Abstract
Background
The primary objective of this study was to evaluate the quality of life following limb lengthening surgery in patients with achondroplasia. The complications and different lengthening techniques have and effects on mid-term results were also investigated.
Methods
We performed a retrospective, multicenter study by evaluating the records of patients with achondroplasia operated in our clinic between 1999 and 2014 for limb lengthening with a minimum follow-up of 3 years. Forty nine patients were underwent bilateral lower limb lengthening surgery and 21 of 49 patients underwent bilateral humerus lengthening surgery. Patients were evaluated by the Pediatric Quality of Life Inventory (PedsQL) 4.0 Generic Core Scales to assess the health-related quality of life (HRQOL) of children. Twenty patients with achondroplasia who had no lengthening surgery history were also evaluated with the PedsQL score as the control group.
Results
The average age at the time of first surgery was 6.17 years. The average follow-up period was 100.2 months. The average age at the time of study 14.70 ± 2.44 (11–18) years. There were significant differences between the patients with humeral lengthening and patients who did not undergo humeral lengthening in all scores. Transient complications had minimal effects on scores. Although all scores in the operated group were higher than non-operated patients with achondroplasia, there were no significant differences.
Conclusion
Quality of life was significantly improved as a result of humerus lengthening surgery of patients with achondroplasia, despite minor complications compared with Lower limb lengthening surgery.
Level of Evidence
Level III, case control study.
Keywords: Congenital short extremity, Lengthening rhythm, Congenital femoral deficiency, Congenital tibia pseudarthrosis, Quality of callus
Introduction
Patients with achondroplasia have physical and psychological limitations owing to the disproportionate stature of the body and difficulty in making routine activities of daily life such as perianal-perineal hygiene and decreased walking distance [1, 2]. Limb lengthening surgery is usually required for both the upper and lower limbs of these patients [1–3]. According to the literature, 85% of these patients were satisfied with their improved physical and psychological status as a result of the lengthening surgery [3].
There are many tests for assessing the quality of life outcomes for children and adolescents. The Pediatric Quality of Life Inventory (PedsQL) is considered one of the most promising health-related quality of life (HRQOL) instruments for children and adolescents, integrating generic core scales and disease-specific modules into one measurement system [4]. The main purpose of this study was to compare the patients with achondroplasia who underwent limb lengthening surgery and had no lengthening surgery history via the PedsQL 4.0 to evaluate the HRQOL. The complications and different lengthening techniques have and effects on mid-term results were also investigated. We hypothesize that limb lengthening surgery has a favorable effect on the quality of life in patients with achondroplasia despite minor complications and different lengthening techniques.
Material and Methods
Demographic Data of the Patients
Institutional Review Board (IRB) approval was obtained for this study. This retrospective study was performed in single center at Istanbul University Faculty of Medicine Department of Orthopedics and Traumatology clinic. Records of 64 patients with diagnosed achondroplasia underwent limb lengthening surgery in our institution between 1999 and 2014 were retrospectively reviewed. All information about the study was explained by a child psychiatrist to the parents and children and parental informed consent and child assent to participate were obtained.
Inclusion criteria were patients diagnosed with achondroplasia, operated with external fixator, minimum 3 years follow-up, bilateral femur and tibial lengthening, available demographics, and medical records.
Exclusion criteria were patients operated with intramedullary nailing, only tibial or femur lengthening, patients or parents not accept a participant for this study.
49 patients (29 female, 20 male) were included in this study who have suitable the above criteria. Patients with bilateral lengthening of the femur and tibia at the same time were named as simultaneous bilateral lengthening. Patients with bilateral lengthening of the femur and then bilateral tibia lengthening in other sections or vice versa, at a different time was named as consecutively bilateral lengthening. Twenty patients with achondroplasia who had no lengthening surgery history were also evaluated as the control group who regularly follow-up in our pediatric endocrinology department.
Humeral lengthening was performed in patients with no ability to perform personal hygiene and perineal care. We determined the extent of humeral lengthening with the ability to enable the patient to reach the perineum for the goal of personal hygiene.
All patients were divided into subgroups which described in Table 1. Thirty patients had complication in lower extremity lengthening and ten patients in upper extremity lengthening.
Table 1.
The main subgroups of patients with limb lengthening
| Bilateral humeral lengthening | No humeral lengthening | Total | |
|---|---|---|---|
| Simultaneous bilateral lengthening (n) | 12 | 14 | 26 |
| Consecutively bilateral lengthening (n) | 9 | 14 | 23 |
| Total (n) | 21 | 28 |
The average age at the first time of surgery was 6.17 ± 2.70 (3–13) years for lower extremity and 10.2 ± 3.1 (6–15) for humeral lengthening. The mean follow-up was 100.20 ± 41.15 (37–197) months. The average age at the time of study 14.70 ± 2.44 (11–18) years. The mean external fixation time was 8.1 (5–13) months for the femur, 8.6 (5–13) months for the tibia and 6.5 (4–9) months for the humerus. The average age of non-operated patients was 15.7 (13–18) years. There was no significant difference between the ages of the two groups at time of study (p: 071).
The mean amount of femoral lengthening was 7.4 (6–11) cm and the mean amount of tibial lengthening was 7.1 (6–10) cm, lower limb total lengthening was 14.5 (12–20) cm. The mean amount of humeral lengthening was 7.7 (6.5–10) cm (Table 2). The mean lengthening ratio for the original segment was 43.1% in the femur (range 23.3–75.0%), 53.6% in the tibiae (range 24.7–98.0%) and 62% (40–96%) in the humerus.
Table 2.
Demographic data of all patients’ results
| Mean | S.D. | Min–max | |
|---|---|---|---|
| Age | 6.17 | 2.7 | 3–13 |
| Follow-up/months | 100.2 | 41.15 | 37–197 |
| Femur; length (cm) | 7.4 | 1.50 | 6–11 |
| Fixator Time (months) | 8.1 | 2.18 | 5–13 |
| Tibia; Length (cm) | 7.1 | 1.92 | 6–10 |
| Fixator time (months) | 8.6 | 2.31 | 5–13 |
| Humerus; length (cm) | 7.7 | 0.84 | 6–10 |
| Fixator time (months) | 6.5 | 1.39 | 4–9 |
The mean external- fixator index (EFI) was 33.4 days/cm for the femur (range 16.2–45.3 days/cm), 36.1 days/cm for the tibia (range 18.9–63.5 days/cm) and 24.7 day/cm (17.1–34.9 days/cm).
Operation and Follow-up Procedure
Ilizarov, classical-type (Tasarım Med, Istanbul, Turkey) or hexapod-type (Smart Correction; Gotham Medical LLC, Fort Lee, NJ, USA) circular external fixators were used for tibial lengthening with Gigli osteotomy technique which was preferred for proximal metaphyseal osteotomy. Orthofix LRS (OrtofixSrl., Bussolengo Verona, Italy) mono lateral fixators were used for femoral lengthening and multiple drill technique was preferred for distal diaphysometaphyseal femoral osteotomy. Monorail external fixators (Tasarım Med, Istanbul, Turkey) were used for humeral lengthening and osteotomy of the mid diaphysis is performed using a multiple drill-hole technique (Figs. 1, 2, 3).
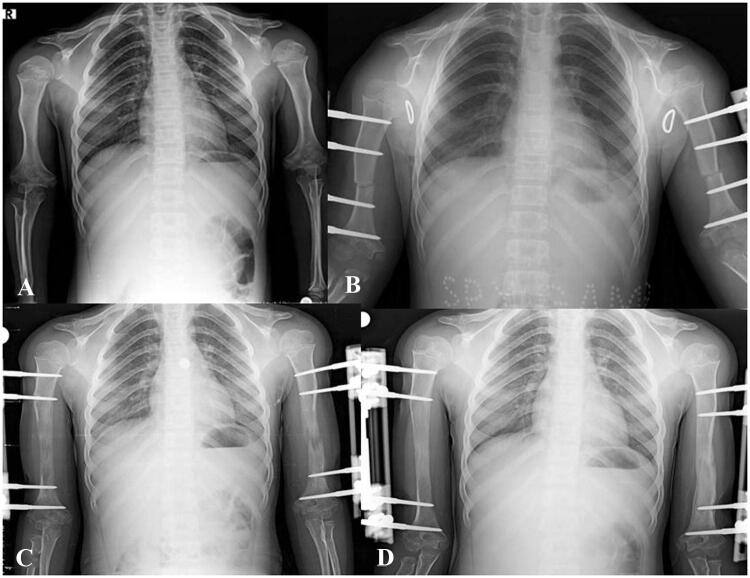
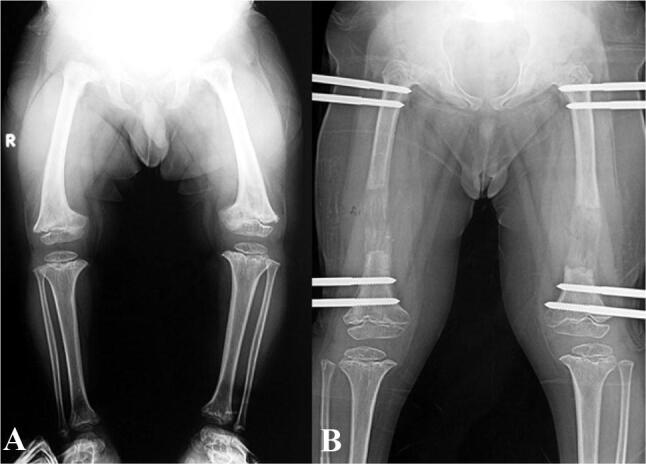
Fig. 1.
a Preoperative full-length weight-bearing lower-extremity radiograph of patients with achondroplasia. b Full-length weight-bearing lower-extremity radiograph of patients with simultaneous bilateral lengthening of femur and tibia. c Postoperative view of the patient
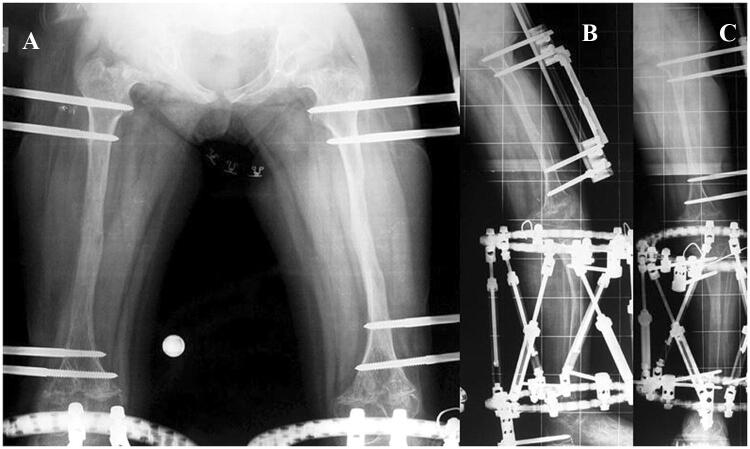
Fig. 2.
a Preoperative full-length weight-bearing lower-extremity radiographs of patients with achondroplasia. b X-Ray view of bilateral femoral lengthening the patients
Fig. 3.
a Preoperative bilateral humerus X-ray view, b, c Bilateral humeral lengthening view. d Postoperative bilateral humerus view of the patients
Distraction started seven days after the surgery at a rate of 0.25 mm, four times a day (1 mm/day) and arranged according to the clinical and radiological follow up. Starting from the next day of operation, patients were allowed to weight bearing as much as they could tolerate with the walker. Patients were followed up in the orthopedic department every two weeks until the end of the lengthening period and monthly until fixator removal. According to X-ray control made every 2 weeks, in the event of insufficient callus formation, we decreased the rhythm.
When sufficient callus formation and consolidation were achieved at one or two cortices, dynamization was applied to all patients approximately one month prior to removal of the fixator. After the consolidation seen at three cortices, we removed the external fixator and applied external brace for a mean of 34 days (range 28–42 days) to prevent plastic deformation and regenerate fracture.
Assessment of HRQOL
The PedsQL Measurement Model (Children's Hospital and Health Center, San Diego, California) consists of 4 subscales with a total of 23 questions and is intended to measure "the patient's and the parent's perceptions of the patient's HRQOL, as defined in terms of the impact of disease and treatment on an individual's physical, psychological, social and school functioning [5]. The four subscales or functional dimensions are as follows: (1) Physical Functioning (8 items); (2) Psychological Functioning (5 items); (3) Social Functioning (5 items); and (4) School Functioning (5 items). The first three subscales evaluate dimensions that are required at a minimum by the World Health Organization for an HRQOL instrument to be considered valid. Responses were scored as described by Varni et al. [4], by converting raw scores of 0–4 to HRQOL scores on a 100-point scale as follows: 0 = 100; I = 75; 2 = 50; 3 = 25; O = 4, on which higher scores denote a better HRQOL. A single score was calculated for each individual's responses (Individual Total Scale Score) by adding the scores of all items answered and dividing by the number of items answered. The Physical Functioning Subscale Score (sum of responses to 8 items) is considered the Physical Health Summary Score. The Psychosocial Health Summary Score (responses to 15 items) was computed as the sum of the items divided by the number of items answered in the Emotional, Social, and School Functioning subscales.
Evaluations of Complications
The complications were divided according to the classification proposed by Caton [6]. With this classification, there were three categories of patients and three categories of complications. Category I patients had no or minor complications and healed at the end of the lengthening procedure. Category II patients required an additional surgical intervention that was not envisaged in the initial strategy. These complications did not leave sequelae and the lengthening procedure was completed. Category III patients had major complications that left sequelae and/or the lengthening program could not be carried out as expected.
20 non-operated patients with achondroplasia who were followed-up by our pediatric clinics were evaluated with the same PedsQL scoring test. These patients were also evaluated for a basal value of the quality of life.
Statistical Analysis
All the statistical analysis was performed using the SPSS version 22 statistics software program (IBM Corp, 2011, Armonk, NY). Descriptive statistical methods (mean, standard deviation, frequency, minimum, maximum) were used to evaluate the study data. The independent Student’s t test was used to analyze the differences with regard to the different groups; simultaneous group, consecutive group, non-operated group, complication groups, humeral lengthening, and other groups. Differences in the number of complications were assessed with the Pearson χ2 test. Pearson correlation also used for between all scores and sex, age, amount of lengthening and fixator time, and a p value of < 0.05 was regarded as significant.
Result
HRQOL Results
The operated group's physical score was 81.72 ± 7.7 (65–90), psychological total score was 80.18 ± 5.67 (71–90) and total score was 80.80 ± 4.48 (73–90). The non-operated group's physical score was 76.34 ± 6.9 (65–83), psychological total score was 78.52 ± 6.79 (65–89) and total score was 77.41 ± 6.68 (78–88). All score was higher in an operated group but there were no significant differences (p: 0.712, p: 0.641 and p: 0.701). There was no significant difference between the simultaneous group and consecutive group psychological total summary score and total score did not show a significant difference (p > 0.05). But the physical score was significantly different, simultaneous group physical scores were higher than the consecutive group (p: 0.026) (Table 3). The all scores were significantly higher in the patients with bilateral humeral lengthening than no humeral lengthening (p < 0.05) (Table 4).
Table 3.
Comparison of the simultaneous group and consecutive group all scores
| Simultaneous lengthening of bilateral femur and tibia | Consecutive lengthening of bilateral femur and tibia | p value | |||
|---|---|---|---|---|---|
| Mean | S.D. | Mean | S.D. | ||
| Physical health | 84.08 | 5.93 | 79.03 | 8.70 | 0.026* |
| Psychosocial health | 80.13 | 5.28 | 80.23 | 6.22 | 0.901 |
| Total score | 80.82 | 4.82 | 80.79 | 5.09 | 0,923 |
*p < 0,05
Table 4.
Comparison of the humerus lengthening patients’ scores and scores of patients who did not undergo humeral lengthening
| Patients with humeral lengthening | Patients without humeral lengthening | p value | |||
|---|---|---|---|---|---|
| Mean | S.D | Mean | S.D | ||
| Physical health | 85.12 | 4.77 | 78.75 | 8.59 | 0.004* |
| Psychosocial health | 82.20 | 5.92 | 78.68 | 5.36 | 0.043* |
| Total score | 82.58 | 4.32 | 79.44 | 4.42 | 0.02* |
*p < 0,05
There was no significant difference in all scores of males and females. There was also no significant correlation between age at surgery time, lower and upper limb fixator time, % of lengthening increase in femur, tibia and humerus, amount of femoral, tibial and humeral lengthening and all patients’ scores.
Complication Results
Lower Extremity
There was no major complication that consists of category 3 was observed. There were ten patients with the category 2 which require surgery, two of which were regenerate fracture treated with Steinman pin and the other one was knee flexion deficiency treated with surgery. There were nine (18.3%) patients with regenerate fracture, sixteen (32.6%) patients, thirty-six (18.3%) segments (16 femur, 20 tibia) with pin tract infection, seven (14.28%) patients with transient nerve paralyzes and eight (16.8%) patients with knee contractures. Eight patients had unilateral (7 femur, 1 tibia) regenerate fractures and one had bilateral femur regenerate fracture. Regenerate fracture with unilateral treated with long knee cast for the femur and above the knee for tibial. Bilateral femur regenerate was treated with Steinmann pins (Figs. 4, 5). All pin-track infections were resolved after antibiotic therapy and local wound care. Spontaneous recovery was observed in all patients with transient nerve paralyses within 6 months period. Seven of eight patients were treated with redressement operation (straightening by force under general anesthesia) before the removal of external fixator and one of them was treated with quadricepsplasty surgery. There was no limitation in these knees in the last visit. There were no significant differences in all scores between patients with complication and without complication who underwent lower limb lengthening surgery (Table 5).
Fig. 4.
a–c Patients underwent simultaneous bilateral lengthening surgery
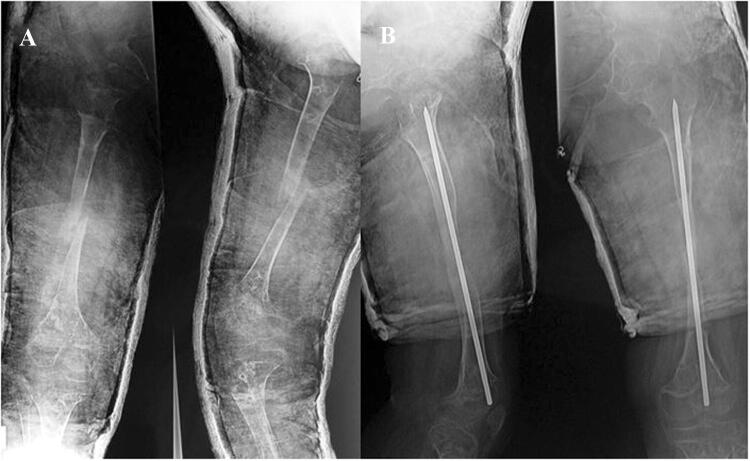
Fig. 5.
a This patient has regenerate fracture after removal of the fixator. b This patient was treated with Steinman pin
Table 5.
Comparison of all scores between patients with complication and without complication who underwent lower limb lengthening surgery
| Patients with complication (n: 30) | Patients without complication (n: 19) | p value | |||
|---|---|---|---|---|---|
| Mean | S.D | Mean | S.D | ||
| Physical health | 80.62 | 6.17 | 83.01 | 5.19 | 0.13 |
| Psychosocial health | 78.12 | 4.78 | 81.89 | 6.10 | 0.27 |
| Total score | 79.11 | 5.13 | 82.27 | 5.71 | 0.19 |
Upper Extremity
There were five patients (11.9%) with pin-track infections which resolved after antibiotic therapy and local wound care, three patients (7.1%) with transient radial nerve palsy occurring after surgery but diminishing spontaneously, and four patients (9.5%) with regenerate fracture which treated with cast application, one of them bilateral regenerate fracture. There were no significant differences in all scores between patients with complication and without complication who underwent bilateral humeral lengthening surgery.
Discussion
The first conclusion of this study is that limb lengthening surgery has minimal effect on midterm quality of life in patients with achondroplasia. The transient or minor complications may influence the patient’s quality of life during the lengthening time. The second conclusion is that transient or minor complications have minimal effects on the midterm quality of life patients with achondroplasia. There were no significant differences in the rate of complication and midterm quality of life between simultaneous and consecutive lengthening of femur and tibia. When the scores of these groups were evaluated, only physical scores were found to be significantly different. The main conclusion is that humeral lengthening surgery by itself had a significant effect on patient quality of life.
There are many studies looking at the results of lengthening surgery in achondroplasia patients in the literature [2, 3, 6, 7]. Kocaoglu et al. [7] report that 22 patients with simultaneous bilateral lower limb lengthening surgery result in their study, in which the fixator time in the simultaneous group was reduced half and half. In a study reporting twenty-two patients with achondroplasia, all the patients who had no or only minor complications were satisfied with their results [8]. Additionally, in our study, a physical score was significantly higher than a consecutive group. In our study, rates of complications were similar compared to the other series [9, 10]. Similarly, according to our result, a transient complication has minimal effect on the midterm quality of life patients with achondroplasia.
In our experience, bilateral humeral lengthening is an effective surgery in patients with achondroplasia. Despite minor complications, the physical health summary score, psychosocial health summary score, and total score were significantly higher than patients with no humeral lengthening in our series [11]. In a study by Kim et al. [12], patients underwent bilateral femoral and humeral lengthening surgery. The authors compared the result of upper and lower limb satisfaction with Rosenberg self-esteem questionnaire and Short Form-36 (SF-36) quality-of-life instrument score. These scores were significantly improved as a result of humeral lengthening in their series [12].
There are many studies evaluation of quality of life in patients with achondroplasia [12, 13]. Kim et al. investigated quality-of-life patients with achondroplasia who underwent lower limb lengthening surgery using the SF-36 quality-of-life instrument score [12]. Matsushita et al. investigated whether final height had an impact on the quality of life and evaluated what kinds of medical interventions were positively or negatively associated with health-related quality of life. They used the SF-36 scoring system and found that the physical component summary was improved in the patients who had a height of 140 cm or taller. They also recommended that a treatment strategy would be planned to gain a final height of 140 cm or taller during childhood in combination with growth hormone administration and limb lengthening surgeries [13]. We chose the PedsQL4.0 to measure the HRQOL in our study of patients with achondroplasia who underwent limb lengthening surgery due to the fact that the questions on the PedsQL are written in age-appropriate language for several age groups, and the stability and validity of the PedsQL have been evidenced in literature and the questionnaire is quick and easy to administer.
The PedsQL differentiated HRQOL between healthy children and those with acute or chronic health conditions and was correlated with measures of morbidity and illness [14]. The PedsQL 4.0 is the only generic pediatric HRQOL measurement instrument that we are aware of ages 2–18 for self-report and proxy-report while maintaining item and scale construct consistency. Validation analyses confirmed a high internal consistency and could successfully differentiate between healthy people and young ones with chronic diseases [15]. Varni et al. used the 4 PedsQL 4.0 which were administered to 963 children and 1629 parents (1677 subjects accrued overall) recruited from pediatric health care settings. They founded that demonstrate the reliability and validity of the PedsQL 4.0. The PedsQL 4.0 may be applicable in clinical trials, research, clinical practice, school health settings and community populations [4]. It was founded in their study that the physical score was 84.41, the psychological total score was 82.38 and the total score was 83.0 in 401 healthy children who average age 10.7 years and the physical score was 77.36, the psychological total score was 77.10 and the total score was 77.19 in 367 chronically ill patients. In our study, the operated group's physical score was 81.72 ± 7.7 (65–90), the psychological total score was 80.18 ± 5.67 (71–90) and the total score was 80.80 ± 4.48 (73–90). The non-operated group's physical score was 76.34 ± 6.9 (65–83), psychological total score was 78.52 ± 6.79 (65–89) and the total score was 77.41 ± 6.68 (78–88). Although patients with achondroplasia who underwent limb lengthening had lower scores than healthy patients, they had higher scores than chronically ill patients. Non-operated achondroplasia had scores lower than chronically ill patients and healthy children.
This study has some limitations. This study is a retrospective case series. We have not taken into account other factors that affect the quality of life in patients with achondroplasia, such as respiratory problems, obesity, and other neurologic disorders. Last, we just took one stage lengthening procedure for the limbs. In fact, one stage lengthening is enough for humerus but to reach more than 140–145 cm length we need mostly second lengthening procedure. If the second lengthening is also taken into consideration, statistically significant results for lower extremity can be obtained.
Conclusion
Although there is no statistical difference, scores were high as a result of lengthening surgery patients with achondroplasia. The effect of transient complications on patient satisfaction was not statistically determined. Patients who undergo humeral lengthening besides lower limb lengthening procedures have higher scores. This study suggests that quality of life is significantly improved as a result of humerus lengthening surgery of patients with achondroplasia.
Acknowledgements
Authors thank all siblings and parents of children with a chronic disease for their voluntarily participation.
Funding
There is no funding source.
Compliance with Ethical Standards
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical standard statement
Ethical approval was given by the institutional review board.
Informed consent
The procedures were explained in detail and written informed consent was obtained from all patients.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Paley D. Current techniques of limb lengthening. Journal of Pediatric Orthopedics. 1998;8:73–92. doi: 10.1097/01241398-198801000-00018. [DOI] [PubMed] [Google Scholar]
- 2.Cattaneo R, Villa A, Catagni M, Tentori L. Limb lengthening in achondroplasia by Ilizarov’s method. International Orthopaedics. 1988;2:173–179. doi: 10.1007/BF00547160. [DOI] [PubMed] [Google Scholar]
- 3.Lavini F, Renzi-Brivio L, de Bastiani G. Psychologic, vascular, and physiologic aspects of lower limb lengthening in achondroplastics. Clinical Orthopaedics and Related Research. 1990;250:138–142. [PubMed] [Google Scholar]
- 4.Varni JW, Seid M, Kurtin PS. PedsQL (TM) 4.0: Reliability and validity of the pediatric quality of life Inventory (TM) Version 4.0 generic core scales in healthy and patient populations. Medical Care. 2001;39:800–812. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Varni JW, Seid M, Rode CA. The PedsQL: Measurement model for the Pediatric Quality of Life Inventory. Medical Care. 1999;37:126–139. doi: 10.1097/00005650-199902000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Caton J. Treatment of length discrepancies in the lower limbs and small subjects in children and adolescents. Revue de Chirurgie Orthopédique. 1991;77(Suppl.I):31–80. [Google Scholar]
- 7.Kocaoğlu M, Bilen FE, Dikmen G, Balci HI, Eralp L. Simultaneous bilateral lengthening of femora and tibiae in achondroplastic patients. Acta Orthopaedica et Traumatologica Turcica. 2014;48:157–163. doi: 10.3944/AOTT.2014.3274. [DOI] [PubMed] [Google Scholar]
- 8.Kim SJ, Agashe MV, Song SH, Choi HJ, Lee H, Song HR. Comparison between upper and lower limb lengthening in patients with achondroplasia: A retrospective study. Journal of Bone and Joint Surgery British Volume. 2012;94:128–133. doi: 10.1302/0301-620X.94B1.27567. [DOI] [PubMed] [Google Scholar]
- 9.Yun AG, Severino R, Reinker K. Attempted limb lengthening beyond twenty percent of the initial bone length: Results and complications. Journal of Pediatric Orthopedics. 2000;20:151–159. [PubMed] [Google Scholar]
- 10.Vargas Barreto B, Caton J, Merabet Z, Panisset JC, Pracros JP. Complications of Ilizarov leg lengthening: A comparative study between patients of leg length discrepancy and short stature. International Orthopaedics. 2007;31:587–591. doi: 10.1007/s00264-006-0236-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Balci HI, Kocaoglu M, Sen C, Eralp L, Batibay SG, Bilsel K. Bilateral humeral lengthening in achondroplasia with unilateral external fixators: Is it safe and does it improve daily life? The Bone and Joint Journal. 2015;97:1577–1581. doi: 10.1302/0301-620X.97B11.36037. [DOI] [PubMed] [Google Scholar]
- 12.Kim SJ, Balce GC, Agashe MV, Song SH, Song HR. Is bilateral lower limb lengthening appropriate for achondroplasia?: Midterm analysis of the complications and quality of life. Clinical Orthopaedics and Related Research. 2012;470(2):616–621. doi: 10.1007/s11999-011-1983-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Matsushita M, Kitoh H, Mishima K, Yamashita S, Haga N, Fujiwara S, Ozono K, Kubota T, Kitaoka T, Ishiguro N. Physical, mental, and social problems of adolescent and adult patients with achondroplasia. Calcified Tissue International. 2019;104:64–72. doi: 10.1007/s00223-019-00518-z. [DOI] [PubMed] [Google Scholar]
- 14.Dinleyici M, Çarman KB, Özdemir C, Harmancı K, Eren M, Kirel B, Şimşek E, Yarar C, Duyan Çamurdan A, Şahin DF. Quality-of-life evaluation of healthy siblings of children with chronic illness. Balkan Medical Journal. 2019;37(1):34–42. doi: 10.4274/balkanmedj.galenos.2019.2019.7.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Varni JW, Limbers CA. The PedsQL 4.0 generic core scales young adult version: Feasibility, reliability and validity in a university student population. Journal of Health Psychology. 2009;14:611–622. doi: 10.1177/1359105309103580. [DOI] [PubMed] [Google Scholar]