Introduction
Green nail syndrome, also known as chloronychia, is a nail disorder characterized by greenish-black discoloration of the nail with onycholysis. Pseudomonas aeruginosa is known as the causative organism, and it mainly colonizes in an onycholytic nail in relation to green nail syndrome. Herein, we report a rare case of green nail syndrome with P oryzihabitans infection as an adverse event of nail art.
Case report
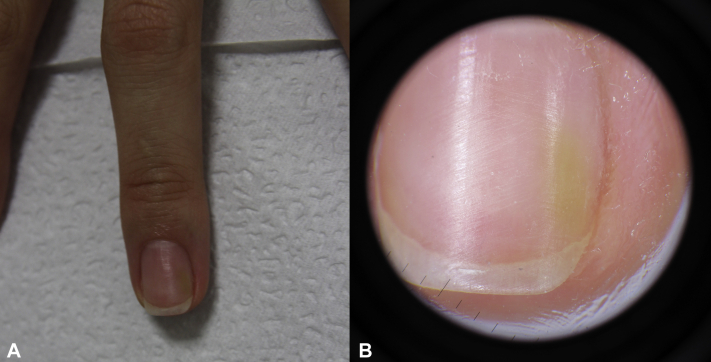
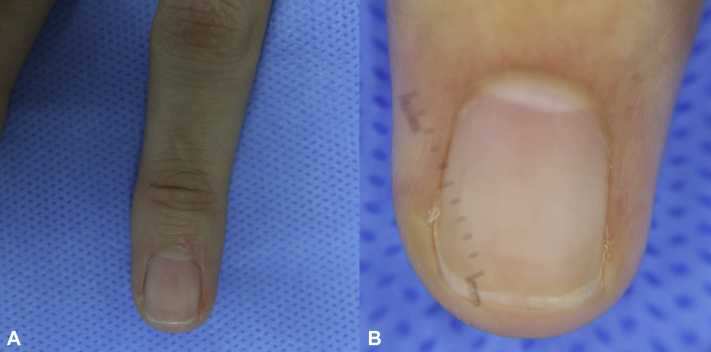
A 24-year-old healthy Korean woman presented with asymptomatic partial color change of the left third fingernail, which she had noticed shortly after removing gel nail polish 4 days earlier. She denied history of trauma or prolonged exposure to moist conditions. Physical examination and dermoscopy demonstrated light yellow-green discoloration of the middle to distal part of the left third fingernail adjacent to the lateral nail fold (Fig 1, A and B). Clinical findings suggested a diagnosis of green nail syndrome. Microorganism stain with culture was implemented, and she was empirically treated with topical nadifloxacin cream. Microorganism culture revealed ciprofloxacin-susceptible P oryzihabitans infection. At 2-month follow-up, the nail discoloration had resolved completely (Fig 2, A and B).
Fig 1.
Clinical (A) and dermoscopic (B) images showing light yellow-green discoloration of the left third fingernail at the initial visit.
Fig 2.
Clinical (A) and dermoscopic (B) images showing complete resolution at 2-month follow-up.
Discussion
Green nail syndrome is caused by an infection of the nails that leads to greenish discoloration of the nail plate with onycholysis.1 P aeruginosa, an aerobic gram-negative bacillus, is a common causative pathogen and its pigments, pyoverdine and pyocyanin, produce the chacteristic greenish hue in the nails.2 P aeruginosa preferentially colonizes in moist environments, and thus affected patients usually have a history of prolonged exposure to water. Other predisposing factors include onycholysis, onychotillomania, microtrauma to the nail fold, chronic paronychia, long-term exposure to soaps or detergents, and associated nail disorders, such as psoriasis.3
P oryzihabitans is a yellow-pigmented, gram-negative bacillus that can trigger sepsis, endophthalmitis, peritonitis, and bacteremia.4 It is an opportunistic pathogen, and thus individuals with major illnesses, including those undergoing surgery or with catheters, are vulnerable.4 To date, skin and soft tissue infections by P oryzihabitans have been reported in the literature5; however, nail infections have not been reported, to our knowledge. In the present case, the nail infection by P oryzihabitans manifested as a yellowish-green discoloration, clinically consistent with green nail syndrome. However, unlike dark green discoloration in typical green nail syndrome by P aeruginosa infection, the patient's nail exhibited a light yellow-green hue, consistent with the yellow pigment production by P oryzihabitans. Therefore, careful observation of the hue in discolored nails may aid in differentiating causative pathogens of green nail syndrome in clinical settings.
Nail art includes various nail cosmetics.6 In particular, nail gel requires specific ultraviolet light exposure to set and harden on the nail and hence has greater endurance. Consequently, gel nail polish can be removed only by completely buffing off the nail plate, which causes microtrauma. In the present case, considering the young age and healthy status of the patient, it was evident that removal of gel nail polish, or nail art in a broad sense, triggered green nail syndrome. Moreover, history of nail art is a significant risk factor for hand colonization of gram-negative rods, including Pseudomonas species.7 Therefore, health care workers, especially those who have frequent contact with immunocompromised patients, should be aware of the adverse effects of nail art and to avoid unintentional harm.
Treatment of green nail syndrome is challenging in many cases because recommendations based on well-designed clinical trials are absent. Treatment options include single or combination therapy with topical antiseptics; topical or, less often, systemic antibiotics; and surgical removal. Regarding topical antiseptics, chlorhexidine, 1% acetic acid, and 0.1% octenidine dihydrochloride solution are possible options, with 1% acetic acid recommended as the treatment of choice.1,8 When green nail syndrome is accompanied by pain, systemic antibiotics may be needed. Because most Pseudomonas species, including P oryzihabitans and P aeruginosa, are resistant to penicillin and the majority of related β-lactam antibiotics, an antibiotic susceptibility test should precede antibiotic use, and empirical antibiotics targeting Pseudomonas species should be prescribed: aminoglycosides, quinolones, carbapenems, antipseudomonal penicillins and cephalosporins, and others.4 In particular, topical tobramycin, topical nadifloxacin, and systemic ciprofloxacin have been reported to be valuable options.3,9,10 In the present case, topical nadifloxacin cream elicited excellent response.
In conclusion, we report a rare case of green nail syndrome most likely caused by P oryzihabitans infection as an adverse event of nail art. Possible adverse events of nail art should be relayed to the general population, especially health care workers, and pathogens other than P aeruginosa should be differentiated, especially in green nail syndrome showing atypical greenish hue.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Kang S. McGraw-Hill Education; New York, NY: 2019. Fitzpatrick's Dermatology. [Google Scholar]
- 2.Bennett J.E., Dolin R., Blaser M.J. Elsevier; Philadelphia, PA: 2019. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. [Google Scholar]
- 3.Rallis E., Paparizos V., Flemetakis A., Katsambas A. Pseudomonas fingernail infection successfully treated with topical nadifloxacin in HIV-positive patients: report of two cases. AIDS. 2010;24:1087–1088. doi: 10.1097/QAD.0b013e32833819aa. [DOI] [PubMed] [Google Scholar]
- 4.Lejbkowicz F., Belavsky L., Kudinsky R., Gery R. Bacteraemia and sinusitis due to Flavimonas oryzihabitans infection. Scand J Infect Dis. 2003;35:411–414. doi: 10.1080/00365540310012208. [DOI] [PubMed] [Google Scholar]
- 5.Tena D., Fernandez C. Pseudomonas oryzihabitans: an unusual cause of skin and soft tissue infection. Infect Dis (Lond) 2015;47:820–824. doi: 10.3109/23744235.2015.1034170. [DOI] [PubMed] [Google Scholar]
- 6.Madnani N.A., Khan K.J. Nail cosmetics. Indian J Dermatol Venereol Leprol. 2012;78:309–317. doi: 10.4103/0378-6323.95445. [DOI] [PubMed] [Google Scholar]
- 7.Moolenaar R.L., Crutcher J.M., San Joaquin V.H. A prolonged outbreak of Pseudomonas aeruginosa in a neonatal intensive care unit: did staff fingernails play a role in disease transmission? Infect Control Hosp Epidemiol. 2000;21:80–85. doi: 10.1086/501739. [DOI] [PubMed] [Google Scholar]
- 8.Rigopoulos D., Rallis E., Gregoriou S. Treatment of pseudomonas nail infections with 0.1% octenidine dihydrochloride solution. Dermatology. 2009;218:67–68. doi: 10.1159/000171816. [DOI] [PubMed] [Google Scholar]
- 9.Bae Y., Lee G.M., Sim J.H., Lee S., Lee S.Y., Park Y.L. Green nail syndrome treated with the application of tobramycin eye drop. Ann Dermatol. 2014;26:514–516. doi: 10.5021/ad.2014.26.4.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chiriac A., Brzezinski P., Foia L., Marincu I. Chloronychia: green nail syndrome caused by Pseudomonas aeruginosa in elderly persons. Clin Interv Aging. 2015;10:265–267. doi: 10.2147/CIA.S75525. [DOI] [PMC free article] [PubMed] [Google Scholar]