Abstract
In order to harness the potential of digital health technologies to enhance the quality of clinical research, it is critical to first understand how to engage patients and research sites when planning and conducting digital health trials. To pave the way for the more effective use of digital health technologies in trials, the Clinical Trials Transformation Initiative has developed the first comprehensive, evidence-based set of recommendations for incorporating patient and site perspectives in digital health trials. While directed primarily at sponsors, these recommendations are expected to be valuable for all stakeholders including investigators.
Keywords: Digital health technology, Patient engagement, Mobile clinical trials, Digital trials, Hybrid trials, Site engagement, Site support, Mobile devices
Abbreviations: DHT, Digital Health Trials
1. Introduction
The ability of digital health technologies to increase efficiency and capture more meaningful data has the potential to transform the clinical research landscape [1]. The use of these technologies offers opportunities to reduce participant burden, streamline study operations, and collect previously unobtainable data that can help accelerate the discovery, development, and approval of new medical products. At the same time, it is critical to understand how to engage patients and research sites when planning and conducting digital health trials in order to optimize these opportunities of using digital health technologies in clinical research.
To pave the way for the more effective use of digital health technologies in trials, the Clinical Trials Transformation Initiative (CTTI) is presenting the first comprehensive, evidence-based set of recommendations for incorporating the perspectives of patients and sites in trials in which digital health technologies are used for data capture. These recommendations are designed to assist research sponsors in: (1) engaging patients and sites in planning clinical trials using digital health technology, (2) maximizing value and minimizing burden for study participants, and (3) addressing challenges for investigative sites. The complete set of recommendations and associated resources is available at the CTTI website at www.ctti-clinicaltrials.org/projects/engaging-patients-and-sites.
2. Methods
CTTI's Digital Health Trials (DHT) Program began in 2015 with the purpose of identifying and addressing the challenges of planning for and conducting clinical trials that use digital health technologies. This work focused on the use of digital health technologies for the collection of objective data (measured directly by the digital technology) in FDA-regulated clinical trials following participant consent. In performing this work, CTTI recognized that, while research had been done on patient preferences around mobile technologies in general [[2], [3], [4], [5]], little research had been conducted on their perspectives on the use of digital health technologies in clinical research, despite the fact that positive reception by these participants is critical to their widespread adoption in clinical research.
To address this gap, CTTI conducted a survey [6] of 193 potential research participants to better understand patients’ preferences, their willingness to use, and concerns with using digital health technology in clinical research [7]. It also conducted qualitative telephone interviews with 12 site investigators with experience in using digital health technologies in clinical trials [8]. CTTI then convened a two-day expert meeting with investigators, patient partners, regulators, sponsors, technology experts, and others to present findings and solicit additional input.
The following findings summarize the consensus-driven, multi-stakeholder recommendations that arose from the aforementioned work.
3. Findings
For digital health trials, patients are uniquely positioned to offer input on topics such as whether participants would find a particular device easy to learn, convenient to operate, and physically comfortable, in addition to providing feedback on other study design elements. Similarly, site personnel can best identify potential technology-related issues associated with site infrastructure, training, and technical support.
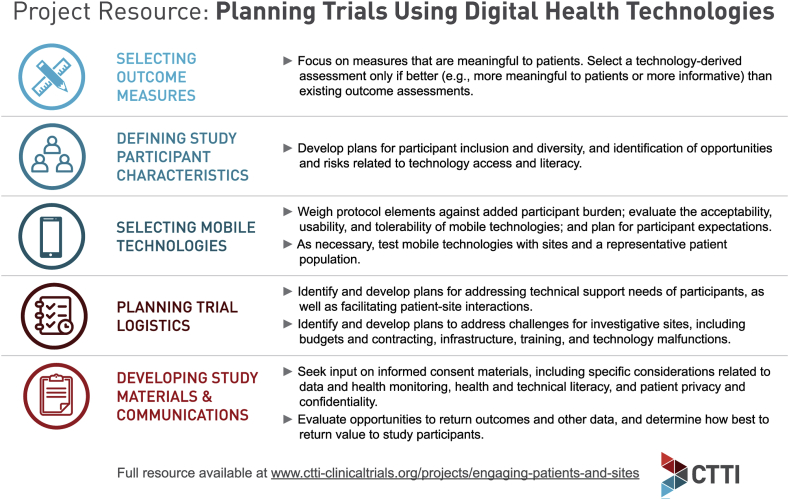
In order to obtain this valuable input, it is critical to seek diverse perspectives from patients and investigative site personnel early and often in planning trials using digital health technologies. As recommended in CTTI's work on Digital Health Technologies [9], outcome measurements that are meaningful to patients should be identified before deciding which (and whether) digital health technology should be used. If the use of digital health technology is determined to be appropriate for a trial, technology selection should be based on the requirements of the study and the needs of the intended user population. Furthermore, it is important to carefully weigh the impact of any technology-related protocol elements on site staff and clinical workflow against the potential benefits, and recognize that digital health technology cannot “fix” a trial that is fundamentally flawed. See Fig. 1 for more considerations for planning trials using digital health technologies.
Fig. 1.
Planning trials using digital health technologies.
When developing the protocol, it is also critical to consider the unique concerns pertaining to the use of digital health technologies from the perspectives of a variety of stakeholders, including regulators, site staff, investigators, and participants. The protocol should address safety signals not previously observed using traditional protocol design and monitoring, as well as data collected and observed by the study participant in the absence of context provided by clinicians [9].
Feasibility and/or pilot studies should also be conducted with sites and a representative patient population prior to trial launch. As a rule, the level of testing should be commensurate with the complexity and novelty of the technology to the research team. At the same time, it is important to recognize that even simple technologies present a number of potential problems related to their use, maintenance, and distribution that need to be carefully assessed.
While the use of digital health technologies in clinical trials offers important opportunities to provide value and reduce burden for participants, it may actually increase burden if risks, needs, and expectations are not considered during study planning and clearly communicated to participants during the enrollment process.
One critical point of communication is the informed consent document. This document should provide a thorough description of the selected digital health technology, including the benefits and risks associated with its use. It is important that the document provide clear guidance on what participants can expect―and what will be expected of them―during a digital health trial. Researchers should accommodate varying levels of participants’ health and technical literacy in the informed consent process and all subsequent communications.
It is also critical to recognize the potential for digital health technologies to change the way participants and site personnel interact during a trial. While some participants may be willing to primarily use forms of communication other than in-person visits, others may still prefer frequent face-to-face interaction [6]. Appropriate measures should be taken to ensure that all participants remain engaged.
Since site personnel can best understand participants’ issues and concerns in the context of the study, they should be the initial point of contact for technical support. If individuals other than site staff will be providing support, they should be made familiar with the study and trained on how to handle inappropriate data disclosures and participant queries.
Researchers should also be mindful of the expectations that participants may bring from their experiences with commercial digital technologies, and address these expectations up front. Participants may, for example, assume that their health is being monitored in real time and fail to call for help in the event of a medical emergency. Similarly, patients may expect real-time access to the data collected about them by digital health technologies; when sharing individual data would jeopardize trial integrity, expectations for what information will be shared, and when, should be clearly communicated during the informed consent process.
It is crucial for researchers to communicate to potential participants that, while every effort will be made to protect their data, confidentiality cannot be guaranteed. All stakeholders, including participants and institutional review boards (IRBs), have a right to fully understand the risks and implications of sharing data via digital health technologies.
The use of digital health technologies, while offering potential benefits to sites, also presents a number of site-specific challenges. Sponsors and sites should be prepared for the additional time needed to train staff and provide technical support, as well as costs for purchasing, storing, setting up, and handling the loss, malfunction, or return of devices. Sponsors should build flexibility into the study budget to account for unforeseen costs and provide any information gathered from pilot studies in advance to facilitate more accurate budgeting.
Sponsors should also clearly delineate the responsibilities of site personnel and consider alternate payment structures in contracts. In trials that rely on remote data collection, lump sum payments may be more feasible and fair than paying sites on a per-visit basis.
Finally, sponsors should ensure that sites have the appropriate infrastructure and training to conduct successful digital health trials. In addition to confirming that sites have the needed hardware, software, and Internet capabilities, sponsors should ensure they are recruiting staff with necessary technical expertise. Training should be offered in a variety of formats, provide the opportunity for hands-on practice, and allow ample time for establishing familiarity with the technology. To enhance efficiency, sponsors should recognize training already completed for other sponsors and customize training to address only those elements of a trial or technology that are new or unique.
4. Conclusion
Incorporating the insights and preferences of patients and sites is crucial to ensuring that all stakeholders derive benefit from clinical trials using digital health technologies and that costly mistakes are avoided. CTTI's recommendations and resources outline steps sponsors and researchers can take to harness the substantial opportunities offered by digital health technologies to advance clinical research and accelerate the development of new medical products.
Data availability
The complete set of recommendations and resources are made publicly available on the CTTI website at https://www.ctti-clinicaltrials.org/projects/engaging-patients-and-sites.
Funding
Funding for this manuscript was made possible, in part, by the U.S. Food and Drug Administration through grant R18FD005292. Views expressed by the authors do not necessarily reflect the official policies of the Department of Health and Human Services, nor does any mention of trade names, commercial practices, or organization imply endorsement by the United States Government. Partial funding was also provided by pooled membership fees and in-kind contributions from CTTI's member organizations.
Author contributions
All authors provided critical review and approval of the submitted version.
Declaration of competing interest
The authors have no conflicting interests to disclose.
Acknowledgements
The authors would like to thank Julia Vail, Duke Clinical Research Institute, for her drafting of the manuscript. The authors would also like to thank Amy Corneli and Brian Perry, Duke University, Department of Population Health Sciences, for their leadership of data collection activities informing development of the recommendations and resources. The authors wish to acknowledge the contributions of the entire Digital Health Trials Engaging Patients and Sites project team as noted on the CTTI project page, https://www.ctti-clinicaltrials.org/projects/engaging-patients-and-sites.
References
- 1.Marquis-Gravel G. Technology-enabled clinical trials: Transforming medical evidence generation. Circulation. 2019;140(17):1426–1436. doi: 10.1161/CIRCULATIONAHA.119.040798. [DOI] [PubMed] [Google Scholar]
- 2.Miller D.P. Usability of a novel mobile health iPad app by vulnerable populations. JMIR mHealth and uHealth. 2017;5(4):e43. doi: 10.2196/mhealth.7268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rai A. Understanding determinants of consumer mobile health usage intentions, assimilation, and channel preferences. J. Med. Internet Res. 2013;15(8):e149. doi: 10.2196/jmir.2635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zarghom S., Di Fonzo D., Leung F.H. Does socioeconomic status affect patients' ease of use of a touch-screen (iPad) patient survey? Interactive Journal of Medical Research. 2013;2(1):e1. doi: 10.2196/ijmr.2314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anderson K. Mobile health apps to facilitate self-care: a qualitative study of user experiences. PloS One. 2016;11(5) doi: 10.1371/journal.pone.0156164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clinical trials transformation initiative, survey questions, mobile in clinical trials: potential research participant perspectives. www.ctti-clinicaltrials.org/sites/www.ctti-clinicaltrials.org/files/mct_sp_survey_2017-7-6_.docx
- 7.Perry B. Patient preferences for using mobile technologies in clinical trials. Contemp. Clin. Trials Commun. 2019;15 doi: 10.1016/j.conctc.2019.100399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McKenna K.C. Investigator experiences using mobile technology in clinical research: a qualitative descriptive study. JMIR Preprints. 2020 doi: 10.2196/19242. https://preprints.jmir.org/preprint/19242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coran P. Advancing the use of mobile technologies in clinical trials: recommendations from the clinical trials transformation initiative. Digital Biomarkers. 2019;3:145–154. doi: 10.1159/000503957. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The complete set of recommendations and resources are made publicly available on the CTTI website at https://www.ctti-clinicaltrials.org/projects/engaging-patients-and-sites.