Abstract
Background
During telephone triage, it is difficult to assign adequate urgency to patients with chest discomfort. Considering the time of calling could be helpful.
Objective
To assess the risk of acute coronary syndrome (ACS) in certain time periods and whether sex influences this risk.
Methods
Cross-sectional study of 1655 recordings of telephone conversations of patients who called the out-of-hours services primary care (OHS-PC) for chest discomfort. Call time, patient characteristics, symptoms, medical history and urgency allocation of the triage conversations were collected. The final diagnosis of each call was retrieved at the patient’s general practice. Absolute numbers of patients with and without ACS were plotted and risks per hour were calculated. The risk ratio of ACS at night (0 to 9 am) was calculated by comparing to the risk at other hours and was adjusted for gender and age.
Results
The mean age of callers was 58.9 (standard deviation ±19.5) years, 55.5% were women and, in total, 199 (12.0%) had an ACS. The crude risk ratio for an ACS at night was 1.80 (confidence interval 1.39–2.34, P < 0.001): 2.33 (1.68–3.22, P < 0.001) for men and 1.29 (0.83–1.99, P = 0.256) for women. The adjusted risk ratio for ACS of all people at night was 1.82 (1.07–3.10, P = 0.039).
Conclusions
Patients calling the OHS-PC for chest discomfort between 0 and 9 am have almost twice a higher risk of ACS than those calling other hours, a phenomenon more evident in men than in women. At night, dispatching ambulances more ‘straightaway’ could be considered for these patients with chest discomfort.
Trial number
NTR7331.
Keywords: Acute coronary syndrome, chest pain, primary health care, risk, time, triage
Key messages.
Risk of acute coronary syndrome in out-of-hours services primary care is twice as high at night compared to daytime.
This effect was evident in men but not significant in women.
Triage may be improved in both safety and efficiency applying this knowledge.
Background
Adequate triage of patients with chest discomfort and timely diagnosis of those with acute coronary syndrome (ACS) is crucial for initiation of lifesaving early interventions in order to prevent or reduce myocardial necrosis (‘time is muscle’) and, thus, improve outcome and prognosis (1). Urgency allocation of patients with chest discomfort based on telephone triage as done in out-of-hours services for primary care (OHS-PC) and emergency medical dispatch centres is, however, challenging because it is very difficult to differentiate ACS from other reasons for chest discomfort. For the diagnosis of ACS, an abnormal electrocardiogram [repolarization abnormalities (ST and/or T wave)] and/or elevated blood levels of troponin I or T are needed. ACS may then be further subdivided into ST-elevated myocardial infarction (STEMI) and non-ST-elevated myocardial infarction (NSTEMI) if the troponin levels are elevated (2). If troponin levels are not elevated (or increased over time), it is called unstable angina pectoris (UAP) (2).
In the Netherlands, around 80% of patients with chest pain first call the general practitioner (GP) or OHS-PC, while 20% directly call the ambulance (112) or are self-referrals (3). In the 20% who called directly the emergency medical dispatch centre, 63% received a Priority 1 ambulance and 10% had an ACS (4). In people who first called the OHS-PC, 70% received a Priority 1 ambulance and also 10% had an ACS (5–7).
Previous studies in the emergency department setting showed circadian variability in the occurrence of acute coronary events, with early morning peak, which was twice as high as in the evening (8–10). This early morning peak of acute myocardial infarction is considered related to physiological changes in these hours, such as a rise in blood pressure and plasma adrenaline levels, that could possibly trigger plaque rupture and thrombosis (8,9,11). Studies in primary care setting are lacking and studies dividing the absolute numbers of ACS by the number of patients who contacted because of chest pain are limited (11). Also, studies about sex differences in the circadian rhythm of ACS are limited. If there were a high incidence of ACS relative to the number of callers for chest discomfort during certain hours, this would facilitate triage at the OHS-PC.
In the Netherlands, the OHS-PC is organized in large services, similar to the UK and Scandinavian countries (12). Dutch triage nurses use the Netherlands Triage Standard (NTS) to assess the urgency and use five priority levels related to the time within which the patients should be seen. The NTS is a semi-automatic computerized decision support system that is based on the Manchester Triage Standard (13). Previous studies showed that chest discomfort is the most common reason (60.7%) for allocating the highest priority (U1; ambulance dispatched, the patient should be seen within 15 minutes) for those contacting the OHS-PC. In the second place came respiratory tract symptoms with just 8.1% ambulances dispatched (7). The Dutch triage system is overall safe with only 0.006% calamities a year, but this incidence is higher with around 0.03% in the domain of chest discomfort (14,15). Besides safety, also efficiency could very likely be improved in the domain chest discomfort because only 1 out of 10 of the referred patients actually has an ACS (5–7,14).
For better safety and efficiency, there is an urgent need for determinants that improve prediction and, thus, help triage nurses in their task (7). If there are hours with a high incidence of ACS as compared to the total number of telephone calls, then considering the time of calling could help to improve the triage. Therefore, we assessed whether there are certain time periods in which there is a higher risk ratio of ACS and whether sex differences influence this risk ratio.
Methods
The study design and data collection are published before in our study design paper (15). In short, we performed a cross-sectional study with a random sample of 1655 calls of people calling the OHS-PC for chest discomfort between 2014 and 2016. We selected calls on the basis of International Classification for Primary Care codes (K01, K02, K03, K24, K74, K75, K76, K77, K93, L04, P74, R02 and R98) and keywords (thoracic pain, chest pain, myocardial infarction, heart attack and their common abbreviations). On purpose, we sampled broadly to capture the entire domain of patients that could be suspected of ACS. We drew a random sample of all available calls of these patients (270 000 between 2014 and 2016) with the Random Number Generator (RAND) function in Microsoft Excel.
We re-listened telephone triage recordings in order to collect information about the characteristics of patients and their conversation on symptoms, medical history, urgency allocation and whether a supervising GP was involved in the triage. Nine OHS-PC in the Netherlands participated, serving a total population of 1.5 million people. The final diagnoses were provided by the patients’ GP, and this was based on the electronic medical file and cardiologist discharge letters. An ACS was based on the cardiologist’s diagnosis, including information on levels of (high sensitivity) troponin and electrocardiography.
In the OHS-PC, trained triage nurses used the NTS to generate an urgency allocation. The NTS is hierarchically ordered with key questions, and answers are linked to urgency recommendations. Linked to the nurse’s urgency allocation is the time frame within which a physician should see the patient (16): direct, within 15 minutes [by ambulance or GP (U1)]; urgently, within 1 hour (U2); less urgent, within 3 hours (U3); non-urgent, the same day (U4) or telephone advice (U5). The GP may see the patient at the patient’s home or at the OHS-PC. Triage nurses can always consult the supervising GP on call (17).
Data analyses
We plotted the absolute numbers of patients calling for chest discomfort hourly, subdivided into patients with and without a final diagnosis ACS, and we calculated the risks of ACS per hour by dividing the absolute number of ACS by the total number of callers with chest discomfort per hour. The risk ratio of ACS was calculated over several time periods. The aim was to find a time period in which the risk of ACS was high and also practical in use. We performed separate analyses for men and women and used the likelihood ratio test to assess the difference. Adjusted risk ratios for ACS were calculated after correction for gender and age below and over 40 years.
We compared patient and call characteristics and urgency allocation between callers at night and callers at other hours. For comparison of dichotomous variables, we used the Chi (2) test and, for continuous variables, the independent sample t-test. Finally, we compared the correlation between urgency allocation and the final diagnosis ACS. Data analysis was performed using SPSS, IBM version 21.
Results
Of the 1655 patients with chest discomfort, the mean age was 58.9 [standard deviation (SD) ±19.5] years, and 919 (55.5%) were women. In total, 199 (12.0%) had an ACS: 82 (8.9%) women and 117 (15.9%) men (P < 0.001); 41.7% an NSTEMI, 26.6% a STEMI, 24.1% UAP and 7.5% a non-classified ACS.
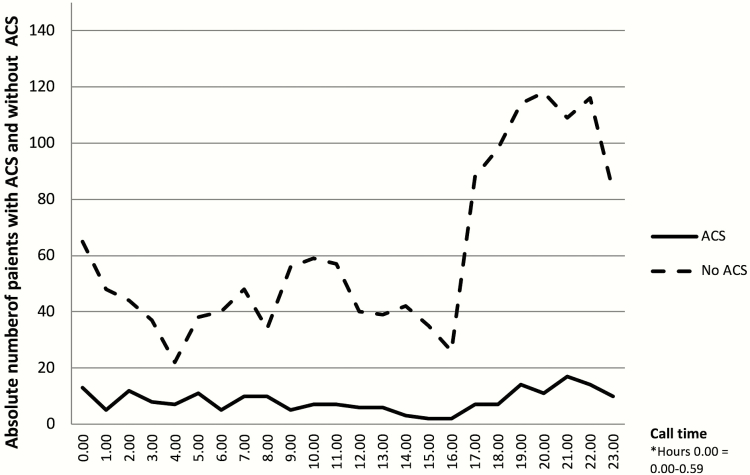
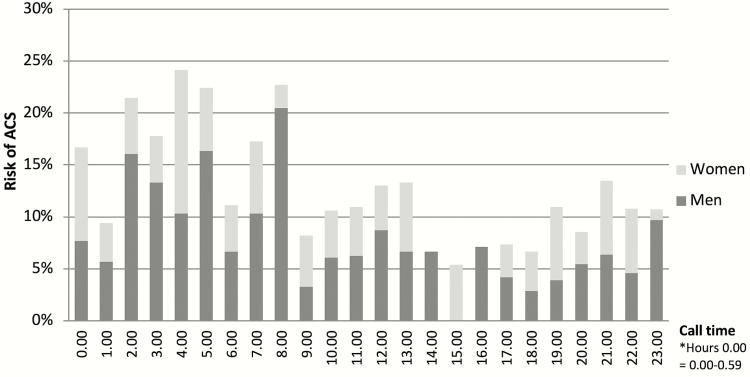
Variation was small in the absolute numbers of ACS during 24 hours (see Fig. 1). The incidence of ACS varied with a peak from 0 to 9 am of 17.7% compared to 9.8% at the remaining hours. The highest risk of ACS was between 2 and 5 am with 21.5%, and the lowest between 4 and 7 pm with 6.8%. In Figure 2, the distribution of risks for ACS per hour is plotted, subdivided for men and women. The risk ratio for an ACS from 0 to 9 am was 1.80 [confidence interval (CI) 1.39–2.34, P < 0.001] compared to other hours; for men, 2.33 (CI 1.68–3.22, P < 0.001) and, for women, 1.29 (CI 0.83–1.99, P = 0.256). The difference in risk ratios for men and women was statistically significant (P = 0.030). The adjusted risk ratio for ACS from 0 to 9 am compared to other hours was 1.82 (1.07–3.10, P < 0.001) after correction for both age and sex.
Figure 1.
Call time of 1655 patients with chest discomfort calling the OHS-PC between 2014 and 2016, subdivided into those with and without ACS. ACS: acute coronary syndrome. OHS-PC: out-of-hours services for primary care.
Figure 2.
Risk of ACS per hour of 1655 patients with chest discomfort calling the OHS-PC between 2014 and 2016, subdivided for men and women. ACS: acute coronary syndrome. OHS-PC: out-of-hours services for primary care.
The baseline characteristics for those calling at night and those calling at other hours are presented in Table 1. Patients calling between 0 and 9 am were significantly older [61.4 (SD ±19.7) years vs. 57.9 (±19.3) years, P = 0.001], had less patient decision delay (calling <12 hours after symptom onset, 83.1% vs. 70.4%, P < 0.001) and received more often the highest urgency 1 (54.5% vs. 42.1%, P < 0.001) than those calling at other hours.
Table 1.
Baseline characteristics of 1655 patients calling the OHS-PC with chest discomfort between 2014 and 2016, divided into those who called between 0 am and 9 am and other hours
| Total 1655 | 0 am–9 am No. (%) n = 457 | Other hours No. (%) n = 1198 | P-value | ||
|---|---|---|---|---|---|
| Patient characteristics | Mean age (SD) | 1655 | 61.4 (19.7) | 57.9 (19.3) | 0.001 |
| Male sex | 736 | 193/457 (42.2) | 543/1198 (45.3) | 0.759 | |
| Call characteristics | Call duration in minutes:seconds (SD) | 1655 | 7:02 (3:40) | 7:42 (3:47) | 0.001 |
| Medical history | Cardiovascular disease | 1350* | 227/365 (62.2) | 592/985 (60.1) | 0.485 |
| Coronary artery disease | 902* | 88/251 (35.1) | 225/651 (34.6) | 0.888 | |
| Hypertension | 701* | 70/188 (37.2) | 189/513 (36.8) | 0.924 | |
| Diabetes mellitus | 686* | 32/185 (17.3) | 89/501 (17.8) | 0.887 | |
| Symptoms | Chest pain | 1601* | 412/442 (93.2) | 1090/1159 (94.0) | 0.536 |
| Pain lasting <12 hours | 1438* | 320/385 (83.1) | 741/1053 (70.4) | <0.001 | |
| Radiation of pain | 1283* | 239/348 (68.7) | 593/935 (63.4) | 0.080 | |
| Autonomous nervous system related symptoms** | 1599* | 257/434 (59.2) | 658/1165 (56.5) | 0.325 | |
| Shortness of breath | 1260* | 214/333 (64.3) | 610/927 (65.8) | 0.612 | |
| GP participated in triage | In consultation or taking over the call | 1655 | 233/457 (51.0) | 650/1198 (54.3) | 0.233 |
| Urgency allocation | U1 | 753 | 249/457 (54.5) | 504/1198 (42.1) | <0.001*** |
| U2 | 371 | 85/457 (18.6) | 286/1198 (23.9) | ||
| U3,U4,U5 | 531 | 123/457 (26.9) | 408/1198 (34.1) | 0.005**** | |
| Diagnosis ACS | 1655 | 81/457(17.7) | 118/1198 (9.8) | <0.001 |
The bold values in the previous version of the tables were the statistically significant P-values.
*For these variables there were missing data.
**Autonomous nervous system (ANS) related symptoms consist of one or more of the following: nausea and/or vomiting, sweating, pallor/ashen skin, and (near) collapse.
***P-value comparing U1 vs. U2–U5.
****P-value comparing U1,U2 vs. U3–U5.
In Table 2, the correlations between urgency allocation and diagnosis of ACS are presented. Triage nurses dispatched significantly more ambulances to patients who turned out to have an ACS than no ACS (70.4% vs. 42.1%, P < 0.001) and this was more so at night (80.2% vs. 48.9%, P < 0.001).
Table 2.
Correlation between urgency allocation and final diagnosis ACS of 1655 patients with chest discomfort calling the OHS-PC between 2014 and 2016
| Total calls | ACS n = 199 (%) | No ACS n = 1456 (%) | P-value 1* | P-value 2** |
|---|---|---|---|---|
| U1 | 140 (70.3) | 613 (42.1) | <0.001 | <0.001 |
| U2 | 31 (15.6) | 340 (23.4) | ||
| U3, U4 and U5 | 28 (14.1) | 503 (34.5) | ||
| 0 am–9 am | ACS n = 81 (%) | No ACS n = 376 (%) | ||
| U1 | 65 (80.2) | 184 (48.9) | <0.001 | <0.001 |
| U2 | 11 (13.6) | 74 (19.7) | ||
| U3, U4 and U5 | 5 (6.2) | 118 (31.4) | ||
| Other hours | ACS n = 118 (%) | No ACS n = 1080 (%) | ||
| U1 | 75 (63.6) | 429 (39.7) | <0.001 | <0.001 |
| U2 | 20 (17.0) | 266 (24.6) | ||
| U3, U4 and U5 | 23 (19.4) | 385 (35.7) |
The bold values in the previous version of the tables were the statistically significant P-values.
*P-value 1: U1 vs. U2–U5.
**P-value 2: U1/U2 vs. U3–U5.
The final diagnoses of patients without ACS (n = 1456) were in 2.6% diseases that need urgent treatment (e.g. thoracic aortic dissection, acute severe heart failure, and pulmonary embolism) and in the remaining 85.4% non-urgent disorders (e.g. musculoskeletal, pulmonary, psychiatric or gastrointestinal causes).
Discussion
Patients with chest discomfort who called the OHS-PC between 0 and 9 am had almost twice as high a risk of an ACS than patients calling at other hours. This effect remained after adjustment for sex and age, but the risk was highest for men and less evident for women.
An important strength of our study is that we analyzed all patients calling for chest discomfort, not selectively those with ACS. Another strength is that the original and very first conversations with patients were available, and analyzed before knowledge of the eventual diagnosis, which assures that our results are not affected by recall bias as was, possibly, in many of the previous studies.
A limitation is missing values on some clinical variables, a phenomenon common for research with routine care data. Importantly, however, we had no missing data for the time of calling, sex category, age or the outcome (ACS/no ACS) and, thus, we could perform our multivariable analysis without the need for imputing data. Finally, the less pronounced circadian effects among women compared to men should be interpreted carefully because our study could be under-powered for this subgroup analysis.
To the best of our knowledge, this is the first study in the OHS-PC setting assessing risks of ACS over 24 hours of patients with chest discomfort. Most previous studies analyzed patients with established ACS and reported absolute numbers, not risks or risk ratios. They reported a peak of ACS early mornings if considering the time of arrival at the hospital (8,10,18). A Swedish study reported likelihoods for ACS among patients with chest pain seen at the emergency department (ED) and reported a peak incidence from 8 to 10 am of 10.6% and a trough between 6 and 8 pm of 5.6% based on arrival time at the ED (9). The incidence peak of ACS from 0 to 9 am in our study could at least partly be explained by the fact that we used the time of calling (9). Interestingly, in the Swedish study, the incidence peak of ACS at the ED was lower than in our study, and the contrast between peak and trough was less. In another Swedish study, among 2205 patients with chest pain calling the dispatcher centre, the odds ratio among patients with an ACS for calls arriving before lunch at the dispatch centre was 2.02 (95% CI 1.22–3.43) compared with midnight (11). Possibly, differences in patient decision delay and organization of health care between Sweden and the Netherlands could have played a role.
We found a significant lower risk of ACS among women than men (8.9% vs. 15.9%, P < 0.001) and, among women, there was less difference in ACS between 0 and 9 am and other hours: 1.29 (CI 0.83–1.99) vs. 2.33 (CI 1.68–3.22) among men. In the aforementioned Swedish study, in an emergency department setting, women also had a lower likelihood for ACS than men, but they did not find a sex difference in the circadian pattern of ACS (9).
To appreciate our findings, presence of radiation of chest pain to the left arm had a likelihood ratio of ACS of 1.30 (CI 1.13–1.47), presence of sweating 1.34 (1.09–1.65) and nausea and/or vomiting 1.32 (CI 1.09–1.65) in a meta-analyses of 16 studies with non-selected patients (19). These symptoms typically are considered important items during triage op patients with chest discomfort, but their impact is fairly low. Currently, pre-hospital decision rules do not consider the time of calling as a valuable triage item and there seems to be no awareness among lay people about these ‘critical hours’ (20–22). Some awareness about a higher risk of ACS at night seems to be present among triage nurses and GPs working at the OHS-PC, as ACS patients received more often Priority 1 with ambulance straightaway if calls arrived between 0 and 9 am than during other hours (80.2% vs. 63.6%, P < 0.001). A previous study reported that missed diagnoses of ACS most often occurred at night (14). Also, this study stresses the importance of considering the time of calling with triage of patients with chest discomfort; it helps improve patient safety and accuracy of pre-hospital telephone triage.
Conclusion
Patients calling the OHS-PC for chest discomfort between 0 and 9 am have almost twice a higher risk of ACS than those calling at other hours, a phenomenon more evident in men than in women. At night, dispatching ambulances more ‘straightaway’ than during daytime could be considered for these patients with chest discomfort.
Acknowledgements
We would like to thank the primary care OHS foundation ‘Primair Huisartsenposten’ in Utrecht for their willingness to participate and Peter Zuithoff for statistical help.
Declarations
Funding: we received an unrestricted grant from (i) the Department of General Practice of the University Medical Center Utrecht, (ii) a personal promotion grant of DLZ, (iii) an unrestricted grant from the foundation ‘The Netherlands Triage Standard’ and (iv) the foundation ‘Stoffels-Hornstra’.
Ethical approval: the study was approved by the Medical Ethics Committee of the University Medical Center Utrecht (reference number WAG/mb/16/003208). All research data were stored de-identified according to the principles of the European General Data Protection Regulation.
Conflict of interest: the authors have declared no competing interests.
References
- 1. Bösner S, Haasenritter J, Becker A et al. Ruling out coronary artery disease in primary care: development and validation of a simple prediction rule. CMAJ 2010; 182: 1295–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Roffi M, Patrono C, Collet JP et al.; ESC Scientific Document Group 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: task force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European society of cardiology (ESC). Eur Heart J 2016; 37: 267–315. [DOI] [PubMed] [Google Scholar]
- 3. Mol KA, Smoczynska A, Rahel BM et al. Non-cardiac chest pain: prognosis and secondary healthcare utilisation. Open Heart 2018; 5: e000859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rawshani A, Larsson A, Gelang C et al. Characteristics and outcome among patients who dial for the EMS due to chest pain. Int J Cardiol 2014; 176: 859–65. [DOI] [PubMed] [Google Scholar]
- 5. Hoorweg BB, Willemsen RT, Cleef LE et al. Frequency of chest pain in primary care, diagnostic tests performed and final diagnoses. Heart 2017; 103: 1727–32. [DOI] [PubMed] [Google Scholar]
- 6. Frese T, Mahlmeister J, Heitzer M, Sandholzer H. Chest pain in general practice: frequency, management, and results of encounter. J Family Med Prim Care 2016; 5: 61–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Plat FM, Peters YAS, Loots FJ et al. Ambulance dispatch versus general practitioner home visit for highly urgent out-of-hours primary care. Fam Pract 2018; 35: 440–44. [DOI] [PubMed] [Google Scholar]
- 8. Bhalla A, Sachdev A, Lehl SS, Singh R, D’Cruz S. Ageing and circadian variation in cardiovascular events. Singapore Med J 2006; 47: 305–8. [PubMed] [Google Scholar]
- 9. Ekelund U, Akbarzadeh M, Khoshnood A, Björk J, Ohlsson M. Likelihood of acute coronary syndrome in emergency department chest pain patients varies with time of presentation. BMC Res Notes 2012; 5: 420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Leiza JR, de Llano JM, Messa JB, Lopez CA, Fernandez JA; ARIAM Study Group New insights into the circadian rhythm of acute myocardial infarction in subgroups. Chronobiol Int 2007; 24: 129–41. [DOI] [PubMed] [Google Scholar]
- 11. Rawshani A, Rawshani N, Gelang C et al. Emergency medical dispatch priority in chest pain patients due to life threatening conditions: a cohort study examining circadian variations and impact of the education. Int J Cardiol 2017; 236: 43–8. [DOI] [PubMed] [Google Scholar]
- 12. Kroneman M, Boerma W, van den Berg M et al. Netherlands: health system review. Health Syst Transit 2016; 18: 1–240. [PubMed] [Google Scholar]
- 13. van Ierland Y, van Veen M, Huibers L, Giesen P, Moll HA. Validity of telephone and physical triage in emergency care: the Netherlands triage system. Fam Pract 2011; 28: 334–41. [DOI] [PubMed] [Google Scholar]
- 14. Rutten MH, Kant J, Giesen P. What can we learn from calamities at out-of-hours services in primary care? [Wat kunnen we leren van calamiteiten op de huisartsenpost?]. Huisarts Wet 2018; 6: 39–42. [Google Scholar]
- 15. Erkelens DC, Wouters LT, Zwart DL et al. Optimisation of telephone triage of callers with symptoms suggestive of acute cardiovascular disease in out-of-hours primary care: observational design of the safety first study. BMJ Open 2019; 9: e027477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Smits M, Keizer E, Ram P, Giesen P. Development and testing of the KERNset: an instrument to assess the quality of telephone triage in out-of-hours primary care services. BMC Health Serv Res 2017; 17: 798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Keizer E, Maassen I, Smits M, Wensing M, Giesen P. Reducing the use of out-of-hours primary care services: a survey among dutch general practitioners. Eur J Gen Pract 2016; 22: 189–95. [DOI] [PubMed] [Google Scholar]
- 18. Cohen MC, Rohtla KM, Lavery CE, Muller JE, Mittleman MA. Meta-analysis of the morning excess of acute myocardial infarction and sudden cardiac death. Am J Cardiol 1997; 79: 1512–6. [DOI] [PubMed] [Google Scholar]
- 19. Bruyninckx R, Aertgeerts B, Bruyninckx P, Buntinx F. Signs and symptoms in diagnosing acute myocardial infarction and acute coronary syndrome: a diagnostic meta-analysis. Br J Gen Pract 2008; 58: 105–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bruins Slot MH, Rutten FH, van der Heijden GJ et al. Gender differences in pre-hospital time delay and symptom presentation in patients suspected of acute coronary syndrome in primary care. Fam Pract 2012; 29: 332–7. [DOI] [PubMed] [Google Scholar]
- 21. Grijseels EW, Deckers JW, Hoes AW et al. Implementation of a pre-hospital decision rule in general practice. Triage of patients with suspected myocardial infarction. Eur Heart J 1996; 17: 89–95. [DOI] [PubMed] [Google Scholar]
- 22. Haasenritter J, Donner-Banzhoff N, Bösner S. Chest pain for coronary heart disease in general practice: clinical judgement and a clinical decision rule. Br J Gen Pract 2015; 65: e748–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Zwaanswijk M, Hek K. ICPC coding at the out-of-hours service in primary care [ICPC-codering op de huisartsenpost]. Huisarts Wet 2013; 11: 577. [Google Scholar]