Abstract
Objective
Stenting of coarctation of aorta with covered or uncovered stents is the accepted modality of treatment in older children and adults. The indications which mandate the use of covered stents are still unclear. We attempted to study the early and late outcomes after stenting of native and recurrent coarctation of aorta with uncovered and covered stents.
Method
This is a retrospective study of patients who underwent stenting for coarctation of aorta with covered or non-covered stents at our institute. Early and late outcome for both the groups were studied.
Results
Twenty patients underwent implantation of covered stent and twenty five patients had uncovered stent implantation. Patients in the covered stent group were older and had greater basal pressure gradient. More patients in the covered stent group had residual gradient >10 mm Hg after the procedure. There was no mortality or aortic wall injury in either group. Four patients in the covered stent group underwent planned re-intervention and two had unplanned re-intervention. None of the patients in the uncovered stent group had re-intervention. Higher incidence of late lumen loss was noted in the covered stent group.
Conclusion
Uncovered stents can be safely implanted with minimal risk of aortic wall injury in patients with low risk anatomic features. Covered stent implantation is associated with higher incidence of planned and unplanned re-intervention.
Keywords: Coarctation of aorta, Stent implantation, Congenital heart disease, Intervention
1. Background
Interventional therapy for coarctation of aorta has evolved over the past three decades from balloon angioplasty to covered stents.1 Stand-alone balloon angioplasty is seldom done as aortic complications are higher with this technique. Elective use of stents tackle most of the aortic wall complications.2,3 Covered stents were initially used as bail-out strategy to treat major aortic wall injury.4, 5, 6 As favourable data on safety and efficacy of covered stents became available, many centres consider covered stents as the primary modality of transcatheter treatment of coarctation of aorta.7, 8, 9, 10, 11, 12 However, the anatomical features that mandate the use of covered stents is still not fully established.
Covered stent implantation is not without associated risks. Implantation of covered stent requires larger vascular access, with increased risk of access site complications. Obstruction to aortic branches can occur after implantation of covered stents. Complications like aortic rupture,9,10,13 stent fracture,14 aneurysm formation,15 in-stent restenosis16 and infolding of stent17 have been described with covered stents. Moreover, in the rare event of embolization of a covered stent, there is possibility of aortic branch occlusion. Covered stent implantation is contra-indicated in transverse arch hypoplasia, which can be successfully treated by implantation of non-covered stents. This suggests that elective covered stent implantation is not required in all patients with coarctation. Non covered balloon expandable and self expanding stents have both been shown in numerous studies to be safe and effective in low risk anatomical substrates.18,19
We have attempted to review the evolution of this procedure in our institute. We started with covered stent in all patients, as we had a few cases of severe aortic dissection in the balloon angioplasty era. Later on we, along with many other centres, learned that non-covered stents are as good and have its own advantages in the young. With increasing experience, we now implant non-covered stents for most of the patients with coarctation. Currently we reserve covered stent for high risk anatomic indications. This is a descriptive study on early and late outcome after stenting of native and recurrent coarctation of aorta with non-covered and covered stents.
2. Methods
Ethics committee approval was obtained from our institute for the conduct of this study. We retrospectively studied 45 patients who underwent covered or non-covered stenting of native or recurrent coarctation of aorta, at our institute between 2003 and 2017. As described above, we used to electively implant covered stents in all patients undergoing this procedure. Considering the increased risk of vascular complications in smaller children, we switched over to implanting non-covered stents in most patients. Covered stents are currently used in patients with presumed high risk of acute aortic wall injury, such as adults with severe coarctation and children with risk factors for aortopathy, such as bicuspid aortic valve with aortic root dilation.
All relevant clinical data, anatomical information and details of drug therapy of systemic hypertension were collected from hospital records. Only patients weighing more than 20 kg were considered for stenting. All patients underwent pre-procedure imaging by CT or MR angiogram and the procedure was done under general anaesthesia. Stents were chosen based on the transverse arch diameter and were either the same size or 1–2 mm more than the diameter of transverse arch. The coarctation segment was crossed retrogradely in most patients. Aortograms were taken in left anterior oblique projection in all patients and additional projections were obtained in selected patients. Balloon dilatation was done in selected cases to facilitate tracking of delivery sheath across the segment. Pressure gradient across the segment was obtained before and after stenting. Data on stent related complications, aortic wall complications and vascular complications were collected. Procedural success was defined as reduction of ascending to descending aortic systolic gradient less than 10 mm Hg without major aortic wall injury and stent migration. Follow-up data on number of antihypertensive drug use and clinical pressure gradient were obtained. Majority of patients underwent CT angiography 6 months after the index procedure and were assessed for loss of stent integrity, late aortic wall complications and re-obstruction, which was classified as mild (narrowing of <10% of stent lumen), moderate (10–30% lumen narrowing) and severe (>30% lumen narrowing).1 Long term outcomes studied were survival, need for re-intervention (planned and unplanned) and presence of residual clinical gradient and hypertension.
3. Statistical analysis
Statistical analysis was done by the Statistical Package for Social Sciences (version 21.0, SPSS Inc., Chicago, Illinois). Quantitative data were presented as mean ± SD or as median and range and qualitative data were presented as frequency (percentages). The categorical parameters were compared by chi-square test, and the continuous variables were compared by Student t test for independent continuous data and Mann–Whitney U test for nonparametric data.
4. Results
4.1. Baseline characteristics
Forty-five patients underwent coarctation stenting in this period, of whom 20 were implanted with covered stents and 25 were implanted with non-covered stents (Table 1). 71% of the patients were males. Covered stents used were covered Cheatham-Platinum stent (NuMed, Hopkinton, New York) in 7 patients and the Advanta V12 stent (Atrium, Mijdrecht, The Netherlands) in 13 patients. The non-covered stents used were Cheatham-Platinum stent in 17 patients, AndraXL and XXL stents (Andramed, Reutlingen, Germany) in 6 patients and Palmaz XL (Johnson and Johnson, Cordis, Roden, The Netherlands) stent in 2 patients.
Table 1.
Baseline characteristics.
| Covered (20) | Uncovered (25) | |
|---|---|---|
| Mean age (years) | 34.8 ± 17 | 18.6 ± 7.5 |
| Males | 13 | 19 |
| Mean weight, kg | 51.3 ± 16 | 46 ± 14.5 |
| Native coarctation | 16 | 19 |
| Recurrent coarctation | 4 | 6 |
| Associated anomalies | ||
| Bicuspid aortic valve | 12 | 8 |
| Turner syndrome | 0 | 2 |
| Marfan | 1 | 0 |
| Phaces syndrome | 0 | 1 |
| Site of coarctation | ||
| Post-subclavian | 20 | 21 |
| Juxta subclaivan | 0 | 2 |
| Transverse aortic arch | 0 | 1 |
| Mean number of anti-hypertensives | 2.2 ± 1.2 | 1.5 ± 1 |
Patients who had covered stent implantation were older (mean age 34.8 ± 17 Vs18.6 ± 7.5- p = 0.001). In the covered stent group, all patients had post-subclavian coarctation and in the non-covered stent group, 23 patients had post subclavian coarctation and two had aortic arch narrowing. More patients in covered stent group had associated bicuspid aortic valve (57% vs 32%).
4.2. Procedural characteristics
Patients who underwent covered stent implantation had greater basal pressure gradient (58.3 ± 23.9 vs 35.8 ± 15.4; p = 0.001) and greater requirement of balloon pre-dilation and ventricular pacing during stent implantation (Table 2). Systolic pressure gradient after stent implantation was higher in the covered stent group (6.29 ± 9.76 mm Hg vs 2.68 ± 4.18 mmHg; p = 0.08, NS). Procedural success (ascending to descending aorta systolic gradient < 10 mm Hg without aortic wall injury) was attained in 15/20 in the covered group and 22/25 in the non-covered stent group (p = 0.06). None developed acute major aortic wall injury. Three patients developed vascular access site complications after the procedure and stent malposition occurred in one patient. More patients in covered stent group were planned for elective re-intervention after index procedure.
Table 2.
Procedural details.
| Covered (21) | Uncovered (25) | |
|---|---|---|
| Mean systolic pressure gradient before stenting (mm Hg) | 58.3 ± 23.9 | 35.8 ± 15.4 |
| Mean systolic pressure gradient after stenting (mm Hg) | 6.3 ± 9.8 | 2.7 ± 4.2 |
| Pacing | 17 | 12 |
| Predilatation | 10 | 4 |
| Procedural success | 15 | 22 |
| Staged re-intervention planned | 4 | 0 |
| Vascular closure device used | 10 | 15 |
| Access site complications | 2 | 2 |
4.3. Follow-up data
The patients were followed up for a median of 57 months in the covered stent group and 35 months in the non-covered stent group (Table 3). None died during this follow-up period. Number of antihypertensive drugs required came down significantly for both groups (p = 0.02). Four patients underwent planned re-intervention (balloon angioplasty) and two patients underwent unplanned re-intervention (balloon angioplasty) for stent collapse (Table 4), in the covered stent group. Re-dilation of the covered stents was free of complications and effective in majority of the patients. One patient in the covered stent group continues to have >20 mm Hg pressure gradient after re-dilation. Three patients in the covered stent group and one patient in the non-covered stent group have pressure gradient between 10 and 20 mm Hg, across the coarctation segment. Cumulative adverse late outcome (defined as need for re-intervention and/or presence of upper limb-lower limb BP difference >10 mm Hg) was worse in the covered stent group (p = 0.01).
Table 3.
Outcome.
| Covered (20) | Uncovered (25) | |
|---|---|---|
| Median follow-up,months | 57 (12–129) | 35 (14–86) |
| Upper limb/lower limb BP gradient > 10 mm Hg | 3 | 1 |
| Mean number of anti-hypertensives | 1.38 ± 0.74 | 1 + 0.7 |
| Imaging on follow-up | 18 | 8 |
| Late lumen loss | ||
| No or mild | 2 (Advanta 1, CP 1) | 4 (CP 3, Palmaz 1) |
| Moderate | 12 (Advanta 7, CP 4, Andra 1) | 4 (CP3, Palmaz 1) |
| Severe | 4 (Advanta 3, CP 1) | 0 |
| Strut fracture | 1 (Advanta) | 0 |
Table 4.
Re-intervention.
| Planned reintervention (4) | Unplanned reintervention (2) | |
|---|---|---|
| Type of stent | Covered (4) Uncovered (0) |
Covered (2) Uncovered (0) |
| Indication | Residual gradient (4) Advanta (3) CP (1) |
Proximal stent collapse (1) (Advanta) Mid part of stent collapse (1) (Advanta) |
| Reintervention | Balloon angioplasty | Balloon angioplasty |
| Outcome | Residual gradient 10–20 mm Hg (2) No residual gradient (2) |
Residual gradient > 20 mm Hg (1) No residual gradient (1) |
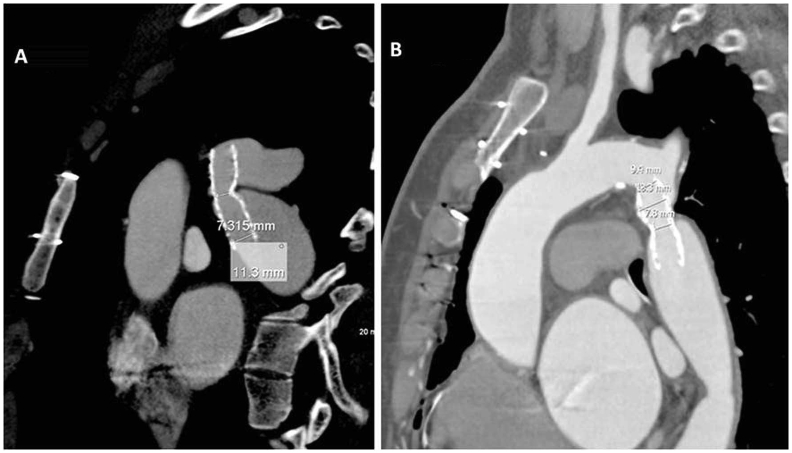
4.4. Follow-up imaging
Twenty six patients underwent imaging on follow-up - non invasive angiography in 22 patients and invasive angiography in 4 patients. 12 of 18 patients who underwent covered stenting had moderate late lumen loss (Fig. 1A) and 4 had severe late lumen loss (Fig. 1B). 4 of the non-covered stent group had moderate late lumen loss. One patient in the covered stent group had single strut fracture (Fig. 2), but it was not causing significant lumen loss. None of the patients had late aneurysm formation.
Fig. 1.
A): CT image showing coarctation stent with moderate lumen narrowing; (B): CT image showing coarctation stent with severe lumen narrowing.
Fig. 2.
Axial CT image showing single strut fracture without luminal narrowing (yellow arrow).
5. Discussion
Transcatheter therapy with stenting has shown comparable efficacy profile to surgical correction for coarctation of aorta, with lower rate of acute complications.1 Balloon angioplasty and stenting produces desired effect by tearing the aortic wall, which is inevitable in this procedure. The metal scaffold of the stent apposes the intimal flap to the media, thereby reducing the risk of late aneurysm formation. Stent also provides radial support to the vessel wall, preventing recoil. Risk of aortic wall injury is approximately 10% after balloon angioplasty and 4% after stenting.2 Adult patients with sub-atretic coarctation and patients with aortic wall weakening carries high risk of severe vessel trauma, resulting in adventitial dissection, aneurysm formation and vessel rupture. This catastrophic situation is managed by immediate implantation of covered stent, which might take few minutes. During this time period life threatening major bleeding continues. Elective use of covered stents prevents these complications, and is the preferred stenting option in these patients.7, 8, 9, 10, 11
Some centres electively implant covered stents in all patients with coarctation, so as to prevent acute major aortic wall injury and late aneurysm formation. In this observational study, we studied the incidence of these two parameters in our cohort. We could not find even a single case of major aortic wall injury or late aneurysm formation, in our low risk coarctation cohort implanted with non-covered stent. We electively implanted covered stents in our high-risk cohort and no patient in this group developed major aortic wall injury. However, more patients in the covered stent group had hemodynamically significant pressure gradient after index procedure, requiring staged re-intervention. Two patients in the covered stent group required unplanned re-dilatation for re-obstruction as well. This was in contrast to another study that compared the outcomes after bare or covered stent implantation, which showed similar procedural success in both groups with a non-significant decrease in re-coarctation in the covered stent group.12 Overall, we noted greater procedural success and freedom from re-intervention in the non-covered stent group after index procedure (p = 0.06). We also observed greater incidence of severe late lumen loss (>30% lumen loss) in the covered stent group on follow-up. This phenomenon was brand specific (Advanta V12 stent). The Advanta V12 LD stent (Atrium Medical, NH) is a balloon expandable laser cut 316L stainless steel stent with a covering made of expanded PTFE. The design of the Advanta stent is such that it is encapsulated by PTFE covering on both the internal and external aspects. This could contribute to elastic recoil and inadequate anchorage to vessel wall, thus leading to late lumen loss. Single strut fracture which was not causing any lumen obstruction was also noted in one Advanta V12 stent. The stents have an open cell stent geometry with consequent less radial strength. A previous study on Advanta stent implantation in 25 patients did not show any complications related to the stent. However, the median period of follow-up in that study was only 4.9 months and longer follow-up is needed to look for recoarcattion or aneurysm formation.20 Another study described 2 patients with Advanta stent implantation who developed infolding of the proximal edge of the stent on follow-up and both the cases were managed by restenting.17 We had a similar proximal stent collapse in a patient who had Advanta stent implantation, which was managed by balloon angioplasty. Though the residual gradient was 5 mm Hg immediately after the balloon angioplasty, the gradient increased to 25 mm Hg on follow-up and he underwent a repeat balloon angioplasty with good result.21
Smaller vascular sheath sizes (2 F smaller than that for a corresponding sized covered stent) were used for implanting non-covered stents and this offered a significant advantage in children. Vascular haemostasis can be achieved without using vascular closure devices up to sheath size of 10 F. This is of advantage in children; as suture based vascular closure devices produce minor narrowing of common femoral artery, which could be hazardous in children with small femoral arteries.
Outcome from our study suggest that non-covered stent implantation is a safe and effective option in low risk patients with aortic coarctation. It is also a more cost effective option when compared to covered stents. Accepted criteria for low risk include younger age, non-critical coarctation, and absence of calcification and lack of evidence of aortopathy. Elective covered stent implantation in all patients with coarctation of aorta is not desirable.
6. Conclusions
Stenting of coarctation using non-covered or covered stents is an effective therapy for native and recurrent coarctation in older children and adults. Non-covered stents can be safely implanted with minimal risk of aortic wall injury in patients with low risk anatomic features. Covered stent implantation was associated with higher incidence of planned and unplanned re-intervention in our study.
7. Limitation
This study is an observational study with selection bias, as patients with presumed high risk features underwent elective covered stent implantation. Follow-up invasive or non-invasive angiography was performed in 57% of patients only.
Funding
None.
Conflict of interest
There are no conflict of interests.
Acknowledgement
None.
References
- 1.Forbes T.J., Kim D.W., Du W. Comparison of surgical, stent, and balloon angioplasty treatment of native coarctation of the aorta: an observational study by the CCISC (Congenital Cardiovascular Interventional Study Consortium) J Am Coll Cardiol. 2011 Dec 13;58(25):2664–2674. doi: 10.1016/j.jacc.2011.08.053. [DOI] [PubMed] [Google Scholar]
- 2.Salcher M., Naci H., Law T.J. Balloon dilatation and stenting for aortic coarctation: a systematic review and meta-analysis. Circulation Cardiovasc Intervent. 2016 Jun;9(6) doi: 10.1161/CIRCINTERVENTIONS.115.003153. [DOI] [PubMed] [Google Scholar]
- 3.Forbes T.J., Moore P., Pedra C.A. Intermediate follow-up following intravascular stenting for treatment of coarctation of the aorta. Cathet Cardiovasc Interv. 2007 Oct 1;70(4):569–577. doi: 10.1002/ccd.21191. [DOI] [PubMed] [Google Scholar]
- 4.Gunn J., Cleveland T., Gaines P. Covered stent to treat coexistent coarctation and aneurysm of the aorta in a young man. Heart. 1999;82:351. doi: 10.1136/hrt.82.3.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Forbes T., Matisoff D., Dysart J., Aggarwal S. Treatment of coexistent coarctation and aneurysm of the aorta with covered stent in a pediatric patient. Pediatr Cardiol. 2003;24:289–291. doi: 10.1007/s00246-002-0262-9. [DOI] [PubMed] [Google Scholar]
- 6.Holzer R., Concilio K., Hijazi Z. Selffabricated covered stent to exclude an aortic aneurysm after balloon angioplasty for post-surgical recoarctation. J InvasiveCardiol. 2005;17:177–179. [PubMed] [Google Scholar]
- 7.De Giovanni J.V. Covered stents in the treatment of aortic coarctation. J Intervent Cardiol. 2001;14:187–190. doi: 10.1111/j.1540-8183.2001.tb00732.x. [DOI] [PubMed] [Google Scholar]
- 8.Qureshi S.A., Zubrzycka M., Brzezinska-Rajszys G., Kosciesza A., Ksiazyk J. Use of covered Cheatham-platinum stents in aortic coarctation and recoarctation. CardiolYoung. 2004;14:50–54. doi: 10.1017/s104795110400109x. [DOI] [PubMed] [Google Scholar]
- 9.Kenny D., Margey R., Turner M.S., Tometzki A.J., Walsh K.P., Martin R.P. Self-expanding and balloon expandable covered stents in the treatment of aortic coarctation with or without aneurysm formation. Cathet Cardiovasc Interv. 2008;72:65–71. doi: 10.1002/ccd.21559. [DOI] [PubMed] [Google Scholar]
- 10.Tanous D., Collins N., Dehghani P., Benson L.N., Horlick E.M. Covered stents in the management of coarctation of the aorta in the adult: initial results and 1-year angiographic and hemodynamic follow-up. Int J Cardiol. 2010;140:287–295. doi: 10.1016/j.ijcard.2008.11.085. [DOI] [PubMed] [Google Scholar]
- 11.Tzifa A., Ewert P., Brzezinska-Rajszys G. Covered Cheatham-platinum stents for aortic coarctation. Early and intermediate results. J Am Coll Cardiol. 2006;47:1457–1463. doi: 10.1016/j.jacc.2005.11.061. [DOI] [PubMed] [Google Scholar]
- 12.Sohrabi B., JamshidiP, Yaghoubi A. Comparison between covered and bare cheatham-platinum stents for endovascular treatment of patients with native post-ductal aortic coarctation. J Am Coll Cardiol Intv. 2014;7:416–423. doi: 10.1016/j.jcin.2013.11.018. [DOI] [PubMed] [Google Scholar]
- 13.Collins N., Mahadevan V., Horlick E. Aortic rupture following a covered stent for coarctation: delayed recognition. Cathet Cardiovasc Interv. 2006;68:653–655. doi: 10.1002/ccd.20831. [DOI] [PubMed] [Google Scholar]
- 14.Ewert P., Schubert S., Peters B., Abdul-Khaliq H., Nagdyman N., Lange P. The CP stent – short, long, covered – for the treatment of aortic coarctation, stenosis of pulmonary arteries and caval veins, and Fontan anastomosis in children and adults: an evaluation of 60 stents in 53 patients. Heart. 2005;81:948–953. doi: 10.1136/hrt.2004.040071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pedra C., Fontes V., Esteves C. Use of covered stents in the management of coarctation of aorta. Pediatr Cardiol. 2005;26:431–439. doi: 10.1007/s00246-004-0814-2. [DOI] [PubMed] [Google Scholar]
- 16.Butera G., Piazza L., Chessa M. Covered stents in patients with complex aortic coarctations. Am Heart J. 2007;154:795–800. doi: 10.1016/j.ahj.2007.06.018. [DOI] [PubMed] [Google Scholar]
- 17.Wan A.W., Lee K.J., Benson L.N. Infolding of covered stents used for aortic coarctation: report of two cases. Catheter Cardiovasc Interv. 2014;83(1):104–108. doi: 10.1002/ccd.24998. 16. [DOI] [PubMed] [Google Scholar]
- 18.Tyagi S., Singh S., Mukhopadhyay S., Kaul U.A. Self-and balloon-expandable stent implantation for severe native coarctation of aorta in adults. Am Heart J. 2003 Nov 1;146(5):920–928. doi: 10.1016/S0002-8703(03)00434-4. [DOI] [PubMed] [Google Scholar]
- 19.Patnaik A.N., Srinivas B., Rao D.S. Endovascular stenting for native coarctation in older children and adolescents using adult self –expanding (nitinol) iliac stents. Indian Heart J. 2009;61:353–357. [PubMed] [Google Scholar]
- 20.Bruckheimer E., Birk E., Santiago R., Dagan T., Esteves C., Pedra C.A. Coarctation of the aorta treated with the Advanta V12 large diameter stent: acute results. Cathet Cardiovasc Interv. 2010;75:402–406. doi: 10.1002/ccd.22280. [DOI] [PubMed] [Google Scholar]
- 21.Saran M., Sasidharan B., Sivasubramonian S. Late stent collapse in aortic coarctation—an interplay of residual pressure gradient and radial strength. IHJ Cardiovasc Case Rep (CVCR) 2017 Jan 1;1(1):12–13. [Google Scholar]