Abstract
Background
Coronavirus Disease is one of the most highly infectious diseases was reported worldwide as pandemic. This infectious virus transmits through several methods among individuals, for controlling this transmission most effective nonpharmacological strategy to controlling the infections is Quarantine the affected or suspected asymptomatic individuals.
Aim
To assess the psychological impact of quarantine period on asymptomatic individuals with COVID-19.
Methodology
Descriptive research design was used in the study. A total of 380 individuals approached for the study, participants on a structured research proforma and Depression Anxiety and stress scale.
Result
The average age of the quarantine people was 33.5 years and 72% of them are males, all are educated and 66% of them are well qualified. Stress was severe or extremely severe among 46% of participants followed by anxiety and depression is 14 and 8 respectively.
Conclusion
Control freedom of quarantine period and limited almost nil interaction with others worsens their psychological health and daily functioning. Psychological distress was multifolded due to lack of proper mental health facilities and the availability of factual information about the virus.
Keywords: COVID-19, Depression, Anxiety, Stress, Quarantine
1. Introduction
Coronavirus Disease (COVID-19) is a highly infectious disease ever known across the globe. Covid-19 first case was diagnosed from Wuhan (Hubei Peovince, China) on December 31st, 2019 (Holshure et al., 2020. On January 30th, 2020 the World Health Organization (WHO) declared a global health outbreak emergency, on March 11th, 2020, a pandemic (WHO, 2020a). Many individuals all across the world are affected by the COVID-19 pandemic. Direct contact with COVID-19 or fear of infection increased psychological stress and worry among all who have contact with positive cases including asymptomatic individuals. People who are affected by COVID-19 have all the rights of their life; they deserve proper treatment, support and equal respect of other community people (WHO, 2020b).
The world is working together to produce proper treatment for COVID-19. But due to unavailability of proper pharmacological intervention or curable vaccines to treat or prevent COVID-19 is the biggest task across the globe. Currently, non-pharmacological measures of public health uses such as social distancing, isolation, and quarantine to prevent community outbreak are the best techniques. In the current time WHO and the Center for Disease and Prevention (CDG) recommended 14 days quarantine for individuals who were in direct contact with a confirmed case, which duration based on the estimated incubation period of SARS-CoV-2 (WHO, 2020c).
Stress, anxiety, depression, somatization and adverse behaviour are very common in general public. In the current unpredicted situation specify that fear of the unknown and uncertainty can lead the psychological and emotional consequences of COVID-19 (Shigemura et al., 2020). Wang et al. (2020) reported 16.5% depressive symptoms, 28.8% symptoms of anxiety and 8.1% stress among the residents of 194 different cities of China.
Controlling disease transmission to other community members from individuals who have travel history or history of direct connection with diagnosed people were quarantined under state-run facilities. This method is very effective for other’s safety, but the individual who admitted to quarantine canters they face various psychological issues during the 14 days. Disrupted daily living and worry for their family and future were reported frequently among the quarantine individuals. For reducing the risk of infection to others, the facility of separation, and living in a restricted area is the best option for individuals exposed to a contagious disease. Individuals stay at home due to COVID-19, had higher level of Stress, Anxiety and Depression (Brooks et al., 2020). Mental health of quarantine people is affected in all the age groups (Brooks et al., 2020; Ozamiz-Etxebarria et al., 2020). High level of depression, stress and anxiety and worse psychological impact on young student was stressed (Antunez et al., 2012; Martín, 2007; Velez et al., 2010). Suspected people carrying various substantial mental health problems, this type of situation is known to be linked to depression, post-traumatic stress disorder, acute stress, insomnia, irritability, and anger faced by individual quarantine and isolated (Brooks et al., 2020). Its new illness and very new management strategy for individuals with exposure to COVID-19 dearth of literature from India in this perspective emphasises the need of current research.
2. Material and methods
Study aim to assess psychological impact of quarantine period on asymptomatic individuals with COVID-19. Ethical permission was granted by district officials of North India.
Study was a cross sectional onetime assessment in three centers created for quarantine facility in the selected district for suspected case of COVID-19. Total 380 individuals were included for the study from quarantined centers of Kaimur, Bihar, from 14th-30th April 2020. Written consent was sought from the individuals before initiating the assessment. All the individuals who were placed in quarantine center after a contact or travel history were approached for the participation on the 7th day of their stay. Confirm positive cases, miners and having co morbidity of physical illness were excluded from the study. Descriptive research design was used for the study 310 individual (Fig. 1 ) matched the study criteria were approached. Semi structured socio-demographic data sheet for assessing age, gender, occupation, education, domicile, education and marital status was used.
Fig. 1.
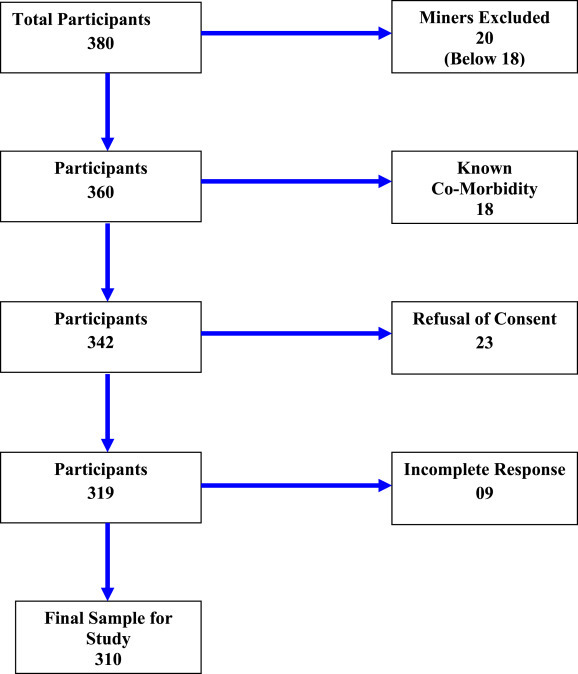
Final sampling process.
Self administered Depression Anxiety Stress Scale (DASS, 2006) Hindi adaptation (Singh et al., 2013) was used for assessing psychological distress of COVID-19 in the form of depression, anxiety and stress of participants in quarantine period. This scale has 21 questions divided in three parts and 7 questions for each depression, anxiety and stress sub domains. Scale provides range from extremely severe to normal for depression anxiety and stress.
Data was collected from all the individuals on the starting of 2nd week of their quarantine period. All the data was prepared for SPSS 16 and descriptive and inferential statistics was used for analysis.
3. Result
In the study total 310 asymptomatic individual participated. Table 1 shows Mean age of the participants 33.54 ± 12.49 years. Most of the participants were male 72.9%, 33.9% participants were educated up to higher secondary, and 25.8%, were graduates. Majority of the participants 37.1% were professional following by student, former (they engaged agriculture work only), homemakers 17.1, 18.7, 14.8% respectively. Daily labour and business man found in the study were 8.4 & 3.9%. Total 64.5% participants were married comparison to 27.4 & 8.1% unmarried and separated. Half of participants belong to rural area, 33.6% belong to urban and 15.8% were belonging to semi-urban area respectively.
Table 1.
Demographic characteristics.
| Variables | Participants % (N = 120) |
|---|---|
| Age | |
| Mean ± SD | 33.54 ± 12.49 |
| Gender | |
| Male | 72.9 |
| Female | 27.1 |
| Education | |
| Primary | 11.6 |
| Secondary | 22.6 |
| Higher Secondary | 33.9 |
| Graduate | 25.8 |
| PG & Above | 06.1 |
| Occupation | |
| Daily Labour | 08.4 |
| Former | 17.1 |
| Homemaker | 14.8 |
| Students | 18.7 |
| Professional | 37.1 |
| Business | 3.9 |
| Marital status | |
| Married | 64.5 |
| Unmarried | 27.4 |
| Separated | 08.1 |
| Domicile | |
| Rural | 50.6 |
| Semi-urban | 15.8 |
| Urban | 33.6 |
Table 2, shows that the 23.2% individual were faced mild level depression followed by 18.2% moderate, 6.1% reported that severe and 1.9% extremely severe level of depression respectively. Anxiety level was reported more than half 59.1% normal compression to 14.8% moderate level followed by 11.9% mild level, 10.0% severe and 4.2% extremely severe level respectively. Stress domain reported that total 30.3% of participants face externally severe stress comparison to 21.9% moderate, 16.5% severe level and 7.1% mild stress respectively.
Table 2.
Frequency of Depression, Anxiety and stress among the participants (N = 310).
| Variable | Depression | Anxiety | Stress |
|---|---|---|---|
| Normal | 50.6 | 59.1 | 24.2 |
| Mild | 23.2 | 11.9 | 07.1 |
| Moderate | 18.2 | 14.8 | 21.9 |
| Severe | 06.1 | 10.0 | 16.5 |
| Extremely Severe | 01.9 | 04.2 | 30.3 |
Table no 3 explain depression, anxiety and stress were 5.03 ± 3.30, 4.47 ± 2.87 and 7.38 ± 4.42 respectively and significantly high among all the participants at quarantine center. It also explainsthe relationship between three dependent variables that shows high significant positive relationship between depression anxiety and stress.
Table 3.
Correlation between depression anxiety and stress among quarantine individuals.
| Variables | Depression | Anxiety | Stress |
|---|---|---|---|
| Mean (sd) | 5.03 (3.30) | 4.47(2.87) | 7.38 (4.42) |
| Depression | 1 | .732a | .472a |
| Anxiety | 1 | .545a | |
| Stress | 1 |
= Significant at 0.001.
4. Discussion
Separation with family and loved ones often an unpleasant experience the condition of quarantine with limited freedom, uncertainty over disease status, dullness event can create several psychological problems (Barbish et al., 2015; Shigemura et al., 2020, wang et al., 2020). People are facing several problems during lockdown that include basic survival to fake and endless information on COVID-19 pandemic period. Lack of proper information and awareness in community and low adherence attitude people did not follow proper instructions and met to infection spreading conditions. Symptomatic individual were send to isolation wards and asymptomatic individual quarantined at quarantine centers this identification of the contact with COVID-19 patient, directly impact on psychological health of asymptomatic individual. Individuals facing fear and anxiety (Shigemura et al., 2020 wang et al., 2020) putting them in quarantine center increases the vulnerability of being traumatized of asymptomatic individual.
In the present study reported that psychological impact of asymptomatic individual at quarantine center was quite high than the normal conditions. The mean age of the participants was 33.54 years, majority of the individual were young, and very few of them were miner those are excluded due the ethical guidelines. Maximum participants were male covered 73% of total sample size that reflected Indian gender biasness in the work and social interaction where male are suppose to move out for earning and female kept inside the home for household chores also the restriction of dressing with face covering reduces the chances of infection for the females. 34% individuals completed their education up to higher secondary and 26% were Graduate. Study found that approx 37% of the participants were engaged in government and private sector.
Quarantine is public health measure which helps to prevent spread of infectious disease but along with that worse effect on psychological health of quarantined individuals was reported. Isolation is known for increasing the anxious and depressive disorder (Ieraci et al., 2016) and it has been reported in the current pandemic (Shigemura et al., 2020 wang et al., 2020, Brooks et al., 2020; Ozamiz-Etxebarria et al., 2020) also. Disturbed daily life and lack of proper work schedule furnish the chances for access use of media that increases the stress and anxiety among the quarantine period (Help guide). Present study found that approx 50% individuals reported with depressive symptoms whereas 8% of them are in severe or extremely severe category. Similar findings were reported by Lee et al. (2005) during Severe Acute respiratory Syndrome (SARS) that 73% people experienced low mood and other research in COVID-19 period also reported high level of depression anxiety and stress (Shigemura et al., 2020, Wang et al., 2020, Brooks et al., 2020; Ozamiz-Etxebarria et al., 2020).
Previous study (Liu et al., 2012) also reported that 9% (48 of 549) of participants found highly depressive and the same group reported 15% low depressive symptoms after completing quarantined period similarly in present study 18% participants reported moderate depression. In the present study 40% participants reported anxiety symptoms, 10% of them have severe level and 4% participants experienced extremely severe anxiety level during the quarantine period. Presence of significant anxiety, insomnia, irritability, reduce work performance and poor concentration are common difficulties in quarantined individuals (Bai et al., 2004). Similarly online survey conducted at King George Medical Univeristy during the COVID-19 pandemic in India shows, panic and anxiety symptoms that duration this affected individual mental health of larger population (Roy et al., 2020). Questions without answer health condition without clear prognosis and lack of clear information increases the stress condition among individuals. Present study reports 30% participants felt extremely severe stress which can be explained due to uncertainty of health condition and nonexistence of treatment or vaccine for coronavirus. Previous research on SARS quarantined, shows that the individual face acute stress disorder during quarantine period (Bai et al., 2004). Being quarantine in hospital individuals reported highly stressed even three years later of quarantine period we also found 22% participants experienced moderate, 17% severe level of stress during quarantined period.14 Previous findings also reported present of 23% depressive and 19% anxiety symptoms among the students during the quarantine period (Xie et al., 2020).
Expected fear of losing job/earning resources, infection of himself/herself or beloved one are the causes of high stress and anxiety which leaded the high level of depression. We found high level of positive correlation between depression anxiety and stress that is showed high level of any one can influence the remaining two variables. Stress can cause the depression in and anxiety and they all can elevate each other (Priya et al., 2020).
5. Conclusion
The COVID-19 Pandemic condition makes many individuals to staying at home sitting down and many of them were found positive and hospitalised with major to miner health issues. Quarantine center is another option for reducing the virus transmission. Although it’s one of the most effective public health measures to prevent the spread of an infectious disease. Social contacts are the part of general social life. Quarantine reduces the social connection that created worries about self and family members which further developed depression, anxiety and stress among the individuals. Isolation in quarantine centers affected adversely on mental health and psycho social health of individuals.
Authors’ contributions
RU took permission to ethics committee for conducting research and completed data collection.
S designed the review, developed the inclusion criteria and abstracts appraised the quality of included papers.
BS worked in analysis and writing of paper include review of the study, screened titles and drafted the manuscript.
US reviewed the study protocol, read and screened articles for inclusion. All authors critically reviewed drafts and approved the final manuscript.
Financial support
None.
Declaration of competing interest
The authors declare that they have no competing interests.
Acknowledgment
None.
References
- Antúnez Z., Vinet E.V. Depression anxiety stress scales (DASS-21): Validation of the abbreviated version in Chilean university students. Terapia Psicologica. 2012;30(3):49–55. [Google Scholar]
- Bai Y., Lin C.C., Lin C.Y., Chen J.Y., Chue C.M., Chou P. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatric Services. 2004;55(9):1055–1057. doi: 10.1176/appi.ps.55.9.1055. [DOI] [PubMed] [Google Scholar]
- Barbisch D., Koenig K.L., Shih F.Y. Is there a case for quarantine? Perspectives from SARS to ebola. Disaster Medicine and Public Health Preparedness. 2015;9(5):547–553. doi: 10.1017/dmp.2015.38. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DASS . 2006. Depression anxiety stress scales (DASS) psychology foundation of Australia.http://www.psy.unsw.edu.au/Groups/Dass [Google Scholar]
- Holshue M.L., DeBolt C., Lindquist S., Lofy K.H., Wiesman J., Bruce H.…Diaz G. First case of 2019 novel coronavirus in the United States. New England Journal of Medicine. 2020 doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Help guide: Mental health. https://www.helpguide.org/articles/mental-health/social-media-and-mental-health.htm
- Ieraci A., Mallei A., Popoli M. Neural plasticity; 2016. Social isolation stress induces anxious-depressive-like behavior and alterations of neuroplasticity-related genes in adult male mice. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S., Chan L.Y., Chau A.M., Kwok K.P., Kleinman A. The experience of SARS-related stigma at Amoy Gardens. Social Science & Medicine. 2005;61(9):2038–2046. doi: 10.1016/j.socscimed.2005.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., Kakade M., Fuller C.J., Fan B., Fang Y., Kong J., Wu P. Depression after exposure to stressful events: Lessons learned from the severe acute respiratory syndrome epidemic. Comprehensive Psychiatry. 2012;53(1):15–23. doi: 10.1016/j.comppsych.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martín I. Estrésacadémico en estudiantesuniversitarios. Apuntes de Psicología. 2007;25:87–99. [Google Scholar]
- Ozamiz-Etxebarria N., Dosil-Santamaria M., Picaza-Gorrochategui M., Idoiaga-Mondragon N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cadernos de Saúde Pública. 2020;36 doi: 10.1590/0102-311X00054020. [DOI] [PubMed] [Google Scholar]
- Priya A., Garg S., Tigga N.P. Predicting anxiety, depression and stress in modern life using machine learning algorithms. Procedia Computer Science. 2020;167:1258–1267. [Google Scholar]
- Roy D., Tripathy S., Kar S.K., Sharma N., Verma S.K., Kaushal V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian Journal of Psychiatry. 2020 doi: 10.1016/j.ajp.2020.102083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shigemura J., Ursano R.J., Morganstein J.C., Kurosawa M., Benedek D.M. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: Mental health consequences and target populations. Psychiatry and Clinical Neurosciences. 2020;74(4):281. doi: 10.1111/pcn.12988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh B., Prabhuappa K.P., Eqbal S., Singh A.R. Depression, anxiety and stress scale: Reliability and validity of Hindi adaptation. Int J Educ Manage Stud. 2013;3:446–449. [Google Scholar]
- Vélez L.P.M., Gutiérrez J.A., Isaza B.E.T. Depresión en estudiantesuniversitarios y suasociación con el estrésacadémico. CesMedicina. 2010;24(1) [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . 2020. Mental health and psychosocial considerations during the COVID-19 outbreak. [Google Scholar]
- World Health Organization . World Health Organization; 2020. Considerations for quarantine of individuals in the context of containment for coronavirus disease (COVID-19): Interim guidance. [Google Scholar]
- World Health Organization (WHO) Rolling updates on coronavirus diseases (COVID-19) 2020. www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-theyhappen Available from:
- Xie X., Xue Q., Zhou Y., Zhu K., Liu Q., Zhang J., Song R. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA pediatrics. 2020 doi: 10.1001/jamapediatrics.2020.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]


