Abstract
Background
In low- and middle-income countries (LMICs) where echocardiography experts are in short supply, training non-cardiologists to perform Focused Cardiac Ultrasound (FoCUS) could minimise diagnostic delays in time-critical emergencies. Despite advocacy for FoCUS training however, opportunities in LMICs are limited, and the impact of existing curricula uncertain. The aim of this study was to assess the impact of FoCUS training based on the Focus Assessed Transthoracic Echocardiography (FATE) curriculum. Our primary objective was to assess knowledge gain. Secondary objectives were to evaluate novice FoCUS image quality, assess inter-rater agreement between expert and novice FoCUS and identify barriers to the establishment of a FoCUS training programme locally.
Methods
This was a pre-post quasi-experimental study at a tertiary hospital in Nairobi, Kenya. Twelve novices without prior echocardiography training underwent FATE training, and their knowledge and skills were assessed. Pre- and post-test scores were compared using the Wilcoxon signed-rank test to establish whether the median of the difference was different than zero. Inter-rater agreement between expert and novice scans was assessed, with a Cohen's kappa >0.6 indicative of good inter-rater agreement.
Results
Knowledge gain was 37.7%, with a statistically significant difference between pre-and post-test scores (z = 2.934, p = 0.001). Specificity of novice FoCUS was higher than sensitivity, with substantial agreement between novice and expert scans for most FoCUS target conditions. Overall, 65.4% of novice images were of poor quality. Post-workshop supervised practice was limited due to scheduling difficulties.
Conclusions
Although knowledge gain is high following a brief training in FoCUS, image quality is poor and sensitivity low without adequate supervised practice. Substantial agreement between novice and expert scans occurs even with insufficient practice when the prevalence of pathology is low. Supervised FoCUS practice is challenging to achieve in a real-world setting in LMICs, undermining the effectiveness of training initiatives.
Keywords: Focused cardiac ultrasound, Training, Capacity building, Low and middle-income
Highlights
-
•
Where cardiologists are in short supply, focused cardiac ultrasound (FoCUS) by non-cardiologists may minimise diagnostic delays in time-critical emergencies.
-
•
A shortage of echocardiography experts hinders FoCUS capacity-building efforts however, as the supervised practice required to achieve competence is not assured.
-
•
Solutions to the supervision problem are vital, without which FoCUS training for non-cardiologists in Africa may be an exercise in futility.
Background
Low and middle-income countries (LMICs) are constrained in their ability to meet the needs of acutely ill patients in urgent need of echocardiographic evaluation [1]. Kenya for instance has only 50 cardiologists and 30 cardiac sonographers for a population of 46.6 million [2]. There is consensus among various professional societies that training non-cardiologists in acute care areas to perform a focused cardiac ultrasound (FoCUS) improves efficiency of care in time-critical emergencies [[3], [4], [5]]. This training however has not been established in many LMICs, nor has its educational impact been validated, despite the fact that its utility is presumably greatest here [1,[6], [7], [8]].
In the absence of a universal FoCUS protocol and with the diversity of curricula currently available, the European Association for Cardiovascular Imaging (EACVI) in 2018 made recommendations for a FoCUS core syllabus and core curriculum [9]. No recognised FoCUS courses are offered in Kenya however, requiring travel to accredited training centres abroad, making the process of training both costly and time-consuming for clinicians. Where trainings are conducted in Kenya on the other hand, there is lack of clarity regarding what oversight, if any, is provided during the period of supervised practice, rendering the quality of FoCUS performed by novices thereafter uncertain.
The Aga Khan University Hospital Nairobi is a 254-bed tertiary referral centre accredited by the Joint Commission International since 2013, that serves as the teaching hospital for Aga Khan University's Medical College [10]. The hospital has a busy accident and emergency (A&E) department with over 100,000 visits annually, oversight for which is provided an emergency physician with Level 1 basic emergency ultrasound accreditation from the Emergency Medicine Society of South Africa (EMSSA). The institution has 35 critical care beds with an average of 2400 admissions every year, staffed by six intensivists, only one of whom has formal training in FoCUS. With the lack of training opportunities locally for novices in echocardiography, bedside echocardiograms in acute care areas of AKUHN are almost exclusively performed by cardiologists and cardiac sonographers. As a result, critically ill patients in urgent need of echocardiographic evaluation are referred to the cardiology team for this service in the first instance, response time for which varies. Development of local FoCUS training programmes for novices in individual LMICs is key to capacity-building efforts, but must be guided by evidence to support the educational impact of these trainings. The aim of this study was therefore to assess the educational impact of FoCUS training based on the basic Focus Assessed Transthoracic Echocardiography (FATE) curriculum. Our primary objective was to assess knowledge gain in FoCUS following basic FATE training. Secondary objectives were to evaluate novice FoCUS image quality, assess inter-rater agreement between expert and novice FoCUS and identify barriers to the establishment of a FoCUS training programme locally.
Methods
This was a pre-post quasi-experimental study conducted at the Aga Khan University Hospital in Nairobi (AKUHN), Kenya. Novices of all cadres from critical care, anaesthesia and emergency medicine with no prior training in cardiology or echocardiography were invited to participate. Participation was voluntary and consecutive enrolment performed until the desired sample size was achieved. Ethical approval was granted by the Aga Khan University Institutional Ethics Review Committee (IERC) prior to commencement (Ref. 2018/RE-58), and written informed consent obtained from all participants.
The FoCUS curriculum selected for this study was the basic Focus Assessed Transthoracic Echocardiography (FATE) protocol, practiced since 1989 and endorsed by professional societies in South Africa, North America and Europe [11]. The protocol consists of six FoCUS views in the following order: subcostal, apical 4-chamber, parasternal long axis (PLAX), parasternal short axis (PSAX) and pleural scanning (see Supplementary material). FATE training materials are made available by the USabcd (Ultrasound Blood Circulation Dolor) centre (Risskov, Denmark) [12], which also offers training to countries outside Europe via a combination of self-directed e-learning and hands-on workshops. Initial workshops in non-accredited centres seeking to become accredited for FATE training are supervised by a USabcd Chief Instructor, a condition for which is the payment of honoraria and the meeting of attendant travel costs. We selected this particular FoCUS curriculum because FATE trainings, under the tutelage of trainers from South Africa, have grown increasingly popular in Kenya in recent years and because we sought to become an accredited centre for this training [13]. Additionally, its brief curriculum would not require significant time commitment from our target clinicians.
Conduct of the study
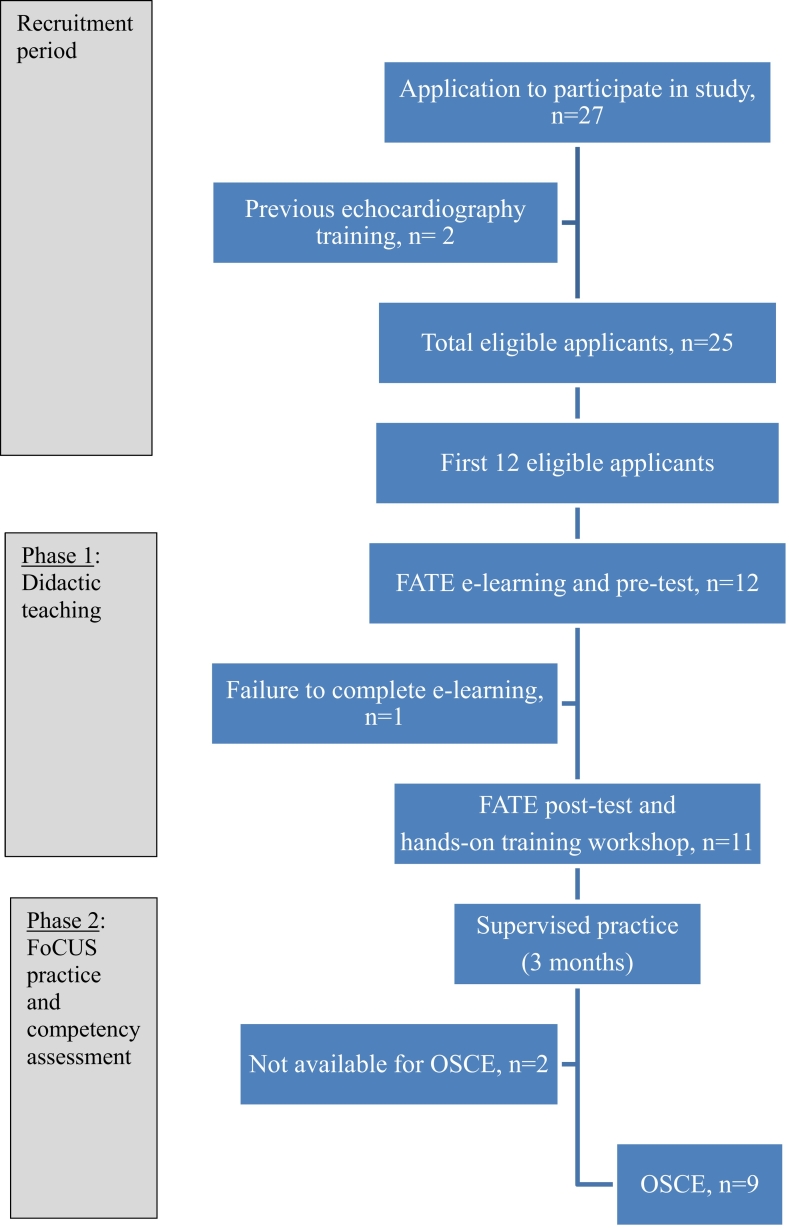
The study was conducted in two phases (Fig. 1).
Fig. 1.
Study flow diagram.
Key: FATE, Focus Assessed Transthoracic Echocardiography; OSCE, Observed Structured Clinical Examination; FoCUS, focused cardiac ultrasound.
Phase 1: Didactic teaching
This involved online FATE e-learning followed a month later by a hands-on workshop.
Online e-learning
FATE e-learning consisted of two interactive, modular sections: one on basic cardiac ultrasound and the other on basic ultrasound physics, proprietary material only accessible to learners following the payment of a subscription fee. The USabcd waived this fee for our study. Each section had a multiple-choice question (MCQ) pre-test to assess knowledge of basic FATE views, M-mode, cardiac function and pathology. Following completion, online post-test MCQs were administered.
Hands-on training workshop
Progression to the one-day workshop held at the General Electric (GE) training centre in Nairobi was limited to participants who had completed the e-learning. Equipment available was the Vivid iq®, LOGIQ e® and LOGIQ F8® ultrasound machines (GE Healthcare), each with a 3sc-Rs (1.5–4 MHz) sector array transducer. Novices in groups of four scanned healthy volunteers, rotating through three stations manned by FATE trainers, an emergency physician with Level 1 EMSSA ultrasound training, a cardiologist and a USabcd Chief Instructor. Each novice performed up to six supervised scans, before undergoing a brief vignette-based assessment.
Phase 2. FoCUS practice and competency assessment
Over a period of three months, novice scanners were expected to perform 10 supervised scans and to save another 10 for off-line review and feedback, as outlined in the FATE curriculum. A research assistant identified potential patients for practice scans, obtaining informed consent from them or a proxy before novice scans were performed. The WhatsApp® mobile application facilitated communication between novices, trainers and the research assistant. A Philips Lumify® handheld ultrasound machine with an S4-1 broadband sector array probe was available for practice. The hospital portable echocardiography machine, a Vivid iq ® (GE Healthcare), was also available where a formal echocardiogram had been requested on clinical grounds, and the hospital cardiac sonographer was willing to supervise a brief period of novice scanning. Logbooks were submitted for review at the end of the study. Novices who did not maintain a formal logbook were contacted directly at study closeout for feedback regarding total number of scans performed and the proportion of these that were supervised. Novice feedback summarising the entire training experience and challenges faced was also requested.
OSCE format
At the end of the three months, an OSCE was conducted. Of the 45 patients who were in the general medical ward and high dependency unit (HDU) at the time, 25 were selected by simple randomisation, nine of whom gave consent to participate and were recruited into the study. The study expert performed FoCUS examinations on these patients, documenting his findings on a structured form (see Supplementary material). Each novice then performed a FoCUS examination on three randomly selected patients from this patient pool, as trainers assigned scores for probe position, probe orientation, identification of anatomy, image interpretation and image quality (see Supplementary material). Expert and novice scans were limited to 10 min each and took place within an hour of each other. At the end of the FoCUS exam, novices summarised their findings by documenting the presence or absence of seven possible FoCUS target conditions, i.e. reduced ejection fraction, hyperdynamic contractility, right ventricular dilatation, pericardial effusion, left sided pleural effusion, right-sided pleural effusion or a normal scan (see Supplementary material). The Philips Lumify® handheld ultrasound machine was used by both expert and novices, and de-identified images recorded. A second, blinded study expert, a cardiologist evaluated the quality of these images.
Statistical analysis
Twelve novices were required to give the study 90% power to detect a 20% difference in knowledge between the pre- and post-test assessments, assuming a standard deviation of 15% in both tests, a two-sided alpha of 0.05 and a confidence interval of 95% [14]. Simple descriptive statistics were used to summarize novice baseline demographics and pre- and post-test responses. Descriptive analysis was performed, and count variables reported using means, medians, interquartile ranges and 95% confidence intervals. Pre- and post-training numerical scores were compared using the Wilcoxon signed-rank test to assess whether the median of the difference in pre- and post-test scores was different than zero. Inter-rater agreement between expert and novice scans, and of the assessments of image quality between the FATE trainers and the blinded expert, were assessed using Cohen's kappa statistic, with a value >0.6 taken as indicative of good inter-rater agreement [15]. Chi-squared tests were used to test for association between novice performance (pretest scores, knowledge gain, image quality and inter-rater agreement with expert scans) and department, previous ultrasound use and number of post-workshop supervised scans. Logistic regression analysis was used to adjust for cadre and gender. Statistical significance was set at 0.05 for all tests. Statistical analyses were performed using STATA version 14.2 (StataCorp LP, Texas, USA).
Results
The study was conducted between July and November 2018. Twenty-seven doctors from the departments of anaesthesia, critical care and emergency medicine at AKUHN applied to participate in the study, and the first 12 of those eligible were enrolled (Fig. 1).
The final cohort of 12 was predominantly female (n = 8, 66.7%), consisting mainly of senior house officers (n = 6, 50%) who were occasional users of ultrasound (n = 9, 75%). The majority were from the emergency department (n = 4, 33.3%) and critical care (n = 5, 41.7%).
Eleven (91.7%) of the 12 novices completed the FATE e-learning and proceeded to the hands-on training workshop.
The median pre-test score was 58.7% (SD 13.9, IQR 51–69), with a post-test median of 97.3% (SD 3.5, IQR 94–99), a knowledge gain of 37.7% (Table 1). The median of the difference between pre-and post-test scores was statistically significant (z = 2.934, p = 0.001).
Table 1.
FATE e-learning scores.
| Range (%) | IQR (%) | Mean (%) (95% CI) |
SD | Median (%) | |
|---|---|---|---|---|---|
| Test 1 (basic cardiac ultrasound), n = 12 | |||||
| Pre-test scores | 31–89 | 43–79 | 59.0 (46.6, 71.3) | 19.4 | 60.0 |
| Post-test scores | 91–100 | 95–100 | 97.2 (95.1, 99.2) | 3.1 | 98.8 |
| Test 2 (basic ultrasound physics), n = 11 | |||||
| Pre-test scores | 41–79 | 51–68 | 60.3 (53.0, 67.6) | 10.8 | 62.5 |
| Post-test scores | 83–100 | 96–98 | 95.7 (92.1, 99.3) | 5.3 | 98.3 |
| Test 1 + test 2 average, n = 11 | |||||
| Pre-test scores | 36–80 | 51–69 | 59 (49.4, 68.0) | 13.9 | 58.7 |
| Post-test scores | 89–100 | 94–99 | 97 (94.1, 98.7) | 3.5 | 97.3 |
| Knowledge gain, n = 11 | |||||
| Knowledge gain_test1 | 12–69 | 21–58 | 40 (27.3, 52.7) | 18.9 | 44 |
| Knowledge gain_test2 | 20–56 | 21–47 | 35 (27.1, 43.7) | 12.4 | 34 |
| Overall knowledge gain | 16–58 | 30–47 | 37.7 (28.3, 47.1) | 14 | 35.9 |
CI, confidence interval; IQR, interquartile range; SD, standard deviation.
Pre-test scores were higher for doctors from critical care (median 71.2%, SD 5.3, IQR 69.2–76.7), compared to those from A&E (median 51.2%, SD 9.4, IQR 43.3–55.4) and anaesthesia (median 51.1%, SD 11.9, IQR 41–64.7). This difference however was not statistically significant (chi = 22, p = 0.341). Analysis of pretest scores by department based on the basic cardiac ultrasound pre-test score taken by all 12 participants also did not achieve statistical significance (chi 24, p = 0.155). There was also no association between pre-test scores and gender or previous ultrasound use.
Post-workshop practice
Novices reported varying degrees of FoCUS practice during the three-month period (range 0–30 scans, mean 15.5, median 7), with three (33%) of the nine who did practice maintaining a logbook. Logbook entries ranged from 10 to 11 practice scans, an average of 2 or 3 of which were supervised (20–27%) per novice. A total of 96 logged and self-reported practice scans were performed in total, 26 (27%) of which were supervised, eleven (42%) by hospital cardiac sonographers. The proportion of supervised scans overall ranged from 0 to 93.3% (mean 22, median 10, IQR 0–29). Reasons given by nine novices who provided feedback for lack of supervised practice included difficulty integrating supervised practice with patient care in a busy clinical setting (n = 3, 33.3%), inability to harmonise novice and trainer schedules in-hours (n = 2, 22.2%) and out-of-hours shift working patterns for novices when trainers were no longer on site (n = 3, 33.3%).
FoCUS competency assessment
Nine of eleven novices were available to participate in the OSCE on the day it was held. Twenty-seven independent novice studies were performed on seven of the nine patients who gave consent to participate, each consisting of the six FATE views. Between 16 and 18 FATE views were generated per novice. For ten (6%) of 162 possible FATE views, an image was not obtained as the novice was unable to complete the scan within the 10 min assigned.
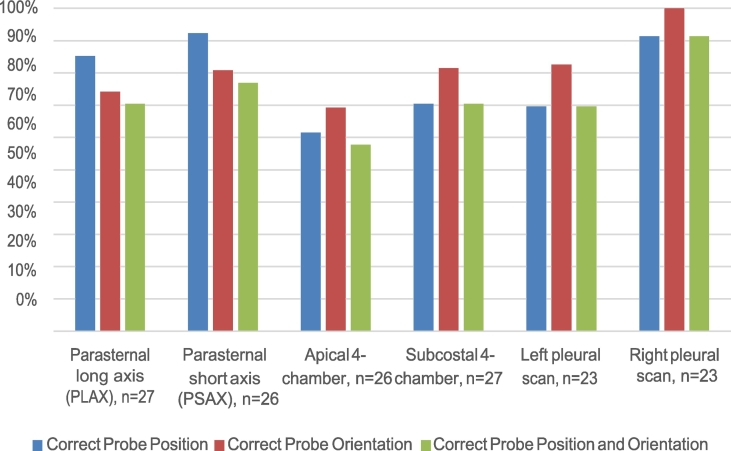
Novice probe position and orientation
The highest proportion of novice scans with correct probe position and probe orientation of the 152 performed were right pleural scans (n = 21/23, 91.3%), PSAX (n = 20/26, 76.9%), PLAX (n = 19/27, 70.4%) and subcostal 4-chamber views (n = 19/27, 70.4%), as shown in Fig. 2. The apical 4-chamber view had the lowest proportion of correctly positioned and oriented probes (n = 15/26, 57.7%).
Fig. 2.
Novice probe position and orientation, n = 152.
Key: PLAX Parasternal long axis; PSAX Parasternal short axis; Ap4-Ch Apical 4-Chamber; SC4-Ch Subcostal 4-Chamber; LPS Left pleural scan; RPS Right pleural scan.
Image interpretation
Novices correctly interpreted anatomical structures in 116 (76.3%) of 152 images generated. Good image interpretation scores (scores ≥2) were noted for right pleural scans (n = 21/23, 91.3%), the PLAX (n = 23/27, 85.2%) and apical 4-chamber views (n = 22/26, 84.6%), while the subcostal 4-chamber view had the lowest proportion of correctly interpreted images (n = 16/27, 59.3%).
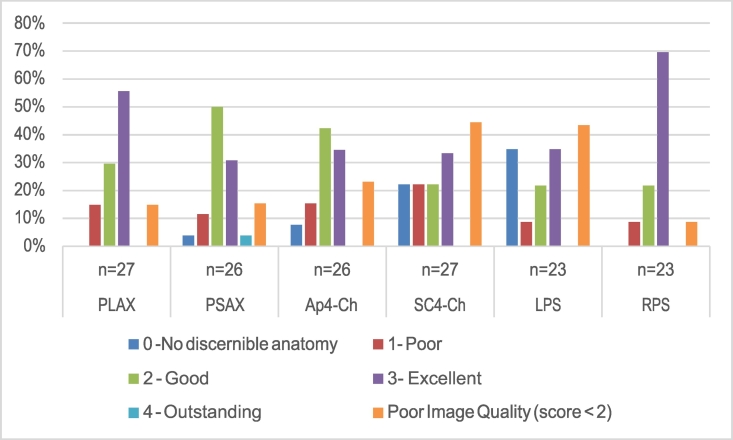
Image quality
A total of 37 (24.3%) of 152 novice images received a score of < 2 for image quality during the OSCE, while 115 (75.7%) were rated as good. The subcostal 4-chamber view and left pleural scan had the largest proportion of poor-quality images at 44.4% (n = 12/27) and 43.5% (n = 10/23) respectively (Fig. 3). When the marks awarded for the variables assessed during the OSCE were averaged, the best performed view was the right pleural scan, followed by the parasternal views (PLAX and PSAX).
Fig. 3.
Novice image quality, n = 152.
Key: PLAX Parasternal long axis; PSAX Parasternal short axis; Ap4-Ch Apical 4-Chamber; SC4-Ch Subcostal 4-Chamber; LPS Left pleural scan; RPS Right pleural scan.
Comparative scoring of image quality
A total of 138 of the 152 novice images obtained during the OSCE were recorded. These, together with the 42 generated by the study expert, were reviewed by a second, blinded expert. Of these, 90 (50%) were rated as poor quality (score < 2), with 15 (35.7%) of 42 expert images and 75 (54.4%) of 152 novice images receiving this score. This difference was statistically significant (Pearson chi 4.47, p = 0.03). Overall, 82 (59.4%) of 138 novice scans were considered poor quality by both experts, with fair inter-rater agreement (agreement 58.7%, kappa 0.21, SE 0.07, p = 0.01).
Diagnostic accuracy of novice FoCUS
Novices correctly identified one of seven possible FoCUS target conditions as absent in 114 (79.2%) of 144 scans and identified findings as present in 23 (51.1%) of 45 scans (Table 2). Specificity of novice FoCUS was highest for hyperdynamic contractility while sensitivity was highest for reduced ejection fraction. Overall, the specificity and negative predictive value of novice FoCUS were higher than its sensitivity and positive predictive value.
Table 2.
Diagnostic accuracy of novice FoCUS by target condition.
| FoCUS target condition |
Diagnostic accuracy of novice FoCUS |
|||||
|---|---|---|---|---|---|---|
| Target condition | True positives (no. %) |
True negatives (no. %) |
Sensitivity (no. %) |
Specificity (no. %) |
PPV (%) | NPV (%) |
| Reduced ejection fraction | 13/27 (48.2) | 14/27 (51.9) | 10/13 (76.9) | 8/14 (57.1) | 62.5 | 72.7 |
| Hyperdynamic contractility | 0 (0.0) | 27/27 (100.0) | NA | 26/27 (96.3) | NA | 100.0 |
| Right ventricular dilatation | 4/27 (14.8) | 23/27 (85.2) | 2/4 (50.0) | 17/23 (73.9) | 25.0 | 89.5 |
| Pericardial effusion | 5/27 (18.5) | 22/27 (81.5) | 2/5 (40.0) | 19/22 (86.4) | 40.0 | 86.4 |
| Left pleural effusion | 5/27 (18.5) | 22/27 (81.5) | 2/5 (40.0) | 16/22 (72.7) | 25.0 | 84.2 |
| Right pleural effusion | 5/27 (18.5) | 22/27 (81.5) | 0/5 (0.0) | 18/22 (81.8) | 0.0 | 78.3 |
| Normal scan | 13/27 (48.2) | 14/27 (51.8) | 7/13 (53.9) | 10/14 (71.4) | 63.6 | 62.5 |
PPV = positive predictive value; NPV = negative predictive value; NA = not applicable.
Inter-rater agreement between expert and novice FoCUS
Inter-rater agreement between expert and novice scans for most FoCUS target conditions was high, with a Cohen's kappa ranging between 0.7 and 0.96, denoting substantial to almost perfect agreement (Table 3). The lowest interrater agreement was found for pleural effusions, with a kappa of 0.06, p < 0.001. There was no association between inter-rater agreement and novice cadre, department, and number of practice scans performed or maintenance of a logbook.
Table 3.
Interrater agreement between novice and expert scans by FoCUS target.
| FoCUS target | Agreement | Cohen's kappa | Standard error | z-Statistic | p-Value |
|---|---|---|---|---|---|
| Reduced ejection fraction | 83.3% | 0.73 | 0.1 | 7.47 | <0.001 |
| Hyperdynamic contractility | 98.2% | 0.96 | 0.13 | 7.28 | <0.001 |
| Right ventricular dilatation | 85.2% | 0.75 | 0.11 | 6.92 | <0.001 |
| Pleural effusion | 9.26% | 0.06 | 0.02 | 3.13 | <0.001 |
| Pericardial effusion | 87.0% | 0.77 | 0.11 | 6.77 | <0.001 |
| Normal scan | 81.5% | 0.70 | 0.10 | 7.09 | <0.001 |
Discussion
We performed this study to assess the ability of novices in low and middle-income countries (LMICs) to perform focused cardiac ultrasound (FoCUS) following a brief period of training, in an attempt to mitigate the shortage of echocardiography experts in our setting. Our objective was to identify a curriculum that is easy to teach and implement, that confers an acceptable level of competence in FoCUS within a brief period. We found however that the shortage of echocardiography experts in our country is also a major stumbling block in our attempts to build capacity in FoCUS, as supervised practice is difficult to achieve without them. Our findings support the idea that there is a discordance between knowledge and application of FoCUS in LMICs following brief trainings.
The knowledge gain observed following a month of online e-learning was higher than expected, suggesting that the quality of the FATE curriculum is high. The proportion of good quality novice images in our study was significantly lower however than has been found from similar work [14,16,17]. Additionally, novices were better able to correctly identify the presence of an abnormal scan than they were to confirm the presence of a normal one. Lack of confidence due to inadequate supervised practice may have contributed to these findings. Our findings lend credence to the recommendation that a formal echocardiogram by an expert should be performed as soon as possible even where a novice has already performed a FoCUS examination [5,9 18]. FoCUS trainings in LMICs should in the meantime perhaps lay emphasis on good image acquisition by novices rather than interpretation, with remote image interpretation supported by experts via cloud-based platforms [18]. The challenge of irregular power supply and inadequate internet data networks in LMICs would however need to be addressed.
Interrater agreement between novice and expert scans for FoCUS target conditions was substantial, perhaps due to the high specificity of novice FoCUS in a patient population with predominantly negative findings. The significant proportion of patients who declined to participate and the subsequently low prevalence of pathology in those who agreed to may have contributed to this finding. This reluctance to participate in clinical research is likely because we are a private institution with patients who are managed by specific physicians. Our request to involve these patients in clinical research therefore may have been viewed with suspicion. Where FoCUS training and evaluation efforts are hampered by the lack of a sufficient patient pool with identifiable pathology for training purposes, or otherwise need to be supported, simulation has been found to be a suitable alternative [19],[20],[21].
That insufficient supervised practice leads to poor performance in FoCUS is not surprising as this is well-established [9]. The difficulties we faced ensuring supervised FoCUS practice in our setting were unexpected however, as a lot of effort had gone into ensuring the availability of equipment and enhancing communication between novices and trainers. Post-workshop supervised practice was significantly hampered by scheduling difficulties between novices and trainers, all of whom had clinical care responsibilities. Nevertheless, the ideal number of practice scans necessary to achieve competency in FoCUS is still a matter of contention [22]. While the 2018 EACVI consensus document recommends a minimum of 50 practice scans [9], the FATE curriculum that we followed recommends 20, ten of which must be supervised. Irrespective of the guidelines followed however, ongoing exposure to FoCUS following brief trainings in LMICs must be ensured, to improve the accuracy of novice scanners in these settings.
To increase the capacity of novices in LMICs to perform FoCUS, the focal point of training initiatives should be the training of trainers, to maximise the benefit of subsequent training efforts. Clinicians who have undergone brief trainings should be freed up to regularly engage with FoCUS, to develop competence. Consideration should be given to the creation of locally accessible FoCUS curricula, eliminating the costs associated with the use of proprietary material. Incorporation of point-of-care-ultrasound into undergraduate medical school curricula would facilitate the acquisition of FoCUS skills by the next generation of clinicians in LMICs and should be encouraged. National cardiac and critical care societies should be involved from the outset, to provide oversight. Regional and international collaborative efforts should be encouraged, to provide support during this period of capacity building in LMICs, where experts are in short supply. Enhanced online learning, and remote supervision via telemedicine and available cloud-based platforms, should be explored as possible solutions to the supervision challenge.
We identified a number of barriers to the scaling up of FoCUS training programmes in a LMIC such as ours. These include the costs associated with accessing proprietary FoCUS training material and of having trainers from accredited programmes oversee trainings locally, difficulties accessing dedicated ultrasound equipment and an inadequate number of trainers for supervised practice. Of these, the human resource element will require the most thought to overcome, as the shortage of experts in LMICs that makes FoCUS training for novices necessary is also a significant barrier to its successful implementation. A more formal analysis of feasibility of scaling up FoCUS training is in order, should a revised programme yield more consistent results between experts and novices.
The use of a handheld ultrasound device (HUD) may have influenced our results. While HUDs are capable of providing reasonably good imaging and functional assessments, a 2018 EACVI position statement highlighted inherent limitations in the use of HUDs for FoCUS, including the reduction in diagnostic accuracy in the hands of inexperienced operators 18]. We were however unable to obtain a dedicated full-functionality machine for supervised practice. Secondly, three months may have been too short to expect novices to have gained competence in FoCUS. However, we are a busy institution with many opportunities for FoCUS practice in our clinical areas. It is therefore unlikely that the difficulties that led to limited supervised practice would have improved with time. Thirdly, we based our reference standard on only one expert and did not capture patient factors that could have contributed to some of the poor quality views obtained. Although this was a small study, the quality of our initial training was high and our assessment of novice competence objective. Our results are therefore robust, and informative for other LMICs that would like to scale up FoCUS trainings within their boundaries.
Conclusion
Our study demonstrates that while knowledge gain is high following a brief period of training in FoCUS, novice FoCUS image quality is poor and sensitivity low when supervised practice is not assured. In spite of this, substantial agreement between novice and expert scans for FoCUS target conditions is observed when the prevalence of pathology is low. Supervised FoCUS practice is challenging to achieve in a real-world setting in LMICs, undermining the effectiveness of training initiatives. Emphasis should be placed on the training of trainers, remote supervision and the provision of opportunities for regular practice, without which FoCUS training in LMICs may be an exercise in futility.
Dissemination of Results
The results of this study were shared with study participants through an informal presentation.
Authors’ Contribution
Authors contributed as follows to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content: WW contributed 40%; AB 15%; BW 10%; DN, BK, FJ, GW, HO, GSB and ES contributed 5% each. All authors approved the version to be published and agreed to be accountable for all aspects of the work.
Declaration of Competing Interests
Dr Benjamin Wachira is an editor of the African Journal of Emergency Medicine. Dr Wachira was not involved in the editorial workflow for this manuscript. The African Journal of Emergency Medicine applies a double blinded process for all manuscript peer reviews. This study was supported by the Aga Khan University Research Council (URC) grant number 181010ANES-EA. The Lumify handheld ultrasound device used for the study was loaned to the study team by Philips. The USabcd waived subscription fees for the FATE e-learning material. Professor Erik Sloth is a co-founder of the USabcd ApS that provided the FATE training materials for the study. Neither the USabcd, nor Philips or the URC had any influence on study design, the collection, analysis and interpretation of data, the writing of the report, or in the decision to submit the article for publication. The authors declared no further conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.afjem.2020.04.011.
Appendix A. Supplementary data
FATE Protocol Scanning Guide
References
- 1.Becker T.K., Tafoya C.A., Osei-Ampofo M., Tafoya M.J., Kessler R.A., Theyyunni N. Cardiopulmonary ultrasound for critically ill adults improves diagnostic accuracy in a resource-limited setting: the AFRICA trial. Trop Med Int Health. 2017;22(12):1599–1608. doi: 10.1111/tmi.12992. [DOI] [PubMed] [Google Scholar]
- 2.Council KMPaD . 2019. Online registers. [Google Scholar]
- 3.Heiberg J., El-Ansary D., Canty D.J., Royse A.G., Royse C.F. Focused echocardiography: a systematic review of diagnostic and clinical decision-making in anaesthesia and critical care. Anaesthesia. 2016;71(9):1091–1100. doi: 10.1111/anae.13525. [DOI] [PubMed] [Google Scholar]
- 4.Acar Y., Tezel O., Salman N., Cevik E., Algaba-Montes M., Oviedo-Garcia A. 12th WINFOCUS world congress on ultrasound in emergency and critical care. Crit Ultrasound J. 2016;8(Suppl. 1):12. doi: 10.1186/s13089-016-0046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Via G., Hussain A., Wells M., Reardon R., ElBarbary M., Noble V.E. International evidence-based recommendations for focused cardiac ultrasound. J Am Soc Echocardiogr. 2014;27(7):683 e1–e33. doi: 10.1016/j.echo.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 6.Stachura M., Landes M., Aklilu F., Venugopal R., Hunchak C., Berman S. Evaluation of a point-of-care ultrasound scan list in a resource-limited emergency centre in Addis Ababa Ethiopia. Afr J Emerg Med. 2017;7(3):118–123. doi: 10.1016/j.afjem.2017.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Atkinson P.R., Milne J., Diegelmann L., Lamprecht H., Stander M., Lussier D. Does point-of-care ultrasonography improve clinical outcomes in emergency department patients with undifferentiated hypotension? An international randomized controlled trial from the SHoC-ED investigators. Ann Emerg Med. 2018;72(4):478–489. doi: 10.1016/j.annemergmed.2018.04.002. [DOI] [PubMed] [Google Scholar]
- 8.Becker D.M., Tafoya C.A., Becker S.L., Kruger G.H., Tafoya M.J., Becker T.K. The use of portable ultrasound devices in low and middle-income countries: a systematic review of the literature. Trop Med Int Health. 2016;21(3):294–311. doi: 10.1111/tmi.12657. [DOI] [PubMed] [Google Scholar]
- 9.Neskovic A.N., Skinner H., Price S., Via G., De Hert S., Stankovic I. Focus cardiac ultrasound core curriculum and core syllabus of the European Association of Cardiovascular Imaging. European Heart Journal-Cardiovascular Imaging. 2018;19:475–481. doi: 10.1093/ehjci/jey006. [DOI] [PubMed] [Google Scholar]
- 10.The Aga Khan University Hospital Nairobi: About Us 2019. https://hospitals.aku.edu/nairobi/AboutUs/Pages/OurProfile.aspx Available from.
- 11.USabcd Basic cardiac ultrasound (FATE) https://usabcd.org/product/basic-cardiac-ultrasound-fate/ Available from.
- 12.USabcd USabcd: about us: USabcd ApS. https://usabcd.org/about-us/ Available from.
- 13.Kenya CCSo Focus assessed transthoracic echocardiography. 2018. https://criticalcarekenya.co.ke/events/focus-assessed-transthoracic-echocardiography Available from.
- 14.Frederiksen C.A., Juhl-Olsen P., Nielsen D.G., Eika B., Sloth E. Limited intervention improves technical skill in focus assessed transthoracic echocardiography among novice examiners. BMC Med Educ. 2012;12:65. doi: 10.1186/1472-6920-12-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Landis J.R., Koch G.G. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 16.Mark D.G., Ku B.S., Carr B.G., Everett W.W., Okusanya O., Horan A. Directed bedside transthoracic echocardiography: preferred cardiac window for left ventricular ejection fraction estimation in critically ill patients. Am J Emerg Med. 2007;25(8):894–900. doi: 10.1016/j.ajem.2007.01.023. [DOI] [PubMed] [Google Scholar]
- 17.Andruszkiewicz P., Sobczyk D., Gorkiewicz-Kot I., Kowalik I., Gelo R., Stach O. Reliability of focused cardiac ultrasound by novice sonographer in preoperative anaesthetic assessment: an observational study. Cardiovasc Ultrasound. 2015;13:45. doi: 10.1186/s12947-015-0039-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cardim N., Dalen H., Voigt J.-U., Ionescu A., Price S., Neskovic A.N. The use of handheld ultrasound devices: a position statement of the European Association of Cardiovascular Imaging (2018 update) Eur Heart J Cardiovasc Imaging. 2019;20(3):245–252. doi: 10.1093/ehjci/jey145. [DOI] [PubMed] [Google Scholar]
- 19.Reacts. Reacts for remote ultrasound training and supervision.
- 20.Wilson J., Ng L., Browne V., Lewiss R.E. An easy-to-make, low-cost ultrasound phantom for simulation training in abscess identification and aspiration. J Ultrasound Med. 2017;36(6):1241–1244. doi: 10.7863/ultra.16.04077. [DOI] [PubMed] [Google Scholar]
- 21.Lewiss R.E., Hoffmann B., Beaulieu Y., Phelan M.B. Point-of-care ultrasound education: the increasing role of simulation and multimedia resources. J Ultrasound Med. 2014;33(1):27–32. doi: 10.7863/ultra.33.1.27. [DOI] [PubMed] [Google Scholar]
- 22.Bowcock E.M., Morris I.S., McLean A.S., Orde S.R. Basic critical care echocardiography: how many studies equate to competence? A pilot study using high fidelity echocardiography simulation. J Intensive Care Soc. 2017;18(3):198–205. doi: 10.1177/1751143717700166. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
FATE Protocol Scanning Guide