Abstract
COVID-19 pandemic, in addition to being a global health emergency, has multiple socioeconomic and psychological ramifications. COVID-19 research and media reports have revealed a rise in fears related to contracting the virus. Though fear is a common psychological outcome during pandemics, the COVID-19 pandemic is a continuously evolving disease outbreak and has unique risk factors. Therefore, fear related to COVID-19 might manifest in not only fear and anxiety related to disease contraction and dying, but also associated sociooccupational stress. We attempt to understand the psychosocial process of the development of coronaphobia and postulate what constitutes coronaphobia, a new emerging phobia specific to COVID-19. We present a conceptual model delineating the risk factors causing coronaphobia and the underlying mechanisms, for a better understanding of its developmental process. From review of relevant research, the factors identified are, an unforeseen reality, unending uncertainties, need of acquiring new practices and avoidance behavior, loss of faith in health infrastructure, contraction of COVID-19 by head of states, cautionary statements from international bodies, and infodemia. These factors are assumed to cause interference with routine life, catastrophizing interpretation of benign symptoms, and social amplification of risk which lead to coronaphobia. The conceptualization of coronaphobia and the model will aid future research in developing psychometric measure of coronaphobia for use in clinical and research settings and design of policies and interventions for mitigating risk factors.
Keywords: COVID-19, Coronaphobia, Fear, Anxiety, Pandemic
1. Introduction
In the COVID-19 pandemic, as in other pandemics, fear, anxiety, and worries have been the major psychological consequences (Roy et al., 2020; Tandon, 2020a; Xiang et al., 2020). COVID-19 related fear, mortality rates, unemployment, protective strategies have become the most searched topics in Google search history (Charlton, 2020; Sullivan, 2020). Researchers have used the expressions “fear of COVID-19” (Ahorsu et al., 2020; Mertens et al., 2020) and ‘coronaphobia’ (Asmundson and Taylor, 2020) to indicate the fear of contracting COVID-19. Now that there is unanimity that COVID-19 is an endemic (BBC, 2020b; Kissler et al., 2020) and living with the coronavirus with constant precautions becomes the new normal, fear may become more pronounced (Tanner, 2020). COVID-19 affects all spheres of life and the risk factors are more unique, numerous, and diverse than in other pandemics. Therefore, fear may extend beyond falling ill or dying due to contracting the virus and evoke other fears such as that of economic adversity (Yoon, 2020) and infecting others. This paper attempts to postulate the contents and antecedents of coronaphobia, identify the associated risk factors and the underlying mechanisms of its development which might inform policy decisions and healthcare activities.
2. Conceptualizing coronaphobia
A phobia is an anxiety disorder characterized by persistent, excessive, unrealistic fear of an object, person, animal, activity or situation. Phobia makes people avoid the triggers of fear; when such avoidance is not possible, it causes anxiety and distress (American Psychiatric Association, 2013).
A search in the Scopus database using the keywords "COVID-19" and "Coronavirus" with "fear", "anxiety/anxious", "uncertainty", "worry/worries/worried", "phobia", "public place" and "public transport" resulted in 499 studies after excluding studies with no abstract or in a language other than English. Various components and outcomes of COVID-19 fear have been reported such as functional impairment leading to hopelessness, suicidal ideation, and coping deficits (Lee, 2020), fatal cognitions leading to association of COVID-19 with terminal end (Dubey et al., 2020; Goyal et al., 2020), and anxiety and depression while coping with the ‘new normal’ (Cao et al., 2020; Chakraborty and Chatterjee, 2020; Haleem et al., 2020, Huang and Zhao, 2020).
Based on a review of these studies, we define coronaphobia as an excessive triggered response of fear of contracting the virus causing COVID-19, leading to accompanied excessive concern over physiological symptoms, significant stress about personal and occupational loss, increased reassurance and safety seeking behaviors, and avoidance of public places and situations, causing marked impairment in daily life functioning. The triggers involve situations or people involving probability of virus contraction, such as, meeting people, leaving house, travelling, reading the updates or news, falling ill or going for work outside.
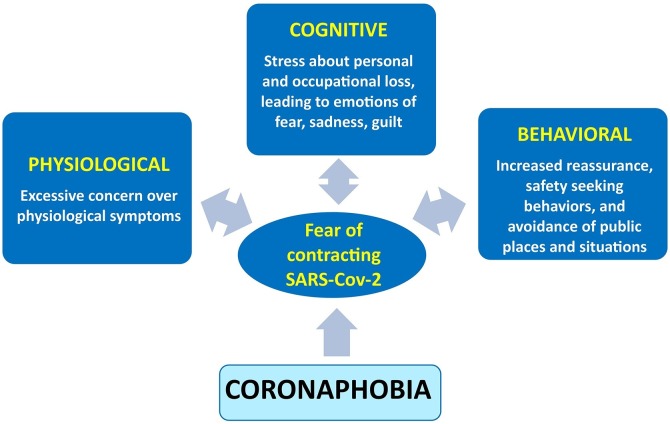
The definition implies three essential components (Figure 1 ), which reinforces the process of fear:
-
i
Physiological: The fight or flight response of fear is triggered, on being exposed to antecedent event. Constant worry can cause symptoms such as palpitations, tremors, difficulty in breathing, dizziness, change in appetite, and sleep (Wang et al., 2020).
-
ii
Cognitive: Fear of virus would involve preoccupation with threat provoking cognitions (Chakraborty and Chatterjee, 2020), e.g. ‘I will die if I contract the virus, ‘I will not be able to go to my job and will be unemployed’; ‘My family is under danger and they may die’. The cognitions may further trigger emotional responses, like sadness, guilt, and anger.
-
iii
Behavioral: In order to prevent the consequences, individuals engage in avoidance behaviors. There is marked fear of using public transportation, touching any surface, being at open places (markets, beaches, stadiums) and at enclosed places (hotels, shopping malls, movie theatres, indoor stadiums), attending any public gatherings, and standing in queue (Tanner, 2020). The individual fears and/or avoids situations like meeting people or overindulges into health-related safety behaviors (like washing hands). Reassurance behaviors such as constantly checking body vitals, confirming absence of illness, self-medicating or rechecking sanitation perpetuates fear (Li et al., 2020), leading to phobia. Besides, the zoonotic origin of the virus (Andersen et al., 2020), may further lead to the fear of having exotic meat based food. Though the fear is realistic, it can disturb the overall quality of everyday functioning of the individual.
Fig. 1.
Coronaphobia and its components.
2.1. Comparing coronaphobia with other phobias
To understand the spectrum of pathology where coronaphobia belongs, we present a comparative analysis with three other phobias as laid down in DSM-5 (American Psychiatric Association, 2013) (Table 1 ). We observe fear of specific stimuli in all kinds of phobia, accompanying triggered physiological responses, cognitions of lack of control, helplessness, and/or death. Phobias share pattern of behavioral avoidance and reassurance which is beyond realistic proportions. While coronaphobia shares similarities with the other phobias, the fear in it is not only limited to public places/situations/objects, but, primarily coming in contact with humans, physically. Given the novelty and transmission rate of the COVID-19, the coronaphobia is intense, widespread, and involves sociooccupational and personal domains, with apprehensions ranging beyond the self and the present time. It might be perceived as an equivalent entity in syndromes of phobia, given the presence of unique triggers and fear of the unknown.
Table 1.
A comparative analysis of phobias in DSM-5 with coronaphobia.
| Domains | Agoraphobia | Social phobia | Specific phobia | Coronaphobia (as proposed) |
| Feared stimuli | Places and situations that might cause panic, helplessness or embarrassment. | Social situations where individual is exposed to possible scrutiny by others | Fear about a specific object or situation (e.g. flying, heights, animals, etc.) | Fear of contracting SARS-CoV-2 and/or dying of it and socio-personal-occupational loss |
| Physiological response | Rapid heart rate, excessive sweating, trouble breathing, tingling | Rapid heart rate, trouble breathing, sweating, trembling, dry mouth, stumbling speech | Palpitations, sweating, trembling, trouble breathing, dry mouth | Rapid heart rate, trouble breathing, sweating, sleep disturbances/ deprivation |
| Cognition | If I go there, I am going to be completely unable to breathe and die! | I am looking like a fool, people will think I am stupid! | The snake is venomous, it will kill me! | If I get coronavirus disease, I will die, lose job, infect others! |
| Behavioral manifestations | Active avoidance of situations where a person fears getting a panic attack, or embarrassing symptoms; seeking reassurance of a support. | Active avoidance of social situations; failing to speak to people; clinging to support (in children). | Active avoidance of object or situation; freezing behavior; clinging to support (in children) | Active avoidance of public places, transportation, objects and/or people; reassurance of not having illness; safety seeking behavior to prevent infection. |
| Intensity of fear | Out of realistic proportion | Out of realistic proportion | Out of realistic proportion | Out of realistic proportion |
2.2. Risk factors of coronaphobia
Traumatic events can lead to specific phobias (Garcia, 2017). With 377,889 casualties, and 6,389,493 confirmed cases in 213 countries and territories (Worldometer, 2020a), and global socioeconomic and political consequences, the COVID-19 pandemic is a traumatic event of greater proportions than previous disease outbreaks of recent times. Given below are the factors that make COVID-19 pandemic unique and form the basis for development of coronaphobia.
2.2.1. The unending uncertainties
The uniqueness of the COVID-19 pandemic lies in the uniqueness of the agent, SARS-Cov-2. Even after five months of being identified, studies are still divided whether the SARS-Cov-2 originated due to zoonotic transfer, through either Malayan Pangolins or bats (Anderson et al., 2020) or whether it is a lab-engineered virus (Goodenough, 2020). The genetic mutation of the virus is quite mysterious with asymptomatic cases, fast mutation, incubation period of 2–14 days with some cases even reaching 19–27 days, adaptability to changing environments, and variable strains (Kaplan et al., 2020; Kumar, 2020; Worldometer, 2020b).
2.2.2. Unforeseen reality
Change in any form is threatening initially, as it disturbs the equilibrium and the stability, seeding insecurity. The enforced instability due to COVID-19 is threatening, compulsive, and unpleasing. The terms — lockdown, quarantine, and self-isolation, which now are frequently in use among the masses, normally carries negative connotations and were assigned to prisoners, making them experience chronophobia (Naguy et al., 2020). Similarly, people locked during the early and peak days of this pandemic, dwelt over thoughts related to the unlocking of the lockdown and the hardships.
2.2.3. Acquiring new practices and avoidance behavior
Acquiring new behavioral change requires considerable thoughts, mindfulness, and change in habits. The recent forced behavioral changes— social distancing, wearing mask, consistent hygiene practices of hand washing, and avoidance behavior including avoiding touching face and large gatherings— will initiate a vicious loop of discomfort, fear, and anxiety. A human normally touches their face on an average 23 times an hour (Kwok et al., 2015). Now that touching face is a risk factor, people have to be mindful of not engaging in a practice which was practiced mindlessly since birth (Markman, 2020). Inculcating a habit of not performing a practice is primarily discomforting, ineffective, and requires a habit reprograming, which further requires 68–254 days to acquire and done involuntarily (Lally et al., 2010). Unable to acquire such changes in a short span will further create fear and anxiety. People then tend to panic more and lose control, making them more susceptible to the coronaphobia. Even our unconscious mind operates to reduce the contagion and produce unconscious psychological responses, termed behavioral immune system (Murray and Schaller, 2016), acting as a first line of defense, warning us from the possible infection. However, being instinctive in nature, the system attacks rationality and leads to alternations and errors in decision-making.
2.2.4. Statements from the international organizations
People deeply rely on international organizations and their predictions for hope and optimism. UN and IMF terming the COVID-19 as the worst global crisis ever since the Great Depression of 1930s respectively (BBC, 2020a; United Nations Conference on Trade and Development, 2020), has further set the tone for a scary future and uncertainty. World Economic Forum (Scott, 2020), has even referred this pandemic as several crises packed in one, namely, healthcare crisis, economic crisis, energy crisis, and humanitarian crisis, worsening the geopolitical risks, globally. WHO and recent studies have further cautioned that COVID-19 hasn’t run its full course with the worst yet to unravel (Tandon, 2020b).
2.2.5. Failure of powerhouses and lack of faith in health care facilities
Countries (mostly developed) on the top of the ladder in providing health securities and capabilities globally such as US, UK, France, Spain, and Italy (Global Health Security Index, 2019) have not been able to address the crisis effectively. During crisis such as this, the faith and trust of people in their national healthcare facilities become paramount. Failure of national healthcare systems could set a ripple effect across the globe. Moreover, one can imagine the plight in middle and lower income countries where people were already suspicious of their country’s healthcare facilities, associated poor hygiene, and lack of infrastructure, furthering anxiety and panic during the pandemic.
2.2.6. Leaders and famous celebrities contracting COVID-19
The powerful leaders and their close ones of developed countries have contracted COVID-19, such as Boris Johnson (Prime Minister, UK), Jair Bolsonaro (President, Brazil), Prince Charles (Prince of Wales), wives of Canadian and Spanish Prime Ministers, and few health ministers. A leader represents the collective bestowed faith of the citizens, a face of valor and spirit, and is viewed as the most powerful person of that country or even globally. Witnessing their leaders contracting the virus, might induce a sense of helplessness and deepens the anxiety of the citizens. Furthermore, the perception that their leaders and governments are not doing enough or are incapable can also lead to despair (Prado, 2020). Also, rich and famous celebrities and sportspersons testing positive might make people feel that even the rich and privileged are not safe, which may further create a sense of helplessness.
2.2.7. The relentless infodemia taking the shape of an infodemic
The pandemic is witnessing global infodemia facilitated by social media and other online resources. WHO had warned of the infodemic accompanying COVID-19, an over-abundance of information – some accurate and some not – that makes it hard for people to find trustworthy sources and reliable guidance (World Health Organization, 2020a, February 2). The COVID-19 infodemic is considered as the first true social media infodemic (Hao and Basu, 2020). It has established how social media can be global public health threat (Larson, 2018) due to conflicting and manipulative misinformation in the form of fake news about possible cures, symptoms, and mortalities. These platforms have become breeding grounds for distorted thinking, leading to panic, confusion, racism, and threat perception of an unrealistic intensity (Kulkarni et al., 2020).
2.3. How coronaphobia builds up?
2.3.1. Interference with routine life
Why do people become fearful or fall into a panic state? Epidemic psychology has seen its roots in the order and routine of human species (Schutz, 1970). The human brain is pre-wired to thrive on certainty and has disdain for uncertainty, which represents danger (Robinson, 2020). For the brain, anticipating a pain is acceptable, but not an uncertainty. Stability is indispensable to humans’ schema and meaning-making. Normally, people have a blueprint of each day, with a taken-for-granted array of solutions for the life tasks which is a part of their personal consciousness (Strong, 1990). A daily life is more assumed rather than planned. We do innumerous tasks daily, pay attention to few, while others are done on ‘auto-pilot’ mode. A crisis like the current pandemic disturbs the set system and questions the certainty with which we were habituated, forcing us to reset. The mystery over the origin of the virus and the associated and prolonged uncertainties give rise to fear of the unknown, considered a fundamental fear of human (Carleton, 2016). Less portion of our life remains steady, demanding us to change our ways and coping mechanisms. Such an attack of uncertainty on our fragile life and temporal stability lead to outburst of irrational and negative emotions, like panic and phobia. Furthermore, humans are cognitive miser (Fiske and Taylor, 1984), making them more vulnerable during crisis to fall for decision-making biases, fueling anxiety and fear.
2.3.2. Cognitive behavioral perspective
Based on the cognitive-behavioral model, it can be said that pandemic reactions such as misinterpretations of health-related stimuli, cognitive distortions, irrational beliefs, maladaptive behaviors, and attention processes have a central role in coronaphobia (Leventhal et al., 2016; Taylor and Asmundson, 2017). For instance, in agoraphobia, the person fears getting a panic attack in a ‘specific’ situation (Mineka and Zinbarg, 2006) or appraises the bodily sensations in catastrophizing manner (Barlow, 2004). Hence, it is the appraisal of the threat in the situation which causes phobia.
Appraisal of bodily sensations, such as fever, cough, tiredness, and breathing difficulty, reported as the most felt symptom of COVID-19 (World Health Organization, 2020b), together with the self-evaluation of inability to cope with such threatening cues can lead to health anxiety. Subsequently, individuals may then seek consultation, not only because of the physical discomfort, but also due to presence of varied anxiety-provoking cognitive events. For instance, the knowledge that COVID-19 spreads through human contact, may get connected to an outside visit the person might have made, say to a nearby grocery shop recently. Later, the appraisal of any physical symptom may be labeled as ‘contraction of infection’. Moreover, many of the COVID-19 cases are asymptomatic (ICMR COVID Study Group and VRDLN Team, 2020) further spiraling a cycle of fear among the people and making them scrutinize even the mildest of bodily signs or any social engagement. In the current pandemic, as in past disease outbreaks (HIV-AIDS, H1N1 Influenza, and Ebola; Taylor, 2019), helplines have been flooded with distress calls from people worried that their benign symptoms are related to COVID-19 (Sinha and Dev, 2020). Such catastrophic interpretations may not be satisfied by the clinical measurements and hence, they are preoccupied with symptoms and seek repeated reassurance, leading us to the behavioral part of coronaphobia.
Reassurance can be sought in a variety of subtle ways, including repeated checking of bodily sensations, measuring fever, self-medicating, reading news, and discussing with family, as in agoraphobia, where patients seek presence of a ‘safe’ reassuring person (Carter et al., 1995) to cope. Long term engagements in such safety seeking behaviors may lead to overdoing of activities which will provide them gratification and sense of protection, or prevent the threat fueling physical changes and elevation of the stress, consequently leading to state of coronaphobia.
2.3.3. Sociocultural amplification of risk
The social and cultural model of pandemic encapsulates fear and phobia as born out of risk perception and response based on psychological, sociological, and cultural factors, commonly referred as ‘social amplification of risk’ (Kasperson, 2017). Factual risk of events combines with sociocultural perspectives and amplifies public responses. This occur through two processes — (a) transfer of information about risk, and (b) mechanism of social response. In the former, individuals learn about risk from various sources, called ‘amplification stations’. Such information colors risk perceptions and levels of concern and act as a key factor in deciding the volume of risk, disputation of information, and its symbolic connotations. This is followed by the interpretation of the risk in the context of social, institutional, and cultural factors, such as social groups, stigma attached, and polarized social views. Hence, an amplified risk perception builds up, leading to heightened behavioral response, like phobia.
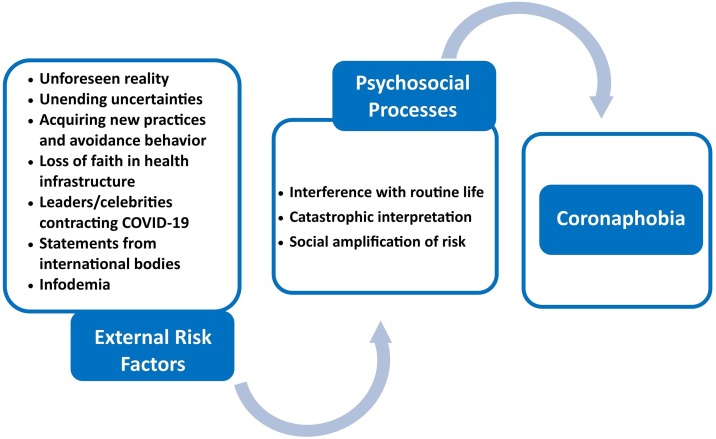
The ‘amplification stations’ enormously influence the social construction of the risk presentation and transmission. These include loved ones, scientists, researchers, risk managing organizations, leaders, and news agencies (Kasperson, 2017) with social media and networking sites being the latest entrants. During the SARS outbreak in 2002−03, news agencies were held responsible for the exaggerated display of news, leading to mass anxiety, and xenophobia (Muzzatti, 2005). Hence, the perception of the health threat comes from the perceptual and symbolic representation, created by the media and digital platforms. At present, two of the widely used social media platforms – Facebook and WhatsApp – are flooded with unverified information related to COVID-19 and contain inaccurate information (Tewari, 2020). The rapid spread of unverified news can create a ripple effect of misinformation. Elevated worries and avoidance behavior has been reported in people with agoraphobia, wherever they were exposed to catastrophic visuals of infections, deaths, and separation from family (Day et al., 2004). Such unreliable information creates panic and phobia for even neutral things, places, and situations (Figure 2 ).
Fig. 2.
Conceptual model of coronaphobia.
Hence, we postulate that coronaphobia develops out of the interaction of external causes which act as risk factors with the psychosocial processes of interference with routine life, catastrophic interpretations, and social amplification of risk, which act as underlying route of development. Managing coronaphobia shall hence require measures specific to these dual mechanisms.
3. Contribution
The paper attempts to extend the existing limited research on fear of COVID-19 through a detailed conceptualization of coronaphobia including definition, risk factors, and underlying psychosocial processes. This conceptualization can aid future research on development of psychometric measures of coronaphobia and help all stakeholders in understanding the cause, framing the diagnosis, and devising policies and interventions for the masses to mitigate coronaphobia.
Author agreement
Alisha Arora and Amrit Kumar Jha conceptualized the idea of coronaphobia and researched relevant literature. Priya Alat and Sitanshu Sekhar Das contributed to the design of the manuscript. All the authors contributed to writing the manuscript.
Declaration of Competing Interest
Authors have no conflict of interest to declare.
Acknowledgement
None.
References
- Ahorsu D.K., Lin C.-Y., Imani V., Saffari M., Griffiths M.D., Pakpour A.H. The fear of COVID-19 scale: development and initial validation. Int. J. Ment. Health Addict. 2020 doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association . American Psychiatric Publishing; 2013. Diagnostic and Statistical Mental Disorders (DSM-5®) [Google Scholar]
- Andersen K.G., Rambaut A., Lipkin W.I., Holmes E.C., Garry R.F. The proximal origin of SARS-CoV-2. Nat. Med. 2020;26:450–452. doi: 10.1038/s41591-020-0820-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asmundson G.J.G., Taylor S. Coronaphobia: Fear and the 2019-nCoV outbreak. J. Anxiety Disord. 2020;70 doi: 10.1016/j.janxdis.2020.102196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow D.H. Guilford press; 2004. Anxiety and Its Disorders: the Nature and Treatment of Anxiety and Panic. [Google Scholar]
- BBC . 2020. Coronavirus: Worst Economic Crisis Since 1930s Depression, IMF Says.https://www.bbc.com/news/business-52236936 URL. [Google Scholar]
- BBC . 2020. Coronavirus May Never Go Away, World Health Organization Warns.https://www.bbc.com/news/world-52643682 URL. [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carleton R.N. Fear of the unknown: One fear to rule them all? J. Anxiety Disord. 2016;41:5–21. doi: 10.1016/j.janxdis.2016.03.011. [DOI] [PubMed] [Google Scholar]
- Carter M.M., Hollon S.D., Carson R., Shelton R.C. Effects of a safe person on induced distress following a biological challenge in panic disorder with agoraphobia. J. Abnorm. Psychol. 1995;104:156–163. doi: 10.1037//0021-843x.104.1.156. [DOI] [PubMed] [Google Scholar]
- Chakraborty K., Chatterjee M. Psychological impact of COVID-19 pandemic on general population in West Bengal: a cross-sectional study. Indian J. Psychiatry. 2020;62:266–272. doi: 10.4103/psychiatry.IndianJPsychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlton E. World Economic Forum; 2020. How COVID-19 Has Changed What We Search for Online.https://www.weforum.org/agenda/2020/05/google-trends-search-online-coronavirus-covid-19/ URL. [Google Scholar]
- Day S.J., Holmes E.A., Hackmann A. Occurrence of imagery and its link with early memories in agoraphobia. Memory. 2004;12:416–427. doi: 10.1080/09658210444000034. [DOI] [PubMed] [Google Scholar]
- Dubey S., Biswas P., Ghosh R., Chatterjee S., Dubey M.J., Chatterjee S., Lahiri D., Lavie C.J. Psychosocial impact of COVID-19. Diabetes Metab. Syndr. Clin. Res. Rev. 2020;14:779–788. doi: 10.1016/j.dsx.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiske S.T., Taylor S.E. Random; New York: 1984. Social Cognition. [Google Scholar]
- Garcia R. Neurobiology of fear and specific phobias. Learn. Mem. 2017;24:462–471. doi: 10.1101/lm.044115.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Global Health Security Index . 2019. 2019 Global Health Security Index. [Google Scholar]
- Goodenough P. CNSNews; 2020. Questions Swirl about Source of China’s Coronavirus Outbreak.https://www.cnsnews.com/article/international/patrick-goodenough/questions-swirl-about-source-chinas-coronavirus-outbreak URL. [Google Scholar]
- Goyal K., Chauhan P., Chhikara K., Gupta P., Singh M.P. Fear of COVID 2019: First suicidal case in India ! Asian J. Psychiatr. 2020;49 doi: 10.1016/j.ajp.2020.101989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haleem A., Javaid M., Vaishya R. Effects of COVID-19 pandemic in daily life. Curr. Med. Res. Pract. 2020;10:78–79. doi: 10.1016/j.cmrp.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao K., Basu T. 2020. The Coronavirus Is the First True Social Media “infodemic”. MIT Technology Review.https://www.technologyreview.com/2020/02/12/844851/the-coronavirus-is-the-first-true-social-media-infodemic/ URL. [Google Scholar]
- Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020 doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ICMR COVID Study Group and VRDLN Team Laboratory surveillance for SARS-CoV-2 in India: performance of testing & descriptive epidemiology of detected COVID-19, January 22-April 30, 2020. Indian J. Med. Res. 2020;151(5):424–437. doi: 10.4103/ijmr.IJMR_1896_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan S., Wan W., Achenbach . Washington Post; 2020. The Coronavirus Isn’t Alive. That’s Why It’s so Hard to Kill.https://www.washingtonpost.com/health/2020/03/23/coronavirus-isnt-alive-thats-why-its-so-hard-kill/ URL. [Google Scholar]
- Kasperson R.E. Social amplification of risk and extreme events. In: Bier V.M., editor. Risk in Extreme Environments: Preparing, Avoiding, Mitigating, and Managing. Routledge; 2017. [Google Scholar]
- Kissler S.M., Tedijanto C., Goldstein E., Grad Y.H., Lipsitch M. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science. 2020;368:860–868. doi: 10.1126/science.abb5793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulkarni P., Prabhu S., Dumar S.D., Ramraj B. COVID -19-Infodemic overtaking Pandemic? Time to disseminate facts over fear. Indian J. Community Heal. 2020;32:264–268. [Google Scholar]
- Kumar C. Times of India; 2020. 50% Virus Strains in India Have ‘Spike Mutation’ That’s Scaring the World.https://timesofindia.indiatimes.com/india/50-virus-strains-in-india-have-spike-mutation-thats-scaring-the-world/articleshow/75607613.cms URL. [Google Scholar]
- Kwok Y.L.A., Gralton J., McLaws M.L. Face touching: a frequent habit that has implications for hand hygiene. Am. J. Infect. Control. 2015;43:112–114. doi: 10.1016/j.ajic.2014.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lally P., Van Jaarsveld C.H., Potts H.W., Wardle J. How are habits formed: Modelling habit formation in the real world. Eur. J. Soc. Psychol. Eur. 2010;40:625–634. doi: 10.1002/ejsp. [DOI] [Google Scholar]
- Larson H.J. The biggest pandemic risk? Viral misinformation. Nature. 2018;562:309–310. doi: 10.1038/d41586-018-07034-4. [DOI] [PubMed] [Google Scholar]
- Lee S.A. Coronavirus Anxiety Scale: a brief mental health screener for COVID-19 related anxiety. Death Stud. 2020;44:393–401. doi: 10.1080/07481187.2020.1748481. [DOI] [PubMed] [Google Scholar]
- Leventhal H., Phillips L.A., Burns E. The Common-Sense Model of Self-Regulation (CSM): a dynamic framework for understanding illness self-management. J. Behav. Med. 2016;39:935–946. doi: 10.1007/s10865-016-9782-2. [DOI] [PubMed] [Google Scholar]
- Li W., Yang Y., Liu Z.-H., Zhao Y.-J., Zhang Q., Zhang L., Cheung T., Xiang Y.-T. Progression of mental health services during the COVID-19 outbreak in China. Int. J. Biol. Sci. 2020;16:1732–1738. doi: 10.7150/ijbs.45120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markman A. Fast company; 2020. Why it’s so hard not to touch your face.https://www.fastcompany.com/90476831/why-its-so-hard-not-to-touch-your-face URL. [Google Scholar]
- Mertens G., Gerritsen L., Duijndam S., Salemink E., Engelhard I.M. Fear of the coronavirus (COVID-19): predictors in an online study conducted in March 2020. J. Anxiety Disord. 2020;74 doi: 10.1016/j.janxdis.2020.102258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mineka S., Zinbarg R. A contemporary learning theory perspective on the etiology of anxiety disorders: it’s not what you thought it was. Am. Psychol. 2006;61:10–26. doi: 10.1037/0003-066X.61.1.10. [DOI] [PubMed] [Google Scholar]
- Murray D.R., Schaller M. Advances in Experimental Social Psychology. 1st ed. Elsevier Inc.; 2016. The behavioral immune system: implications for social cognition, social interaction, and social influence. [DOI] [Google Scholar]
- Muzzatti S.L. Bits of falling sky and global pandemics: moral panic and Severe Acute Respiratory Syndrome (SARS) Illn. Cris. Loss. 2005;13:117–128. doi: 10.1177/105413730501300203. [DOI] [Google Scholar]
- Naguy A., Moodliar-Rensburg S., Alamiri B. Coronaphobia and chronophobia – A psychiatric perspective. Asian J. Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prado B. COVID-19 in Brazil: “So what?”. Lancet. 2020;395:1461. doi: 10.1016/S0140-6736(20)31095-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson B. Forbes; 2020. The Psychology of Uncertainty: How to Cope With COVID-19 Anxiety.https://www.forbes.com/sites/bryanrobinson/2020/03/12/the-psychology-of-uncertainty-how-to-cope-with-covid-19-anxiety/#61199014394a URL. [Google Scholar]
- Roy D., Tripathy S., Kar S.K., Sharma N., Verma S.K., Kaushal V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J. Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schutz A. University of Chicago Press; 1970. Alfred Schutz on Phenomenology and Social Relations. [Google Scholar]
- Scott J. World Economic Forum; 2020. Several Crises in One: What Effects Will COVID-19 Have on the Global Risk Landscape?https://www.weforum.org/agenda/2020/05/covid-19-global-risk-landscape/ URL. [Google Scholar]
- Sinha M., Dev A. The Times of India; 2020. Doctors Flooded With Calls on Covid-19 Symptoms.https://timesofindia.indiatimes.com/city/noida/noida-doctors-flooded-with-calls-on-covid-19-symptoms/articleshow/74783678.cms URL. [Google Scholar]
- Strong P. Philip Strong Epidemic psychology : a model. Soc. Heal. Illn. 1990;12:249–259. [Google Scholar]
- Sullivan M. Fast Company; 2020. Coronavirus Might Be the Biggest Trend in Google Search History.https://www.fastcompany.com/90477301/what-are-americans-googling-during-the-coronavirus-outbreak-celebrities-and-disney-world URL. [Google Scholar]
- Tandon R. COVID-19 and mental health: preserving humanity, maintaining sanity, and promoting health. Asian J. Psychiatr. 2020 doi: 10.1016/j.ajp.2020.102256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tandon R. The COVID-19 pandemic, personal reflections on editorial responsibility. Asian J. Psychiatr. 2020 doi: 10.1016/j.ajp.2020.102100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner C. When coronaphobia turns into agoraphobia: ‘I struggle to even go out for a walk’. inews. 2020 Retrieved fromhttps://inews.co.uk/news/coronavirus-uk-latest-lockdown-restrictions-coronaphobia-agoraphobia-mental-health-434506, June 6, 2020. [Google Scholar]
- Taylor S. Cambridge Scholars Publishing; 2019. The Psychology of Pandemics: Preparing for the Next Global Outbreak of Infectious Disease. [Google Scholar]
- Taylor S., Asmundson G.J.G. Treatment of health anxiety. In: Abramowitz J.S., McKay D., Storch E.A., editors. Handbook of Obsessive-Compulsive Disorders: Obsessive-Compulsive Related Disorders. Wiley; Chichester: 2017. pp. 977–989. [Google Scholar]
- Tewari S. The Livemint; 2020. Covid-19: Social Media Platforms Fight Fake News Under Pressure From Government.https://www.livemint.com/industry/media/covid-19-social-media-platforms-fight-fake-news-under-pressure-from-government-11586843895979.html URL. [Google Scholar]
- United Nations Conference on Trade and Development Impact of the Covid 19 pandemic on global FDI and GVCs. Investment Trends Monitor. 2020 https://unctad.org/en/PublicationsLibrary/diaeiainf2020d3_en.pdf [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . 2020. Coronavirus Disease (COVID-19) Situation Report – 13.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200202-sitrep-13-ncov-v3.pdf?sfvrsn=195f4010_6 URL. [Google Scholar]
- World Health Organization . 2020. Coronavirus.https://www.who.int/health-topics/coronavirus#tab=tab_3 URL. [Google Scholar]
- Worldometer . 2020. COVID-19 Coronavirus Pandemic.https://www.worldometers.info/coronavirus/ URL. [Google Scholar]
- Worldometer . 2020. Coronavirus Incubation Period.https://www.worldometers.info/coronavirus/coronavirus-incubation-period/ URL. [Google Scholar]
- Xiang Y.T., Yang Y., Li W., Zhang L., Zhang Q., Cheung T., Ng C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon E. Harvard Business Review; 2020. Behavioral Trends That Will Reshape Our Post-covid World.https://hbr.org/2020/05/3-behavioral-trends-that-will-reshape-our-post-covid-world URL. [Google Scholar]