., Zhang D. F., Xu M., Luo R., Wang D., Alzheimer's Disease Neuroimaging Investigators, Fang Y., Li T., Zhang C. and Yao Y. G. (2017). Female-specific effect of the BDNF gene on Alzheimer's disease. Neurobiol. Aging 53, e111-e192.e119. 10.1016/j.neurobiolaging.2016.12.023 [DOI] [PubMed] [Google Scholar]
- Lightbody G., Haberland V., Browne F., Taggart L., Zheng H., Parkes E. and Blayney J. K. (2019). Review of applications of high-throughput sequencing in personalized medicine: barriers and facilitators of future progress in research and clinical application. Brief. Bioinform. 20, 1795-1811. 10.1093/bib/bby051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin K. A., Choudhury K. R., Rathakrishnan B. G., Marks D. M., Petrella J. R. and Doraiswamy P. M. and Alzheimer's Disease Neuroimaging Investigators (2015). Marked gender differences in progression of mild cognitive impairment over 8 years. Alzheimers Dement (N Y) 1, 103-110. 10.1016/j.trci.2015.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Y. T., Seo J., Gao F., Feldman H. M., Wen H. L., Penney J., Cam H. P., Gjoneska E., Raja W. K., Cheng J. et al. (2018). APOE4 causes widespread molecular and cellular alterations associated with Alzheimer's disease phenotypes in human iPSC-derived brain cell types. Neuron 98, 1141-1154.e1147. 10.1016/j.neuron.2018.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin-Lee Y. C., Bradley W. A. and Chan L. (1981). mRNA-dependent synthesis of rat apolipoprotein E in vitro: cotranslational processing and identification of an endoglycosidase H-sensitive glycopeptide intermediate. Biochem. Biophys. Res. Commun. 99, 654-661. 10.1016/0006-291X(81)91794-0 [DOI] [PubMed] [Google Scholar]
- Lioudyno V., Abdurasulova I., Bisaga G., Skulyabin D. and Klimenko V. (2017). Single-nucleotide polymorphism rs948854 in human galanin gene and multiple sclerosis: a gender-specific risk factor. J. Neurosci. Res. 95, 644-651. 10.1002/jnr.23887 [DOI] [PubMed] [Google Scholar]
- Love S., Siew L. K., Dawbarn D., Wilcock G. K., Ben-Shlomo Y. and Allen S. J. (2006). Premorbid effects of APOE on synaptic proteins in human temporal neocortex. Neurobiol. Aging 27, 797-803. 10.1016/j.neurobiolaging.2005.04.008 [DOI] [PubMed] [Google Scholar]
- Love J. E., Day R. J., Gause J. W., Brown R. J., Pu X., Theis D. I., Caraway C. A., Poon W. W., Rahman A. A., Morrison B. E. et al. (2017). Nuclear uptake of an amino-terminal fragment of apolipoprotein E4 promotes cell death and localizes within microglia of the Alzheimer's disease brain. Int. J. Physiol. Pathophysiol. Pharmacol. 9, 40-57. [PMC free article] [PubMed] [Google Scholar]
- Lubomski M., Louise Rushworth R., Lee W., Bertram K. L. and Williams D. R. (2014). Sex differences in Parkinson's disease. J. Clin. Neurosci. 21, 1503-1506. 10.1016/j.jocn.2013.12.016 [DOI] [PubMed] [Google Scholar]
- Luchetti S., van Eden C. G., Schuurman K., van Strien M. E., Swaab D. F. and Huitinga I. (2014). Gender differences in multiple sclerosis: induction of estrogen signaling in male and progesterone signaling in female lesions. J. Neuropathol. Exp. Neurol. 73, 123-135. 10.1097/NEN.0000000000000037 [DOI] [PubMed] [Google Scholar]
- Lumbroso S., Sandillon F., Georget V., Lobaccaro J. M., Brinkmann A. O., Privat A. and Sultan C. (1996). Immunohistochemical localization and immunoblotting of androgen receptor in spinal neurons of male and female rats. Eur. J. Endocrinol. 134, 626-632. 10.1530/eje.0.1340626 [DOI] [PubMed] [Google Scholar]
- Magistri M., Velmeshev D., Makhmutova M. and Faghihi M. A. (2015). Transcriptomics profiling of Alzheimer's disease reveal neurovascular defects, altered amyloid-β homeostasis, and deregulated expression of long noncoding RNAs. J. Alzheimers Dis. 48, 647-665. 10.3233/JAD-150398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahady L., Nadeem M., Malek-Ahmadi M., Chen K., Perez S. E. and Mufson E. J. (2019). HDAC2 dysregulation in the nucleus basalis of Meynert during the progression of Alzheimer's disease. Neuropathol. Appl. Neurobiol. 45, 380-397. 10.1111/nan.12518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahley R. W., Weisgraber K. H. and Huang Y. (2009). Apolipoprotein E: structure determines function, from atherosclerosis to Alzheimer's disease to AIDS. J. Lipid Res. 50, Suppl, S183-S188. 10.1194/jlr.R800069-JLR200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mailleux J., Timmermans S., Nelissen K., Vanmol J., Vanmierlo T., van Horssen J., Bogie J. F. J. and Hendriks J. J. A. (2017). Low-density lipoprotein receptor deficiency attenuates neuroinflammation through the induction of Apolipoprotein E. Front. Immunol. 8, 1701 10.3389/fimmu.2017.01701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangold C. A., Wronowski B., Du M., Masser D. R., Hadad N., Bixler G. V., Brucklacher R. M., Ford M. M., Sonntag W. E. and Freeman W. M. (2017). Sexually divergent induction of microglial-associated neuroinflammation with hippocampal aging. J. Neuroinflammation 14, 141 10.1186/s12974-017-0920-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mani S. T. and Thakur M. K. (2006). In the cerebral cortex of female and male mice, amyloid precursor protein (APP) promoter methylation is higher in females and differentially regulated by sex steroids. Brain Res. 1067, 43-47. 10.1016/j.brainres.2005.10.006 [DOI] [PubMed] [Google Scholar]
- Manjaly Z. R., Scott K. M., Abhinav K., Wijesekera L., Ganesalingam J., Goldstein L. H., Janssen A., Dougherty A., Willey E., Stanton B. R. et al. (2010). The sex ratio in amyotrophic lateral sclerosis: A population based study. Amyotroph Lateral Scler. 11, 439-442. 10.3109/17482961003610853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mano T., Nagata K., Nonaka T., Tarutani A., Imamura T., Hashimoto T., Bannai T., Koshi-Mano K., Tsuchida T., Ohtomo R. et al. (2017). Neuron-specific methylome analysis reveals epigenetic regulation and tau-related dysfunction of BRCA1 in Alzheimer's disease. Proc. Natl. Acad. Sci. USA 114, E9645-E9654. 10.1073/pnas.1707151114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manson J. E., Aragaki A. K., Rossouw J. E., Anderson G. L., Prentice R. L., LaCroix A. Z., Chlebowski R. T., Howard B. V., Thomson C. A., Margolis K. L. et al. (2017). Menopausal hormone therapy and long-term all-cause and cause-specific mortality: the women's health initiative randomized trials. JAMA 318, 927-938. 10.1001/jama.2017.11217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marais A. D. (2019). Apolipoprotein E in lipoprotein metabolism, health and cardiovascular disease. Pathology 51, 165-176. 10.1016/j.pathol.2018.11.002 [DOI] [PubMed] [Google Scholar]
- Marioni R. E., Harris S. E., Zhang Q., McRae A. F., Hagenaars S. P., Hill W. D., Davies G., Ritchie C. W., Gale C. R., Starr J. M. et al. (2018). GWAS on family history of Alzheimer's disease. Transl. Psychiatry 8, 99 10.1038/s41398-018-0150-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marongiu R. (2019). Accelerated ovarian failure as a unique model to study peri-menopause influence on Alzheimer's disease. Front. Aging Neurosci. 11, 242 10.3389/fnagi.2019.00242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marron T. U., Guerini V., Rusmini P., Sau D., Brevini T. A., Martini L. and Poletti A. (2005). Androgen-induced neurite outgrowth is mediated by neuritin in motor neurones. J. Neurochem. 92, 10-20. 10.1111/j.1471-4159.2004.02836.x [DOI] [PubMed] [Google Scholar]
- Mata I. F., Leverenz J. B., Weintraub D., Trojanowski J. Q., Hurtig H. I., Van Deerlin V. M., Ritz B., Rausch R., Rhodes S. L., Factor S. A. et al. (2014). APOE, MAPT, and SNCA genes and cognitive performance in Parkinson disease. JAMA Neurol. 71, 1405-1412. 10.1001/jamaneurol.2014.1455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathys H., Davila-Velderrain J., Peng Z., Gao F., Mohammadi S., Young J. Z., Menon M., He L., Abdurrob F., Jiang X. et al. (2019). Single-cell transcriptomic analysis of Alzheimer's disease. Nature 570, 332-337. 10.1038/s41586-019-1195-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matyi J., Tschanz J. T., Rattinger G. B., Sanders C., Vernon E. K., Corcoran C., Kauwe J. S. K. and Buhusi M. (2017). Sex differences in risk for Alzheimer's disease related to neurotrophin gene polymorphisms: the cache county memory study. J. Gerontol. A Biol. Sci. Med. Sci. 72, 1607-1613. 10.1093/gerona/glx092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mauch D. H., Nagler K., Schumacher S., Goritz C., Muller E. C., Otto A. and Pfrieger F. W. (2001). CNS synaptogenesis promoted by glia-derived cholesterol. Science 294, 1354-1357. 10.1126/science.294.5545.1354 [DOI] [PubMed] [Google Scholar]
- McGuire V., Longstreth W. T. Jr, Koepsell T. D. and van Belle G. (1996). Incidence of amyotrophic lateral sclerosis in three counties in western Washington state. Neurology 47, 571-573. 10.1212/WNL.47.2.571 [DOI] [PubMed] [Google Scholar]
- Medway C., Combarros O., Cortina-Borja M., Butler H. T., Ibrahim-Verbaas C. A., de Bruijn R. F., Koudstaal P. J., van Duijn C. M., Ikram M. A., Mateo I. et al. (2014). The sex-specific associations of the aromatase gene with Alzheimer's disease and its interaction with IL10 in the Epistasis Project. Eur. J. Hum. Genet. 22, 216-220. 10.1038/ejhg.2013.116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng F. T., Wang Y. L., Liu J., Zhao J., Liu R. Y. and Zhou J. N. (2012). ApoE genotypes are associated with age at natural menopause in Chinese females. Age (Dordr) 34, 1023-1032. 10.1007/s11357-011-9287-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirowska-Guzel D., Mach A., Gromadzka G., Czlonkowski A. and Czlonkowska A. (2008). BDNF A196G and C270T gene polymorphisms and susceptibility to multiple sclerosis in the Polish population. Gender differences. J. Neuroimmunol. 193, 170-172. 10.1016/j.jneuroim.2007.10.013 [DOI] [PubMed] [Google Scholar]
- Miteva L., Trenova A., Slavov G. and Stanilova S. (2019). IL12B gene polymorphisms have sex-specific effects in relapsing-remitting multiple sclerosis. Acta Neurol. Belg. 119, 83-93. 10.1007/s13760-018-01066-3 [DOI] [PubMed] [Google Scholar]
- Montagne A., Nation D. A., Sagare A. P., Barisano G., Sweeney M. D., Chakhoyan A., Pachicano M., Joe E., Nelson A. R., D'Orazio L. M. et al. (2020). APOE4 leads to blood-brain barrier dysfunction predicting cognitive decline. Nature 581, 71-76. 10.1038/s41586-020-2247-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morahan J. M., Yu B., Trent R. J. and Pamphlett R. (2007). Genetic susceptibility to environmental toxicants in ALS. Am. J. Med. Genet. B Neuropsychiatr. Genet. 144B, 885-890. 10.1002/ajmg.b.30543 [DOI] [PubMed] [Google Scholar]
- Mosconi L., Berti V., Quinn C., McHugh P., Petrongolo G., Osorio R. S., Connaughty C., Pupi A., Vallabhajosula S., Isaacson R. S. et al. (2017a). Perimenopause and emergence of an Alzheimer's bioenergetic phenotype in brain and periphery. PLoS ONE 12, e0185926 10.1371/journal.pone.0185926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosconi L., Berti V., Quinn C., McHugh P., Petrongolo G., Varsavsky I., Osorio R. S., Pupi A., Vallabhajosula S., Isaacson R. S. et al. (2017b). Sex differences in Alzheimer risk: Brain imaging of endocrine vs chronologic aging. Neurology 89, 1382-1390. 10.1212/WNL.0000000000004425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukai H., Kimoto T., Hojo Y., Kawato S., Murakami G., Higo S., Hatanaka Y. and Ogiue-Ikeda M. (2010). Modulation of synaptic plasticity by brain estrogen in the hippocampus. Biochim. Biophys. Acta 1800, 1030-1044. 10.1016/j.bbagen.2009.11.002 [DOI] [PubMed] [Google Scholar]
- Muller M., den Tonkelaar I., Thijssen J. H., Grobbee D. E. and van der Schouw Y. T. (2003). Endogenous sex hormones in men aged 40-80 years. Eur. J. Endocrinol. 149, 583-589. 10.1530/eje.0.1490583 [DOI] [PubMed] [Google Scholar]
- Nathan B. P., Chang K. C., Bellosta S., Brisch E., Ge N., Mahley R. W. and Pitas R. E. (1995). The inhibitory effect of apolipoprotein E4 on neurite outgrowth is associated with microtubule depolymerization. J. Biol. Chem. 270, 19791-19799. 10.1074/jbc.270.34.19791 [DOI] [PubMed] [Google Scholar]
- Nathan B. P., Barsukova A. G., Shen F., McAsey M. and Struble R. G. (2004). Estrogen facilitates neurite extension via apolipoprotein E in cultured adult mouse cortical neurons. Endocrinology 145, 3065-3073. 10.1210/en.2003-1707 [DOI] [PubMed] [Google Scholar]
- Nathan B. P., Tonsor M. and Struble R. G. (2010). Acute responses to estradiol replacement in the olfactory system of apoE-deficient and wild-type mice. Brain Res. 1343, 66-74. 10.1016/j.brainres.2010.04.070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nazarian A., Yashin A. I. and Kulminski A. M. (2019). Genome-wide analysis of genetic predisposition to Alzheimer's disease and related sex disparities. Alzheimers Res. Ther. 11, 5 10.1186/s13195-018-0458-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson P. T., Wang W. X., Janse S. A. and Thompson K. L. (2018). MicroRNA expression patterns in human anterior cingulate and motor cortex: A study of dementia with Lewy bodies cases and controls. Brain Res. 1678, 374-383. 10.1016/j.brainres.2017.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neu S. C., Pa J., Kukull W., Beekly D., Kuzma A., Gangadharan P., Wang L. S., Romero K., Arneric S. P., Redolfi A. et al. (2017). Apolipoprotein E genotype and sex risk factors for Alzheimer disease: a meta-analysis. JAMA Neurol 74, 1178-1189. 10.1001/jamaneurol.2017.2188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen D., Dhanasekaran P., Nickel M., Mizuguchi C., Watanabe M., Saito H., Phillips M. C. and Lund-Katz S. (2014). Influence of domain stability on the properties of human apolipoprotein E3 and E4 and mouse apolipoprotein E. Biochemistry 53, 4025-4033. 10.1021/bi500340z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nilsen J., Irwin R. W., Gallaher T. K. and Brinton R. D. (2007). Estradiol in vivo regulation of brain mitochondrial proteome. J. Neurosci. 27, 14069-14077. 10.1523/JNEUROSCI.4391-07.2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishitsuji K., Hosono T., Nakamura T., Bu G. and Michikawa M. (2011). Apolipoprotein E regulates the integrity of tight junctions in an isoform-dependent manner in an in vitro blood-brain barrier model. J. Biol. Chem. 286, 17536-17542. 10.1074/jbc.M111.225532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nitkowska M., Tomasiuk R., Czyzyk M. and Friedman A. (2015). Prolactin and sex hormones levels in males with Parkinson's disease. Acta Neurol. Scand. 131, 411-416. 10.1111/ane.12334 [DOI] [PubMed] [Google Scholar]
- Norton S., Matthews F. E., Barnes D. E., Yaffe K. and Brayne C. (2014). Potential for primary prevention of Alzheimer's disease: an analysis of population-based data. Lancet Neurol. 13, 788-794. 10.1016/S1474-4422(14)70136-X [DOI] [PubMed] [Google Scholar]
- Nott A., Holtman I. R., Coufal N. G., Schlachetzki J. C. M., Yu M., Hu R., Han C. Z., Pena M., Xiao J., Wu Y. et al. (2019). Brain cell type-specific enhancer-promoter interactome maps and disease-risk association. Science 366, 1134-1139. 10.1126/science.aay0793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Numakawa T., Matsumoto T., Numakawa Y., Richards M., Yamawaki S. and Kunugi H. (2011). Protective action of neurotrophic factors and estrogen against oxidative stress-mediated neurodegeneration. J. Toxicol. 2011, 405194 10.1155/2011/405194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nygren I., Larsson A., Johansson A. and Askmark H. (2002). VEGF is increased in serum but not in spinal cord from patients with amyotrophic lateral sclerosis. Neuroreport 13, 2199-2201. 10.1097/00001756-200212030-00007 [DOI] [PubMed] [Google Scholar]
- Operto G., Cacciaglia R., Grau-Rivera O., Falcon C., Brugulat-Serrat A., Rodenas P., Ramos R., Moran S., Esteller M., Bargallo N. et al. (2018). White matter microstructure is altered in cognitively normal middle-aged APOE-epsilon4 homozygotes. Alzheimers Res. Ther. 10, 48 10.1186/s13195-018-0375-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orr-Urtreger A., Shifrin C., Rozovski U., Rosner S., Bercovich D., Gurevich T., Yagev-More H., Bar-Shira A. and Giladi N. (2007). The LRRK2 G2019S mutation in Ashkenazi Jews with Parkinson disease: is there a gender effect? Neurology 69, 1595-1602. 10.1212/01.wnl.0000277637.33328.d8 [DOI] [PubMed] [Google Scholar]
- Ossenkoppele R., van der Flier W. M., Zwan M. D., Adriaanse S. F., Boellaard R., Windhorst A. D., Barkhof F., Lammertsma A. A., Scheltens P. and van Berckel B. N. (2013). Differential effect of APOE genotype on amyloid load and glucose metabolism in AD dementia. Neurology 80, 359-365. 10.1212/WNL.0b013e31827f0889 [DOI] [PubMed] [Google Scholar]
- Ozaki Y., Yoshino Y., Yamazaki K., Sao T., Mori Y., Ochi S., Yoshida T., Mori T., Iga J. I. and Ueno S. I. (2017). DNA methylation changes at TREM2 intron 1 and TREM2 mRNA expression in patients with Alzheimer's disease. J. Psychiatr. Res. 92, 74-80. 10.1016/j.jpsychires.2017.04.003 [DOI] [PubMed] [Google Scholar]
- Palaniappan M., Nguyen L., Grimm S. L., Xi Y., Xia Z., Li W. and Coarfa C. (2019). The genomic landscape of estrogen receptor α binding sites in mouse mammary gland. PLoS ONE 14, e0220311 10.1371/journal.pone.0220311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panizzon M. S., Hauger R., Dale A. M., Eaves L. J., Eyler L. T., Fischl B., Fennema-Notestine C., Franz C. E., Grant M. D., Jak A. J. et al. (2010). Testosterone modifies the effect of APOE genotype on hippocampal volume in middle-aged men. Neurology 75, 874-880. 10.1212/WNL.0b013e3181f11deb [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park S. Y., Tournell C., Sinjoanu R. C. and Ferreira A. (2007). Caspase-3- and calpain-mediated tau cleavage are differentially prevented by estrogen and testosterone in beta-amyloid-treated hippocampal neurons. Neuroscience 144, 119-127. 10.1016/j.neuroscience.2006.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Payami H., Montee K. R., Kaye J. A., Bird T. D., Yu C. E., Wijsman E. M. and Schellenberg G. D. (1994). Alzheimer's disease, apolipoprotein E4, and gender. JAMA 271, 1316-1317. 10.1001/jama.1994.03510410028015 [DOI] [PubMed] [Google Scholar]
- Peng S., Zhao S., Yan F., Cheng J., Huang L., Chen H., Liu Q., Ji X. and Yuan Z. (2015). HDAC2 selectively regulates FOXO3a-mediated gene transcription during oxidative stress-induced neuronal cell death. J. Neurosci. 35, 1250-1259. 10.1523/JNEUROSCI.2444-14.2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pike C. J. (2001). Testosterone attenuates beta-amyloid toxicity in cultured hippocampal neurons. Brain Res. 919, 160-165. 10.1016/S0006-8993(01)03024-4 [DOI] [PubMed] [Google Scholar]
- Poirier J., Davignon J., Bouthillier D., Kogan S., Bertrand P. and Gauthier S. (1993). Apolipoprotein E polymorphism and Alzheimer's disease. Lancet 342, 697-699. 10.1016/0140-6736(93)91705-Q [DOI] [PubMed] [Google Scholar]
- Portet F., Cadilhac C., Touchon J. and Camu W. (2001). Cognitive impairment in motor neuron disease with bulbar onset. Amyotroph Lateral Scler Other Motor Neuron Disord 2, 23-29. 10.1080/146608201300079382 [DOI] [PubMed] [Google Scholar]
- Pozzilli C., Tomassini V., Marinelli F., Paolillo A., Gasperini C. and Bastianello S. (2003). ‘Gender gap’ in multiple sclerosis: magnetic resonance imaging evidence. Eur. J. Neurol. 10, 95-97. 10.1046/j.1468-1331.2003.00519.x [DOI] [PubMed] [Google Scholar]
- Praline J., Blasco H., Vourc'h P., Garrigue M. A., Gordon P. H., Camu W., Corcia P., Andres C. R. and French A. L. S. S. G. (2011). APOE ε4 allele is associated with an increased risk of bulbar-onset amyotrophic lateral sclerosis in men. Eur. J. Neurol. 18, 1046-1052. 10.1111/j.1468-1331.2010.03330.x [DOI] [PubMed] [Google Scholar]
- Prince M., Ali G. C., Guerchet M., Prina A. M., Albanese E. and Wu Y.-T. (2016). Recent global trends in the prevalence and incidence of dementia, and survival with dementia. Alzheimers Res. Ther. 8, 23 10.1186/s13195-016-0188-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prokopenko D., Hecker J., Kirchner R., Chapman B. A., Hoffman O., Mullin K., Hide W., Bertram L., Laird N., DeMeo D. L. et al. (2020). Identification of novel Alzheimer's disease loci using sex-specific family-based association analysis of whole-genome sequence data. Sci. Rep. 10, 5029 10.1038/s41598-020-61883-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu Z., Crutcher K. A., Hyman B. T. and Rebeck G. W. (2003). ApoE isoforms affect neuronal N-methyl-D-aspartate calcium responses and toxicity via receptor-mediated processes. Neuroscience 122, 291-303. 10.1016/j.neuroscience.2003.08.017 [DOI] [PubMed] [Google Scholar]
- Qureshi M., Hatem M., Alroughani R., Jacob S. P. and Al-Temaimi R. A. (2017). PLXNA3 variant rs5945430 is associated with severe clinical course in male multiple sclerosis patients. Neuromolecular Med. 19, 286-292. 10.1007/s12017-017-8443-0 [DOI] [PubMed] [Google Scholar]
- Raber J., Akana S. F., Bhatnagar S., Dallman M. F., Wong D. and Mucke L. (2000). Hypothalamic-pituitary-adrenal dysfunction in Apoe(−/−) mice: possible role in behavioral and metabolic alterations. J. Neurosci. 20, 2064-2071. 10.1523/JNEUROSCI.20-05-02064.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raber J., Bongers G., LeFevour A., Buttini M. and Mucke L. (2002). Androgens protect against apolipoprotein E4-induced cognitive deficits. J. Neurosci. 22, 5204-5209. 10.1523/JNEUROSCI.22-12-05204.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramagopalan S. V., Byrnes J. K., Orton S. M., Dyment D. A., Guimond C., Yee I. M., Ebers G. C. and Sadovnick A. D. (2010). Sex ratio of multiple sclerosis and clinical phenotype. Eur. J. Neurol. 17, 634-637. 10.1111/j.1468-1331.2009.02850.x [DOI] [PubMed] [Google Scholar]
- Rapp A., Gmeiner B. and Huttinger M. (2006). Implication of apoE isoforms in cholesterol metabolism by primary rat hippocampal neurons and astrocytes. Biochimie 88, 473-483. 10.1016/j.biochi.2005.10.007 [DOI] [PubMed] [Google Scholar]
- Ratnakumar A., Zimmerman S. E., Jordan B. A. and Mar J. C. (2019). Estrogen activates Alzheimer's disease genes. Alzheimers Dement (N Y) 5, 906-917. 10.1016/j.trci.2019.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiman E. M., Chen K., Alexander G. E., Caselli R. J., Bandy D., Osborne D., Saunders A. M. and Hardy J. (2005). Correlations between apolipoprotein E epsilon4 gene dose and brain-imaging measurements of regional hypometabolism. Proc. Natl. Acad. Sci. USA 102, 8299-8302. 10.1073/pnas.0500579102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiman E. M., Arboleda-Velasquez J. F., Quiroz Y. T., Huentelman M. J., Beach T. G., Caselli R. J., Chen Y., Su Y., Myers A. J., Hardy J. et al. (2020). Exceptionally low likelihood of Alzheimer's dementia in APOE2 homozygotes from a 5,000-person neuropathological study. Nat. Commun. 11, 667 10.1038/s41467-019-14279-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rentz D. M., Weiss B. K., Jacobs E. G., Cherkerzian S., Klibanski A., Remington A., Aizley H. and Goldstein J. M. (2017). Sex differences in episodic memory in early midlife: impact of reproductive aging. Menopause 24, 400-408. 10.1097/GME.0000000000000771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rettberg J. R., Dang H., Hodis H. N., Henderson V. W., St John J. A., Mack W. J. and Brinton R. D. (2016). Identifying postmenopausal women at risk for cognitive decline within a healthy cohort using a panel of clinical metabolic indicators: potential for detecting an at-Alzheimer's risk metabolic phenotype. Neurobiol. Aging 40, 155-163. 10.1016/j.neurobiolaging.2016.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds W. F., Rhees J., Maciejewski D., Paladino T., Sieburg H., Maki R. A. and Masliah E. (1999). Myeloperoxidase polymorphism is associated with gender specific risk for Alzheimer's disease. Exp. Neurol. 155, 31-41. 10.1006/exnr.1998.6977 [DOI] [PubMed] [Google Scholar]
- Rodriguez-Perez A. I., Valenzuela R., Villar-Cheda B., Guerra M. J., Lanciego J. L. and Labandeira-Garcia J. L. (2010). Estrogen and angiotensin interaction in the substantia nigra. Relevance to postmenopausal Parkinson's disease. Exp. Neurol. 224, 517-526. 10.1016/j.expneurol.2010.05.015 [DOI] [PubMed] [Google Scholar]
- Rosario E. R., Chang L., Head E. H., Stanczyk F. Z. and Pike C. J. (2011). Brain levels of sex steroid hormones in men and women during normal aging and in Alzheimer's disease. Neurobiol. Aging 32, 604-613. 10.1016/j.neurobiolaging.2009.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg C. K., Cummings T. J., Saunders A. M., Widico C., McIntyre L. M. and Hulette C. M. (2001). Dementia with Lewy bodies and Alzheimer's disease. Acta Neuropathol. 102, 621-626. 10.1007/s004010100415 [DOI] [PubMed] [Google Scholar]
- Roses A. D. (1996). Apolipoprotein E alleles as risk factors in Alzheimer's disease. Annu. Rev. Med. 47, 387-400. 10.1146/annurev.med.47.1.387 [DOI] [PubMed] [Google Scholar]
- Rosvall L., Rizzuto D., Wang H. X., Winblad B., Graff C. and Fratiglioni L. (2009). APOE-related mortality: effect of dementia, cardiovascular disease and gender. Neurobiol. Aging 30, 1545-1551. 10.1016/j.neurobiolaging.2007.12.003 [DOI] [PubMed] [Google Scholar]
- Ruitenberg A., Ott A., van Swieten J. C., Hofman A. and Breteler M. M. (2001). Incidence of dementia: does gender make a difference? Neurobiol. Aging 22, 575-580. 10.1016/S0197-4580(01)00231-7 [DOI] [PubMed] [Google Scholar]
- Ryan J., Carriere I., Carcaillon L., Dartigues J. F., Auriacombe S., Rouaud O., Berr C., Ritchie K., Scarabin P. Y. and Ancelin M. L. (2014). Estrogen receptor polymorphisms and incident dementia: the prospective 3C study. Alzheimers Dement 10, 27-35. 10.1016/j.jalz.2012.12.008 [DOI] [PubMed] [Google Scholar]
- Ryl A., Jasiewicz A., Grzywacz A., Adler G., Skonieczna-Zydecka K., Rotter I., Sipak-Szmigiel O., Rumianowski B., Karakiewicz B., Jurczak A. et al. (2016). Analysis of the relationship between estradiol and follicle-stimulating hormone concentrations and polymorphisms of apolipoprotein E and leptingenes in women post-menopause. Int. J. Environ. Res. Public Health 13 10.3390/ijerph13060543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saito Y., Ruberu N. N., Sawabe M., Arai T., Kazama H., Hosoi T., Yamanouchi H. and Murayama S. (2004). Lewy body-related alpha-synucleinopathy in aging. J. Neuropathol. Exp. Neurol. 63, 742-749. 10.1093/jnen/63.7.742 [DOI] [PubMed] [Google Scholar]
- Sampedro F., Vilaplana E., de Leon M. J., Alcolea D., Pegueroles J., Montal V., Carmona-Iragui M., Sala I., Sanchez-Saudinos M. B., Anton-Aguirre S. et al. (2015). APOE-by-sex interactions on brain structure and metabolism in healthy elderly controls. Oncotarget 6, 26663-26674. 10.18632/oncotarget.5185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanfilippo C., Castrogiovanni P., Imbesi R., Tibullo D., Li Volti G., Barbagallo I., Vicario N., Musumeci G. and Di Rosa M. (2019). Middle-aged healthy women and Alzheimer's disease patients present an overlapping of brain cell transcriptional profile. Neuroscience 406, 333-344. 10.1016/j.neuroscience.2019.03.008 [DOI] [PubMed] [Google Scholar]
- Sar M. and Stumpf W. E. (1977). Androgen concentration in motor neurons of cranial nerves and spinal cord. Science 197, 77-79. 10.1126/science.867053 [DOI] [PubMed] [Google Scholar]
- Sárvári M., Hrabovszky E., Kalló I., Solymosi N., Tóth K., Likó I., Széles J., Mahó S., Molnár B. and Liposits Z. (2011). Estrogens regulate neuroinflammatory genes via estrogen receptors alpha and beta in the frontal cortex of middle-aged female rats. J. Neuroinflammation 8, 82 10.1186/1742-2094-8-82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savettieri G., Messina D., Andreoli V., Bonavita S., Caltagirone C., Cittadella R., Farina D., Fazio M. C., Girlanda P., Le Pira F. et al. (2004). Gender-related effect of clinical and genetic variables on the cognitive impairment in multiple sclerosis. J. Neurol. 251, 1208-1214. 10.1007/s00415-004-0508-y [DOI] [PubMed] [Google Scholar]
- Savica R., Grossardt B. R., Bower J. H., Boeve B. F., Ahlskog J. E. and Rocca W. A. (2013). Incidence of dementia with Lewy bodies and Parkinson disease dementia. JAMA Neurol 70, 1396-1402. 10.1001/jamaneurol.2013.3579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schachter F., Faure-Delanef L., Guenot F., Rouger H., Froguel P., Lesueur-Ginot L. and Cohen D. (1994). Genetic associations with human longevity at the APOE and ACE loci. Nat. Genet. 6, 29-32. 10.1038/ng0194-29 [DOI] [PubMed] [Google Scholar]
- Scheper W. and Hoozemans J. J. (2015). The unfolded protein response in neurodegenerative diseases: a neuropathological perspective. Acta Neuropathol. 130, 315-331. 10.1007/s00401-015-1462-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmechel D. E., Saunders A. M., Strittmatter W. J., Crain B. J., Hulette C. M., Joo S. H., Pericak-Vance M. A., Goldgaber D. and Roses A. D. (1993). Increased amyloid beta-peptide deposition in cerebral cortex as a consequence of apolipoprotein E genotype in late-onset Alzheimer disease. Proc. Natl. Acad. Sci. USA 90, 9649-9653. 10.1073/pnas.90.20.9649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmid S., Rammes G., Blobner M., Kellermann K., Bratke S., Fendl D., Kaichuan Z., Schneider G. and Jungwirth B. (2019). Cognitive decline in Tg2576 mice shows sex-specific differences and correlates with cerebral amyloid-beta. Behav. Brain Res. 359, 408-417. 10.1016/j.bbr.2018.11.022 [DOI] [PubMed] [Google Scholar]
- Schneider J. A., Arvanitakis Z., Leurgans S. E. and Bennett D. A. (2009). The neuropathology of probable Alzheimer disease and mild cognitive impairment. Ann. Neurol. 66, 200-208. 10.1002/ana.21706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoonheim M. M., Popescu V., Rueda Lopes F. C., Wiebenga O. T., Vrenken H., Douw L., Polman C. H., Geurts J. J. and Barkhof F. (2012). Subcortical atrophy and cognition: sex effects in multiple sclerosis. Neurology 79, 1754-1761. 10.1212/WNL.0b013e3182703f46 [DOI] [PubMed] [Google Scholar]
- Schulz K. and Korz V. (2010). Hippocampal testosterone relates to reference memory performance and synaptic plasticity in male rats. Front. Behav. Neurosci. 4, 187 10.3389/fnbeh.2010.00187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarz J. M., Sholar P. W. and Bilbo S. D. (2012). Sex differences in microglial colonization of the developing rat brain. J. Neurochem. 120, 948-963. 10.1111/j.1471-4159.2011.07630.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shang Y., Hu X., DiRenzo J., Lazar M. A. and Brown M. (2000). Cofactor dynamics and sufficiency in estrogen receptor-regulated transcription. Cell 103, 843-852. 10.1016/S0092-8674(00)00188-4 [DOI] [PubMed] [Google Scholar]
- Shang Y., Mishra A., Wang T., Wang Y., Desai M., Chen S., Mao Z., Do L., Bernstein A. S., Trouard T. P. et al. (2020). Evidence in support of chromosomal sex influencing plasma based metabolome vs APOE genotype influencing brain metabolome profile in humanized APOE male and female mice. PLoS ONE 15, e0225392 10.1371/journal.pone.0225392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi L., Du X., Zhou H., Tao C., Liu Y., Meng F., Wu G., Xiong Y., Xia C., Wang Y. et al. (2014). Cumulative effects of the ApoE genotype and gender on the synaptic proteome and oxidative stress in the mouse brain. Int. J. Neuropsychopharmacol. 17, 1863-1879. 10.1017/S1461145714000601 [DOI] [PubMed] [Google Scholar]
- Solla P., Cannas A., Ibba F. C., Loi F., Corona M., Orofino G., Marrosu M. G. and Marrosu F. (2012). Gender differences in motor and non-motor symptoms among Sardinian patients with Parkinson's disease. J. Neurol. Sci. 323, 33-39. 10.1016/j.jns.2012.07.026 [DOI] [PubMed] [Google Scholar]
- Sowers M. R., Symons J. P., Jannausch M. L., Chu J. and Kardia S. R. (2006). Sex steroid hormone polymorphisms, high-density lipoprotein cholesterol, and apolipoprotein A-1 from the Study of Women's Health Across the Nation (SWAN). Am. J. Med. 119, S61-S68. 10.1016/j.amjmed.2006.07.008 [DOI] [PubMed] [Google Scholar]
- Spencer-Segal J. L., Tsuda M. C., Mattei L., Waters E. M., Romeo R. D., Milner T. A., McEwen B. S. and Ogawa S. (2012). Estradiol acts via estrogen receptors alpha and beta on pathways important for synaptic plasticity in the mouse hippocampal formation. Neuroscience 202, 131-146. 10.1016/j.neuroscience.2011.11.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone D. J., Molony C., Suver C., Schadt E. E. and Potter W. Z. (2010). ApoE genotyping as a progression-rate biomarker in phase II disease-modification trials for Alzheimer's disease. Pharmacogenomics J. 10, 161-164. 10.1038/tpj.2009.58 [DOI] [PubMed] [Google Scholar]
- Strittmatter W. J., Saunders A. M., Schmechel D., Pericak-Vance M., Enghild J., Salvesen G. S. and Roses A. D. (1993). Apolipoprotein E: high-avidity binding to beta-amyloid and increased frequency of type 4 allele in late-onset familial Alzheimer disease. Proc. Natl. Acad. Sci. USA 90, 1977-1981. 10.1073/pnas.90.5.1977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundermann E. E., Tran M., Maki P. M. and Bondi M. W. (2018). Sex differences in the association between apolipoprotein E epsilon4 allele and Alzheimer's disease markers. Alzheimers Dement (Amst) 10, 438-447. 10.1016/j.dadm.2018.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szewczyk-Krolikowski K., Tomlinson P., Nithi K., Wade-Martins R., Talbot K., Ben-Shlomo Y. and Hu M. T. (2014). The influence of age and gender on motor and non-motor features of early Parkinson's disease: initial findings from the Oxford Parkinson Disease Center (OPDC) discovery cohort. Parkinsonism Relat. Disord. 20, 99-105. 10.1016/j.parkreldis.2013.09.025 [DOI] [PubMed] [Google Scholar]
- Tachibana M., Holm M. L., Liu C. C., Shinohara M., Aikawa T., Oue H., Yamazaki Y., Martens Y. A., Murray M. E., Sullivan P. M. et al. (2019). APOE4-mediated amyloid-beta pathology depends on its neuronal receptor LRP1. J. Clin. Invest. 129, 1272-1277. 10.1172/JCI124853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tasaki S., Gaiteri C., Mostafavi S., De Jager P. L. and Bennett D. A. (2018). The molecular and neuropathological consequences of genetic risk for Alzheimer's dementia. Front. Neurosci. 12, 699 10.3389/fnins.2018.00699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tempfer C. B., Riener E. K., Keck C., Grimm C., Heinze G., Huber J. C., Gitsch G. and Hefler L. A. (2005). Polymorphisms associated with thrombophilia and vascular homeostasis and the timing of menarche and menopause in 728 white women. Menopause 12, 325-330. 10.1097/01.GME.0000141760.98678.ED [DOI] [PubMed] [Google Scholar]
- Tensaouti Y., Stephanz E. P., Yu T. S. and Kernie S. G. (2018). ApoE regulates the development of adult newborn hippocampal neurons. eNeuro 5, ENEURO.0155-18.2018 10.1523/ENEURO.0155-18.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tepper P. G., Randolph J. F. Jr, McConnell D. S., Crawford S. L., El Khoudary S. R., Joffe H., Gold E. B., Zheng H., Bromberger J. T. and Sutton-Tyrrell K. (2012). Trajectory clustering of estradiol and follicle-stimulating hormone during the menopausal transition among women in the Study of Women's Health across the Nation (SWAN). J. Clin. Endocrinol. Metab. 97, 2872-2880. 10.1210/jc.2012-1422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teyssier C., Belguise K., Galtier F. and Chalbos D. (2001). Characterization of the physical interaction between estrogen receptor α and JUN proteins. J. Biol. Chem. 276, 36361-36369. 10.1074/jbc.M101806200 [DOI] [PubMed] [Google Scholar]
- Theendakara V., Peters-Libeu C. A., Spilman P., Poksay K. S., Bredesen D. E. and Rao R. V. (2016). Direct transcriptional effects of apolipoprotein E. J. Neurosci. 36, 685-700. 10.1523/JNEUROSCI.3562-15.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tosun D., Schuff N., Truran-Sacrey D., Shaw L. M., Trojanowski J. Q., Aisen P., Peterson R. and Weiner M. W. and Alzheimer's Disease Neuroimaging Investigators (2010). Relations between brain tissue loss, CSF biomarkers, and the ApoE genetic profile: a longitudinal MRI study. Neurobiol. Aging 31, 1340-1354. 10.1016/j.neurobiolaging.2010.04.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van de Stolpe A., Slycke A. J., Reinders M. O., Zomer A. W., Goodenough S., Behl C., Seasholtz A. F. and van der Saag P. T. (2004). Estrogen receptor (ER)-mediated transcriptional regulation of the human corticotropin-releasing hormone-binding protein promoter: differential effects of ERalpha and ERbeta. Mol. Endocrinol. 18, 2908-2923. 10.1210/me.2003-0446 [DOI] [PubMed] [Google Scholar]
- van der Kant R., Langness V. F., Herrera C. M., Williams D. A., Fong L. K., Leestemaker Y., Steenvoorden E., Rynearson K. D., Brouwers J. F., Helms J. B. et al. (2019). Cholesterol metabolism is a druggable axis that independently regulates tau and amyloid-beta in iPSC-derived Alzheimer's disease neurons. Cell Stem Cell 24, 363-375.e369. 10.1016/j.stem.2018.12.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vemuri P., Lesnick T. G., Przybelski S. A., Knopman D. S., Lowe V. J., Graff-Radford J., Roberts R. O., Mielke M. M., Machulda M. M., Petersen R. C. Jr et al. (2017). Age, vascular health, and Alzheimer disease biomarkers in an elderly sample. Ann. Neurol. 82, 706-718. 10.1002/ana.25071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villa A., Gelosa P., Castiglioni L., Cimino M., Rizzi N., Pepe G., Lolli F., Marcello E., Sironi L., Vegeto E. et al. (2018). Sex-specific features of microglia from adult mice. Cell Rep 23, 3501-3511. 10.1016/j.celrep.2018.05.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitek M. P., Brown C. M. and Colton C. A. (2009). APOE genotype-specific differences in the innate immune response. Neurobiol. Aging 30, 1350-1360. 10.1016/j.neurobiolaging.2007.11.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voskuhl R. R., Itoh N., Tassoni A., Matsukawa M. A., Ren E., Tse V., Jang E., Suen T. T. and Itoh Y. (2019). Gene expression in oligodendrocytes during remyelination reveals cholesterol homeostasis as a therapeutic target in multiple sclerosis. Proc. Natl. Acad. Sci. USA 116, 10130-10139. 10.1073/pnas.1821306116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahjoepramono E. J., Asih P. R., Aniwiyanti V., Taddei K., Dhaliwal S. S., Fuller S. J., Foster J., Carruthers M., Verdile G., Sohrabi H. R. et al. (2016). The effects of testosterone supplementation on cognitive functioning in older men. CNS Neurol. Disord. Drug Targets 15, 337-343. 10.2174/1871527315666151110125704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Tanila H., Puolivali J., Kadish I. and van Groen T. (2003). Gender differences in the amount and deposition of amyloidβ in APPswe and PS1 double transgenic mice. Neurobiol. Dis. 14, 318-327. 10.1016/j.nbd.2003.08.009 [DOI] [PubMed] [Google Scholar]
- Wang J. M., Irwin R. W. and Brinton R. D. (2006). Activation of estrogen receptor alpha increases and estrogen receptor beta decreases apolipoprotein E expression in hippocampus in vitro and in vivo. Proc. Natl. Acad. Sci. USA 103, 16983-16988. 10.1073/pnas.0608128103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y. Q., Qu D. H. and Wang K. (2016). Therapeutic approaches to Alzheimer's disease through stimulating of non-amyloidogenic processing of amyloid precursor protein. Eur. Rev. Med. Pharmacol. Sci. 20, 2389-2403. [PubMed] [Google Scholar]
- Waters E. M., Thompson L. I., Patel P., Gonzales A. D., Ye H. Z., Filardo E. J., Clegg D. J., Gorecka J., Akama K. T., McEwen B. S. et al. (2015). G-protein-coupled estrogen receptor 1 is anatomically positioned to modulate synaptic plasticity in the mouse hippocampus. J. Neurosci. 35, 2384-2397. 10.1523/JNEUROSCI.1298-14.2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wawrusiewicz-Kurylonek N., Chorazy M., Posmyk R., Zajkowska O., Zajkowska A., Kretowski A. J., Tarasiuk J., Kochanowicz J. and Kulakowska A. (2018). The FOXP3 rs3761547 gene polymorphism in multiple sclerosis as a male-specific risk factor. Neuromolecular Med. 20, 537-543. 10.1007/s12017-018-8512-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisgraber K. H. (1990). Apolipoprotein E distribution among human plasma lipoproteins: role of the cysteine-arginine interchange at residue 112. J. Lipid Res. 31, 1503-1511. [PubMed] [Google Scholar]
- Weisgraber K. H. (1994). Apolipoprotein E: structure-function relationships. Adv. Protein Chem. 45, 249-302. 10.1016/S0065-3233(08)60642-7 [DOI] [PubMed] [Google Scholar]
- Weisgraber K. H. and Shinto L. H. (1991). Identification of the disulfide-linked homodimer of apolipoprotein E3 in plasma. Impact on receptor binding activity. J. Biol. Chem. 266, 12029-12034. [PubMed] [Google Scholar]
- Weiss G., Skurnick J. H., Goldsmith L. T., Santoro N. F. and Park S. J. (2004). Menopause and hypothalamic-pituitary sensitivity to estrogen. JAMA 292, 2991-2996. 10.1001/jama.292.24.2991 [DOI] [PubMed] [Google Scholar]
- Wennberg A. M., Tosakulwong N., Lesnick T. G., Murray M. E., Whitwell J. L., Liesinger A. M., Petrucelli L., Boeve B. F., Parisi J. E., Knopman D. S. et al. (2018). Association of apolipoprotein E epsilon4 with transactive response DNA-binding protein 43. JAMA Neurol 75, 1347-1354. 10.1001/jamaneurol.2018.3139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westlye L. T., Reinvang I., Rootwelt H. and Espeseth T. (2012). Effects of APOE on brain white matter microstructure in healthy adults. Neurology 79, 1961-1969. 10.1212/WNL.0b013e3182735c9c [DOI] [PubMed] [Google Scholar]
- Wetterau J. R., Aggerbeck L. P., Rall S. C. Jr and Weisgraber K. H. (1988). Human apolipoprotein E3 in aqueous solution. I. Evidence for two structural domains. J. Biol. Chem. 263, 6240-6248. [PubMed] [Google Scholar]
- Wijesekera L. C., Mathers S., Talman P., Galtrey C., Parkinson M. H., Ganesalingam J., Willey E., Ampong M. A., Ellis C. M., Shaw C. E. et al. (2009). Natural history and clinical features of the flail arm and flail leg ALS variants. Neurology 72, 1087-1094. 10.1212/01.wnl.0000345041.83406.a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson C., Wardell M. R., Weisgraber K. H., Mahley R. W. and Agard D. A. (1991). Three-dimensional structure of the LDL receptor-binding domain of human apolipoprotein E. Science 252, 1817-1822. 10.1126/science.2063194 [DOI] [PubMed] [Google Scholar]
- Wilson C., Mau T., Weisgraber K. H., Wardell M. R., Mahley R. W. and Agard D. A. (1994). Salt bridge relay triggers defective LDL receptor binding by a mutant apolipoprotein. Structure 2, 713-718. 10.1016/S0969-2126(00)00072-1 [DOI] [PubMed] [Google Scholar]
- Winkler J. M. and Fox H. S. (2013). Transcriptome meta-analysis reveals a central role for sex steroids in the degeneration of hippocampal neurons in Alzheimer's disease. BMC Syst. Biol. 7, 51 10.1186/1752-0509-7-51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu L., Zhang X. and Zhao L. (2018). Human ApoE isoforms differentially modulate brain glucose and ketone body metabolism: implications for Alzheimer's disease risk reduction and early intervention. J. Neurosci. 38, 6665-6681. 10.1523/JNEUROSCI.2262-17.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao E., Chen Q., Goldman A. L., Tan H. Y., Healy K., Zoltick B., Das S., Kolachana B., Callicott J. H., Dickinson D. et al. (2017). Late-onset Alzheimer's disease polygenic risk profile score predicts hippocampal function. Biol. Psychiatry Cogn Neurosci. Neuroimaging 2, 673-679. 10.1016/j.bpsc.2017.08.004 [DOI] [PubMed] [Google Scholar]
- Xu Q., Bernardo A., Walker D., Kanegawa T., Mahley R. W. and Huang Y. (2006). Profile and regulation of apolipoprotein E (ApoE) expression in the CNS in mice with targeting of green fluorescent protein gene to the ApoE locus. J. Neurosci. 26, 4985-4994. 10.1523/JNEUROSCI.5476-05.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xue S. and Jia J. (2006). Genetic association between Ubiquitin Carboxy-terminal Hydrolase-L1 gene S18Y polymorphism and sporadic Alzheimer's disease in a Chinese Han population. Brain Res. 1087, 28-32. 10.1016/j.brainres.2006.02.121 [DOI] [PubMed] [Google Scholar]
- Yaffe K., Lindquist K., Sen S., Cauley J., Ferrell R., Penninx B., Harris T., Li R. and Cummings S. R. (2009). Estrogen receptor genotype and risk of cognitive impairment in elders: findings from the Health ABC study. Neurobiol. Aging 30, 607-614. 10.1016/j.neurobiolaging.2007.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang J. J., Cho L. Y., Lim Y. J., Ko K. P., Lee K. S., Kim H., Yim S. V., Chang S. H. and Park S. K. (2010). Estrogen receptor-1 genetic polymorphisms for the risk of premature ovarian failure and early menopause. J Womens Health 19, 297-304. 10.1089/jwh.2008.1317 [DOI] [PubMed] [Google Scholar]
- Yang X., Zhao Q., An R., Zheng J., Tian S. and Xu Y. (2015). Association of the functional SNP rs2275294 in ZNF512B with risk of amyotrophic lateral sclerosis and Parkinson's disease in Han Chinese. Amyotroph Lateral Scler Frontotemporal Degener 17, 142-147. 10.3109/21678421.2015.1054291 [DOI] [PubMed] [Google Scholar]
- Yao J., Hamilton R. T., Cadenas E. and Brinton R. D. (2010). Decline in mitochondrial bioenergetics and shift to ketogenic profile in brain during reproductive senescence. Biochim. Biophys. Acta 1800, 1121-1126. 10.1016/j.bbagen.2010.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeh F. L., Wang Y., Tom I., Gonzalez L. C. and Sheng M. (2016). TREM2 Binds to Apolipoproteins, Including APOE and CLU/APOJ, and Thereby Facilitates Uptake of Amyloid-Beta by Microglia. Neuron 91, 328-340. 10.1016/j.neuron.2016.06.015 [DOI] [PubMed] [Google Scholar]
- Yin F., Yao J., Sancheti H., Feng T., Melcangi R. C., Morgan T. E., Finch C. E., Pike C. J., Mack W. J., Cadenas E. et al. (2015). The perimenopausal aging transition in the female rat brain: decline in bioenergetic systems and synaptic plasticity. Neurobiol. Aging 36, 2282-2295. 10.1016/j.neurobiolaging.2015.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yong S. M., Lim M. L., Low C. M. and Wong B. S. (2014). Reduced neuronal signaling in the ageing apolipoprotein-E4 targeted replacement female mice. Sci. Rep. 4, 6580 10.1038/srep06580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yue M., Hanna A., Wilson J., Roder H. and Janus C. (2011). Sex difference in pathology and memory decline in rTg4510 mouse model of tauopathy. Neurobiol. Aging 32, 590-603. 10.1016/j.neurobiolaging.2009.04.006 [DOI] [PubMed] [Google Scholar]
- Zannis V. I., McPherson J., Goldberger G., Karathanasis S. K. and Breslow J. L. (1984). Synthesis, intracellular processing, and signal peptide of human apolipoprotein E. J. Biol. Chem. 259, 5495-5499. [PubMed] [Google Scholar]
- Zhang L., Blackman B. E., Schonemann M. D., Zogovic-Kapsalis T., Pan X., Tagliaferri M., Harris H. A., Cohen I., Pera R. A., Mellon S. H. et al. (2010). Estrogen receptor beta-selective agonists stimulate calcium oscillations in human and mouse embryonic stem cell-derived neurons. PLoS ONE 5, e11791 10.1371/journal.pone.0011791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao L., Morgan T. E., Mao Z., Lin S., Cadenas E., Finch C. E., Pike C. J., Mack W. J. and Brinton R. D. (2012). Continuous versus cyclic progesterone exposure differentially regulates hippocampal gene expression and functional profiles. PLoS ONE 7, e31267 10.1371/journal.pone.0031267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao J., Davis M. D., Martens Y. A., Shinohara M., Graff-Radford N. R., Younkin S. G., Wszolek Z. K., Kanekiyo T. and Bu G. (2017). APOE epsilon4/epsilon4 diminishes neurotrophic function of human iPSC-derived astrocytes. Hum. Mol. Genet. 26, 2690-2700. 10.1093/hmg/ddx155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao N., Attrebi O. N., Ren Y., Qiao W., Sonustun B., Martens Y. A., Meneses A. D., Li F., Shue F., Zheng J. et al. (2020a). APOE4 exacerbates alpha-synuclein pathology and related toxicity independent of amyloid. Sci. Transl. Med. 12, eaay1809 10.1126/scitranslmed.aay1809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao N., Ren Y., Yamazaki Y., Qiao W., Li F., Felton L. M., Mahmoudiandehkordi S., Kueider-Paisley A., Sonoustoun B., Arnold M. et al. (2020b). Alzheimer's risk factors age, APOE genotype, and sex drive distinct molecular pathways. Neuron 106, 727-742.e6. 10.1016/j.neuron.2020.02.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng M., Wei J., Tang Y., Yang C., Wei Y., Yin X. and Liu Q. (2014). ApoE-deficient promotes blood-brain barrier disruption in experimental autoimmune encephalomyelitis via alteration of MMP-9. J. Mol. Neurosci. 54, 282-290. 10.1007/s12031-014-0291-x [DOI] [PubMed] [Google Scholar]
- Zhou C. N., Chao F. L., Zhang Y., Jiang L., Zhang L., Luo Y. M., Xiao Q., Chen L. M. and Tang Y. (2018). Sex differences in the white matter and myelinated fibers of APP/PS1 mice and the effects of running exercise on the sex differences of AD mice. Front. Aging Neurosci. 10, 243 10.3389/fnagi.2018.00243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou M., Zhao H., Wang X., Sun J. and Su J. (2019). Analysis of long noncoding RNAs highlights region-specific altered expression patterns and diagnostic roles in Alzheimer's disease. Brief. Bioinform. 20, 598-608. 10.1093/bib/bby021 [DOI] [PubMed] [Google Scholar]
- Zhou X. and Xu J. (2015). Identification of Alzheimer's disease-associated long noncoding RNAs. Neurobiol. Aging 36, 2925-2931. 10.1016/j.neurobiolaging.2015.07.015 [DOI] [PubMed] [Google Scholar]
- Zhu Y., Nwabuisi-Heath E., Dumanis S. B., Tai L. M., Yu C., Rebeck G. W. and LaDu M. J. (2012). APOE genotype alters glial activation and loss of synaptic markers in mice. Glia 60, 559-569. 10.1002/glia.22289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu K., Teng J., Zhao J., Liu H. and Xie A. (2016). Association of TLR9 polymorphisms with sporadic Parkinson's disease in Chinese Han population. Int. J. Neurosci. 126, 612-616. 10.3109/00207454.2015.1050591 [DOI] [PubMed] [Google Scholar]