Abstract
Background
This study aimed to investigate the incidences of pre- and post-operative lower extremity deep venous thrombosis (DVT) in hospitalized patients with intertrochanteric fractures and to analyze the relevant risk factors.
Methods
A retrospective study was conducted between July 2014 and October 2016 in 218 intertrochanteric fracture patients who presented at Xi’an Honghui Hospital and underwent Doppler ultrasonography for DVT diagnosis. We divided DVT into distal, proximal, and mixed thrombosis. Patients were divided into either the thrombosis or no thrombosis group according to preoperative and postoperative ultrasonography results. All patients were evaluated for the risk factors associated with thrombosis.
Results
A total of 37.61% of preoperative patients had DVT, and the postoperative incidence increased to 58.72%. The days between fracture and hospitalization and the days between fracture and surgery were independent risk factors for preoperative DVT. The days between fracture and hospitalization and d-dimer levels at postoperative 1 day were independent risk factors of postoperative DVT. In total 23.4% of the patients progressed from having no thrombosis preoperatively to having distal, proximal, or mixed DVT postoperatively (22.02%, 0.46%, and 0.92%, respectively). Distal DVT constituted 86.59% and 90.63% of all preoperative and postoperative DVTs, respectively.
Conclusion
Intertrochanteric fracture is a common type of hip fracture in the elderly, and the incidence of DVT after intertrochanteric fracture may be underestimated. Early intervention (early admission and early surgery) might reduce the incidence of DVT.
Keywords: Deep vein thrombosis, Ultrasonography, Intertrochanteric fracture, Anticoagulation, Low molecular weight heparin
Background
Fractures of the proximal femur (commonly known as neck of femur or intertrochanteric fractures) are very common in the elderly population and carry significant morbidity and mortality. They occur mainly as osteoporotic or fragility fractures, but a small proportion may result from major trauma in a younger age group. Rapid aging of the population in China has led to a predicted increase in the incidence of hip fractures. Studies have reported that the number of hip fractures occurring worldwide each year will increase from 1.66 million in 1990 to 6.26 million in 2050, and half of these will be intertrochanteric fractures [1–3]. While the rate of hip fractures have been declining for women and to a lower extent for men, there will be a rise in the absolute number of hip fractures [4, 5]. DVT is a common complication in patients with intertrochanteric fractures that can lead to a potentially fatal pulmonary embolism (PE). In recent studies, the prevalence of DVT of the hip after trauma is reported to range from 11.1 to 29.4% [6–8]. Patients with intertrochanteric fractures often have other diseases and present in a poor physical condition. It is necessary to actively prevent DVT after admission. This study aimed to retrospectively analyze the data of patients with intertrochanteric fractures at Xi’an Honghui Hospital. The purpose was to investigate the incidences of DVT before and after surgery in inpatients with intertrochanteric fractures in both lower extremities, and to provide guidance on the clinical management to reduce the incidence of DVT.
Patients and Methods
Inclusion and Exclusion Criteria
The inclusion criteria were as follows: age ≥ 16 years; fresh intertrochanteric fractures that required surgical treatment; hospital stay of > 48 h; willing to undergo anticoagulant therapy to prevent thrombosis and submission of a signed informed consent form; and no bleeding risk. The exclusion criteria were as follows: intertrochanteric fractures with delayed treatment (> 3 weeks from injury to surgery); serious medical problems that make patients unsuitable for surgery; pathological fractures; poor compliance; and refusal to participate in the study.
Ethical Statement
The study was approved by the institutional review board of Xi’an JiaoTong University (2014026), and a signed informed consent form was obtained from each participant.
Methods
After admission, all patients were routinely assessed for thromboembolic risk using the risk assessment profile thromboembolism (RAPT) score [9]. For patients without anticoagulation contraindications, subcutaneous injection of low molecular weight heparin (LMWH) (0.4 mL, once a day; Glaxo Wellcome Production, GlaxoSmithKline, Tianjin, China,) to prevent DVT, and mechanical thrombo-prophylaxis (plantar venous pressure pump, 20 min, twice a day) was used. Blood samples were collected at the time of admission (2 h after admission), 1 day before surgery, and 1 and 5 days after surgery. The aim testing index included d-dimer, coagulation, and routine blood tests.
All patients received ultrasonography in both lower limbs 1 day before surgery and on days 3–5 after surgery. According to the ultrasonography results, patients were divided into the thrombosis or non-thrombosis group. If venous thrombosis presented in any anatomical part of both lower limbs, the patient was assigned to the thrombosis group. DVT was classified as proximal, distal, or mixed DVT [10]. A proximal DVT was defined as thrombosis at the level of the popliteal veins or above, including the femoral and iliac veins. Distal DVT was defined as thrombosis affecting the axial calf veins, including the calf muscle veins, fibular vein, and anterior/posterior tibial vein. Mixed DVT was defined as thrombosis in both proximal and distal regions. When ultrasonography results showed proximal or mixed thrombosis preoperatively, evaluation was performed by the department of vascular surgery and an inferior vena cava (IVC) filter was used to prevent fatal pulmonary embolism if needed. The anticoagulant therapy was discontinued 12 h before the surgery and resumed 24 h after the surgery. When the patients were discharged, the protocol was changed to rivaroxaban (prophylaxis dose 10 mg once daily and therapeutic dose 20 mg once daily; Bayer Pharma AG, Germany) until 35 days after operation [11].
Statistical Analysis
All analyses were performed using SPSS 19.0 (SPSS Inc., Chicago, IL, USA). The measurement data used Shapiro–Wilk test to determine whether the data were normally distributed, and mean ± SD was used to indicate the data that conformed to the normal distribution and the variance was uniform, independent sample t test was used. Non-normally distributed measurement data are expressed by the median and interquartile range M (Q1, Q3). The median is used to describe its central tendency, the interquartile range is used to describe its degree of dispersion, and the Mann–Whitney U test was used for analysis. The count data used χ2 test. Logistic regression modeling was used for identifying risk factors for DVT. P < 0.05 was considered statistically significant.
Results
Patient Characteristics
After applying the exclusion criteria, 218 patients with intertrochanteric fractures who were admitted to our hospital between July 2015 and October 2017 were included in this retrospective study. The patients’ mean (± SD) age was 76.03 (± 11.85) years (range 32–102 years). Of these patients, 133 (61.01%) were women and 85 (38.99%) were men. All patients underwent surgery, with 213 patients undergoing open reduction internal fixations (ORIFs), 4 undergoing hemiarthroplasty, and 1 undergoing external fixation. Of the 218 patients, there was no patient who underwent placement of an IVC filter before surgery. No fatal bleeding events were found in this study.
The Result of Preoperative Ultrasound
All patients underwent preoperative ultrasonography of the deep venous of the lower extremities. We found that 82 cases (37.61%) had thrombosis and 136 cases had no thrombosis (62.39%). Of the thrombosis patients, 71 (32.57%) were distal thrombosis, 3 (1.37%) were proximal thrombosis, and 8 (3.67%) were mixed thrombosis. Distal DVTs constituted 86.59% (71/82) of all DVTs (Table 1).
Table 1.
Patient characteristics according to preoperative ultrasound
| Thrombosis | No thrombosis | χ2/Z | P | |
|---|---|---|---|---|
| Number | 82 | 136 | ||
| Age | 77.54 ± 10.77 | 75.13 ± 12.40 | − 1.460 | > 0.05 |
| Gender | ||||
| Female | 52 | 81 | 0.320 | > 0.05 |
| Male | 30 | 55 | ||
| Unilateral or bilateral | ||||
| Left low limb | 47 | 75 | 0.098 | > 0.05 |
| Right low limb | 35 | 61 | ||
| Medical morbidity (%) | ||||
| Hypertension | 24 (29.27) | 47 (34.56) | 0.652 | > 0.05 |
| Diabetes | 8 (9.76) | 17 (12.5) | 0.379 | > 0.05 |
| Coronary heart disease | 31 (37.80) | 52 (38.23) | 0.004 | > 0.05 |
| Arrhythmia | 17 (20.73) | 17 (12.5) | 2.633 | > 0.05 |
| Stroke | 7 (8.53) | 18 (13.23) | 1.112 | > 0.05 |
| Associated trauma | 5 (6.10) | 10 (7.35) | 0.126 | > 0.05 |
| BMI [kg/m2, M (Q1, Q3)] | 22.0 (20.9, 24.2) | 22.0 (19.6, 24.3) | 0.481 | > 0.05 |
| Days between fracture and hospitalization [days, M (Q1, Q3)] | 0 (0, 2) | 0 (0, 1) | 1.624 | < 0.05 |
| Days between fracture and operation [days, M (Q1, Q3)] | 5 (4, 8) | 5 (3, 6) | 2.535 | < 0.05 |
| ASA classification | ||||
| 1 | 2 | 4 | 1.410 | > 0.05 |
| 2 | 53 | 79 | ||
| 3 | 27 | 52 | ||
| 4 | 0 | 1 | ||
| Serum markers [mg/L, M (Q1, Q3)] | ||||
| d-Dimer at admission | 12.1 (5.5, 17.8) | 11.5 (4.4, 25.0) | − 0.032 | > 0.05 |
| d-Dimer at preoperation | 6.9 (4.3, 10.9) | 4.2 (2.9, 6.1) | 3.501 | < 0.05 |
| CRP at admission | 5.1 (0.5, 16.0) | 1.5 (0.6, 11.8) | 0.698 | > 0.05 |
Univariate Analysis of Preoperative DVT
No statistically significant differences were observed in age, gender, unilateral or bilateral limb location, medical morbidity, body mass index (BMI), American society of anesthesiologists (ASA) classification, d-dimer at admission, or admission CRP between the two groups. However, d-dimer before surgery, the number of days between the fracture and hospitalization, and the number of days between the fracture and surgery were vital factors contributing to thrombosis, as shown in Table 1.
Multivariate Analysis of Preoperative DVT
We analyzed the days between the fracture and hospitalization and days between the fracture and surgery by multivariate analysis to identify risk factors. We found that days between the fracture and hospitalization (OR 1.109; 95% CI 1.003–1.225; p = 0.043) and days between the fracture and surgery (OR 1.090; 95% CI 1.007–1.180; p = 0.033) were independent risk factors of preoperative DVT (Table 2).
Table 2.
The contributing factors to preoperative DVT
| Factor | B | P | OR | 95% CI |
|---|---|---|---|---|
| Days between fracture and hospitalization | 0.103 | 0.043 | 1.109 | 1.003–1.225 |
| Days between fracture and operation | 0.086 | 0.033 | 1.090 | 1.007–1.180 |
| d-Dimer at preoperation | 0.043 | 0.331 | 1.044 | 0.989–1.101 |
The Result of Postoperative Ultrasound
All patients underwent ultrasonography of the deep venous of the lower extremities after surgery. We found that 128 cases (58.72%) had thrombosis, 90 cases had no thrombosis (41.28%). Of the thrombosis patients, 116 (53.21%) were distal thrombosis, 4 (1.83%) were proximal thrombosis, and 8 (3.68%) were mixed thrombosis. Distal DVTs constituted 90.63% (116/128) of all DVTs (Table 3).
Table 3.
Patient characteristics according to postoperative ultrasound
| Thrombosis | No thrombosis | χ2/Z | P | |
|---|---|---|---|---|
| Number | 128 | 90 | ||
| Age | 76.05 ± 11.56 | 76.00 ± 12.30 | − 0.033 | > 0.05 |
| Gender | ||||
| Female | 82 | 51 | 1.215 | > 0.05 |
| Male | 46 | 39 | ||
| Unilateral or bilateral | ||||
| Left low limb | 73 | 49 | 0.143 | > 0.05 |
| Right low limb | 55 | 41 | ||
| Medical morbidity (%) | ||||
| Hypertension | 42 (32.81) | 29 (32.22) | 0.008 | > 0.05 |
| Diabetes | 14 (10.94) | 11 (12.22) | 0.086 | > 0.05 |
| Coronary heart disease | 51 (39.84) | 32 (35.56) | 0.412 | > 0.05 |
| Arrhythmia | 21 (16.41) | 13 (14.44) | 0.154 | > 0.05 |
| Stroke | 13 (10.16) | 12 (13.33) | 0.525 | > 0.05 |
| Associated trauma | 9 (7.03) | 6 (6.67) | 0.011 | > 0.05 |
| BMI [kg/m2, M (Q1, Q3)] | 22.0 (20.8, 24.9) | 22.0 (20, 24.2) | 1.332 | > 0.05 |
| Length of hospital [days, M (Q1, Q3)] | 9 (7, 11) | 9 (7, 11) | 0.959 | > 0.05 |
| Days between fracture and hospitalization [days, M (Q1, Q3)] | 0(0, 1) | 0(0, 1) | 0.702 | < 0.05 |
| Days between fracture and operation [days, M (Q1, Q3)] | 5(4, 7) | 5(3, 6) | 2.200 | < 0.05 |
| ASA classification | ||||
| 1 | 4 | 2 | 3.933 | > 0.05 |
| 2 | 83 | 49 | ||
| 3 | 40 | 39 | ||
| 4 | 1 | 0 | ||
| Surgical procedures | ||||
| ORIF | 124 | 89 | 4.257 | > 0.05 |
| Hemiarthroplasty | 4 | 0 | ||
| EF | 0 | 1 | ||
| Duration of operation [min, M (Q1, Q3)] | 90 (70, 113.75) | 85 (65, 110) | 1.486 | > 0.05 |
| Transfusion [U, M (Q1, Q3)] | 2 (0, 2) | 2 (0, 2) | 0.975 | > 0.05 |
| Blood loss [mL, M (Q1, Q3)] | 200 (150, 400) | 200 (150, 300) | 1.292 | > 0.05 |
| Liquid transfusion [mL, M (Q1, Q3)] | 1600 (1100, 1600) | 1600 (1100, 1600) | − 0.753 | > 0.05 |
| Drainage [mL, M (Q1, Q3)] | 200 (100, 200) | 150 (100, 200) | 0.918 | > 0.05 |
| Serum markers [mg/L, M (Q1, Q3)] | ||||
| d-Dimer at admission | 12.1 (5.3, 20.5) | 11.5 (5.1, 21.5) | 0.195 | > 0.05 |
| d-Dimer at preoperation | 5.1 (3.5, 9.5) | 4.9 (3.3, 7.9) | 1.867 | > 0.05 |
| d-Dimer at postoperative 1 days | 7.4 (4.7, 15.1) | 6.4 (4.5, 11.7) | 2.883 | < 0.05 |
| d-Dimer at postoperative 5 days | 12.0 (6.1, 17.3) | 7.3 (5.9, 13.8) | 2.062 | < 0.05 |
| CRP at admission | 2.6 (0.5, 15.8) | 1.9 (0.6, 13.9) | − 0.062 | > 0.05 |
| CRP at postoperative 5 days | 8.6 (1.0, 56.8) | 1.4 (0.8, 39.1) | 2.505 | < 0.05 |
Univariate Analysis of Postoperative DVT
No statistically significant differences were observed in age, gender, unilateral or bilateral limb, medical morbidity, length of hospital stay, BMI, ASA, surgical procedures, surgery duration, transfusion, blood loss, liquid transfusion, drainage, d-dimer before surgery, d-dimer at admission, or admission CRP between the two groups. However, the number of days between the fracture and hospitalization, the number of days between the fracture and surgery, d-dimer levels at postoperative 1 day, d-dimer levels at postoperative 5 days, and CRP at postoperative 5 days were vital contributing factors to thrombosis, as shown in Table 3.
Multivariate Analysis of Postoperative DVT
We analyzed days between the fracture and hospitalization, days between the fracture and surgery, d-dimer levels prior to surgery, at postoperative 1 day, and postoperative 5 days, and CRP at postoperative 5 days by multivariate analysis to identify risk factors. We found that days between fracture and hospitalization (OR 1.137; 95% CI 1.002–1.290; p = 0.047) and d-dimer levels at postoperative 1 day (OR 1.087; 95% CI 1.033–1.142; p = 0.001) were independent risk factors of postoperative DVT (Table 4).
Table 4.
The contributing factors to postoperative DVT
| Factor | B | P | OR | 95% CI |
|---|---|---|---|---|
| Days between fracture and hospitalization | 0.128 | 0.047 | 1.137 | 1.002–1.290 |
| Days between fracture and operation | 0.087 | 0.052 | 1.091 | 0.999–1.191 |
| d-Dimer at postoperative 1 day | 0.083 | 0.001 | 1.087 | 1.033–1.142 |
| d-Dimer at postoperative 5 days | 0.107 | 0.126 | 1.155 | 0.926–1.031 |
| CRP at postoperative 5 days | 0.012 | 0.054 | 1.012 | 1.000–1.025 |
Dynamic Changes of DVT and the Location in Lower Extremities Before and After Operation
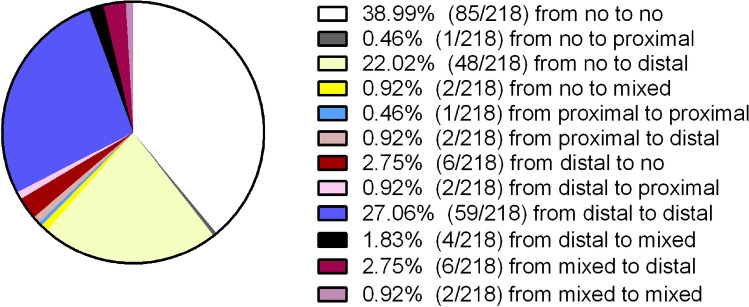
The dynamic changes of DVT before and after surgery are shown in Fig. 1. As the figure shows, 38.99% of patients had no thrombosis during the duration of hospitalization. In addition, 23.4% of the patients progressed from having no thrombosis preoperatively to having distal, proximal, or mixed DVT postoperatively (22.02%, 0.46%, and 0.92%, respectively). In total, 2.75% of the patients who had preoperative distal DVT no longer had thrombosis postoperatively.
Fig. 1.
Dynamic changes in DVT before and after operation
The locations of DVT in the lower extremities before and after surgery are shown in Table 5. Before surgery, 53 patients had single injured lower extremity DVT and 14 had DVT in both lower extremities. In addition, 15 had DVT in the uninjured side. In all patients after surgery, 69 had single injured lower extremity DVT and 46 had DVT in both lower extremities. In addition, 13 had DVT in the uninjured side.
Table 5.
The location of DVT in lower extremities before and after operation
| Case(s) | The location of DVT | |||
|---|---|---|---|---|
| DVTs occurred on the injured side | DVTs occurred on the uninjured side | DVT in both lower extremities | ||
| Preoperative | 82 | 53 (64.63%) | 15 (18.29%) | 14 (17.08%) |
| Postoperative | 128 | 69 (53.90%) | 13 (10.16%) | 46 (35.94%) |
Discussion
The results of this study are as follows: (1) of preoperative patients, 37.61% had DVT, and the postoperative incidence increased to 58.72%, (2) the days between fracture and hospitalization and the days between fracture and surgery have been shown to be independent risk factors of preoperative DVT, (3) the days between fracture and hospitalization and d-dimer at postoperative 1 day were shown to be independent risk factors of postoperative DVT, 4) of the thrombosis patients, 23.4% of the patients progressed from having no thrombosis preoperatively to having distal, proximal, or mixed DVT (22.02%, 0.46%, and 0.92%, respectively) postoperatively, and 5) distal DVT constituted 86.59% and 90.63% of all preoperative and postoperative DVTs, respectively.
Many factors, including the trauma of the initial injury and subsequent surgery, blood loss secondary to fracture and again at surgery, and fluid resuscitation before and after surgery, may contribute to the hypercoagulability state [12]. Intertrochanteric fractures may result in a large amount of blood being lost (up to 1 L) [13]. This is a boosting thrombosis factor, and may be the main contributing factor to this phenomenon (from 37.61% of preoperative patients to 58.72% of postoperative patients). More attention should be paid to the incidence of thrombosis after surgery. Asymptomatic patients with DVT were therefore identified, raising the observed rate when compared to studies where only symptomatic patients were identified. In addition, this population of patients (elderly, intertrochanteric fracture) represents a particularly high-risk group of patients for the development of DVT.
In previous studies, there have been many factors reported to contribute to the formation of thrombosis after trauma, including age, gender, fracture, surgery, duration of hospital stay, past history of DVT, varicose veins, high-energy injury, and immobilization [14–18]. We found the days between fracture and hospitalization to be an independent risk factor of pre- and postoperative DVT and days between the fracture and surgery to be an independent risk factor of preoperative DVT. These results are similar to those of previous studies [19–21]. The results suggest that there is a substantial risk of venous thromboembolic disease in patients who have an intertrochanteric fracture, and this risk increases if the time of admission or surgery is delayed. Smith et al. [20] reported that the increase in the incidence of DVT development was 14.5% if surgery was delayed > 1 day to 33.3% if surgery was delayed > 7 days. A delay may result from preoperative medical evaluation or from a transfer from community hospitals to our hospital. According to the guideline from Scottish Intercollegiate Guideline Network (SIGN), surgery should be performed on patients with hip fractures as soon as possible, and the duration of pain and dependence should be reduced. Intertrochanteric fracture patients should be admitted as soon as possible after the injury, and receive early anticoagulant therapy and surgery.
Previous reports have suggested that d-dimer levels correlate with thrombosis [22–26], in line with the findings of this study. However, another study suggested that there was no role for d-dimer levels in the prediction of venous thromboembolism (VTE) in trauma patients [27]. Crowther et al. [28] reported that, in critically ill patients, d-dimer levels do not predict patients at risk of DVT and they should not be used to guide diagnostic testing for DVT. d-Dimer levels naturally increase with age and the specificity of d-dimer testing for VTE is therefore lower in older people [29]. A negative d-dimer result indicates the absence of DVT [30]. The variability of timing of d-dimer measurement, the diagnostic modalities of DVT, and patients with or without chemical anticoagulant prescriptions may result in the differing conclusions. Some studies have reported that anticoagulant drugs can affect the diagnostic sensitivity of d-dimer levels. All patients in this study were treated with anticoagulant drugs after admission, which is the reason for their reduced sensitivity [31, 32]. The value of d-dimer levels in predicting the significance of DVT is still controversial, and further research is needed.
With the promotion of the American College of Chest Physicians evidence-based clinical practice guidelines and the extensive application of thromboprophylaxis agents, the incidence of proximal DVT has decreased significantly in patients undergoing hip fracture surgery [33]. In this study, it was observed that cases of proximal DVT were rare and cases with calf muscular vein thrombosis (CMVT) were often noted. Furthermore, distal DVTs constituted 86.59% of all preoperative DVTs, and 90.63% of postoperative DVTs. Of the patients, there were 52 new postoperative DVTs, 49 of which were distal DVTs, primarily CMVT. After intertrochanteric fracture, because of pain and staying in bed, stagnation of blood occurs in the relaxed calf muscle veins; therefore, CMVT develops more commonly in senile patients with fractures [34, 35]. A study reported that 16.3% of the CMVT extended to the level of the adjacent tibial or peroneal veins, or higher but only 2.9% of all CMVT progressed to the level of the popliteal veins [36]. Calf muscle contractions compress the muscular veins and promote venous flow. Boutitie et al. [37] reported that LMWH combined with a plantar venous pump can significantly reduce the incidence of thrombosis. In this study, only 2.75% distal DVT extended to the level above the popliteal veins, and no PEs occurred.
There were a few limitations to this study. First, this was a retrospective study, and as we eliminated the incomplete data, the authenticity of the results needs to be evaluated. Nevertheless, owing to the large sample size, the effect might be insignificant. Second, although ultrasonography is not the gold standard for diagnosing DVT, and the operating skills of different sonographers vary, our study was conducted by senior sonographers, which minimizes the impact on outcomes.
Conclusion
The incidence of DVT after intertrochanteric fracture may be underestimated. Early intervention (early admission and early surgery) might reduce the incidence of DVT.
Acknowledgements
We thank all the authors who contributed to this article. There was no conflict of interest by any of the authors including financial and personal relationships with other people or organizations that inappropriately influenced this study.
Abbreviations
- ASA
American Society of Anesthesiologists
- BMI
Body mass index
- CRP
C-reactive protein
- CMVT
Calf muscular vein thrombosis
- DVT
Deep vein thrombosis
- EF
External fixation
- LMWH
Low molecular weight heparin
- ORIF
Open reduction internal fixation
- PE
Pulmonary embolism
- VTE
Venous thromboembolism
Author contributions
CF and B-F Z designed the study, analyzed the data, and wrote the manuscript. P-F W, S-W Q, and KS, KY, ZL collected the data and participated in the design of the study. YZ and KZ analyzed the data and helped in writing the manuscript. All authors have read and approved the final manuscript.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and publication of this article: this work was supported by the Social Development Foundation of Shaanxi Province [Grant number 2017ZDXM-SF-009].
Availability of data and material
The datasets generated and/or analyzed during the current study are not publicly available due to data privacy but are available from the corresponding author on reasonable request.
Compliance with Ethical Standards
Conflict of interest
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article. The manuscript has been read and approved by all the authors.
Ethics approval and consent to participate
The study was approved by the institutional review board of Xi’an JiaoTong University (2014026), and a signed informed consent form was obtained from each participant.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Chen Fei, Email: 18729553305@163.com.
Peng-Fei Wang, Email: pengfei_wang@163.com.
Shuang-Wei Qu, Email: qushuangwei0920@126.com.
Kun Shang, Email: zj322mh39@163.com.
Kun Yang, Email: 18829072152@163.com.
Zhi Li, Email: xayxylz@163.com.
Yan Zhuang, Email: zhuangyan2512@126.com.
Bin-Fei Zhang, Email: zhangbf07@gmail.com.
Kun Zhang, Email: hhzhangkun@163.com.
References
- 1.Cooper C, Campion G. Hip fractures in the elderly: A world-wide projection. Osteoporosis International. 1992;2:285–289. doi: 10.1007/BF01623184. [DOI] [PubMed] [Google Scholar]
- 2.Kovar FM, Endler G, Wagner OF, Jaindl M. Basal haemoglobin levels as prognostic factor for early death in elderly patients with a hip fracture—a twenty year observation study. Injury-international Journal of the Care of the Injured. 2015;46:1018–1022. doi: 10.1016/j.injury.2015.01.010. [DOI] [PubMed] [Google Scholar]
- 3.Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporosis International. 1997;7:407–413. doi: 10.1007/PL00004148. [DOI] [PubMed] [Google Scholar]
- 4.Hopkins RB, Pullenayegum E, Goeree R, et al. Estimation of the lifetime risk of hip fracture for women and men in Canada. Osteoporosis International. 2012;23:921–927. doi: 10.1007/s00198-011-1652-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brauer CA, Cocaperraillon MM, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302:1573–1579. doi: 10.1001/jama.2009.1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shin WC, Woo SH, Lee SJ, et al. Preoperative prevalence of and risk factors for venous thromboembolism in patients with a hip fracture: An indirect multidetector CT venography study. Journal of Bone and Joint Surgery-american. 2016;98:2089–2095. doi: 10.2106/JBJS.15.01329. [DOI] [PubMed] [Google Scholar]
- 7.Song K, Yao Y, Rong Z, et al. The preoperative incidence of deep vein thrombosis (DVT) and its correlation with postoperative DVT in patients undergoing elective surgery for femoral neck fractures. Archives of Orthopaedic and Trauma Surgery. 2016;136:1459–1464. doi: 10.1007/s00402-016-2535-4. [DOI] [PubMed] [Google Scholar]
- 8.Luksameearunothai K, Sangasoongsong P, Kulachote N, et al. Usefulness of clinical predictors for preoperative screening of deep vein thrombosis in hip fractures. Bmc Musculoskeletal Disorders. 2017;18:208. doi: 10.1186/s12891-017-1582-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greenfield LJ, Proctor MC, Rodriguez JL, et al. Posttrauma thromboembolism prophylaxis. Journal of Trauma and Acute Care Surgery. 1997;42:100–103. doi: 10.1097/00005373-199701000-00017. [DOI] [PubMed] [Google Scholar]
- 10.Wang CJ, Lu H, Lee K, et al. Deep-vein thrombosis rates after major orthopedic surgery in Asia. An epidemiological study based on postoperative screening with centrally adjudicated bilateral venography. Journal of thrombosis and haemostasis: JTH. 2005;3:2664–2670. doi: 10.1111/j.1538-7836.2005.01236.x. [DOI] [PubMed] [Google Scholar]
- 11.Schulman S, Witt DM, Vandvik PO, et al. Evidence-based management of anticoagulant therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141:e152S–e184. doi: 10.1378/chest.11-2295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wilson D, Cooke EA, McNally MA, et al. Changes in coagulability as measured by thromboelastography following surgery for proximal femoral fracture. Injury-international Journal of the Care of the Injured. 2001;32:765–770. doi: 10.1016/S0020-1383(01)00139-5. [DOI] [PubMed] [Google Scholar]
- 13.Parker M, Johansen A. Hip fracture. BMJ British Medical Journal. 2006;333:27–30. doi: 10.1136/bmj.333.7557.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Park MS, Perkins SE, Spears GM, et al. Risk factors for venous thromboembolism after acute trauma: A population-based case-cohort study. Thrombosis Research. 2016;144:40–45. doi: 10.1016/j.thromres.2016.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sharma SK, Gupta V, Kadhiravan T, et al. A prospective study of risk factor profile & incidence of deep venous thrombosis among medically-ill hospitalized patients at a tertiary care hospital in northern India. Indian Journal of Medical Research. 2009;130:726. [PubMed] [Google Scholar]
- 16.Jang JH, Park KY, Moon NH. High energy injury is a risk factor for preoperative venous thromboembolism in the patients with hip fractures: A prospective observational study. Injury. 2018;49:1155–1161. doi: 10.1016/j.injury.2018.04.026. [DOI] [PubMed] [Google Scholar]
- 17.Woo SH, Lee SJ, Lee JS, et al. Preoperative prevalence of and risk factors for venous thromboembolism in patients with a hip fracture: An indirect multidetector CT venography study. The Journal of bone and joint surgery American. 2016;98:2089–2095. doi: 10.2106/JBJS.15.01329. [DOI] [PubMed] [Google Scholar]
- 18.National Clinical Guideline Centre-A, Chronic C Venous thromboembolism: Reducing the risk of venous thromboembolism (deep vein thrombosis and pulmonary embolism) in patients admitted to hospital. BMJ. 2010;334:1053–1054. [Google Scholar]
- 19.Zahn HR, Skinner JA, Porteous MJ. The preoperative prevalence of deep vein thrombosis in patients with femoral neck fractures and delayed operation. Injury-International Journal of the Care of the Injured. 1999;30:605–607. doi: 10.1016/S0020-1383(99)00163-1. [DOI] [PubMed] [Google Scholar]
- 20.Smith EB, Javad P, Purtill JJ. Delayed surgery for patients with femur and hip fractures-risk of deep venous thrombosis. Journal of Trauma and Acute Care Surgery. 2011;70:113–116. doi: 10.1097/TA.0b013e31821b8768. [DOI] [PubMed] [Google Scholar]
- 21.Hefley FG, Nelson CL, Puskarich-May CL. Effect of delayed admission to the hospital on the preoperative prevalence of deep-vein thrombosis associated with fractures about the hip. Journal of Bone and Joint Surgery American. 1996;78:581–583. doi: 10.2106/00004623-199604000-00012. [DOI] [PubMed] [Google Scholar]
- 22.Schmidt U, Enderson BL, Chen JP, Maull KI. d-Dimer levels correlate with pathologic thrombosis in trauma patients. Journal of Trauma and Acute Care Surgery. 1992;33:312–319. doi: 10.1097/00005373-199208000-00023. [DOI] [PubMed] [Google Scholar]
- 23.Yao Y, Rong Z, Shen Y, et al. The preoperative incidence of deep vein thrombosis (DVT) and its correlation with postoperative DVT in patients undergoing elective surgery for femoral neck fractures. Archives of Orthopaedic and Trauma Surgery. 2016;136:1459–1464. doi: 10.1007/s00402-015-2337-0. [DOI] [PubMed] [Google Scholar]
- 24.Squizzato A, Rutjes AW, Büller HR, et al. Diagnostic accuracy of d-dimer test for exclusion of venous thromboembolism: a systematic review. Journal of Thrombosis and Haemostasis: JTH. 2007;5:296–304. doi: 10.1111/j.1538-7836.2007.tb03082.x. [DOI] [PubMed] [Google Scholar]
- 25.Palareti G, Aguilar C, Legnani C, et al. A multicenter evaluation of a new quantitative highly sensitive d-dimer assay for exclusion of venous thromboembolism. Thrombosis and haemostasis. 2008;100:505–512. doi: 10.1160/TH08-04-0202. [DOI] [PubMed] [Google Scholar]
- 26.Shi D, Zhang C, Chen D, et al. Postoperative plasma d-dimer value for predicting deep venous thrombosis following hip arthroplasty with nadroparin prophylaxis. Hip International: the Journal of Clinical and Experimental Research on Hip Pathology and Therapy. 2013;23:411–416. doi: 10.5301/hipint.5000039. [DOI] [PubMed] [Google Scholar]
- 27.Selby R, Geerts Wofosu FA. Hypercoagulability after trauma: Hemostatic changes and relationship to venous thromboembolism. Thrombosis Research. 2009;124:281–287. doi: 10.1016/j.thromres.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 28.Crowther MA, Cook DJ, Griffith LE, et al. Neither baseline tests of molecular hypercoagulability nor d-dimer levels predict deep venous thrombosis in critically ill medical-surgical patients. Intensive Care Medicine. 2005;31:48. doi: 10.1007/s00134-004-2467-2. [DOI] [PubMed] [Google Scholar]
- 29.Kraaijpoel N, Le Gal G, Wells PS. Venous thromboembolism: Advances in diagnosis and treatment. JAMA. 2018;320:1583–1594. doi: 10.1001/jama.2018.14346. [DOI] [PubMed] [Google Scholar]
- 30.Jiang Y, Li J, Liu Y, et al. Risk factors for deep vein thrombosis after orthopedic surgery and the diagnostic value of d-dimer. Annals of Vascular Surgery. 2015;29:675–681. doi: 10.1016/j.avsg.2014.12.022. [DOI] [PubMed] [Google Scholar]
- 31.Tan M, Re VRC. Diagnostic management of clinically suspected acute deep vein thrombosis. British Journal of Haematology. 2010;146:347–360. doi: 10.1111/j.1365-2141.2009.07732.x. [DOI] [PubMed] [Google Scholar]
- 32.Sudo A, Niimi R, Hasegawa M, Shi DQ. The influence of fondaparinux on the diagnosis of postoperative deep vein thrombosis by soluble fibrin and d-dimer. Thrombosis Research. 2012;130:759–764. doi: 10.1016/j.thromres.2011.11.046. [DOI] [PubMed] [Google Scholar]
- 33.Kearon C, Akl EA, Comerota AJ, et al. Antithrombotic therapy for VTE disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141:e278S. doi: 10.1378/chest.11-2301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cotton LT, Clark C. Symposium on thrombosis: Anatomical localization of venous thrombosis. Annals of the Royal College of Surgeons of England. 1965;36:214. [PMC free article] [PubMed] [Google Scholar]
- 35.Su H, Liu H, Liu J, Wang X. Elderly patients with intertrochanteric fractures after intramedullary fixation : analysis of risk factors for calf muscular vein thrombosis. Orthopade. 2018;47:341–346. doi: 10.1007/s00132-018-3552-5. [DOI] [PubMed] [Google Scholar]
- 36.Macdonald PS, Kahn SR, Miller N, Obrand D. Short-term natural history of isolated gastrocnemius and soleal vein thrombosis. Journal of Vascular Surgery. 2003;37:523–527. doi: 10.1067/mva.2003.149. [DOI] [PubMed] [Google Scholar]
- 37.Boutitie F, Pinede L, Schulman S, et al. Influence of preceding length of anticoagulant treatment and initial presentation of venous thromboembolism on risk of recurrence after stopping treatment: Analysis of individual participants’ data from seven trials. BMJ British Medical Journal. 2011;342:1296. doi: 10.1136/bmj.d3036. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due to data privacy but are available from the corresponding author on reasonable request.