To the Editor,
We read with interest the article by Zhao et al. describing personal protective-equipment (PPE) usage among different groups of health-care workers (HCWs) during the coronavirus disease 2019 (COVID-19) epidemic in Wuhan [1]. However, ancillary HCWs (excluding doctors and nurses) formed a minority (5.7%, 55/960) of the HCWs surveyed [1]. Emphasis has been placed on clinical staff as being at-risk HCWs. However, ancillary HCWs, such as cleaning staff and security officers, also have substantial risk for work-related transmission of COVID-19 [2]. Furthermore, compliance with infection prevention and control measures may not be uniform; lower rates of hand hygiene have been reported among cleaners [3]. Monitoring PPE compliance among ancillary HCWs is essential during the pandemic.
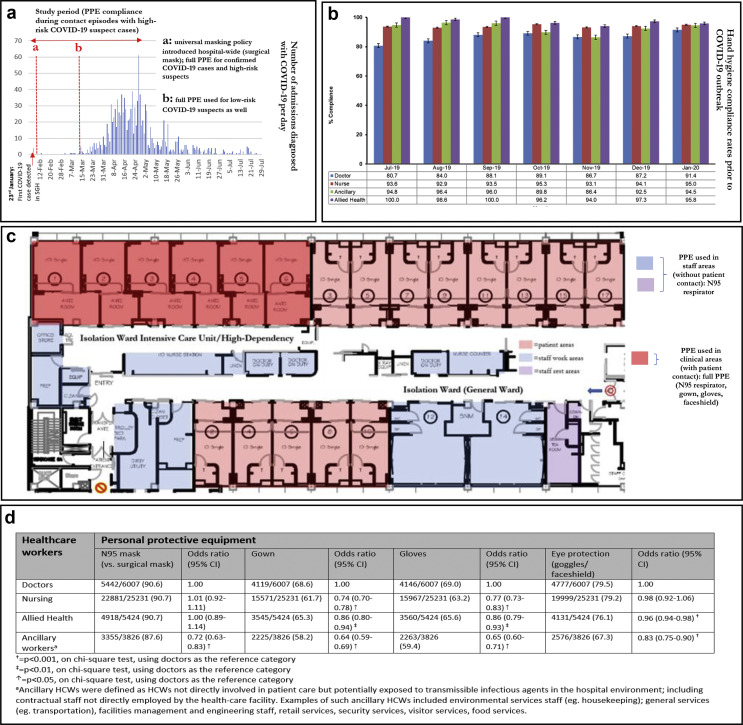
In Singapore, the COVID-19 outbreak has been ongoing since the end of January 2020. Access to adequate PPE was a key strategy at our institution, the largest tertiary hospital in Singapore, with almost 10 000 HCWs, 1780 of which were ancillary HCWs [4]. A universal masking policy was adopted in early February 2020 (Fig. 1 a). Rates of hand hygiene compliance were generally high among all HCWs before the COVID-19 outbreak (Fig. 1b); during the COVID-19 outbreak, hand hygiene compliance rose to 100% across all HCWs. All HCWs were required to use full PPE (consisting of N95 respirator, disposable gown and gloves, and eye protection) during contact with high-risk suspected COVID-19 cases/confirmed COVID-19 cases (Fig. 1c). Ancillary HCWs (e.g. porters accompanying suspected cases to isolation ward, security staff controlling lifts used by suspected cases, and cleaning staff in areas used by confirmed/suspected cases) were mandated to use full PPE, provided by our institution. We monitored PPE compliance among all HCWs working in high-risk areas. Waiver of informed consent was approved (CIRB Ref 2020/2436).
Fig. 1.
Prevailing personal protective-equipment (PPE) guidelines, hand hygiene compliance, layout of isolation ward and PPE usage by area and compliance with PPE during contact episodes with suspected COVID-19 cases (n = 40 488) at a Singaporean tertiary hospital during a COVID-19 outbreak.
Over a 3-month study period (1 February 2020 to 30 April 2020), contact logs (describing contact time, contact distance and PPE used) were maintained in hospital areas where suspected COVID-19 cases were managed (isolation wards and ‘fever areas’ in the emergency room). This log was maintained daily; HCWs were mandated to fill this log prospectively during patient contact. A contact episode was defined as being in the same room, or sharing an enclosed space, with a suspected COVID-19 case. For each contact episode, HCWs indicated the contact nature (ranging from touching the patient to being in the same room) and the contact duration (ranging from <5 minutes to ≥30 minutes), and PPE used. During the study period, 1850 suspected cases were managed in our institution, of which 386 subsequently tested positive for COVID-19 by PCR. Only contact episodes before the confirmation of COVID-19 results were analysed, given that compliance with PPE was universal once a patient was confirmed to have COVID-19. Compliance with the contact log was monitored by ward-based nursing staff and audited by hospital infection control. All suspected COVID-19 cases were managed in access-controlled areas with a unidirectional traffic flow and single entry/exit points; this facilitated monitoring of individuals' entry/exit from the isolation wards. Contact log records were also cross-checked against individuals' entries in the electronic medical record. From March 2020 onwards, the contact log was switched from manual entry to digital logging via an app; the error rate decreased from 1.08 errors per 100 contact-episodes to 0.88 errors per 100 contact-episodes post-digitization (incidence-rate-ratio 0.81, 95% CI 0.68–0.97, p 0.02).
A total of 40 488 contact episodes were recorded; close to 90% of episodes were significant based on time or distance criteria (see Supplementary material, Table S1). Although PPE usage was high among all HCWs, ancillary workers had lower odds of PPE adherence during contact episodes with suspected COVID-19 cases, compared with other HCWs (Fig. 1d). Ancillary workers had lower odds of using N95 respirators (versus surgical masks), disposable gowns, gloves and eye protection during contact episodes. In total, 16 cases of COVID-19 were detected among all HCWs (0.17%, 16/9322); all cases were linked to known community cases or clusters of COVID-19, and there was no evidence of transmission in clinical areas [4,5]. Free COVID-19 testing via PCR was offered to all symptomatic HCWs [4], to date close to two-thirds of HCWs (5845/9322) have been tested at least once. Although overall rates of infection among HCWs were low, rates of infection were higher in ancillary HCWs compared with medical and nursing staff (0.32%, 5/1548, versus 0.10%, 5/5101; incidence-rate ratio 3.29, p 0.04). A number of our ancillary HCWs were migrant workers; in April 2020, significant outbreaks of COVID-19 were recorded in migrant worker dormitories in Singapore [5]. Beyond occupational risk and lower PPE adherence, other factors unique to ancillary HCWs, such as socio-economic status and accommodation type, could also increase the risk profile of this group. A solitary undetected case of COVID-19 in a minimally symptomatic ancillary worker resulted in the exposure of 68 other HCWs; however, onward transmission was mitigated because of PPE usage and social distancing [5]. Inclusion of not just clinical staff but also ancillary HCWs is crucial to maintain a goal of zero health-care-associated transmission of COVID-19.
Transparency declaration
The authors report no conflicts of interest. This work was not grant-funded.
Author contributions
Concept and design was by LEW, JXYS and MLL; analysis of data was by LEW, EPC, IMN and MKAung. The manuscript was drafted by LEW, EPC, JXYS and MLL and the study was supervised by MLL.
Editor: J. Rodriguez-Baño
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.cmi.2020.08.040.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Zhao Y., Liang W., Luo Y., Chen Y., Liang P., Zhong R. Personal protective equipment protecting healthcare workers in the Chinese epicentre of COVID-19. Clin Microbiol Infect. 2020:S1198–S1743. doi: 10.1016/j.cmi.2020.07.029. X(20)30437-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lan F.Y., Wei C.F., Hsu Y.T., Christiani D.C., Kales S.N. Work-related COVID-19 transmission in six Asian countries/areas: a follow-up study. PLoS One. 2020:15. doi: 10.1371/journal.pone.0233588. e0233588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sendall M.C., McCosker L.K., Halton K. Cleaning staff's attitudes about hand hygiene in a metropolitan hospital in Australia: a qualitative study. Int J Environ Res Public Health. 2019;16:1067. doi: 10.3390/ijerph16061067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wee L.E., Sim J.X.Y., Conceicao E.P., Aung M.K., Goh J.Q., Yeo D.W.T. Containment of COVID-19 cases amongst healthcare workers: the role of surveillance, early detection and outbreak management. Infect Control Hosp Epidemiol. 2020 doi: 10.1017/ice.2020.219. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wee L.E., Sim J.X.Y., Conceicao E.P., Aung M.K., Tan J.Y., Venkatachalam I. Containment of COVID-19 amongst ancillary healthcare workers: an integral component of infection control strategies. J Hosp Infect. 2020 doi: 10.1016/j.jhin.2020.08.002. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.