Abstract
The coronavirus disease 2019 (COVID-19) has amazed by its distinct forms of presentation and severity.
COVID-19 patients can develop large-scale ischemic strokes in previously healthy patients without risk factors, especially in patients who develop an acute respiratory distress syndrome (SARS-CoV-2).
We hypothesize that ischemic events are usually the result of the combined process of a pro-inflammatory and pro-coagulant state plus vascular endothelial dysfunction probably potentiated by hypoxia, hemodynamic instability, and immobilization, as reported in other cases.
To the best of our knowledge, we report the first case of partial obstruction of a vertebral artery in a patient with COVID-19.
Decompressive surgery remains a life-saving maneuver in these patients (as in other non-COVID-19 strokes) and requires further investigation.
Keywords: Cerebrovascular disease, COVID-19, Coronavirus, Stroke, Decompressive craniectomy, Cerebellar, SARS-CoV-2
Abstract
La enfermedad por coronavirus 2019 (COVID-19) ha sorprendido por sus distintas formas de presentación y gravedad.
Los pacientes con COVID-19 pueden desarrollar accidentes cerebrovasculares isquémicos a gran escala, incluso aquellos previamente sanos, sin factores de riesgo, y especialmente los que desarrollan un síndrome de dificultad respiratoria aguda (SARS-CoV-2).
Presumimos que los eventos isquémicos son generalmente el resultado del proceso combinado de un estado proinflamatorio y procoagulante, más una posible disfunción endotelial vascular, probablemente potenciada por hipoxia, inestabilidad hemodinámica e inmovilización, como se ha reportado en otros casos.
Hasta nuestro conocimiento reportamos el primer caso de una obstrucción parcial de una arteria vertebral en un paciente con COVID-19.
La cirugía descompresiva sigue siendo una maniobra que salva vidas (como en otros accidentes cerebrovasculares que no están relacionados con la COVID-19) y requiere más investigación.
Palabras clave: Enfermedad cerebrovascular, COVID-19, Coronavirus, Ictus, Cirugía descompresiva, Cerebelo, SARS-CoV-2
Introduction
The coronavirus disease 2019 (COVID-19) that affects worldwide since December 2019 has amazed by its distinct forms of presentation and severity.1 The reported incidence of strokes in COVID-19 patients lies between 2.8 and 5%.2, 3
The presence of a stroke increases the severity and mortality of patients with COVID-19.3, 4
We present two massive supra and infratentorial strokes in people of young age with no known risk factors and with the severe acute respiratory syndrome (SARS-CoV-2), requiring Endotracheal Intubation (ETI). One of them is a case of partial obstruction of the right vertebral artery. As far as we know, this could be the first reported case of this type.
Case 1
Cough, fever, nausea, and dyspnea that lasted for a week developed in a previously healthy 35-year-old man. He had bilateral interstitial pneumonia with COVID-19 positive, being diagnosed with SARS-CoV-2 and admitted to the intensive care unit (ICU).
Blood analysis showed a pattern of a high systemic inflammatory response (Table 1 ).
Table 1.
Summary of relevant variables of young patients with stroke-COVID-19.
| Variable | Case 1 | Case 2 | Reference normal values |
|---|---|---|---|
| Age (years) | 35 | 51 | |
| Day stroke (from admission) | 9 | 8 | |
| Leukocytes (10^6 μL) | 12.8 | 14.6 | 4.0–10.5 |
| Lymphocytes (10^3 μL) | 8 | 9 | 1.5–3.5 |
| Platelets (10^3 μL) | 278 | 288 | 150–45 |
| Fibrinogen (mg/dL) | 820 | 502 | 150–450 |
| C-reactive protein CRP (mg/dL) | 39 | 14.42 | <0.1 |
| Ferritin (ng/mL) | 1947 | 1716 | 10–150 |
| D-Dimer (ng/mL) | 1385 | 1495 | 0.1–500 |
| Interleukin 6 IL6 (pg/mL) | 282 | 72.8 | 1–5 |
| Treatment SARS-CoV-2 | Hydroxychloroquine, tocilizumab, methylprednisolone and enoxaparin (40 mg daily). | Hydroxychloroquine, methylprednisolone and enoxaparin (40 mg daily). | |
| Stroke | Massive infratentorial stroke | Malignant supratentorial stroke | |
| Artery | Vertebral artery | Middle cerebral artery | |
| Stroke treatment | Thrombectomy and suboccipital craniectomy | Thrombectomy and right decompressive hemicraniectomy |
The patient began treatment with hydroxychloroquine, Tocilizumab, Methylprednisolone, and Enoxaparin 40 mg daily (Table 1).
On day 5, nausea, vomiting, central nystagmus, dysmetria of the four extremities, and dysarthria suddenly appeared. Computed tomography (CT) showed subtle hypodensity in the upper margin of the left cerebellar hemisphere. Hypoplasia of the right vertebral artery (Fig. 1 B) and thrombus with partial obstruction at the level of the left vertebral artery – segment V2 (Fig. 1C, D). We also observed the anatomical absence of both posterior communicating cerebral arteries. We performed a successful mechanical thrombectomy using a direct aspiration first-pass technique.
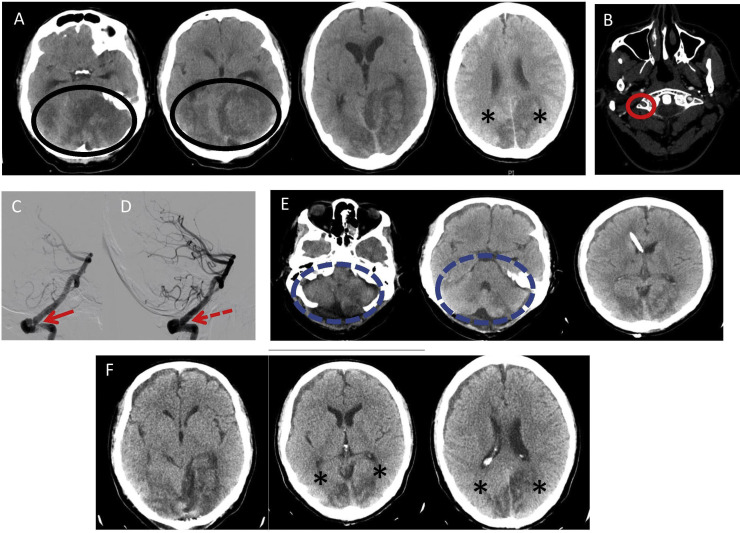
Fig. 1.
Infratentorial massive stroke. Left VA partial obstruction. (A) CT: Massive ischemic stroke in left cerebellar hemisphere and edema (Black Circle). (B) CTA: Hypoplasia of the right VA (red circle). (C) Angiography: thrombus at the level of left VA-V2 segment (Red Arrow) evidencing low flow in posterior circulation). (D) Flow restored after thrombectomy (Red Dotted Arrow). (E) CT: Suboccipital craniectomy and ventricular drain. A notably radiological improvement of the posterior fossa stroke (Blue Dotted Circle). (F) CT: The resolution of hydrocephalus and improvement of the bilateral occipital strokes. * Bilateral stroke in occipital lobes, CTA: CT-Angio, CT: computerized tomography, VA: vertebral artery.
On day 9, he developed a suddenly reduced level of consciousness with bilateral mydriasis. CT shows a massive posterior fossa (PF) stroke with bilateral occipital involvement (Fig. 1A).
We perform an extensive suboccipital craniectomy and place external ventricular drainage (EVD). CT showed improvement in hydrocephalus and adequate decompression of the PF (Fig. 1E).
On day 16, we removed ETI and EVD (Fig. 1F). On day 21, the patient's level of consciousness is alert; he answers simple questions and obeys simple orders, with no apparent motor deficit. He can stand. However, he remains with mild dysarthria, dysmetria, dysdiadochokinesia, and bilateral cortical blindness. He has no fever or respiratory distress. We maintain treatment with Enoxaparin 40 mg daily and Acetylsalicylic Acid 100 mg per day. We began a rehabilitation program seeking to regain walking and coordination.
Case 2
A 51-year-old man admitted on April 29th for cough, fever, and dyspnea for a week. He had bilateral interstitial pneumonia with COVID-19 positive and admitted to the ICU. We started treatment with Hydroxychloroquine, Enoxaparin, and Methylprednisolone.
Blood analysis showed a pattern of a systemic inflammatory response (Table 1).
On day 4, he developed acute respiratory failure (SARS-CoV-2). On day 8, we observed a sudden onset left hemiplegia and hemineglect. The CT angiography showed occlusion in the M1 segment of the right middle cerebral artery (r-ACM) (Fig. 2A and B). Non-contrast CT revealed a slight loss of right frontoparietal cortical differentiation and petechial hemorrhage that contraindicated thrombolysis. We performed a mechanical thrombectomy 2 h after the onset, with complete reperfusion achieved (Fig. 2F–I).
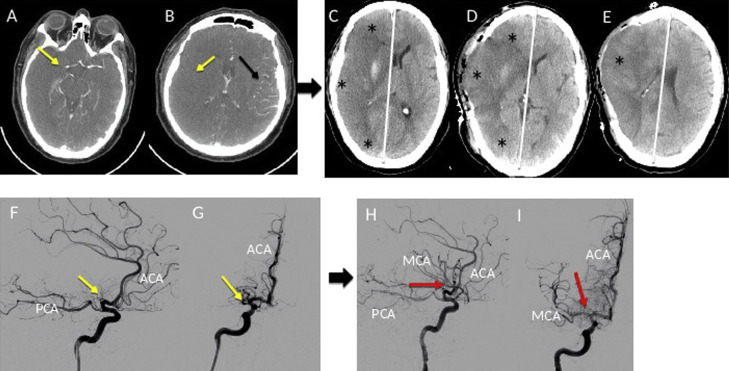
Fig. 2.
Malignant stroke. Right ACM obstruction. (A, B) CTA: Stop in M1 and absence of flow in the right insular region of the r-ACM (Yellow Arrow); contralateral normal flow (Black Arrow). (C) A malignant infarction (*) of the r-ACM that exerts midline deviation. (D, E) Right decompressive hemicraniectomy with an improvement of midline displacement. (F, G) Angiography: The absence of flow in the r-ACM. Thrombus in segment M1 (yellow Arrow). (H, I) Flow restored in r-ACM after thrombectomy (Red Arrow). CTA: CT-Angio, CT: Computerized Tomography, r-MCA: Right Middle Cerebral Artery, ACA (Anterior Cerebral artery), PCA (Posterior Cerebral Artery).
On day 9, the patient showed signs of intracranial hypertension. CT revealed a malignant infarction of r-ACM (Fig. 2C). We performed an extensive right decompressive hemicraniectomy, observing a severe cerebral infarction. Control CT showed no postoperative complications and confirmed an extensive ischemic stroke with a significant transcranial herniation (Fig. 2D and E). The patient is awake, ETI removed, mobilizes the right side of the body and obeys simple orders.
Decision making in these patients was based on clinical and radiological findings. Surgery was indicated as in other patients with this type of stroke. COVID-19 status did not influence the surgical decision. Face masks, face shields, and personal protective equipment were worn during surgery. COVID-19 test was still positive 48 h before surgery.
Discussion
In COVID-19 patients, a stroke secondary to a significant vessel obstruction is infrequent.5 Literature reports thrombotic events in patients with COVID-19.6 We hypothesize ischemic events result from a combined process: (1) A pro-inflammatory and procoagulant/coagulopathy state seen in COVID-19 patients. (2) Vascular endothelial dysfunction potentiated by hypoxia. (3) Hemodynamic instability and immobilization.1, 6, 7
The latter manifested as the elevation of parameters such as C reactive protein, ferritin, d-dimer, fibrinogen and cytokines (Table 1).1, 6, 7 However, we observe infrequently an obstruction of a large-vessel of brain circulation.5, 7
It is worth noting the development of thrombi in these patients despite the use of enoxaparin prophylaxis (40 mg/day) from the beginning in both patients, as in other cases.6 A pro-coagulant state in SARS-CoV-2 may be responsible for the cerebrovascular accident because of thrombus formation 5–7. The question remains whether the “prophylactic” dose in these patients should be higher than usual or to use another type of heparin.6
We believe that congenital hypoplasia of right vertebral artery and the anatomical absence of both posterior communicating cerebral arteries has possibly contributed to the development of a more extensive stroke given the lack of collateral circulation in case 1.
Rapid decompression (facilitated by the appearance of a stroke in the hospital in case1) has possibly played an essential role in preventing definitive damage to the brain stem, as in other stroke cases not related to COVID-198; possibly helping to his progressive neurological recovery, despite having presented bilateral mydriasis (case 1).
In both cases, mechanical thrombectomy did not allow to minimize the size of the stroke (both massive). We need further future clinical trials to test the efficacy of this technique in patients with SARS-CoV-2.
Conclusions
COVID-19 patients can develop large-scale ischemic strokes in previously healthy patients without risk factors.
The blockage of large arterial vessels, such as the vertebral artery, is possible. To the best of our knowledge, is the first reported case of partial obstruction of a vertebral artery in a patient with COVID-19. It is crucial to determine the type and dose of “prophylactic” heparin in these patients because of the potentially devastating sequelae, for which scientific studies are necessary.
The literature on the development of strokes in SARS-CoV-2 is still in development. We need more studies on the consequences of SARS-CoV-2 infection in the central nervous system and the appearance of neurological complications.
Decompressive surgery remains a life-saving maneuver in these patients (as in other non-COVID-19 strokes) and requires further investigation.
Acknowledgements
The authors thank Osman A. Salazar-Asencio (M.D.) for the editing and revision of the English language.
References
- 1.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang M., Zhou Y., Chang J., et al. Acute cerebrovascular disease following COVID-19: a single center, retrospective, observational study. SSRN Electron J. 2020 doi: 10.2139/ssrn.3550025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gabriel, Galán J.M.T. Ictus como complicación y como factor pronóstico de COVID-19. Neurología. 2020 doi: 10.1016/j.nrl.2020.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aggarwal G., Lippi G., Michael Henry B. Cerebrovascular disease is associated with an increased disease severity in patients with Coronavirus Disease 2019 (COVID-19): a pooled analysis of published literature. Int J Stroke. 2020 doi: 10.1177/1747493020921664. 1747493020921664. [DOI] [PubMed] [Google Scholar]
- 5.Oxley T.J., Mocco J., Majidi S., Kellner C.P., Shoirah H., Singh I.P., et al. Large-vessel stroke as a presenting feature of COVID-19 in the young. N Engl J Med. 2020 doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Klok F.A., Kruip M.J.H.A., van der Meer N.J.M., Arbous M.S., Gommers D.A.M.P.J., Kant K.M., et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020 doi: 10.1016/j.thromres.2020.04.013. S0049-3848(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Umapathi T., Kor A.C., Venketasubramanian N., Lim C.C., Pang B.C., Yeo T.T., et al. Large artery ischaemic stroke in severe acute respiratory syndrome (SARS) J Neurol. 2004;251:1227–1231. doi: 10.1007/s00415-004-0519-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ayling O.G.S., Alotaibi N.M., Wang J.Z., Fatehi M., Ibrahim G.M., Benavente O., et al. Suboccipital decompressive craniectomy for cerebellar infarction: a systematic review and meta-analysis. World Neurosurg. 2018;110 doi: 10.1016/j.wneu.2017.10.144. 450–59.e5. [DOI] [PubMed] [Google Scholar]