Abstract
INTRODUCTION:
Proton pump inhibitors (PPIs) increase the risk for enteric infections that is likely related to PPI-induced hypochlorhydria. Although the impact of acid suppression on severe acute respiratory syndrome coronavirus 2 is unknown thus far, previous data revealed that pH ≤3 impairs the infectivity of the similar severe acute respiratory syndrome coronavirus 1. Thus, we aimed to determine whether use of PPIs increases the odds for acquiring coronavirus disease 2019 (COVID-19) among community-dwelling Americans.
METHODS:
From May 3 to June 24, 2020, we performed an online survey described to participating adults as a “national health survey.” A multivariable logistic regression was performed on reporting a positive COVID-19 test to adjust for a wide range of confounding factors and to calculate adjusted odds ratios (aORs) and 95% confidence intervals (CIs).
RESULTS:
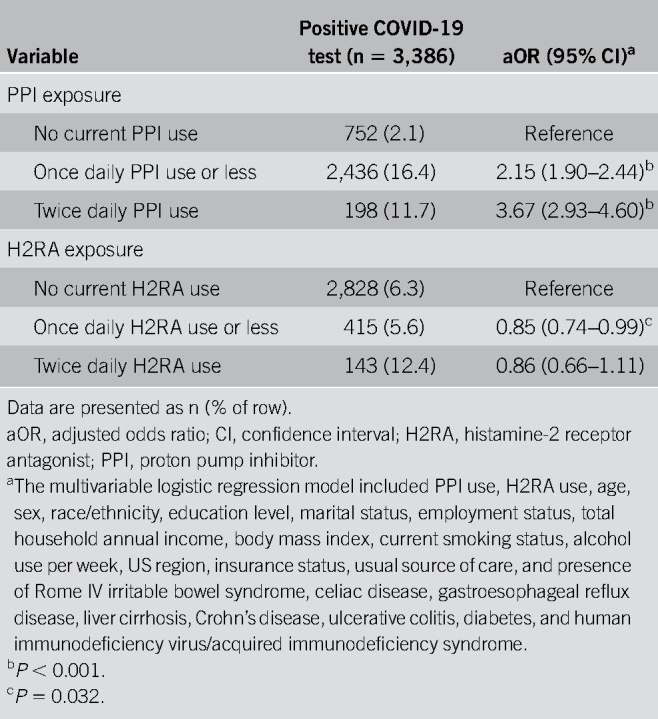
Of 53,130 participants, 3,386 (6.4%) reported a positive COVID-19 test. In regression analysis, individuals using PPIs up to once daily (aOR 2.15; 95% CI, 1.90–2.44) or twice daily (aOR 3.67; 95% CI, 2.93–4.60) had significantly increased odds for reporting a positive COVID-19 test when compared with those not taking PPIs. Individuals taking histamine-2 receptor antagonists were not at elevated risk.
DISCUSSION:
We found evidence of an independent, dose-response relationship between the use of antisecretory medications and COVID-19 positivity; individuals taking PPIs twice daily have higher odds for reporting a positive test when compared with those using lower-dose PPIs up to once daily, and those taking the less potent histamine-2 receptor antagonists are not at increased risk. These findings emphasize good clinical practice that PPIs should only be used when indicated at the lowest effective dose, such as the approved once-daily label dosage of over-the-counter and prescription PPIs. Further studies examining the association between PPIs and COVID-19 are needed.
INTRODUCTION
Proton pump inhibitors (PPIs) are among the most commonly used medications in the United States and have been linked to side effects including bone fracture, chronic kidney disease, and gastrointestinal (GI) infections, among others (1). Although a recent randomized controlled trial did not confirm most of these purported complications, it found that once daily PPI use increased the odds for enteric infection by 33% (2). Meta-analyses also reveal that PPIs are associated with increased risk of both enteric infections and small intestinal bacterial overgrowth (3–5), and a 2019 study by Vilcu et al. (6) found that continuous use of PPIs is associated with increased risk of viral infection during periods of high endemic prevalence. Thus, although most hypothesized complications from PPIs have not withstood the test of time (1), enteric infection is one adverse event supported by both meta-analyses and randomized controlled trial data. This effect is likely related to PPI-induced hypochlorhydria, which impairs the body's proximal defense against ingested bacteria and viruses (1), and may also occur because prolonged use of PPIs reduces microbial diversity in the gut (7), an effect believed to enable colonization of some enteric pathogens (8).
Although the impact of acid suppression on severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is unknown thus far, previous data revealed that pH ≤3—the normal pH of a healthy stomach—impairs the infectivity of the similar severe acute respiratory syndrome coronavirus 1, whereas less acidic pH in the range achieved with PPI therapy does not inactivate the virus (9). This is relevant because SARS-CoV-2 can enter the body not only through the respiratory system but also through the GI system (10,11). The virus uses the angiotensin-converting enzyme-2 receptor, which is widely expressed throughout the intestinal tract (12), to rapidly invade and replicate within enterocytes (13). Once SARS-CoV-2 colonizes the GI tract, it can lead to gastritis, enteritis, and colitis (10,14), and a recent report posted by the US Centers for Disease Control and Prevention documented evidence of infectious virus—not just viral RNA—in the stool from a patient with severe coronavirus disease 2019 (COVID-19) infection (15). Similarly, another study also described finding “live” virus in the feces (16). Other reports reveal that nearly half of patients with COVID-19 have viral RNA in their stool (17), at times when not concurrently found in the respiratory tract (18), and research suggests that monitoring SARS-CoV-2 levels in sewage may provide a lead-time indicator for COVID-19 cases and hospitalizations within a community (19–22); this technique is now being tested by municipalities around the world. Taken together, this body of research, in addition to other studies (23,24), strongly implicates the GI system as a major portal for SARS-CoV-2 infection.
In addition, because the gut is the largest immune organ in the body and can host colonies of rapidly replicating SARS-CoV-2 (13), there is concern that the virus could spread beyond the GI tract not only by causing digestive symptoms but also by seeding infection or promoting inflammation in other organ systems, including the respiratory tract via a “gut-lung axis” (11,25,26). Previous research with the Middle East Respiratory Syndrome coronavirus found that pretreating mice with pantoprazole, a PPI, showed “exaggerated” evidence of not only enteric infection but also revealed epithelial degeneration in the small bowel. Notably, the virus was subsequently found to emerge in lung tissue. The authors note that the spread of virus from intestine to lungs indicates “development of sequential respiratory infection” after inoculating the stomach—not the lungs—with a coronavirus that uses the angiotensin-converting enzyme-2 receptor to gain gut entry into the body (26). Other investigators posit that SARS-CoV-2's disruption of the epithelial layer can lead to release of endotoxins and microbial metabolites that subsequently trigger inflammation and cytokine release in distant organs, such as the lungs (11,25). Because PPIs may undermine the gastric barrier to SARS-CoV-2 entry and reduce microbial diversity in the gut, coupled with the established link between PPIs and GI infection shown in meta-analyses (3–5) and randomized controlled trial data (2), it is possible that PPIs might also increase the risk for COVID-19, a hypothesis previously posed by other researchers (27,28). In this study, we further investigated the potential link between PPIs and COVID-19 in a nationwide survey of Americans.
METHODS
To test our a priori hypothesis, based on a foundation of biological plausibility, we used data from an online, self-administered survey of Americans collected from May 3 to June 24, 2020. We collaborated with an online survey research firm (Cint; www.cint.com) that sought to recruit a nationwide, representative sample based on US Census data on age, sex, and region. The Cint research panels have been widely used by investigators across the globe on a range of studies, including GI research supported by the National Institutes of Health and the Rome Foundation (29–37). The Cint platform complies with European Society for Opinion and Marketing Research, Market Research Society, Advertising Research Foundation, Marketing Research and Intelligence Association, American Marketing Association, Association of Market and Social Research Organizations, and Insight Association standards for quality control and fraud detection of survey respondents. Details regarding the Cint Quality Charter may be found at this website: www.cint.com/quality. The authors have no relationship, financial or otherwise, with Cint. Adult panelists received an email inviting them to complete a “national health survey,” which was administered solely in English. The Cedars-Sinai Institutional Review Board approved this study (Pro56183).
All participants who were 18 years of age or older were eligible for the study. Respondents were first shown a list of common GI symptoms, and those endorsing a history of abdominal pain or discomfort, acid reflux, heartburn, or regurgitation were separately asked about any current PPI and/or histamine-2 receptor antagonist (H2RA) use. For those currently taking PPIs and H2RAs, we assessed their frequency and duration of use. We also examined whether respondents were tested for COVID-19; those with a positive test were asked about new symptoms they experienced, if any, at the time of diagnosis, including ageusia, anosmia, GI (abdominal pain, diarrhea, and nausea/vomiting), respiratory, or systemic symptoms. Individuals taking a PPI or H2RA for ≤1 month and who were diagnosed with COVID-19 at least 2 months before survey completion were classified as nonusers to help reduce the risk of protopathic bias.
All statistical analyses were performed in Stata 13.1 (StataCorp LP, College Station, TX), and a 2-tailed P value < 0.05 was considered statistically significant. We performed a multivariable logistic regression on reporting a positive COVID-19 test to adjust for a wide range of potentially confounding factors and to calculate adjusted odds ratios (aORs) and 95% confidence intervals (CIs). Among respondents who were COVID-19 positive, we also conducted a regression model on the presence of GI symptoms associated with COVID-19 (abdominal pain, diarrhea, nausea/vomiting). Both regression models included PPI and H2RA exposures and relevant demographic, socioeconomic, lifestyle, and comorbidity variables.
RESULTS
Overall, 264,058 individuals were invited by Cint to complete the survey, of whom 128,847 (48.8%) accessed the site. Of the 86,602 eligible respondents who completed the survey, 53,130 (61.3%) noted previous abdominal pain or discomfort (n = 36,498, 68.7%), acid reflux or heartburn (n = 39,969, 75.2%), or regurgitation (n = 25,522, 48.0%) and were thus asked about use of antisecretory medications. The study cohort's demographics are shown in Table 1 with comparisons to the general US population noted in Table 1, Supplementary Digital Content 1, http://links.lww.com/AJG/B613. The cohort resembled the general US population across most sociodemographic strata with the notable exception of age 60 years and older (29.8% of US population; 13.3% of cohort).
Table 1.
Demographics of the study cohort
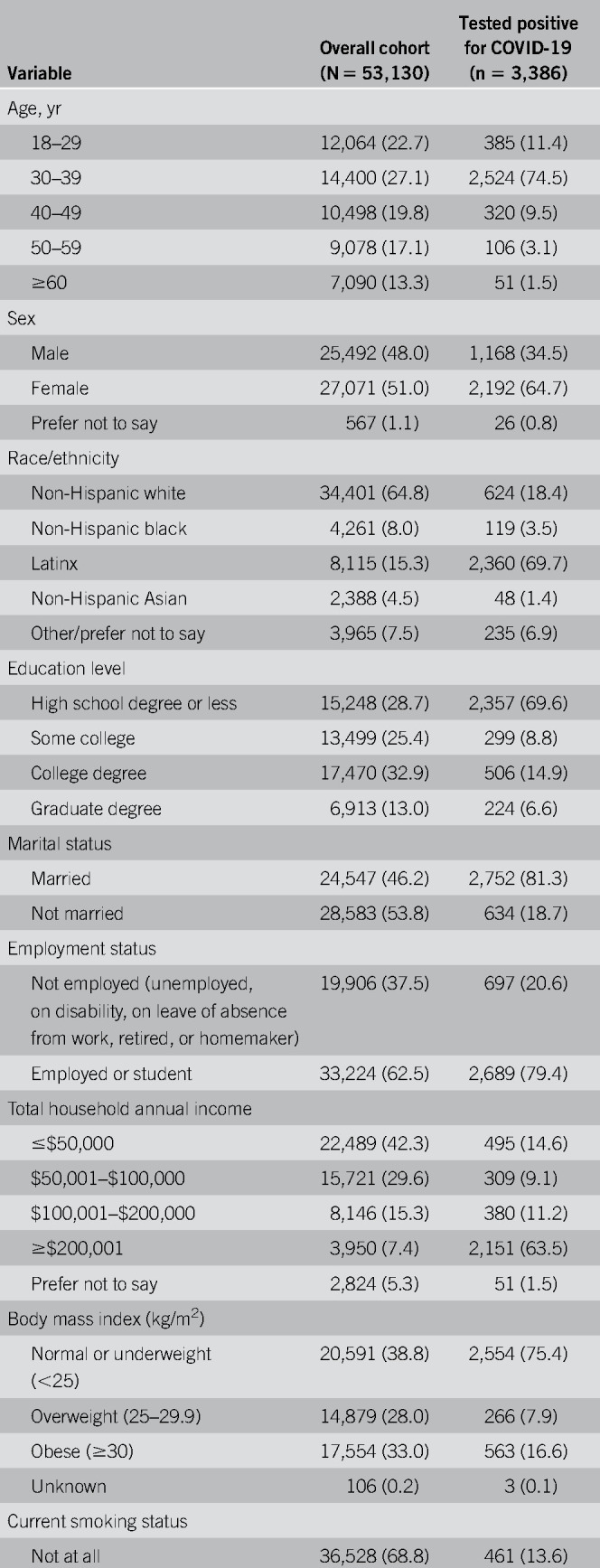
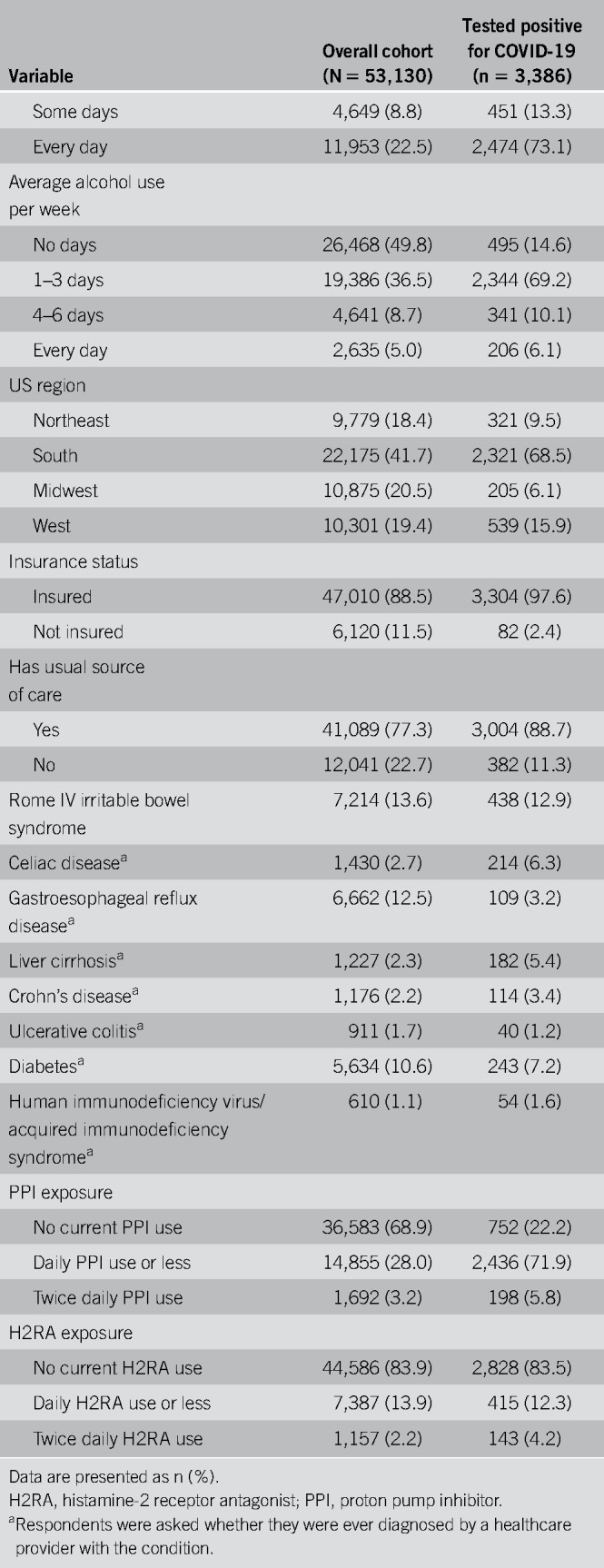
We found that 3,386 participants (6.4%) reported a positive COVID-19 test; Table 1 presents the demographics of those who tested positive. Because this study was conducted between early May and late June 2020, during a time of dynamic epidemiologic changes in the COVID-19 pandemic in America, we divided the cohort into first half vs second half groups to examine potential differences in the study population over time (see Table 2, Supplementary Digital Content 2, http://links.lww.com/AJG/B614). The data revealed shifts in the respondent profile as the study progressed; the latter group was meaningfully different from the initial group across many sociodemographic characteristics. For example, in the first half of the survey period, the COVID-19 positivity rate was 2.5% and the overall demographics seemed more consistent with the overall US population. In the second half the self-reported positivity rate rose substantially. Similarly, as the study progressed, the COVID-19 population of survey takers became younger, more likely to be from the South region of the United States, more likely to be Latinx, less educated, and more likely to report a total annual household income ≥$200,001. We comment on these demographic results further in the Discussion section.
In multivariable regression analysis across the full sample, PPI use was independently associated with increased odds for reporting a positive COVID-19 test, even after adjusting for a wide range of sociodemographic, lifestyle, and clinical variables (Table 2). When compared with individuals not using PPIs, those taking PPIs up to once daily (aOR 2.15; 95% CI, 1.90–2.44) or twice daily (aOR 3.67; 95% CI, 2.93–4.60) had significantly increased odds for reporting a positive COVID-19 test. Regarding H2RAs, which cause less hypochlorhydria than PPIs, use of lower-dose H2RAs was associated with slightly decreased odds for reporting a positive test while no association was seen for higher-dose H2RAs. In addition to PPI usage, we found that men (aOR 1.23; 95% CI, 1.10–1.38), everyday smokers (aOR 5.05; 95% CI, 4.39–5.80), non-Hispanic Blacks (aOR 1.80; 95% CI, 1.45–2.24), and Latinxs (aOR 3.54; 95% CI, 3.09–4.04) were significantly more likely to report being positive for COVID-19, consistent with previous data (38–45).
Table 2.
Results from the multivariable logistic regression model on reporting a positive COVID-19 test (N = 53,130)
In another regression analysis among the overall cohort that included duration of antisecretory use, we found the following regarding PPI exposure: no current PPI use—reference; up to once-daily PPI for ≤6 months—aOR 3.25 (95% CI, 2.81–3.77); up to once-daily PPI use for >6 months—aOR 1.44 (95% CI, 1.22–1.70); twice daily PPI use for ≤6 months—aOR 2.31 (95% CI, 1.42–3.77); twice daily PPI use for >6 months—aOR 3.81 (95% CI, 2.97–4.87).
Given the shifts in the COVID-19 study population observed in Table 2, Supplementary Digital Content 2, http://links.lww.com/AJG/B614, we sought to confirm whether our results could be reproduced across multiple sensitivity analyses. First, we repeated the analyses within the first vs second half cohorts. We found that in both groups, regardless of the sociodemographic makeup of that group, those taking PPIs up to once daily or twice daily remained at significantly increased odds for reporting a positive COVID-19 test in a dose-response manner; no statistically significant associations were seen for H2RA use in either period (see Table 3, Supplementary Digital Content 3, http://links.lww.com/AJG/B615). To test the robustness of this finding, we repeated the analyses again for every 2-week block of the study (4 blocks in total) and again found a dose-response effect for each analysis despite smaller sample sizes by subgroup. In short, although the demographics of the population changed throughout the study, the relationship between PPIs and COVID-19 remained stable and significant in an apparent dose-response pattern; this relationship seemed invariant despite demographic shifts.
Because of comments related to the demographic mix of participants with COVID-19 in the study (46), we conducted another series of sensitivity analyses to further test whether the results could reproduce under different scenarios. First, we excluded Latinx participants and repeated the regression analyses; the results were again consistent with a PPI dose-response effect (see Table 3, Supplementary Digital Content 3, http://links.lww.com/AJG/B615). Then, we progressed a step further by excluding all Latinx subjects with total annual household income ≥$200,001; we observed similar findings. We next excluded all Latinx subjects with total annual household income ≥$200,001 and with a high school education or less—a combination suggested to be unlikely by some readers (46); nonetheless, removing this subgroup did not affect the results. In all, we conducted a total of 17 separate sensitivity analyses and found a statistically significant PPI dose-response relationship in all but one geographical subanalysis (Midwest US region).
Among those who tested positive for COVID-19 (n = 3,386), 3,267 (96.5%) were symptomatic (ageusia, anosmia, GI, respiratory, or systemic symptoms) and 674 (19.9%) reported new onset of abdominal pain, diarrhea, or nausea/vomiting. In regression analysis, we found that individuals taking lower-dose PPIs (n = 266, 10.9%; aOR 0.62 [95% CI, 0.49–0.78]) had lower odds for reporting GI COVID-19 symptoms vs those not on PPIs (n = 297, 39.5%; reference). Conversely, no association was seen with twice daily use (n = 111, 56.1%; aOR 1.04 [95% CI, 0.70–1.57]).
DISCUSSION
In a nationwide study of individuals with a history of GI symptoms, we found that use of PPIs is associated with increased odds for reporting a positive COVID-19 test. The highest risk is seen among individuals taking PPIs twice daily—a common off-label practice in both primary and secondary care (47,48)—because they are nearly 4-times more likely to report COVID-19 positivity when compared with those not on PPIs. Because meta-analysis reveals that twice daily PPIs do not offer clinically meaningful benefits over once daily dosing for gastroesophageal reflux disease (GERD) (49) and given that many patients on PPIs have no clear indication for use (50–56), our findings further emphasize that PPIs should only be used when clinically indicated at the lowest effective dose. Data also indicate that 80% of patients on greater than single-dose PPI are able to step-down to daily PPI without recurrence of reflux symptoms (57). Moreover, investigators tested a step-down therapy approach among patients whose GERD symptoms were under control with PPIs and found that 34% were able to switch to H2RAs and 15% remained asymptomatic off PPI therapy 1 year later (58).
Our study has several strengths. To our knowledge, this is the first study examining the relationship between PPIs and COVID-19 among a nationwide sample of Americans. Our finding that PPI use is associated with increased odds for acquiring SARS-CoV-2, which invades and replicates within enterocytes (13), is consistent with previous literature showing that PPIs also increase the risk for other enteric infections (1–6). Most of these studies, though, did not assess the impact of twice-daily dosing; further research examining whether PPI twice daily increases the risk for such infections over once-daily dosing are needed. We also examined the association between PPIs and GI COVID-19 symptoms and found that PPIs do not increase the odds for reporting such symptoms. Because GI symptoms are prevalent in those with COVID-19 (14), further studies assessing the mechanisms behind its differential presentations are needed. Moreover, unlike many studies that use retrospective data to examine potential PPI side effects (1), we prospectively constructed this online survey to test an a priori hypothesis. Although this approach has inherent limitations, as described below, leveraging an online, self-administered platform allows for efficient recruitment of a national sample; findings from single-site studies with limited sample sizes of patients presenting with COVID-19 may be less generalizable to other settings and populations.
There are also limitations to our study. First, the prevalence of COVID-19 in the overall study population (6.4%) was higher than current national estimates (46). As previously noted, this was not a study of the general population; it was a study of individuals with previous abdominal pain or discomfort, acid reflux, heartburn, or regurgitation and was not designed to arrive at a population estimate for COVID-19. Because most survey questions focused on GI symptoms, those with such symptoms may have been predisposed to completing the survey (the COVID-19 questions came at the end of the survey). Because COVID-19 commonly leads to GI symptoms (14), this selection may have contributed to the higher than expected positivity rate. There are other potential explanations for this finding. Although we generically positioned our survey at the outset as a “national health survey” and not as a COVID-19- or PPI-focused study, our results may be subject to participation bias because it occurred during a pandemic and, as a result, may have oversampled patients with COVID-19 who considered a “health survey” particularly relevant at a time of illness. It is also possible that those with COVID-19 may have been more likely to complete an online health survey while quarantined at home or may have heard about it from friends or family who received the survey.
Even with these potential explanations, it is possible that some respondents were simply dishonest regarding their diagnosis of COVID-19, particularly among those who completed the survey toward the end of the recruitment period when the prevalence rose considerably at a rate outpacing national data. Although it is unclear why an individual would falsify his or her COVID-19 status, it is also less clear how dishonesty would fall along a biological gradient of acid suppression. For example, it is not clear why people using twice daily PPI would be more dishonest about COVID-19 than patients on once daily PPI or why those on once daily PPI would be more dishonest than those using H2RAs. Perhaps use of PPIs—but not H2RAs—is a surrogate marker for other factors associated with dishonesty, but we are challenged to offer a reasonable explanation. In addition, self-reported COVID-19 status has been used in other recent surveys regarding pandemic epidemiology (59,60).
Although there are many appropriate indications for PPIs, few individuals in the cohort specifically endorsed having received a formal diagnosis of GERD by a physician. That does not mean, however, that this cohort of PPI users did not experience GERD-related symptoms because 75.2% and 48.0% of respondents reported experiencing acid reflux/heartburn or regurgitation, respectively. This disconnect between the high prevalence of GERD symptoms but low rate of formal physician diagnosis suggests that many individuals in this sample were self-managing their GERD symptoms with over-the-counter PPIs or H2RAs without guidance from a clinician, consistent with published data (61), and thus would not have received a formal diagnosis. It is also possible that some respondents mistakenly failed to endorse “GERD”—a medical term—in contrast to “acid reflux” when they were asked to select among a list of physician-diagnosed conditions but did endorse symptoms when presented with a list of cardinal GERD symptoms. Some may also have forgotten having received a formal diagnosis of GERD. In any event, the PPI users did have a high prevalence of GERD symptoms, as expected.
Regarding sex, we noted in unadjusted analysis that there was a higher proportion of women than men among those with COVID-19. However, in adjusted analysis, men had slightly increased odds for being positive. At first glance, this may seem paradoxical. However, in bivariate analyses, we found that women in this sample were more likely to be insured (potentially allowing easier access to COVID-19 testing), more likely to be Latinx (a group disproportionately affected by COVID-19 (45)), and more likely to be from the South (a region with a high and increasing prevalence of COVID-19 during the conduct of this study (62)). Thus, there were multiple imbalances likely operating together to increase risk of COVID-19 among women in this cohort. When multivariable regression analysis was performed while accounting for these multiple imbalances, the analysis revealed that being a man was independently associated with slightly increased risk of COVID-19. That is, being a woman was a surrogate for several predictors of COVID-19 but was not, itself, a predictor of COVID-19. Although men seem to have higher rates for COVID-19-related hospitalizations vs women (63), the pandemic is rapidly evolving and time will determine whether there are also disparities regarding cases of COVID-19.
As the survey progressed, there was an increasing proportion of Latinxs reporting a high school education or less while also reporting a total household income of ≥$200,001. Because we did not obtain data on number of individuals in the household, we do not know whether there were other cohabitants contributing to the reported total annual household income (in contrast to personal income, which we did not ask about). Of note, Latinx individuals in the United States are considerably more likely to live in multigenerational households than other groups (64). It is also possible that more respondents in the second half of the study were simply dishonest about their income or education.
Although it is unclear why the proportion of younger and Latinx individuals with COVID-19 was so pronounced in the latter part of the study, it is important to note that during the study period the median age for cases decreased (65) when compared with the start of the pandemic (66) and that Latinxs continue to be disproportionately affected (45). As of July 12, 2020, California, Florida, and Texas—states that are COVID-19 “hot spots” (62) and have the highest share of the US Hispanic population (64)—reported the following regarding the age groups with the highest proportion of cases and overall percentage that are Latinx (45,67–69): California—age group: 18–34 years old; Latinx: 55% (vs 39% of state population); Florida—age group: 25–34 years old; Latinx: 44% (vs 25% of state population); Texas—age group: 20–39 years old; Latinx: 50% (vs 39% of state population).
We inquired with the survey research firm, Cint, to determine whether there had been any changes in their inclusion or exclusion criteria during the course of the study or whether any other change in their procedure might explain the differences in COVID-19 demographics between the first and second halves of the study. Cint indicated no changes were made in their recruitment process during the study. They enforced standard measures to reduce fraudulent answers and bots, as outlined in their Quality Charter (70). They did note, however, that during the COVID-19 pandemic, there has been a surge of engagement with Cint surveys in tandem with the conduct of this study, possibly because people have been social distancing and staying home, or have lost a job or suffered a pay cut, and therefore joined survey panels for additional income and to pass time at home. Others may have been quarantined because they had COVID-19. As the COVID-19 pandemic has expanded sociodemographic disparities, particularly among Latinx and less educated individuals who have experienced pay cuts and job losses at a higher rate than other groups (71,72), it is plausible to observe a disproportionate increase in these demographics in the second half of this survey. We do not believe this summarily invalidates the second half respondents but does indicate they may be systematically different from the first half respondents. In any event, we found the same results in both groups.
These evolving demographics during the survey period notwithstanding, we found consistent evidence that those using PPIs remained at significantly increased odds for being COVID-19 positive in each timeframe, whereas those on H2RAs were not, following a lockstep biological gradient in each period. Thus, although there were potential demographic anomalies in the latter period of the survey, the results of the study remained stable throughout all periods despite dynamic changes in the study population. In the first 2 weeks of the study, when the demographic distributions of the COVID-19 sample seemed more closely tied to the general population, there was a dose-response effect between use of PPIs and COVID-19. Similarly, in every period thereafter, no matter the demographic shifts that occurred, the same result remained consistent.
As with all observational studies, our study is susceptible to residual confounding. Although the aOR of 3.67 seen with twice-daily PPI use is in the “zone of interest” (odds ratio [OR] >3) (1), suggesting that bias alone might not entirely explain that degree of effect size, the aOR of 2.15 noted with up to once daily PPI use falls within the “zone of potential bias” (0.33 < OR<3) and may reflect residual confounding from unmeasured variables not included in the model. For instance, individuals with certain comorbidities that increase the risk for severe COVID-19 (e.g., cardiovascular disease, chronic obstructive pulmonary disease, and chronic kidney disease (63)) may also be more likely to take PPIs. However, it is unclear whether these risk factors apply to acquiring COVID-19, which was the subject of this study, in contrast to developing severe COVID-19. Nevertheless, although our regression model included age and smoking status as surrogates for these conditions, their noninclusion is a potential limitation of the study.
Selection bias may also be an issue because those severely ill and hospitalized with COVID-19 were unlikely to have taken the survey. Our survey was also conducted solely online and thus had a lower than expected proportion of individuals 60 years of age and older; although 73% of those 65 years of age and older currently use the internet (73), we may have selected for an elderly population that was more functional and independent.
There are also potential risks for misclassification and recall biases for medications. It is unclear, however, why misreporting of PPIs vs H2RAs would vary by COVID-19 status. That is, it seems unlikely that people with COVID-19 would misreport using a PPI (but not an H2RA), while people without COVID-19 would correctly classify such use. The short recall period also reduces risk of recall bias, and it is less of a concern for the medication data because we asked respondents about their current usage. Another potential limitation is that we did not determine how respondents tested positive for COVID-19 (e.g., polymerase chain reaction or serology testing) nor did we measure disease severity. We suspect, though, that most participants underwent polymerase chain reaction testing, in contrast to antibody surveillance, because most respondents had symptomatic COVID-19. Finally, there are limitations related to generalizability because the survey was administered only in English and did not assess reading ability; the findings may not be generalizable to non-English speakers or those with limited literacy.
In light of the strengths and limitations of this study, it is useful to place the results within the context of the traditional Hill criteria for establishing causality between a risk factor and an outcome, particularly because Vaezi et al. (1) recommended applying these criteria when assessing purported PPI associations. In the case of PPIs, it is vital to first pose and defend a biological mechanism linking the PPI to the adverse event; this can help protect against spurious or random associations that may be inadvertently discovered during data analysis in the absence of an a priori hypothesis. In the case of PPIs and COVID-19, we believe that there is sufficient biological plausibility based on the literature discussed in the Introduction section, although we recognize that biological plausibility does not imply biological certainty.
Next, it is worth considering the strength of association. Vaezi et al. (1) emphasized that an OR of 0.1–0.33 suggests “reduced risk,” an OR of 0.33–3 implies “potential bias” from residual confounders or other data anomalies, and an OR of 3 or greater implies “increased risk” and is considered a “zone of interest”. In this study, we found an aOR of 3.67 for use of twice daily PPIs, which falls within the “zone of interest.” By contrast, up to once daily use of PPIs was associated with an aOR of 2.15, which falls within the upper range of the “zone of potential bias.” On this criterion, it would seem that the risk of twice daily PPI should be more closely noted and that the once daily dose, although conferring a statistically higher odds of COVID-19 than nonuse, is of lower interest.
One must also consider whether there is a biological gradient, often manifesting as a dose-response relationship between the PPI and adverse event. Here, we find that twice daily PPI has a higher aOR than up to once daily PPI and that up to once daily PPI has a higher aOR than use of H2RA, following a stepwise biological gradient of gastric acid suppression.
Another criterion is consistency, meaning reproducibility of the findings among multiple analyses and studies. For the current study, the consistency criterion can be addressed in both general and specific forms. Generally, this study reveals a link between use of PPIs and acquiring an enteric pathogen. Of all the purported adverse events linked to PPIs, Vaezi et al. acknowledge that “consistency has been shown among various studies examining this association” based on the strength of meta-analyses and prospective, randomized data discussed earlier (1–6). Moreover, the pooled OR in meta-analysis is 3.33 (4), a value similar to the aOR of 3.67 for twice daily PPI found in this study, supporting consistency with the published literature. In addition, we found consistent results across subgroup analyses, such as across study time periods and when excluding certain subgroups, further supporting the durability of the findings. The specific form of consistency relates to the link between PPIs and SARS-CoV-2 as an instance of enteric infection risk. Here, there is currently very little published data because this study represents the first large effort, to our knowledge, evaluating the relationship. We are aware of other efforts underway to evaluate the link between PPI exposure and COVID-19 outcomes, including mortality, and await the results of those analyses. As with any hypothesis-generating observational study, the results may ultimately be supported by other work or not.
The temporality criterion refers to the timing between PPI exposure and onset of the adverse event. For example, if the event occurred before the exposure, then clearly there would be no causal link. Protopathic bias is a form of time bias in which a drug is used to manage the adverse event itself. In the case of COVID-19 and PPIs, one might imagine someone with COVID-19 developing GI symptoms and then turning to a PPI for relief. Failing to account for protopathic bias would artificially inflate the effect of PPIs. For that reason, individuals taking a PPI or H2RA for ≤1 month and who were diagnosed with COVID-19 at least 2 months before survey completion were classified as nonusers to help reduce the risk of protopathic bias. Another related form of bias is time lag between the expected effect of PPIs and the onset of the adverse effect. For example, it is possible that patients on long-term PPIs have a different gastric acid profile than those on short-term PPIs. For that reason, we compared results among those using PPIs for ≤6 months vs those using it for >6 months and found significant results for all analyses, with the highest odds seen for those on long-term twice daily PPI (aOR 3.81). However, despite these efforts to address protopathic bias and time lag, only a prospective study can generate sufficient data to satisfy the temporality criterion.
In short, we found preliminary evidence of an association between use of PPIs and COVID-19, most notably among those using twice daily PPIs. Evidence for association includes biological plausibility, the strength of effect of twice daily PPIs within the “zone of interest” noted by Vaezi et al., evidence of a dose-response biological gradient, consistency with other literature examining the link between PPIs and enteric infections, and partial evidence in support of temporality. However, this study does not offer evidence of causation in the absence of a prospective trial and should be further investigated in different populations and settings. In the meantime, our findings support good clinical practice that PPIs should only be used when indicated at the lowest effective dose, such as the approved once-daily label dosage of over-the-counter and prescription PPIs. Additional studies should also assess whether there is an association between PPIs and indicators of COVID-19 severity, such as hospitalization, need for intubation, or mortality.
CONFLICTS OF INTEREST
Guarantor of the article: Brennan M.R. Spiegel, MD, MSHS.
Specific author contributions: C.V.A.; W.D.C.; B.M.R.S.: substantial contributions to the conception and design of the work; acquisition, analysis, and interpretation of data for the work; drafting the work and revising it critically for important intellectual content; final approval of the version to be published.
Financial support: The data used in this analysis were derived from a larger study evaluating gastrointestinal symptoms in America funded by a grant from Ironwood Pharmaceuticals. In response to the COVID-19 pandemic and before launching the parent study, we added additional questions regarding self-reported COVID-19 testing and related symptoms. Separate funding was not received for the analyses presented in this report. The Cedars-Sinai Center for Outcomes Research and Education (CS-CORE) is supported by The Marc and Sheri Rapaport Fund for Digital Health Sciences & Precision Health. C.V.A. and B.M.R.S. are supported by a National Institutes of Health/National Center for Advancing Translational Science UCLA Clinical and Translational Science Institute (CTSI) grant (UL1TR001881).
Potential competing interests: C.V.A. has a stock option grant in My Total Health, has served on advisory boards for Bayer Healthcare and Synergy Pharmaceuticals, has served as a consultant for Alnylam Pharmaceuticals and Arena Pharmaceuticals, and received a one-time speaker's fee from Takeda Pharmaceuticals. After the paper was accepted for publication, C.V.A. served on an advisory board for Phathom Pharmaceuticals. W.D.C. has served as a consultant for Ironwood Pharmaceuticals, Phathom Pharmaceuticals, RedHill Biopharma Ltd., and Takeda Pharmaceuticals. B.M.R.S. has served on advisory boards for Allergan Inc, Alnylam Pharmaceuticals, Arena Pharmaceuticals, Ironwood Pharmaceuticals, Salix Pharmaceuticals, Synergy Pharmaceuticals, and Takeda Pharmaceuticals. B.M.R.S. served as a judge for a digital health competition held by Eli Lilly and Company, and has received research funding to his institution from Alnylam Pharmaceuticals, Ironwood Pharmaceuticals, Pfizer, Shire Pharmaceuticals, and Takeda Pharmaceuticals.
Study Highlights.
WHAT IS KNOWN
✓ Meta-analyses and randomized controlled trial data have shown that PPIs increase the risk for enteric infections, which is likely related to PPI-induced hypochlorhydria.
✓ Although the impact of acid suppression on SARS-CoV-2 is unknown thus far, pH ≤3 impairs the infectivity of the similar SARS-CoV-1.
✓ As SARS-CoV-2 is a proven enteropathic virus, it has been posited that PPIs might increase the risk for acquiring COVID-19.
WHAT IS NEW HERE
✓ In a nationwide survey, use of PPIs is associated with increased odds for reporting a positive COVID-19 test; the highest risk is seen among individuals taking PPIs twice daily.
✓ Use of H2RAs is not associated with an elevated risk for reporting COVID-19.
✓ These findings support good clinical practice that PPIs should only be used when indicated at the lowest effective dose, such as the approved once-daily label dosage of over-the-counter and prescription PPIs.
✓ Further studies examining the potential risk of PPIs and COVID-19, including clinical outcomes, should be conducted to further investigate this preliminary association.
Footnotes
SUPPLEMENTARY MATERIAL accompanies this paper at https://links.lww.com/AJG/B613, links.lww.com/AJG/B614, links.lww.com/AJG/B615
REFERENCES
- 1.Vaezi MF, Yang YX, Howden CW. Complications of proton pump inhibitor therapy. Gastroenterology 2017;153:35–48. [DOI] [PubMed] [Google Scholar]
- 2.Moayyedi P, Eikelboom JW, Bosch J, et al. Safety of proton pump inhibitors based on a large, multi-year, randomized trial of patients receiving rivaroxaban or aspirin. Gastroenterology 2019;157:682–91.e2. [DOI] [PubMed] [Google Scholar]
- 3.Bavishi C, Dupont HL. Systematic review: The use of proton pump inhibitors and increased susceptibility to enteric infection. Aliment Pharmacol Ther 2011;34:1269–81. [DOI] [PubMed] [Google Scholar]
- 4.Leonard J, Marshall JK, Moayyedi P. Systematic review of the risk of enteric infection in patients taking acid suppression. Am J Gastroenterol 2007;102:2047–56; quiz 2057. [DOI] [PubMed] [Google Scholar]
- 5.Lo WK, Chan WW. Proton pump inhibitor use and the risk of small intestinal bacterial overgrowth: A meta-analysis. Clin Gastroenterol Hepatol 2013;11:483–90. [DOI] [PubMed] [Google Scholar]
- 6.Vilcu AM, Sabatte L, Blanchon T, et al. Association between acute gastroenteritis and continuous use of proton pump inhibitors during winter periods of highest circulation of enteric viruses. JAMA Netw Open 2019;2:e1916205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kanno T, Matsuki T, Oka M, et al. Gastric acid reduction leads to an alteration in lower intestinal microflora. Biochem Biophys Res Commun 2009;381:666–70. [DOI] [PubMed] [Google Scholar]
- 8.Seto CT, Jeraldo P, Orenstein R, et al. Prolonged use of a proton pump inhibitor reduces microbial diversity: Implications for Clostridium difficile susceptibility. Microbiome 2014;2:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Darnell ME, Subbarao K, Feinstone SM, et al. Inactivation of the coronavirus that induces severe acute respiratory syndrome, SARS-CoV. J Virol Methods 2004;121:85–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xiao F, Tang M, Zheng X, et al. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology 2020;158:1831–3.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Trottein F, Sokol H. Potential causes and consequences of gastrointestinal disorders during a SARS-CoV-2 infection. Cell Rep 2020;32:107915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hamming I, Timens W, Bulthuis ML, et al. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol 2004;203:631–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lamers MM, Beumer J, van der Vaart J, et al. SARS-CoV-2 productively infects human gut enterocytes. Science 2020;369:50–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sultan S, Altayar O, Siddique SM, et al. AGA Institute rapid review of the GI and liver manifestations of COVID-19, meta-analysis of international data, and recommendations for the consultative management of patients with COVID-19. Gastroenterology 2020;159:320–34.e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xiao F, Sun J, Xu Y, et al. Infectious SARS-CoV-2 in feces of patient with severe COVID-19. Emerg Infect Dis 2020;26:1920–1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang W, Xu Y, Gao R, et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA 2020;323:1843–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cheung KS, Hung IFN, Chan PPY, et al. Gastrointestinal manifestations of SARS-CoV-2 infection and virus load in fecal samples from a Hong Kong cohort: Systematic review and meta-analysis. Gastroenterology 2020;159:81–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen L, Lou J, Bai Y, et al. COVID-19 disease with positive fecal and negative pharyngeal and sputum viral tests. Am J Gastroenterol 2020;115:790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Foladori P, Cutrupi F, Segata N, et al. SARS-CoV-2 from faeces to wastewater treatment: What do we know? A review. Sci Total Environ 2020;743:140444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nabi G, Siddique R, Khan S. Detecting viral outbreaks in future using enhanced environmental surveillance. Environ Res 2020;188:109731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Daughton CG. Wastewater surveillance for population-wide Covid-19: The present and future. Sci Total Environ 2020;736:139631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peccia J, Zulli A, Brackney DE, et al. SARS-CoV-2 RNA concentrations in primary municipal sewage sludge as a leading indicator of COVID-19 outbreak dynamics. medRxiv 2020. [Google Scholar]
- 23.Yeo C, Kaushal S, Yeo D. Enteric involvement of coronaviruses: Is faecal-oral transmission of SARS-CoV-2 possible? Lancet Gastroenterol Hepatol 2020;5:335–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wu Y, Guo C, Tang L, et al. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. Lancet Gastroenterol Hepatol 2020;5:434–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dhar D, Mohanty A. Gut microbiota and Covid-19- possible link and implications. Virus Res 2020;285:198018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhou J, Li C, Zhao G, et al. Human intestinal tract serves as an alternative infection route for Middle East Respiratory Syndrome coronavirus. Sci Adv 2017;3:eaao4966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Uno Y. Why does SARS-CoV-2 invade the gastrointestinal epithelium? Gastroenterology 2020. [Epub ahead of print April 10, 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Horner KJ. Hypothesis: Increased Risk of COVID-19 Infection with Proton Pump Inhibitor Use. (https://onedrive.live.com/?authkey=%21Ash2T9ZGcT7ozdw&cid=4D5E0A2E1FAED8C5&id=4D5E0A2E1FAED8C5%21574&parId=4D5E0A2E1FAED8C5%21252&o=OneUp) (2020). Accessed July 12, 2020. [Google Scholar]
- 29.Palsson OS, Whitehead WE, Van Tilburg MA, et al. Development and validation of the Rome IV diagnostic questionnaire for adults. Gastroenterology 2016;150:1481–91. [Google Scholar]
- 30.Parish SJ, Faubion SS, Weinberg M, et al. The MATE survey: Men's perceptions and attitudes towards menopause and their role in partners' menopausal transition. Menopause 2019;26:1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Robin SG, Keller C, Zwiener R, et al. Prevalence of pediatric functional gastrointestinal disorders utilizing the Rome IV criteria. J Pediatr 2018;195:134–9. [DOI] [PubMed] [Google Scholar]
- 32.Spiegel BM, Hays RD, Bolus R, et al. Development of the NIH Patient-Reported Outcomes Measurement Information System (PROMIS) gastrointestinal symptom scales. Am J Gastroenterol 2014;109:1804–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Van Tilburg MA, Hyman PE, Walker L, et al. Prevalence of functional gastrointestinal disorders in infants and toddlers. J Pediatr 2015;166:684–9. [DOI] [PubMed] [Google Scholar]
- 34.Wilkins CH, Mapes BM, Jerome RN, et al. Understanding what information is valued by research participants, and why. Health Aff 2019;38:399–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bryant C, Szejda K, Parekh N, et al. A survey of consumer perceptions of plant-based and clean meat in the USA, India, and China. Front Sustain Food Syst 2019;3:11. [Google Scholar]
- 36.Gliklich J, Maurer R, Bergmark RW. Patterns of texting and driving in a US national survey of millennial parents vs older parents. JAMA Pediatr 2019;173:689–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stephens SE, Foley KL, Miller D, et al. The effects of health disparities on perceptions about lung cancer screening (LCS): Survey results of a patient sample. Lung 2019;197:735–40. [DOI] [PubMed] [Google Scholar]
- 38.Azar KMJ, Shen Z, Romanelli RJ, et al. Disparities in outcomes among COVID-19 patients in a large health care system in California. Health Aff (Millwood) 2020;39:1253–62. [DOI] [PubMed] [Google Scholar]
- 39.Stelzig KE, Canepa-Escaro F, Schiliro M, et al. Estrogen regulates the expression of SARS-CoV-2 receptor ACE2 in differentiated airway epithelial cells. Am J Physiol Lung Cell Mol Physiol 2020;318:L1280–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vardavas CI, Nikitara K. COVID-19 and smoking: A systematic review of the evidence. Tob Induc Dis 2020;18:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wadhera RK, Wadhera P, Gaba P, et al. Variation in COVID-19 hospitalizations and deaths across New York City boroughs. JAMA 2020;323:2192–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Webb Hooper M, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA 2020. [Epub ahead of print May 11, 2020.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sood N, Simon P, Ebner P, et al. Seroprevalence of SARS-CoV-2-specific antibodies among adults in Los Angeles County, California, on April 10-11, 2020. JAMA 2020;323:2425–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Anyane-Yeboa A, Sato T, Sakuraba A. Racial disparities in COVID-19 deaths reveal harsh truths about structural inequality in America. J Intern Med 2020. [Epub ahead of print May 25, 2020.] [DOI] [PubMed] [Google Scholar]
- 45.COVID Tracking Project. Racial Data Dashboard. (https://covidtracking.com/race/dashboard) (2020). Accessed July 12, 2020. [Google Scholar]
- 46.Dahly D, Elia M, Johansen M. A Letter of Concern Regarding Increased Risk of COVID-19 Among Users of Proton Pump Inhibitors by Almario, Chey, and Spiegel. (https://zenodo.org/record/3940578) (2020). Accessed July 12, 2020. [Google Scholar]
- 47.Chey WD, Mody RR, Wu EQ, et al. Treatment patterns and symptom control in patients with GERD: US community-based survey. Curr Med Res Opin 2009;25:1869–78. [DOI] [PubMed] [Google Scholar]
- 48.Targownik LE, Metge C, Roos L, et al. The prevalence of and the clinical and demographic characteristics associated with high-intensity proton pump inhibitor use. Am J Gastroenterol 2007;102:942–50. [DOI] [PubMed] [Google Scholar]
- 49.Zhang H, Yang Z, Ni Z, et al. A meta-analysis and systematic review of the efficacy of twice daily PPIs versus once daily for treatment of gastroesophageal reflux disease. Gastroenterol Res Pract 2017;2017:9865963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Eid SM, Boueiz A, Paranji S, et al. Patterns and predictors of proton pump inhibitor overuse among academic and non-academic hospitalists. Intern Med 2010;49:2561–8. [DOI] [PubMed] [Google Scholar]
- 51.George CJ, Korc B, Ross JS. Appropriate proton pump inhibitor use among older adults: A retrospective chart review. Am J Geriatr Pharmacother 2008;6:249–54. [DOI] [PubMed] [Google Scholar]
- 52.Glew CM, Rentler RJ. Use of proton pump inhibitors and other acid suppressive medications in newly admitted nursing facility patients. J Am Med Dir Assoc 2007;8:607–9. [DOI] [PubMed] [Google Scholar]
- 53.Kelly OB, Dillane C, Patchett SE, et al. The inappropriate prescription of oral proton pump inhibitors in the hospital setting: A prospective cross-sectional study. Dig Dis Sci 2015;60:2280–6. [DOI] [PubMed] [Google Scholar]
- 54.Leri F, Ayzenberg M, Voyce SJ, et al. Four-year trends of inappropriate proton pump inhibitor use after hospital discharge. South Med J 2013;106:270–3. [DOI] [PubMed] [Google Scholar]
- 55.Metaxas ES, Bain KT. Review of proton pump inhibitor overuse in the US Veteran population. J Pharm Technol 2015;31:167–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Patterson Burdsall D, Flores HC, Krueger J, et al. Use of proton pump inhibitors with lack of diagnostic indications in 22 Midwestern US skilled nursing facilities. J Am Med Dir Assoc 2013;14:429–32. [DOI] [PubMed] [Google Scholar]
- 57.Inadomi JM, McIntyre L, Bernard L, et al. Step-down from multiple- to single-dose proton pump inhibitors (PPIs): A prospective study of patients with heartburn or acid regurgitation completely relieved with PPIs. Am J Gastroenterol 2003;98:1940–4. [DOI] [PubMed] [Google Scholar]
- 58.Inadomi JM, Jamal R, Murata GH, et al. Step-down management of gastroesophageal reflux disease. Gastroenterology 2001;121:1095–100. [DOI] [PubMed] [Google Scholar]
- 59.Menni C, Valdes AM, Freidin MB, et al. Real-time tracking of self-reported symptoms to predict potential COVID-19. Nat Med 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Covid Near You. (https://www.covidnearyou.org/us/en-US/) (2020). Accessed June 3, 2020. [Google Scholar]
- 61.Chang DW, Grotts J, Tseng CH, et al. Time trends in physician visits for gastroesophageal reflux disease before and after the Rx-to-OTC switch of proton pump inhibitors. J Clin Pharmacol 2017;57:452–8. [DOI] [PubMed] [Google Scholar]
- 62.Centers for Disease Control and Prevention. United States COVID-19 Cases and Deaths by State. (https://www.cdc.gov/covid-data-tracker/#cases) (2020). Accessed July 12, 2020. [Google Scholar]
- 63.Garg S, Kim L, Whitaker M, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019—COVID-NET, 14 States, March 1–30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:458–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pew Research Center. Facts on Latinos in the U.S. 2020. (https://www.pewresearch.org/hispanic/fact-sheet/latinos-in-the-u-s-fact-sheet/) (2020). Accessed July 12, 2020. [Google Scholar]
- 65.Bosman J, Mervosh S. As Virus Surges, Younger People Account for “Disturbing” Number of Cases. (https://www.nytimes.com/2020/06/25/us/coronavirus-cases-young-people.html) (2020). Accessed July 12, 2020. [Google Scholar]
- 66.Stokes EK, Zambrano LD, Anderson KN, et al. Coronavirus disease 2019 case surveillance - United States, January 22-May 30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:759–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Florida Health. Coronavirus: Summary of Persons Being Monitored, Persons under Investigation, and Cases. (http://ww11.doh.state.fl.us/comm/_partners/covid19_report_archive/state_reports_latest.pdf) (2020). Accessed July 12, 2020. [Google Scholar]
- 68.California Department of Public Health. Cases and Deaths Associated with COVID-19 by Age Group in California. (https://www.cdph.ca.gov/Programs/CID/DCDC/Pages/COVID-19/COVID-19-Cases-by-Age-Group.aspx) (2020). Accessed July 12, 2020. [Google Scholar]
- 69.Texas Department of State Health Services. Texas COVID-19 Data. (https://dshs.texas.gov/coronavirus/additionaldata.aspx) (2020). Accessed July 12, 2020. [Google Scholar]
- 70.Cint. Cint Quality Charter. (https://www.cint.com/quality) (2020). Accessed July 15, 2020. [Google Scholar]
- 71.Kochhar R. Hispanic Women, Immigrants, Young Adults, Those with Less Education Hit Hardest by COVID-19 Job Losses. (https://www.pewresearch.org/fact-tank/2020/06/09/hispanic-women-immigrants-young-adults-those-with-less-education-hit-hardest-by-covid-19-job-losses/) (2020). Accessed July 14, 2020. [Google Scholar]
- 72.Krogstad JM, Gozalez-Barrera A, Noe-Bustamante L. U.S. Latinos Among Hardest Hit by Pay Cuts, Job Losses Due to Coronavirus. (https://www.pewresearch.org/fact-tank/2020/04/03/u-s-latinos-among-hardest-hit-by-pay-cuts-job-losses-due-to-coronavirus/) (2020). Accessed July 14, 2020. [Google Scholar]
- 73.Pew Research Center. Internet Use Over Time. (http://www.pewinternet.org/data-trend/internet-use/internet-use-over-time/) (2020). Accessed May 31, 2020. [Google Scholar]


