Abstract
Background
Dietary diversity is one of the key elements of diet quality. Even though different measures were taken to increase dietary diversity feeding practice in Ethiopia, the problem still remains high. Therefore, this study was done to identify determinants of inadequate minimum dietary practice among children aged 6-59 months in Ethiopia.
Method
Secondary analysis of the data from the 2016 Ethiopian Demographic and Health Survey was done on a weighted sample of 5161 children aged 6-59 months. Data analysis was done using STATA v.14. Variables with P value < 0.05 in the bivariable analysis were candidates for the multivariable analysis to identify independent determinants of dietary diversity. Odds ratios (OR) were calculated at 95% confidence interval (CI).
Results
A total of 5161 children aged 6 to 59 months were enrolled in the study. Only 8.5% of the children had the recommended minimum dietary diversity. Mother's education (adjusted odds ratio (AOR) = 2.51 (1.65, 3.83)), mothers currently working (adjusted odds ratio (AOR) = 1.83 (1.47, 2.29)), mother's wealth index (adjusted odds ratio (AOR) = 4.75 (3.31, 6.81)), age of a child (adjusted odds ratio (AOR) = 1.72 (1.24, 2.39)), and number of under-five children (adjusted odds ratio (AOR) = 1.49 (1.12, 2.00)) were significantly associated with the minimum dietary diversity.
Conclusion
The minimum dietary diversity was not achieved by most children 6-59 months of age in Ethiopia. Ensuring large-scale interventions that focus on the identified factors should be considered by concerned bodies to improve the dietary diversity practice.
1. Background
Globally, malnutrition remains a serious burden of a public health concern. It affects social and economic development. It accounts directly or indirectly for 45% of the 5.9 million deaths of under-five children in 2015 [1]. This is the reason why adequate nutrition is identified as one of the pillars of public health interventions worldwide [2].
South Asia and sub-Saharan Africa are the home of a majority of the world's chronically undernourished children than elsewhere in the world [3]. Consequently, over 200 million African children under the age of five years suffer from malnutrition and fail to reach their full cognitive potential [4]. In Ethiopia, a child undernutrition is a major public health problem. The prevalence of stunting in under-five children in Ethiopia is 37% [5].
The main cause of malnutrition at the individual level is inadequate dietary diversity that does not provide adequate calories and micronutrients [6]. Micronutrient deficiency is a risk to children and is referred to as hidden hunger [7]. It is caused by chronic deficiency of vitamins and minerals as a consequence of nutrient inadequacy [8, 9].
Dietary assessment is an essential component of nutritional adequacy and provides information about the quantity and quality of food consumed in terms of nutrient adequacy and also consumption patterns and behaviors of the people [10]. It is a quantification of the number of different foods or food groups consumed over a reference time period [11]. The dietary diversity score has been identified as a potentially useful indicator of nutrient adequacy of children's diets [12–14]. This score can be used to assess the macro- and micronutrient consumption levels [15, 16].
The World Health Organization (WHO) recommends that children should consume foods from among the seven food groups [17]. Infant and Young Child Feeding (IYCF) practices recommend that children aged 6–23 months on breastfeeding should consume 4 or more other food groups daily [18]. Nonbreastfed children should consume milk or milk products, in addition to the four or more food groups [19].
The previous studies state about determinants of inadequate diet diversity practice, studies from Bangladesh [20], Dejen District, North West Ethiopia [21], and Malawi: findings from nationally representative data [22] showed that younger children and children from the poor household were less likely to meet the minimum dietary diversity. From the study finding in Myanmar [23] and Ghana [24], children from the illiterate mothers were less likely to meet the minimum dietary diversity. Despite poor dietary diversity which was visible among 6-59-month-old children in Ethiopia, however, a previous study in Ethiopia had identified determinants of dietary diversity among 6-23-month-old children [25].
Likewise, pouch studies were conducted on determinants of dietary diversity among 6-59-month-old children in various settings of the country and most shreds of evidence lack consistency and unrepresentative samples. Hence, until now, there was no population-based study permitting generalization about the determinant of dietary diversity among children 6-59 months. Therefore, this community-based and the national wide study was conducted to assess the determinant factors of minimum dietary diversity among age of six up to fifty-nine-month children. The result of this study will be used for national-level policymaking and programming by concerned bodies to intervene the identified gaps.
2. Methods
2.1. Study Setting
Ethiopia is located in the Horn of Africa. It is bordered by Eritrea to the north, Djibouti and Somalia to the east, Sudan and South Sudan to the west, and Kenya to the south. It has a high central plateau that varies from 1290 to 3000 m (4232 to 9843 ft) above sea level, with the highest mountain reaching 4533 m (14,872 ft). Ethiopia is home to about 13 million children under 5 years of age—approximately 16 percent of the total population of 96 million.
2.2. Data Source
The data source is nationally representative 2016 Ethiopian Demographic and Health Survey (EDHS) of children aged 6-59 months and their mothers. The survey was designed to provide population and health indicator estimates at the national, regional, and residence levels. The EDHS used a two-stage cluster sampling design with rural-urban and regions as strata yielding 21 sampling strata.
In the first stage, a total of 645 enumeration areas (EAs) were selected. For this study, child and women's data were extracted from the EDHS 2016 dataset. This analysis was restricted to the 5146 children aged 6-59 months having no missing value. The dataset used in this analysis contained information on the food items which was used to calculate the dietary diversity score.
2.3. Assessment of Dietary Diversity
The dietary quality of children was assessed using dietary diversity score. To measure dietary quality, we adopted the FAO 2011 Infant and Young Children Feeding (IYCF) guidelines. This was designed to measure dietary diversity for both breastfed and nonbreastfed children. The food items were categorized into seven major food groups based on the guidelines [26]. Structured 24-hour dietary recall of mothers was used to assess the foods consumed by the children.
2.4. Variables
2.4.1. Outcome Variable
The minimal dietary diversity is defined as the proportion of children aged 6–23 months who consumed at least four food groups out of the seven referenced food groups within a 24-hour time. These food groups are (1) grains, roots, and tubers; (2) legumes and nuts; (3) dairy products; (4) flesh foods (meats/fish/poultry); (5) eggs; (6) vitamin A-rich fruits and vegetables; and (7) other fruits and vegetables [27].
The group scores were then summed to obtain the dietary diversity score, which ranges from zero to seven, where zero represents nonconsumption of any of the food items and seven represents the highest level of diet diversification. Children who took at least four food groups in the last 24 hours before the interview were considered to have achieved the adequate minimum dietary diversity (MDD). Therefore, the outcome variable was categorized as 0 = adequate MDD and 1 = inadequate MDD.
2.4.2. The Independent Variables
The independent variables were identified from various literatures and grouped as characteristics of the family/household, child, parental, healthcare services, and the community. The child characteristics included sex, age, birth order, and having common childhood illnesses. The paternal characteristics included each parent's educational level, literacy level, working status, and maternal age marital status.
The wealth index and exposure to media were considered key household characteristics, whereas the place of residence (urban or rural) was considered a community-level variable. As health service characteristics, antenatal visits, place of delivery, and time of post natal care were included in this study.
3. Data Management and Analysis
Data analysis was carried out using STATA v.14; descriptive statistics were used to provide sample characteristics, including sociodemographic characteristics, individual, parental, household, healthcare, and community-level characteristics. Secondly, bivariate analysis between each explanatory variable and the outcome variable was done to determine the variables to include in the multivariable model.
Explanatory variables that were significantly associated with the outcome variable at P value less than 5% were included in the multivariable logistic regression model to identify independent determinants of MDD. Odds ratios (OR) were calculated to determine the strength of associations between independent variables and the outcome variable at 95% confidence interval (CI).
Sample weights were applied to compensate for the unequal probability of selection between the strata, which has also been geographically defined for nonresponses. A detailed explanation of the weighting procedure can be found in the EDHS methodology report [28]. We used “svy” in STATA v.14 to weight the survey data and perform the analyses. Variance inflation factor (VIF) > 10 was considered having multicollinearity effect.
4. Results
4.1. Sociodemographic Characteristics of Mothers
A total of 5161 children aged 6 to 59 months were enrolled along with their mothers in the study. The mean age (±SD) of the mothers was 27 ± 9.16 years. Out of the total mothers interviewed, almost half (2761) (53.5%) belong to the age group of 25–34 years. Two-thirds (3351) (64.9%) of the mothers' educational status were illiterate. Three-fourth (3889) (75.4%) of the mothers were not working at the time of data collection. (Table 1).
Table 1.
Sociodemographic characteristics and other characteristics of the mothers, EDHS 2016.
| Variables | Un weighted frequency | Un weighted percentage | Weighted frequency |
|---|---|---|---|
| Maternal | |||
| Age of mothers | |||
| <20 | 197 | 3.8 | 193 |
| 20-29 | 2761 | 53.5 | 2804 |
| 30-39 | 1906 | 36.9 | 2010 |
| ≥40 | 297 | 5.8 | 334 |
| Mother's educational level | |||
| Illiterate | 3351 | 64.9 | 3523 |
| Primarily | 1295 | 25.1 | 1481 |
| Secondary | 335 | 6.5 | 229 |
| Higher | 180 | 3.5 | 108 |
| Marital status | |||
| Never in union | 24 | 0.5 | 21 |
| Living with partner | 4920 | 95.3 | 5089 |
| Widowed | 41 | 0.8 | 57 |
| Divorced | 42 | 0.8 | 36 |
| No longer living together/separated | 98 | 2.6 | 91 |
| Religion | |||
| Orthodox | 1362 | 26.4 | 1454 |
| Catholic | 32 | 0.6 | 33 |
| Protestant | 835 | 16.1 | 821 |
| Muslin | 2837 | 55.0 | 2955 |
| Other and traditional | 95 | 1.9 | 35 |
| Mothers currently working | |||
| No | 3889 | 75.4 | 4030 |
| Yes | 1272 | 24.6 | 1311 |
| ANC visit | |||
| None | 892 | 31.6 | 1017 |
| 1-3 | 843 | 29.9 | 901 |
| >4 | 1085 | 38.5 | 1030 |
| Community related | |||
| Residence | |||
| Urban | 918 | 17.8 | 523 |
| Rural | 4243 | 82.2 | 4818 |
| Wealth index combined | |||
| Poorest | 1981 | 38.4 | 1396 |
| Poorer | 889 | 17.2 | 1226 |
| Middle | 731 | 14.2 | 1152 |
| Richer | 604 | 11.7 | 894 |
| Richest | 956 | 18.5 | 673 |
| Source of drinking water | |||
| Nonimproved | 2563 | 50.3 | 2216 |
| Improved | 2598 | 49.7 | 3125 |
4.2. Household- and Community-Related Factors
Greater than two-thirds of the household (3853) (74.5%) have greater than four number of household members, no radio (3855) (74.7%), and male household head (4103) (79.5%). More than three-fourths of the mothers (1981) (38.4%) were poorest and less than one-fourth 956 (18.5%) were richest wealth index. More than one-fourth of mothers (892) (31.6%) were not able to visit antenatal care in the health facilities. Majority of fathers are currently working (4635) (89.8%). Majority of the community were rural residence (4243) (82.2%), and greater than half of the community 2563 (57.2%) were using unsafe drinking water (Table 1).
4.3. Child Characteristics
Nearly equal number of female (2590) (50.2%) and male (2571) (49.8%) children participated in the study. The mean (±SD) age was 26.6 months (SD ±2.1).Breastfeeding is common in Ethiopia, and most children (4451) (86.2%) were still breastfed during their second year of life. From the total of children, 1905 (37%) of them were in the age group 12-23 months. More than two-thirds (3710) (71%) of the households have less than three number of children. More than half (2790) (54.1) of children in this study were not taking vitamin A in the last 6 months (Table 2).
Table 2.
Sociodemographic characteristics and other characteristics of the mothers and children, EDHS 2016.
| Variables | Categories | MDDS | Odds ratio (95% CI) |
|---|---|---|---|
| Age of the child in months | |||
| 6-11 | 1014 | 19.6 | 1065 |
| 12-23 | 1907 | 37.0 | 1988 |
| 24-35 | 460 | 8.9 | 438 |
| 36-47 | 886 | 17.2 | 906 |
| Sex of the child | |||
| Male | 2571 | 49.8 | 2614 |
| Female | 2590 | 50.2 | 2727 |
| Birth interval of the child | |||
| First order | 1084 | 21.0 | 1030 |
| <24months | 1049 | 20.3 | 974 |
| ≥24months | 3028 | 58.7 | 3337 |
| Birth order | |||
| ≤3 | 2779 | 53.8 | 2713 |
| >3 | 2382 | 46.2 | 2628 |
| Number of under-5 children | |||
| <3 | 3710 | 71.9 | 4005 |
| ≥3 | 1451 | 28.1 | 1336 |
| Minimal dietary score | |||
| ≤3 | 4722 | 91.5 | 4853 |
| ≥4 | 439 | 8.5 | 488 |
| Currently breast feeding | |||
| Yes | 4451 | 86.2 | 4748 |
| No | 710 | 13.8 | 593 |
| Had diarrhea recently | |||
| No | 4510 | 87.4 | 4622 |
| Yes, last two weeks | 643 | 12.5 | 711 |
4.4. Frequency of Dietary Diversity
The dietary diversity determined based on a 24 h recall method showed that only 439 (8.5%) of the children had received the recommended minimum dietary diversity (children who fed four or more food items within 24 h preceding data collection) (Table 2). Grains, tubers, and roots (4490) (86.9%) were consumed by the greatest number of children within 24 hours preceding the survey. However, the intake of flesh food or organ meat was low, of the total children, only 392 (7.4%) (Figure 1).
Figure 1.
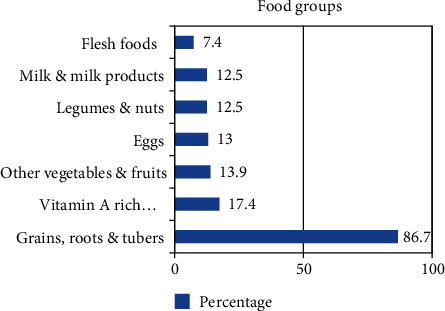
Food groups consumed among 6-59-month-old children in the last 24 hours, Ethiopian Demographic and Health Survey 2016 (n = 5161).
The dietary diversity determined based on a 24 h recall method among children showed that there were great variations among different regions of Ethiopia. Children in Addis Ababa (capital city) had received the highest recommended minimum dietary diversity (25%), and children in the following regions had received the least recommended minimal dietary diversity: Afar (0.6%), Somali (1.9%), Amhara (2.2%), and Tigray (7%) (Figure 2). Children born from mothers who had the highest wealth index have high percentage of using minimal dietary diversify food groups than those who had the poorest wealth index (Figure 3).
Figure 2.
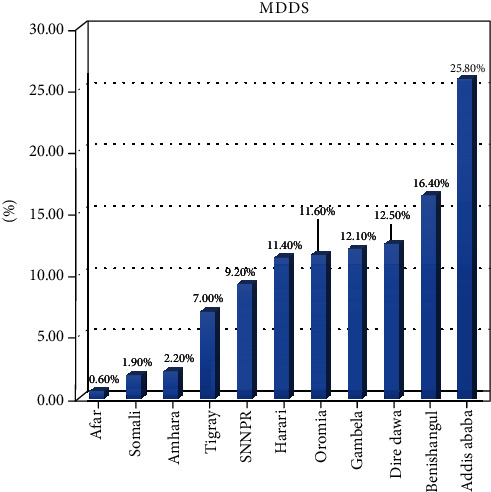
Regional variation of MDDS, Ethiopian Demographic and Health Survey 2016 (n = 5161).
Figure 3.
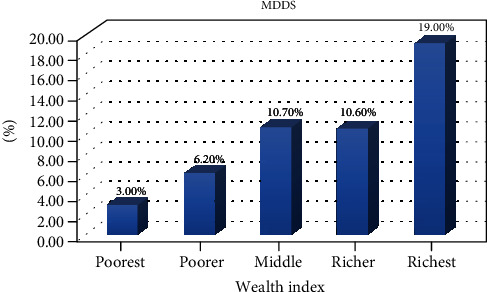
Wealth index of the households and MDDS, Ethiopian Demographic and Health Survey 2016 (n = 5161).
4.5. Factors Which Predict Dietary Diversity
In the binary logistic regression, mother's educational status, husband's educational status, mother currently working, residence, wealth index, child age, birth order, the birth interval of the child, number of under-five children, the household has radio, and the household has television were significantly associated.
The study found that children born from mothers who had the highest education level (adjusted odds ratio (AOR) = 2.51 (1.65, 3.83)) had greater odds of feeding diversified foods. Another most vital factor significantly associated with minimum dietary diversity was the age of a child. Children aged 12–23 months ((AOR 1.72; 95% CI (1.24, 2.39)) have a minimum dietary diversity compared to children aged 6–11 months.
It was found that mother's working status had a significant association with dietary diversity. Children born from mother currently working (AOR 1.83; 95% CI (1.47, 2.29)) have a higher odds of having the minimum dietary diversity compared with those born from mother not currently working.
This study also indicated that wealth index had a significant association with dietary diversity. Children born from mother's wealth index of richest (AOR 4.75; 95% CI (3.31, 6.81)), richer (AOR 3.23; 95% CI (2.19, 4.77)), middle (AOR 3.63; 95% CI (2.52, 5.23)), and poorer (AOR 1.95; 95% CI (1.32, 2.89)) have higher odds of having the minimum dietary diversity compared with those born from poorest mothers.
Furthermore, this study revealed that the number of under-five children in the household had a significant association with dietary diversity. The number of children less than three in the household (AOR 1.49; 95% CI (1.12, 2.01)) has higher odds of having the minimum dietary diversity compared with greater than three number of children (Table 3).
Table 3.
Bivariate and multivariable logistic regression between different level predictors and minimum dietary diversity of children aged 6–59 months, EDHS 2016.
| Variables | Categories | MDDS | Odds ratio (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| <4 (n (%) | ≥4 (n (%) | COR (95% CI) | P value | AOR (95% CI) | P value | ||
| Mother's educational status | Illiterate | 196 (5.8) | 3155 (94.2) | 1 | 1 | ||
| Primary | 134 (10.3) | 1161 (89.7) | 1.858 (1.476, 2.339) | <0.001∗ | 1.270 (0.989, 1.631) | 0.061 | |
| Secondary | 51 (15.2) | 284 (84.8) | 2.891 (2.076, 4.025) | <0.001∗ | 1.322 (0.900, 1.941) | 0.155 | |
| Higher | 58 (32.2) | 122 (67.8) | 7.653 (5.424, 10.798) | <0.001∗ | 2.514 (1.651,3.829) | <0.001∗ | |
|
| |||||||
| Husband's educational status | No education | 121 (5.0) | 2322 (95.0) | 0.222 (0.162, 0.305) | <0.001∗ | 0.759 (0.486, 1.184) | 0.224 |
| Primarily | 151 (9.2) | 1492 (90.8) | 0.432 (0.317, 0.588) | <0.001∗ | 0.924 (0.613, 1.393) | 0.706 | |
| Secondary | 74 (14.8) | 427 (85.2) | 0.740 (0.517, 1.057) | 0.098 | 1.141 (0.758, 1.717) | 0.528 | |
| Higher | 71 (19.0) | 303 (81.0) | 1 | ||||
|
| |||||||
| Age of mothers at birth | <20 | 16 (8.1) | 181 (91.9) | 1 | |||
| 20-29 | 228 (8.3) | 2533 (91.7) | 1.018 (600, 1.728) | 0.947 | |||
| 30-39 | 173 (9.1) | 1733 (90.9) | 1.129 (0.662, 1.927) | 0.656 | |||
| ≥40 | 22 (7.4) | 275 (92.6) | 0.905 (0.463, 1.770) | 0.771 | |||
|
| |||||||
| Mother currently working | Not working | 252 (6.5) | 3637 (93.5) | 1 | 1 | ||
| Working | 187 (14.7) | 1085 (85.3) | 2.487 (2.035, 3.041) | <0.001∗ | 1.833 (1.468, 2.288) | <0.001∗ | |
|
| |||||||
| Residence | Rural | 269 (6.3) | 3974 (93.7) | 1 | 1 | ||
| Urban | 170 (18.5) | 748 (81.5) | 3.358 (2.729, 4.131) | <0.001∗ | 1.307 (0.865, 1.974) | 0.204 | |
|
| |||||||
| Wealth index | Poorest | 60 (3.0) | 1921 (97.0) | 1 | 1 | ||
| Poorer | 55 (6.2) | 834 (93.8) | 2.111 (1.451, 3.071) | <0.001∗ | 1.955 (1.322, 2.890) | 0.001∗ | |
| Middle | 78 (10.7) | 653 (89.3) | 3.824 (2.700, 5.417) | <0.001∗ | 3.631 (2.519, 5.233) | <0.001∗ | |
| Richer | 64 (10.6) | 540 (89.4) | 3.795 (2.634, 5.466) | <0.001∗ | 3.235 (2.195, 4.766) | <0.001∗ | |
| Richest | 182 (19.0) | 774 (81.0) | 7.528 (5.558, 10.198) | <0.001∗ | 4.746 (3.308, 6.809) | <0.001∗ | |
|
| |||||||
| Child age (months) | 6-11 | 80 (7.9) | 934 (92.1) | 1.307 ((0.915, 1.865) | 0.141 | 1.078 (0.738, 1.575) | 0.697 |
| 12-23 | 227 (11.9) | 1680 (88.1) | 2.061 (1.518, 2.799) | <0.001∗ | 1.720 (1.240, 2.387) | 0.001∗ | |
| 24-35 | 23 (5.0) | 437 (95.0) | 0.803 (0.487, 1.324) | 0.390 | 0.991 (0.582, 1.688) | 0.974 | |
| 36-47 | 54 (6.1) | 832 (93.9) | 0.990 (0.672, 1.459) | 1.079 (0.715, 1.628) | 0.717 | ||
| 48-59 | 55 (6.2) | 839 (93.8) | 1 | 1 | |||
|
| |||||||
| Sex of the child | Male | 211 (8.2) | 2360 (91.8) | 0.926 (0.762, 1.126) | 0.443 | ||
| Female | 228 (8.8) | 2362 (91.2) | 1 | ||||
|
| |||||||
| Birth order | ≤3 | 281 (10.1) | 2498 (89.9) | 1 | |||
| >3 | 158 (6.6) | 2224 (93.4) | 0.632 (0.515, 0.774) | <0.001∗ | 1.008 (0.775, 1.311) | 0.951 | |
|
| |||||||
| Birth interval of the child | First order | 126 (11.6) | 958 (88.4) | 1 | |||
| <24 months | 59 (5.6) | 990 (94.4) | 0.453 (0.328, 0.625) | <0.001∗ | 0.889 (0.607, 1.302) | 0.889 | |
| ≥24months | 254 (8.4) | 2774 (91.6) | 0.696 (0.555, 0.873) | 0.002∗ | 0.932 (0.716, 1.214) | 0.932 | |
|
| |||||||
| Number of under 5 children | <3 | 367 (9.9) | 3343 (90.1) | 12.103 (1.621, 2.728) | <0.001∗ | 1.497 (1.118, 2.004) | 0.007∗ |
| ≥3 | 72 (5.0) | 1379 (95.0) | 1 | 1 | |||
|
| |||||||
| HH has radio | Yes | 163 (13.0) | 1094 (87.0) | 1 | 1 | ||
| No | 276 (7.1) | 3628 (92.9) | 0.511 (0.416, 0.627) | <0.001∗ | 0.812 (0.645, 1.023) | 0.812 | |
|
| |||||||
| HH has television | Yes | 151 (21.5) | 552 (78.5) | 1 | |||
| No | 288 (6.5) | 4170 (93.5) | 0.252 (0.203, 0.313) | <0.001∗ | 0.719 (0.486, 1.063) | 0.719 | |
|
| |||||||
| Sex of HH head | Male | 359 (8.7) | 3744 (91.3) | 1 | |||
| Female | 80 (7.6) | 978 (92.4) | 0.853 (0.663, 1.098) | 0.217 | |||
Maximum SE 0.272; Hosmer and Lemeshow 0.169; COR: crude odds ratio; AOR: adjusted odds ratio.
5. Discussion
This community-based cross-sectional study assessed determinants of minimum dietary diversity among children aged 6-59 months in Ethiopia. The main goal of dietary diversity is to promote households to consume diversified diets rather than consuming repetitive diets throughout twenty-four hours.
This study revealed that only 8.5% of children received minimum dietary diversity throughout twenty-four hours. The finding is similar to a study done in Dembecha, northwest Ethiopia (8.6%) [29], and Gorche District, Southern Ethiopia (10.6%) [30].
Furthermore, it is higher than the study in Kenya (6.8%) [31]. However, it is lower compared to the study conducted in Rwanda and Burundi Demographic and Health Surveys (Rwanda 23%, Burundi 16%) [32]; Tanzania [33]; Addis Ababa, Ethiopia 59.9% [34]; and Morondava (47.6%) and Moramanga (42.1%) districts of Madagascar, respectively [35].
The differences might be due to the fact that this study was community-based; the overall estimate of minimum dietary diversity could be lower than small-scale and health facility-based studies. These differences might be also due to variations in socioeconomic status, dietary habit, culture, study design, and self-reported measurement, and recall method could also affect the estimated minimum dietary diversity.
Children born from illiterate mothers were less likely to practice minimum dietary diversity.
It was concurrent with a study conducted in Wolaita Sodo town, Southern Ethiopia [36], Northwest Ethiopia [37], and urban Zambia [38]. We also show that a low education level of mothers increased the likelihood of having a low dietary diversity score. Similar report is also observed in Madagascar and Afar, North Ethiopia [35, 39].
The possible reason might be as the education level of the mother increased and as the mother engaged in paid work, there is access to more information on educational messages and different mass media like radio, television, and newspaper. They also participate actively in health education sessions and child feeding demonstrations in health facilities; as a result, their children are more likely to fulfill the minimum dietary diversity requirement.
Another important determinant of the minimum dietary diversity of children in the study area is household economical status. Similar results are observed in Nepal DHS (26%) [40], Dejen District, North West Ethiopia, and the Philippines [21, 41]. This may indicate that family income has a direct association with household food security, since food consumption is believed to be heavily influenced by income of the household.
There is also a regional variation for the requirement of minimum dietary diversity score among 6-59-month-old children in Ethiopia. This might be due to differences in agroecology, feeding habits, lifestyles, and demography among the regions. The places with the highest minimum dietary diversity score are in Addis Ababa, Ethiopia, and lowest in nomadic regions (Afar and Somali). This might be because Addis Ababa is located in the urban center, the capital city of Ethiopia; mothers' might have easy access to information, market, and health services about dietary diversity and child feeding practices.
Children age 12–23 months were significantly associated with minimum dietary diversity. This might be due to infant's mothers during 6–11 months who did not introduce solid and semisolid food; they are only introducing simply feeding milk along with breast milk. Many children in the household have less minimum dietary diversity intake than older children.
In this study, the number of children in the household is significantly associated with minimum dietary diversity. A possible explanation might be families with many numbers of children are less likely to purchase diversified food groups and unable to fulfill their children's dietary requirement.
5.1. Limitation of the Study
The major limitation of this study was its cross-sectional design, which does not allow the identification of the precedence in time between exposure and end point.
6. Conclusion
Less than one-fifth of the children aged 6–59 months received minimum dietary diversity in Ethiopia. Mother's education level, mothers' wealth index, mothers' working status, age of a child, and number of under-five children were the factors statistically associated with minimum dietary diversity of children aged 6–59 months. Interventions which focus on improving the socioeconomic status of households, educational status of mothers, and diversified food consumption of children aged 6-59 months should be strengthened.
Acknowledgments
Our sincere and deepest gratitude goes to Tigray Health Research Institute for creating a conducive environment to analyze the DHS data. We are also very grateful to Measure DHS for making the data freely available.
Abbreviations
- AOR:
Adjusted odds ratio
- EA:
Enumeration areas
- EDHS:
Ethiopian Demographic and Health Survey
- MDDS:
Minimum dietary diversity score
- IYCF:
Infant and Young Child Feeding
- VIF:
Variance inflation factor.
Data Availability
The data used to analyze the current study are available from the corresponding author upon reasonable request.
Ethical Approval
Ethical clearance was obtained from the Institutional Review Board of Tigray Health Research Institute, and the analyses of this study are confined to secondary data, approval to analyze the secondary data is requested from the CSA or ORC Macro (Demographic and Health Survey), and we have been authorized to download data from the Demographic and Health Surveys (DHS) online.
Conflicts of Interest
The authors declare that they have no competing interests relevant to this manuscript.
Authors' Contributions
A.G. contributed to the concept and data collection tool; conducted data collection, analysis, and interpretation of data; and wrote the first draft of the manuscript and revised it. AD, AB, TW, and GG contributed to the concept, participated in protocol development, reviewed the assessment tool, and reviewed analysis findings, and KF revised the draft and final manuscript. All authors read and approved the final manuscript.
References
- 1.WHO. WHO|Children: reducing mortality. July 2016, http://www.who.int/mediacentre/factsheets/fs178/en/
- 2.Elmadfa I., Meyer A. L. Importance of food composition data to nutrition and public health. European Journal of Clinical Nutrition. 2010;64(S3):S4–S7. doi: 10.1038/ejcn.2010.202. [DOI] [PubMed] [Google Scholar]
- 3.Black R. E., Victora C. G., Walker S. P., et al. Maternal and child undernutrition and overweight in low-income and middle- income countries. The Lancet. 2013;382(9890):427–451. doi: 10.1016/s0140-6736(13)60937-x. [DOI] [PubMed] [Google Scholar]
- 4.Grantham-McGregor S., Cheung Y. B., Cueto S., Glewwe P., Richter L., Strupp B. Developmental potential in the first 5 years for children in developing countries. The Lancet. 2007;369(9555):60–70. doi: 10.1016/S0140-6736(07)60032-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO. Ethiopia Mini Demographic and Health Survey. WHO; 2019. [Google Scholar]
- 6.UNICEF. Joint child malnutrition estimates—levels and trends. 2013. p. p. 2014.
- 7.Ruel-Bergeron J. C., Stevens G. A., Sugimoto J. D., et al. Global update and trends of hidden hunger, 1995-2011: the hidden hunger index. PLoS One. 2015;10(12, article e0143497) doi: 10.1371/journal.pone.0143497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ruel M. T., Deitchler M., Arimond M. Developing simple measures of Women's diet quality in developing countries: overview. The Journal of Nutrition. 2010;140(11):2048S–2050S. doi: 10.3945/jn.110.123695. [DOI] [PubMed] [Google Scholar]
- 9.Wieser S., Plessow R., Eichler K., et al. Burden of micronutrient deficiencies by socio-economic strata in children aged 6 months to 5 years in the Philippines. BMC Public Health. 2013;13(1) doi: 10.1186/1471-2458-13-1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maqbool A., Olsen I. E., Stallings V. A. Nutrition in Pediatrics. basic science and clinical applications. 4th. Hamiliton: BC Decker Inc; 2008. Clinical assessment of nutritional status; pp. 5–12. [Google Scholar]
- 11.Wiesmann D., Bassett L., Benson T., Hoddinott J. International Food Policy Research & Institute (IFPRI); 2009. Validation of the world food programmer’s food consumption score and alternative indicators of household food security. April 2015, http://www.indiaenvironmentportal.org.in/files/validation-wfp.pdf. [Google Scholar]
- 12.Hatloy A., Torheim L. E., Oshaug A. Food variety–a good indicator of nutritional adequacy of the diet? A case study from an urban area in Mali, West Africa. European Journal of Clinical Nutrition. 1998;52(12):891–898. doi: 10.1038/sj.ejcn.1600662. [DOI] [PubMed] [Google Scholar]
- 13.Steyn N. P., Nel J. H., Nantel G., Kennedy G., Labadarios D. Food variety and dietary diversity scores in children: are they good indicators of dietary adequacy. Public Health Nutrition. 2006;9(5):644–650. doi: 10.1079/phn2005912. [DOI] [PubMed] [Google Scholar]
- 14.Moursi M. M., Arimond M., Dewey K. G., Treche S., Ruel M. T., Delpeuch F. Dietary diversity is a good predictor of the micronutrient density of the diet of 6- to 23-month-old children in Madagascar. The Journal of Nutrition. 2008;138(12):2448–2453. doi: 10.3945/jn.108.093971. [DOI] [PubMed] [Google Scholar]
- 15.Steyn N. P., Nel J., Labadarios D., Maunder E. M. W., Kruger H. S. Which dietary diversity indicator is best to assess micronutrient adequacy in children 1 to 9 y? Nutrition. 2014;30(1):55–60. doi: 10.1016/j.nut.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 16.Gewa C., Leslie T. Young child complementary food diversity in the east African region: 409 cross-country differences, geographic distribution and relationship with health-care utilization. The FASEB Journal. 2013;27(1):p. 411. [Google Scholar]
- 17.Menon P. The crisis of poor complementary feeding in South Asia: where next? Maternal & Child Nutrition. 2012;8:1–4. doi: 10.1111/j.1740-8709.2011.00394.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ethiopia Central Statistical Agency and ICF International. 2011 Ethiopia Demographic and Health Survey. Key findings. Calverton: Ethiopia Central Statistical Agency and ICF International; 2012. [Google Scholar]
- 19.EthiopiaFdro. National nutrition program. 2016-2020.
- 20.Ali N. B., Tahsina T., Hoque D. M. E., et al. Association of food security and other socio-economic factors with dietary diversity and nutritional statuses of children aged 6-59 months in rural Bangladesh. PLoS One. 2019;14(8, article e0221929) doi: 10.1371/journal.pone.0221929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kumera G., Tsedal E., Ayana M. Dietary diversity and associated factors among children of Orthodox Christian mothers/caregivers during the fasting season in Dejen District, North West Ethiopia. Nutrition & Metabolism. 2018;15(1) doi: 10.1186/s12986-018-0248-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jones A. D., Shrinivas A., Bezner-Kerr R. Farm production diversity is associated with greater household dietary diversity in Malawi: findings from nationally representative data. Food Policy. 2014;46:1–12. doi: 10.1016/j.foodpol.2014.02.001. [DOI] [Google Scholar]
- 23.Hein A. K., Hong S. A., Puckpinyo A., Tejativaddhana P. Dietary diversity, social support and stunting among children aged 6–59 months in an internally displaced persons camp in Kayin State, Myanmar. Clinical Nutrition Research. 2019;8(4):307–317. doi: 10.7762/cnr.2019.8.4.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Issaka A. I., Agho K. E., Burns P., Page A., Dibley M. J. Determinants of inadequate complementary feeding practices among children aged 6–23 months in Ghana. Public Health Nutrition. 2015;18(4):669–678. doi: 10.1017/s1368980014000834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eshete T., Kumera G., Bazezew Y., Mihretie A., Marie T. Determinants of inadequate minimum dietary diversity among children aged 6–23 months in Ethiopia: secondary data analysis from Ethiopian Demographic and Health Survey 2016. Agriculture & Food Security. 2018;7(1) doi: 10.1186/s40066-018-0219-8. [DOI] [Google Scholar]
- 26.WHO. Report of proceedings, WHO; 2008. Strengthening action to improve feeding of infants and young children 6–23 months of age in nutrition and child health programmers. https://www.who.int/maternal_child_adolescent/documents/9789241597890/en/ [Google Scholar]
- 27.World Health Organization. World Health Statistics 2018: Monitoring Health for the SDGs Sustainable Development Goals. World Health Organization; 2018. [Google Scholar]
- 28.Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia demographic and health survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF; 2016. [Google Scholar]
- 29.Mulat E., Alem G., Woyraw W., Temesgen H. Uptake of minimum acceptable diet among children aged 6–23 months in orthodox religion followers during fasting season in rural area, DEMBECHA, north West Ethiopia. BMC Nutrition. 2019;5(1) doi: 10.1186/s40795-019-0274-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dangura D., Gebremedhin S. Dietary diversity and associated factors among children 6-23 months of age in Gorche district, Southern Ethiopia: Cross-sectional study. BMC Pediatrics. 2017;17(1):p. 6. doi: 10.1186/s12887-016-0764-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kiboi W., Kimiywe J., Chege P. Determinants of dietary diversity among pregnant women in Laikipia County, Kenya: a cross-sectional study. BMC Nutrition. 2017;3(1) doi: 10.1186/s40795-017-0126-6. [DOI] [Google Scholar]
- 32.Custodio E., Herrador Z., Nkunzimana T., Węziak-Białowolska D., Perez-Hoyos A., Kayitakire F. Children’s dietary diversity and related factors in Rwanda and Burundi: a multilevel analysis using 2010 Demographic and Health Surveys. PLoS One. 2019;14(10, article e0223237) doi: 10.1371/journal.pone.0223237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Khamis A. G., Mwanri A. W., Ntwenya J. E., Kreppel K. The influence of dietary diversity on the nutritional status of children between 6 and 23 months of age in Tanzania. BMC Pediatrics. 2019;19(1):p. 518. doi: 10.1186/s12887-019-1897-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Solomon D., Aderaw Z., Tegegne T. K. Minimum dietary diversity and associated factors among children aged 6–23 months in Addis Ababa, Ethiopia. International Journal for Equity in Health. 2017;16(1):p. 181. doi: 10.1186/s12939-017-0680-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rakotonirainy N. H., Razafindratovo V., Remonja C. R., et al. Dietary diversity of 6- to 59-month-old children in rural areas of Moramanga and Morondava districts, Madagascar. PLoS One. 2018;13(7, article e0200235) doi: 10.1371/journal.pone.0200235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mekonnen T. C., Workie S. B., Yimer T. M., Mersha W. F. Meal frequency and dietary diversity feeding practices among children 6–23 months of age in Wolaita Sodo town, Southern Ethiopia. Journal of Health, Population and Nutrition. 2017;36(1):p. 18. doi: 10.1186/s41043-017-0097-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Beyene M., Worku A. G., Wassie M. M. Dietary diversity, meal frequency and associated factors among infant and young children in Northwest Ethiopia: a cross- sectional study. BMC Public Health. 2015;15(1) doi: 10.1186/s12889-015-2333-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mallard S. R., Houghton L. A., Filteau S., et al. Dietary diversity at 6 months of age is associated with subsequent growth and mediates the effect of maternal education on infant growth in urban Zambia. The Journal of Nutrition. 2014;144(11):1818–1825. doi: 10.3945/jn.114.199547. [DOI] [PubMed] [Google Scholar]
- 39.Wuneh A. G., Ahmed W., Bezabih A. M., Reddy P. S. Dietary diversity and meal frequency practices among children aged 6-23 months in agro pastoral communities in Afar region, Ethiopia: a cross-sectional study. Ecology of Food and Nutrition. 2019;58(6):575–596. doi: 10.1080/03670244.2019.1644328. [DOI] [PubMed] [Google Scholar]
- 40.Baek Y., Chitekwe S. Sociodemographic factors associated with inadequate food group consumption and dietary diversity among infants and young children in Nepal. PLoS One. 2019;14(3, article e0213610) doi: 10.1371/journal.pone.0213610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Guirindola M. O., Maniego M. L. V., Silvestre C. J., Acuin C. C. S. Minimum acceptable diet among Filipino children aged 6-23 months. Philippine Journal of Science. 2018;147(1) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to analyze the current study are available from the corresponding author upon reasonable request.


