Introduction
Pyoderma gangrenosum is a rare, inflammatory, neutrophilic dermatosis that is a diagnosis of exclusion. We present a unique case of recalcitrant pyoderma gangrenosum attributable to levamisole-adulterated cocaine with variable, nonsustained responses to several systemic immunosuppressants and ultimate remission with oral tofacitinib.
Case report
A 64-year-old man with a history of chronic rhinosinusitis and cocaine abuse presented with a 10-month history of recurrent “boils” that worsened during periods of cocaine use. He was treated with several courses of antibiotics for presumed recurrent bacterial folliculitis but continued to develop new lesions. Two lesions were excised and appeared to heal briefly, but after several weeks, ulcerations occurred in the same areas, suggesting that pathergy was at play. He was referred to dermatology, and physical examination was notable for multiple exquisitely tender ulcerations involving the face, scalp, torso, arms, legs, and groin, measuring up to 10 cm. He denied skin picking. Ulcerations were deep into fat in many locations and characterized by undermined borders with gunmetal-gray rims, erythematous edematous surrounding skin, and purulence and fibrinoid exudate at the bases (Figs 1 and 2).
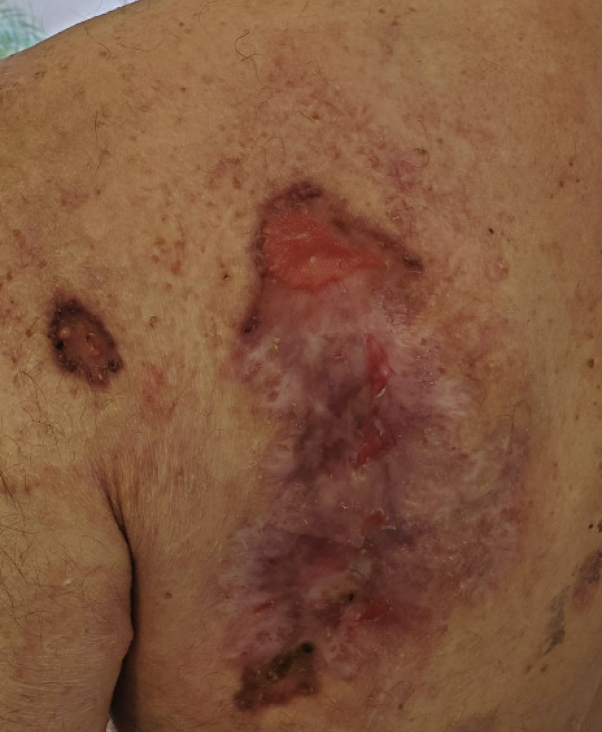
Fig 1.

On the patient's initial presentation, he had large, beefy, erythematous ulcers with violaceous undermined rims on his trunk and upper extremities (left upper portion of the back shown here).
Fig 2.
Patient's left shoulder at initial presentation, showing an ulcer with purulent exudate and violaceous undermined rim (pretreatment).
Histopathologic examination revealed dermal granulomatous and suppurative inflammatory infiltrates composed of lymphocytes, histiocytes, and multinucleated giant cells with extensive neutrophilic abscess formation and focal underlying fat necrosis without evidence of vasculitis or vasculopathy. Periodic acid–Schiff, acid-fast bacilli, and gram staining, as well as Treponema pallidum immunostaining were performed with negative results, and no polarizable material was identified. Tissue culture results for bacteria, fungus, and acid-fast bacilli were negative.
Systemic evaluation included chest radiography, hepatitis B serology, hepatitis C antibody, HIV antibody, Quantiferon Gold testing, erythrocyte sedimentation rate, antinuclear antibody, dilute Russell viper venom time, anticardiolipin antibodies, and antineutrophil cytoplasmic antibody. All results were negative or within normal limits except for a c-antineutrophil cytoplasmic antibody titer of 1:2560 and positive result for dilute Russell viper venom time (indicating the presence of lupus anticoagulant).
The combination of classic morphologic features, pathergy, histopathologic findings, and history of illicit drug use allowed a diagnosis of levamisole-adulterated cocaine-induced pyoderma gangrenosum to be rendered.
The patient was initially treated with oral prednisone (60 mg daily) with marginal improvement. Dapsone (100 mg daily) was added without significant benefit. Intravenous methylprednisolone (1000 mg daily for 3 days) was added. After initial improvement with the steroids, a prednisone taper was attempted, resulting in flaring of his disease. Infliximab infusions were initiated (5 mg/kg every 6 weeks). Because of suboptimal response, azathioprine was added (100 mg daily). The patient then transferred his care to a wound care specialist, who discontinued all his immunosuppressants and opted to pursue topical therapy. Several weeks later, he was admitted for adrenal insufficiency and intractable pain related to widespread eruption of cutaneous lesions. He received intravenous methylprednisolone (500 mg daily) for 3 days and began receiving cyclosporine (200 mg twice daily), with significant improvement. Maintenance prednisone (10 mg daily) was started for his adrenal insufficiency. Cyclosporine was stopped because of acute renal injury. In the interim, weekly urine drug screening was mandated in the setting of multiple failed treatment regimens and notable for cocaine metabolites. After a verbal agreement, including the initiation of weekly drug monitoring, the patient began receiving adalimumab (40 mg per week) and significant improvement was noted after 2 weeks. However, after an initial approximately 90% improvement with adalimumab, his lesions recurred. Oral tacrolimus (0.2 mg/kg/d, divided into 2 doses) was added. His prednisone was increased to 25 mg daily. The combination of adalimumab and tacrolimus proved ineffective. He was transitioned to rituximab (a series of 4 infusions dosed at 600 mg weekly). Rituximab was stopped because he developed a drug-induced exanthem with minimal improvement in the pyoderma gangrenosum. He was transitioned to oral tofacitinib (5 mg twice daily and up-titrated to 10 mg twice daily), with significant improvement after 2 weeks and sustained remission. At his last follow-up after 3 months of therapy, there was 95% improvement of his lesions with only focal superficial erosions in several of the larger lesions on his back attributable to continued friction (Figs 3 and 4). He is undergoing a prednisone taper and continues to have negative drug-screening results without recurrence of his pyoderma gangrenosum. He is currently receiving rivaroxaban for atrial fibrillation.
Fig 3.
Posttreatment, the patient's ulcers had healed except for focal areas of superficial erosion attributable to friction.
Fig 4.
Posttreatment photograph of the left shoulder.
Discussion
Levamisole-adulterated cocaine is now known to cause significant dermatologic complications and classically presents with retiform purpura and hemorrhagic bullae distributed on the extremities, face, and ears. These lesions are thought to be secondary to vasculitis and vasculopathy related to levamisole. Patients with these lesions are found to have positive immunologic titer results, including antinuclear, antiproteinase 3, antiphospholipid, and antineutrophil cytoplasmic antibodies.1
Recently, there have been an increasing number of reports of pyoderma gangrenosum secondary to levamisole-adulterated cocaine. In a case series of 8 consecutive patients, the authors highlighted the distinction between classic retiform purpura and pyoderma gangrenosum related to levamisole.2 In the series, pyoderma gangrenosum lesions involved primarily the upper and lower extremities. Histologically, the presence of a diffuse, dermal infiltrate of neutrophils, with or without necrosis and ulceration, was the unifying feature, which mirrors the pattern observed in conventional forms of pyoderma gangrenosum. In this cohort, the development of pyoderma gangrenosum lesions was temporally correlated to their last use of cocaine, with a median interval of 1 week after use with positive urine toxicology results for cocaine metabolites. All patients noted either improvement or stable disease with cocaine avoidance and supportive care.
Our case is unique in its protracted, recalcitrant, and remitting course requiring several different immunosuppressants with variable, nonsustained results and medication-related adverse effects. The recalcitrant nature was attributable to the patient's continued drug use, which was not halted until weekly urine toxicology screenings were established. Adalimumab has been used in other cases of pyoderma gangrenosum—specifically for patients with inflammatory bowel disorder—with significant improvement of these lesions, and is recommended as consideration for first-line treatment.3 After the patient's initial improvement with adalimumab followed by recurrence of his pyoderma gangrenosum, tofacitinib was chosen because it has also been used in other cases of pyoderma gangrenosum.4 This case highlights a rare, protracted course of an increasingly reported entity of levamisole-induced pyoderma gangrenosum that demonstrated significant initial improvement with multiple systemic immunosuppressants, and ultimately achieved remission with tofacitinib.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Pearson T., Bremmer M., Cohen J. Vasculopathy related to cocaine adulterated with levamisole: a review of the literature. Dermatol Online J. 2012;18(7):1. [PubMed] [Google Scholar]
- 2.Jeong H.S., Layher H., Cao L., Vandergriff T., Dominguez A.R. Pyoderma gangrenosum (PG) associated with levamisole-adulterated cocaine: clinical, serologic, and histopathologic findings in a cohort of patients. J Am Acad Dermatol. 2016;74(5):892–898. doi: 10.1016/j.jaad.2015.11.040. [DOI] [PubMed] [Google Scholar]
- 3.Agarwal A., Andrews J.M. Systematic review: IBD-associated pyoderma gangrenosum in the biologic era, the response to therapy. Aliment Pharmacol Ther. 2013;38:563–572. doi: 10.1111/apt.12431. [DOI] [PubMed] [Google Scholar]
- 4.Kochar B., Herfarth N., Mamie C. Tofacitinib for the treatment of pyoderma gangrenosum. Clin Gastroenterol Hepatol. 2019;17(5):991–993. doi: 10.1016/j.cgh.2018.10.047. [DOI] [PubMed] [Google Scholar]