Abstract
Purpose of the Review
Rotator cuff repair has excellent outcomes for many patients but continues to be suboptimal for large, retracted tears, and revision procedures. In these situations, patch augmentation may be considered in order to improve healing. The purpose of this article is to review the history, graft options, indications, surgical technique, outcomes, and complications associated with arthroscopic patch augmentation for rotator cuff repair.
Recent Findings
Patch augmentation has been shown in several studies to improve healing rates. After multiple investigations into different materials available for patch augmentation, acellular dermal allograft seems to be the graft with the best scientific support. While multiple techniques have been presented, few studies have compared their performance.
Summary
While the arthroscopic technique for patch augmentation can be challenging, we present a systematic approach to this procedure with the potential to reliably and predictably perform patch augmentation. This technique is a valuable tool for surgeons that treat rotator cuff pathology.
Keywords: Rotator cuff repair, Patch augmentation, Dermal allograft, Surgical technique, Biologic augmentation
Introduction
The structural outcomes following rotator cuff repair continue to be suboptimal, with high re-tear rates reported in many series [1–3]. The natural history of rotator cuff tears is not necessarily benign, with progression in tear size, muscular atrophy, and eventually the development of the characteristic articular degenerative changes of rotator cuff tear arthropathy [1,3,6]. Consequently, the primary goal of rotator cuff repair should be a healed tendon-bone interface. Several studies have shown that if a rotator cuff repair heals, good outcomes are usually maintained in the long-term [1, 4, 7]. Thus, there has been substantial research focus and commercial investment directed to increase the likelihood of tendon healing, with much of the focus being upon the number and arrangement of anchors and other factors to improve the mechanical properties of the repair [2, 5, 8]. However, despite decades of research and investment in repair techniques, little to no progress seem to have been made in reducing re-tear rates after rotator cuff repair [4, 10, 11••]. There is thus a somewhat urgent need for innovative treatment alternatives that will allow surgeons to improve healing rates after rotator cuff repair, and they likely involve biologic augmentation (Table 1).
Table 1.
Pearls and Pitfalls to all-arthroscopy patch augmentation in rotator cuff repair
| Pearls | Pitfalls |
|---|---|
| Perform extensive intraarticular and subacromial releases prior to repair | Leaving residual subacromial bursa limiting vision |
| Pass all anchor stitches first; Then pass medial independent stitches in the rotator cuff using a retrograde suture shuttle to avoid tangling sutures from the anchors | Tangling sutures during passage; Confirm that tangling has not occurred prior to tying by passing a suture retriever over each limb passed through the graft to confirm a lack of tangles |
| When retrieving limbs out the lateral portal to pass through the graft, work either anterior to posterior or posterior to anterior making keeping all passed limbs in the anterior or posterior aspect of the cannula respectively to avoid tangling | Utilize a 3.0-mm or thicker graft as a thinner graft tends to tear with suture tying |
| Push and pull the graft into the subacromial space using a rotator cuff grasper to push the graft as a taco and the limbs of the mulberry knot stitches to pull the graft | |
| Make sure the lateral cannula is at least 10 mm in diameter | |
| Tie the medial graft stitches first, then the anchor horizontal mattress stitches and then perform the bridging to the lateral anchors in that order |
Patch Augmentation Types
Patch augmentation of rotator cuff repair may potentially fill the gap described above. After early results were reported in the 2000s [4, 7, 11••], there has been accelerating interest in techniques to improve rotator cuff repair using patch augmentation. Patch augmentation may be performed in a number of forms. First, in a tear that cannot be advanced to the tuberosity, the patch can bridge the gap between the tendon and the tuberosity. This technique is typically referred to as a patch interposition technique [6, 13, 16]. Second, in a tear that can be advanced only to the medial aspect of the tuberosity, the patch can be placed on the bursal side of the tendon and tuberosity to both reinforce the repair and resurface the uncovered tendon footprint [4, 8, 12]. Third, in a tear that can be fully advanced to the native footprint, the patch can be interposed between the tendon and the bone in an attempt to improve restoration of the native enthesis [4,8,14••]. No published clinical outcomes exist for this third method, and thus, it will not be further discussed in this manuscript. Fourth, the patch can be placed between the tuberosity and the glenoid without connection to the rotator cuff [6,18,21]. This technique, referred to as “superior capsular reconstruction” is addressed elsewhere within this topical collection and will not be discussed in this manuscript either.
Patch Types
A variety of materials have been reported for rotator cuff patch augmentation. These materials can be divided into xenograft, synthetic, and allograft materials.
Xenograft
Several early studies used xenograft small intestine submucosa (SIS) patches [4,9,15]. Published results using these patches have been disappointing overall. Sclamberg et al. reported a 91% failure rate [3,15,26]. In a randomized clinical trial, Iannotti et al. reported better outcomes in the group of patients treated without the SIS patch, and a 20% sterile inflammatory reaction rate in the group of patients receiving the patch [11••]. In another study, the SIS patch was associated with a 40% rate of open debridement for sterile inflammatory reactions [8,23,28••]. As a result, xenograft SIS patches have been largely abandoned for use in rotator cuff augmentation.
The results of xenograft dermal grafts have been more encouraging but remain somewhat mixed [4,10,19]. Gupta and colleagues reported on 27 shoulders that underwent open patch interposition of an irreparable rotator cuff tear using a porcine xenograft dermal graft (Conexa, Tornier, Warsaw, IN) and showed significant improvements in elevation, strength, and patient-reported outcome scores, with a 73% rate of a structurally completely intact reconstruction at 2 years postoperatively [12]. In another prospective multicenter study using the same graft for repair augmentations, 50 patients followed for a minimum of 2 years of experience, significant improvements in range of motion, strength, and functional outcomes scores, with a retear of 34% [16]. A subsequent prospective study using the patch as an interposition demonstrated again similar findings: 92% of the grafts were intact by ultrasound, 61 shoulders followed for a minimum of 2 years [24]. In a nonrandomized comparative study using the same patch, Maillot et al. compared arthroscopic debridement, rotator cuff repair, and rotator cuff repair with patch augmentation and found no difference in outcomes, but a higher complication rate in the patch group; these authors thus recommended against patch augmentation [18]. Interestingly, the patch reported in this studies is no longer available on the market.
Ciampi et al. reported on 49 patients that underwent open rotator cuff repair with augmentation using a bovine pericardial xenograft (Tutopatch, Tutogen Medical, Neunkirchen am Brand, Germany) and reported a 51% retear rate, which was higher than the 41% within their control group of repairs without augmentation. These authors suggested that biologic absorbable patches do not provide much value [4,11••,20]. There are two reports on a cross-linked porcine dermal xenograft (Zimmer Collagen Repair, Warsaw, IN). The results are very different, with one report demonstrating 80% graft integrity [2] and the other demonstrating 0% graft integrity [3,20,32]. This graft is no longer on the market. Consigliere et al. reported on 10 patients who underwent arthroscopic rotator cuff repair with a porcine dermal xenograft (DX reinforcement Matrix, Arthrex, Naples, FL) and reported significant improvements in Constant score, Oxford score, and pain scores; however, this study did not provide any follow-up imaging, and the minimum follow was only 3 months [4,12,21]. A comparative matched-pair study of 40 patients using the same patch demonstrated no difference in outcomes or structural continuity of the rotator cuff between the patch and control groups [11••]. Overall, the results summarized above suggest that dermal xenografts do not appear to suffer the same issues with sterile inflammatory responses as a graft. However, all of the comparative studies suggest that they do not provide much value either.
Synthetic
A variety of synthetic materials have been used to augment rotator cuff repair. In other areas of soft-tissue repair surgery, such as in hernia repair [3,21,33] and knee extensor tendon repair [5,13,22], synthetic mesh has demonstrated utility. In the field of rotator cuff augmentation, reports are more limited and largely from outside of the USA. Audenaert et al. reported on 41 patients followed for a minimum of 2 years after open interposition with an 8-layer Mersilene mesh (Ethicon, Somerville, NJ) and demonstrated significant improvements in Constant and pain scores [2]. However, a recent report of 13 patients with a minimum of 17-year follow-up after open interposition with a Dacron patch (DuPont, Wimington, DE) demonstrated that 70% of patches had retorn and that there were no differences in radiographic evidence of rotator cuff tear arthropathy between the patch side and contralateral side, suggesting that patch interposition with a synthetic device may not alter the natural history of rotator cuff disease [31]. In another long-term follow-up study, Shepherd et al. followed five patients for a mean of 9.7 years after interposition with a polytetrafluoroethylene patch (Gore, Newark, DE) and found that in 80% of patients, the repair was intact and that external rotation and abduction motion were improved from preoperatively [4,22,35••]. In a more recent and larger study using the same patch, Seker et al. described minimum 2-year outcomes in 58 patients and found significant improvements in strength and range of motion, with 91% of patches intact on ultrasound [4,22,36]. Ciampi et al. reported upon 52 patients with a minimum of 1-year follow-up that underwent open rotator cuff repair augmented with a polypropylene patch (Repol Angimesh, Angiologica, Pavia, Italy) and showed significantly improved healing rates (17% vs. 41%), functional outcomes, strength, and elevation as compared to a repair-alone control group [7]. While these international results are promising, no published clinical outcomes are available in the USA, despite several synthetic patches being available on the market, including a polyurethane urea patch (SportMesh, Biomet, Warsaw, IN) and a poly-l-lactide patch (X-Repair, Synthasome, San Diego, CA).
Allograft
Within the USA, most recent publications have reported on the use of acellular dermal allograft [5,13,25••]. Dermal allograft is more readily available than allograft rotator cuff, and it is thus more commonly utilized. In a prospective comparative study of 35 patients followed for a mean of 2 years, Gilot et al. demonstrated a higher retear rate in the control group compared with the patch group (27% vs. 10%) [5,13,26]. In a prospective randomized clinical trial of 42 patients followed for a mean of 24 months, Barber et al. demonstrated a higher retear rate in the control group compared with the patch group as well (60% vs. 15%) [6,14••,27]. These studies, and others, have lead a recently conducted metaanalysis to conclude that patch augmentation with allograft improves tendon healing and clinical outcomes compared with repair without graft-provided xenografts are excluded from the analysis [5,27,38].
Autograft
In countries where allograft is culturally unacceptable, autograft is considered as an option, although limited donor sites are available. The tendon of the long head of the biceps is perhaps the most frequently utilized autograft for cuff augmentation, but given the structural and geometric differences between this graft and the others discussed within the review, we will not discuss it further in this review. Scheibel et al. described 20 patients with a mean follow-up of 14 months treated with rotator cuff repair augmentation using humeral periosteum and found significant improvements in Constant scores, simple shoulder test scores, but a 20% retear rate and a 20% rate of heterotopic ossification [5,27,39]. Fascia lata autograft has been used for superior capsular reconstruction [9,32,34] and also as a graft for rotator cuff augmentation [12,37,41]. Mori et al. described 24 patients who underwent patch interposition of an irreparable rotator cuff tear with fascia lata autograft and described significantly better outcomes when compared with a partial repair control group as measured with ASES scores, Constant scores, strength, and retear rates (8% vs. 42%) [9,32,35••]. Overall, these studies suggest a potentially promising role for autograft. Based upon these results, a recently conducted systematic review also concluded that patch interposition improves functional outcomes as compared with partial repair, although only two comparative studies were included [24].
Surgical Technique
Patch augmentation can be technically challenging and requires the surgeon to be patient and organized. While a variety of surgical techniques have been presented for arthroscopic patch augmentation for rotator cuff repair [8,16,29], the senior author has developed the following technique for patch augmentation. The procedure described is specifically used to augment posterosuperior rotator cuff tears that are completely reparable. This technique is not recommended to address either completely irreparable or partially reparable tears.
Surgical repair is performed in a beach chair position. Equipment required for the procedure include a standard 30° arthroscope, multiple 7-mm cannulas, one 10-mm cannula, and anterograde and retrograde suture passing devices. Sutures anchors utilized include standard triple loaded 5.5-mm screw-in suture anchors and 5.5-mm knotless suture anchors. The graft used is a 3.0-mm thick acellular dermal matrix allograft. Finally, multiple strands of number 2 high tensile strength suture are used.
The procedure starts with an intraarticular evaluation and management of any subscapularis pathology or biceps lesions encountered. Once the intraarticular work has been completed, the scope is redirected subacromially. Working portals are established 3 to 4 cm off the anterolateral and posterolateral corners of the acromion along with a lateral portal halfway between these other portals. Seven-millimeter cannulas are placed in the anterolateral and posterolateral portals, and a 10-mm cannula is placed in the lateral portal. A complete subacromial bursectomy is performed included removal of bursal tissue and adhesions in the anterior, posterior, and lateral gutters. Mobilization of the rotator cuff with releases between the rotator cuff and labrum as well as release around the base of the scapular spine, and the coracoid are often required. Typically an intraarticular release of the rotator cuff interval as well as subacromial release of the coracohumeral ligament with preservation of the lateral margin of the rotator cuff interval is preferred (Fig. 1).
Fig. 1.

View of massive rotator cuff tear from posterolateral portal
Once the rotator cuff has been mobilized and it has been determined that a complete repair is possible, the repair with augmentation is initiated. Because these are typically large retracted tears (and oftentimes revision procedures), a medialized single row repair is most commonly performed. A row of triple loaded 5.5-mm anchors is placed along the medial aspect of the greater tuberosity (Fig. 2). Usually three anchors are required. The most anterior two sutures from the anterior anchor and most posterior two sutures from the posterior anchor are placed in a simple fashion. The last suture from the anterior anchor is placed posterior to the previously passed sutures from this anchor in a mattress fashion. The last suture from the posterior anchor is placed anterior to the previously passed sutures from this anchor in a mattress fashion. The three sutures from the middle anchor are placed in a simple fashion between the anterior and posterior mattress stitches. Finally, three number 2 high strength sutures are placed medial to the previously passed anchor stitches in a mattress fashion through rotator cuff tissue usually at the muscle-tendon junction—one anterior, one middle, and one posterior—with the anterior and posterior stitches placed at the most anterior and posterior aspects of the tear (Figs. 3 and 4).
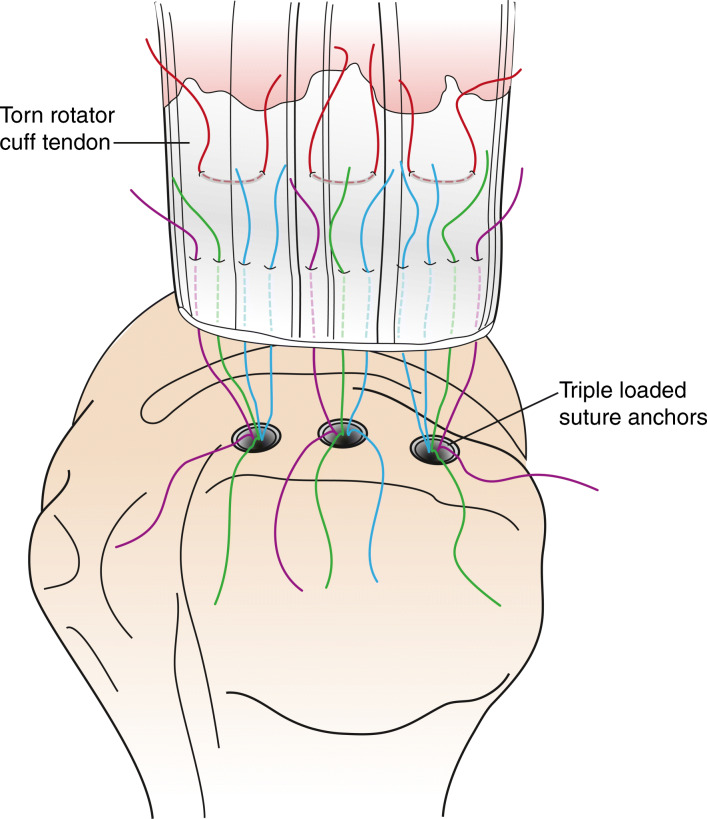
Fig. 2.

Three triple loaded anchors placed at the medial aspect of the anatomic neck of the greater tuberosity
Fig. 3.
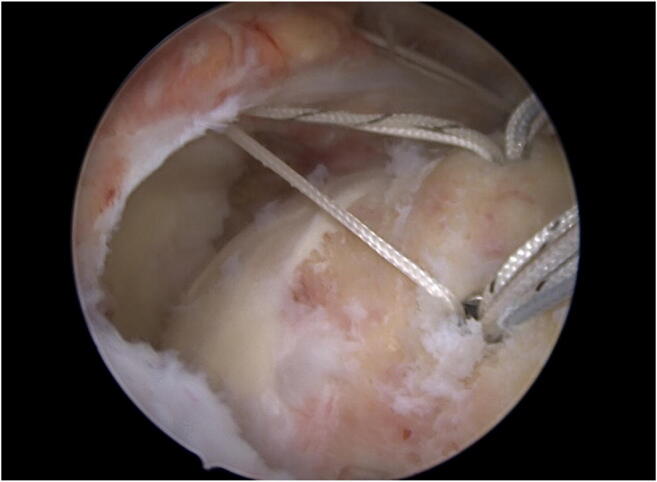
View of stitches passed from anchors (2 simple stitches and 1 mattress stitch from the anterior and posterior anchors and 3 simple stitches from the middle anchor)
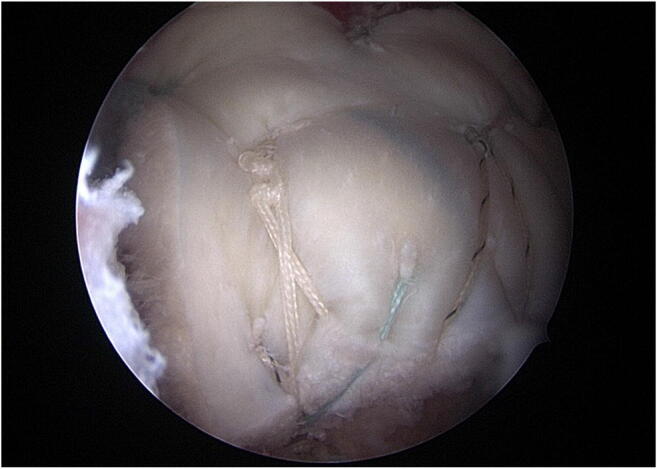
Fig. 4.

View from the lateral portal after the simple stitches from the anchors are tied leaving the mattress stitches from the anterior and posterior anchors untied. The trailing stitch in the image is one limb from the independent stitches passed through the rotator cuff medial to the anchor stitches
The simple sutures from the anchors are then tied completing the rotator cuff repair (Fig. 4). This leaves the mattress stitches from the anterior and posterior anchors as well as the medially placed horizontal sutures untied. An arthroscopic measuring device is then used to measure the graft size. The anterior to posterior dimension is measured from the most anterior mattress suture not coming from the anchor to the most posterior mattress suture not coming from an anchor. The medial lateral dimension of the graft is measured from the middle mattress suture not coming from an anchor to the lateral aspect of the greater tuberosity. The acellular dermal matrix graft is then cut to these dimensions.
Three new separate number 2 high strength sutures are then placed in the lateral aspect of the graft. One stitch is placed in the anterolateral corner in a simple fashion and another is placed in the posterolateral corner in a simple fashion. Between these two sutures, an inverted mattress suture is placed along the lateral margin with the tails exiting the superior surface of the graft. At this point, the tails of the sutures passed through the rotator cuff but not tied will be exteriorized through the lateral 10-mm portal for passage through the graft. The scope should be placed in the posterolateral portal during this portion of the surgery.
A suture retriever is placed through the lateral portal and one limb of the most posterior medial mattress suture that is not from the anchor is retrieved and passed through the most posterior medial aspect of the graft with the tail of the suture passed to the superior surface of the graft. A mulberry knot is then created using this tail and the other tail of this suture is pulled, securing the knot to the superior aspect of the graft. Next the most posterior tail of the posterior mattress suture from the posterior anchor is placed in the graft halfway between the medial and lateral edge of the graft and approximately 5 mm from the posterior edge of the graft. Next, the more anterior tail of this posterior anchor mattress is retrieved and passed about 5- to 10-mm anterior to the previously passed tail in the graft. Next, one tail of the middle mattress suture is retrieved and passed through the middle of the medial aspect of the graft with the tail of the suture passed to the superior surface of the graft. A mulberry knot is then created using this tail, and the other tail of this suture is pulled securing the knot to the superior aspect of the graft. Next, the most posterior tail of the anterior mattress suture coming from the anterior anchor is passed in the graft halfway between the medial and lateral edge of the graft approximately 15 mm from the anterior edge of the graft. Next, the most anterior tail of the anterior mattress from the anterior anchor is passed about 5–10-mm anterior to the last tail of this same suture. Finally, one tail of the anterior most mattress suture not coming from an anchor is passed into the anterior medial corner of the graft with the tail of the suture passed to the superior surface of the graft. A mulberry knot is then created using this tail, and the other tail of this suture is pulled securing the knot to the superior aspect of the graft. At this point, one tail of the posterior mattress not from an anchor should be coming out the posterior portal and one tail of the anterior mattress not from an anchor should be coming out a standard anterior portal. A Nevaiser portal can be created and the remaining limb of the medial mattress suture not coming from an anchor should be pulled out this portal with a retriever. Care must be taken during this process to not cross sutures while retrieving or passing sutures through the graft (Fig. 5).
Fig. 5.
Diagram showing the placement of stitches from the anchors in the rotator cuff along with medial independent stitches in the rotator cuff.
All slack is then taken out of the sutures. The graft is then folded like a taco with the anterior and posterior edges folded up. A rotator cuff grasper is then used the grasp the folded edges and push the graft through the lateral cannula. At the same time, the three tails of the medial mattress sutures coming out the anterior and posterior and Nevaiser portals should be pulled, so there is a combined push–pull during the delivery of the graft. Once in the subacromial space, slack should be taken out of the sutures. The lateral portal should be cleared of sutures by docking the tails from the anterior mattress from the anchor, the tails from the anterolateral suture through the anterolateral corner of the graft, and the anterior limb of the middle lateral inverted mattress in the anterolateral cannula. The remaining limbs should be similarly docked in the posterolateral cannula. With the lateral cannula now cleared, the posterior mulberry knot is retrieved, cutoff, and the corresponding suture tail retrieved and tied securing the posteromedial corner. The same steps are performed for the middle and anterior mulberry knots. The tails of these are cut.
Next, the posterior mattress limbs from the posterior anchor are retrieved and tied and the knot cut. The anterior mattress limbs from the anterior anchor are managed similarly. The arm is then brought into slight forward flexion and abduction, exposing the lateral gutter. The scope is placed back into the posterior portal. One of the limbs from the anterior tied mattress from the anterior anchor and one of the limbs from the posterior tied mattress from the posterior anchor plus the two limbs of the simple suture through the anterolateral corner of the graft and the anterior limb of the middle lateral inverted mattress suture and are placed into a 5.5-mm knotless suture anchor. The anchor is then placed about 5–10 mm lateral to the edge of the greater tuberosity just posterior to the biceps groove as the anterior anchor of the suture bridge construct. Finally, the remaining anterior and posterior limbs from the tied mattress sutures from the anchors as well as the simple suture tails from the suture in the posterolateral corner and the remaining tail of the middle lateral inverted mattress suture are retrieved out the lateral portal and placed into the final 5.5-mm knotless suture anchor. This anchor is placed about 5–10 mm lateral to the edge of the greater tuberosity at the posterior margin of the tear (Figs. 6, 7 and 8).
Fig. 6.
Diagram showing the simple stitches from the anchors tied and the remaining limbs from the mattress anchor stitches as well as one limb of the medial independent stitches in the rotator cuff passed through the graft. Finally, three independent stitches are also passed through the lateral margin of the graft.
Fig. 7.
Lateral view after the graft has been passed in the subacromial space, the medial graft stitches have been tied and cut, the anchor mattress stitches have been tied and their tails have been brought over to 2 lateral row knotless anchors along with three independent stitches passed through the lateral margin of the graft
Fig. 8.
Diagram of final construct with tied medial graft stitches, tied horizontal mattress anchor stitches through the tendon and graft and tails of the tied stitches brought over to two knotless lateral row anchors along with the stitches from the lateral margin of the graft
Postoperative Rehabilitation
After this procedure, patients are in an abduction sling for 6 weeks. Passive supine forward elevation is started at 2 weeks and allowed to 90° along with pendulums and active assisted external rotation at the side. At 6 weeks postoperative, the sling is discontinued and the patients can start lifting up to 5 lbs. Passive and active motion is allowed in all directions except for internal rotation with extension. At 12 weeks, motion is allowed in all planes and isometric and resistive strengthening of the rotator cuff, deltoid, and scapular stabilizers is initiated; at that point, patients are allowed to lift up to 20 lbs. At 18 weeks, patients are allowed to lift up to 40 lb. and return to most activities except contact or collision sports and heavy lifting manual labor. At 6 months postoperative, patients are allowed to return to work as tolerated.
Future Directions
Certainly, further research is necessary to better define the indications for patch augmentation and interposition. Given the high healing rates of small- and medium-sized tears the cost of patch augmentation is difficult to justify in these settings [8,17,30]. However, other questions remain: Are these patches better for younger or older patients? What is the role of patch interposition as compared to superior capsular reconstruction? What is the role of partial repair and patch interposition as compared with tendon transfers? These questions will require careful prospective comparative research. In addition, future research will be necessary to compare synthetic patches to acellular dermal allograft, as well as to determine whether there may be newer xenografts that should be investigated further.
Conclusions
The current research suggests that patch augmentation may improve healing rates and outcomes when used to augment in the repair of large and massive rotator cuff tears, and that patch interposition may improve outcomes with irreparable rotator cuff tears as compared with partial repair. The shoulder surgeon who evaluates patients with large rotator cuff tears should be aware of the potential benefits of patch augmentation.
Compliance with Ethical Standards
Conflict of Interest
Peter Chalmers is a paid consultant for Depuy-Mitek and Arthrex. Robert Tashjian is a paid consultant for Zimmer Biomet, Wright Medical and Depuy-Mitek; has stock in Conextions, INTRAFUSE, Genesis and KATOR; receives intellectual property royalties from Wright Medical, Shoulder Innovations, and Zimmer Biomet; receives publishing royalties from Springer, the Journal of Bone and Joint Surgery and the Journal of the American Association of Orthopaedic Surgeons, and serves on the editorial board for the Journal of the American Association of Orthopaedic Surgeons.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Surgical Management of Massive Irreparable Cuff Tears
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Abdel MP, Salib CG, Mara KC, Pagnano MW, Perry KI, Hanssen AD. Extensor mechanism reconstruction with use of Marlex mesh. J Bone Jt Surg. 2018;100(15):1309–1318. doi: 10.2106/jbjs.17.01165. [DOI] [PubMed] [Google Scholar]
- 2.Audenaert E, Nuffel VJ, Schepens A, Verhelst M, Verdonk R. Reconstruction of massive rotator cuff lesions with a synthetic interposition graft: a prospective study of 41 patients. Knee Surg Sports Traumatology Arthrosc. 2006;14(4):360–364. doi: 10.1007/s00167-005-0689-7. [DOI] [PubMed] [Google Scholar]
- 3.Badhe SP, Lawrence TM, Smith FD, Lunn PG. An assessment of porcine dermal xenograft as an augmentation graft in the treatment of extensive rotator cuff tears. J Shoulder Elb Surg. 2008;17(1):S35–S39. doi: 10.1016/j.jse.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 4.Barber AF, Burns JP, Deutsch A, Labbé MR, Litchfield RB. A prospective, randomized evaluation of acellular human dermal matrix augmentation for arthroscopic rotator cuff repair. Arthrosc J Arthrosc Relat Surg. 2012;28(1):8–15. doi: 10.1016/j.arthro.2011.06.038. [DOI] [PubMed] [Google Scholar]
- 5.Cai Y-Z, Zhang C, Jin R-L, Shen T, Gu P-C, Lin X-J, et al. Arthroscopic rotator cuff repair with graft augmentation of 3-dimensional biological collagen for moderate to large tears: a randomized controlled study. Am J Sports Medicine. 2018;46(6):1424–1431. doi: 10.1177/0363546518756978. [DOI] [PubMed] [Google Scholar]
- 6.Chalmers PN, Frank RM, Gupta AK, Yanke AB, Trenhaile SW, Romeo AA, Bach BR, Jr, Verma NN. All-arthroscopic patch augmentation of a massive rotator cuff tear: surgical technique. Arthrosc Techniques. 2013;2(4):e447–e451. doi: 10.1016/j.eats.2013.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chalmers PN, Granger E, Nelson R, Yoo M, Tashjian RZ. Factors affecting cost, outcomes, and tendon healing after arthroscopic rotator cuff repair. Arthrosc J Arthrosc Relat Surg. 2018;34:1393–1400. doi: 10.1016/j.arthro.2017.11.015. [DOI] [PubMed] [Google Scholar]
- 8.Chalmers PN, Ross H, Granger E, Presson AP, Zhang C, Tashjian RZ. The effect of rotator cuff repair on natural history. Jbjs Open Access. 2018;3(1):e0043. doi: 10.2106/jbjs.oa.17.00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chalmers PN, Salazar DH, Steger-May K, Chamberlain AM, Stobbs-Cucchi G, Yamaguchi K, Keener JD. Radiographic progression of arthritic changes in shoulders with degenerative rotator cuff tears. J Shoulder Elb Surg. 2016;25(11):1749–1755. doi: 10.1016/j.jse.2016.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ciampi P, Scotti C, Nonis A, Vitali M, Serio C, Peretti GM, et al. The benefit of synthetic versus biological patch augmentation in the repair of posterosuperior massive rotator cuff tears. Am J Sports Medicine. 2014;42(5):1169–1175. doi: 10.1177/0363546514525592. [DOI] [PubMed] [Google Scholar]
- 11.Collin P, Kempf J-F, Accent D, Meyer N, Agout C, Saffarini M, et al. Ten-year multicenter clinical and MRI evaluation of isolated supraspinatus repairs. J Bone Jt Surg. 2017;99(16):1355–1364. doi: 10.2106/jbjs.16.01267. [DOI] [PubMed] [Google Scholar]
- 12.Consigliere P, Polyzois I, Sarkhel T, Gupta R, Levy O, Narvani AA. Preliminary results of a consecutive series of large & massive rotator cuff tears treated with arthroscopic rotator cuff repairs augmented with extracellular matrix. Archives Bone Jt Surg. 2017;5(1):14–21. doi: 10.22038/abjs.2016.7932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Derwin KA, Badylak SF, Steinmann SP, Iannotti JP. Extracellular matrix scaffold devices for rotator cuff repair. J Shoulder Elb Surg. 2010;19(3):467–476. doi: 10.1016/j.jse.2009.10.020. [DOI] [PubMed] [Google Scholar]
- 14.Diebold G, Lam P, Walton J, Murrell GA. Relationship between age and rotator cuff retear: a study of 1,600 consecutive rotator cuff repairs. J Bone Jt Surg. 2017;99(14):1198–1205. doi: 10.2106/jbjs.16.00770. [DOI] [PubMed] [Google Scholar]
- 15.Ferguson DP, Lewington MR, Smith DT, Wong IH. Graft utilization in the augmentation of large-to-massive rotator cuff repairs. Am J Sports Medicine. 2016;44(11):2984–2992. doi: 10.1177/0363546515624463. [DOI] [PubMed] [Google Scholar]
- 16.Flury M, Rickenbacher D, Jung C, Schneider MM, Endell D, Audigé L. Porcine dermis patch augmentation of supraspinatus tendon repairs: a pilot study assessing tendon integrity and shoulder function 2 years after arthroscopic repair in patients aged 60 years or older. Arthrosc J Arthrosc Relat Surg. 2018;34(1):24–37. doi: 10.1016/j.arthro.2017.06.024. [DOI] [PubMed] [Google Scholar]
- 17.Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. The Journal of Bone and Joint Surgery. 2004;86-A(2):219–224. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Gupta AK, Hug K, Berkoff DJ, Boggess BR, Gavigan M, Malley PC, Toth AP. Dermal tissue allograft for the repair of massive irreparable rotator cuff tears. Am J Sports Medicine. 2012;40(1):141–147. doi: 10.1177/0363546511422795. [DOI] [PubMed] [Google Scholar]
- 19.Gupta AK, Hug K, Boggess B, Gavigan M, Toth AP. Massive or 2-tendon rotator cuff tears in active patients with minimal glenohumeral arthritis. Am J Sports Medicine. 2013;41(4):872–879. doi: 10.1177/0363546512475204. [DOI] [PubMed] [Google Scholar]
- 20.Hartzler RU, Melapi S, de Beer JF, Burkhart SS. Arthroscopic joint preservation in severe glenohumeral arthritis using interpositional human dermal allograft. Arthrosc J Arthrosc Relat Surg. 2017;33(11):1920–1925. doi: 10.1016/j.arthro.2017.04.005. [DOI] [PubMed] [Google Scholar]
- 21.Hebert-Davies J, Teefey SA, Steger-May K, Chamberlain AM, Middleton W, Robinson K, et al. Progression of fatty muscle degeneration in atraumatic rotator cuff tears. J Bone Jt Surg. 2017;99(10):832–839. doi: 10.2106/jbjs.16.00030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hohn EA, Gillette BP, Burns JP. Outcomes of arthroscopic revision rotator cuff repair with acellular human dermal matrix allograft augmentation. J Shoulder Elb Surg. 2018;27(5). 10.1016/j.jse.2017.09.026. [DOI] [PubMed]
- 23.Keener JD, Galatz LM, Stobbs-Cucchi G, Patton R, Yamaguchi K. Rehabilitation following arthroscopic rotator cuff repair. J Bone Jt Surg. 2014;96(1):11–19. doi: 10.2106/jbjs.m.00034. [DOI] [PubMed] [Google Scholar]
- 24.Keener JD, Galatz LM, Teefey SA, Middleton WD, Steger-May K, Stobbs-Cucchi G, et al. A prospective evaluation of survivorship of asymptomatic degenerative rotator cuff tears. J Bone Jt Surg. 2015;97(2):89–98. doi: 10.2106/jbjs.n.00099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.•• Kim J, Lee J-H, Kim K-S, Ji J-H, Koh S-J, Lee J-H. Rotator cuff bridging repair using acellular dermal matrix in large to massive rotator cuff tears: histologic and clinical analysis. J Shoulder Elb Surg. 2017;26(11). 10.1016/j.jse.2017.04.010This histology study shows that acellular dermal allograft patches can incorporate. [DOI] [PubMed]
- 26.Lederman ES, Toth AP, Nicholson GP, Nowinski RJ, Bal GK, Williams GR, Iannotti JP. A prospective, multicenter study to evaluate clinical and radiographic outcomes in primary rotator cuff repair reinforced with a xenograft dermal matrix. J Shoulder Elb Surg. 2016;25(12):1961–1970. doi: 10.1016/j.jse.2016.02.029. [DOI] [PubMed] [Google Scholar]
- 27.Lee NM, Erisken C, Iskratsch T, Sheetz M, Levine WN, Lu HH. Polymer fiber-based models of connective tissue repair and healing. Biomaterials. 2017;112:303–312. doi: 10.1016/j.biomaterials.2016.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lewington MR, Ferguson DP, Smith DT, Burks R, Coady C, Wong I. Graft utilization in the bridging reconstruction of irreparable rotator cuff tears: a systematic review. Am J Sports Medicine. 2017;45(13):3149–3157. doi: 10.1177/0363546517694355. [DOI] [PubMed] [Google Scholar]
- 29.Linderman SW, Golman M, Gardner TR, Birman V, Levine WN, Genin GM, et al. Enhanced tendon-to-bone repair through adhesive films. Acta Biomater. 2018. 10.1016/j.actbio.2018.01.032. [DOI] [PMC free article] [PubMed]
- 30.Mascarenhas R, Chalmers PN, Sayegh ET, Bhandari M, Verma NN, Cole BJ, Romeo AA. Is double-row rotator cuff repair clinically superior to single-row rotator cuff repair: a systematic review of overlapping meta-analyses. Arthrosc J Arthrosc Relat Surg. 2014;30(9):1156–1165. doi: 10.1016/j.arthro.2014.03.015. [DOI] [PubMed] [Google Scholar]
- 31.McElvany MD, McGoldrick E, Gee AO, Neradilek M, Matsen FA. Rotator cuff repair: published evidence on factors associated with repair integrity and clinical outcome. Am J Sports Medicine. 2014;43(2). 10.1177/0363546514529644. [DOI] [PubMed]
- 32.Mihata T, Lee TQ, Fukunishi K, Itami Y, Fujisawa Y, Kawakami T, et al. Return to sports and physical work after arthroscopic superior capsule reconstruction among patients with irreparable rotator cuff tears. Am J Sports Medicine. 2018;46(5):1077–1083. doi: 10.1177/0363546517753387. [DOI] [PubMed] [Google Scholar]
- 33.Mihata T, Lee TQ, Hasegawa A, Kawakami T, Fukunishi K, Fujisawa Y, Itami Y, Ohue M, Neo M. Arthroscopic superior capsule reconstruction can eliminate pseudoparalysis in patients with irreparable rotator cuff tears. Am J Sports Medicine. 2018;46(11):2707–2716. doi: 10.1177/0363546518786489. [DOI] [PubMed] [Google Scholar]
- 34.Mihata T, Lee TQ, Watanabe C, Fukunishi K, Ohue M, Tsujimura T, et al. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthrosc J Arthrosc Relat Surg. 2013;29(3):459–470. doi: 10.1016/j.arthro.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 35.Moosmayer S, Lund G, Seljom US, Haldorsen B, Svege IC, Hennig T, et al. At a 10-year follow-up, tendon repair is superior to physiotherapy in the treatment of small and medium-sized rotator cuff tears. J Bone Jt Surg Am. 2019;101(12):1050–1060. doi: 10.2106/jbjs.18.01373. [DOI] [PubMed] [Google Scholar]
- 36.Mori D, Funakoshi N, Yamashita F. Arthroscopic surgery of irreparable large or massive rotator cuff tears with low-grade fatty degeneration of the Infraspinatus: patch autograft procedure versus partial repair procedure. Arthrosc J Arthrosc Relat Surg. 2013;29(12):1911–1921. doi: 10.1016/j.arthro.2013.08.032. [DOI] [PubMed] [Google Scholar]
- 37.Neumann JA, Zgonis MH, Rickert KD, Bradley KE, Kremen TJ, Boggess BR, Toth AP. Interposition dermal matrix xenografts: a successful alternative to traditional treatment of massive rotator cuff tears. Am J Sports Medicine. 2017;45(6):1261–1268. doi: 10.1177/0363546516683945. [DOI] [PubMed] [Google Scholar]
- 38.Ranebo MC, Hallgren HC, Norlin R, Adolfsson LE. Long-term clinical and radiographic outcome of rotator cuff repair with a synthetic interposition graft: a consecutive case series with 17 to 20 years of follow-up. J Shoulder Elb Surg. 2018;27(9). 10.1016/j.jse.2018.03.011. [DOI] [PubMed]
- 39.Scheibel M, Brown A, Woertler K, Imhoff AB. Preliminary results after rotator cuff reconstruction augmented with an autologous periosteal flap. Knee Surg Sports Traumatology Arthrosc. 2007;15(3):305–314. doi: 10.1007/s00167-006-0173-z. [DOI] [PubMed] [Google Scholar]
- 40.Shepherd HM, Lam PH, Murrell GA. Synthetic patch rotator cuff repair: a 10-year follow-up. Shoulder Elb. 2013;6(1):35–39. doi: 10.1111/sae.12046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Soler AJ, Gidwani S, Curtis MJ. Early complications from the use of porcine dermal collagen implants (Permacol) as bridging constructs in the repair of massive rotator cuff tears. A report of 4 cases. Acta Orthop Belg. 2007;73(4):432–436. [PubMed] [Google Scholar]